Abstract
Background: Although there is a great deal of conversation on social media, there may not be good communication.
Objective: We sought to investigate communicaton activity online by examining digital footprints (or “sociomes”) of asthma stakeholders on Twitter.
Methods: Tweets containing the word “asthma” and the hashtag #asthma were collected using Symplur Signals. Characteristics of usage and tweets were analyzed and compared first between the word “asthma” and the hashtag #asthma, and then among four different stakeholder groups: clinicians, patients, healthcare organizations, and industry.
Results: The #asthma sociome was significantly smaller than the “asthma” sociome, with fewer users and tweets per month. However, the #asthma sociome correlated better to asthma seasons and was less susceptible to vulgarity and viral memes. For the #asthma sociome, there were 695,980 tweets by 308,370 users between April 2015 and November 2018. Clinicians were responsible for 16% of tweets, patients 9%, healthcare organizations 22%, and industry 0.3%. There were significant differences in the tweet characteristics, with healthcare organizations more likely to tweet with links, clinicians more likely to mention other users, and industry more likely to use visuals. Each April–May, there were significant spikes in the frequency of tweets by patients, healthcare organizations, and industry, whereas the usage patterns of clinicians were more random. There were also differences in the top terms and hashtags tweeted with #asthma in the stakeholder groups.
Conclusion: Asthma stakeholder groups tweet differently, at different times, and use different associated terms. Further exploration may help improve health care–related communication and help guide education of patients and clinicians.
Keywords: asthma, social media, healthcare communication, digital health, patient-centered care
Increasingly, people are living their lives online. In 1995 just 14% of American adults used the Internet, but by 2014 87% were regular Internet users (1). According to recent studies, 80% of Internet users are searching for health information online, and >40% of patients report that material found on social media affects the way they deal with their health (2, 3).
Patients and caregivers are turning to social media for education and support. They use social media to get feedback from others about doctors, to discover the latest treatments and medications, and to form online groups to support one another during difficult times (4–9). Clinicians are using social media to teach and to learn from each other, to advocate for causes, and to educate the public (10–20). Healthcare organizations and industry also have an active social media presence and regularly post educational and marketing content (21).
It is unclear, however, whether these online discussions overlap (22, 23). In order to gain insight into these conversations, we sought to investigate the patterns of activity online by examining the digital footprints (or “sociomes”) of asthma stakeholders on Twitter and to define sociomes for each stakeholder group. An understanding of the similarities and differences in the sociomes of clinicians, patients, and caregivers may allow us to improve health care–related communication and ultimately provide more patient-centered care. This work was previously published in abstract form (24).
Methods
Twitter, one of the most commonly used microblogging websites, was used to characterize the sociomes. Symplur Signals (Symplur, LLC), an online analytic tool, was used to track all tweets. First, we sought to determine the best methodology to characterize the activity regarding asthma on Twitter. Our goal was to determine whether the activity surrounding the hashtag #asthma provided less irrelevant and inappropriate data than the activity surrounding the word “asthma.” We collected and compared all tweets between April 2015 and September 2018 that contained the word “asthma” or the hashtag #asthma. These datasets were independent and did not overlap unless a tweet included both the word “asthma” and the hashtag #asthma. Monthly data were collected on the number of tweets and users, the characteristics of these tweets, impressions (i.e., potential views of the tweets based on the number of followers of the user tweeting), and other terms most commonly used with the word “asthma” or the hashtag #asthma. Positive sentiment was determined by Symplur Signals using a proprietary natural language processing algorithm optimized for healthcare conversations (25).
Next, we analyzed all tweets that contained the hashtag #asthma by users in different stakeholder groups between April 2015 and November 2018. Users were classified by Symplur Signals and were spot-checked for accuracy by C.L.C. and V.K. Symplur uses machine learning models, algorithms, and manual human evaluation and quality control to categorize 19 different categories of stakeholders (26). We aggregated these categories into four stakeholder groups (clinicians, patients, healthcare organizations, and industry). The tweets of users identified by Symplur Signals as spam accounts were excluded. Spam accounts were defined as accounts that posted large volumes of unsolicited highly irrelevant tweets, often automatically. Clinicians were defined as user accounts classified by Symplur as “doctor,” “researcher,” “healthcare provider,” or “individual other-health.” Healthcare organizations were defined as user accounts classified by Symplur as “provider organization,” “research/academic organization,” “other healthcare organization,” or “advocacy organization.” Patients were defined as user accounts classified by Symplur as “caregiver/advocate,” “patient,” or “individual non-health.” Industry was defined as user accounts classified by Symplur as “organization pharma” or “organization med device.”
