Abstract
BACKGROUND/OBJECTIVES:
The purpose of this study was to: (1) examine relationships between body mass index (BMI) stability and cognitive decline in older African Americans; and (2) investigate differences in the relationships between women and men.
DESIGN:
The present study is a secondary data analysis of the Minority Aging Research Study, which is a longitudinal, cohort study of risk factors for cognitive decline and Alzheimerʼs disease among older African Americans living in the Chicago, IL, area. The study entails annual clinical evaluations, including measures of 19 neuropsychological tests that represent five cognitive domains, including episodic, semantic, and working memory, perceptual speed, and visuospatial ability.
PARTICIPANTS:
Participants (n = 671; mean age = 73.5 years; standard deviation = 6.2 years) were included in the present analysis if they were dementia free at baseline and completed at least two clinical evaluations, on average 1 year apart, that included valid cognitive and BMI assessments.
RESULTS:
Mixed-effects models showed higher baseline BMI was related to slower global cognitive decline, whereas changes in BMI (instability) were related to faster global cognitive decline. These effects were the same for four of five cognitive domains and remained after controlling for various health characteristics. However, women and men did not differ in any of the relationships.
CONCLUSION:
Higher BMI is related to slower cognitive decline in older African Americans, but greater BMI instability is related to faster decline. Stability of BMI should be considered in the cognitive aging of African Americans. J Am Geriatr Soc 68:2662–2667, 2020.
Keywords: Blacks/African Americans, cognition, body mass index, obesity
INTRODUCTION
Obesity or adiposity has become a “public health crisis” in the United States.1 One in three adults is overweight,2 whereas nearly 40% are obese.1 Overweight/obesity is linked to increased risk for numerous chronic conditions, including cardiovascular diseases, such as atrial fibrillation, congestive heart failure, and stroke.3 Interestingly, obesity leads to more detrimental health effects in midlife than in old age. This has led some to refer to an “obesity paradox,”4 where there is an apparent “protective” effect of high adiposity for health, including cognitive decline, in late life.5–8 Obesity is most often measured by body mass index (BMI), and several studies have demonstrated being overweight (BMI = 25–29 kg/m2) or obese (BMI ≥ 30 kg/m2) in midlife is related to faster cognitive decline9,10 compared with overweight/obese in late life, which shows an inconsistent association with cognition. For example, some studies have demonstrated overweight/obesity is related to faster decline over time,10,11 slower decline in late life,5,7 or no relationship at all.12
African Americans are, on average, more likely to experience overweight/obesity. As a whole, African Americans are 1.4 times more likely to be obese relative to non-Latino White Americans.13 Statistics also show African American women have the highest rates overall, with 80% being overweight/obese.13 Despite the prevalence of obesity among African Americans, particularly African American women, few studies have examined the relationship between obesity and cognitive decline in this population. Among the longitudinal studies that have focused on race, most examine race differences7,12,14 between African Americans and non-Latino Whites and show that lower baseline BMI is related to faster cognitive decline7 or incidence of mild cognitive impairment and dementia.14 We are aware of one study that did not find a longitudinal effect of overweight and obesity on cognitive decline in a biracial population; rather, they reported better performance only at baseline and only among African Americans.12 One possible explanation for the discrepant results overall is the inattention to dynamic changes in weight and BMI over time that may influence cognitive status. Another consideration is the effect of sex, which is known to be associated with overweight/obesity. For example, men and women exhibit significant differences in obesity,15 with women having a larger prevalence of obesity than men, and studies that examine racial/ethnic differences in BMI and BMI change demonstrate that variation in weight changes exist primarily among women.16–18 However, despite known differences between men and women in BMI/obesity and changes in weight, we are unaware of any studies that examined the intersection of race and sex relating to cognitive decline in longitudinal analyses of dynamic weight changes.
