Abstract
Background: Early experience during the coronavirus disease (COVID-19) pandemic and predictive modeling indicate that the need for respiratory therapists (RTs) will exceed the current supply.
Objective: We present an implemented model to train and deploy medical students in the novel role of “respiratory therapist extender” (RTE) to address respiratory therapist shortage during the COVID-19 pandemic.
Methods: The RTE role was formulated through discussions with respiratory therapists. A three-part training, with both online and in-person components, was developed and delivered to 25 University of Michigan Medical Students. RTEs were trained in basic respiratory care, documentation, equipment preparation, and equipment processing for clinically stable patients. They operate in a tiered staffing model in which RTEs report to a single RT, thereby extending his/her initial capacity.
Results: The first cohort of safely trained RTEs was deployed to provide patient care within 1 week of volunteer recruitment.
Conclusion: Our experience has demonstrated that healthcare professionals, including medical students, can be quickly trained and deployed in the novel RTE role as a surge strategy during the COVID-19 pandemic. Because we urgently developed and implemented the RTE role, we recognize the need for ongoing monitoring and adaptation to ensure patient and volunteer safety. We are sharing the RTE concept and training openly to help address RT shortages as the pandemic evolves.
Keywords: respiratory therapist extender, oxygen, COVID-19
Respiratory failure requiring oxygen support and/or mechanical ventilation is the signature injury of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Care requires not only adequate equipment, but also the expertise of trained respiratory therapists. Early experience during the coronavirus disease (COVID-19) pandemic, and predictive modeling, suggest that the need for respiratory therapists (“RTs”) will exceed the current supply. We therefore present an approach to train and deploy healthcare professionals, including medical students, in the novel role of “respiratory therapist extender” (“RTE”) to address the projected respiratory therapist shortage and improve patient outcomes during the COVID-19 pandemic.
Our RTE solution aligns with Michigan Governor Gretchen Whitmer’s Executive Order 2020-30, which granted scope of practice flexibility for healthcare workers at the discretion of the employing healthcare facility during the COVID-19 pandemic (1). Paragraph 2b of this order specifically “allow[s] medical students, physical therapists, and emergency medical technicians to volunteer or work within the facility as “respiratory therapist extenders” under the supervision of physicians, respiratory therapists, or advanced practice registered nurses. Such extenders may assist respiratory therapists and other health care professionals in the operation of ventilators or related devices.”
Senior medical students in particular are qualified candidates for this role, given their knowledge of respiratory physiology and pathophysiology as well as their clinical exposure and experience. Most medical students nearing completion of their training will have cared for patients requiring oxygen therapy and the intervention of respiratory therapists; already be comfortable working in a healthcare setting, including under infection control precautions; understand contemporary electronic health records and be facile at documentation; and have sufficient background in infectious diseases to make an informed personal decision about the risks and benefits of volunteering during a viral outbreak.
Methods
Needs Assessments
To determine which tasks and responsibilities to entrust to the RTE, we conducted both an internal and external needs assessment through informal discussions with RT leadership. We spoke with individuals active in the American Association for Respiratory Care (AARC), who confirmed that there was an evolving need for such an “extender” in areas where COVID-19 was most prevalent. We approached the Michigan Medicine Director of Respiratory Therapy to conduct an internal assessment. Through our discussions with respiratory therapy representatives, we weighed the following factors: 1) need for oversight 2), level of expertise required, and 3) impact on respiratory care workflow. Through this scaffolding, we determined that the initial RTE responsibilities would include oxygen and humidity therapy, patient respiratory assessments, incentive spirometry, equipment processing, and documentation. As RTEs show mastery in basic respiratory care, plans to introduce more advanced tasks like aerosolized treatments, suctioning, and continuous or bilevel positive airway pressure (CPAP/BiPAP) could be initiated.
The RTE role builds on and supplements existing respiratory therapy surge plans. Those surge plans often depend on RT recruitment from other institutions or the redeployment of other professionals such as Certified Registered Nurse Anesthesists (CRNAs) during a period in which RT capacity is stretched. However, these plans may require supplementation during a widespread pandemic as other facilities are also surging and CRNAs already redeployed as ICU providers.
