Abstract
Some healthcare providers work with gender expansive youth, and preliminary evidence notes that many of these youth do not disclose their gender identity to all of their healthcare providers. No previous research focused on youth has explored gender identity disclosure to healthcare providers, nor linked youth disclosure to negative mental health outcomes (e.g., symptoms of depression). Data were drawn from the LGBTQ National Teen Survey in order to test the relationship between gender identity disclosure, symptoms of depression, and self-esteem among 5,637 13- to 17-year old (Mage = 15.6) participants who identified as transgender boys, transgender girls, non-binary youth who were assigned female at birth (AFAB), or assigned male non-binary youth who were assigned male at birth (AMAB). Transgender boys reported the highest symptoms of depression and the lowest levels of self-esteem in comparison to other groups. Among the full sample, 66.8% had not disclosed their gender identity healthcare providers—non-binary AMAB youth were least likely to disclose (77.6%). Symptoms of depression were the highest and self-esteem was the lowest for transgender boys with mixed levels of disclosure. Transgender girls reported the lowest symptoms of depression – these youth had also disclosed their identities the most. Findings suggest that mixed disclosure to healthcare providers is problematic for gender expansive youth, especially transgender boys. Findings suggest a need to better prepare health professionals to understand not all gender expansive youth may feel comfortable disclosing their gender identities in medical contexts. Future research should explore gender affirmative healthcare as a potential protective factor in combatting negative mental health outcomes.
Keywords: Gender identity, transgender, non-binary, healthcare
Gender expansive (e.g., transgender, non-binary) youth are consistently faced with the decision of whether or not to disclose their gender identity to people within their lives (Savin-Williams & Dubé, 1998). As it relates to their healthcare, gender expansive youth must decide if sharing their gender identity with their provider (e.g., pediatricians, therapists, social workers, psychologists) will provide them with gender identity-related support (e.g., potentially obtaining hormones or gender affirmation surgery). Consequently, these decisions to disclose or not to disclose may be linked to gender expansive mental health outcomes. A dearth of scholarship has explored gender expansive youth mental health (e.g., symptoms of depression) in terms of gender identity disclosure to healthcare providers. There is, however, limited literature that examines mental health outcomes as they exist amongst gender expansive subgroups (For an exception, Pflum, et al., 2015).
Gender Minority Stress
Scholarship focused on gender identity and mental health is oftentimes situated within the context of minority stress. The minority stress model (Meyer, 2003) was developed to focus on the potential negative life outcomes and adverse experiences that are associated with cisgender sexual minority individuals. Minority stress is explained as chronic stress associated with stigmatization, discrimination, and socio-cultural pressures (Meyer, 2003) experienced by sexual minority and gender expansive people. Another model that explains the health of gender minorities, in particular, is the gender minority stress and resilience (GMSR) model (Hendricks & Testa, 2012; Testa et al., 2015). This model draws from Meyer’s minority stress model (Meyer, 1995, 2003) and explores the ways in which external (i.e., distal) and internal (i.e., proximal) stressors related to gender expansive identity can impact the mental health and well-being of gender expansive people (Hendricks & Testa, 2012; Testa et al., 2017). Specifically, the GMSR model proposes that chronic stress can result from such external processes such as gender minority-based victimization, rejection, discrimination, and identity non-affirmation (Hendricks & Testa, 2012; Testa et al., 2015). Gender minority-based victimization involves any act (e.g., verbal, physical) committed against a gender minority individual due to their gender identity or expression. Gender minority-based rejection involves any form of rejection due to the gender identity of an individual. Gender minority-based discrimination involves the hardships of obtaining social services, employment, medical care, or legal representation due to an individual’s gender identity. Last, gender identity non-affirmation describes the refusal of individuals or society to acknowledge an individual’s true gender identity. Hendricks and Testa (2012) convey that these external (i.e. distal) experiences can contribute to internal (i.e., proximal) stress-induced experiences such as negative expectations, internalized transphobia, and non-disclosure of gender identity. Several studies have conveyed that internalized transphobia can be associated with poor coping skills (Mizock & Mueser, 2014) and may compound mental health issues (Breslow et al., 2015). Last, gender identity non-disclosure is the behavior of concealing one’s true gender identity as a means of protection from discrimination and harassment (Hendricks, & Testa, 2012; Testa et al., 2017; Testa et al., 2015).
