Abstract
Background:
In June 2020, the National Academies of Sciences, Engineering, and Medicine hosted a virtual workshop focused on integrating the science of aging and environmental health research. The concurrent COVID-19 pandemic and national attention on racism exposed shortcomings in the environmental research field’s conceptualization and methodological use of race, which have subsequently hindered the ability of research to address racial health disparities. By the workshop’s conclusion, the authors deduced that the utility of environmental aging biomarkers—aging biomarkers shown to be specifically influenced by environmental exposures—would be greatly diminished if these biomarkers are developed absent of considerations of broader societal factors—like structural racism—that impinge on racial health equity.
Objectives:
The authors reached a post-workshop consensus recommendation: To advance racial health equity, a “compound” exposome approach should be widely adopted in environmental aging biomarker research. We present this recommendation here.
Discussion:
The authors believe that without explicit considerations of racial health equity, people in most need of the benefits afforded by a better understanding of the relationships between exposures and aging will be the least likely to receive them because biomarkers may not encompass cumulative impacts from their unique social and environmental stressors. Employing an exposome approach that allows for more comprehensive exposure–disease pathway characterization across broad domains, including the social exposome and neighborhood factors, is the first step. Exposome-centered study designs must then be supported with efforts aimed at increasing the recruitment and retention of racially diverse study populations and researchers and further “compounded” with strategies directed at improving the use and interpretation of race throughout the publication and dissemination process. This compound exposome approach maximizes the ability of our science to identify environmental aging biomarkers that explicate racial disparities in health and best positions the environmental research community to contribute to the elimination of racial health disparities. https://doi.org/10.1289/EHP8392
Introduction
A Pandemic, a Movement, and a Workshop
In June, 2020, with the concurrent backdrop of a global COVID-19 pandemic (that has disproportionately impacted racial/ethnic minorities) (Sze et al. 2020) and growing national outrage over unremitting racism (institutional and interpersonal) (Churchwell et al. 2020), the National Academies of Sciences, Engineering, and Medicine (NASEM) hosted a virtual workshop focused on integrating the science of aging and environmental health research (NASEM 2020). NASEM convened leading scientists—representing multiple disciplines—from across the United States to discuss emerging findings integral to advancing our understanding of aging and environmental exposures. Appropriately, current events illuminated limitations in our conceptual and methodological approaches that subsequently create shortfalls in our ability to use our research to address health disparities. Recent events simultaneously spurred deeper reflection on how we as environmental researchers can design and mobilize our future research to help address the systemic marginalization of disenfranchised populations. Importantly, it is the authors’ opinion that achieving a more equitable health future involves instituting changes in our field that address and mitigate the disparities stemming from our past behaviors and inaction, while remaining ever-vigilant of how current research and innovation in environmental research potentially creates, sustains, and exacerbates the disparities we are trying to eliminate.
In the specific circumstance of biomarkers reflecting environmental exposures (i.e., exposure biomarkers) and nonmutually exclusive biomarkers reflecting physiological changes in human aging (i.e., aging biomarkers), it is the authors’ view that there remains a need to consider the utility of these biological measures across race and ethnicity and in the broader contexts of structural factors, such as racism. Research on the various single-cell, epigenetic, omics, and telomere biomarkers discussed at the NASEM workshop undoubtedly provide novel opportunities for understanding the biological and phenotypic relationships between environmental toxicants and aging processes. However, the authors maintain that it is simply insufficient to ask whether new exposure and aging biomarkers can substantially improve our ability to understand these interconnected relationships. The authors believe that the field must also consider “for whom” these relationships apply, ensure that the “whom” is as inclusive as possible, and understand the contexts that shape such relationships.
A Compound Exposome Scope
Environmental aging biomarkers—that is, current and future aging biomarkers shown to be specifically influenced by environmental exposures—remain an active area of research because they offer the possibility of detecting adverse changes in human physiology before the development of clinical diseases like cancer (Bell et al. 2019; Dhingra et al. 2018). Although research is still emerging as to whether all these markers are truly precursors of disease or simply noncausal correlates of disease processes, these markers maintain promising utility even in the latter circumstance as a means of monitoring disease progression or response to interventions and treatments (Hägg and Jylhävä 2020). Still, we must proactively ensure that the research working to develop and involving these biomarkers—especially in the context of racial disparities in health—is carried out with the understanding that race is primarily a social construct and a poor proxy for genetic and geographic diversity (Keita et al. 2004). The evolution of research on telomeres [nucleoprotein structures at the ends of chromosomes that shorten over time with cell divisions (Lulkiewicz et al. 2020)] provides a notable example of how environmental aging biomarkers can be better leveraged to characterize the cumulative impacts of environmental and social stressors that disproportionately affect communities of color. In particular, studies that previously stopped at describing telomere length differences across races are now being met with evidence that these differences may in fact be related to socioeconomic status (SES; Needham et al. 2019) and neighborhood characteristics (Thierry 2020). In other cases, structural factors like institutional discrimination are now being linked to telomere length (Thomas et al. 2020) and further suggest that similar social elements may be driving factors for previously reported “racial” differences.
The aforementioned literature on telomeres provides added impetus for research efforts that deemphasize race while simultaneously emphasizing racism and other structural factors. However, one important caveat for environmental aging biomarkers is that, at present, there is no single so-called gold standard for biological aging (Bell et al. 2019). Hence, all racial health equity concerns need to be integrated broadly for the numerous environmental aging biomarkers being explored. Different biomarkers are known to reflect different aspects of aging (Nwanaji-Enwerem et al. 2017, 2020) and may also have different relationships with racism, social, and environmental factors.
After the NASEM workshop, the authors acknowledged that the utility of environmental aging biomarkers would be greatly diminished if proportionate attention were not placed on incorporating the many factors that hinder racial health equity. Specifically, developing relevant environmental aging biomarkers (and clinical or environmental interventions based on these biomarkers) without the explicit consideration of their function in, validity for, and benefit to populations disproportionately affected by health disparities will only maintain existing disparities and possibly create new ones for one primary reason: Namely, those in most need of the benefits afforded by a better understanding of environmental aging biomarkers will be the least likely to receive the benefits because the biomarkers may not encompass impacts from their distinct, unique lived experiences and cumulative environmental conditions. In an effort to advance racial health equity, the authors reached a consensus recommendation that a compound exposome approach should be adopted in environmental aging biomarker research.
