Abstract
The Dunning-Kruger premise assumes that unqualified people are unaware of their limited skills. We tested this hypothesis in the context of the coronavirus disease 2019 (COVID-19) pandemic. In this cross-sectional study, 2487 participants had to self-estimate their knowledge about COVID-19 in a questionnaire on the topic. Poor performers were more likely to use mass media and social networks as sources of information and had lower levels of education. The mean self-assessment (SD) was 6.88 (2.06) and was not linked to actual level of knowledge. This observation should prompt regulatory agencies and media to apply rules that limit dissemination of “infodemics” during global health crises.
Keywords: agnotology, cognitive bias, COVID-19, cross-sectional survey, perception
A tremendous feature of the coronavirus disease 2019 (COVID-19) pandemic is the unprecedented production of medical information in a short period of time. Given the urgency to contain the outbreak and treat patients, messages delivered by the scientific community were immediately broadcasted worldwide through general and social media. Among the outstanding volume of literature, some studies with unconfirmed findings have been broadly disseminated. As the majority of the audience was unaware of the subtleties of scientific methodology, there has been unbalanced appraisal of articles’ content [1]. A theory suggested in 1999 by Dunning and Kruger postulates that less qualified persons overestimate their abilities and knowledge about a given topic [2]. We aimed to assess the reproduction of the Dunning-Kruger premise in the context of novel medical information in a networked world.
METHODS
We conducted a cross-sectional survey at the COVID-19 collection unit of the Princess Grace Hospital Center, Monaco. This unit was dedicated to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibody detection as part of a seroprevalence survey in people working during the lockdown. We invited individuals visiting the unit between May 4 and June 13, 2020, to complete a self-administered questionnaire (Supplementary Data) recording demographics, professional and education characteristics, COVID-19 exposure, sources of information about COVID-19 (participants had to quote 3 main sources), and self-perception of expertise regarding COVID-19. Participants were asked 9 questions about their scientific knowledge of COVID-19 and questioned on their degree of certainty about the answer they provided (doubtful, rather doubtful, rather certain, and certain). The questionnaire dealt with popular topics debated during the outbreak, with 1 exception (question 4: coronaviruses and seasonal epidemic rhinopharyngitis).
Statistical Analysis
Participants were distributed into quartiles (lower quartile, Q1; intermediate low, Q2; intermediate high, Q3; upper, Q4) depending on (i) the number of correct answers on the scientific questionnaire, (ii) the number of definite answers to the scientific questionnaire, and (iii) self-perception of COVID-19 knowledge (scale range from 0 to 10). Statistical comparisons used Pearson’s chi-square test for 2 categorical variables, the Mann-Whitney or Kruskal-Wallis rank sum test for 1 categorical and 1 rank variable, and the Spearman rank correlation coefficient for 2 rank variables. All tests were 2-sided, and P values <.05 were considered statistically significant. All statistical analyses were performed using SPSS statistical software, version 21.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
In total, 2487 individuals were asked to complete the questionnaire (characteristics detailed in the Supplementary Data). The mean age was 43 years, and 60% were female. A majority (57%) achieved a university degree. Health care professionals represented 54% of the sample. The main sources of information were mass media (77%), social networks (30%), and discussion with health care professionals (43%).