Minority stress manifests as discrimination and victimization for many gender expansive youth. Relative to their cisgender peers, gender expansive youth report more discrimination, stigmatization, and victimization (i.e., bullying; Boza & Nicholson Perry, 2014; Goldblum et al., 2012), and are at a two- to three-fold greater risk for symptoms of depression (Reisner et al., 2015), anxiety (Reisner et al., 2015), and suicidal ideation (Reisner et al., 2015; Testa et al., 2017). Given these findings, it seems that gender affirmative care by healthcare providers could have significant influence on the mental health outcomes among gender expansive youth (i.e., depression, self-esteem).
Gender Identity Disclosure
Gender expansive youth are now disclosing their gender identities more frequently and at younger ages, due, in part, to the accessibility and importance of social media in everyday life (Bethea & McCollum, 2013; Maguen, Shipherd, Harris, & Welch, 2007). Disclosing to healthcare providers is not always possible for gender expansive youth and in some situations may put a youth in danger or at higher risk for rejection. After all, previous research finds the decision not to disclose gender identity can create stressful experiences (Galupo et al., 2014; Pachankis et al., 2015), such as anxiety about others learning of one’s identity before one is ready to share, decisions concerning whom to disclose, and feeling separated from one’s true identity (Pachankis, 2007). Previous research has also suggested that situations in which gender expansive identity disclosure is received with positivity and support is associated with greater self-acceptance (Pachankis, 2007), self-confidence (Riggle, Rostosky, McCants, & Pascale-Hague, 2011), and better mental health outcomes (Strain & Shuff, 2010). These distinctions, however, do not ignore the fact that “coming out is a socially complex process that is mitigated by too many contextual factors to be understood linearly or moralistically” (Klein et al., 2015, p. 324).
Gender expansive individuals experience a combination of negative and positive feelings during the process of identity disclosure (Bethea & McCollum, 2013) which ultimately may lead to non-disclosure— including feeling obligated to disclose and being bothered by the unpredictability of the disclosure process. In positive experiences, individuals may experience a feeling of freedom that results after their gender identity disclosure. In one study, gender expansive individuals reported experiencing internal and/or external stressors when they felt an obligation to disclose their gender identity to their family and friends (Bethea, & McCollum, 2013). Among these gender expansive individuals, one main reason for avoiding disclosure was related to the anticipation of social rejection. Gender expansive individuals reported that despite their preparedness to disclose, they were uncertain about the way in which the recipient would react (Bethea & McCollum, 2013).
Scholarship finds that of the gender expansive individuals who seek treatment for healthcare and mental health-related issues, not all choose not to disclose their gender identity to healthcare providers, in part due to the anticipation of transphobic rejection (Rossman, Salamanca, & Macapagal, 2017). Other youth do not disclose because of the dangers associated with non-supportive social networks (Mills-Koonce, Rehder, & McCurdy, 2018; Pflum, Testa, Balsam, Goldblum, Bongar, 2015); thus, disclosure simply may not be an option for some youth. Some studies have found that gender expansive individuals experience gender identity-based discrimination by health care providers (Buxton, 2006; Glynn & van den Berg, 2017; Hines, 2006; Lev 2004; Wren, 2002), which may explain why some of these gender expansive youth continue not to disclose their identities.
Disclosure to healthcare providers.