The current study had two aims. First, we examined whether person-specific BMI fluctuations over several time points of BMI collected for each participant explain, in part, the paradoxical relationship between overweight/obesity and cognition, with a particular focus on older African Americans who disproportionately experience the overweight/obesity epidemic. Focusing exclusively on one of the cohorts from our previous report,7 we hypothesized that BMI stability, despite being overweight or obese, compared with dramatic changes in weight (i.e., rapid weight gain or loss) would explain the positive association of high BMI in late life with cognitive decline. Second, we investigated whether sex modifies the relation between BMI, BMI stability, and cognitive decline. We hypothesized that the relationship between BMI and decline would be stronger for women than men in this sample. Specifically, overweight/obese women would have slower cognitive decline than men after controlling for demographic and other relevant covariates. We also predicted that the relationship between BMI stability and cognitive decline would be stronger for women than men, with instability in BMI related to faster cognitive decline for women.
METHODS
Procedure
The Minority Aging Research Study (MARS) is a longitudinal cohort study of risk factors for cognitive decline and Alzheimerʼs disease in older adults who self-identify as African American and live in the metropolitan Chicago, IL, area. Details regarding the study design of MARS have been published previously.19
Participants
The present analytic sample included 671 participants who were dementia free at baseline and completed at least two cognitive assessments to examine change. Baseline sample characteristics are presented in Table 1. The Institutional Review Board of Rush University Medical Center approved the study, and all participants provided written informed consent.
Table 1.
Baseline Sample Characteristics by Sex
| Characteristic | Female (N = 513) | Male (N = 158) | Total (N = 671) |
|---|---|---|---|
| Age, mean (SD), y | 73.47 (6.34) | 73.37 (5.76) | 73.45 (6.20) |
| Education, mean (SD), y | 15.08 (3.41) | 14.86 (3.56) | 15.03 (3.44) |
| BMI, mean (SD), kg/m2 | 30.94 (6.89) | 28.97 (4.98) | 30.47 (6.54) |
| BMI range, mean (SD), kg/m2 | 3.27 (2.60) | 2.91 (1.90) | 3.18 (2.46) |
| Motor hand strength, mean (SD), lbs of pressure | 1.01 (0.25) | 1.00 (0.27) | 1.01 (0.25) |
| Vascular risk score, mean (SD) | 1.50 (0.83) | 1.66 (0.88) | 1.54 (0.85) |
| CES-D (10-item) score, mean (SD) | 1.37 (1.74) | 0.96 (1.40) | 1.27 (1.67) |
Note: BMI range = person-specific range average of the two largest values minus the average of the two lowest values during the study period. Mean number of BMI assessments = 6.69; SD = 3.62.
Abbreviations: BMI, body mass index; CES-D, Center for Epidemiological Studies Depression Scale; SD, standard deviation.
Clinical Evaluations
Clinical evaluations were conducted at baseline and thereafter on an annual basis. Annual follow-up evaluations were identical to the baseline evaluation in all essential details. These evaluations included a physical examination (including direct measurements of height, weight, and muscle strength), a detailed medical history, and neuropsychological assessment using a battery of 19 neuropsychological tests.19 After review of all clinical data, a clinician with expertise in the evaluation of persons with dementia classified each person with respect to dementia status, as previously described.7,20
Assessment of BMI
Height and weight were measured and recorded at each annual evaluation. BMI values were calculated by dividing weight (kilograms) by median height (meters) squared (kg/m2). BMI category group was defined based on Centers for Disease Control and Prevention criteria (2017): underweight BMI = 18.5 kg/m2; normal weight BMI = 18.6 to 24.9 kg/m2; overweight BMI = 25 to 29.9 kg/m2; and obese BMI = 30 kg/m2 or greater. To examine if departures from stable body mass over time contribute to changes in cognitive performance, we used the several time points of BMI data for each participant and calculated each person-specific BMI range.21 A range of person-specific BMI equal to zero represents a stable body mass, and values above zero represent departures from stable body mass.
Assessment of Cognitive Function
A battery of 19 cognitive function tests was administered annually to all participants. From the neuropsychological assessment, composite measures of global cognition and five cognitive domains were derived. There were seven tests of episodic memory, three tests of semantic memory, three tests of working memory, four tests of perceptual speed, and two tests of visuospatial ability. Both the global composite and the five domains were created by converting raw test scores to z scores using the baseline mean and standard deviation for the entire cohort. The z scores of individual tests were then averaged to yield each of the composite scores, as previously described.22
Demographic Variables and Relevant Covariates
Race was self-reported using 1990 U.S. Census categories. Age (years based on date of birth), sex (male or female), and self-reported years of education were collected at baseline.
