Abstract
Background
Marketing of unhealthy foods and beverages is recognized as a contributing factor to the global increase in overweight and obesity, particularly among children. Such marketing negatively affects children’s dietary preferences, food choices, purchasing requests, and consumption patterns. Given that little is known about food marketing in Africa, including in Uganda, monitoring children’s exposure to food marketing is essential to generate evidence on the problem and develop meaningful policy responses. The aim of this study was to describe the food and beverage marketing environment surrounding schools in urban and peri-urban areas of Kampala city.
Methods
Outdoor advertising around 25 randomly sampled primary and secondary schools within a radius of 250 m of each school was mapped. Information on size, setting, type, and position of the advertisements and the healthiness of the foods and beverages promoted was collected using the INFORMAS Outdoor Advertising Protocol. The occurrence of advertising was described using frequencies, median, and density per 100m2.
Results
A total of 1034 branded advertisements were identified around the schools. Of these, 86% featured unhealthy products, 7% healthy products, and 7% miscellaneous products. The most advertised products were sugar-sweetened beverages and alcoholic beverages (51 and 23%, respectively). Schools in the urban area were surrounded by more unhealthy ads than those in the peri-urban areas (median of 45 vs 24 advertisements).
Conclusion
The widespread extent of unhealthy food and beverage advertisements around primary and secondary schools highlights the need for food marketing regulation in Uganda, in line with the World Health Organization’s recommendations, to ensure that young people are protected from unhealthy food marketing.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-10661-8.
Keywords: Food marketing, Outdoor food advertising, Unhealthy foods, Sugar-sweetened beverages, Alcoholic beverages, Primary and secondary schools
Introduction
Childhood obesity has become one of the most pressing public health concerns of the twenty-first century [1]. Overweight in children under five is rising in most of the regions of the world [2], exposing them to a greater risk of obesity and diet-related non-communicable diseases as young adults [3]. There is a particular increase in overweight and obesity among school-aged children between 5 and 19 years, with the prevalence having increased tenfold in the last four decades and most rapidly in urban settings in low- and middle-income countries [1, 4, 5].
Among the contributing factors to the global increase in childhood obesity is the marketing of energy-dense, nutrient-poor foods and beverages [6–9]. Children represent a key target for the marketing of food and beverage products [10]. It is well known that marketing of unhealthy foods and beverages (i.e. foods high in sugar, salt, saturated fat and/or trans-fat) can affect children’s dietary preferences, purchasing requests and consumption patterns [6–9], and consequently encourage unhealthy dietary practices [11] which in turn can contribute to rapid weight gain in early childhood [12]. Growing evidence suggests that the vulnerability to, and negative impact of, unhealthy food marketing is not limited to young children, but extends to adolescents [13]. A global study benchmarked children’s exposure to television advertising of unhealthy foods and beverages across 22 countries and found that children are exposed to a large volume of television advertising of unhealthy foods [14]. Similarly, studies have consistently shown that most outdoor food advertisements (ads) are featuring unhealthy foods and beverages [12, 15–18]. Examples of such ads are branded billboards, posters or banners (free-standing/attached, painted or digital), and store merchandise. However, information on the prevalence of outdoor food and beverage advertising in low- and middle-income countries is still limited [9].
During the last 30 years, food companies have increasingly targeted markets in low- and middle-income countries, resulting in the introduction of highly processed foods to the domestic food supply [19–21]. Food marketing is one underlying driver of the worldwide nutrition transition characterized by a shift in dietary patterns from hitherto low fat, low sugar, and high fiber diets to diets that are rich in saturated fat, refined sugars, and low in fiber [22]. Correspondingly, several low- and middle-income countries, including Uganda, are fighting with persistent problems of undernutrition, stunting, and wasting while concurrently experiencing a rapid rise in overweight, obesity, and diet-related non-communicable diseases [23].
The increase in overweight and obesity among children and adolescents in sub-Saharan Africa has been described as alarming but varying from country to country [24]. While there is limited data on the national prevalence of overweight and obesity among school-aged children in Uganda [25–29], modelled estimates indicate a steep increase in overweight among children aged 5–19 years during the timeframe 2001 to 2016 [30, 31].
Given that Uganda has been classified as in the early stage of nutrition transition [32], there may be a “window of opportunity” to implement internationally agreed, knowledge-based prevention measures that support healthy diets at the population level, in particular among children. In the context of food marketing, such measures have been recognized at the World Health Assembly, with Member States having agreed on a set of non-binding recommendations to restrict such unhealthy food and beverage marketing to children [33].
The World Health Organization (WHO) has recommended that national governments should monitor children’s exposure to, and the persuasive power of, food and beverage marketing messages. The exposure is defined as the reach and frequency of the message, while power is defined as the creative content, design, and execution of the marketing message [33, 34]. Furthermore, the WHO underscores the importance of developing a consistent system for monitoring food and beverage marketing within a country over time and enabling comparison between countries. Such monitoring is essential to determine appropriate and effective policy responses both in a global, national, and local perspective [33].
In light of the evidence linking marketing of products that are high in fat, salt and sugar to childhood obesity, there is also an increasing recognition that countries should, as part of their duties under international human rights law [35, 36], restrict unhealthy food marketing to reduce its negative impact on children, and to realize their rights to health and to adequate food [13, 37].
In Uganda, whereas there are relevant policies on food and nutrition in place, there are presently no specific policy and regulations being implemented with regard to regulating food and beverage marketing. There is also no mechanism in place to monitor and safeguard children’s exposure to food and beverage marketing. Given this knowledge gap, we aimed to map the outdoor food and beverage advertising environment, in terms of extent and power, around selected schools in the capital of Uganda, Kampala.
Methods
Study design and setting
The study was carried out in two out of five divisions of Kampala, namely Kampala Central Division and Kawempe Division. Data was obtained in late 2018. The methodology of the International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support framework (INFORMAS) which has been used for similar studies, was applied to investigate the extent and power of the marketing of unhealthy foods and beverages to children. INFORMAS is an independent entity whose work is complementary to monitoring efforts of the WHO, to strengthen the accountability systems needed to help reduce the burden of obesity, NCDs and their related inequalities [38, 39]. The framework provides ten modules including one for monitoring and benchmarking food and beverage promotion [38, 39]. The Outdoor Advertising Protocol of the INFORMAS’ module on food promotion [40] guided the conceptualization of this study. The study was part of a larger project which also included qualitative approaches to explore national policymakers’ perspectives on unhealthy food marketing; the qualitative part will be reported in a separate publication.