The exposome represents the cumulative environmental influences throughout the human lifespan that include exposures and factors from the physical, social, and natural environment (Miller and Jones 2014). We recommend the adoption of a compound exposome approach to address methodological challenges of characterizing complex relationships between multiple chemical and nonchemical stressors and biomarkers of aging. This approach involves compounding robust exposome frameworks with efforts aimed at increasing the recruitment and retention of racially/ethnically diverse study populations along with clearly theorizing and interpreting the use of race throughout the analytical, publication, and dissemination processes. An analogy to contrast a traditional vs. a compound approach to exposome and aging biomarker research is shown in Figure 1, which compares a simple light with a compound light microscope. A compound exposome microscope reveals the complexity of environment and aging relationships better than the simple exposure microscope does. Furthermore, we believe that taking a compound exposome approach will improve the identification of clinical and public health intervention targets and best position research findings to help address racial disparities in aging and environmental health. Still, before unpacking our recommendation, we first take time to acknowledge the existing disproportionate burden of adverse aging experiences, poor health outcomes, and environmental injustices endured by various racial groups in the United States.
Figure 1.
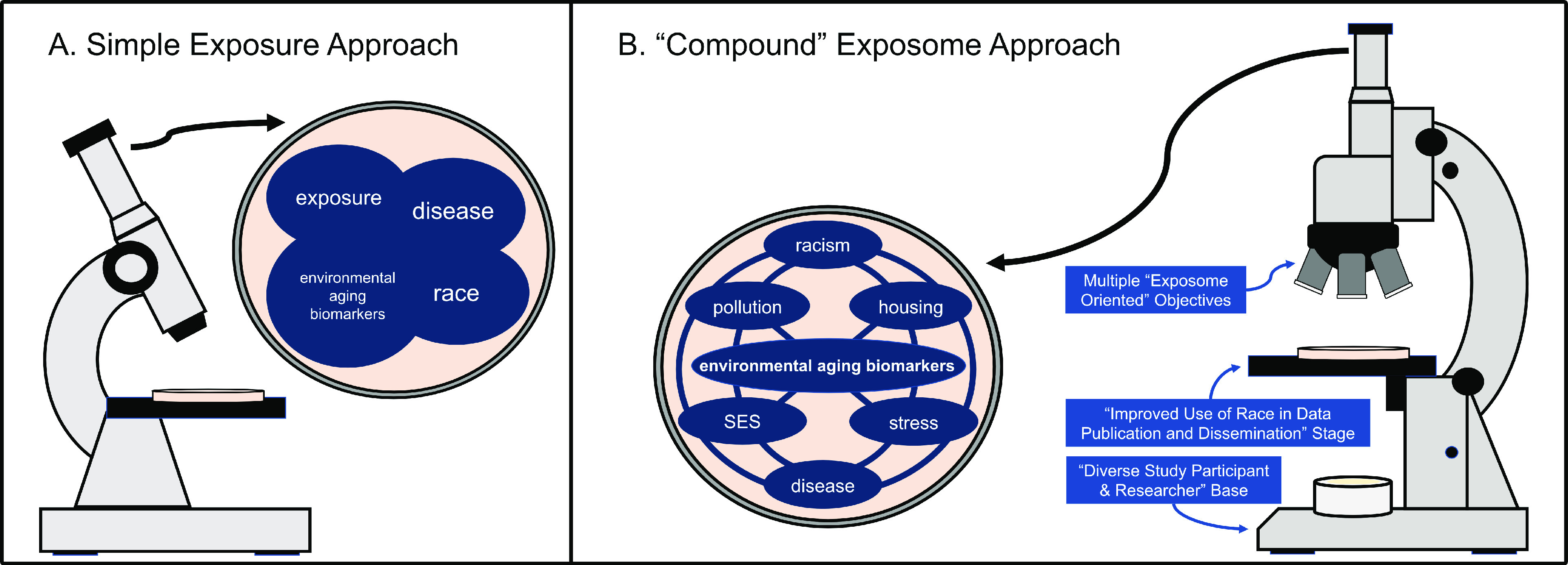
A “compound” exposome approach. A compound exposome approach for environmental aging biomarker studies joins operationalizing the exposome framework in research study design with efforts aimed at increasing the recruitment and retention of racially diverse study populations and researchers. This approach is further compounded with strategies directed at improving the use of race throughout the publication and dissemination process. With a simple (or reductionist) exposure approach (A), researchers may fail to appreciate the true connections among exposures, environmental aging biomarkers, and disease. In some instances, they may even falsely attribute relationships to race. Similar to how a compound light microscope (when compared with a simple light microscope) improves the detail that the operator is able to observe in his or her subject of study, the compound exposome approach (B) maximizes the ability of our research to appreciate the true and complex relationships of environmental aging biomarkers with physical (e.g., pollution) and social (e.g., racism) factors. In the authors’ opinion, this approach better positions the environmental research community to contribute to the elimination of racial health disparities. Note: SES, socioeconomic status.
Disparate Health, Aging, and Environmental Exposures
As defined by the National Institute on Minority Health and Health Disparities (NIMHD), health disparities represent differences in health outcomes that adversely affect disadvantaged populations (Duran and Pérez-Stable 2019). At present, racial and ethnic minorities, socioeconomically disadvantaged communities, sexual and gender minorities, and rural underserved communities are among the NIMHD-designated health disparity populations (Alvidrez et al. 2019). Racial disparities in health, in particular, are created and sustained by past and current interlocking systems of racial oppression that systematically constrain the economic, political, and social engagement of racial and ethnic minorities at institutional, interpersonal, and individual levels (Daftary 2020). The unequal burden of toxic environmental exposures across race and ethnicity is a manifestation of racial oppression and only furthers this process of health decline and increased mortality among racial and ethnic minorities (Tessum et al. 2019). Moreover, experiences of disadvantage accumulate over a lifetime and can be passed down generationally through social, behavioral, and biological mechanisms (Ferraro et al. 2017; Goosby and Heidbrink 2013) such as epigenetics, which is also a basis for some environmental aging biomarkers (Dhingra et al. 2018; Notterman and Mitchell 2015). For this reason, healthy aging in the United States is a privilege not afforded to all. In 2017, the average life expectancy at birth in the United States was 78.6 y. However, that number was one or more years lower for Black and Native American infants (Arias et al. 2019; The Office of Minority Health 2018). By adulthood, the observed difference in the life expectancy for Blacks and Native Americans compared with whites was greater than 3.5 y (Arias et al. 2019). Similarly, notable differences in life expectancy are also observed by geography, a factor that is often tied to the physical distribution of environmental exposures (Colmer et al. 2020; Hill et al. 2019; Thind et al. 2019; Vierboom and Preston 2020) as well as the spatial distribution of racial and ethnic groups and SES due to residential segregation (Beyer et al. 2019; Nardone et al. 2020; Williams and Collins 2001). When one considers healthy aging, the disparities are equally as troubling. Empirical evidence demonstrates that even among age-matched individuals, diseases accumulate disproportionately across race and ethnicities and that distinct differences exist in the total volume and kinds of comorbidities that different races and ethnicities acquire (Lee et al. 2018; Quiñones et al. 2019).
