Abstract
Background
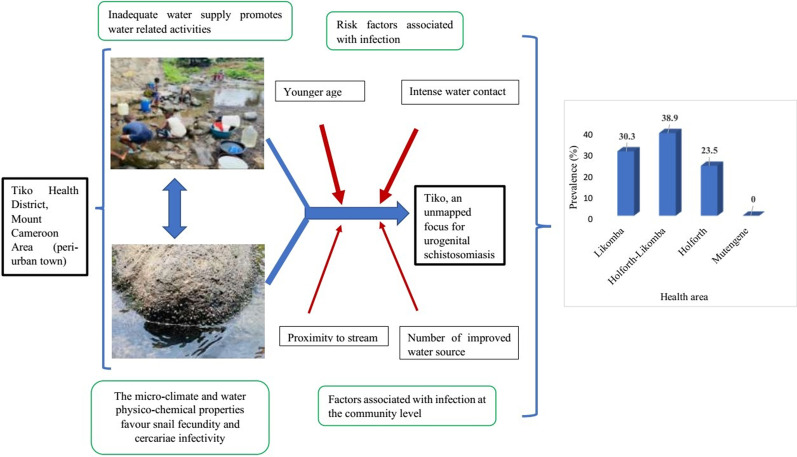
Increased risk of schistosomiasis in peri-urban and urban towns is not uncommon. An epidemiological survey was carried out in the Tiko Health District (THD), an unmapped transmission focus for urogenital schistosomiasis (UGS), to assess the distribution, intensity, and risk factors associated with the occurrence of UGS.
Methods
In this cross-sectional survey, 12 communities were purposively selected from four health areas (HAs) (Likomba, Holforth, Holforth-Likomba, and Mutengene) in South West Region of Cameroon between June and August 2018. Consenting individuals were enrolled using a convenient sampling technique and administered a semi-structured questionnaire to document information on socio-demographic and water contact behaviour. Urine samples were examined for Schistosoma haematobium infection using test strip, filtration, and microscopy methods. Bivariate and binary logistic regression analyses were used to identify predictors of infection.
Results
The overall prevalence of UGS in Likomba, Holforth-Likomba and Holforth was 31.5% [95% confidence interval (CI): 28.3–34.8] with geometric mean (GM) egg count of 28.7 (range: 2–450) eggs per 10 ml of urine. S. haematobium infection was not found in Mutengene HA. Infection was unevenly distributed among the HAs, Holforth-Likomba and Holforth being the most and least affected, respectively. The prevalence of infection varied (P < 0.001) among the affected communities, ranging from 12.0 to 56.9%. Infection status of the community related positively (P < 0.001) with proximity to stream (< 100 m), the degree of contact with water and number of improved water sources. Younger age group (5–14 years) [adjusted odds ratio (aOR): 3.7, 95% CI: 1.1–12.2] and intense water contact (degree II) (aOR: 5.2, 95% CI: 3.4–8.1) were associated with increased risk of infection. Similarly, significantly higher egg load was observed among younger aged groups (P = 0.02) and those who carried out intense water contact activities (P < 0.001).
Conclusions
Generally, THD is a moderate risk endemic focus for UGS but prevalence higher than 50.0% was observed in some communities. These findings warrant immediate mass chemotherapy with praziquantel to reduce morbidity. Provision of portable water and health education are proposed measures to reduce and eventually eliminate transmission in the area.
Graphic abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s40249-021-00827-2.
Keywords: Urogenital schistosomiasis, Prevalence, Distribution, Risk factor, Tiko Health District, Cameroon
Background
Schistosomiasis is the third highest burden among the neglected tropical diseases (NTDs) and is endemic in 78 countries worldwide, where an estimated 800 million people are at risk of the disease [1]. Of the 250 million infected individuals, 200 million live in Africa where the two predominant disease sub-types are intestinal and urogenital schistosomiasis caused by Schistosoma mansoni and S. haematobium, respectively [2, 3]. Globally, an estimated 1.43 million disability-adjusted life years (DALYs) is lost to schistosomiasis [4]. Over 150 000 deaths are attributable to chronic infection with S. haematobium in Africa [5, 6].
The transmission of schistosomiasis is governed by social–ecological systems such as conditions of poverty and living near open freshwater bodies [7]. Children are at a greater risk of acquiring the infection as well as re-infection [8], and this might lead to growth retardation, anaemia and low school performance [9]. Nonetheless, in endemic areas, where there is lack of adequate water supply, poverty, ignorance and poor hygienic practices, any demographical groups, irrespective of age or gender in contact with unsafe water is at risk of infection [10]. The current mainstay of schistosomiasis control is preventive chemotherapy—the periodic administration of praziquantel to at-risk groups (e.g., school-age children). While this strategy does not prevent infection or reinfection, it reduces morbidity and might also impact on transmission [11]. Schistosomiasis can be prevented by avoiding contact with contaminated freshwater, and the risk of infection can be reduced through improved access to water, sanitation, and hygiene (WASH), information, education, and communication (IEC) [12].
Although schistosomiasis is classically described as a rural disease that occurs in areas without potable water and adequate sanitation [13], urban foci of parasites in tropical areas can no longer be ignored [14]. Increased risk of schistosomiasis in urban areas has been linked to migration of people to neighbouring towns for more attractive employment opportunities [13, 15], water resource development to curb inadequacy in water supply [16] and small multipurpose dams that may lead to ecological changes [17, 18]. Outbreak of neglected tropical diseases in urban areas has been reported due to rapid urbanization which at the same time can also fail to sustain healthy populations when it surpasses clean water reserve and sewage management systems [19]. More so, in this era of global warming and climate change, the epidemiology of temperature dependent infectious diseases is rapidly changing [16].
In the South West Region of Cameroon, records of urogenital schistosomiasis are mostly from rural areas [8, 20–23]. An unmapped transmission focus has been reported in peri-urban communities in the Tiko Health District (THD) [24]. It remains unknown whether urogenital schistosomiasis (UGS) has existed in the THD for an undetermined period or has recently been introduced. In low and middle-income countries experiencing urbanization, the problem of access to water and sanitation is more critical in secondary cities because of the lower basic infrastructure compared with the situation in the primary cities [18]. Inadequate water supply and sanitation has been reported as a major concern in the THD [25] and in addition to extensive rural–urban migration probably due to interurban trading or political unrest in the English-speaking part of Cameroon [26], transmission intensity of UGS may be exacerbated in this peri-urban setting. The previous survey conducted in this new focus was geographically limited to a single community and involved only children aged 5–20 years [24]. In addition, a less sensitive method (urine sedimentation) was used for the diagnosis of S. haematobium infection and this might have underestimated true infection levels. In view of these limitations and to identify the mechanisms for transmission and maintenance of this disease in THD, an epidemiological survey was carried out among the different population groups, to assess the distribution, intensity as well as describe the risk factors associated with occurrence of UGS in the study area.
