Abstract
The coronavirus disease (COVID-19) pandemic has disrupted not only clinical care but also medical education. Physical distancing and shift rearrangements for both trainees and faculty have led to abrupt cancelation of many in-person didactics. These have been replaced by distance learning options, which include both synchronous and asynchronous curricula. Unfortunately, many medical educators have been forced to quickly create distance-learning options for trainees with little prior experience. In this perspective, we review the evidence base for distance learning and discuss practical considerations for transitioning traditional in-person curricula to distance platforms. We review technical aspects of distance learning as well as educational principles essential for success. The goal is for medical educators to optimize distance learning not just during this COVID-19 pandemic but beyond this crisis as well.
Keywords: education, distance, education, medical, graduate
With the rapid spread of coronavirus disease (COVID-19) throughout the United States, educators in graduate medical education (GME) programs have had to balance the competing tasks of continuing trainee education with protection of trainee health and safety through physical distancing requirements. Increased clinical demands on trainees have placed constraints on available time for scheduled didactic education.
Distance learning (occurring in separate physical spaces), whether synchronous (occurring at the same time) or asynchronous (occurring at separate times), provides a potential solution to these challenges. Both asynchronous and synchronous distance learning are common (1) though not universally used, with a 2017 survey of internal medicine program directors suggesting that the former was more commonly used than the latter (2).
Though educators may have no choice but to implement distance learning at this time, there is some evidence to suggest that distance learning techniques can be successful. A meta-analysis of electronic learning curricula found that asynchronous curricula had improved educational outcomes compared with no educational intervention and comparable effects compared with traditional forms of instruction (3). A successful asynchronous curriculum for trainees rotating in a pediatric emergency department provides an example suggesting that at least some learners will indeed access completely asynchronous curricula (4). Based on successful implementation of such curricula, the Emergency Medicine Residency Review Committee of the Accreditation Council for Graduate Medical Education has allowed up to 20% of required residency didactics to be presented asynchronously under the moniker “individualized interactive instruction” (5), stressing learning that is tailored to the individual and requiring active participation.
In this review, we will discuss practical considerations for beginning distance learning (synchronous and asynchronous) curricula in a GME program. The authors searched PubMed and Education Resource Information Centre (ERIC) databases for “e-learning,” “asynchronous learning,” “synchronous learning,” “remote learning,” “distance learning,” and related variations of these terms. We selected articles based on greatest relevance to GME. Given the abundance of free, open-access education on these topics, we also performed Google searches for the same topics for additional localization of resources outside of the medical literature. Institutional experience was used to supplement publications.
Tips for Synchronous Videoconferencing
Content can be delivered synchronously in a location-independent manner via any of several available videoconferencing platforms (Zoom, Webex, Blue Jeans, and others). Practical considerations for successful videoconferencing are listed in Table 1. Presenters and learners will likely need assistance at first navigating the platform, and it can be beneficial to have someone online to help (fellowship coordinator, program director, associate program director, core faculty member, or another administrator). This person can avoid technical issues by helping presenters screen share, mute, and unmute appropriately. A faculty emcee is also important to moderate chat traffic and facilitate discussion. Ensuring that presenters and learners are familiar with the platform and that learners have access to the hardware, software, and space to focus on didactics is crucial. For instance, if fellows are no longer meeting in a group in a small conference room for weekly didactics, will they be joining a videoconference from a loud and busy intensive care unit team room (where distractions might provide a challenge), or is there a quiet space with a computer available to them?
Table 1.
Practical considerations for using a videoconferencing platform for simultaneous distance learning
| Security issues - HIPAA compliance, institutional firewalls |
| Cost |
| Recording capabilities |
| Storage capabilities |
| Number of allowed participants and length of conference allowed |
| Hardware and software issues (institution computer, personal laptop, need for software installation, or application download) |
| Quiet space for learners to use, especially those on clinical rotations |
Definition of abbreviation: HIPAA = Health Insurance Portability and Accountability Act.
For conferences in which protected health information or sensitive information may be shared (such as morbidity and mortality conferences), it is essential to ensure that the platform is Health Insurance Portability and Accountability Act compliant. Double check with your institution before beginning. Additional technical considerations for videoconferencing are listed in Table 2.
Table 2.