From our perspective, to simply document the presence and magnitude of these disparities in environmental exposures, aging, and health should not be the main goal of the research community. Instead, understanding the etiologies, determinants, and consequences of such disparities and intervening (through policies and practice) to address these disparities should be the ultimate goals. This moment calls for intentional and explicit research-based strategies, from environmental scientists, that mobilize the research community towards producing work grounded in health equity considerations.
Discussion
Contextualizing Race by Operationalizing the Exposome
In contemporary environmental aging biomarker research and in broader epidemiological and biomedical studies, race is often ill-defined and used as a surrogate for an unspecified combination of mainly genetic ancestry components but also of environmental and behavioral factors (Gravlee 2009; Lin and Kelsey 2000). The notions of genetic ancestry and the social construct of race must be intentionally and explicitly disentangled to fully understand the effects of the environment, including the impacts of systemic racism in producing aging and health disparities (Dressler et al. 2005; Non and Gravlee 2015). When considering “race-based” disparities, it becomes even more important to avoid simplified reductionist approaches to identifying exposures, given that disparities exist across all domains of the exposome (e.g., physical-chemical, social, lifestyle) (Juarez et al. 2020; Senier et al. 2017). This point is illustrated by studies of epigenetic aging (i.e., biological clocks), which are widely viewed as predictors of health and lifespan (Horvath 2013; Levine et al. 2018; Lu et al. 2019) and have been associated with a wide range of physical and social environmental exposures (e.g., air pollution, trauma) (Dhingra et al. 2018). Racial differences in these markers have been reported (Horvath et al. 2016; Tajuddin et al. 2019). The work by Horvath et al. (2016) differentiated “groups according to ‘race/ethnicity,’ mindful about existing controversies over rigid racial definitions” and recognized that “the term race/ethnicity thus combines elements of genetic ancestry, population history, and culture.” Tajuddin et al. (2019) performed analyses exploring poverty as a modifier of the association of race with epigenetic aging. Although the authors should be recognized for their efforts, making such concessions about the use of simplified race correlations and singular measures of SES (e.g., poverty solely based on income), in our opinion, is insufficient when one considers the implications that these studies can have on policy and clinical practice. An additional impetus for requiring more from simplified race correlations comes from more recent studies of epigenetic aging that demonstrate race-based DNA methylation array biases (Philibert et al. 2020), and studies that report associations of increased epigenetic aging with exposure to violence (Jovanovic et al. 2017) and early life socioeconomic disadvantage (Austin et al. 2018). To overcome these challenges, researchers need to collect data that sufficiently include information beyond these simplified constructs and include information on experiences of racism, social stress, and marginalization that are implicit and explicit within built environments.
Moving forward, we believe that biomarker studies involving race should be required to employ a more integrated exposome approach that broadens the definition of environment to include social and other contextual factors that shape physiological responses and could confound or modify associations. Along with data on race and chemical environmental exposures, studies should incorporate more robust measures of societal stress exposure, including perceived stress from life and everyday discrimination. The online Stress and Adversity Inventory (STRAIN) represents one example of a quick and comprehensive means of measuring lifetime exposure to more than 50 types of acute and chronic stressors across major domains (e.g., education, relationships, finances) (Slavich and Shields 2018). An important benefit of using STRAIN is the finding that cumulative stress measured via STRAIN has been associated with worse health (Epel et al. 2018). Area-based socioeconomic measures and metrics of indicators that operationalize structural racism through changing neighborhood dynamics, economics, and growth over time should also be included in the broader social exposome construct when considering health disparities (Gravlee 2009; Krieger et al. 2003, 2005). For instance, neighborhood segregation is an example of a well-appreciated form of structural racism (Khazanchi et al. 2020; Kramer and Hogue 2009). Measures like area and neighborhood deprivation indexes are likely to outperform a simple poverty score when it comes to capturing the impact of structural racism because these indexes incorporate data on housing quality, education, and employment in addition to income (Kind and Buckingham 2018).
The power of including such variables in analyses as part of an exposome approach is exemplified by a recent study examining racial disparities in human immunodeficiency virus viral suppression in a population from Omaha, Nebraska (Khazanchi et al. 2020). Initially, the researchers observed significantly lower rates of viral suppression in Black persons in comparison with their White counterparts. However, after adjusting for neighborhood deprivation and other social factors, this difference was no longer significant. Additionally, neighborhood deprivation and lower income were both found to be directly associated with a lower odds of viral suppression (Khazanchi et al. 2020). In a study of air pollution in Milwaukee, Wisconsin, one of the most segregated communities in the United States, air pollution was associated with worse lung function specifically in individuals experiencing neighborhood stress, perceived threats to safety, and crime (Malecki et al. 2018). These findings further highlight the importance of context and lived experiences in shaping the exposome. At present, only a few studies of epigenetic aging have incorporated such variables and have reported significant associations of epigenetic aging with neighborhood deprivation (Lawrence et al. 2020) and other neighborhood factors like nonart graffiti, poor streets, and abandoned cars (Ward-Caviness et al. 2020). Importantly, each of these studies demonstrate that area-based variables as well as social and structural factors should not only be included as covariates to be adjusted for in models or variables to be used for stratified analyses, but they should also be considered in the mechanisms leading to racial health disparities as the primary drivers of harmful biological consequences.