Data were collected on the activity, including the number of users and tweets for each month, as well as the words, phrases, and hashtags commonly used with the hashtag #asthma. Impressions (or potential views of the tweets based on the number of followers of the user tweeting) were also collected. Characteristics of the tweets were also reviewed to ascertain whether they contained links to websites, mentions of other users, visual media (pictures, graphics interchange format, or video), average sentiment of the tweets, and whether the tweets were retweeted or replied to. These data were compared among the four stakeholder groups.
Descriptive and comparative statistics were obtained for both of these phases. Data were analyzed using JMP statistical software (version 10.0.1; SAS Institute Inc.) in consultation with the Office of Research at Connecticut Children’s. Data are reported as frequencies (%), as mean ± standard deviation, or as median with 25–75% interquartile range depending on the type and distribution of the variables. A Shapiro-Wilk test was used to assess normality. Stakeholder groups were compared using appropriate parametric tests and nonparametric statistics, including chi-square, t tests, and Wilcoxon rank sum. A P value < 0.05 was considered statistically significant. This study was reviewed by Connecticut Children’s Institutional Review Board and considered exempt.
Results
Comparing “Asthma” and #Asthma
Between April 2015 and September 2018, the dataset that included all of the tweets with the hashtag #asthma was significantly smaller, with fewer monthly tweets, monthly users, and monthly impressions than the “asthma” dataset (Table 1). An examination of tweet characteristics showed that tweets containing the hashtag #asthma included significantly higher percentages of links and visual media (images, graphics interchange format, or video). Tweets containing the hashtag #asthma also had significantly higher positive sentiment and lower percentages of replies, although the frequencies for both of these were quite close (Table 1).
Table 1.
Comparing #asthma and asthma datasets
| #Asthma | Asthma | P Value | |
|---|---|---|---|
| Monthly totals | |||
| Tweets | 14,276 (13,134–15,703) | 148,021 (132,172–168,778) | <0.0001 |
| Users | 6,570 (5,949–7,158) | 95,013 (88,416–112,719) | <0.0001 |
| Impressions | 70.7 million (61.5–87.7 million) | 718.2 million (616.8–848.2 million) | <0.0001 |
| Characteristics of tweets | |||
| Percentage of tweets with links | 71% (67–76%) | 39% (36–44%) | <0.0001 |
| Percentage of tweets with mentions | 59% (53–66%) | 55% (51–66%) | 0.39 |
| Percentage of tweets with visual media | 37% (24–49%) | 18% (15–24%) | <0.0001 |
| Percentage of tweets with replies | 1% (1–2%) | 8% (7–9%) | <0.0001 |
| Percentage of retweets | 47% (41–53%) | 43% (39–51%) | 0.57 |
| Percentage of tweets with positive sentiment | 60% (56–63%) | 52% (49–55%) | <0.0001 |
Data are presented as median (interquartile range).