Sampled sites
This study included 13 primary schools and 12 secondary schools which covered children in the age group 6–19 years. Considering the number of schools that have been included in previous similar studies in high-income [17] and low- and middle income [41, 42] countries, and taking into account the explorative nature of the study, twenty-five schools were deemed to be a reasonable sample size. Since the term ‘child’ covers all children and adolescents under the age of 18 years [3, 33, 43], it was essential to include both primary and secondary schools in this study. Both day schools, and mixed day and boarding schools were included. Boarding schools were excluded since children attending these schools were encamped and not allowed to go outside the school area during the semester; thus, they were not usually exposed to outdoor food marketing.
The sample of schools was selected through a multi-stage sampling approach following the Outdoor Advertising Protocol [40]. In the first stage of sampling, the most urban division, and a less urban [hereinafter called peri-urban] division of Kampala were selected: Kampala Central Division and Kawempe Division, respectively. Kampala Central is the smallest division in Kampala District, located in an urban area, the city center, while Kawempe is the largest division, located in the Northern part of Kampala District, and is a more peri-urban area with a lower population density and income level than Kampala Central. Separate lists of primary and secondary schools in each of the two divisions were generated following a mapping and listing exercise using information available from the Directorate of Education and Social Services at Kampala Capital City Authority (KCCA). In the second stage of the sampling, 7 out of 25 primary schools in Kampala Central, and 6 out of 56 primary schools in Kawempe were selected from the lists of primary schools using the simple random number generator in Microsoft Excel. The same process was followed for secondary schools where 6 out of 8 secondary schools in Kampala Central and 6 out of 25 secondary schools in Kawempe were randomly selected. Of the sampled schools, however, nine were either permanently closed, not locatable, or located outside the division boarder. Consequently, an equal number of schools were replaced by selecting the following school on the respective list. The study involved no human subjects.
Data collection
For each school, an electronic map was generated with circles to indicate a radius of 250 m from the entrance/boundary of the school, with the use of Map Developers [44]. The radius of 250 m around the schools is in accordance with the INFORMAS protocol [40], and has been used in other comparable studies [17, 41]. These studies have however also included an additional 500 m radius around schools, whereas a study from Mexico used a 100 m radius [42].
The maps were printed and used manually during the data collection. The Outdoor Advertising Protocol’s standard template [40] was used to record the ads. For each advertisement, information was collected on:
-
i)
The distance of the food/beverage advertisement from school (within 250 m).
-
ii)
The size of the advertisement (small (21 cm × 30 cm - 1.3 m × 1.9 m), medium (> 1.3 m × 1.9 m - 2.0 m × 2.4 m), large (≥ above 2 m × 2.5 m).
-
iii)
The setting of the advertisement (food shop, roads, building, bus shelter, train station, cart/stall).
-
iv)
The type and position of the advertisement (billboard, poster, free-standing, painted, digital/LED, store merchandising).
-
v)
Whether the subject of the advertisement was for single or multiple foods and beverages.
-
vi)
The food/beverage brand name(s) and product type(s).
-
vii)
Major food category (core/healthy, non-core/unhealthy, miscellaneous).
-
viii)
Minor food category (e.g. sugar-sweetened beverages, alcoholic beverages, savoury food snacks, healthy food snacks, water, baby foods, baby and toddler milk), divided into 37 food categories [40].
-
ix)
Any promotional character and premium offers.
Three locally recruited public health nutritionists with at least a bachelor’s degree qualification were hired and trained to assist in the data collection processtogether with the first author (EWD). The data was recorded manually, and each sample site was visited once. The school zones were cross-checked to ensure that all ads in every street and corner were included. The data collection was completed within two weeks, to ensure that all ads were recorded in the same time period, and thus, limiting the risk of any seasonal fluctuations that occur in advertising frequency and power of exposure over a year cycle.
Coding
The ads were coded by the first author (EWD) on the day of data collection. An ‘advertisement’ was defined as a sign with branded information, pictures, or logos for food or beverage products or companies. This included billboards, posters, free-standing signs, neon signs, stickers, electronic boards, banners, bus shelter signs and signs on outdoor furniture, bridge/awning signs, and painted buildings. Store signages that also had a product logo and served not just as a store identifier but also as promotional material for a product were considered ads. Ads smaller than A4 size, signage used mainly for store identification, and pictures of unbranded restaurant foods or other foods were excluded from the study. All A-frame double-sided bus shelters and standing signs where ads appeared on two sides with different content on each side were identified and coded separately to ensure that accurate information was collected.
An advertisement was considered ‘unhealthy’ when at least one food product in the advertisement was categorized as unhealthy following the Outdoor Advertising Protocol and the WHO nutrient profiling model [45, 46].
Data analyses
Data was imported into IBM SPSS for Windows version 24 (SPSS Inc., Chicago, IL.). The schools were divided into tertiles of school fee, as an indicator of the school’s socio-economic status. Additionally, the schools were classified into government-funded schools and private schools to serve as another proxy of socio-economic status. The rationale behind this was that private schools have fee structures that some families from low-income groups may not fully afford, while government-funded schools have lower school fees [47].
The density of ads within a radius of 250 m (school zone) was calculated (ads per 100 m2). For each site, descriptive analyses were conducted to determine the frequency, median, and density of food ads by product type and content, setting and size, school areas (divisions), school types (primary and secondary), school fees (low, medium, and high) and school categories (government-funded and private). Non-parametric tests were used since the data was not normally distributed [48]. Mann-Whitney U test was used to compare two independent groups, and Kruskal-Wallis test to compare three independent groups. The statistical significance level was set at α < 0.05 for all analyses.
Henceforth, the term “food” in this paper, is used to refer to foods and beverages.
Results
Characteristics of the study population
The sample consisted of 13 primary schools and 12 secondary schools. Table 1 presents the total number of schools by type, category, fee structure respectively, and the number of schools distributed by urban and peri-urban areas.
Table 1.