Vascular risk factors (i.e., the sum of hypertension, diabetes mellitus, and smoking history) were assessed via a combination of self-report questions, clinical evaluation, and medication inspection. Each risk factor was given a score of 0 or 1 (absence vs presence) and summed to form a composite variable, resulting in a total score from 0 to 3. Higher scores indicated greater burden of vascular risk, as previously described.20
Depression symptoms were measured with the modified 10-item version of the Center for Epidemiological Studies Depression Scale.23 The 10-item version asks whether participants have experienced any of 10 depressive symptoms (e.g., I felt depressed; my sleep was restless) within the past week. The total score was a sum of the number of depressive symptoms and ranged from 0 to10. Two items were reverse coded (i.e., I was happy; I enjoyed life) to be consistent with depressed mood.
Motor hand strength was calculated as a composite score derived from two motor function tests: grip strength and pinch strength. Both measures (in pounds of pressure) were taken bilaterally using the Jamar Hydraulic Hand and Pinch Dynamometers (Lafayette Instruments). Participants were assessed twice with each hand, and the average of all four trials was computed. These scores were then transformed into z scores (separately for men and women) and included as a covariate in the analyses, as previously described.24
Statistical Analyses
Mixed-effects models were conducted to examine the relation of BMI to cognitive decline (global cognition and the five separate cognitive domains). The core models included terms for time on study, baseline BMI (centered at the mean value of 30 kg/m2), range of person-specific BMI (stability), and covariates (age, education, and sex), and all terms included interactions with time. Next, we conducted models that included a term for the interaction of sex and baseline BMI and the three-way interaction of sex, baseline BMI, and time, as well as interaction terms for sex by BMI range and sex by BMI range by time. These interaction terms were included to examine sex differences in the association of BMI and BMI range with cognitive performance and decline. Finally, we examined whether adjusting for vascular risk factors, depressive symptoms, or motor hand strength modified results. Analytic programming was done in SAS version 9.4 (SAS Institute Inc). Models were validated graphically and analytically.
RESULTS
BMI and Global Cognitive Decline
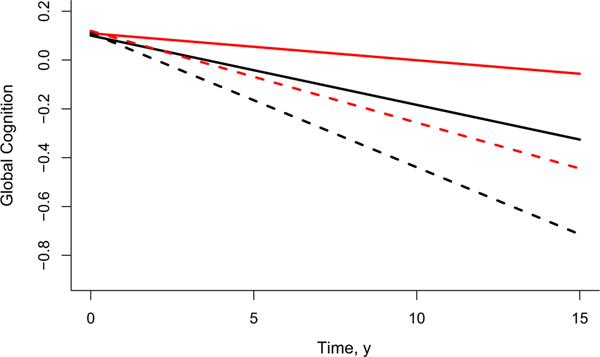
For global cognition, higher baseline BMI was related to slower cognitive decline (estimate = 0.002; standard error (SE) = 0.001; P = .0051), whereas higher person-specific BMI range was related to faster cognitive decline (estimate = −0.010; SE = 0.002; P < .0001). As shown in Figure 1, the additive effect of low BMI level at baseline and high BMI oscillation on global cognitive decline is illustrated for participants with low and high BMI level at baseline and person-specific ranges at the first and third quartiles. Estimates are from a linear mixed effect model that included terms for BMI and BMI range, controlling for age, sex, and education, and their interactions with time from baseline. These findings suggest that starting with a higher BMI at baseline offered protective benefit, whereas person-specific fluctuations in BMI were related to faster global cognitive decline (Table 2).
Figure 1.
Relations between high and low body mass index (BMI) at baseline and BMI stability at first and third quartiles on global cognitive decline. The additive effects of low BMI level at baseline and high BMI oscillation on global cognitive decline are illustrated for participants with a BMI level at baseline and person-specific range on the first and third percentiles. Estimates are from a linear mixed effect model, controlling for age, sex, and education, and their interaction with time from baseline. Black solid line: BMI level at baseline = 26.1 kg/m2 and BMI range = 1.5 kg/m2; red solid line: BMI level at baseline = 33.5 kg/m2 and BMI range = 1.5 kg/m2; black dashed line: BMI level at baseline = 26.1 kg/m2 and BMI range = 4.3 kg/m2; red dashed line: BMI level at baseline = 33.5 kg/m2 and BMI range = 4.3 kg/m2.