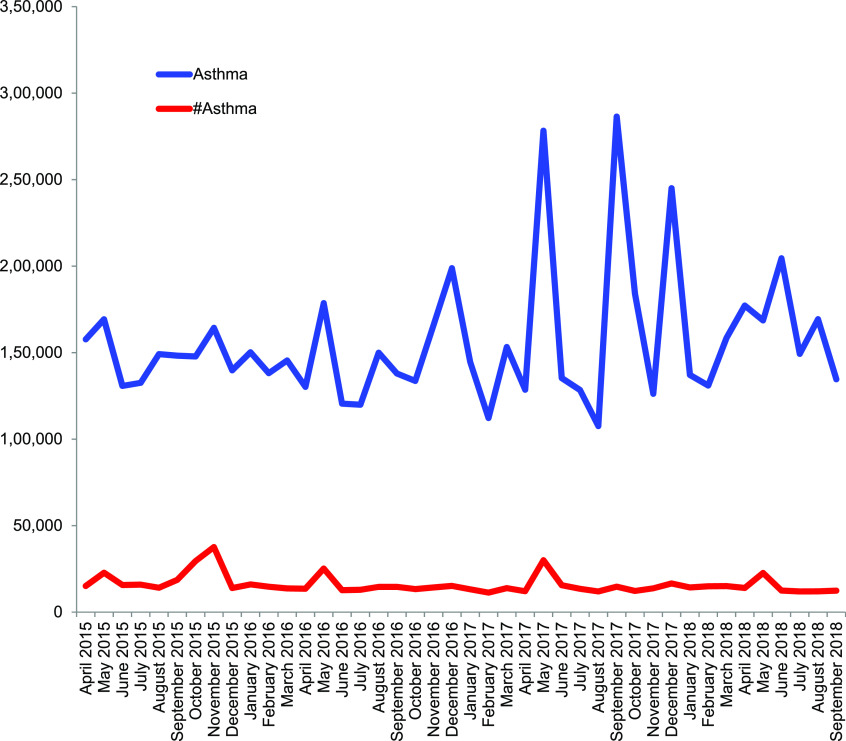
When we examined trends in usage over time, we found that tweets containing the hashtag #asthma had regular spikes in usage during April and May each year, corresponding to spring and Asthma Awareness Month, whereas spikes in tweets containing the word “asthma” occurred randomly (Figure 1). An examination of terms commonly used with either #asthma or “asthma” showed that almost half of the top 10 terms most commonly tweeted with “asthma” contained either vulgarity or phrases found in viral memes (27), whereas no vulgarity or memes were found in terms commonly tweeted with the hashtag #asthma (Figure 2).
Figure 1.
Comparing monthly tweets containing the word “asthma” and the hashtag #asthma.
Figure 2.
Top 10 phrases most commonly used with the keyword “asthma” and the hashtag #asthma (blue, asthma; red, #asthma). The size of the term reflects the relative frequency of usage. Profanity has been removed.
Characterizing the #Asthma Sociome of Stakeholder Groups
Next, the sociomes of four different stakeholder groups (clinicians, patients, healthcare organizations, and industry) containing the hashtag #asthma were analyzed and compared. Between April 2015 and November 2018, there were 695,980 tweets containing the hashtag #asthma by 308,370 users, with 3.5 billion impressions. Among the identifiable stakeholders, healthcare organizations were responsible for a larger number of the total tweets, users, and impressions than clinicians, patients, and industry (Table 2).
Table 2.
Comparing stakeholder sociomes for #asthma from April 2015 to November 2018
| Clinicians | Patients | Industry | Healthcare Organizations | |
|---|---|---|---|---|
| Total | ||||
| Tweets | 108,735 | 59,521 | 2367 | 154,884 |
| Users | 43,362 | 28,335 | 625 | 40,211 |
| Impressions | 366,630,356 | 330,859,987 | 92,990,920 | 1,076,588,415 |
| Monthly | ||||
| Tweets/mo | 2,154 (1,956–3,089) | 1,274 (1,110–1,503) | 35 (26–65) | 3,370 (2,555–4,065) |
| Tweets/h/mo | 2.9 (2.6–4.1) | 1.7 (1.5–2.0) | 0.1 (0.04–0.1) | 4.6 (3.5–5.5) |
| Percentage of tweets with links/mo | 69% (62–76%) | 71% (63–76%) | 60% (51–77%) | 79% (77–85%) |
| Percentage of tweets with mentions/mo | 78% (75–81%) | 65% (55–69%) | 44% (34–61%) | 48% (41–55%) |
| Percentage of tweets with visual media/mo | 37% (25–43%) | 39% (29–44%) | 59% (42–73%) | 41% (27–51%) |
| Percentage of tweets with replies/mo | 1% (1–2%) | 2% (1–2%) | 0% (0–0%) | 1% (0–1%) |
| Percentage of retweets/mo | 64% (56–68%) | 57% (47–62%) | 28% (16–41%) | 35% (29–41%) |
| Positive sentiment/mo | 59% (56–63%) | 52% (50–55%) | 66% (59–76%) | 59% (55–61%) |
| Users/mo | 943 (833–1,070) | 624 (514–727) | 12 (10–18) | 859 (804–949) |
| Percentage of users with one tweet/mo | 72% (71–74%) | 75% (73–77%) | 40% (32–53%) | 61% (59–62%) |
| Percentage of users with >10 tweets/mo | 2% (2–3%) | 2% (2–3%) | 0% (0–9%) | 5% (5–6%) |
| Tweets/user/mo | 2.2 (2.0–2.5) | 2.0 (1.9–2.2) | 3.2 (2.3–4.3) | 3.8 (3.2–4.0) |
| Impressions/mo | 7.3 million (5.8–10.6 million | 6.7 million (4.9–9.5 million) | 1.1 million (0.5–2.3 million) | 20.6 million (18.3–23.8 million) |
Data are presented as median (interquartile range).