Medical students’ foundation in respiratory physiology, pathophysiology, and management make them candidates for the RTE role. However, medical students lack the basic technical skills needed for the role. Therefore, the RTE training was designed to address these gaps by offering a basic review of respiratory physiology, pathophysiology, and management followed by an in-depth discussion on the practical skills required for the RTE role.
At the time of submission of this article, no formal medical school COVID-19 curriculum had been implemented at the University of Michigan. Many medical schools, including the University of Michigan, were rapidly moving toward the development of content, training, or guidelines to attempt to enable continued medical student learning during the pandemic. The RTE role was developed to address the projected healthcare worker shortage; however, it will also fill the medical student core competencies of service, professionalism, and interprofessional education. The RTE role is a purely voluntary opportunity, and although we intended to articulate and build upon the developing medical school curriculum, the role was structured such that it neither depended upon the medical school curriculum (because the RTEs were needed faster than the medical school curriculum could be deployed), nor was a mandatory part of it (as the RTE was a purely voluntary service opportunity, not part of the formal curriculum).
Recruitment
Following the American Association of Medical College’s guidelines recommending withdrawal of medical students from clinical rotations (2), University of Michigan medical students quickly organized the “M-Response Corps,” a student-led organization focused on coordinating volunteer COVID-19 response initiatives. The M-Response Corps has emphasized as a guiding principle that medical student involvement in various initiatives be purely voluntary. To reinforce the voluntary nature of the RTE role and emphasize that it is distinct from the formal medical school curriculum, our team chose to operate within the pre-existing M-Response Corps infrastructure. In collaboration with M-Response Corps and medical school administration, a formal document was drafted and distributed to students detailing the voluntary nature, as well as the associated risks, of participation. To ensure that RTE volunteers were operating in an appropriate role for their level of training, applications were restricted to third- and fourth-year medical students who previously completed their core clerkships. Of those who expressed interest, 25 volunteers were randomly selected to undergo RTE training.
RTE Training
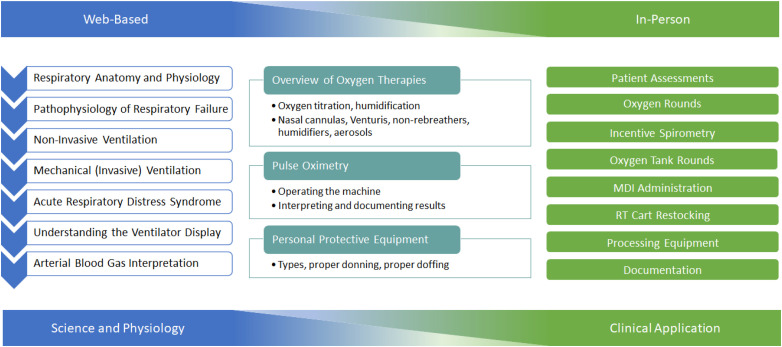
An overview of the RTE training is shown in Figure 1. The online portion of RTE training was created by medical students to address the review of respiratory physiology, pathophysiology, and ventilator mechanics. Information was presented in a series of seven PowerPoint lectures, with each followed by short comprehension assessments (see Appendix B in the data supplement). The training was independently reviewed by two pulmonary and critical care physicians to verify the accuracy of the presented information and ensure that our learning objectives were appropriate for the RTE role. These slides are available under a Creative Commons Attribution-NonCommercial 4.0 International, allowing noncommercial adaptation and sharing at www.drive.google.com/drive/u/1/folders/1whouEBqBgb_UZDaYeXN8AOwVvK945WvP.
Figure 1.
Overview of respiratory therapist extender training and its delivery. MDI = metered dose inhaler; RT = respiratory therapist.
To teach RTE-specific functions and skills, we collaborated with RTs to develop and deliver a hybrid online/skills-based module followed by an in-person skills training session (Appendix C in the data supplement). The first module covered oxygen and humidity therapy, pulse oximetry, equipment overview, and documentation, and had multiple built-in learning checks and competency assessments to ensure that RTEs were progressing appropriately. At the end of the in-person session, RTEs were assessed via an in-person practical proctored by trained RTs to ensure competency.