Table 2.
Relations Between BMI, BMI Range, and Decline Among Global Cognition and Cognitive Domains
| Variable | Global cognition estimate (SE), P value | Episodic memory estimate (SE), P value | Semantic memory estimate (SE), P value | Working memory estimate (SE), P value | Perceptual speed estimate (SE), P value | Visuospatial ability estimate (SE), P value |
|---|---|---|---|---|---|---|
| Age | −0.030 (0.003), <.0001 | −0.037 (0.004), <.0001 | −0.024 (0.004), <.0001 | −0.012 (0.004), .0054 | −0.043 (0.004), <.0001 | −0.021 (0.004), <.0001 |
| Sex | −0.075 (0.078), .3352 | −0.233 (0.097), .0169 | 0.113 (0.108), .2965 | 0.042 (0.117), .7195 | −0.242 (0.103), .0196 | 0.336 (0.114), .0033 |
| Education | 0.063 (0.005), .0001 | 0.045 (0.007), <.0001 | 0.082 (0.007), <.0001 | 0.061 (0.008), <.0001 | 0.077 (0.007), <.0001 | 0.061 (0.008), <.0001 |
| BMI | −0.000 (0.003), .8932 | 0.000 (0.004), .9192 | −0.007 (0.004), .1316 | 0.005 (0.005), .3424 | 0.001 (0.004), .7382 | −0.007 (0.005), .1151 |
| BMI range | 0.004 (0.008), .6397 | 0.001 (0.010), .6735 | 0.020 (0.011), .0781 | 0.003 (0.012), .8108 | −0.012 (0.011), .2673 | 0.005 (0.012), .6993 |
| Time | −0.001 (0.008), .8558 | 0.013 (0.010), .1921 | −0.005 (0.010), .5921 | 0.012 (0.008), .1564 | −0.039 (0.007), <.0001 | −0.002 (0.007), .8195 |
| BMI × time | 0.002 (0.001), .0051 | 0.003 (0.001), .0055 | 0.003 (0.001), .0035 | 0.002 (0.001), .0173 | 0.001 (0.001), .1481 | 0.001 (0.001), .1771 |
| BMI range × time |
−0.010 (0.002), <.0001 | −0.013 (0.002), <.0001 | −0.011 (0.002), <.0001 | −0.008 (0.002), <.0001 | −0.006 (0.001), .0001 | −0.003 (0.001), .0335 |
| Sex × BMI × time |
0.003 (0.002), .1193 | 0.003 (0.002), .2412 | 0.003 (0.002), .2603 | 0.002 (0.002), .1723 | 0.003 (0.001), .0633 | 0.000 (0.002), .8920 |
| Sex × BMI range × time | 0.006 (0.005), .2098 | 0.010 (0.006), .0930 | 0.008 (0.006), .1763 | 0.004 (0.005), .3900 | −0.002 (0.004), .6450 | −0.001 (0.004), .7866 |
Note: Mean number of cognitive assessments = 7.11; standard deviation = 3.67.
Abbreviations: BMI, body mass index; SE, standard error.
Next, we controlled for the effects of health covariates known to be associated with BMI and cognition: motor hand strength, depressive symptoms, and vascular risk factors. Adjusting for each of these factors separately did not change results for either baseline BMI or BMI range. Finally, in a sensitivity analysis to determine the robustness of the results, we used person-specific standard deviation of BMI instead of range. In this analysis, fluctuations of BMI with cognitive decline remained significant.
BMI and Separate Cognitive Domains
To determine whether BMI and BMI range were related to decline in certain cognitive domains but not others, we assessed change in five different cognitive domains (episodic memory, semantic memory, working memory, visuospatial ability, and perceptual speed). There were similar patterns of findings for each domain as with global cognition, except perceptual speed and visuospatial ability (Table 2). In these cases, baseline BMI was not significantly related to cognitive decline (perceptual speed estimate = 0.001; SE = 0.001; P = .1481; visuospatial ability estimate = 0.001; SE = 0.001; P = .1771).