In a comparison of patient and clinician sociomes, the clinician sociome was larger in terms of overall tweets and users, as well as monthly tweets (P < 0.0001) and users (P < 0.0001). Industry had the smallest number of users and tweets but relatively higher numbers of total and monthly impressions (Table 2).
There were also significant differences in tweet characteristics among the stakeholder groups. Healthcare organizations were most likely to tweet with links (P < 0.001), clinicians were most likely to mention other users (P < 0.0001), and industry was most likely to use visual media (P < 0.001). There were also more retweets in the clinician and patient sociomes than in the industry and healthcare organization sociomes (P < 0.0001) (Table 2).
When we compared just the clinician and patient sociome tweet characteristics, we found that the clinician sociome had a higher frequency of tweets with mentions (P < 0.0001), higher positive sentiment (P < 0.0001), and lower frequency of tweets with replies (P = 0.04), although overall the frequency of replies was very low in all stakeholder groups (Table 2).
The clinician and patient sociomes had higher frequencies of users with only one tweet per month (P < 0.0001) than healthcare organizations and industry. Healthcare organizations had the highest frequency of users with more than 10 tweets per month (P < 0.0001), although all stakeholder groups had low percentages of users with more than 10 tweets per month (Table 2).
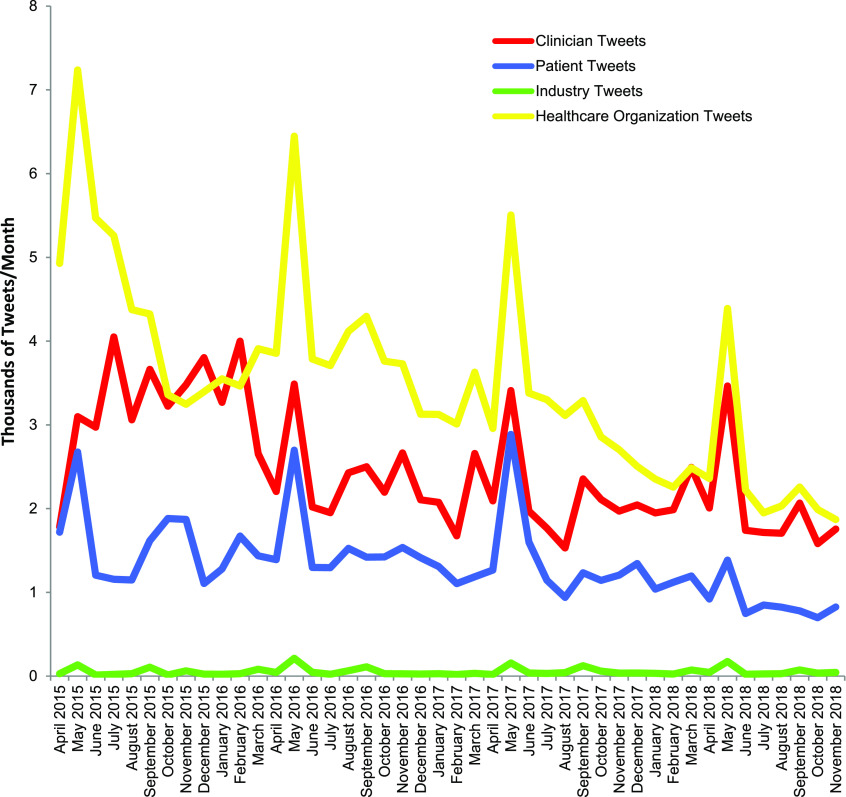
All of the stakeholder groups, except for clinicians, had significant spikes in frequency of tweets in April–May of each year (patients P = 0.02, healthcare organizations P = 0.01, industry P = 0.04) (Figure 3). The pattern of tweets by clinicians was more random. Industry also had an increased number of tweets in September of each year (P = 0.01).