Technical aspects of common distance-learning platforms
| Platform* | Zoom | Webex | Blue Jeans | GoTo Meeting | CyberLink U Meeting |
|---|---|---|---|---|---|
| Cost | Varies; free version available for smaller group sizes and shorter meetings | Varies; free version available for smaller group sizes and shorter meetings | Varies; no free option | Varies; no free option | Varies; free version available for smaller group sizes and shorter meetings |
| HIPAA compliance† | Possible but not automatic; confirm with subscription and your institution—some institutions have a HIPAA compliant and noncompliant version (16) | Possible but not automatic; confirm with subscription and your institution | Possible but not automatic; confirm with subscription and your institution and ensure encryption turned on | Possible but not automatic; confirm with subscription and your institution | Unclear |
| Application download required for viewing or hosting? | Not for viewing; yes for hosting | Not for viewing | Not for viewing; yes for hosting | No | No, platform is entirely browser based |
| Chat function | Yes | Yes | Yes | Yes | Yes |
| Recording | Yes | Yes | Yes | Yes, with some plans | Yes |
| Limit on duration | Yes, varies with subscription | No‡ | No | No | Varies (30 min with free version) |
| Notable security issues | Easy for hackers to access unless meeting is password protected; limit screen sharing to the host to prevent attacks. AES 256-bit encryption | TLS 1.2 and AES 256-bit encryption and backed by Cisco's networking | There is a telehealth version, need to ensure encryption is turned on; AES 256-bit encryption; fraud detection | Added feature, “meeting lock” and “risk-based authentication” (fraud detection). SSL and AES 256-bit encryption | “End-to-end encryption” on Enterprise version; all versions passed Information Security Certification by Mobile Application Security Alliance and Worldwide Server Security Certificate |
Definition of abbreviations: AES = Advanced Encryption Standard; HIPAA = Health Insurance Portability and Accountability Act; SSL = Secure Sockets Layer; TLS = Transport Layer Security.
Other platforms include Freeconference, Skype, and Google Hangouts Meet.
Be very careful to ensure your institution’s version of any platform is HIPAA compliant and that you are using all security features correctly, such as encryption. Recording to the cloud will not be HIPAA compliant, so ensure recording is off for sensitive topics. Your institution will need to have a business associate agreement with the platform.
Some platforms have temporarily expanded the services available for free because of coronavirus disease (COVID-19).
As much as you would for an in-person presentation, arrive early to work out the kinks: ensure the presenter is able to share his or her screen successfully and that you know how to mute and unmute attendees, minimize echo, and resolve other technical quirks of videoconference learning. For a large group, assign someone to be the chat moderator to relay questions from the chat platform at regular intervals to the presenter (6). Some platforms do not save the chat discussion, so assigning someone to export it and share with learners is important if valuable points have been raised.
In our experience, attendees may be less willing to interrupt presenters on videoconference than in person, so careful attention to making presentations interactive is crucial. Having the presenter pause regularly and solicit questions can help lower this barrier to interaction. In general, it is important to anticipate a transition period for both learners and teachers when moving to a distance platform and to set expectations for both groups (7).
Many of the best practices of small-group teaching and facilitating also apply to video conference learning (8): ensure that one person is not dominating the conversation, invite participation from quieter learners, keep learners engaged, and use techniques to encourage active learning on a regular basis. We have observed that when traditional teaching was moved from an in-person small-group setting to a videoconference platform, interaction dropped without formal opportunities for engagement, whereas in person, learners and faculty created interaction (i.e., interrupting for conversation). Therefore, priming speakers to use active learning techniques is particularly important in videoconferencing.
A virtual platform may require educators to use different strategies for learner engagement than they would typically use with an in-person session. For instance, peer teaching strategies such as think-pair-share will not be feasible if everyone is watching individually (although at least one platform—Zoom—will allow splitting an audience into groups for breakout sessions for more prolonged sessions of teamwork that might take 5–10 min). Therefore, educators might need to use techniques for individual learners to actively process content (9). These include the “1 minute paper,” in which learners are given a question with 1 minute to respond in writing; these responses could be written into the chat box, pasted to a shared online document, or emailed to the presenter. Another technique is the “muddiest point,” in which the teacher asks learners to share what is most confusing about material just presented (10).
Using audience response software according to best practices (11) can be a good mechanism to engage learners who are not together in one room. Even if audience response software is not used, teachers should build in opportunities for learner engagement every 10–15 minutes or in the middle of the session when learners’ attention is likely to be at a minimum; practical suggestions and a review of the theory behind this timing is found here (12).