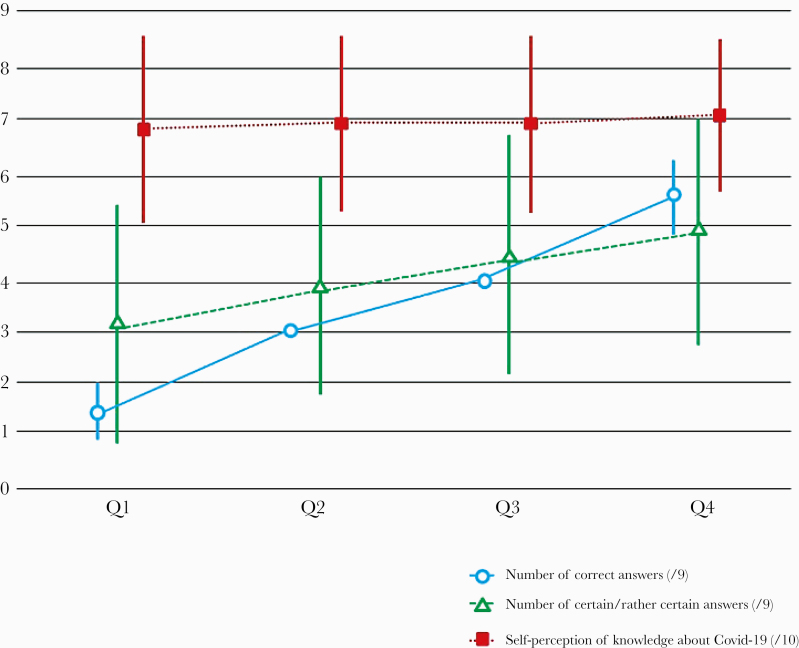
We excluded 84 participants who did not answer any question. The median number of correct answers was 3/9; 343 participants (15%) answered 1 question or no questions correctly. Distribution of the answers is presented in Table 1. Responders were allocated as follows (Figure 1): 817 Q1 (35%; 0–2 correct answers); 562 Q2 (23%; 3 correct answers); 485 Q3 (20%; 4 correct answers); 539 Q4 (22%; 5–9 correct answers). Nearly 80% assumed that their level of knowledge about COVID-19 was above average, and two-thirds perceived their knowledge to be above average because of their occupation. The median self-estimation of knowledge was 7/10 (Supplementary Data); a weak although significant association was observed between participants’ self-assessment and the number of correct answers (r = 0.06; P = .002). Self-estimation of knowledge by quartile is shown in Figure 1. Contrary to what we expected from the Dunning-Kruger effect hypothesis, better responders expressed a higher level of certainty with regard to their answers (r = 0.32; P < .0001). Participants without a university degree had lower rates of correct answers (P < .001), and those with a PhD or equivalent (eg, Medical Doctors) were more able to answer correctly (P < .001). However, being a health care professional other than a physician and working in direct contact with COVID-19 patients did not alter the rate of correct answers (P = .28). Mass media and social networks were more frequently quoted as sources of information in lower quartiles, with, respectively, 81% for Q1 vs 74% for Q4 (P < .001) and 36% for Q1 vs 25% for Q4 (P < .001). Conversely, discussion with health care professionals about the scientific literature recurred in upper quartiles with, respectively, 39% for Q1 vs 49% for Q4 (P < .001) and 7% for Q1 vs 23% for Q4 (P < .001).
Table 1.
Distribution of Answers on the Scientific Questionnaire
| Which factor is not associated with an increased risk of the severe form of COVID-19? | |
| Obesity | 94 (4) |
| Blood group | 1458 (63) |
| Epilepsy (correct answer) | 706 (31) |
| Diabetes | 54 (2) |
| No answer | 175 |
| With symptoms, a single person might contaminate: | |
| 1 person | 35 (1) |
| 2 to 3 people (correct answer) | 1463 (62) |
| 5 to 8 people | 644 (27) |
| More than 10 people | 210 (9) |
| No answer | 135 |
| Heard immunity is reached when what percentage of the population has been sick: | |
| 20% | 105 (5) |
| 40% | 257 (11) |
| 60% (correct answer) | 1517 (65) |
| 80% | 438 (19) |
| No answer | 170 |
| Contribution of coronaviruses in seasonal rhinopharyngitis epidemic: | |
| 0.1% | 236 (11) |
| 1% | 657 (30) |
| 5% | 911 (41) |
| 15% (correct answer) | 402 (18) |
| No answer | 281 |
| What percentage of genome is shared between COVID-19 and HIV? | |
| Less than 0.1% (correct answer) | 563 (27) |
| Between 0.1% and 1% | 868 (41) |
| Between 1% and 10% | 579 (27) |
| Between 10% and 20% | 101 (5) |
| No answer | 376 |
| On average, COVID-19 can survive on cardboard: | |
| Around 30 min | 185 (8) |
| Around 3 h | 1178 (51) |
| Around 12 h | 392 (17) |
| Around 24 h (correct answer) | 537 (23) |
| No answer | 195 |
| (Hydroxy-)chloroquine prescription for COVID-19 infection can be written: | |
| By all general practioners | 579 (25) |
| By all pneumologists | 233 (10) |
| By all infectious disease physicians | 416 (18) |
| Only for patients included in clinical trials (correct answer) | 1053 (46) |
| No answer | 206 |
| In France, the actual number of people infected by COVID-19 is: | |
| Fewer than 50 000 people | 292 (13) |
| Between 50 000 and 100 000 people | 646 (28) |
| Between 100 000 and 150 000 people (correct answer) | 901 (39) |
| More than 200 000 people | 455 (20) |
| No answer | 193 |
| On average, for every 100 people who test positive for COVID-19, the number of hospitalizations is: | |
| Fewer than 5 people (correct answer) | 701 (31) |
| Between 5 and 10 people | 934 (41) |
| Between 10 and 20 people | 479 (21) |
| More than 20 people | 171 (7) |
| No answer | 202 |
Data are presented as No. (%).