Better Recruitment/Retention of Diverse Study Populations and Researchers
We believe that any attempts to address current health disparities and mitigate the emergence of new ones—even with the application of an exposome approach—are diminished without the inclusion of diverse populations in the implementation of environmental aging biomarker research. Although novel methods for assessing the biological and environmental determinants of aging are rapidly evolving, their usefulness in the growing population of aging adults is stymied by the insufficient representation of communities of color in research (Oh et al. 2015). The impact of the underrepresentation of diverse populations in research is evidenced in genome-wide association studies that are primarily based on cohorts with European ancestry and therefore lack validity and reproducibility across non-European populations (Haga 2010). What use are these studies and advances in genomic and biomarker research if their application and usefulness are restricted to one segment of a larger population? What advances toward health equity can be achieved when disparities exist in the populations (the “for whom”) to which our novel technologies apply? The reality is that if diversity in scientific research remains at its present state, the widely impacting decisions of scientists, medical professionals, policy makers, and many others will remain informed by research extrapolated from a mostly homogenous segment of society, usually males and White persons (Oh et al. 2015).
For the sake of achieving a health understanding that works for all persons, we must actively work toward identifying and addressing impediments to inclusivity. Although the legacy of the Tuskegee Syphilis Study (Brandon et al. 2005)—and the numerous other ethical violations committed against racial and ethnic minorities (especially African Americans)—has rightfully contributed to high levels of community mistrust and limited participation in research studies, the broader enduring legacy of racial, social, and economic injustice is also a significant deterrent to participation (Scharff et al. 2010; Washington 2006). Racism and discrimination, whether implicit or explicit, experienced in academic, medical, and government settings further impede the recruitment and retention of diverse populations into research studies, while also directly harming their health and well-being through increased stress exposure and limitations in the access to and receipt of quality health care (Brandon et al. 2005). Overcoming these structural barriers to the engagement of diverse populations in biomarker, aging, and environmental research requires deliberate solutions that acknowledge past indiscretions and rebuilds and earns the trust of communities being studied.
Community-based participatory research (CBPR) approaches, developed and advanced in the field of public health, have been successful in this regard and offer concrete strategies for repairing the broken trust between research institutions and marginalized communities (O’Fallon and Dearry 2002). The foundation of these approaches includes a) acknowledging past and current traumas committed against racial and ethnic minorities; b) building a shared understanding of the historical context of research in a community; c) being consistently present in the community and actively listening to its members throughout the research process; d) acknowledging and valuing the expertise that community members bring to the table; e) being upfront about expectations and intentions; and f) training and educating community students (K–12, community college, and local four-year college) about science and scientific research (Christopher et al. 2008). Through this process of trust-building and the creation of more equitable, transparent, and mutually beneficial community partnerships, environmental researchers can better recruit and retain diverse populations to improve the development and validation of environmental aging biomarkers.
Furthermore, we believe that one specific domain that will merit very close attention in environmental aging biomarker CBPR approaches is the dissemination of research findings in formats that communities find meaningful. The importance of sharing research findings with communities is becoming better appreciated in all CBPR contexts, but there are unique considerations for biomarker researchers (Yusuf and Elsabbagh 2015). Among the primary considerations is the fact that many of the biomarkers being explored are still preclinical in nature and should not—at this stage—be used for any medical decision-making. Consequently, researchers should take care in how they communicate that these markers may indicate disease risks that are potentially mitigable with the appropriate interventions (Sae‐Lee et al. 2018). Researchers should maintain humility in recognizing that both they and the community are in a perpetual state of learning from each other. Hence, one suggestion is that scientists express that they “can envision a future where these biomarkers can help shape human health practices; however, it is only through partnerships with the community that enough knowledge can be gained to make such a future possible.” Moreover, keeping with the basic tenants of CBPR, the researchers should aim to establish bidirectional communication that fosters an environment for colearning (Minkler et al. 2008). The North Carolina-based Preventing Agricultural Chemical Exposure (PACE) CBPR initiative is among many environmental health CBPR initiatives that have been successful in achieving meaningful bidirectional communication by developing approaches that promote active participation from the community (O’Fallon and Dearry 2002). Their action plan for building community engagement includes having community members on their project steering or advisory committee, formative data collection interviews to acquire social network insights and garner community member perceptions about environmental health concerns, community forums tailored to more active community residents, and public presentations tailored to less-active residents. We suggest that these strategies and others should at the least be considered in environmental aging biomarker CBPR initiatives.
A complementary line of thinking about the recruitment and retention of diverse study populations can be extended to the recruitment and retention of diverse researchers. There remains a significant need to identify new talent and to promote existing scholars from diverse racial and ethnic backgrounds in all academic, industry, nonprofit, and government research enterprises (Sierra-Mercado and Lázaro-Muñoz 2018; Trejo 2017). As part of these efforts, institutions must be willing to restructure their recruitment, hiring, promotion, and tenure practices in ways that systematically value community engaged research and scientific initiatives aimed at promoting racial health equity (Campbell et al. 2020; Lewis 2020; Mahoney et al. 2008). This commitment to improved racial diversity and representation is particularly critical for the advancement of environmental aging research—and of environmental health as a whole—given the disproportionate burden of adverse environmental exposures borne by minority communities and the potential for communities of color to prefer working with researchers who reflect their community and possess needed cultural humility (Frierson et al. 2019; Fryer et al. 2016).
These systematic changes can be further extended to the grant review practices and guidelines of funding institutions. Research has shown that Black scientists are more likely to perform research on community-focused topics and that topic choice accounts for more than 20% of the funding disparity between Black applicants for National Institutes of Health (NIH) grants and their White peer applicants (Hoppe et al. 2019). We believe that it is only through concerted efforts that recognize the importance of such research—for instance, revising grant review criteria and prioritizing the funding of such topics—that these disparities can be addressed. A recent work has highlighted additional steps that federal funding bodies like the NIH can take to help mitigate these racial funding disparities (Taffe and Gilpin 2021). Their recommendations include greater data transparency (including the publishing of standing study section racial/ethnic data annually), making discretionary funding decisions with attention to racial equity, and top-down quota-based affirmative action procedures similar to those used to address disparities in early stage investigator grant funding (Taffe and Gilpin 2021).