Materials and methods
Study area
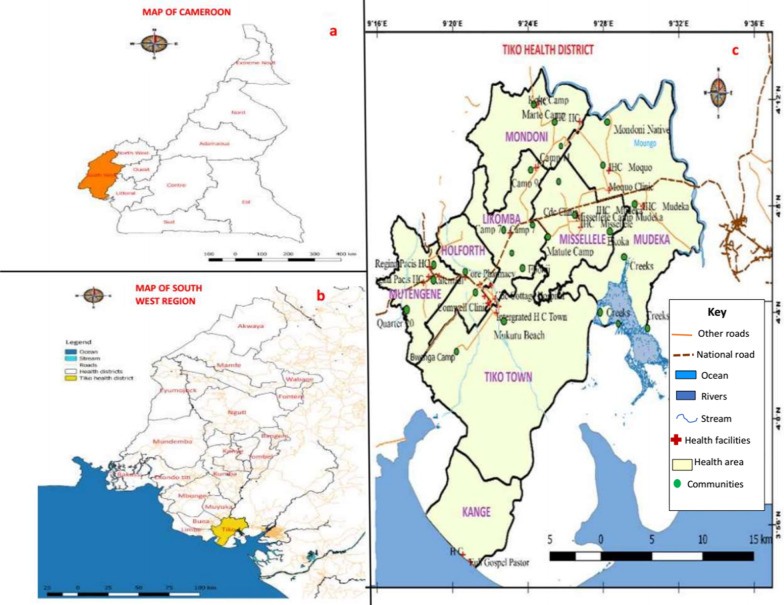
This study was carried out in the THD, located in Fako Division of the South West Region of Cameroon. The coordinates of THD ranged from altitude 18 m, latitude 9° 32′ 2″ N to 9° 40′ 9″ N to altitude 220 m, longitude 9° 25′ 7″ E to 9° 55′ 7″ E, with a total surface area of 4840 km2. This Health District is not geographically isolated from the UGS focus in Munyenge, Bafia Health Area, Muyuka Health District (Fig. 1b). Tiko health district is made up of eight HAs (Holforth, Kange, Likomba, Mutengene, Mondoni, Mudeka, Missellele, and Tiko Town) (Fig. 1c) and inhabited by a heterogenous population of approximately 124 423 inhabitants [27]. This area is characterized by the presence of a local seaport that allows for fishing, import as well as export of goods between neighbouring countries. The rich volcanic soil encourages farming activities and industrial agriculture. This health district hosts the Cameroon Development Corporation (CDC) plantations where banana, rubber and oil palm are cultivated and exported.
Fig. 1.
Maps showing location of study site a Map of Cameroon showing the location of South West Region. b Map of South West Region. c Map of Tiko Health District
Tiko Health District has a coastal equatorial climate with two distinct seasons: a rainy season, which lasts from March to October and a short dry season of four months (November–February). The mean annual rainfall is about 4524 mm. The temperature is relatively uniform throughout the year, with daily mean temperatures ranging from 28 to 33 °C [25]. This temperature range favours the development rate of the parasite within snails and the infectivity of cercaria [28]. The main water courses in the Tiko municipality include Moungo River, the Ombe River, Ndongo and Benyo streams which empty into the sea. The slow flow or stagnation of these streams favours the breeding of the snail intermediate host (Fig. 2a). Access to safe water is poor due to frequent non-flow of community and household water [25] and requirement for immediate payment of water fetched from private owned pipe-borne water sources (personal observation). Consequently, the local population makes frequent use of the streams for their daily household chores (Fig. 2b, c).
Fig. 2.

Photographs of snail infested open water and human water contact behaviour in an affected community. a Snail infested stream, b and c Typical stream contact activities
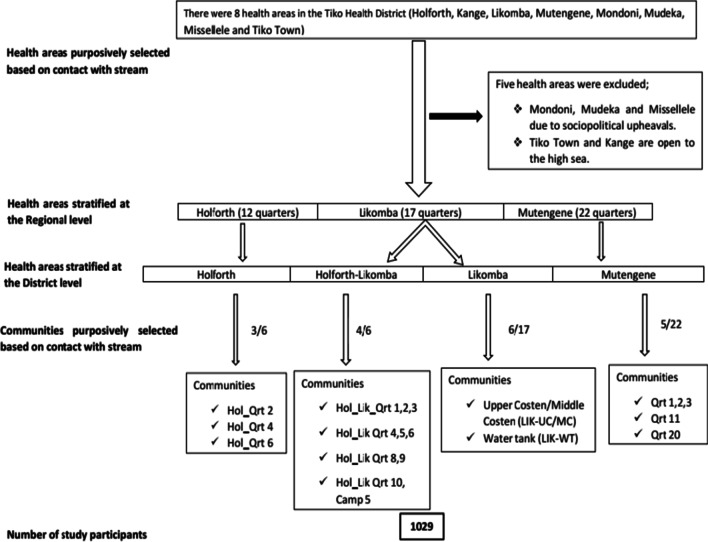
Study design and sampling technique
The study was a cross-sectional community-based design carried out between June to August 2018. Out of the eight HAs, five were excluded from the study; Tiko town and Kange are open to the high sea while Mondoni, Mudeka and Missellele were the riskiest areas during the era of political unrest in the English-speaking part of the Country [26] (Fig. 3). Thus, three out of the eight HAs within the THD were selected for this study namely, Likomba, Holforth and Mutengene. However, at the district level, the Holforth HA (the largest and most populated) is divided into Holforth and Holforth-Likomba areas. In principle, four HAs were considered for the survey; Likomba, Holforth-Likomba, Holforth and Mutengene. Information on the population size of each selected HA and number of communities (neighbourhoods) were sorted from the Regional Delegation of Public Health, South West Region [27]. Twelve communities were purposively selected considering the water contact points [29] (Fig. 1) and a convenient sampling method was used to recruit study participants. The minimum sample size allocated per community was estimated from the total population size of the entire THD.
Fig. 3.
Flow diagram showing selection of study communities
Sample size determination
The sample size for this study was determined based on the Yaro Yamane’s approach for finite population [30] using the formula; n = N/[1 + N (e)2].
where, n = the expected sample size, N = the finite population out of which the sample was drawn, e = the level of significance (or limit of tolerable error).
For this work, the estimated population size (N) from the 2017 population statistics was 124 500 [27], and the level of significance (e) was 0.05 or 5%. Thus, the estimated sample size = 124 500/[1 + 124 500 (0.05)2] = 124 500/312.25 ≈ 398. The minimum estimated sample size calculated per HA was 399. This was multiplied by 3 (i.e. number of HAs included in the survey) to give 1197. However, due to logistics, we had a sample size of 1029 consented participants which is well above 90% of the expected sample size calculated.
Ethical approval and administrative clearances were obtained prior to the commencement of the study. Community engagement in the selected communities were conducted with the support of the Health District, local chiefs, administrative and community health workers (CHW). Participants were invited to temporary data collection location in each community, and coordination was organized with the help of the CHW and leaders within the neighbourhood. Before enrolment into the study, informed consent/assent forms and information sheets (which highlights the purpose, risks and benefits of the study) were given to potential participants; for children less than 13 years old, assent was gotten from the parents or legal guardians, while for those less than 18 years old, consent was obtained from both the parent and the child. Individuals above 18 years gave their consent. The study team proceeded for sample collection upon obtaining consent/assent from the participants. A global positioning system (GPS) was used to get the accurate placement of the communities and water contact points.
Inclusion and exclusion criteria
This study was designed to target individuals both males and females from five years and above living within the THD. Only respondents who have lived for at least two months in the study area and volunteered to participate in the study were enrolled. Enrolled individuals who failed to submit urine sample after the interview were excluded from the study.
Questionnaire survey
Before data collection, a pilot testing of the questionnaire was done to ensure that the questions being asked, accurately reflect the information desired by the researcher and can be answered by the respondents. Challenges were identified and the changes effected accordingly. During the survey, participants were interviewed by a field researcher to record socio-demographic characteristics (age, gender, and residence), socioeconomic status (educational level and occupation) and history of S. haematobium infection (visible haematuria). Information on whether the participant had been living in the health district or came from other areas was noted. Access to the different water sources for household use (communal or household pipe-borne water), distance to open water sources as well as water-related activities such as agricultural practices, fishing, swimming, bathing, washing, laundry and crossing the stream were documented.
The degree of water contact was calculated using the formula, Σ (R × F), as described by Lima et al. [31]; where R is the score for the reason for the contact and F is the score for the frequency of contact. The reasons were given the following scores: 5 (for bathing, swimming, or playing in the streams), 4 (laundering or agricultural purpose), 3 (collecting water for the household, dish-washing or car/motor bike washing), and 2 (fishing or crossing the streams). The frequency of contacts was scored as 28 (daily or at least one contact a day), 4 (weekly or at least one contact a week), 2 (at least two contacts a month), and 1 (less than two a month). Totals of 2–99 were considered as degree I and ≥ 100 as degree II.