Abbreviation: COVID-19, coronavirus disease 2019.
Figure 1.
Perceived knowledge about coronavirus disease 2019, actual score on the questionnaire, and level of certainty about the answers (mean, SD). Q1, lower quartile (0–2 correct answers); Q2, intermediate low quartile (3 correct answers); Q3, intermediate high quartile (4 correct answers); Q4, upper quartile (5–9 correct answers).
DISCUSSION
Our findings inform the debate about public perception of one’s knowledge regarding COVID-19. Overall, a high level of self-confidence contrasted with low performance on the test. Less literate people had a poor assessment of their skills but did doubt their knowledge. Physicians were better responders, and accurate knowledge was significantly associated with sources of information and education level. However, being a health care professional (nurse or care assistant) did not improve the rate of correct answers.
Conceptually, no one wants to be average. A cognitive bias exists as individuals usually judge themselves being superior to the majority, mostly in fields with significant social value. In their seminal publication [1], Dunning-Kruger recognized the “superiority illusion” in various fields, such as sense of humor, grammar, and logic. Here we verify the concept of “over average syndrome” in a unique situation. Indeed, self-appraisal of knowledge about COVID-19 was equivalent whatever the performance on the questionnaire. The source of information may account for this discrepancy.
Speculations about a genetic link between HIV and SARS-CoV-2 have circulated online. This false claim revolves around a broader conspiracy theory about the source of COVID-19. In a convenience sample of US and UK residents, more than 20% answered that SARS-CoV-2 could be “a bioweapon developed by a government or a terrorist organization” [3]. In our survey, a minority correctly answered this question. This does not indicate belief in conspiracy theories, but does underline the potential influence of these ideas on social media, a frequent source of information for participants with lower rates of correct answers. Because of population distrust toward government policies, the Organisation for Economic Co-operation and Development released guidelines to improve communication initiatives in the setting of COVID-19, stressing the need to combat misinformation and target more vulnerable social groups [4].
Indeed, misinformation on social media affects medical science and is a major public health threat [5]. In terms of the COVID-19 pandemic, misinformation and conspiracy theories are fostered on social media more than mainstream sources of information [6]. Despite high regulation of mainstream media content, misstatements are sometimes released [7] in traditional media, although quantification of this phenomenon and its actual impact is unclear. Our questionnaire was inspired by the hot topics discussed during the pandemic. Surprisingly, the level of knowledge was weak for most items even though mainstream media was the principal source of information. However, questions answerable with firm scientific knowledge, such as herd immunity, obtained high ratings. Those on more speculative topics could have been difficult to answer. This underlines the importance of fair and transparent information [4].
Level of medical literacy obviously altered quality of response, and in our survey physicians had the best rating. Other health care professionals did not perform well. This puzzling observation has been previously reported in a population with a high level of education [8]. In our study, higher level of education was unsurprisingly related to better rating. This refers to the usual difficulties experienced by those with lower levels of education in understanding medical information and dealing with the complexity of scientific data [9].