Improved Use of Race throughout the Publication Process
As part of our recommendation for a compound exposome approach in environmental aging biomarker research, we call for new standards for publishing research on racial health inequities (e.g., defining race within a sociopolitical framework and as a construct rather than a proxy for inherent biological difference). This change would emphasize that aging biomarkers are best used to assess the biological consequences of factors like racism as the primary determinants of racial and ethnic health disparities (Boyd et al. 2020). To make this point more compelling, let us consider the dangerous impact on population health that a flawed marker can have when it is not met with the appropriate publication checkpoints and is allowed to shape race-specific clinical care practices (Vyas et al. 2020). Research supporting a “race correction” or adjustment in algorithms estimating glomerular filtration rate (eGFR) (Levey et al. 1999) (the rate at which the kidneys remove waste and fluids from the body) failed to acknowledge and account for the contribution of social processes in racial and ethnic differences in health and has been scrutinized for a lack of supporting evidence for the correction (Norris et al. 2020; Vyas et al. 2020; Waddell 2020). The correction results in a higher eGFR—estimated renal function—among African Americans. Consequently, African Americans may be less likely to be diagnosed with and treated for kidney disease, which may contribute to race-based disparities that we observe in kidney disease and related outcomes like dialysis utilization (Ahmed et al. 2021). Again, the fatal flaw in this body of research and other research touting race-specific physiological processes is the belief in race as biology and the seemingly intentional disregard of the social and political construction of race. One could imagine a similar situation occurring where aging biomarkers inappropriately attribute differential aging to biology or genetic ancestry rather than broader societal or structural factors.
In recent months, we have observed a backlash on Twitter and other social media platforms calling for more accountability from journals and editors after the publication of inherently flawed studies that inappropriately make assertions about race. In the event that grant reviewers and funding agencies do not call attention to these flawed methodologies (including interpretations) and in the event that researchers fail to recognize inappropriate study designs and produce harmfully misguided manuscripts, we believe that journals and editors must step forward as additional checkpoints to safeguard the integrity of published science. As such, we recommend that journals publishing environmental aging biomarker studies—and biomedical research broadly—establish or revise publication guidelines to ensure that findings pertaining to race are contextualized within sociopolitical frameworks such as Critical Race Theory (Ford and Airhihenbuwa 2010), the Exposure-Disease-Stress Model for environmental health disparities (Gee and Payne-Sturges 2004), and, more broadly, the Fundamental Causes Model for health disparities (Phelan et al. 2004; Williams and Collins 2001). To facilitate this process, journal editors should recruit reviewers with expertise in the social and pathophysiological mechanisms of racism when evaluating such manuscripts. Reviewers should be critical of and request rigorous explanations for research defining race in a biological context or positing a genetic basis for racial differences in health outcomes. It is the authors’ belief that this approach will help mitigate the confounding of racism—rather than race—with other societal factors when elucidating the observed relationships between race and environmental aging biomarkers in biomarker studies. This distinction is critical for promoting greater biomarker utility and societal change, given the implications that racial health inequities research has for broader public policy and clinical practice.
Conclusion
In summary, it is our belief that the exposome provides an avenue forward and outlines an approach in which racism, racial disparities, and contributing factors can be a valid component of environmental aging biomarker development and research. If they can be properly identified, natural, built, and social environmental determinants stand out as critical public health intervention targets for mitigating and preventing health disparities (Nelson et al. 2020; Satcher and Higginbotham 2008). Furthermore, we believe that a) establishing diverse study populations; and b) ensuring that the publication process incorporates more profound considerations of race will reinforce (compound) exposome study designs and help facilitate the identification of environmental aging biomarkers that explicate racial disparities in longevity, health, and disease. In the end, the overall compound exposome approach is aimed at synchronously pushing the environmental research community toward the creation of a more equitable health future through the production of sound research that addresses racial disparities of the past and safeguards against any unfortunate racial disparities in the future.
Acknowledgments
This work was funded, in part, by the Intramural Program at the NIH, National Institute of Environmental Health Sciences [NIEHS; Z1AES103325-01 (CLJ)]. J.C.N. and A.C. were partially supported by NIH grants R03AG067064 and R01ES031259.
J.C.N. and U.A.M. conceived of the commentary idea, provided the initial draft, and took the lead on subsequent edits and revisions. All authors contributed to, revised, and approved the manuscript. C.L.J. contributed to the recommendation of an exposome approach along with more rigorous publishing standards for research on racial/ethnic health disparities and provided general editorial input. A.M.G. contributed to editorial content emphasizing the importance of social science approaches and linking the social exposome to health disparities, biomarkers of exposure and adverse health effects, the aging phenotype, and conditions in overburdened communities and provided general editorial input. M.A.O. contributed to the editorial content focused on aging processes and adverse effects of exposure to environmental chemicals, conceptualizing lifelong adverse outcomes in terms of the exposome, and the importance of the entire suite of factors affecting vulnerable communities and provided general editorial input. The authors would also like to acknowledge the NASEM staff, particularly A. Hodgson, E. Alme, K. Sawyer, and J. DeMouy for helping to coordinate the “Integrating the Science of Aging and Environmental Health” workshop and subsequent meetings for this paper. The authors wish to also thank J. Harry (NIEHS) for her valuable contributions to the editing of this manuscript.
This work has been subjected to review by the Office of Research and Development, U.S. Environmental Protection Agency and approved for publication. Approval does not signify that the contents reflect the views of the agency, nor does mention of trade names or commercial products constitute endorsement or recommendation for use.