Previous studies note several themes with regard to negative experiences of gender identity disclosures to healthcare providers. Specifically, 21% of gender expansive patients described experiencing some form of discrimination that included micro-aggressions (Lambda Legal, 2010) including outright refusal of treatment (Lambda Legal, 2010; Poteat et al., 2013; Rossman, Salamanca, & Macapagal, 2017). In their study that explored gender expansive patient’s reasons for non-disclosure to healthcare providers, Rossman and colleagues (2017) identified three main themes: Healthcare providers’ factors in non-disclosure, patients’ resistance to disclosure, and patients’ beliefs regarding the connection between their gender identity and their healthcare needs (Rossman, Salamanca, & Macapagal, 2017). Some gender expansive individuals have described the disclosure of a gender expansive identity to a healthcare provider as a difficult experience (Rossman, Salamanca, & Macapagal, 2017). If gender expansive youth are seeking puberty-blocking medication or hormones but doctors are not practicing gender affirmative care, there may be miscommunication and subsequently a lack of gender expansive-inclusive care.
Current Study
We sought to explore gender identity disclosure to healthcare providers as a means to understand whether there are connections between (non-)disclosure and symptoms of depression and self-esteem among gender expansive subgroups. No previous scholarship has examined the potential associations between disclosure to healthcare providers and negative mental health outcomes. The present study addresses three questions to build upon current gender expansive literature: 1) Do symptoms of depression and self-esteem differ by gender identity?; 2) Does gender identity disclosure to health care providers differ by gender expansive identity?; and 3) Do symptoms of depression and self-esteem differ by gender identity disclosure to health care providers?
Method
Study Design and Participant Recruitment
We utilized data from the LGBTQ National Teen Survey, which was specifically designed to advance the understanding of victimization, health behaviors, and family relationships of LGBTQ adolescents. Data were collected in partnership with the Human Rights Campaign (HRC) between April and December 2017. All respondents were English-speaking, identified as LGBTQ, 13–17 years of age, and resided in the United States at the time of the survey.
LGBTQ adolescents were invited to participate in an anonymous, online, self-report survey hosted by the survey website Qualtrics.com. The online survey platform prevented bots from taking the survey, and the authors employed multiple data cleaning measures such as the identification and deletion of mischievous responders (see Watson, Wheldon, & Puhl, 2019 for an overview of the survey process), Participants were recruited through social media, along with HRC’s wide-reaching network of community partners. Specifically, the HRC posted Facebook messages and Twitter messages with a short message and link to the Qualtrics survey. Some advertisements also included photos of diverse young teens. HRC partner organizations (e.g., Youth Link, Trevor Project, Advocates for Youth) helped disseminate the survey link to their networks via e-mail or direct communication. For their participation, respondents were given the option to enter a drawing for one of 10 Amazon.com gift cards, and all participants were offered HRC wristbands. All study procedures were approved by the University of Connecticut Institutional Review Board protocol #16–809.
Sample
This project utilized data from a larger sample of 17,112 (M = 15.57, SD = 1.27) sexual and/or gender minority 13 to 17-year-old youth across the United States who completed the LGBTQ National Teen Survey. Overall, 5,637 (33%) teens indicated they were transgender. Additionally, 2,396 (14%) of the sample chose “non-binary” as their gender identity. To categorize gender minority youth, we used a combination of the sex assigned at birth and current gender identity information (see Measures below). Only participants with valid responses on survey questions were included within our analysis (n = 3624).
Respondents represented diverse subgroups of LGBTQ adolescents from all 50 states across the US. The ethnic/racial composition of our sample of 3,624 Gender expansive youth was 68% White (n = 2461), 3.1% Black (n = 111), 0.6% Native American (n = 22), 2.9% Asian American (n = 106), 8.1% Hispanic/Latino (n = 294), 15.5% Bi/multiracial (n = 560), and 1.9% of participants (n = 67) indicated another race that was not listed.
Measures
The online survey created for this study assessed the following topics: sex, gender identity, gender identity disclosure (e.g., being “out” to various contexts), symptoms of depression, and levels of self-esteem.
Sex assigned at birth.