Parasitology
Sample collection and processing
Each consented participant received a sterile, dry, screw-top, transparent, pre-labelled urine bottle. Participants were instructed to collect 20 ml of mid-stream urine sample in the container between 10:00 and 14:00. Immediately, samples were assessed for macrohaematuria and later tested for microhaematuria using urine reagent strips (URIT Medical Electronic Co., Ltd. P.R. China) following manufacturer’s instructions. Using the manufacturer colour chart, microhaematuria was detected as reagent strip colour reaction with varying levels indicated as trace, +, + +, + + +. The urine samples were later placed in a cool box and transported to the Malaria Research Laboratory, University of Buea, where, samples were processed using the syringe filtration technique [32].
Briefly, each urine specimen was well mixed, and 10 ml aliquot of urine sample was withdrawn into a syringe and filtered through a membrane filter (diameter, 25 mm; pore size, 8 µm) [Sterlitech Polycarbonate (PCTE) membrane filters, USA], fitted into a syringe holder, to separate the ova. Filter holder was then disassembled to expose the membrane. With the aid of a blunt forceps, each membrane was carefully removed and placed upside down onto a microscope slide. A drop of Lugol’s iodine was added and membranes examined for S. haematobium eggs under the × 10 objective of an Olympus NYUSA microscope (Wincom Company Ltd, China). Microhaematuria is considered as a proxy indicator of UGS and an accepted marker in the rapid diagnosis of S. haematobium infection in urine [33]. Thus, an individual was considered positive for S. haematobium when he/she was diagnosed positive by microscopic examination and/or urine reagent strip. The number of eggs was counted per 10 ml of urine and classified as light (< 50 eggs/10 ml of urine) or heavy (≥ 50 eggs/10 ml of urine) infection [34].
Data management and statistical analysis
All data were entered, validated, and analysed using SPSS Statistics version 20 (SPSS Inc., Chicago, USA). Proportion of S. haematobium was compared between different groups (HAs, sex, age groups, level of education, occupation, source of water for household use and degree of contact) using Pearson Chi square test. Crude odds ratios were estimated, and factors associated with infection identified to be included in the multivariate logistic regression model. Variables that had a P-value < 0.20 in bivariate analysis or biological plausibility were included in the multivariate logistic regression model. Using the enter method, variables which showed independent association with infection at a significance level of P < 0.05 were retained in the model. Mean egg load was compared between groups using non-parametric Mann–Whitney and Kruskal Wallis test. Relationship between presence and intensity of S. haematobium eggs with microhaematuria and proteinuria was determined using Pearson Correlation. A P-value < 0.05 was considered significant.
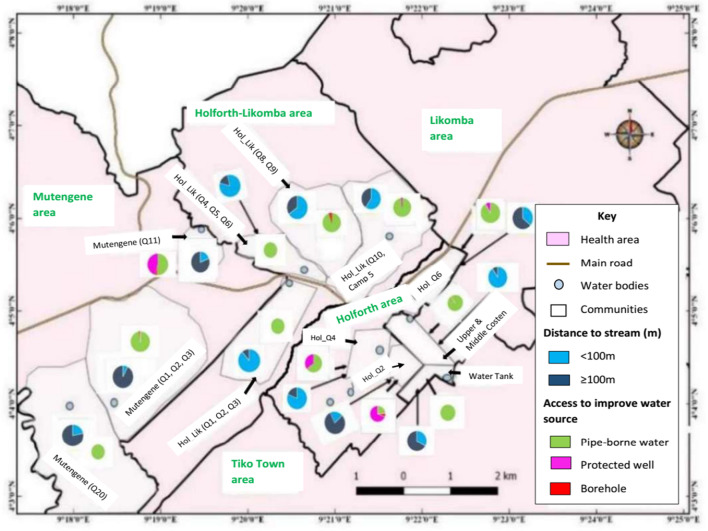
Cartographic analysis
ArcGIS Version 2.18 (Environmental Systems Research Institute, Inc., Redlands, USA) was used to evaluate the spatial distribution of UGS infection and behavioural risk factor (measured by degree of water contact). Types of improved water sources and distance to stream were mapped. Association between the distribution of UGS and explanatory variables were evaluated at community scale (community as geographic unit).
Results
Characteristics of study participants
A total of 1029 individuals (age range: 5–75 years) were enrolled from four HAs namely; Likomba, Holforth-Likomba, Holforth, and Mutengene HAs. For drinking water, domestic and recreational purposes, people living in THD use both the stream and improved water sources (pipe-borne water, boreholes, or protected wells). Despite high access (84.5%) to improved water facilities, more than half of the population reported the use of stream water (Table 1). A considerable number of people rely on the stream for two or more water-related activities such as water collection, laundry, bathing, playing, swimming, fishing, and farming. Compared with household pipe-borne water source, communal water supply is predominant (82.5%) in the area (Table 1), nevertheless, on most occasions, the water supply is irregular (personal observation).
Table 1.
Characteristics of study participants
| Characteristics | Number examined (n) | Proportion (%) |
|---|---|---|
| Health area | ||
| Likomba | 234 | 22.7 |
| Holforth-Likomba | 301 | 29.3 |
| Holforth | 243 | 23.6 |
| Mutengene | 251 | 24.4 |
| Sex | ||
| Male | 525 | 51.0 |
| Female | 504 | 49.0 |
| Age group (years) | ||
| 5–14 | 543 | 52.8 |
| 15–24 | 159 | 15.4 |
| 25–34 | 123 | 12.0 |
| ≥ 35 | 204 | 19.8 |
| Level of education | ||
| At least secondary | 469 | 45.6 |
| At least primary | 560 | 54.4 |
| Occupation | ||
| Housewife | 59 | 5.7 |
| CDC worker | 106 | 10.3 |
| Pupil/student | 659 | 64.0 |
| Business/civil servant | 121 | 11.8 |
| Farmer | 84 | 8.2 |
| Stream usage | ||
| Yes | 563 | 54.7 |
| No | 466 | 45.3 |
| Activities in the stream | ||
| Water collection | 46 | 4.5 |
| Washing | 96 | 9.3 |
| Bathing | 70 | 6.8 |
| Playing/swimming | 24 | 2.3 |
| Farming/fishing | 10 | 1.0 |
| Two or more activities | 317 | 30.8 |
| Reported no contact | 466 | 45.3 |
| Frequency to stream | ||
| Daily | 284 | 50.4 |
| Weekly | 245 | 43.5 |
| Monthly | 34 | 6.1 |
| Source of water | ||
| Improved water source/streama | 563 | 54.7 |
| Improved water source only | 466 | 45.3 |
| Pipe-borne water status | ||
| Communal water | 717 | 82.5 |
| Household water | 152 | 17.5 |
CDC Center for Disease Control and Prevention
aCommunal/household pipe-borne water source, bore hold, protected well
Prevalence of S. haematobium infection in the study area
Schistosoma haematobium infection was not detected in the Mutengene HA. Thus, the overall prevalence of S. haematobium infection in the Likomba, Holforth-Likomba and Holforth HAs was 31.5% [245/778, 95% confidence interval (CI): 28.3–34.8%]. The prevalence of microhaematuria was 24.9% (194/778).