Figure 3.
Monthly tweets containing the hashtag #asthma by stakeholder group.
There were also differences in the top 10 terms and top 10 hashtags most commonly tweeted with the hashtag #asthma in the stakeholder groups. Only the term “asthma” and the hashtag #COPD were included in the top 10 for all stakeholder groups. Patients, clinicians, and healthcare organizations all had the hashtags #allergy and #allergies in their top 10. Several other themes emerged. Industry had several hashtags of international meetings within their top 10, whereas none of the other stakeholder groups did. In addition, in the patient sociome, 6 of the 10 associated hashtags were hashtags of other disease states or hashtags associated with marijuana. There were also some common themes across the stakeholder groups in the associated words. Terms related to “children,” “help,” and “learn” were in the top 10 associated terms in all stakeholder groups (Table 3).
Table 3.
Top 10 hashtags and words commonly tweeted with the hashtag #asthma by a stakeholder group between April 2015 and November 2018
| Stakeholder Group |
|||
|---|---|---|---|
| Clinician |
Patient |
Industry |
Healthcare Organization |
| Associated Hashtag (Number of Times Used) | |||
| #medicalresearch (15,232) | #copd (4,624) | #copd (275) | #copd (9,478) |
| #copd (7,024) | #cancer (2,927) | #worldasthmaday (164) | #allergies (7,420) |
| #allergy (3,897) | #allergies (2,873) | #ERScongress (115) | #allergy (6,388) |
| #allergies (3,075) | #health (2,712) | #DYK (102) | #breatheez (6,384) |
| #health (2,639) | #cannabis (2,339) | #ERSLDN2016 (82) | #health (4,814) |
| #worldasthmaday (2,330) | #allergy (1,866) | #severeasthma (75) | #worldasthmaday (2,907) |
| #respiratory (1,643) | #fibro (1,794) | #remedies (72) | #children (2,242) |
| #foodallergy (1,041) | #autism (1,783) | #ERS2015 (71) | #respiratory (2,082) |
| #airpollution (993) | #marijuana (1,731) | #ATS2017 (68) | #tempe (1,693) |
| #diabetes (933) | #medicalmarijuana (1,670) | #respiratory (65) | #chandler (1,689) |
| Clinician |
Patient |
Industry |
Healthcare Organization |
|---|---|---|---|
| Associated Word (Number of Times Used) | |||
| post (9,770) | asthma (4,640) | asthma (260) | asthma (19,186) |
| asthma (7,231) | help (2,417) | patients (204) | symptoms (7,506) |
| children (3,395) | benefit (2,208) | learn (155) | children (6,073) |
| discuss (3,172) | smoke (1,537) | symptoms (153) | help (4,963) |
| patients (3,105) | learn (1,091) | people (117) | learn (4,384) |
| love (2,425) | info (1,052) | severe (94) | patients (4,248) |
| help (2,068) | research (973) | help (89) | people (3,898) |
| severe (2,036) | children (881) | control (85) | risk (2,779) |
| study (1,602) | kids (814) | treatment (43) | kids (2,514) |
| risk (1,430) | people (797) | 55 countries (27) | severe (2,436) |
Discussion
Establishing definitions is a key step in any research, and especially research in social media. In this analysis, we outlined parameters to define a digital footprint (or “sociome”) for health care–related stakeholders and established a methodology and framework for future analyses. This is the first time that data from Twitter have been used to define the characteristics of how a group of healthcare stakeholders use social media involving a clinical condition. We hope that this may serve as a guide for others to define stakeholder sociomes for other disease states.
Characterizing health care–related activity on social media could serve as an important step in understanding how to use this platform to engage key stakeholders for different disease states, disseminate timely information, encourage dialogue to dispel myths, and break down traditional barriers to access source-verified information. Moreover, there is a huge amount of health care–related activity on social media. The asthma sociome alone contains an enormous number of tweets and views and is only one small part of the vast landscape of health care–related activity occurring on social media. It is critical that healthcare stakeholders understand how different groups are participating in this landscape.
In addition, the associated terms used in the patient sociome suggest a need for improved education and communication with other stakeholder groups. For example, patients frequently used terms associated with other disease states and marijuana use when tweeting about asthma. Clinicians, healthcare organizations, and industry need to be present on these social media platforms to provide much-needed knowledgeable voices.