Characteristics of the study units
| Total schools | Schools in Kampala Central Division (urban) | Schools in Kawempe Division (peri-urban) | |
|---|---|---|---|
| School characteristics | n | n | n |
| School type | |||
| Primary schools | 13 | 7 | 6 |
| Secondary schools | 12 | 6 | 6 |
| School category | |||
| Government-funded schools | 9 | 8 | 1 |
| Private schools | 16 | 5 | 11 |
| School fee | |||
| Low school fee | 9 | 6 | 3 |
| Medium school fee | 8 | 4 | 4 |
| High school fee | 8 | 3 | 5 |
| Total | 25 | 13 | 12 |
Description of the advertised foods and beverages
The study mapped 1034 branded ads around 25 schools (Table 2). Most of the adverts were for unhealthy foods and beverages (86%), 7% were for healthy foods and 7% were for miscellaneous foods (tea/coffee/condiments). The most frequently advertised food products were sugar-sweetened beverages (51% of all ads), followed by alcoholic beverages (23%) and high fat and/or sugar flavoured dairy products (5%). The number of ads varied between the schools, of which the majority ranged between 20 to 70 adverts (Supplementary Table 1, Additional file 1). There was an almost absence of infant formula advertising (n = 9, 1% of the total ads (Table 2).
Table 2.
Type and frequency of promoted foods and beverages around the schools (% of total ads)
| Major and minor food categoriesa | Number | Percent |
|---|---|---|
| Healthy foods | 85 | 7 |
| Bottled water | 31 | 3 |
| Healthy oils and low-fat savory sauces | 21 | 2 |
| Staple foods/plain starch products | 12 | 1 |
| Low-fat dairy and dairy alternatives, and drinks | 11 | 1 |
| Meat and meat alternatives | 4 | 0 |
| Low sugar, high fiber cereals | 2 | 0 |
| Fruit/fruits products without added sugar | 2 | 0 |
| Healthy snacks | 2 | 0 |
| Unhealthy foods | 887 | 86 |
| Sugar-sweetened beverages | 522 | 51 |
| Alcohol | 233 | 23 |
| High fat and/or sugar flavoured dairy products | 56 | 5 |
| Chocolate and candy | 25 | 2 |
| Fast food | 15 | 2 |
| Savoury snack food | 9 | 1 |
| Other high fat/salt products | 9 | 1 |
| Sweet breads, biscuits, pies, and pastries | 6 | 1 |
| Ice cream and desserts | 3 | 0 |
| Fruit juice/drinks (< 98%) | 3 | 0 |
| Sugar-rich, low fiber cereals | 3 | 0 |
| Ultra-processed meat and meat alternatives | 2 | 0 |
| Miscellaneous | 62 | 7 |
| Condiments, seasonings and recipe additions | 47 | 5 |
| Baby and toddler milk formulae | 9 | 1 |
| Vitamin or dietary supplements | 4 | 1 |
| Tea and coffee | 2 | 0 |
| Total | 1034 | 100 |
a Major food categories (in bold): healthy/unhealthy/miscellaneous. Minor food categories: the type of food product advertised under their respective major food category
Types of advertised foods and beverages
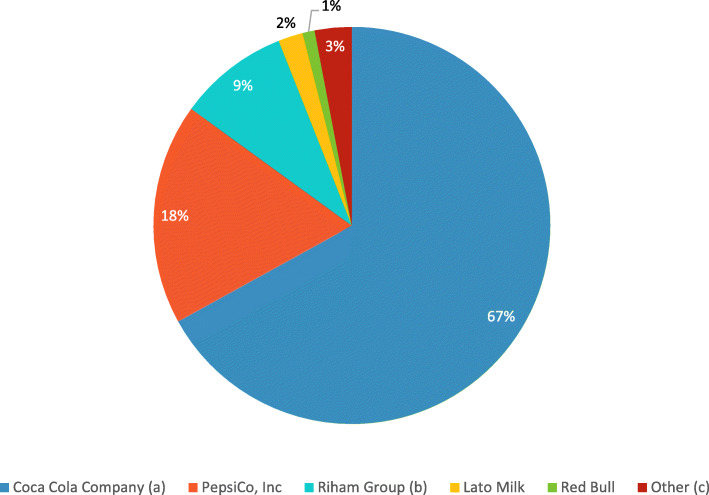
Eighty-eight percent of the schools were predominantly exposed to sugar-sweetened beverage ads, followed by alcoholic beverage ads (Supplementary Table 2, Additional file 1). A total of 115 different companies were identified as advertisers in the study. Of these companies, Coca-Cola Company, PepsiCo Ink, and Uganda Breweries Ltd. accounted for 35%, 9%, and 9% of the ads surrounding schools, respectively. Within the sugar-sweetened beverages category, Coca Cola accounted for 67% of the ads (Fig. 1).
Fig. 1.
The proportion of sugar-sweetened beverages by advertising companies. a Excluding Coca-Cola ads promoted with fast foods. Instead, the nine ads where Coca Cola and fast food was combined in one ad were coded as minor food category 22 titled “fast food”. b Riham Group under Hariss International Limited. c Companies that in total accounted for less than 1 % of the sugar-sweetened advertisements fell under the category titled “other”
Food and beverage advertisements by setting and display type
In terms of setting, half of the ads were on buildings (51%), followed by food shops (32%) and roads (13%). Less commonly marketing settings were mobile charts, stalls or vending machines (4%) and bus shelters (2 ads). By display type, almost two-thirds of the ads were posters or banners (66%), followed at by-store merchandising (15%), free-standing signs/signage (11%), painted building/wall (6%), billboards and digital signs or LED (1% in both).
Food and beverage advertisements by urban and peri-urban areas
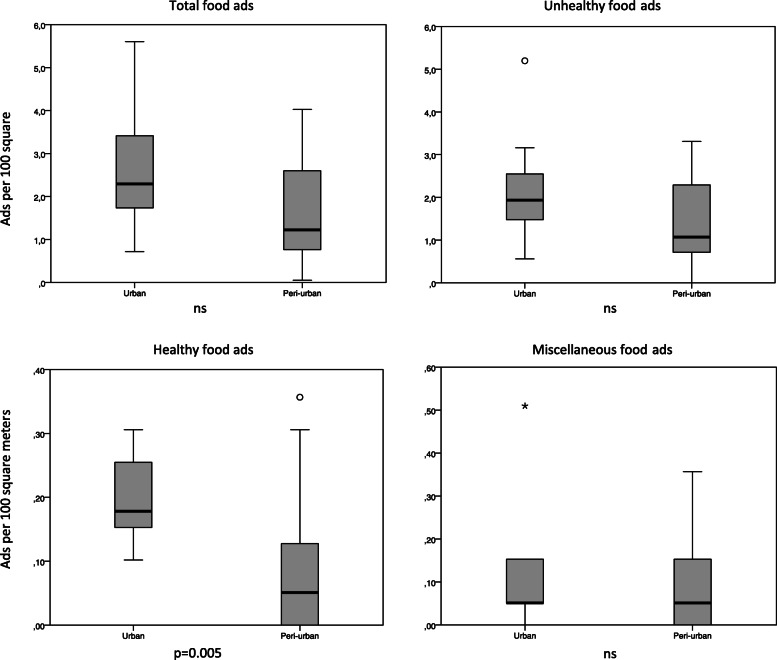
The number of ads was higher around schools in the urban area compared to the peri-urban area, with a median of 45 and 24, respectively (Table 3), but the difference was not significant. This translated to an overall density of ads of 2.6/100 m2 in the urban and 1.6/100 m2 in the peri-urban area (Fig. 2) (Supplementary Table 1, Additional file 1). In terms of unhealthy ads, there was no significant difference between the respective areas. Although healthy ads were infrequently observed, the number of healthy ads was significantly higher around schools in the urban area compared to the peri-urban area (4 vs. 1, p = 0.005, Table 3).