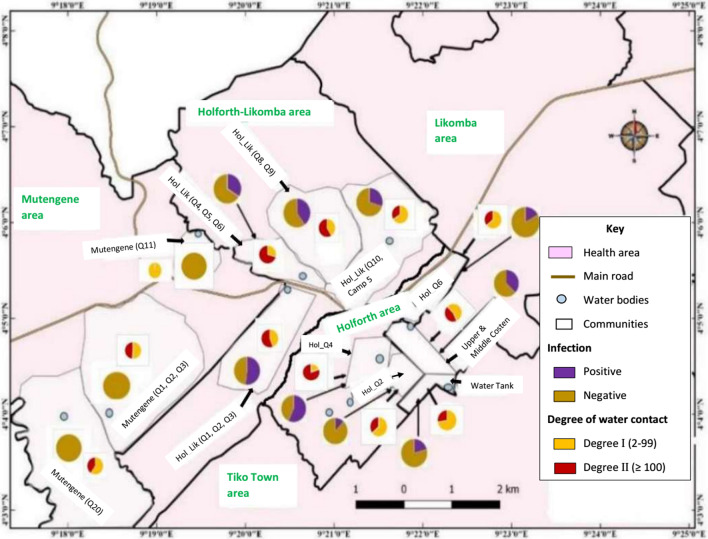
Using urine filtration technique as gold standard, the sensitivity and specificity of urine reagent strip in the diagnosis of S. haematobium infection were 70.3% (95% CI: 63.1–76.7%) and 87.9% (95% CI: 85.1–90.3%), respectively. The Holforth-Likomba HA had the highest prevalence at 38.9% and Holforth HA having the least prevalence (23.5%). Figure 4 shows the spatial distribution of the twelve communities sampled in the four HAs and the respective prevalence of S. haematobium infection ranging from 0 to 56.9%. Nine out of twelve communities were affected. The prevalence of infection varied significantly (χ2 = 66.21; P < 0.001) among the affected communities. According to the endemicity of the disease, UGS was hyperendemic (prevalence ≥ 50%) in Holforth quarter 4 (HOL Q4) and Holforth-Likomba quarter 1, 2, 3 (HOL-LIK Q1, 2, 3) neighbourhoods, and mesoendemic (10% ≤ prevalence < 50%) in the other five communities (Additional file 1).
Fig. 4.
Prevalence of Schistosoma haematobium infection and degree of contact within different communities of Tiko Health District
At the community level, the prevalence of UGS had a significant positive linear relationship (r = 0.8, P = 0.01) with the intensity of contact with water body; as the degree of contact with water increases, the chances of its inhabitants having S. haematobium infection increased. Most of the individuals living in highly affected communities (HOL Q4 and HOL-LIK Q1, 2, 3) indicated residence in proximity (< 100 m) to water bodies (Fig. 4). In addition, the distance of residence to stream was a determinant of infection with S. haematobium (χ2 = 6.65; P = 0.010). This association was particularly evident for HOL Q2 (χ2 = 9.00; P = 0.003) (Additional file 2). More improved water sources (χ2 = 433.65; P < 0.001) were noted in the Holforth HA (Additional file 3). It is worth noting that, HOL Q2 and HOL Q6 communities were less affected by UGS. Individuals living in these neighbourhoods either live far (≥ 100 m) from surface water points or have access to more improved water sources as well as make less contact with surface water (Figs. 4 and 5).
Fig. 5.
Distribution of proximity to stream and access to improved water
source within different communities of Tiko Health District
The univariate analysis of determinant factors of S. haematobium in the THD based on the surveyed sociodemographic and water contact behaviour is summarised in Table 2. The infection was frequent among the age group 5–14 years, pupils/students and individuals who had attained at least secondary level of education. Also, a higher prevalence was observed among those, who made daily contact with stream (χ2 = 173.6; P < 0.001), reported playing and swimming in the stream as well as carry out multiple water contact activities (χ2 = 117.3; P < 0.001) when compared with others in their respective categories.
Table 2.
Univariate analysis of socio-demographic and water contact behaviour associated with urogenital schistosomiasis in the study population
| Variable | Category | Schistosoma haematobium infection, % (n) | χ2 | P value |
|---|---|---|---|---|
| Health area | Likomba | 30.3 (71) | 15.0 | < 0.05 |
| Holforth_Likomba | 38.9 (117) | |||
| Holforth | 23.5 (57) | |||
| Sex | Male | 32.9 (138) | 0.88 | 0.35 |
| Female | 29.8 (107) | |||
| Age group (years) | 5–14 | 37.7 (156) | 22.0 | < 0.05 |
| 15–24 | 31.7 (39) | |||
| 25–34 | 25.8 (24) | |||
| ≥ 35 | 17.6 (26) | |||
| Level of education | Secondary | 35.4 (126) | 4.6 | 0.03 |
| Primary | 28.2 (119) | |||
| Occupation | Housewife | 30.0 (12) | ||
| CDC worker | 18.5 (17) | 18.5 | < 0.05 | |
| Student/Pupil | 36.5 (184) | |||
| Business/Civil servant | 26.3 (21) | |||
| Farmer | 17.7 (11) | |||
| Stream activity | Two/more activities | 53.5 (137) | 117.3 | < 0.05 |
| Water collection | 33.3 (14) | |||
| Washing | 40.3 (25) | |||
| Bathing | 28.3 (15) | |||
| Playing/swimming | 53.8 (7) | |||
| Farming/fishing | 25.0 (2) | |||
| No activity | 13.1 (45) | |||
| Stream frequency | Daily | 62.4 (159) | 173.6 | < 0.05 |
| Weekly | 21.5 (32) | |||
| Monthly | 30.0 (9) | |||
| Degree of contacta | Degree II (≥ 100) | 64.2 (145) | 62.0 | < 0.05 |
| Degree I (2–99) | 26.4 (55) |
CDC Center for disease control and prevention
aΣ (R × F), where R is the score for the reason for the contact and F the score for the frequency of contact
Intensity of S. haematobium egg excretion and associated clinical outcome
Egg excretion was recorded for 172 among whom 61.4% (105/172) (< 50 eggs/ 10 ml urine) had light infection while 38.6% (66/172) (≥ 50 eggs/10 ml of urine) had heavy infection. The geometric mean (GM) egg count was 28.7 eggs per 10 ml of urine (range: 2–450) with no significant variability (P = 0.55) among the different HAs (Table 3). Mean egg count decreased significantly (P = 0.02) with increased age, where the 5–14 years age group had the highest egg load excretion and the least egg counts were recorded among older individuals (25–34 and ≥ 35 years). In addition, intense contact with stream (degree II) was associated with higher egg load excretion than less contact with stream (degree I). The difference was highly significant (P < 0.001). While more individuals with light infection (P < 0.001) showed no urothelial clinical symptoms when compared with heavy infection, higher mean egg count was associated with the presence of microhaematuria and proteinuria (Table 3).
Table 3.