This study has limitations. First, the participants were not representative of the general population because of their occupational positions. In particular, high levels of education were overrepresented. Generalization of the findings is, therefore, limited. Second, some participants may have randomly selected responses. However, people were free to participate without any incentive, answering the questionnaire required little time, and the subject was publicly debated. Of note, only 84 persons did not answer any questions. The validity of our results is still debatable, as our survey relies on few questions. However, we specifically targeted prominent topics covered by media at the time of the survey. Methodologically, the optimal number of questions is difficult to estimate and should be balanced by rate of participants, which we believe was acceptable in our study. Finally, we cannot exclude the possibility that some participants sought out the answers to questions online before filling out the questionnaire. To limit this bias, questionnaires were provided at the collection unit before participants had a COVID-19 test. However, we cannot exclude cheating because of worldwide access to web connection [10]. More likely, participants were unwilling to answer tricky questions; indeed, an inverse correlation existed between the number of participants answering a question and rate of correct response (r = –0.65).
CONCLUSIONS
During the pandemic, populations have been demanding regarding delivery of treatment whose efficacy was still controversial, causing unexpected behavior of the scientific and medical community [1]. Ability to manipulate changeable and moving scientific knowledge requires specific training to acutely weigh its validity. Whereas the public was strongly aware of the outbreak through broad information channels, overall knowledge was weak, with participants overestimating skills to apprehend information. These observations should prompt regulatory agencies and media to apply rules that limit dissemination of “infodemics” [4].
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
We thank all patients for participating in this study and members of the MONACOVID Study Group. Department of Anaesthesiology and Intensive Care Medicine: M Bourregba, JP Guerin, G Rousseau, I Rouquette. Department of Biology: C Fissore-Magdelein, S Gabriel-Solean. Department of Biostatistics: F Berthier. Department of Cardiologie: G Chironi, V Dupasquier, A Pathak. Department of Clinical Research: C Dugourd, M Nicolai, N Rijo. Department of Emergency Medicine: N Beau, YE Claessens, X Magdelein. Department of Gastrotrenterology: F Olyve. Department of Infectious Diseases: S Chaillou-Orpitz, RL Farhad, O Keita-Perse. Department of Nuclear Medicine: M Faraggi. Department of Pneumology: J Lépine, M Lorillou, C Maincent, C Perrin. Department of Radiology: S Bertrand, P Brunner, C Dittlot, F Fuerxer, M Liberatore. Administration: B de Sevelinges, C Lecerf, S Couture, M Bigorgne, S Diaz.
Financial support. None.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Patient consent. Not applicable.
Author contributions. A.C., Y.E.C., and J.R. designed the study. O.K.P., S.C., G.C., A.P., and G.R. enrolled the participants. Y.E.C. supervised the study. O.K.P., F.B., and J.R. performed statistical analysis. A.C., F.B., O.K.P., J.R., and Y.E.C. wrote the manuscript. G.C., H.R., V.A., C.P., and B.M. contributed to critical revision of the report. All authors approved the final draft of the manuscript.
References
- 1. Oliveira J E Silva L, Vidor MV, Zarpellon de Araújo V, et al. Flexibilization of science, cognitive biases, and the COVID-19 pandemic. Mayo Clin Proc 2020; 95:1842–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol 1999; 77:1121–34. [DOI] [PubMed] [Google Scholar]
- 3. Geldsetzer P. Knowledge and perceptions of COVID-19 among the general public in the United States and the United Kingdom: a cross-sectional online survey. Ann Intern Med 2020; 173:157–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. OCDE. Transparency, communication and trust: the role of public communication in responding to the wave of disinformation about the new coronavirus. 2020. Available at: https://www.oecd.org/coronavirus/policy-responses/transparency-communication-and-trust-bef7ad6e/. Accessed 30 December 2020.
- 5. Wang Y, McKee M, Torbica A, et al. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med 2019; 240:112552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Allington D, Duffy B, Wessely S, et al. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ofcom. London real: COVID-19. Ofcom broadcast and on demand bulletin.2020. Available at: https://www.ofcom.org.uk/__data/assets/pdf_file/0020/194402/sanction-decision-estv.pdf. Accessed 17 September 2020.
- 8. Bachmann LM, Gutzwiller FS, Puhan MA, et al. Do citizens have minimum medical knowledge? A survey. BMC Med 2007; 5:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Health literacy: report of the Council of Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA 1999; 281:552–7. [PubMed] [Google Scholar]
- 10. Roberts JA, Wasieleski DM. Moral reasoning in computer-based task environments: exploring the interplay between cognitive and technological factors on individuals’ propensity to break rules. J Business Ethics 2012; 110:355–76. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.