These findings may also have significant implications for medical education. Clinicians are increasingly using social media to learn and to educate themselves (15). Learners follow specific accounts or hashtags related to clinical topics or disease processes and form strong online communities by doing so (20, 28). However, choosing which accounts and hashtags to follow may have significant implications. In this analysis, we found that searching by keyword rather than a hashtag linked to activity with more viral memes and unrelated keywords. In addition, we found that some stakeholder groups shared more tweets with unrelated keywords and possibly junk. It is likely that different user accounts differ with regard to the quality of their tweets and content. When choosing accounts and hashtags to follow, learners should be careful to choose reliable voices.
We found significant differences in the way different health care–related stakeholder groups tweet about asthma. Different stakeholder groups had different frequencies and types of tweets, posted at different times of the year, and used different terms when they tweeted about asthma. In order to target education and health behavior changes, we need to speak the same language. A closer examination of how these sociomes relate may improve health care–related communication and ultimately help provide more patient-centered care.
Healthcare organizations were the stakeholder group responsible for the largest share of the tweets. This is perhaps not surprising. Healthcare organizations expend significant resources on the use of social media to educate the public, to promote causes, and to market their organizations (21). We found that healthcare organizations were most likely to tweet with links, and industry was most likely to tweet with visuals. This suggests that these stakeholders use more sophisticated and crafted tweets composed by professional staff experienced in social media.
We found that analyzing the digital footprint around the hashtag #asthma seemed to be a better methodology to characterize a digital health footprint than examining the footprint around the keyword “asthma.” The sociome of the hashtag #asthma was smaller, but it correlated better to asthma seasons, had more structured tweets with more links and visuals, and was less susceptible to vulgarity and viral memes. When determining the characteristics of stakeholder groups tweeting in a particular area, researchers may obtain more relevant data by identifying key disease-specific hashtags.
Compared with the sociomes of healthcare organizations and industry, those of clinicians and patients had a higher frequency of users with only one tweet per month using the hashtag #asthma. One possible explanation for this is that healthcare organizations and industry may have a more focused marketing and education plan for asthma, whereas clinicians and patients use the hashtag #asthma more sporadically. Compared with other stakeholder groups, clinicians were more likely to mention other users in their tweets. It may be that clinicians are networking more in their tweets than the other groups.
Each year, April and May had higher numbers of tweets by industry, healthcare organizations, and patients. This is also unsurprising. May is Asthma Awareness Month in the United States and the United Kingdom, and World Asthma Day also falls in May. Healthcare organizations around the world have supported asthma education efforts during the month of May. In addition, April corresponds to spring, which annually sees an increase in symptomatology in allergy-sensitive patients with asthma.
Impressions are a flawed measure and overestimate reach in social media analysis (29). Although users with higher numbers of followers will generate a larger impression, this does not necessarily mean that users saw or interacted with that tweet. In our sample, the industry sociome had the smallest number of users (0.2% of all tweets with #asthma) and tweets (0.3%) but had a relatively higher number of impressions (3% of all tweets with #asthma). This suggests that industry Twitter accounts had larger numbers of followers, leading to higher numbers of impressions, but does not necessarily mean that industry has a larger reach. Similarly, a comparison of patient and clinician sociomes showed that the two groups had a similar number of impressions, even though the patient sociome had a smaller number of users and tweets. This suggests that users in the patient sociome had higher numbers of followers than those in the clinician sociome. And although consumers of information on Twitter are usually not passive (30), these impressions likely do not represent active engagement.
Although users with higher numbers of followers will generate a larger impression, this does not necessarily mean that users saw or interacted with that tweet.