Intensity of Schistosoma haematobium infection in the study population stratified according to socio-demographic, water contact behaviour and clinical presentation
| Factors | Intensity of infection | χ2 | P value$ | GM egg load/10 ml urine | Range/10 ml urine | P value | |
|---|---|---|---|---|---|---|---|
| Light % (n) | Heavy % (n) | ||||||
| Health area | |||||||
| Likomba | 60.4 (29) | 39.6 (19) | 0.46 | 0.79 | 25.8 | 2–317 | 0.55b |
| Holforth_Likomba | 60.0 (48) | 40.0 (32) | 26.9 | 2–450 | |||
| Holforth | 65.9 (29) | 34.1 (15) | 36.4 | 2–225 | |||
| Sex | |||||||
| Male | 59.3 (67) | 40.7 (46) | 0.76 | 0.38 | 29.5 | 2–450 | 0.76a |
| Female | 66.1 (39) | 33.9 (20) | 27.3 | 2–400 | |||
| Age group (years) | |||||||
| 5–14 | 57.6 (72) | 42.4 (53) | 5.57 | 0.13 | 34.4 | 2–450 | 0.02*b |
| 15–24 | 69.0 (20) | 31.0 (9) | 22.2 | 2–330 | |||
| 25–34 | 90.9 (10) | 9.1 (1) | 10.2 | 2–53 | |||
| ≥ 35 | 57.1 (4) | 42.9 (3) | 16.8 | 2–216 | |||
| Level of education | |||||||
| Secondary | 57.0 (49) | 43.0 (37) | 1.53 | 0.21 | 29.4 | 2–317 | 0.65a |
| Primary | 66.3 (57) | 33.7 (29) | 28.1 | 2–450 | |||
| Occupation | |||||||
| Housewife | 80.0 (4) | 20.0 (1) | 3.81 | 0.34 | 25.8 | 9–57 | 0.17b |
| CDC worker | 81.8 (9) | 18.2 (2) | 11.6 | 2–216 | |||
| Student/Pupil | 59.4 (85) | 40.6 (58) | 31.9 | 2–450 | |||
| Business/Civil servant | 75.0 (6) | 25.0 (2) | 17.8 | 3–330 | |||
| Farmer | 40.0 (2) | 60.0 (3) | 24.7 | 2–183 | |||
| Stream activity | |||||||
| Two/more activities | 58.6 (68) | 41.4 (48) | 11.4 | 0.08 | 31.3 | 2–400 | 0.04*b |
| Water collection | 75.0 (6) | 25.0 (2) | 17.1 | 2–450 | |||
| Washing | 81.8 (18) | 18.2 (4) | 25.3 | 5–330 | |||
| Bathing | 53.3 (8) | 46.7 (7) | 31.7 | 3–280 | |||
| Playing/swimming | 33.3 (2) | 66.7 (4) | 55.4 | 7–215 | |||
| Farming/fishing | 0.0 (0) | 100.0 (1) | 54.0 | – | |||
| No contact | 100.0 (4) | 0.0 (0) | 2.9 | 2–4 | |||
| Stream frequency | |||||||
| Daily | 55.2 (80) | 44.8 (65) | 16.37 | 0.001 | 33.8 | 2–450 | < 0.001*b |
| Weekly | 94.1 (16) | 5.9 (1) | 15.6 | 5–51 | |||
| Monthly | 100.0 (6) | 0.0 (0) | 14.5 | 7–34 | |||
| No contact | 100.0 (4) | 0.0 (0) | 2.9 | 2–4 | |||
| Degree of contact | |||||||
| Degree II (≥ 100) | 53.7 (72) | 46.3 (62) | 13.54 | < 0.001 | 35.9 | 2–400 | < 0.001*a |
| Degree I (2–99) | 88.2 (30) | 11.8 (4) | 15.5 | 2–450 | |||
| Microhaematuria | |||||||
| Yes | 50.4 (61) | 49.6 (60) | 21.7 | < 0.001 | 40.1 | 2–450 | < 0.001*a |
| No | 88.2 (45) | 11.8 (6) | 13.0 | 2–280 | |||
| Dysuria | |||||||
| Yes | 85.7 (12) | 14.3 (2) | 3.74 | 0.05 | 22.8 | 2–450 | 0.47 a |
| No | 59.5 (94) | 40.5 (64) | 29.3 | 2–400 | |||
| Frequent urination | |||||||
| Yes | 37.5 (3) | 62.5 (5) | 2.06 | 0.15 | 22.8 | 2–450 | 0.25a |
| No | 62.8 (103) | 37.2 (61) | 29.3 | 2–400 | |||
| Proteinuria | |||||||
| Yes | 48.3 (43) | 51.7 (46) | 13.82 | < 0.001 | 41.2 | 2–450 | < 0.001*a |
| No | 75.9 (63) | 24.1 (20) | 19.5 | 2–280 | |||
GM geometrical mean, CDC Center for Disease Control and Prevention
aDifference in egg load determined by Mann–Whitney U test
bDifference in egg load determined by Kruskal–Wallis test
$Values are from Pearson Chi square test
*Statistically significant P value
Risk factors associated with S. haematobium infection in the THD
The binary logistic regression analysis presents determinant factors associated with the risk of S. haematobium infection based on sociodemographic factors and water contact behaviour in THD (Table 4). The most important factors associated with infection in the study area were age, secondary level of education and degree of water contact. Individuals in the younger age group (5–14 years) were observed to be 3.7 times (95% CI: 1.1–12.2) more likely to be infected when compared with those of the older age groups. More so, individuals who had secondary level of education were twice (95% CI: 1.2–3.2) more likely to be infected with S. haematobium compared with those who had at most primary level of education. Participants who were classified as having high degree contact (degree II) with water had 5.2 times increased odds (95% CI: 3.4–8.1) of infection.
Table 4.
Risk factors associated with Schistosoma haematobium infection in the Tiko health district
| Factors | % (n) positive | Unadjusted OR | 95% CI | P value$ | #Adjusted OR | 95% CI | P value |
|---|---|---|---|---|---|---|---|
| Health area | |||||||
| Likomba | 30.3 (71) | 1.4 | 0.9–2.1 | < 0.05 | 1.3 | 0.7–2.3 | 0.44 |
| Holforth_Likomba | 38.9 (117) | 2.1 | 1.4–3.0 | 1.2 | 0.7–2.1 | 0.40 | |
| Holforth | 23.5 (57) | REF | REF | ||||
| Sex | |||||||
| Male | 32.9 (138) | 1.07 | 0.9–1.2 | 0.35 | 1.2 | 0.8–1.9 | 0.33 |
| Female | 29.8 (107) | REF | REF | ||||
| Age group (years) | |||||||
| 5–14 | 37.7 (156) | 3.8 | 1.8–4.5 | < 0.05 | 3.7 | 1.1–12.2 | 0.03 |
| 15–24 | 31.7 (39) | 2.18 | 1.2–3.8 | 2.5 | 0.8–8.2 | 0.13 | |
| 25–34 | 25.8 (24) | 1.63 | 0.9–3.1 | 2.6 | 0.9–7.3 | 0.07 | |
| ≥ 35 | 17.6 (26) | REF | REF | ||||
| Level of education | |||||||
| Secondary | 35.4 (126) | 1.2 | 1.0–1.4 | 0.03 | 2.0 | 1.2–3.2 | 0.005 |
| Primary | 28.2 (119) | REF | REF | ||||
| Occupation | |||||||
| Housewife | 30.0 (12) | 2.0 | 0.8–5.1 | < 0.05 | 1.2 | 0.3–6.2 | 0.78 |
| CDC worker | 18.5 (17) | 1.0 | 0.4–2.4 | 0.9 | 0.2–3.1 | 0.83 | |
| Pupil/student | 36.5 (184) | 2.7 | 1.3–5.2 | 1.0 | 0.3–3.7 | 0.94 | |
| Business/Civil servant | 26.2 (21) | 1.6 | 0.7–3.7 | 2.5 | 0.7–8.4 | 0.15 | |
| Farmer | 17.7 (11) | REF | REF | ||||
| Source of pipe-borne water | |||||||
| Household pipe-borne water | 34.7 (195) | 1.0 | 0.9–1.1 | 0.32 | NA | NA | |
| Communal pipe-borne water | 29.8 (34) | REF | |||||
| Degree of water contact | |||||||
| Degree II (≥ 100) | 64.2 (145) | 2.0 | 1.7–2.5 | < 0.05 | 5.2 | (3.4–8.1) | < 0.05 |
| Degree I (2–99) | 26.4 (55) | REF | REF | ||||
CDC Center for Disease Control and Prevention, CI confidence interval, OR odd ratio, NA not applicable
$Pearson Chi-square test
#Adjusted OR using multivariate regression analysis
Discussion
The current study reports on the distribution of S. haematobium infection in THD and an unmapped transmission focus in the Mount Cameroon area [24]. Our study confirms that S. haematobium transmission occurs in Likomba, Holforth-Likomba and Holforth HAs with the occurrence of infection at 31.5%. No evidence of human host infection was recorded in Mutengene HA. Although, THD can be classified as moderate risk endemic area [11], the infection levels in affected communities varied from meso to hyperendemic (12.0–56.9%). The occurrence of UGS in THD is linked partly to the presence and use of many fresh waterbodies (such as Moungo River) and its tributaries, which intersperse the Mount Cameroon Area. Also, proximity to stream, intense water contact activities and inadequate improved water sources are important drivers of transmission of S. haematobium in the district.