Table 3.
Median (25-, 75-percentiles) number of food and beverage advertisements (total and by major food categories) within a radius of 250 m around the school, by school characteristics (n = 25)
| Total food ads | Major food categories | |||
|---|---|---|---|---|
| School characteristics | Unhealthy | Healthy | Miscellaneous | |
| School area | ||||
| Urban areas (n = 13) | 45 (34, 67) | 38 (29, 50) | 4 (3, 5) | 1 (1, 3) |
| Peri-urban areas (n = 12) | 24 (15, 51) | 21 (14, 45) | 1 (0, 3) | 1 (0, 3) |
| p-value a | 0.077 | 0.11 | 0.005 | 0.73 |
| School fee level | ||||
| Low (n = 9) | 45 (33, 53) | 36 (29, 45) | 4 (3, 5) | 1 (1, 7) |
| Medium (n = 8) | 44 (22, 63) | 38 (21, 55) | 3 (1, 5) | 1 (1, 3) |
| High (n = 8) | 33 (22, 45) | 31 (19, 42) | 2 (1, 3) | 1 (0, 3) |
| p-value b | 0.69 | 0.75 | 0.33 | 0.41 |
| School type | ||||
| Primary (n = 13) | 41 (33, 58) | 37 (29, 45) | 3 (1, 5) | 2 (1, 7) |
| Secondary (n = 12) | 30 (17, 53) | 27 (15, 50) | 2 (1, 4) | 1 (0, 3) |
| p-value a | 0.29 | 0.47 | 0.27 | 0.25 |
| School category | ||||
| Government-funded (n = 9) | 45 (33, 67) | 39 (29, 50) | 4 (3, 5) | 1 (1, 3) |
| Private (n = 16) | 38 (22, 52) | 33 (19, 45) | 2 (1, 4) | 2 (0, 3) |
| p-value a | 0.56 | 0.56 | 0.084 | 0.85 |
| Total | 40 (22, 55) | 36 (19, 47) | 3 (1, 5) | 1 (0,3) |
a Differences between groups measured with Mann-Whitney U test
b Differences between groups measured with Kruskal Wallis test
Fig. 2.
Density (per 100 m2) of food and beverage advertisements (total and by major food categories) by urban and peri-urban areas
Food and beverage advertisements by school type, school fee, and school category
There were no significant differences in the median number of unhealthy or healthy ads around the different types of schools when comparing primary schools versus secondary schools; schools with low, medium, and high school fees; or between government-funded and private schools (Table 3) (Supplementary Table 1, Additional file 1).
Size of food and beverage advertisements
When ranging the size of the ads, small or medium ads were most frequently occurring around schools, while large size comprised of approximately a quarter of the ads (40, 38, 22%, respectively). There was no association between the size of the ads and the proportion of unhealthy ads (Table 4).
Table 4.
Food advertising (total and by major food categories) by the size of the advertisement and by use of promotional characters (n = 1034)
| Total food ads N = 1034 |
Major food categories | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Unhealthy n = 889 |
Healthy n = 84 |
Miscellaneous n = 61 |
p-valuea | ||||||
| n | % | n | % | n | % | n | % | ||
| Advertisement size | n.s. | ||||||||
| Small ad | 409 | 39.6 | 351 | 39.5 | 34 | 40.5 | 24 | 39.4 | |
| Medium ad | 396 | 38.3 | 340 | 38.2 | 30 | 36.9 | 25 | 38.3 | |
| Large ad | 229 | 22.1 | 198 | 22.3 | 19 | 22.6 | 12 | 22.1 | |
| Promotional characters | 0.002 | ||||||||
| No | 957 | 92.6 | 825 | 92.8 | 71 | 84.5 | 61 | 100 | |
| Yes | 77 | 7.4 | 64 | 7.2 | 13 | 15.5 | 0 | 0 | |
a Pearson’s Chi square
The power of promotion
Of all the ads (n = 1034), 7.4% included promotional characters (n = 77) (Table 4). Promotional characters were found in a higher proportion of the healthy food ads compared with the unhealthy food ads (15% vs 7%, p = 0.002). The promotional characters most used were cartoons or company-owned characters (74%), followed by an unknown character (9%), licensed characters (8%), ‘for kids’ images and messages (7%), and famous sportspersons, celebrities, and events (1% in all). Premium offers were less commonly used and only found in unhealthy ads (n = 13, 1.3%).
Discussion
The results demonstrate a total of 1034 food ads around 25 randomly selected schools in two divisions in Kampala. There were on average 40 ads within a radius of 250 m around each of the schools. Of these, a large majority (86%) were for unhealthy foods with an average of 36 unhealthy food ads around each school. Whereas there is a scarcity of previous comparable studies from low-income countries, Kelly et al. [41] documented a lower number of ads around schools in Ulaanbaatar in Mongolia (mean of 18 ads), whereas a higher number (128 ads) was documented around schools in Manila, the Philippines [41]. In line with the present study, unhealthy foods accounted for the majority of the ads in both settings (92% in Ulaanbaatar and 85% in Manila).
Our findings are consistent with research in a high-income country (Australia) that documented ads within a 500 m radius of forty primary schools in Sydney and Wollongong. Out of a total of 2287 food ads, 80% were for unhealthy foods, and the density was twice as high in the area closest to schools (≤ 250 m) [17]. The increasing number of studies that monitor food advertising thus indicate that unhealthy food advertising is a public health challenge, particularly in urban areas in both low-, middle-, and high-income countries [15, 17, 41, 42, 49]. Particularly for the low- and middle-income countries, it has been postulated that food marketing, in the form of advertising and product placement in communities that otherwise have limited access to these food items, may potentially accelerate the nutrition transition [50]. A recent study explored the urban and rural environments in cities of different income levels, and documented that Uganda had the highest in-community food advertising when compared to South Africa and Sweden [51].