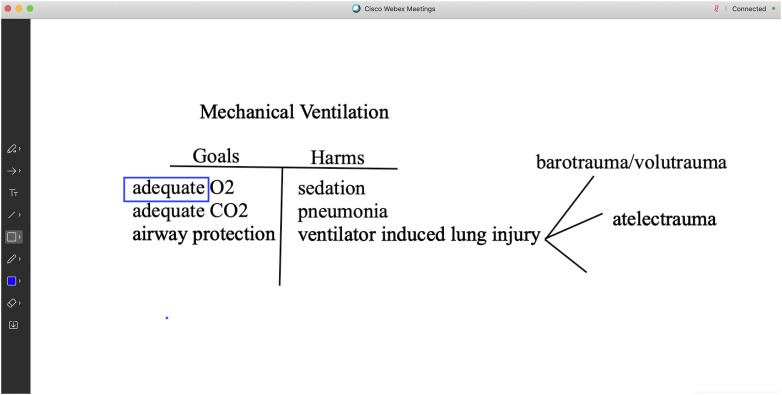
PowerPoint slide presentations will work well on any of the major platforms. A chalk talk can also be recorded but will require careful preparation and rehearsal to ensure that the writing is legible, the entire board is visible, and the speaker is audible. Some videoconferencing platforms have a “whiteboard” function that will allow for creating a virtual chalk talk, although we recommend practicing your chalk talk on the videoconference platform before delivering it, as the effect is somewhat different from a traditional whiteboard (an example is shown in Figure 1).
Figure 1.
Example “whiteboard” talk in Webex. A “whiteboard” talk can be created in several videoconferencing platforms, with the example shown here in Webex. This particular platform allows for erasing (icon second from the bottom left), use of different colors, and exporting screens to save what you’ve drawn.
Tips for Completely Asynchronous Learning
We do not recommend transitioning your entire curriculum to an asynchronous platform. First, some learners prefer traditional didactic curricula (13), and even when learners prefer asynchronous curricula, they may not actually utilize asynchronous resources in the manner educators intended. In one study of an emergency medicine clerkship for fourth-year medical students, over a third did not use asynchronous resources at all during the clerkship, though nearly 70% stated they preferred that modality (14). Furthermore, faculty time requirements may be prohibitive; a critical appraisal of recent flipped classroom literature suggested that creating high-quality asynchronous content can be more time and labor intensive for faculty than creating traditional didactics (15).
However, making some content completely asynchronous will allow flexibility for learners when scheduling does not permit a synchronous activity (e.g., night float rotations). Even in situations in which some in-person teaching is necessary (e.g., teaching new learners a procedure in a simulation laboratory), asynchronous learning may help streamline or truncate in-person didactics. For instance, flipped classroom and blended learning approaches have good success when used for procedural teaching (15) and could minimize the time learners need to spend in a simulation center.
The first option is to record all conferences; depending on the level of service purchased, most videoconferencing platforms allow recording. Consider your resources: there may be recorded didactics already available to you (e.g., other departments’ grand rounds) if speakers are unable to adapt their talks to a virtual platform. Note that prerecorded sessions are entirely passive, so it is crucial to add an active exercise to keep learners engaged. This will require some work ahead of time by a faculty moderator, such as creating a series of questions learners should address while watching. Learners can write a reflection or post on a discussion board. Alternatively, learners can watch a recorded lecture during a weeklong window and then have a facilitated discussion via one of the videoconferencing platforms above or on another platform such Skype (16).
When recording new content that is planned for asynchronous learning, educators will also have to avoid reliance on peer-teaching techniques for engagement and instead use individual processing strategies as highlighted above (10). Audience response software may be less meaningful in an asynchronous platform, but use of multiple-choice questions with sufficient time for learners to process can still be used. Avoiding simply passive content is essential. The Council of Residency Directors in Emergency Medicine specifically recommends against using purely passive methods (e.g., podcasts and videos) and question banks as the main methods of asynchronous learning (5).
One option for coordinating interaction and content in asynchronous learning is use of a learning management system (LMS), such as Sakai, Blackboard, Brightspace, or Moodle. An LMS allows for delivery of content, facilitation of communication, monitoring participation, and both general and focused assessment, whether with multiple choice questions or other tools (17). However, unless your program routinely uses a given LMS, learners may be unfamiliar with the platform. Usability of these systems can vary (18), and excess time spent navigating the LMS can be a deterrent to use. Some educators have gone so far as to create their own LMS to meet learners’ needs of simplicity and usability (19).
In addition to multiple-choice questions that can be offered through an LMS, discussion boards or forums can be very valuable tools to help learners process content and allow for asynchronous interaction. Thoughtful facilitation and attention to learners’ social needs in addition to cognitive needs is important in an asynchronous forum if learners are no longer meeting in person (20). If you are not using an LMS for your curriculum, you can still create a discussion board by using a Google document or other similar tool.