BMI and Cognitive Decline as a Function of Sex
Next, we examined potential sex by BMI interaction effects by adding interaction terms that included sex to the core models. For global cognition, there were no significant three-way interactions between sex, baseline BMI, and time, or between sex, BMI range, and time (Table 2). That is, the effects of BMI and BMI range on global cognitive decline did not differ among women and men for the global composite (Table 2).
Regarding specific cognitive domains, sex did not modify the association of BMI or BMI range with decline in any domains (data not shown).
DISCUSSION
The purpose of this study was to examine relationships between BMI range or stability and cognitive decline and investigate differences by sex among a longitudinal sample of older African Americans. In support of our first hypothesis, results showed BMI stability was related to slower global cognitive decline. Contrary to our second hypothesis, sex did not significantly reduce the persistent protective effect of higher BMI on global cognitive decline or decline in any of the individual cognitive domains.
Previous literature on BMI and cognition has been mixed, with findings showing both detrimental and protective influences of overweight/obesity on cognition and other health outcomes.7,9 With regard to cognition, BMI has been associated with worse cognition in middle age,9,10 whereas in later life, associations have been more inconsistent: BMI in the overweight/obese ranges is often linked with better cognition.5–8 Given the importance of obesity for health in African Americans, we sought to fill gaps in the literature by focusing on this population, accounting for BMI stability, as well as testing interactions with sex. Among the few longitudinal studies examining racial differences between African American and White participants, one longitudinal study found a curvilinear relationship between BMI and cognitive performance.12 Being underweight was related to lower baseline cognitive scores, whereas being overweight and obese were related to better baseline cognitive performance, although among African American participants only.12 Further, higher BMI was related to slower cognitive decline over 6 years12; however, after excluding individuals with Mini-Mental State Examination scores of less than 24, the effect was no longer statistically significant. Another study, which included many participants in this study, showed that lower baseline BMI was related to faster cognitive decline.7 This previous study combined the MARS sample with the Rush Memory and Aging Project (predominately White) and found no racial differences in relations between BMI and cognitive decline. Given the persistent race-related health disparities in obesity and dementia in the United States, we wanted to understand within-group variability among the MARS sample.
Overall, our pattern of results supports the documented “obesity paradox,” where higher BMI and weight status may offer cognitive benefits,9 especially in later life.25 One explanation offered is that BMI does not reliably capture health effects due to differences in adiposity and lean muscle mass.26 For instance, an individual may have a BMI in the obese range due to high lean muscle mass, which is related to better health status, but not have fat mass. To test this possibility, we controlled for motor hand strength in our models. However, upper extremity strength, at least as measured in this study, did not explain the effect of BMI. We also explored depressive symptoms and vascular risk factors, known to be associated with obesity and cognitive outcomes; however, controlling for these factors did not account for the effect of BMI on cognitive decline either.
An additional goal was to explore alternative explanations for the “obesity paradox” among African Americans, because so few studies have included and focused on this population for this line of research. One explanation we tested was the extent to which fluctuations in a personʼs weight status might account for the relationship of BMI to cognitive changes. We did this by calculating the range of person-specific BMI, defined as the difference between the average highest BMI and the average lowest BMI21 (e.g., a difference of “zero” represents stability). Previous studies have used BMI as a continuous or categorical variable, or both; however, our study appears to be the first to also account for the range of BMI in the same model with baseline BMI. Stability of BMI was important in the sample, as BMI instability was related to faster cognitive decline, independent of baseline BMI.
Alternatively, the effect of BMI on cognitive decline may be driven by sex differences. Surprisingly, there is a dearth of research focusing on sex differences among cohorts 65 years and older. Women are on average heavier than men in late life, and African American women have the highest BMI overall among their race/sex counterparts.13 Women also tend to have greater variations in weight change.14–16 Despite these known differences in BMI and change in BMI between women and men, we did not find that sex modified the association of either with cognitive decline or decline in specific cognitive domains. But our sample had more women than men, a typical pattern in studies of aging because of differences in longevity between men and women, and power to detect sex differences could be limited. Future studies with higher numbers of African American men are needed to investigate sex differences in the effects of BMI on cognitive change.