The overall density of ads was higher in urban areas, which has a greater population density and less social disadvantages than peri-urban areas. A similar pattern was observed in Sydney and Wollongong, where there was significantly more advertising in high population density/high socioeconomic status areas [17]. Similarly, the study in Ulaanbaatar found that the overall density of ads was more than twice as high in areas of greater population density and socio-economic status [41].
For the marketing industry, there is value in advertising in high-density areas as more people come in contact with the branded product, thereby increasing the overall brand exposure [17]. Concurrently, urban settings are recognized as more vulnerable to food and lifestyle choices that prioritize the consumption of ‘take away’ and other foods that can be energy-dense and nutrient-poor [52]. In Kampala, a switch from a traditional diet to a diet rich in processed foods high in sugars, salt and fat has been reported [53]. The number of healthy ads surrounding schools in the urban area was significantly higher than in the peri-urban area, reflecting neighbourhood disparities in healthy food promotion. The lower-income areas were scarcely exposed to marketing that promoted healthy eating habits and optimum health, representing a concern that also has been established in previous studies [54–57]. Furthermore, as recognized in The State of Food Security and Nutrition in the World 2019 report, poorer communities often face physical and economic barriers to obtaining nutritious foods, placing them at higher risk of food insecurity and malnutrition [58].
Exposure to sugar-sweetened beverages
More than half of the ads captured in this study were for sugar-sweetened beverages, followed by alcoholic beverages (51 and 23%, respectively). The findings are in line with previous studies that examined outdoor ads around schools. Kelly et al. (2008) found that sugar-sweetened beverages (24%) and alcoholic beverages (22%) were most frequently advertised in New Zealand. Similarly, in Manila, it was estimated that more than half of the unhealthy ads surrounding schools were for sugar-sweetened beverages (56%), followed by alcoholic beverages (7%) [41].
In the present study, Coca-Cola accounted for 35% of the total ads and 67% of the sugar-sweetened beverages. Studies from Ulaanbaatar and Manila have reported similar findings, showing that Coca-Cola is a highly featured brand [41]. Similarly, research from Accra city in Ghana, which used a different methodology, found that the majority of ads featured sugar-sweetened beverages (73%) and that Coca-Cola accounted for 60% of the total ads [59]. The present study identified that two of the schools had large school signs branded by Coca-Cola at their school entrance but cannot confirm whether the schools received any monetary or program support from the sponsoring company. In Western Cape, however, a study identified that 60% of the schools featured a signage board with the school’s name and a branded soft drink, of which 85% were sponsored by a well-known brand [60]. Such ads may imply that the schools are endorsing the marketing message [13]. This type of advertising is in breach with WHO recommendations [33] and indicates the urgent need for national regulations of unhealthy food advertising.
Exposure to alcoholic beverages
The fact that alcoholic beverages was the second most promoted food category around schools (23% of all ads) is of high public health concern. Uganda had an annual per capita alcohol consumption of nearly 24 liters in 2014, which increased to 26 liters in 2016, ranking among the countries with the higher alcohol consumption rates in Africa [61, 62]. A high alcohol consumption rate is also reported to be prevalent among youth in the country [61]. A previous study reported that a sample of schools had not instituted serious measures to prevent the onset of alcohol consumption in schools, nor had the communities where students came from been supportive [63]. Given the harmful effect associated with alcoholic beverages [61, 64] and the age limit of 18 years, such advertising is inconsistent with any health-promoting recommendations. As for unhealthy food, there is an urgent need for regulation of alcohol marketing in Uganda. A complete ban on alcohol advertising has been proposed by both international health organizations [65, 66] and national policy-makers such as Uganda Alcohol Policy Alliance, and by the Parliament of Uganda’s draft on an Alcoholic Drinks Control Bill 2016, reflecting the ongoing momentum for clear policy framework to protect children and the vulnerable populations from both the consumption and effects of alcohol [67].
Policy enforcement and implementation
The study observed an almost absence of marketing of toddler milk/infant formula indicating that Uganda’s Code of Conduct for breastmilk substitutes is strong and well enforced [68–71]. The findings also suggest that an international food marketing framework similar to the Code of Marketing of Breastmilk Substitutes [72] could perhaps serve as a model for future policies designed to reduce unhealthy food marketing practices in Uganda and other parts of the world.
The need to address the double burden of malnutrition, ensure food safety, and encourage healthy food marketing is recognised in the 2020 annual report of the work of WHO in the African Region, where fifteen West African countries were supported to strengthen food and beverage regulation, including alcoholic beverages [73]. This support embodies the growing recognition of unhealthy food marketing as a major health and children’s rights issue. Acting on food environments by discouraging unhealthy food marketing and simultaneously ensuring healthy diet availability, affordability, and appeal is one opportunity to prevent malnutrition in all its forms [74].
Our findings demonstrate that there is a need to reduce the marketing of unhealthy foods and beverages around schools, and in particular of sugar-sweetened beverages and alcoholic beverages. A ban on marketing of unhealthy foods and beverages within a radius of at least 100 m (as recommended by Pan American Health Organization [75] would be an important step towards healthier food environments in proximity to schools. The implementation of such policies also contributes to meeting state obligations to protect, respect, and fulfil children’s rights under international human rights law.
Strengths and limitations
This study has verified the possibility of mapping ads comprehensively with the use of an acknowledged and standardized protocol. Its findings provide insights into the advertising environment in school zones of the most densely populated areas in Uganda. The inclusion of a peri-urban area may, to some extent, provide insight into a partly rural context. Importantly, the findings show that it is essential for future studies to include alcoholic beverage ads when exploring food marketing. A limiting factor is that the sample size was set to 25 schools within two out of five divisions of the city. Consequently, the results cannot be generalized to all schools and zones in the larger city.
At the time of the study, there was no available nutrient profiling model for the African region. Since then, the nutrient profiling model for the African region has been adopted [76]. In this study, we applied the possibility of mapping food marketing in an African city context using a European-developed framework. As such, there is a risk for having overlooked the nature of food environments in Africa. For example, we excluded what could be a significant proportion of outdoor ads; those that were on the inside of the ‘food shop door’ when closed but faced the outside when open. Based on observation, the majority of these were unhealthy food ads. Also, since we set a 250-m buffer around schools, the result may only serve as a proxy for the area of true exposure relevant to children [18], rather than the total exposure of food advertising near schools.