Participants were asked, “What sex were you assigned at birth?” Response options were “male” and “female”.
Gender identity.
Given the growing consideration for multiple gender identities (Hendricks & Testa, 2012; Carroll, Gilroy, & Ryan, 2002; Eyler, 2007; Saeed, Mughal, Farooq, 2017) we asked participants to choose among several different gender identity options. Thus, participants were asked, “What is your current gender identity”. Response options included boy, girl, trans boy, trans girl, non-binary, genderqueer/gender non-conforming, and different identity, with a write-in response. For the purposes of this study, participants whose sex assigned at birth and gender identities were coincident were coded as cisgender. Youth who wrote in responses to this item were back-coded when appropriate (e.g., if a youth wrote in “trans” or “transgender” they were categorized with their respective gender identity category. Youth who reported a binary gender identity that was different from from their sex assigned at birth were coded as transgender. Participants who identified a non-binary gender identity were coded in respect to their sex assigned at birth: non-binary assigned male at birth (AMAB) and non-binary assigned female at birth (AFAB).
Degree of disclosure (outness).
Studies indicate greater vulnerability for victimization when gender expansive youth are out (D’Augelli, Grossman, Starks, 2008; Russell et al., 2014), therefore, identity disclosure to healthcare providers were assessed by a scale adapted from the Outness Inventory Scale (OIS; Mohr & Fassinger, 2000). Questions asked, “For each of the following groups, how many people currently do you think know of your transgender or non-binary identity?” Respondents were able to report the degree of outness to healthcare providers, which included: None (0), A few (1), Some (2), Most (3), and All (4). In addition, respondents could choose an option that indicated “Does not apply to me”. A total of 396 participants chose this option. The OIS has demonstrated good internal consistency and was positively correlated with identification among LGBT communities (Mohr & Fassinger, 2000). Though the original scale included 12 contexts of disclosure (i.e., family members/parents, siblings, grandparents and extended family, LGBTQ friends, non-LGBTQ friends, classmates, co-workers, teachers and adults at school, athletic coaches, religious community, new acquaintances, and doctors/other healthcare providers), this project included three contexts in particular: “family members/parents”, “LGBTQ friends”, and “doctors and other health care providers”.
Depression.
The measure for symptoms of depression was adapted from Kutcher’s Adolescent Depression Scale. The 10-items used to measure symptoms of depression include regularity of “Low mood, sadness, feeling down,” “Irritability,” “Sleep difficulties,” “Decreased interest in activities,” “Feelings of worthlessness,” “Feeling tired or having low energy,” “Difficulty concentrating”, “Loss of interest in previously enjoyed activities,” “Feeling worried,” as well as “Physical symptoms of worry” (i.e., headaches, nausea, restlessness). The rating scale included the time-frame (0) Hardly Ever, (1) Much of the Time, (2) Most of the Time, and (3) All of the Time. The reported scores will represent the mean symptoms of depression. In the current sample, the coefficient alpha was .90.
Self-Esteem.
The measure for self-esteem was modified from the Rosenberg Self-Esteem Scale (Rosenberg, 1989). This modified 10-item scale asked participants to rate their agreement with statements such as “I feel that I am a person of worth, at least on an equal plane as others,” “All in all, I am inclined to feel that I am a failure,” “I am able to do things as well as most other people,” and “I take a positive attitude towards myself.” Respondents rated their agreement with positive or negative statements using a 4-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree). Higher scores reflected higher levels of self-esteem. The mean reported self-esteem scores give an estimate level of self-esteem. In the current sample, the Cronbach’s alpha was .91.