This study was limited by several factors. Given the large number of user accounts involved, we could not manually verify every stakeholder categorization, and some of those that we did not verify may have been miscategorized. The dataset also contained a significant number of unidentifiable users, which may have affected the results. In addition, we did not analyze conversations or networks of communication in this analysis, but rather focused on activity. For example, it may be that patients and caregivers are engaging in conversations parallel to those that clinicians are having, and that these silos are hampering communication between these stakeholder groups. To measure conversations, one must measure the replies to tweets, or what is commonly referred to as a reciprocated vertex pair in computer science (31). Groups may have different thought leaders and may be influenced by different types of links and media. Some of these issues will be the focus of future investigations—the current study serves to outline the parameters of a sociome and establish the feasibility of the analysis presented here. Answering some of these questions would also require a qualitative analysis and a deeper dive into tweet- and user-level metrics. Future directions for analysis include an examination of tweets and links that drive these conversations and a closer examination of interactions among these stakeholder groups. Defining “sociomes” or digital health footprints related to asthma is feasible and provides insight into these networks. In this analysis, we found that different healthcare stakeholder groups using the hashtag #asthma tweet differently, at different times, and use different associated terms. Further exploration may provide improved health care–related communication. In addition, this disease-specific focus provides more specific insights into a methodology that may be generalized to other areas of medicine.
Supplementary Material
Footnotes
Supported by an InCHIP–UConn Center for mHealth and Social Media Seed grant for Research on Social Media and Health.
Author Contributions: Conception and design: C.L.C., V.K., K.A.S., and N.S.D. Data collection: C.L.C. and V.K. Analysis and interpretation: C.L.C., V.K., K.A.S., and N.S.D. Drafting of the manuscript for important intellectual content: C.L.C., V.K., K.A.S., and N.S.D.
Originally Published as DOI: 10.34197/ats-scholar.2019-0014OC
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Fox S, Rainie L.The Web at 25. Pew Research Center. February 2014[accessed 2019 Nov 1]. Available from: http://www.pewinternet.org/2014/02/27/the-web-at-25-in-the-u-s/
- 2.Hamm MP, Chisholm A, Shulhan J, Milne A, Scott SD, Given LM, et al. Social media use among patients and caregivers: a scoping review. BMJ Open. 2013;3:e002819. doi: 10.1136/bmjopen-2013-002819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pennic F.80% of Internet users look online for health information. HIT Consultant; 2012 [accessed 2019 Nov 1]. Available from: https://hitconsultant.net/2012/11/21/80-of-internet-users-look-online-for-health-information-infographic-2/
- 4.Points Group. 10 surprising statistics on how social media is changing the healthcare industry; 2016 [accessed 2019 Nov 1]. Available from: https://www.pointsgroup.com/10-social-media-statistics-for-healthcare/
- 5.Hawn C. Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood) 2009;28:361–368. doi: 10.1377/hlthaff.28.2.361. [DOI] [PubMed] [Google Scholar]
- 6.Househ M. The use of social media in healthcare: organizational, clinical, and patient perspectives. Stud Health Technol Inform. 2013;183:244–248. [PubMed] [Google Scholar]
- 7.Sugawara Y, Narimatsu H, Hozawa A, Shao L, Otani K, Fukao A. Cancer patients on Twitter: a novel patient community on social media. BMC Res Notes. 2012;5:699. doi: 10.1186/1756-0500-5-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Narimatsu H, Matsumura T, Morita T, Kishi Y, Yuji K, Kami M, et al. Detailed analysis of visitors to cancer-related web sites. J Clin Oncol. 2008;26:4219–4223. doi: 10.1200/JCO.2008.18.7468. [DOI] [PubMed] [Google Scholar]
- 9.Fisher J, Clayton M. Who gives a tweet: assessing patients’ interest in the use of social media for health care. Worldviews Evid Based Nurs. 2012;9:100–108. doi: 10.1111/j.1741-6787.2012.00243.x. [DOI] [PubMed] [Google Scholar]
- 10.Chou WY, Hunt YM, Beckjord EB, Moser RP, Hesse BW. Social media use in the United States: implications for health communication. J Med Internet Res. 2009;11:e48. doi: 10.2196/jmir.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choo EK, Ranney ML, Chan TM, Trueger NS, Walsh AE, Tegtmeyer K, et al. Twitter as a tool for communication and knowledge exchange in academic medicine: a guide for skeptics and novices. Med Teach. 2015;37:411–416. doi: 10.3109/0142159X.2014.993371. [DOI] [PubMed] [Google Scholar]