In addition to the highlighted limitations, there is a lack of comparable studies in the African context which limits the transferability to similar country contexts. Going forward, this study may give a basis for situation-analysis, monitoring, guidance, comparison, and referring purposes. The study may also serve as a starting point for future studies, research agendas and collaborations in this field and other related areas of public health nutrition.
Conclusion
Overall, the results suggest that the food marketing landscape around schools in Kampala was not conducive to a health-promoting environment in the dimension of food advertising. Repeated exposure to such food marketing may encourage children to consume these foods and beverages, which is recognized as a major contributing factor to unhealthy diets, obesity, and non-communicable diseases.
The findings have particular implications for policies that regulates advertising of sugar-sweetened beverages and alcoholic beverages. Such policies are presently limited in Uganda, yet it is of the essence to have a robust policy and legal agenda to mitigate the malnutrition and disease risk that may accrue from unregulated advertisement of unhealthy foods and beverages. Despite surveillance data limitations, the prevalence of overweight and obesity among children in Uganda is on the rise and the burden seems to be greater in the urban communities, such as Kampala. A disease preventative and health-promoting measure to prevent acceleration of the double burden of malnutrition, could be to raise attention to unhealthy food marketing to children; and to develop relevant marketing policies and comply with such policies once they are enforced in order to foster accountability.
Supplementary Information
Acknowledgments
We thank INFORMAS for input to the study design. Further appreciation goes to the Kampala Capital City Authority (KCCA) for their cooperation, and the schools for participating in the study. We thank the field assistants who worked with the principal researcher (EWD) in the two districts of Kampala city.
Authors’ contributions
EWD conceived and planned the study, sought the ethical approvals, did the data collection, analysis, and interpretation, and drafted the manuscript. ALL, PMR, and LET supported the conceptualization of the study, reviewed and commented on the drafts. All authors read and approved the final manuscript.
Authors’ information
1 EWD, ALL, and LET at the Department of Nursing and Health Promotion, OsloMet – Oslo Metropolitan University, Norway. 2 PMR at the Department of Human Nutrition and Home Economics, Kyambogo University, Uganda.
Funding
This work received financial support by OsloMet – Oslo Metropolitan University.
Availability of data and materials
The dataset generated and analysed during the current study are available from the first author upon reasonable request and with permission of INFORMAS.
Declarations
Ethics approval and consent to participate
The research study was ethically approved by authorities in Norway and Uganda. Specifically, ethical clearance was sought from the Norwegian Centre for Research Data, Makerere University School of Social Sciences Research Ethics Committee (MAKSS REC 08.18.209) and the Uganda National Council for Science and Technology (Ref. SS 4812). The Kampala Capital City Authority also provided permission to access the schools in in Kawempe and Kampala Central divisions (DES/KCCA/201/17).
Consent for publication
Not applicable.
Competing interests
All authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Taking action on childhood obesity report. World Health Organization; 2018. Available from: http://www.who.int/nutrition/publications/obesity/taking-action-childhood-obesity-report/en/. [cited 2020 Aug 20].
- 2.United Nations Children’s Fund, World Health Organization, World Bank. UNICEF/WHO/The World Bank Group joint child malnutrition estimates: levels and trends in child malnutrition: key findings of the 2020 edition. Available from: https://www.who.int/publications-detail/jme-2020-edition. [cited 2020 Apr 9].
- 3.World Health Organization. Report of the Commission on Ending Childhood Obes. 2016. Available from: http://apps.who.int/iris/bitstream/handle/10665/204176/9789241510066_eng.pdf?sequence=1.
- 4.Abarca Gómez L, Sunyer Deu J, Vrijheid M, Ezzati M. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113). Available from: http://repositori.upf.edu/handle/10230/34253. [cited 2018 June 2]. [DOI] [PMC free article] [PubMed]
- 5.Food and Agriculture Organization of the United Nations, International Fund and Agriculture Development, United Nations Children’s Fund, World Food Programme, World Health Organization . The State of Food Security and Nutrition in the World 2018. Building climate resilience for food security and nutrition. Rome: FAO; 2018. [Google Scholar]
- 6.Boyland EJ, Nolan S, Kelly B, Tudur-Smith C, Jones A, Halford JC, et al. Advertising as a cue to consume: a systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am J Clin Nutr. 2016;103(2):519–33. 10.3945/ajcn.115.120022. [DOI] [PubMed]
- 7.Sadeghirad B, Duhaney T, Motaghipisheh S, Campbell NRC, Johnston BC. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: a systematic review and meta-analysis of randomized trials. Obes Rev Off J Int Assoc Study Obes. 2016;17(10):945–959. doi: 10.1111/obr.12445. [DOI] [PubMed] [Google Scholar]
- 8.Robinson TN, Borzekowski DLG, Matheson DM, Kraemer HC. Effects of fast food branding on young Children’s taste preferences. Arch Pediatr Adolesc Med. 2007;161(8):792–797. doi: 10.1001/archpedi.161.8.792. [DOI] [PubMed] [Google Scholar]
- 9.Cairns G, Angus K, Hastings G, Caraher M. Systematic reviews of the evidence on the nature, extent and effects of food marketing to children. A retrospective summary. Appetite. 2013;62:209–215. doi: 10.1016/j.appet.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 10.European Commission. The Joint Research Centre (JRC). Food an non-alcoholic beverage marketing to children and adolescents. 2017. Retrieved from: https://ec.europa.eu/info/index_en.