Plan of Analysis
Analyses were conducted in SPSS v15. Data were analyzed for missing values and outliers—in this paper we used data from participants who were not missing on all study variables. Across all variables, missingness ranged from 6.1% to 12.8%. Nearly all (92%) youth without full responses to every survey item had terminated the survey early; most of these early terminations only filled out the demographic portion of the survey. Our final sample (N = 7050) of LGBTQ and of gender expansive (N = 3624) youth is representative of those youth who provided valid responses on all study variables. We first used ANOVAs to distinguish whether or not cisgender youth differed from gender expansive youth in levels depression and self-esteem. We then used MANCOVAs, adjusted for age and two contexts of disclosure (i.e., out to family members/parents, out to LGBTQ friends), to model the association between disclosure to health care providers and depression/self-esteem.
Results
The sample demographics are reported in Table 1. On average, youth were 15.57 (SD = 1.27) years old. Nine-hundred and three (24.9%) youth were transgender boys, 122 (3.4%) transgender girls, 237 (6.5%) non-binary AMAB, and 2362 (65.2%) non-binary AFAB youth. Additionally, 22.0% (n = 2,335) youth identified as cisgender males and 44.5% (n = 4,715) as cisgender girls. Table 1 displays the samples’ demographic information by gender identity.
Table 1.
Sample Demographic Characteristics by Gender Identity
| Full Sample | Cisgender boy | Cisgender girl | Transgender boy | Transgender girl | Non-binary AFAB* | Non-binary AMAB* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Heterosexual | 279 | 1.6 | 0 | 0.0 | 0 | 0.0 | 157 | 10.5 | 31 | 16.8 | 74 | 2.1 | 17 | 3.6 |
| Gay/Lesbian | 6401 | 37.4 | 2875 | 70.5 | 2254 | 30.5 | 248 | 17.9 | 33 | 17.8 | 772 | 21.6 | 219 | 46.1 |
| Bisexual | 5970 | 34.9 | 1018 | 25 | 3569 | 48.3 | 388 | 27.6 | 56 | 30.3 | 836 | 23.4 | 103 | 21.7 |
| Pansexual | 2256 | 13.2 | 82 | 2.0 | 761 | 10.3 | 341 | 24.9 | 37 | 20.0 | 968 | 27.1 | 67 | 14.1 |
| Queer | 699 | 4.1 | 27 | 0.7 | 210 | 2.8 | 84 | 6.5 | 8 | 4.3 | 345 | 9.7 | 25 | 5.3 |
| Asexual | 725 | 4.2 | 28 | 0.7 | 278 | 3.8 | 80 | 5.6 | 8 | 4.3 | 315 | 8.8 | 16 | 3.4 |
| Questioning | 424 | 2.5 | 29 | 0.7 | 205 | 2.8 | 60 | 3.8 | 7 | 3.8 | 110 | 3.1 | 13 | 2.7 |
| Other | 358 | 2.1 | 20 | 0.5 | 119 | 1.6 | 46 | 3.1 | 5 | 2.7 | 153 | 4.3 | 15 | 3.2 |
| Race/ethnicity | ||||||||||||||
| White | 10225 | 61.9 | 2279 | 58.2 | 4376 | 61.4 | 932 | 68.1 | 120 | 66.7 | 2254 | 64.7 | 264 | 58.8 |
| Black | 952 | 5.8 | 273 | 7.0 | 473 | 6.6 | 47 | 3.4 | 9 | 5.0 | 124 | 3.6 | 26 | 5.8 |
| Hispanic/Latino | 1877 | 11.4 | 556 | 14.2 | 828 | 11.6 | 115 | 8.4 | 13 | 7.2 | 316 | 9.1 | 49 | 10.9 |
| Asian | 677 | 4.1 | 182 | 4.6 | 324 | 4.5 | 36 | 2.6 | 8 | 4.4 | 110 | 3.2 | 17 | 3.8 |
| Native American | 95 | 0.6 | 24 | 0.6 | 29 | 0.4 | 13 | 1.0 | 1 | 0.6 | 21 | 0.6 | 7 | 1.6 |
| Multiracial | 2360 | 14.3 | 519 | 13.3 | 958 | 13.4 | 192 | 14.0 | 27 | 15.0 | 589 | 16.9 | 75 | 16.7 |