Compared with the prevalence of UGS in THD, lower rates have been observed in some urban and semi-urban settings in other Regions of Cameroon: 1.7% in Kékem [35] and 22.9% in Maroua [36]. These areas are targeted regularly for control of schistosomiasis and geohelminths and thus account for the lower prevalence of schistosomiasis in these areas [35]. It is interesting that Mutengene HA which is about 250 m away from Likomba HA had zero prevalence. Mutengene is located at a higher altitude [220 m above sea level (asl)] with a hilly topographic terrain characterized by fast flow of the “Ndongo” stream which slows as it meanders across the Tiko and Limbe towns. The influence of topography on Schistosoma parasite transmission has been emphasized [37]. A study in Nigeria reported absence of schistosomiasis in communities located at higher altitudes [38]. Conversely, lower altitudes could have a significant impact on the Schistosoma snail vector distributions, which are likely to be more concentrated in areas where there is a slow water current [39]. This may explain the predominance of UGS in the Likomba and Holforth HAs located at a lower altitude (18–80 m asl). It is also possible that far distance to and infrequent contact with water bodies may prevent establishment and transmission of S. haematobium in the Mutengene HA, however, this remains to be determined.
Among the nine affected communities, five namely: LK-UC/MC; HOL-LKQ1,2,3; HOL-LKQ4,5,6; HOL-LKQ 8,9 and HOLQ6 had infection > 31.0% with HOL-LKQ 1,2,3 (52.0%) and HOL-LKQ4 (56.9%) observed as high-risk communities (≥ 50%). Majority (> 80%) of the residents in these communities live very close to the stream and are equally involved in intense contact with surface water. On the other hand, low prevalence of infection in communities like HOL Q2 (12.5%) and HOL Q6 (17.0%) may be linked to the fact that most of the people live far (≥ 100 m) (80.0% for HOL Q2 and 63.8% for HOL Q6) from open water surface and have access to alternative improved water sources such as protected wells and boreholes [40]. Our findings strongly demonstrate the focal transmission pattern of schistosomiasis which suggests strategic control of this disease. The maps obtained provide information about the areas where studies and control efforts need to be focused. Preventive chemotherapy with praziquantel should be immediately put in place to prevent morbidity and interrupt transmission. Nevertheless, a malacological study on the distribution of snail intermediate hosts is crucial to elucidate the epidemiology of infection in the THD.
The prevalence of S. haematobium decreased with age where school-aged children (5–14 years) are associated with higher odds and intensity of S. haematobium infection. This agrees with trends established in surveys carried out in Cameroon [21, 41] and other parts of Africa [18, 42]. Individuals of this age group are predisposed to schistosome infections due to their active life; hence increased water contact activities with cercaria infested streams [18]. Children are the most infected group of people in endemic areas, thus contributes significantly to the potential contamination of the aquatic environment [43]. Age-acquired immunity to reinfection underlies the declining trend in infection with increasing age [44].
The education level of the inhabitants was also strongly associated with the transmission of S. haematobium. Contrary to findings in Munyenge, Mount Cameroon Area [45], secondary level of education increased the odds of infection when compared with primary level of education. There is no distinct reason why individuals with secondary education had higher prevalence of infection. However, from statistical analysis, it is reasonable to suggest that the active age group (11–24 years) may fall more into the secondary education category. In Nigeria, the age group 11–20 years was the most active age group frequently engaging in activities that bring them in contact with infested water bodies [46].
The sex dependent pattern of schistosome infections is widely reported [43]. Conversely, the prevalence of infection in males and females was similar in our study. It is likely that, socioeconomic conditions, and habits in the THD could modify sex-biased tendencies towards water contact behaviour [18, 40]. Males and females equally participate in water activities such as bathing, swimming, and laundry, which served as major predisposing factors. Previous studies in Nigeria [47], Cote d’Ivoire [18] and Cameroon [8] have reported similar observations.
Despite the presence of improved water facilities in the HAs, about 50% of the population visit the stream daily and one-third of those who use the stream, engage in two or more water-related activities. In most countries where schistosomiasis is endemic, inadequate access to clean water sources is major concern [48]. Distance from home, limited number of communal piped-borne water sources and requirement for immediate payment of piped-borne water are leading causes for limited access to water [45, 49]. Many natural water bodies, infested with snails and schistosome cercariae, are common sources for domestic water in most schistosomiasis endemic areas [50]. In THD, the flow of pipe-borne water is inconsistent, consequently, streams and springs are common sources of water for majority of the people in this District. Usually people become infected with schistosomes when they make contact with infested water and cercariae penetrate the skin. Humans excrete eggs in water bodies through faecal or urine contamination, the eggs hatch into miracidia which finds and penetrate the snail intermediate hosts. In the snail host, the parasite develops into cercariae which are infective to humans [51]. The high dependence of the population on natural water bodies avails each water contact activity a potential risk factor of S. haematobium infection [52]. Intense water contact activity and daily visitation to stream (degree II) was associated with increased risk and intensity of S. haematobium infection. This confirms previous reports in other endemic foci in Cameroon [8, 45, 53] and elsewhere [54]. Water contact at any point in time is linked mostly to practices including domestic activities and bathing. Laundry, bathing, and recreational swimming are the activities that cause the most exposure to cercaria-infested water because these activities do involve the immersion of large body parts, for long periods [31].
This study had some limitations. Only four out of eight HAs were surveyed due to inaccessibility. Future studies to survey the other communities are important and will provide a clearer picture of UGS in the entire district. Secondly, this study relied only on statistical methods to establish the transmission of S. haematobium infection and associated factors in THD. Malacological studies are crucial to confirm that the streams are infested with snails which harbour the infective larvae of the parasite.
Conclusions
THD is a moderate risk endemic focus for UGS with an overall prevalence of 31.5%. Transmission occurs in Likomba, Holforth-Likomba and Holforth HAs and was not observed in Mutengene HA. The infection level varied significantly among affected communities from meso- to hyperendemic (12.0–56.9%). Proximity to stream, intense contact with stream and access to more improved water sources determined infection status of the communities. Among the participants, determinant factors associated with risk of S. haematobium infection and higher egg load excretion were younger age (5–14 years) and high degree of contact with open water surface. A malacological study on snail intermediate host (s) distribution and infectivity is fundamental to elucidate the mechanisms of S. haematobium transmission in THD. Nevertheless, control measures to effectively control and eventually eliminate the infection in this area will entail mass drug administration of praziquantel to affected communities, provision of safe and adequate water supply, health education, and snail control.
Supplementary Information
Additional file 1: Variation in the occurrence of Schistosoma haematobium infection among affected communities in Tiko Health District
Additional file 2: The prevalence of Schistosoma haematobium infection in relation to distance to stream in the different communities in Tiko Health District
Additional file 3: Reported access to improved water sources among the affected communities in Tiko Health District
Acknowledgements
The authors appreciate the support and cooperation of the inhabitants, parents and guardians of the children in THD, the health personnel, and laboratory technicians who took part in the study.
Abbreviations
- THD
Tiko Health District
- CHW
Community Health Worker
- UGS
Urogenital schistosomiasis
- SWR
South west region
- WASH
Water, sanitation and hygiene
Authors’ contributions
AEG: Participated in the design of the study, performed the experiments, and made inputs in manuscript write-up. JKAK: Conceived and designed the study and wrote the manuscript. WGB: Performed the experiment and analyzed the data. VD: Performed the experiment. HKK: Supervised, reviewed, and provided inputs to the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the staff development grant and special fund for research and modernization given to some authors by the Government of Cameroon.