Study Strengths and Limitations
This study has important strengths. First, these data are from a large, longitudinal cohort with comprehensive data across five separate cognitive domains. Second, BMI was objectively measured annually, allowing us to conduct mixed effects models that reliably measured changes in BMI over an average of 6 years. Third, we included data on muscle strength and vascular risks shown in previous studies to be associated with BMI and cognition. It is also important to note study limitations. First, the only available adiposity variable was BMI, which may not be as sensitive to cognitive changes as central adiposity measurements (i.e., waist circumference and waist/hip ratio). Central adiposity measures tend to be more sensitive than BMI, especially for older adults.27 Second, we did not examine frailty in the study. Given that hypertension, diabetes mellitus, and prediabetes (glucose intolerance), when coupled with diminishing grip strength and unintentional weight loss, may be indicative of a frailty syndrome, we were likely underpowered to examine frailty due to low numbers of persons who were underweight or progressed to underweight. Finally, like other aging cohorts, the sample was predominantly female, potentially limiting power to detect sex differences in the relation of BMI and BMI range with cognitive decline.
Conclusions and Future Study
Overall, the present study suggests higher BMI is related to slower cognitive decline, but greater BMI fluctuations are related to faster cognitive decline among an older cohort of African Americans. These results extend the previous literature in important ways, including examining BMI as a time-varying predictor to model the effects of weight changes. As this study focused on cognitive function, future research should investigate how dynamic changes in BMI relate to the clinical syndromes of mild cognitive impairment and dementia among African Americans. Future investigation may also consider unintentional weight loss, regardless of baseline weight, as weight loss is a feature of dementia. Clinicians may choose to monitor weight stability for early detection of changes and possible recommendations to patients about setting healthy weight goals and other measures to maintain brain health. Furthermore, future research should take a lifespan approach to understand the nature of BMI as a risk for cognitive decline, considering the evidence for midlife obesity increasing the risk of future dementia. By investigating these questions, this line of work will help address persistent health disparities in obesity and dementia outcomes that affect African American adults.
ACKNOWLEDGMENTS
The Minority Aging Research Study was funded by National Institute on Aging (NIA) Grant RF1AG22018 (principal investigator (PI): Barnes). A.A.M. was supported by an NIA Diversity Supplement Award 3RF1AG022018–11S2 (PI: Barnes). Drs Arvanitakis and Capuano are funded in part by R01 NS084965 and RF1 AG059621.
Sponsor’s Role: The sponsor (National Institutes of Health) provided funding for the study but did not have a role in the design, methods, participant recruitment, data collection/analysis, or preparation of the manuscript.
Footnotes
Financial Disclosure: This work was supported by the National Institute on Aging (RF1AG22018 and 3RF1AG022018–11S2; principal investigator (PI): Barnes; R01 NS084965 and RF1 AG059621; PI: Arvanitakis).
Conflict of Interest: There are no conflicts of interest.
REFERENCES
- 1.Blumenthal D, Seervai S. Rising obesity in the United States is a public health crisis, to the point, the Commonwealth Fund (Online). https://www.commonwealthfund.org/blog/2018/rising-obesity-united-states-public-health-crisis. Accessed June 27, 2018.
- 2.OECD (Online). Organisation for economic co-operation & development. http://www.oecd.org/health/obesity-update.htm. Accessed June 27, 2018.