Future teachings may include administering aerosolized medications, suctioning, CPAP, and BiPAP. Each forthcoming module will follow the same general format as the first: an online didactic component followed by an in-person clinical skills session. Assessments will continue to include a clinical practical, and RTEs must show competency before performing treatments on actual patients.
Approach to Personal Protective Equipment
At our institutions, we were able to ensure that adequate personal protective equipment (PPE) (i.e., standard droplet and respiratory precautions) was available and that RTEs would receive the same standard of protection as other healthcare workers. All RTEs underwent formalized, in-person training on proper donning, doffing, storage, and disposal of appropriate PPE before in-person RTE training or patient interaction. All RTEs previously underwent official N95 mask and powered air-purifying respirators (PAPR) fitting. Occupational Health Services offered as-needed N95 and PAPR refitting to individuals directly interacting with COVID-19–positive patients.
Assessments
To assess comprehension and competency throughout the online modules, short online assessments (Appendix B in the data supplement) were included after each lecture. These evaluations function as knowledge checks, allowing students to reflect on their progress and to identify concepts that need further review. In addition, RTEs are required to pass an in-person, skills-based practical, proctored by trained RTs, before interacting with patients. To evaluate the educational effectiveness of the RTE training, online pre- and post-course assessments are required (Appendix A in the data supplement). Moving forward, these collected metrics will be used for quality assurance and improvement.
Results
Within 5 days of volunteer recruitment, we trained our first cohort of RTEs, including completion of the online training and the in-person PPE and RTE skills sessions. To ensure ongoing patient and volunteer safety, RTE volunteers are required to complete a standardized survey (Appendix D in the online supplement) after each shift to identify ongoing concerns, such as gaps in knowledge, issues with patient care, or inadequate resource allocation. Within 3 weeks of conceptualizing the role, the first group of RTEs began working in a hospital.
Discussion
Health services research on disaster relief efforts demonstrates that, during a disaster-induced critical health care worker shortage, essential ancillary staff like nurses and RTs are limiting factors more often than physicians (3). Given the natural history of COVID-19, specifically its progression to respiratory failure, the projected number of ventilated patients is expected to increase significantly, further burdening RTs. Although corporations are being asked to manufacture ventilators in anticipation of the increased need, many policy makers are neglecting the projected shortage of healthcare professionals to manage these ventilated patients (4). Thus, respiratory therapists will likely be in high demand due to a relative shortage, and the RTE role aims to address this shortage.
When considering how to most safely and effectively implement the RTE role in our health system, a variety of different models were considered. Currently, there are no well-established, evidence-based guidelines addressing RT:patient ratio (5). However, some estimate that under standard, nondisaster conditions, an RT can safely manage up to 10 stable patients or 4 ventilated patients independently (6, 7). Using this as a basis, a tiered staffing model was developed in which the RTEs report to a single RT, thereby truly extending his/her initial capacity. We hypothesize that this model will enable a single RT, now with RTE assistance, to approximately double his/her capacity to safely manage stable patients. More importantly, redistributing routine work to RTEs will allow RTs to focus on managing the critically ill. We also considered different potential models for RTE responsibilities, but ultimately chose to train RTEs on basic respiratory care, as this model enables us to minimize unnecessary RT oversight (which, in turn, maximizes RT workflow). More advanced RTE responsibilities, like ventilator management, were excluded due to concerns for patient safety, steep learning curves, and the immense oversight needed, all of which would limit the utility of the RTE.
Medical students were selected to be trained as the first wave of RTEs because of their clinical background and familiarity with the hospital system. Balancing patient care needs with medical student autonomy and safety was a cornerstone of our discussion. Medical students were explicitly informed of the voluntary nature of this role, which would be compensated neither monetarily nor in the form of academic credit or advancement. However, we recognized that real or perceived expectations, power dynamics, peer pressure, and social coercion may have undue influences on their decision to volunteer. While these pressures are pervasive throughout medical training, it was critical for our group to consider their ethical implications in the context of disaster response. Medical student involvement in this role will be regularly evaluated to ensure that students are not assuming excessive risk while volunteering, taking into account PPE availability, patient care needs, and availability of RTE volunteers outside the medical school.