References
- Agyeman J, Schlosberg D, Craven L, Matthews C. 2016. Trends and directions in environmental justice: from inequity to everyday life, community, and just sustainabilities. Annu Rev Environ Resour 41(1):321–340, 10.1146/annurev-environ-110615-090052. [DOI] [Google Scholar]
- Ahmed S, Nutt CT, Eneanya ND, Reese PP, Sivashanker K, Morse M, et al. 2021. Examining the potential impact of race multiplier utilization in estimated glomerular filtration rate calculation on African-American care outcomes. J Gen Intern Med 36(2):464–471, PMID: 33063202, 10.1007/s11606-020-06280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. 2019. The National Institute on Minority Health and Health Disparities research framework. Am J Public Health 109(S1):S16–S20, PMID: 30699025, 10.2105/AJPH.2018.304883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias E, Xu J, Division of Vital Statistics. 2019. United States Life Tables, 2017. National Vital Statistics Reports, vol. 68, no. 7. Hyattsville, MD: National Center for Health Statistics, 1–66. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_07-508.pdf [accessed 10 December 2020]. [PubMed] [Google Scholar]
- Austin MK, Chen E, Ross KM, McEwen LM, MacIsaac JL, Kobor MS, et al. 2018. Early-life socioeconomic disadvantage, not current, predicts accelerated epigenetic aging of monocytes. Psychoneuroendocrinology 97:131–134, PMID: 30016711, 10.1016/j.psyneuen.2018.07.007. [DOI] [PubMed] [Google Scholar]
- Bell CG, Lowe R, Adams PD, Baccarelli AA, Beck S, Bell JT, et al. 2019. DNA methylation aging clocks: challenges and recommendations. Genome Biol 20(1):249, PMID: 31767039, 10.1186/s13059-019-1824-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyer KMM, Laud PW, Zhou Y, Nattinger AB. 2019. Housing discrimination and racial cancer disparities among the 100 largest US metropolitan areas. Cancer 125(21):3818–3827, PMID: 31287559, 10.1002/cncr.32358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd RW, Lindo EG, Weeks LD, McLemore MR. 2020. On racism: a new standard for publishing on racial health inequities. Health Affairs Blog 10, 10.1377/hblog20200630.939347. [DOI] [Google Scholar]
- Brandon DT, Isaac LA, LaVeist TA. 2005. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc 97(7):951–956, PMID: 16080664. [PMC free article] [PubMed] [Google Scholar]
- Campbell KM, Hudson BD, Tumin D. 2020. Releasing the net to promote minority faculty success in academic medicine. J Racial Ethn Health Disparities 7(2):202–206, PMID: 31953638, 10.1007/s40615-020-00703-z. [DOI] [PubMed] [Google Scholar]
- Christopher S, Watts V, McCormick AKHG, Young S. 2008. Building and maintaining trust in a community-based participatory research partnership. Am J Public Health 98(8):1398–1406, PMID: 18556605, 10.2105/AJPH.2007.125757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, et al. 2020. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation 142(24):e454–e468, PMID: 33170755, 10.1161/CIR.0000000000000936. [DOI] [PubMed] [Google Scholar]
- Colmer J, Hardman I, Shimshack J, Voorheis J. 2020. Disparities in PM2.5 air pollution in the United States. Science 369(6503):575–578, PMID: 32732425, 10.1126/science.aaz9353. [DOI] [PubMed] [Google Scholar]
- Daftary A-MH. 2020. Critical race theory: an effective framework for social work research. J Ethn Cult Divers Soc Work 29(6):439–416, 10.1080/15313204.2018.1534223. [DOI] [Google Scholar]
- Dhingra R, Nwanaji-Enwerem JC, Samet M, Ward-Caviness CK. 2018. DNA methylation age-environmental influences, health impacts, and its role in environmental epidemiology. Curr Environ Health Rep 5(3):317–327, PMID: 30047075, 10.1007/s40572-018-0203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler WW, Oths KS, Gravlee CC. 2005. Race and ethnicity in public health research: models to explain health disparities. Annu Rev Anthropol 34(1):231–252, 10.1146/annurev.anthro.34.081804.120505. [DOI] [Google Scholar]
- Duran DG, Pérez-Stable EJ. 2019. Novel approaches to advance minority health and health disparities research. Am J Public Health 109(S1):S8–S10, PMID: 30699017, 10.2105/AJPH.2018.304931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel ES, Crosswell AD, Mayer SE, Prather AA, Slavich GM, Puterman E, et al. 2018. More than a feeling: a unified view of stress measurement for population science. Front Neuroendocrinol 49:146–169, PMID: 29551356, 10.1016/j.yfrne.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, Kemp BR, Williams MM. 2017. Diverse aging and health inequality by race and ethnicity. Innov Aging 1(1):igx002, PMID: 29795805, 10.1093/geroni/igx002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford CL, Airhihenbuwa CO. 2010. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health 100(suppl 1):S30–S35, PMID: 20147679, 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frierson GM, Pinto BM, Denman DC, Leon PA, Jaffe AD. 2019. Bridging the gap: racial concordance as a strategy to increase African American participation in breast cancer research. J Health Psychol 24(11):1548–1561, PMID: 29172809, 10.1177/1359105317740736. [DOI] [PubMed] [Google Scholar]
- Fryer CS, Passmore SR, Maietta RC, Petruzzelli J, Casper E, Brown NA, et al. 2016. The symbolic value and limitations of racial concordance in minority research engagement. Qual Health Res 26(6):830–841, PMID: 25769299, 10.1177/1049732315575708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Payne-Sturges DC. 2004. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect 112(17):1645–1653, PMID: 15579407, 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby BJ, Heidbrink C. 2013. Transgenerational consequences of racial discrimination for African American health. Sociol Compass 7(8):630–643, PMID: 24855488, 10.1111/soc4.12054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravlee CC. 2009. How race becomes biology: embodiment of social inequality. Am J Phys Anthropol 139(1):47–57, PMID: 19226645, 10.1002/ajpa.20983. [DOI] [PubMed] [Google Scholar]
- Haga SB. 2010. Impact of limited population diversity of genome-wide association studies. Genet Med 12(2):81–84, PMID: 20057316, 10.1097/GIM.0b013e3181ca2bbf. [DOI] [PubMed] [Google Scholar]
- Hägg S, Jylhävä J. 2020. Should we invest in biological age predictors to treat colorectal cancer in older adults? Eur J Surg Oncol 46(3):316–320, PMID: 31761509, 10.1016/j.ejso.2019.11.003. [DOI] [PubMed] [Google Scholar]