- 12.Carroll CL, Ramachandran P. The intelligent use of digital tools and social media in practice management. Chest. 2014;145:896–902. doi: 10.1378/chest.13-0251. [DOI] [PubMed] [Google Scholar]
- 13.Bosslet GT, Torke AM, Hickman SE, Terry CL, Helft PR. The patient-doctor relationship and online social networks: results of a national survey. J Gen Intern Med. 2011;26:1168–1174. doi: 10.1007/s11606-011-1761-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheston CC, Flickinger TE, Chisolm MS. Social media use in medical education: a systematic review. Acad Med. 2013;88:893–901. doi: 10.1097/ACM.0b013e31828ffc23. [DOI] [PubMed] [Google Scholar]
- 15.Carroll CL, Bruno K, vonTschudi M. Social media and free open access medical education: the future of medical and nursing education? Am J Crit Care. 2016;25:93–96. doi: 10.4037/ajcc2016622. [DOI] [PubMed] [Google Scholar]
- 16.Pearson D, Bond MC, Kegg J, Pillow T, Hopson L, Cooney R, et al. Evaluation of social media use by emergency medicine residents and faculty. West J Emerg Med. 2015;16:715–720. doi: 10.5811/westjem.2015.7.26128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16:e267. doi: 10.2196/jmir.3589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Avcı K, Çelikden SG, Eren S, Aydenizöz D. Assessment of medical students’ attitudes on social media use in medicine: a cross-sectional study. BMC Med Educ. 2015;15:18. doi: 10.1186/s12909-015-0300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grajales FJ, III, Sheps S, Ho K, Novak-Lauscher H, Eysenbach G. Social media: a review and tutorial of applications in medicine and health care. J Med Internet Res. 2014;16:e13. doi: 10.2196/jmir.2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carroll CL, Bruno K, Ramachandran P. Building community through a #pulmcc Twitter chat to advocate for pulmonary, critical care, and sleep. Chest. 2017;152:402–409. doi: 10.1016/j.chest.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Carroll CL, Dangayach NS, Khan R, Carlos WG, Harwayne-Gidansky I, Grewal HS, et al. Social Media Collaboration of Critical Care Practitioners and Researchers (SoMe-CCCPR) Lessons learned from web- and social media-based educational initiatives by pulmonary, critical care, and sleep societies. Chest. 2019;155:671–679. doi: 10.1016/j.chest.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 22.The Conversation. Werder O.Everyone’s talking but no-one’s listening: it’s time to reclaim the art of communication2016 [accessed 2019 Nov 1]. Available from: http://theconversation.com/everyones-talking-but-no-ones-listening-its-time-to-reclaim-the-art-of-communication-67233
- 23.The Conversation. Groshek J.How social media can distort and misinform when communicating science; 2016 [accessed 2019 Nov 1]. Available from: https://theconversation.com/how-social-media-can-distort-and-misinform-when-communicating-science-59044
- 24.Carroll C, Dangayach N, Kaul V, Sala K, Bruno K. Describing the digital health footprints or “sociomes” of asthma on Twitter. Chest 2019;156:A998. [DOI] [PMC free article] [PubMed]
- 25.Symplur. Healthcare sentiment analysis [accessed 2019 Nov 1]. Available from: https://www.symplur.com/technology/sentiment-analysis/
- 26.Utengen A.Healthcare stakeholder segmentation.Symplur [accessed 2019 Nov 1]. Available from: https://help.symplur.com/en/articles/103684-healthcare-stakeholder-segmentation
- 27.@miilkkk. 75 mil, ima know every roach personally “be careful with Benjamin bruh he got asthma” [posted 2015 May 14]. Available from: https://twitter.com/miilkkk/status/599015990643597312?s=20
- 28.Barnes S, Riley C, Kudchadkar S.Social media for dissemination of pediatric critical care content. A hashtag analysis Crit Care Med 20164418026672925 [Google Scholar]
- 29.Mackenzie G.Have we passed “peak tweeting” at medical conferences? (and other final reflections on social media analysis). ScotPublicHealth. February 5, 2019; [accessed 2019 Nov 1]. Available from: https://scotpublichealth.com/2019/02/05/have-we-passed-peak-tweeting-at-medical-conferences-and-other-final-reflections-on-social-media-analysis/
- 30.Pershad Y, Hangge PT, Albadawi H, Oklu R. Social medicine: Twitter in healthcare. J Clin Med. 2018;7:E121. doi: 10.3390/jcm7060121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ranjan S, Sood S. Exploring Twitter for large data analysis. IJARCSSE. 2016;6:325–330. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.