Examples of curricular changes made at two institutions in response to COVID-19 are shown in the Box; common themes include reliance on fellowship and division administrators for help with technical aspects of videoconferencing as well as use of recording to facilitate asynchronous learning. Additional resources for both technological and pedagogical aspects of web-based teaching are available for educators’ review (6, 9, 16, 21, 22).
Examples of Curricular Changes Made in Response to Coronavirus Disease (COVID-19) at Two Institutions
Institution A (Oregon Health & Science University)
• Cancelled research conference and grand rounds, continued fellows’ conference initially; resumed other conferences after clinical workload reached stability
• Used Webex (institution purchased) for morbidity and mortality (M&M) conference and initially used Zoom for fellows’ conference due to fellowship program leadership having greater experience with Zoom, then transitioned to Webex for all conferences given security concerns with Zoom
• Fellowship associate program director (APD) reached out to all fellows’ conference speakers ahead of time to ensure they could transition to virtual platform
• Fellowship APD provided tips for active learning and audience engagement to presenters
• Fellowship coordinator served as administrator to help with technical issues with fellows’ conference; division manager served as admin for M&M conference
• Conferences recorded and posted internally; this proved useful for asynchronous review by learners outside of the Pulmonary division and those on nights
• Use of learning management system (Sakai) to supplement intensive care unit teaching for internal medicine residents had mixed results partially because residents were unfamiliar with the learning management system, so this platform is being abandoned in favor of more familiar infrastructure
Institution B (New York University)
• Canceled traditional journal club and difficult case conference
• Created a COVID journal club and COVID case conference
• Using Webex (institutionally purchased) for both conferences, mainly for ease of use on mobile devices allowing for greater physical distancing, accommodation of large participant size, and reliable security encryption
• Utilizing Fellows and Faculty not on clinical duties (including quarantined individuals) to run these two conferences (to perform deep dives on the latest COVID journal articles for journal club and to collate interesting COVID cases for the case-based conference)
• Fellowship coordinators performing administrative role to schedule conference and handle logistics and technical issues
• Division Chief serving as a resource for mentoring the presenters, along with coordination from Program Director
• Webex feature of screen sharing helpful to display tables and figures for journal club and imaging/data for case-based conference
• Recording of session allowing for asynchronous playback for participants unable to join at the designated conference time
• Presentations emanating from COVID journal club and COVID case conference then lead to local rotation-specific group discussions on patient management (i.e., tying the theoretical and potentially passive learning to clinically meaningful, immediate, and active patient management)
Curricular Considerations
As with any curriculum design and development, it is important to take a comprehensive approach and proceed systematically (23). The first question is one of identifying curricular needs. Through consultation of stakeholders (including teachers, practitioners, and learners), it is important to understand which elements of the trainee education can and should be shifted to distance learning, as not all didactics can or should be offered through fully remote platforms. Instead, it is important to focus on high-yield topics, ones that are likely to successfully transition to a virtual platform. Examples include conferences where real-time input is needed either for patient care or learning, such as morbidity and mortality conferences or consensus management and multidisciplinary conferences such as tumor boards or interstitial lung disease conferences. Core program didactics may also transition well to a remote platform. One of the benefits of the synchronous but remote format is that individuals not at that physical conference location can still participate and contribute, and at least some programs have seen evidence of increased conference attendance with this format change (24).
Second, establishing learning outcomes is the next logical step in outcomes-based education, which will lead to a better understanding and organization of the content necessary to achieve those outcomes. Then, with each individual activity, consideration must be given to the educational strategies and educational environment to be used. Content experts can template out the activities within the curriculum as a first pass and then consider collaboration with an educational expert to better define the agreed educational strategies (25). Determine which activity would benefit from utilizing videos, podcasts, blogs, recorded lectures, flipped classrooms, etc., to best facilitate learning. For example, for critical care education, there are a number of online resources from which to obtain curated content so educators can avoid recreating the wheel (26–28). Guides are also available for creating your own brief educational videos (29). Even simulation-based education may be able to be partially adapted to a remote format (30, 31).
Lastly, consider curricular assessment to ensure learners learn the desired content but also for curricular quality control and iterative improvement (32). The first curriculum that educators transition to remote learning may not be seamless, but with appropriate assessment, an early effort can serve as a starting point for subsequent improvement through feedback.