| Other | 342 | 2.1 | 83 | 2.1 | 144 | 2.0 | 33 | 2.4 | 2 | 1.1 | 69 | 2.0 | 11 | 2.4 |
| Age | ||||||||||||||
| 13 | 1284 | 7.5 | 146 | 3.6 | 596 | 8.1 | 133 | 9.5 | 14 | 7.6 | 370 | 10.4 | 25 | 5.3 |
| 14 | 2542 | 14.9 | 394 | 9.7 | 1210 | 16.4 | 219 | 15.5 | 24 | 13.0 | 634 | 17.7 | 61 | 12.8 |
| 15 | 3594 | 21.0 | 841 | 20.6 | 1540 | 20.8 | 321 | 22.9 | 41 | 22.2 | 766 | 21.4 | 85 | 17.9 |
| 16 | 4481 | 26.2 | 1213 | 29.7 | 1885 | 25.5 | 350 | 24.9 | 51 | 27.6 | 853 | 23.9 | 129 | 27.2 |
| 17 | 5211 | 30.5 | 1485 | 36.4 | 2165 | 29.3 | 381 | 27.1 | 55 | 29.7 | 950 | 26.6 | 175 | 36.8 |
Note AMAB=Assigned male at birth; AFAB=Assigned female at birth
Our first research question involved determining whether there were differences in mental health outcomes (i.e., symptoms of depression and self-esteem) between cisgender and gender expansive youth. We found a difference in symptoms of depression [F (1, 10121) = 742.93, p = .001, μ2 = .068] and self-esteem [F (1, 10121) = 808.83, p < .001, μ2 = .074] when comparing cisgender youth to gender expansive youth. Tukey post hoc analyses indicated that symptoms of depression among gender expansive youth (M = 16.003 SD = 7.30) were higher (p < .05) compared to cisgender youth (M = 11.91, SD = 7.25). Similarly, the mean score for level of self-esteem among gender expansive youth (M = 22.63, SD = 9.07) was different, and consequently much lower (p < .05), than levels of self-esteem among cisgender youth (M = 28.33, SD = 9.95).
Next, we tested whether these differences held across groups of gender expansive youth. Within-group differences were found when comparing gender expansive symptoms of depression [F (3, 3142) = 15.10, p < .001, μ2 = .014] and self-esteem [F (3, 3142) = 16.28, p < .001, μ2 = .015]. Specifically, Tukey post hoc analyses indicated that symptoms of depression among transgender boys were higher (M = 16.97, SD = 7.51, p < .05) compared to all other gender expansive subgroups (see Table 2). Additionally, there were differences in depressive symptoms between non-binary AFAB youth (M = 16.06, SD = 7.09) and all other subgroups (p < .05), as well as between non-binary AMAB youth (M = 13.43, SD = 7.37) and transgender boys (M =16.97, SD = 7.51) and non-binary AFAB youth (M = 16.06, SD = 7.10) at the p < .001 level.
Table 2.
Mean levels of symptoms of depression and self-esteem by gender identity
| Outcome | Gender Subgroup | N | M | SD |
|---|---|---|---|---|
| Depression | Cisgender boy | 2133 | 10.07* | 6.92 |
| Cisgender girl | 4470 | 12.76* | 7.23 | |
| Transgender boy | 885 | 16.97* | 7.51 | |
| Transgender girl | 118 | 13.58* | 7.85 | |
| Non-binary AFAB | 2350 | 16.06* | 7.10 | |
| Non-binary AMAB | 243 | 13.43* | 7.37 | |
| Total | 10199 | 13.35 | 7.53 | |
| Self-Esteem | Cisgender boy | 2133 | 30.89* | 10.35 |
| Cisgender girl | 4470 | 27.10* | 9.48 | |
| Transgender boy | 885 | 21.73* | 9.48 | |
| Transgender girl | 118 | 25.24* | 10.28 | |
| Non-binary AFAB | 2350 | 22.45* | 8.77 | |
| Non-binary AMAB | 243 | 26.31* | 9.70 | |
| Total | 10199 | 26.32 | 10.01 | |
Significant at the .05 level.