- 11.World Health Organization . Global strategy on diet, physical activity and health. 2004. [Google Scholar]
- 12.Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385(9986):2510–20. 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed]
- 13.World Health Organization . Evaluating implementation of the WHO set of recommendations on the marketing of foods and non-alcoholic beverages to children. Copenhagen: The World Health Organization Regional Office for Europe; 2018. [Google Scholar]
- 14.Kelly B, Vandevijvere S, Ng S, Adams J, Allemandi L, Bahena-Espina L, et al. Global benchmarking of children’s exposure to television advertising of unhealthy foods and beverages across 22 countries. Obes Rev. 2019; Available from: http://onlinelibrary.wiley.com/doi/abs/10.1111/obr.12840. [cited 2019 Apr 13] [DOI] [PMC free article] [PubMed]
- 15.Adams J, Ganiti E, White M. Socio-economic differences in outdoor food advertising in a city in northern England. Public Health Nutr. 2011;14(6):945–950. doi: 10.1017/S1368980010003332. [DOI] [PubMed] [Google Scholar]
- 16.Hillier A, Cole BL, Smith TE, Yancey AK, Williams JD, Grier SA, et al. Clustering of unhealthy outdoor advertisements around child-serving institutions: a comparison of three cities. Health Place. 2009;15(4):935–45. 10.1016/j.healthplace.2009.02.014. [DOI] [PubMed]
- 17.Kelly B, Cretikos M, Rogers K, King L. The commercial food landscape: outdoor food advertising around primary schools in Australia. Aust N Z J Public Health. 2008;32(6):522–528. doi: 10.1111/j.1753-6405.2008.00303.x. [DOI] [PubMed] [Google Scholar]
- 18.Velazquez CE, Daepp MIG, Black JL. Assessing exposure to food and beverage advertisements surrounding schools in Vancouver, BC. Health Place. 2019 11; Available from: http://www.sciencedirect.com/science/article/pii/S1353829218304544. [cited 2019 Apr 14] [DOI] [PubMed]
- 19.Hawkes C. Uneven dietary development: linking the policies and processes of globalization with the nutrition transition, obesity and diet-related chronic diseases. Glob Health. 2006;2(1):4. doi: 10.1186/1744-8603-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frandsen SE, Kuyvenhoven A, von Braun J. Case studies in food policy for developing countries: policies for health, Nutrition, Food Consumption, and Poverty. Ithaca: Cornell University Press; 2009.
- 21.Caballero B. A nutrition paradox - underweight and obesity in developing countries. N Engl J Med Boston. 2005;352(15):1514–1516. doi: 10.1056/NEJMp048310. [DOI] [PubMed] [Google Scholar]
- 22.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84(2):289–298. doi: 10.1093/ajcn/84.2.289. [DOI] [PubMed] [Google Scholar]
- 23.Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choukem S-P, Tochie JN, Sibetcheu AT, Nansseu JR, Hamilton-Shield JP. Overweight/obesity and associated cardiovascular risk factors in sub-Saharan African children and adolescents: a scoping review. Int J Pediatr Endocrinol. 2020;2020. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7092532/. [cited 2020 Oct 29] [DOI] [PMC free article] [PubMed]
- 25.Chebet M, Goon DT, Nsibambi C, Otala J. Prevalence of overweight and obesity among primary school children in Kampala central, Uganda. Afr J Phys Health Educ Recreat Dance. 2014;20(4.1):1365–1378. [Google Scholar]
- 26.Baalwa J, Byarugaba B, Kabagambe K, Otim A. Prevalence of overweight and obesity in young adults in Uganda. Afr Health Sci. 2010;10(4):367–373. [PMC free article] [PubMed] [Google Scholar]
- 27.Nsibambi CAN. Body Composition Analysis of Pupils in Urban Schools in Central Uganda. Int J Bus Soc Sci. 2013;4(7). Available from: http://ijbssnet.com/journals/Vol_4_No_7_July_2013/15.pdf
- 28.Uganda Bureau of Statistics and ICF International Inc. Uganda 2016 Demographic and Health Survey - Key Findings. Kampala, Uganda, and Rockville, Maryland, USA: UBOS & ICF; 2016.
- 29.Peltzer K, Pengpid S. Overweight and obesity and associated factors among school-aged adolescents in Ghana and Uganda. Int J Environ Res Public Health. 2011;8(10):3859–3870. doi: 10.3390/ijerph8103859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.NCD Risk Factor Collaboration. Evolution of body-mass index over time. 2016. Available from: http://ncdrisc.org/country-profile.html. [cited 2018 Jun 10]
- 31.NCD Risk Factor Collaboration Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abrahams Z, Mchiza Z, Steyn NP. Diet and mortality rates in sub-Saharan Africa: stages in the nutrition transition. BMC Public Health. 2011;11(1):801. doi: 10.1186/1471-2458-11-801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization . A framework for implementing the set of recommendations on the marketing of foods and non-alcoholic beverages to children. 2012. [Google Scholar]
- 34.World Health Organization . Set of recommendations on the marketing of foods and non-alcoholic beverages to children. 2010. [Google Scholar]
- 35.United Nations General Assembly. International Covenant on Economic, Social and Cultural Rights (No. Resolution 2200A (XXI)). U N. 1966 Dec 16;993:3.
- 36.United Nations General Assembly. Convention on the Rights of the Child (No. Resolution 44/25). U N. 1989 Nov 20;1577.
- 37.Garde A, Byrne S, Nikhil G, Murphy B. A child rights-based approach to food marketing: a guide for policy makers. 2018. [Google Scholar]
- 38.Swinburn B, Vandevijvere S, Kraak V, Sacks G, Snowdon W, Hawkes C, et al. Monitoring and benchmarking government policies and actions to improve the healthiness of food environments: a proposed government healthy food environment policy index. Obes Rev Off J Int Assoc Study Obes. 2013;14(Suppl 1):24–37. 10.1111/obr.12073. [DOI] [PubMed]
- 39.Kelly B, King L, Baur L, Rayner M, Lobstein T, Monteiro C, et al. Monitoring food and non-alcoholic beverage promotions to children. Obes Rev. 2013;14(S1):59–69. 10.1111/obr.12076. [DOI] [PubMed]
- 40.Mackay S, Molloy J, Vandevijvere S. INFORMAS protocol: outdoor advertising (school zones) 2017. [Google Scholar]
- 41.Kelly B, King L, Jamiyan B, Chimedtseren N, Bold B, Medina VM, et al. Density of outdoor food and beverage advertising around schools in Ulaanbaatar (Mongolia) and Manila (the Philippines) and implications for policy. Crit Public Health. 2015;25(3):280–90. 10.1080/09581596.2014.940850.
- 42.Barquera S, Hernández-Barrera L, Rothenberg SJ, Cifuentes E. The obesogenic environment around elementary schools: food and beverage marketing to children in two Mexican cities. BMC Public Health. 2018;18(1):461. doi: 10.1186/s12889-018-5374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Organization of African Unity. African Charter on the Rights and Welfare of the Child. 1990. Available from: http://hrlibrary.umn.edu/africa/afchild.htm. [cited 2020 May 2].