Availability of data and materials
All data sets on which the conclusions of the research rely are presented in the paper and its supplementary file. However, data is available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Ethical clearance (2019/922-01/UB/SG/IRB/FHS) was obtained from the Faculty of Health Sciences Institutional Review Board the University of Buea, and administrative authorisation from the South West Regional Delegation of Public Health, Buea and District Medical Officer for Tiko Subdivision. Written and verbal informed consent was obtained before enrolment into the study. All participants positive for UGS were freely treated with praziquantel tablets (40 mg/kg of body weight) in collaboration with the local health authorities. Each participant was free to withdraw consent at any time. Identification codes were assigned to each study participant and limited access to study data was maintained to ensure confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.World Health Organization. Schistosomiasis fact sheet. 2020. https://www.who.int/news-room/fact-sheets/detail/schistosomiasis. Accessed 21 Feb 2021
- 2.Sturrock RF. The parasite and their life cycles. In: Jordan P, Webbe G, editors. Human schistosomiasis. Wallingford: CAB International; 1993. pp. 1–32. [Google Scholar]
- 3.Brooker S, Kabatereine NB, Smith JL, Mupfasoni D, Mwanje MT, et al. An updated atlas of human helminth infections: the example of East Africa. Int J Health Geogr. 2009;8:42. doi: 10.1186/1476-072X-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2016 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study. Lancet. 2016;390(10100):1260–1344. doi: 10.1016/S0140-6736(17)32130-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Werf MJ, de Vlas SJ, Brooker S, Looman CW, Nagelkerke NJ, Habbema JDF, et al. Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Trop. 2003;86(2–3):125–139. doi: 10.1016/S0001-706X(03)00029-9. [DOI] [PubMed] [Google Scholar]
- 6.Senghor B, Diaw OT, Doucoure S, Seye M, Diallo A, Talla I, et al. Impact of annual praziquantel treatment on urogenital schistosomiasis in sasonal transmission focus in central Senegal. PLoS Negl Trop Dis. 2016;10(3):e0004557. doi: 10.1371/journal.pntd.0004557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silva PB, Barbosa CS, Pieri O, Travassos A, Florencio L. Physico-chemical and biological aspects related to the occurrence of Biomphalaria glabrata in foci of schistosomiasis in coastal areas of the state of Pernambuco, Brazil. Quim Nova. 2006;29:901–6.
- 8.Ndassi VD, Anchang-Kimbi JK, Sumbele IUN, Wepnje GB, Kimbi HK. Prevalence and risk factors associated with S.haematobium egg excretion during the dry season, six months following mass distribution of praziquantel (PZQ) in 2017 in the Bafia Health Area, South West Region Cameroon: a cross-sectional study. J Parasitol Res. 2019;19:4397263. doi: 10.1155/2019/4397263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olds GR, Olveda R, Wu G. Immunity and morbidity in schistosomiasis japonicum infection. Am J Trop Med Hyg. 1996;55:121–126. doi: 10.4269/ajtmh.1996.55.121. [DOI] [PubMed] [Google Scholar]
- 10.Hotez PJ, Savioli L, Fenwick A. Neglected tropical diseases of the Middle East and North Africa: review of their prevalence, distribution, and opportunities for control. PLoS Negl Trop Dis. 2012;6:e1475. doi: 10.1371/journal.pntd.0001475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO . Preventive chemotherapy in human helminthiasis: coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers. Geneva: WHO Press; 2006. [Google Scholar]
- 12.Grimes JET, Croll D, Harrison WE, Utzinger J, Freeman MC, Templeton MR. The roles of water, sanitation and hygiene in reducing schistosomiasis: a review. Parasit Vectors. 2015;8:156. doi: 10.1186/s13071-015-0766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dabo A, Diarra AZ, Machault V, Touré O, Niambélé DS, Kanté A, et al. Urban schistosomiasis and associated determinant factors among school children in Bamako, Mali, West Africa. Infect Dis Poverty. 2015;4:4. doi: 10.1186/2049-9957-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ernould JC, Kaman AK, Labbo R, Couret D, Chippaux JP. Recent urban growth and urinary schistosomiasis in Niamey. Niger Trop Med Int Health. 2000;5(6):431–437. doi: 10.1046/j.1365-3156.2000.00577.x. [DOI] [PubMed] [Google Scholar]
- 15.Olaseha IO, Sridhar MKC. Participatory action research: community diagnosis and intervention in controlling urinary schistosomiasis in an urban community in Ibadan, Nigeria. Int Q Community Health Edu. 2004;24(2):153–160. doi: 10.2190/CBYM-94N2-E7DH-QRAL. [DOI] [PubMed] [Google Scholar]
- 16.Amsalu G, Mekonnen Z, Erko B. A new focus of schistosomiasis mansoni in Hayk town, northeastern Ethiopia. BMC Res Notes. 2015;8:2. doi: 10.1186/s13104-014-0965-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Z, Nie X, Zhang Y, Huang J, Huang B, Zeng G. Assessing the influence of water level on schistosomiasis in Dongting Lake region before and after the construction of Three Gorges Dam. Environ Monit Assess. 2016;188:28. doi: 10.1007/s10661-015-5033-1. [DOI] [PubMed] [Google Scholar]
- 18.M’Bra RK, Kone B, Yapi YG, Silué KD, Sy I, Vienneau D, et al. Risk factors for schistosomiasis in an urban area in northern Côte d’Ivoire. Infect Dis Poverty. 2018;7:47. doi: 10.1186/s40249-018-0431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hotez PJ, Molyneux DH, Fenwick A, Kumaresan J, Sonia PH, Sachs SE, et al. Review, cerrent concepts: control of neglected tropical diseases. N Engl J Med. 2007;357:1018–1027. doi: 10.1056/NEJMra064142. [DOI] [PubMed] [Google Scholar]
- 20.Ndamukong KJ, Ayuk MA, Dinga JS, Akenji TN, Ndiforchu VA, Titanji VP. The pattern of soil- transmitted nematode infections in primary school children of Kumba Health District, South-West, Cameroon. Afr J Health Sci. 2000;7:103–106. [PubMed] [Google Scholar]
- 21.Ntonifor HN, Mbunkur GN, Ndaleh NW. Epidemiological survey of urinary schistosomiasis in some primary schools in a new focus behind Mount Cameroon (Munyenge), South West Region, Cameroon. East Afri Med J. 2012;89(3):82–88. [PubMed] [Google Scholar]
- 22.Kimbi HK, Wepnje G, Anchang-Kimbi J, Tonga C, Ayukenchengamba B, Njabi C, et al. Active case detection and prevalence of urinary schistosomiasis and malaria in pupils of Kotto Barombi, Southwest Cameroon using the CyScope® fluorescence microscope. Int J Trop Dis Health. 2015;8(1):1–12. doi: 10.9734/IJTDH/2015/17109. [DOI] [Google Scholar]
- 23.Ebai CB, Kimbi HK, Sumbele IUN, Yunga JE, Lehman LG. Prevalence and risk factors of urinary schistosomiasis in the Ikata-Likoko area of Southwest Cameroon. Int J Trop Dis Health. 2016;17(2):1–10. doi: 10.9734/IJTDH/2016/26669. [DOI] [Google Scholar]
- 24.Anguh E, Ako S, Numfor EZ, Bimabam J, Ndassi V. Presence of an unmapped focus for urogenital schistosomiasis in the Tiko Health District in Cameroon: implications for control. Int J Trop Dis Health. 2018;32(2):1–8. doi: 10.9734/IJTDH/2018/43575. [DOI] [Google Scholar]
- 25.Tabi ESB, Eyong EM, Akum EA, Löve J, Cumber SN. Soil-transmitted helminth infection in the Tiko Health District, South West Region of Cameroon: a post-intervention survey on prevalence and intensity of infection among primary school children. Pan Afr Med J. 2018;30:74. doi: 10.11604/pamj.2018.30.74.15676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Human Rights Watch. World Report 2019: Cameroon. New York, USA. 2018. http://www.hrw.org/world-report/2019/country-chapters/cameroon. Accessed 22 Oct 2020.