Transgender boys reported lower levels of self-esteem (M = 21.73, SD = 9.21), compared to transgender girls (M = 25.24, SD = 10.28, p < .05) and non-binary AMAB youth (M = 26.31, SD = 9.70, p < .001). Non-binary AFAB youth (M = 22.45, SD = 8.77) also reported lower self-esteem than transgender girls (M = 25.24, SD = 10.28, p < .05) and non-binary AMAB youth (M = 26.31, SD = 9.70, p < .001).
Our second research question asked whether disclosure of gender identity to health professionals differed between subgroups of gender expansive youth. Table 3 presents these findings. We found that disclosure to healthcare providers significantly differed by gender identity, [F (3, 3142) = 44.50, p < .001, μ2 = .041]. Tukey Post hoc comparisons indicated that transgender girls (M = 1.35, SD = 1.61) disclosed their gender expansive identity to healthcare professionals more often than non-binary AMAB (M = .44, SD = .65) and AFAB (M = .65, SD = 1.23) youth, while only disclosing marginally more than transgender boys (M = 1.22, SD = 1.52). Specifically, transgender girls disclosed most, and non-binary AMAB youth disclosed their gender identities least to healthcare providers.
Table 3.
Sample Disclosure Level by Gender Identity
| Disclosure to Healthcare Providers | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender Identity | None | A few | Some | Most | All | Total | |||||||
| n | % | n | % | n | % | n | % | n | % | n | M | SD | |
| Transgender Boy | 463 | 51.3a | 137 | 15.2ab | 65 | 7.2a | 105 | 11.6abc | 133 | 14.7ab | 903 | 1.23 | 1.52 |
| Transgender Girl | 65 | 53.3b | 14 | 11.5b | 7 | 5.7 | 14 | 11.5c | 22 | 18.0b | 122 | 1.30 | 1.61 |
| Non-binary AFAB | 1709 | 72.4ab | 266 | 11.3a | 95 | 4.0a | 124 | 5.2ab | 168 | 7.1a | 2362 | .56 | 1.19 |
| Non-binary AMAB | 184 | 77.6ab | 15 | 6.3a | 12 | 5.1 | 10 | 4.2a | 16 | 6.8a | 237 | .64 | 1.22 |
| Total | 2421 | 66.8 | 432 | 11.9 | 179 | 4.9 | 253 | 7.0 | 339 | 9.4 | 3624 | .80 | 1.34 |
Note. Each subscript letter (a,b,c) denotes where column (e.g., none) proportions significantly differ from each other at the p<.05 level.
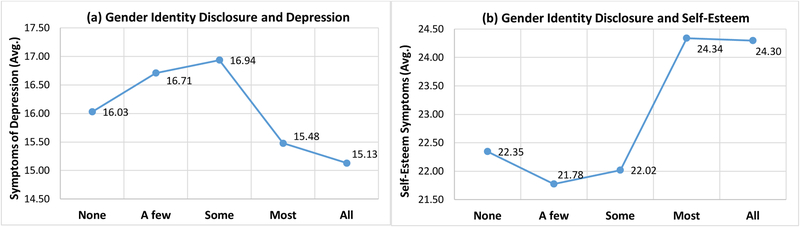
Our third research goal was to examine the correlation between gender identity disclosure to healthcare providers and mental health symptoms (depression, self-esteem) among gender expansive youth. These results are presented in Figure 1. There was a significant difference between disclosure and depressive symptoms as determined by a MANCOVA (adjusted for age, disclosure to family members/parents, and LGBTQ friends), [F (4, 3142) = 2.87, p < .05, μ2 = .004]. Similarly, differences in self-esteem and disclosure were also significant [F (4, 3142) = 6.07, p < .001, μ2 = .008]. Tukey post hoc tests revealed that gender expansive symptoms of depression were statistically higher (p < .05) for disclosure to “A few” healthcare providers (M = 16.71, SD = 7.01) when compared to disclosure to “All” healthcare providers (M = 15.13, SD = 7.68). Symptoms of depression were highest among gender expansive youth who disclosed to “Some” healthcare providers (M = 16.94, SD = 7.66), and symptoms of depression were significantly lowest for youth who had disclosed to “All” or “Most” of their healthcare providers (M = 15.13, SD = 7.68; M = 15.48, SD = 7.68, respectively) when compared to “Some”. Results were similar for self-esteem and disclosure: Tukey post hoc analyses indicated self-esteem was statistically significantly higher (p < .01) for disclosure to “All” healthcare providers (M = 24.29, SD = 10.28) compared to disclosure to “None” (M = 22.35, SD = 8.81) and “A few” (M = 21.78, SD = 8.77).