- 44.Map Developers. Google Map Developers. Available from: https://www.mapdevelopers.com/. [cited 2019 Mar 4]
- 45.World Health Organization. Nutrient Profiling: Report of a WHO/IASO Technical Meeting. London; 2011. Available from: http://www.who.int/nutrition/topics/profiling/en/. [cited 2018 Oct 10].
- 46.World Health Organization. Regional Office for Africa. WHO Regional Office for Europe nutrient profile model. 2015. Available from: http://www.euro.who.int/__data/assets/pdf_file/0005/270716/Nutrient-children_web-new.pdf
- 47.OECD. Public and Private Schools: How Management and Funding Relate to their Socio-economic Profile, OECD Publishing. 2012. doi: 10.1787/19963777. [cited 2018 Nov 29].
- 48.Field A. Discovering statistics using IBM SPSS statistics. 5. Los Angeles: SAGE Publications, Inc; 2018. [Google Scholar]
- 49.Walton M, Pearce J, Day P. Examining the interaction between food outlets and outdoor food advertisements with primary school food environments. Health Place. 2009;15(3):841–848. doi: 10.1016/j.healthplace.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 50.Battersby J, Peyton S. The geography of supermarkets in Cape Town: supermarket expansion and food access. Urban Forum. 2014;25(2):153–164. doi: 10.1007/s12132-014-9217-5. [DOI] [Google Scholar]
- 51.Spires M, Berggreen-Clausen A, Kasujja FX, Delobelle P, Puoane T, Sanders D, et al. Snapshots of urban and rural food environments: EPOCH-based mapping in a high-, middle-, and low-income country from a non-communicable disease perspective. Nutrients. 2020 14;12(2). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7071357/. [cited 2020 Apr 16]. [DOI] [PMC free article] [PubMed]
- 52.Global Panel on Agriculture and Food Systems for Nutrition . Food systems and diets: Facing the challenges of the 21st century. 2016. [Google Scholar]
- 53.Harvey P, Zo R, Dary O. The 2008 Uganda Food Consumption Survey: Determining the Dietary Patterns of Ugandan Women and Children. Washington D.C.; 2010. Available from: https://www.spring-nutrition.org/publications/projects/a2z/2008-uganda-food-consumption-survey-determining-dietary-patterns-ugandan. [cited 2018 Jun 9]
- 54.Bell J, Mora G, Hagan E, Rubin V, Karpyn A. Access to healthy food and why it matters: a review of the research. Oakland: PolicyLink and The Food Trust; 2013. [Google Scholar]
- 55.Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health. 2012;102(9):1644–1654. doi: 10.2105/AJPH.2012.300865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cassady DL, Liaw K, Miller LMS. Disparities in obesity-related outdoor advertising by neighborhood income and race. J Urban Health Bull N Y Acad Med. 2015;92(5):835–842. doi: 10.1007/s11524-015-9980-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yancey AK, Cole BL, Brown R, Williams JD, Hillier A, Kline RS, et al. A cross-sectional prevalence study of ethnically targeted and general audience outdoor obesity-related advertising. Milbank Q. 2009;87(1):155–184. doi: 10.1111/j.1468-0009.2009.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Food and Agriculture Organization of the United Nations, International Fund and Agriculture Development, United Nations Children’s Fund, World Food Programme, World Health Organization . The State of Food Security and Nutrition in the World 2019. Safeguarding against economic slowdowns and downturns. Rome: FAO; 2019. [Google Scholar]
- 59.Bragg MA, Hardoby T, Pandit NG, Raji YR, Ogedegbe G. A content analysis of outdoor non-alcoholic beverage advertisements in Ghana. BMJ Open. 2017;7(5):e012313. doi: 10.1136/bmjopen-2016-012313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Villiers A, Steyn NP, Draper CE, Fourie JM, Barkhuizen G, Lombard CJ, et al. “HealthKick”: Formative assessment of the health environment in low-resource primary schools in the Western Cape Province of South Africa. BMC Public Health. 2012;12(1):794. doi: 10.1186/1471-2458-12-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.World Health Organization . Global status report on alcohol and health 2018. 2018. [Google Scholar]
- 62.World Health Organization . Global Status Report on Alcohol and Health 2014. 2014. [Google Scholar]
- 63.Uganda Youth Development Link . State of alcohol abuse in Uganda: “young people drinking deeper into poverty”. 2008. [Google Scholar]
- 64.Griswold MG, Fullman N, Hawley C, Arian N, Zimsen SRM, Tymeson HD, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2018;392(10152):1015–35. 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed]
- 65.World Health Organization . Global strategy to reduce harmful use of alcohol. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pan American Health Organization . PAHO meeting on alcohol marketing regulation: final report. 2016. [Google Scholar]
- 67.Uganda Alcohol Policy Alliance, Ministry of Health, Makerere University School of Public Health . The First Uganda Alcohol Policy Conference (UAPC18) 2018. [Google Scholar]
- 68.Ministry of Health . Policy Guidelines on Infant and Young Child Feeding. 2012. [Google Scholar]
- 69.Ministry of Health . Ministerial Statement to Parliament on World Breastfeeding Week. 2018. [Google Scholar]
- 70.World Health Organization . Marketing of breast-milk substitutes: National implementation of the international code. 2018. [Google Scholar]
- 71.Ministry of Agriculture, Animal Industry & Fisheries, Ministry of Health . The National Food and Nutrition Strategy. 2005. [Google Scholar]
- 72.World Health Organization . International Code of Marketing of Breast-Milk Substitutes. 1981. [Google Scholar]
- 73.World Health Organization. Regional Office for Africa. The Work of the World Health Organization in the African Region: Report of the Regional Director, 1 July 2019–30 June 2020. 2020. Available from: https://www.afro.who.int/publications/work-world-health-organization-african-region-report-regional-director-1-july-2019-30. [cited 2020 Oct 19]
- 74.Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet. 2020;395(10218):142–155. doi: 10.1016/S0140-6736(19)32506-1. [DOI] [PubMed] [Google Scholar]
- 75.Pan American Health Organization (PAHO). Recommendations from a Pan American Health Organization Expert Consultation on the Marketing of Food and Non-Alcoholic Beverages to Children in the Americas. In. Washington, DC.:; 2011: 130.
- 76.World Health Organization. Regional Office for Africa. Nutrient Profile Model for the WHO African Region: a tool for implementing WHO recommendations on the marketing of foods and non-alcoholic beverages to children. WHO Regional Office for Africa; 2019. Available from: https://apps.who.int/iris/handle/10665/329956
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset generated and analysed during the current study are available from the first author upon reasonable request and with permission of INFORMAS.