- Hill TD, Jorgenson AK, Ore P, Balistreri KS, Clark B. 2019. Air quality and life expectancy in the United States: an analysis of the moderating effect of income inequality. SSM Popul Health 7:100346, PMID: 30627626, 10.1016/j.ssmph.2018.100346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppe TA, Litovitz A, Willis KA, Meseroll RA, Perkins MJ, Hutchins BI, et al. 2019. Topic choice contributes to the lower rate of NIH awards to African-American/black scientists. Sci Adv 5(10):eaaw7238, PMID: 31633016, 10.1126/sciadv.aaw7238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath S. 2013. DNA methylation age of human tissues and cell types. Genome Biol 14(10):3156, PMID: 24138928, 10.1186/gb-2013-14-10-r115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath S, Gurven M, Levine ME, Trumble BC, Kaplan H, Allayee H, et al. 2016. An epigenetic clock analysis of race/ethnicity, sex, and coronary heart disease. Genome Biol 17(1):171, PMID: 27511193, 10.1186/s13059-016-1030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovanovic T, Vance LA, Cross D, Knight AK, Kilaru V, Michopoulos V, et al. 2017. Exposure to violence accelerates epigenetic aging in children. Sci Rep 7(1):8962, PMID: 28827677, 10.1038/s41598-017-09235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juarez PD, Hood DB, Song M-A, Ramesh A. 2020. Use of an exposome approach to understand the effects of exposures from the natural, built, and social environments on cardio-vascular disease onset, progression, and outcomes. Front Public Health 8:379, PMID: 32903514, 10.3389/fpubh.2020.00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keita SOY, Kittles RA, Royal CDM, Bonney GE, Furbert-Harris P, Dunston GM, et al. 2004. Conceptualizing human variation. Nat Genet 36(suppl 11):S17–S20, PMID: 15507998, 10.1038/ng1455. [DOI] [PubMed] [Google Scholar]
- Khazanchi R, Sayles H, Bares SH, Swindells S, Marcelin JR. 2020. Neighborhood deprivation and racial/ethnic disparities in HIV viral suppression: a single-center cross-sectional study in the U.S. Midwest. Clin Infect Dis, PMID: 32845985, 10.1093/cid/ciaa1254. [DOI] [PubMed] [Google Scholar]
- Kind AJH, Buckingham WR. 2018. Making neighborhood-disadvantage metrics accessible — the neighborhood atlas. N Engl J Med 378(26):2456–2458, PMID: 29949490, 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, Hogue CR. 2009. Is segregation bad for your health? Epidemiol Rev 31:178–194, PMID: 19465747, 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. 2003. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures–the Public Health Disparities Geocoding Project. Am J Public Health 93(10):1655–1671, PMID: 14534218, 10.2105/AJPH.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. 2005. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health 95(2):312–323, PMID: 15671470, 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence KG, Kresovich JK, O’Brien KM, Hoang TT, Xu Z, Taylor JA, et al. 2020. Association of neighborhood deprivation with epigenetic aging using 4 clock metrics. JAMA Netw Open 3(11):e2024329, PMID: 33146735, 10.1001/jamanetworkopen.2020.24329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Shin SH, Gu S, Zhao D, Kang D, Joi YR, et al. 2018. Racial differences in comorbidity profile among patients with chronic obstructive pulmonary disease. BMC Med 16(1):178, PMID: 30285854, 10.1186/s12916-018-1159-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. 1999. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 130(6):461–470, PMID: 10075613, 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- Levine ME, Lu AT, Quach A, Chen BH, Assimes TL, Bandinelli S, et al. 2018. An epigenetic biomarker of aging for lifespan and healthspan. Aging (Albany NY) 10(4):573–591, PMID: 29676998, 10.18632/aging.101414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis NA Jr. 2020. What I’ve learned about being a Black scientist. Science. https://www.sciencemag.org/careers/2020/06/what-ive-learned-about-being-black-scientist [accessed 9 December 2020].
- Lin SS, Kelsey JL. 2000. Use of race and ethnicity in epidemiologic research: concepts, methodological issues, and suggestions for research. Epidemiol Rev 22(2):187–202, PMID: 11218371, 10.1093/oxfordjournals.epirev.a018032. [DOI] [PubMed] [Google Scholar]
- Lu AT, Quach A, Wilson JG, Reiner AP, Aviv A, Raj K, et al. 2019. DNA methylation GrimAge strongly predicts lifespan and healthspan. Aging (Albany NY) 11(2):303–327, PMID: 30669119, 10.18632/aging.101684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lulkiewicz M, Bajsert J, Kopczynski P, Barczak W, Rubis B. 2020. Telomere length: how the length makes a difference. Mol Biol Rep 47(9):7181–7188, PMID: 32876842, 10.1007/s11033-020-05551-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney MR, Wilson E, Odom KL, Flowers L, Adler SR. 2008. Minority faculty voices on diversity in academic medicine: perspectives from one school. Acad Med 83(8):781–786, PMID: 18667896, 10.1097/ACM.0b013e31817ec002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malecki KMC, Schultz AA, Bergmans RS. 2018. Neighborhood perceptions and cumulative impacts of low level chronic exposure to fine particular matter (PM2.5) on cardiopulmonary health. Int J Environ Res Public Health 15(1):84, PMID: 29316641, 10.3390/ijerph15010084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GW, Jones DP. 2014. The nature of nurture: refining the definition of the exposome. Toxicol Sci 137(1):1–2, PMID: 24213143, 10.1093/toxsci/kft251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Vásquez VB, Tajik M, Petersen D. 2008. Promoting environmental justice through community-based participatory research: the role of community and partnership capacity. Health Educ Behav 35(1):119–137, PMID: 16861594, 10.1177/1090198106287692. [DOI] [PubMed] [Google Scholar]
- Nardone AL, Casey JA, Rudolph KE, Karasek D, Mujahid M, Morello-Frosch R. 2020. Associations between historical redlining and birth outcomes from 2006 through 2015 in California. PLoS One 15(8):e0237241, PMID: 32764800, 10.1371/journal.pone.0237241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NASEM (National Academies of Sciences, Engineering, and Medicine). 2020. Integrating the Science of Aging and Environmental Health Research: Proceedings of a Workshop—in Brief. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Needham BL, Salerno S, Roberts E, Boss J, Allgood KL, Mukherjee B. 2019. Do black/white differences in telomere length depend on socioeconomic status? Biodemography Soc Biol 65(4):287–312, PMID: 33243026, 10.1080/19485565.2020.1765734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson HD, Cantor A, Wagner J, Jungbauer R, Quiñones A, Stillman L, et al. 2020. Achieving health equity in preventive services: a systematic review for a national institutes of health pathways to prevention workshop. Ann Intern Med 172(4):258–271, PMID: 31931527, 10.7326/M19-3199. [DOI] [PubMed] [Google Scholar]
- Non AL, Gravlee CC. 2015. Biology and culture beyond the genome: race, racism, and health. Am Anthropol 117(4):737–738, 10.1111/aman.12365. [DOI] [Google Scholar]
- Norris KC, Eneanya ND, Boulware LE. 2020. Removal of race from estimates of kidney function: first, do no harm. JAMA 325(2):135–137, PMID: 33263722, 10.1001/jama.2020.23373. [DOI] [PubMed] [Google Scholar]