Conclusions
Necessity is the mother of invention, and COVID-19 certainly will lead many GME programs to try distance learning for the first time. Though using distance learning may be new for some programs, educators should apply familiar best practices for adult learning to any new platform. In particular, in transitioning to a distance-learning curriculum, educators should focus on active-learning techniques rather than passive methods and should foster interaction as much as possible when synchronous techniques are used. The suggestions in this perspective can help avoid some of the technical pitfalls that may be encountered with a transition to a distance-learning platform. Of note, techniques of distance learning applied out of necessity during COVID-19 may prove beneficial for continuation after the pandemic has passed. For sustainability going forward, it will be important for medical educators to cultivate competency with technology used for distance learning and engage in collaboration regarding available content, best practices in educational strategies, and assessment methods for GME curricula.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank Stephanie Nonas, M.D., for the framework used in the chalk talk teaching of mechanical ventilation shown in Figure 1.
Footnotes
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Chatterjee S, Seam N. Web-based learning. In: Kritek P, Richards JB, editors. Medical education in pulmonary, critical care, and sleep medicine. 1st ed. Cham, Switzerland: Springer; 2019. pp. 255–269. [Google Scholar]
- 2.Wittich CM, Agrawal A, Cook DA, Halvorsen AJ, Mandrekar JN, Chaudhry S, et al. E-learning in graduate medical education: survey of residency program directors. BMC Med Educ. 2017;17:114. doi: 10.1186/s12909-017-0953-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Internet-based learning in the health professions: a meta-analysis. JAMA. 2008;300:1181–1196. doi: 10.1001/jama.300.10.1181. [DOI] [PubMed] [Google Scholar]
- 4.Burnette K, Ramundo M, Stevenson M, Beeson MS. Evaluation of a web-based asynchronous pediatric emergency medicine learning tool for residents and medical students. Acad Emerg Med. 2009;16:S46–S50. doi: 10.1111/j.1553-2712.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- 5.Estes M, Gopal P, Siegelman JN, Bailitz J, Gottlieb M. Individualized interactive instruction: a guide to best practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2019;20:363–368. doi: 10.5811/westjem.2018.12.40059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adamson R, Billings M, Coruh B, Morris A, Parsons E. Medical education during COVID: how to make it work online. 2020 [accessed 2020 Apr 17]. Available from: https://www.thoracic.org/members/assemblies/sections/me/webinar/medical_education_during_covid.php.
- 7.He S, Lai D, Mott S, Little A, Grock A, Haas MRC, et al. Remote e-work and distance learning for academic medicine: best practices and opportunities for the future. J Grad Med Educ. 2020;12:256–263. doi: 10.4300/JGME-D-20-00242.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelm DJ, Niven AS. Teaching in the classroom: small groups. In: Kritek P, Richards JB, editors. Medical education in pulmonary, critical care, and sleep medicine. 1st ed. Cham, Switzerland: Springer; 2019. pp. 107–123. [Google Scholar]
- 9.Robins L, Garza A. COVID-19 teaching resources. 2020 [accessed 2020 Apr 2]. Available from: https://clime.washington.edu/covid19-resources-1.
- 10.Luks AM, Stack SW. Teaching in the classroom: large groups. In: Kritek P, Richards JB, editors. Medical education in pulmonary, critical care, and sleep medicine. 1st ed. Cham, Switzerland: Springer; 2019. pp. 83–106. [Google Scholar]
- 11.Premkumar K, Coupal C. Rules of engagement-12 tips for successful use of “clickers” in the classroom. Med Teach. 2008;30:146–149. doi: 10.1080/01421590801965111. [DOI] [PubMed] [Google Scholar]
- 12.Lenz PH, McCallister JW, Luks AM, Le TT, Fessler HE. Practical strategies for effective lectures. Ann Am Thorac Soc. 2015;12:561–566. doi: 10.1513/AnnalsATS.201501-024AR. [DOI] [PubMed] [Google Scholar]