It is important to note that the use of medical students serving in an RTE capacity was not the only strategy used by some of the RT departments involved. Additional measures included utilizing RT students, training RT technicians, and retraining RTs who had previously transferred to other departments (e.g., ECMO, PFT lab) to help fill the workforce gap. These strategies are not mutually exclusive, except to the extent that there are limitations to time and energy to train and plan.
We learned several lessons that may be relevant to others in this and future surges. The first was to involve RTs in design as early as possible. Their expert opinion was invaluable and ultimately redirected the trajectory of our training. For those implementing this role into their hospital system, a second lesson is to consider the logistics that go into creating a new position. RTEs need computer and electronic medical record access, permission to sign notes, permission to administer medications, keys, door codes, schedules, and a model that incorporates them into the preexisting infrastructure. It is important to address these roadblocks early so that they do not become a barrier to patient care in the future, especially in the wake of worker shortages.
The need for rapid creation of the novel RTE role in the presence of an escalating pandemic required our team to make decisions based on limited data. The urgent need for an expanded respiratory care workforce was determined by external predictive modeling, and assumptions were made about the number of patients an RT and RTE could care for based on expert opinion. Furthermore, given the limited size of our initial RTE cohort, insufficient data are available to quantitatively evaluate training efficacy and contribution of RTEs to the workforce. We recognize that assumptions made, and project limitations, indicate the need for continuous monitoring and evaluation of this program to ensure patient and volunteer safety and appropriate resource utilization.
Because of the potential for loss of human life, pandemics and other disasters necessitate the rapid development of inventive, simple solutions to novel challenges. The RTE role was created in response to the anticipated imminent need for additional providers trained in respiratory care during the COVID-19 pandemic. The development of a training to create a new position in the healthcare system would normally take months to years, but this one was developed and implemented over the course of approximately 2 weeks to rapidly deploy volunteers to the clinical setting. We plan to treat both the training and the RTE role as “living,” and will continue to make adjustments to ensure prioritization of patient and volunteer safety. We also plan to share the RTE concept and underlying training openly with other institutions, both to crowd-source continued improvements and to help address the need for expansion of respiratory care during the COVID-19 pandemic.
Supplementary Material
Footnotes
Supported by K12 HL138039 (T.J.I.). This work does not necessarily represent the views of the U.S. Government or Department of Veterans Affairs.
This article has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.State of Michigan, Office of the Governor Exec. Order No. 2020-30 (COVID-19), Temporary relief from certain restrictions and requirements governing the provision of medical services(March 30, 2020) [accessed 2020 Mar 30]. Available from: https://www.michigan.gov/whitmer/0,9309,7–387–90499_90705–523481–,00.html
- 2.Association of American Medical Colleges Important guidance for medical students on clinical rotations during the coronavirus (COVID-19) outbreak 2020[accessed 2020 Apr 12]. Available from: https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak
- 3.Occupational Safety and Health Administration. Pandemic influenza preparedness and response guidance for healthcare workers and healthcare employers. Washington, D.C.: Occupational Safety and Health Administration; 2009. [Google Scholar]
- 4.Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. [online ahead of print] 23 Mar 2020; DOI: 10.1056/NEJMsb2005114. [DOI] [PubMed]
- 5.Haupt MT, Bekes CE, Brilli RJ, Carl LC, Gray AW, Jastremski MS, et al. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Guidelines on critical care services and personnel: recommendations based on a system of categorization of three levels of care. Crit Care Med. 2003;31:2677–2683. doi: 10.1097/01.CCM.0000094227.89800.93. [DOI] [PubMed] [Google Scholar]
- 6.California Society for Respiratory Care Safe staffing standards Oakland, CA: California Society for Respiratory Care; 2016[accessed 2020 Apr 12]. Available from: https://www.csrc.org/resources/Documents/Safe%20Staffing%20files/Final%20Safe%20Staffing%20Papers/CSRC%20Staffing%20Position%20Statement%20and%20White%20Paper%20V10112016.pdf [Google Scholar]
- 7.Parker AM, Liu X, Harris AD, Shanholtz CB, Smith RL, Hess DR, et al. Respiratory therapy organizational changes are associated with increased respiratory care utilization. Respir Care. 2013;58:438–449. doi: 10.4187/respcare.01562. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.