- 3.Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;37(12):e67. [DOI] [PubMed] [Google Scholar]
- 4.Braun N, Gomes F, Schutz P. “The obesity paradox” in disease–is the protective effect of obesity true? Swiss Med Wkly. 2015;145:w14265. [DOI] [PubMed] [Google Scholar]
- 5.Luchsinger JA, Biggs ML, Kizer JR, et al. Adiposity and cognitive decline in the cardiovascular health study. Neuroepidemiology. 2013;40(4):274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim S, Kim Y, Park SM. Body mass index and decline of cognitive function. PLoS One. 2016;11(2):e0148908. 10.1371/journal.pone.0148908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arvanitakis Z, Capuano AW, Bennett D, Barnes LL. Body mass index and decline in cognitive function in older black and white persons. J Gerontol A Biol Sci Med Sci. 2017;73(2):198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim G, Choi S, Lyu J. Body mass index and trajectories of cognitive decline among older Korean adults. Aging Ment Health. 2019;24:758–764. 10.1080/13607863.2018.1550628. [DOI] [PubMed] [Google Scholar]
- 9.Baumgart M, Snyder HM, Carrillo MC, Fazio S, Kim H, Johns H. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective. Alzheimers Dement. 2015;11(6): 718–726. [DOI] [PubMed] [Google Scholar]
- 10.Gunstad J, Lhotsky A, Wendell CR, Ferrucci L, Zonderman AB. Longitudinal examination of obesity and cognitive function: results from the Baltimore longitudinal study of aging. Neuroepidemiology. 2010;34(4):222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hassing LB, Dahl AK, Pedersen NL, Johansson B. Overweight in midlife is related to lower cognitive function 30 years later: a prospective study with longitudinal assessments. Dement Geriatr Cogn Disord. 2010;29(6): 543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sturman MT, de Leon CM, Bienias JL, Morris MC, Wilson RS, Evans DA. Body mass index and cognitive decline in a biracial community population. Neurology. 2008;70(5):360–367. [DOI] [PubMed] [Google Scholar]
- 13.National Center for Health Statistics. Health, United States, 2016: with chartbook on long-term trends in health (Online). Hyattsville, MD; 2017. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=25. Accessed June 27, 2018. [PubMed] [Google Scholar]
- 14.Gao S, Nguyen JT, Hendrie HC, et al. Accelerated weight loss and incident dementia in an elderly African-American cohort. J Am Geriatr Soc. 2011; 59(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Link JC, Reue K. Genetic basis for sex differences in obesity and lipid metabolism. Annu Rev Nutr. 2017;37:225–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walsemann KM, Ailshire JA. BMI trajectories during the transition to oldera dulthood: persistent, widening, or diminishing disparities by ethnicity and education? Res Aging. 2011;33(3):286–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baltrus PT, Lynch JW, Everson-Rose S, Raghunathan TE, Kaplan GA. Race/ethnicity, life-course socioeconomic position, and body weight trajectories over 34 years: the Alameda County study. Am J Public Health. 2005; 95(9):1595–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kahn HS, Williamson DF. Is race associated with weight change in US adults after adjustment for income, education, and marital factors? Am J Clin Nutr. 1991;53:1566S–1570S. [DOI] [PubMed] [Google Scholar]
- 19.Barnes LL, Shah RC, Aggarwal NT, Bennett DA, Schneider JA. The minority aging research study: ongoing efforts to obtain brain donation in African Americans without dementia. Curr Alzheimer Res. 2012;9:736–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bennett DA, Buchman AS, Boyle PA, Barnes LL, Wilson RS, Schneider JA. Religious orders study and Rush memory and aging project. J Alzheimers Dis. 2018;64(s1):S161–S189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Capuano AW, Wilson RS, Leurgans SE, Dawson JD, Bennett DA, Hedeker D. Sigmoidal mixed models for longitudinal data. Stat Methods Med Res. 2018;27(3):863–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson RS, Barnes LL, Kreuger KR, Hoganson G, Bienias JL, Bennett DA.Early and late life cognitive activity and cognitive systems in old age. J Int Neuropsychol Soc. 2005;11:400–407. [PubMed] [Google Scholar]
- 23.Buchman AS, Wilson RS, Yu L, Boyle PA, Bennett DA, Barnes LL. Motor function is associated with incident disability in older African Americans. J Gerontol A Biol Sci Med Sci. 2016;71(5):696–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 25.Skinner JS, Abel WM, McCoy K, Wilkins CH. Exploring the “obesity paradox” as a correlate of cognitive and physical function in community-dwelling black and white older adults. Ethn Dis. 2017;27(4): 387–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abramowitz MK, Hall CB, Amodu A, Sharma D, Androga L, Hawkins M. Muscle mass, BMI, and mortality among adults in the United States: a population-based cohort study. PLoS One. 2018;13(4):e0194697. 10.1371/journal.pone.0194697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luchsinger JA, Patel B, Tang MX, Schupf N, Mayeux R. Measures of adiposity and dementia risk in elderly persons. Arch Neurol. 2007;64(3): 392–398. [DOI] [PMC free article] [PubMed] [Google Scholar]