- 13.Jordan J, Jalali A, Clarke S, Dyne P, Spector T, Coates W. Asynchronous vs didactic education: it’s too early to throw in the towel on tradition. BMC Med Educ. 2013;13:105. doi: 10.1186/1472-6920-13-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lew EK, Nordquist EK. Asynchronous learning: student utilization out of sync with their preference. Med Educ Online. 2016;21:30587. doi: 10.3402/meo.v21.30587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kraut AS, Omron R, Caretta-Weyer H, Jordan J, Manthey D, Wolf SJ, et al. The flipped classroom: A critical appraisal. West J Emerg Med. 2019;20:527–536. doi: 10.5811/westjem.2019.2.40979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yilmaz Y, Zaver F, Thomas AA, Comp G, Chan T, Mott S, et al. Academic Life in Emergency Medicine; 2020. Teaching in the age of COVID-19: real-time video conferencing. [accessed 2020 Mar 27]. Available from: https://www.aliem.com/teaching-age-covid19-real-time-video-conferencing. [Google Scholar]
- 17.Tibyampansha D, Ibrahim G, Kapanda G, Tarimo C, Minja A, Kulanga A, et al. Implementation of a learning management system for medical students: a case study of Kilimanjaro Christian Medical University College. MedEdPublish. 2017;6:1–16. doi: 10.15694/mep.2017.000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freire LL, Arezes PM, Campos JC. A literature review about usability evaluation methods for e-learning platforms. Work. 2012;41:1038–1044. doi: 10.3233/WOR-2012-0281-1038. [DOI] [PubMed] [Google Scholar]
- 19.Chu A, Biancarelli D, Drainoni ML, Liu JH, Schneider JI, Sullivan R, et al. Usability of learning moment: features of an E-learning tool that maximize adoption by students. West J Emerg Med. 2019;21:78–84. doi: 10.5811/westjem.2019.6.42657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Costley J. The effects of instructor control on critical thinking and social presence: variations within three online asynchronous learning environments. J Educ Online. 2016;13:109–171. [Google Scholar]
- 21.Reis R. Ten best practices for teaching online. [accessed 2020 Apr 2]. Available from: https://tomprof.stanford.edu/posting/1091.
- 22.NYU School of Medicine Educator Community. Special edition on online teaching and learning. 2020 [accessed 2020 Apr 9]. Available from: https://us7.campaign-archive.com/?u=a2d63cfc8309350d1ea6d5411&id=1e232d41ab.
- 23.Harden RM. AMEE Guide No. 21: curriculum mapping: a tool for transparent and authentic teaching and learning. Med Teach. 2001;23:123–137. doi: 10.1080/01421590120036547. [DOI] [PubMed] [Google Scholar]
- 24.Coruh B. Flattening the curve: minimizing the impact of COVID-19 on a pulmonary and critical care medicine fellowship training program. ATS Scholar. 2020;1:110–118. doi: 10.34197/ats-scholar.2020-0047PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laidlaw JM, Harden RM, Robertson LJ, Anne Hesketh E. The design of distance-learning programmes and the role of content experts in their production. Med Teach. 2003;25:182–187. doi: 10.1080/0142159031000092599. [DOI] [PubMed] [Google Scholar]
- 26.Kleinpell R, Ely EW, Williams G, Liolios A, Ward N, Tisherman SA. Web-based resources for critical care education. Crit Care Med. 2011;39:541–553. doi: 10.1097/CCM.0b013e318206b5b5. [DOI] [PubMed] [Google Scholar]
- 27.Wolbrink TA, Burns JP. Internet-based learning and applications for critical care medicine. J Intensive Care Med. 2012;27:322–332. doi: 10.1177/0885066611429539. [DOI] [PubMed] [Google Scholar]
- 28.Wolbrink TA, Rubin L, Burns JP, Markovitz B. The top ten websites in critical care medicine education today. J Intensive Care Med. 2019;34:3–16. doi: 10.1177/0885066618759287. [DOI] [PubMed] [Google Scholar]
- 29.Lipomi DJ. Video for active and remote learning. Trends Chem. 2020;2:483–485. doi: 10.1016/j.trechm.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Torres A, Domańska-Glonek E, Dzikowski W, Korulczyk J, Torres K. Transition to online is possible: solution for simulation-based teaching during the COVID-19 pandemic. Med Educ. doi: 10.1111/medu.14245. [online ahead of print] 17 May 2020; DOI: 10.1111/medu.14245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hannon P, Lappe K, Griffin C, Roussel D, Colbert-Getz J. An objective structured clinical examination: from examination room to Zoom breakout room. Med Educ. doi: 10.1111/medu.14241. [online ahead of print] 16 May 2020; DOI: 10.1111/medu.14241. [DOI] [PubMed] [Google Scholar]
- 32.Lindeman BM, Lipsett PA. Step 6: evaluation and feedback. In: Kern DE, Thomas PA, Hughes MT, Chen BY, editors. Curriculum development for medical education: a six-step approach. 3rd ed. Baltimore, MD: Springer; 2015. pp. 122–157. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.