- Notterman DA, Mitchell C. 2015. Epigenetics and understanding the impact of social determinants of health. Pediatr Clin North Am 62(5):1227–1240, PMID: 26318949, 10.1016/j.pcl.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwanaji-Enwerem JC, Colicino E, Specht AJ, Gao X, Wang C, Vokonas P, et al. 2020. Individual species and cumulative mixture relationships of 24-hour urine metal concentrations with DNA methylation age variables in older men. Environ Res 186:109573, PMID: 32361261, 10.1016/j.envres.2020.109573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwanaji-Enwerem JC, Dai L, Colicino E, Oulhote Y, Di Q, Kloog I, et al. 2017. Associations between long-term exposure to PM2.5 component species and blood DNA methylation age in the elderly: the VA Normative Aging Study. Environ Int 102:57–65, PMID: 28284819, 10.1016/j.envint.2016.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Fallon LR, Dearry A. 2002. Community-based participatory research as a tool to advance environmental health sciences. Environ Health Perspect 110(suppl 2):155–159, PMID: 11929724, 10.1289/ehp.02110s2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh SS, Galanter J, Thakur N, Pino-Yanes M, Barcelo NE, White MJ, et al. 2015. Diversity in clinical and biomedical research: a promise yet to be fulfilled. PLoS Med 12(12):e1001918, PMID: 26671224, 10.1371/journal.pmed.1001918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. 2004. “Fundamental causes” of social inequalities in mortality: a test of the theory. J Health Soc Behav 45(3):265–285, PMID: 15595507, 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- Philibert R, Beach SRH, Lei M-K, Gibbons FX, Gerrard M, Simons RL, et al. 2020. Array-based epigenetic aging indices may be racially biased. Genes (Basel) 11(6):685, PMID: 32580526, 10.3390/genes11060685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quiñones AR, Botoseneanu A, Markwardt S, Nagel CL, Newsom JT, Dorr DA, et al. 2019. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS One 14(6):e0218462, PMID: 31206556, 10.1371/journal.pone.0218462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sae‐Lee C, Corsi S, Barrow TM, Kuhnle GGC, Bollati V, Mathers JC, et al. 2018. Dietary intervention modifies DNA methylation age assessed by the epigenetic clock. Mol Nutr Food Res 62(23):1800092, PMID: 30350398, 10.1002/mnfr.201800092. [DOI] [PubMed] [Google Scholar]
- Satcher D, Higginbotham EJ. 2008. The public health approach to eliminating disparities in health. Am J Public Health 98(3):400–403, PMID: 18235057, 10.2105/AJPH.2007.123919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. 2010. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved 21(3):879–897, PMID: 20693733, 10.1353/hpu.0.0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senier L, Brown P, Shostak S, Hanna B. 2017. The socio-exposome: advancing exposure science and environmental justice in a post-genomic era. Environ Sociol 3(2):107–121, PMID: 28944245, 10.1080/23251042.2016.1220848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sierra-Mercado D, Lázaro-Muñoz G. 2018. Enhance diversity among researchers to promote participant trust in precision medicine research. Am J Bioeth 18(4):44–46, PMID: 29621450, 10.1080/15265161.2018.1431323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, Shields GS. 2018. Assessing lifetime stress exposure using the stress and adversity inventory for adults (adult STRAIN): an overview and initial validation. Psychosom Med 80(1):17–27, PMID: 29016550, 10.1097/PSY.0000000000000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sze S, Pan D, Nevill CR, Gray LJ, Martin CA, Nazareth J, et al. 2020. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine 29:100630, PMID: 33200120, 10.1016/j.eclinm.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taffe MA, Gilpin NW. 2021. Racial inequity in grant funding from the US National Institutes of Health. eLife 10:e65697, PMID: 33459595, 10.7554/eLife.65697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tajuddin SM, Hernandez DG, Chen BH, Noren Hooten N, Mode NA, Nalls MA, et al. 2019. Novel age-associated DNA methylation changes and epigenetic age acceleration in middle-aged African Americans and whites. Clin Epigenet 11(1):119, PMID: 31426852, 10.1186/s13148-019-0722-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessum CW, Apte JS, Goodkind AL, Muller NZ, Mullins KA, Paolella DA, et al. 2019. Inequity in consumption of goods and services adds to racial–ethnic disparities in air pollution exposure. Proc Natl Acad Sci USA 116(13):6001–6006, PMID: 30858319, 10.1073/pnas.1818859116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Office of Minority Health. 2018. American Indian/Alaska Native. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=62 [accessed 21 June 2020].
- Thierry AD. 2020. Association between telomere length and neighborhood characteristics by race and region in US midlife and older adults. Health Place 62:102272, PMID: 32479352, 10.1016/j.healthplace.2019.102272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thind MPS, Tessum CW, Azevedo IL, Marshall JD. 2019. Fine particulate air pollution from electricity generation in the US: health impacts by race, income, and geography. Environ Sci Technol 53(23):14010–14019, PMID: 31746196, 10.1021/acs.est.9b02527. [DOI] [PubMed] [Google Scholar]
- Thomas MD, Sohail S, Mendez RM, Márquez-Magaña L, Allen AM. 2020. Racial discrimination and telomere length in midlife African American women: interactions of educational attainment and employment status. Ann Behav Med, PMID: 33289498, 10.1093/abm/kaaa104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trejo J. 2017. A reflection on faculty diversity in the 21st century. Mol Biol Cell 28(22):2911–2914, PMID: 29084907, 10.1091/mbc.e17-08-0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierboom YC, Preston SH. 2020. Life beyond 65: changing spatial patterns of survival at older ages in the United States, 2000–2016. J Gerontol B Psychol Sci Soc Sci 75(5):1093–1103, PMID: 31995196, 10.1093/geronb/gbz160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas DA, Eisenstein LG, Jones DS. 2020. Hidden in plain sight - reconsidering the use of race correction in clinical algorithms. N Engl J Med 383(9):874–882, PMID: 32853499, 10.1056/NEJMms2004740. [DOI] [PubMed] [Google Scholar]
- Waddell K. 2020. Medical algorithms have a race problem. https://www.consumerreports.org/medical-tests/medical-algorithms-have-a-race-problem/ [accessed 23 September 2020].
- Ward-Caviness CK, Pu S, Martin CL, Galea S, Uddin M, Wildman DE, et al. 2020. Epigenetic predictors of all-cause mortality are associated with objective measures of neighborhood disadvantage in an urban population. Clin Epigenetics 12(1):44, PMID: 32160902, 10.1186/s13148-020-00830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington HA. 2006. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. New York, NY: Doubleday. [Google Scholar]
- Williams DR, Collins C. 2001. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 116(5):404–416, PMID: 12042604, 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf A, Elsabbagh M. 2015. At the cross-roads of participatory research and biomarker discovery in autism: the need for empirical data. BMC Med Ethics 16(1):, PMID: 26669759, 10.1186/s12910-015-0082-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