- 27.Neglected Tropical Disease Data base for the distribution of mectizan and albendazole for the South West Region, Cameroon. 2017. p 9.
- 28.Thieltges D, Jensen K, Poulin R. The role of Biotic factors in the transmission of free-living endohelminth stages. Parasitology. 2008;135:407–426. doi: 10.1017/S0031182007000248. [DOI] [PubMed] [Google Scholar]
- 29.Mass Drug Administration (MDA) synthesis report for Tiko Health District. 2017. P 1.
- 30.Yamane T. Statistics: an introductory analysis. 2. New York: Harper and Row; 1967. p. 919. [Google Scholar]
- 31.Lima E, Costa MFF, Magalhaes MHAR, Rocha S, Antunes CMF, Katz N. Water-contact patterns and socioeconomic variables in the epidemiology of schistosomiasis mansoni in an endemic area in Brazil. Bull World Health Organ. 1987;65(1):57–66. [PMC free article] [PubMed] [Google Scholar]
- 32.Christensen NO, Gotsche G, Frandsen F. Parasitological techniques for use in routine laboratory maintenance of schistosomes and used in studies on the epidemiology of human and bovine schistosomiasis. Danish Bilharziasis laboratory manual; 1984. p112.
- 33.WHO. Guidelines for the Evaluation of Soil Transmitted Helminthiasis and Schistosomiasis at Community Level: A Guide for Managers of Control Programme, World Health Organisation, Geneva, Switzerland, 1998. p 45.
- 34.WHO. Prevention and control of schistosomiasis and soil transmitted Helminthiasis. Report of a WHO Expert Committee. Technical Report series. 2002; No 912. pp. 63 Geneva, World Health Organization. [PubMed]
- 35.Tchuem Tchuente L-A, Kamwa Ngassam RI, Sumo L, Ngassam P, Dongmo Noumedem C, et al. Mapping of schistosomiasis and soil-transmitted helminthiasis in the regions of Centre, East and West Cameroon. PLoS Negl Trop Dis. 2012;6(3):e1553. doi: 10.1371/journal.pntd.0001553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saotoing P, Vroumsia T, Am N, Tchuenguem FN, Messi J. Epidemiological survey of schistosomiasis due to Schistosoma haematobium in some primary schools on the town of Maroua, far north region Cameroon. Int J Trop Med. 2011;6(2):19–24.
- 37.Leonardo LR, Rivera PT, Crisostoma BA, Sarol JN, Bantayan NC, Tiu WU, et al. A study of the environmental determinants of malaria and schistosomiasis in the Philippines using remote sensing and geographic information system. Parasitologia. 2005;47:105–114. [PubMed] [Google Scholar]
- 38.Adie HA, Okon OE, Arong G, Ekpo UF, Braide EI. Environmental factors and distribution of urinary schistosomiasis in Cross River State, Nigeria. Int J Zool Res. 2014;10(2):42–58. doi: 10.3923/ijzr.2014.42.58. [DOI] [Google Scholar]
- 39.Kihara JH, Kutima HL, Ouma J, Churcher TS, Changoma JM, Mwalisetso MA, et al. Urogenital schistosomiasis in women of reproductive age and pregnant mothers in Kwale County, Kenya. J Helminthol. 2015;89:105–111. doi: 10.1017/S0022149X13000643. [DOI] [PubMed] [Google Scholar]
- 40.Ndukwe YE, Obiezue RN, Aguzie ION, Anunobi JT, Okafor FC. Mapping of urinary schistosomiasis in Anambra State, Nigeria. Ann Glob Health. 2019;85(1):52. doi: 10.5334/aogh.2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sama TM, Oyono E, Retard RC. High risk behaviours and schistosomiasis infection in Kumba, South West Province, Cameroon. Int J Environ. 2007;4:101–105. doi: 10.3390/ijerph2007040003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chipeta MG, Ngwira B, Kazembe LN. Analysis of schistosomiasis haematobium infection prevalence and intensity in Chikhwawa, Malawi: AN application of a two-part model. PLoS Negl Trop Dis. 2013;7:e2131. doi: 10.1371/journal.pntd.0002131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anosike EC, Njoku AJ, Nwoke BEB, Ajero CMU, Osagiede UR, Okoro OU, et al. Epidemiology of urinary schistosomiasis in Ebonyi state, Nigeria. Int J Env Health Hum Dev. 2002;3(1):59–63. [Google Scholar]
- 44.Etard JF, Audibert M, Dabo A. Age-acquired resistance and predisposition to reinfection with Schistosoma haematobium after treatment with praziquantel in Mali. Am J Trop Med Hyg. 1995;52(6):549–58. [DOI] [PubMed]
- 45.Wepnje GB, Anchang-Kimbi JK, Ndassi VD, Lehman LG, Kimbi HK. Schistosoma haematobium infection status and its associated risk factors among pregnant women in Munyenge, South West Region, Cameroon following scale-up of communal piped water sources from 2014 to 2017: a crosss-ectional study. BMC Public Health. 2019;19:e392. [DOI] [PMC free article] [PubMed]
- 46.Afiukwa FN, Nwele DE, Uguru OE, Ibiam GA, Onwe CS, Ikpo AU, et al. Transmission dynamics of urogenital schistosomiasis in the rural community of Ebonyi State, South Eastern Nigeria. J Parasitol Res. 2019;2019:7596069. doi: 10.1155/2019/7596069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Okeke OC, Ubachukwu PO. Urinary schistosomiasis in urban and semi-urban communities in South-Eastern Nigeria. Iran J Parasitol. 2013;8(3):467. [PMC free article] [PubMed] [Google Scholar]
- 48.WHO Schistosomiasis: Number of people treated worldwide in 2014. Wkly Epidemiol Rec. 2016;91(5):53–60. [PubMed] [Google Scholar]
- 49.Abe M, Muhoho DN, Sunahara T, Moji K, Yamamoto T, Aoki Y. Effect of communal piped water supply on pattern of water use and transmission of Schistosoma haematobium in an endemic area of Kenya. Trop Med Health. 2009;37(2):43–53.
- 50.Tchuenté LAT, Rollinson D, Stothard JR, Molyneux D. Moving from control to elimination of schistosomiasis in sub-Saharan Africa: time to change and adapt strategies. Infect Dis Poverty. 2017;6(1):42. doi: 10.1186/s40249-017-0256-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Colley DG, Bustinduy AL, Secor WE, King CH. Human schistosomiasis. Lancet. 2014;383:2253–2264. doi: 10.1016/S0140-6736(13)61949-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sama MT, Ratard RC. Water contact and schistosomiasis infection in Kumba, south-western Cameroon. Ann Trop Med Parasitol. 1994;88(6):629–634. doi: 10.1080/00034983.1994.11812914. [DOI] [PubMed] [Google Scholar]
- 53.Njunda AL, Emmanuel NN, Jules CN, Kamga H, Emmanuel TK. Prevalence and factors associated with urogenital schistosomiasis among primary school children in barrage, Magba sub-division of Cameroon. BMC Public Health. 2017;17:618. doi: 10.1186/s12889-017-4539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anto F, Asoala V, Adjuik M, Anyorigiya T, Oduro A, Akazili J, Akweongo P, Ayivor P, Bimi L, Hodgson A. Water contact activities and prevalence of schistosomiasis infection among school-age children in communities along an irrigation scheme in rural Northern Ghana. J Bacteriol Parasitol. 2013;4:4. doi: 10.4172/2155-9597.1000177. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Variation in the occurrence of Schistosoma haematobium infection among affected communities in Tiko Health District
Additional file 2: The prevalence of Schistosoma haematobium infection in relation to distance to stream in the different communities in Tiko Health District
Additional file 3: Reported access to improved water sources among the affected communities in Tiko Health District
Data Availability Statement
All data sets on which the conclusions of the research rely are presented in the paper and its supplementary file. However, data is available from the corresponding author upon reasonable request.