Figure 1.
Associations between gender identity disclosure to health professionals and symptoms of depression (a) and self-esteem (b) among gender expansive youth.
Discussion
Gender expansive adolescents represent a unique and distinctly heterogeneous population of youth within the United States who are not well understood by healthcare providers or the scientific community. Our scholarship continues to bridge the gap between research and clinical practice for gender expansive youth. Before exploring within-group differences among gender expansive youth, we compared symptoms of depression and levels of self-esteem between gender expansive and cisgender youth. We found that gender expansive youth faced differences in mental health across measures of symptoms of depression and self-esteem when compared to cisgender youth. These findings are supported by previous research that also conveys the existence of greater mental health disparities between gender expansive and cisgender youth (Benotsch et al., 2013; Cochran & Cauce, 2006; Day et al., 2017; Hughes & Eliason, 2002; Lombardi, 2010; Nemoto et al., 2004; Nuttbrock et al., 2014; Peacock, Andrinopoulos, & Hembling, 2015; Reisner et al., 2015; Reisner & Murchison, 2016; Santos et al., 2014; Wolf & Dew, 2012). These findings enhance our growing knowledge of negative mental health outcomes faced by gender expansive youth by utilizing large-scale population comparisons. The significant risks highlighted in these findings underscore the need for further attention to gender affirmative healthcare protocols for doctors, nurses, and therapists alike.
Within-group differences of symptoms of depression and levels of self-esteem were also meaningful when comparing these measures among gender identity subgroups. Specifically, transgender boys reported the highest symptoms of depression and the lowest levels of self-esteem, and transgender girls reported the lowest symptoms of depression when compared to all other gender expansive subgroups. These findings are consistent with previous studies that identified transgender boys as exhibiting more negative mental health outcomes among gender expansive youth (Veale et al., 2017).
Our review of gender identity disclosure to healthcare providers among gender expansive youth also indicated subgroup and age-related trends. Among our sample, two-thirds of gender expansive youth had not disclosed their gender identity to healthcare providers, and less than one-tenth had disclosed to all of their healthcare providers. Non-disclosure to healthcare providers was highest among non-binary AMAB youth, with non-binary AFAB youth close behind. Transgender boys reported highest levels of mixed gender identity disclosure (out to some, but not all) to healthcare providers when compared to gender expansive subgroups, and transgender girls had the highest levels of overall disclosure to healthcare providers.
Non-disclosure amongst non-binary youth has been identified as problematic (Veale et al., 2017). Considering the GMSR model (Hendricks, & Testa 2012; Testa et al., 2015), higher levels of foregoing gender identity disclosure to healthcare providers and notably worse mental health outcomes among non-binary youth may be due to the compounded stress and stigma of not conforming to traditional (Western) binary gender role categories (Skidmore et al., 2006; Veale et al., 2017). This is not to say that some gender expansive youth do not benefit from concealing their gender identity within their social environments. For some youth, their safety may be compromised after disclosing their identity. For these youth, to conceal is to remain safe.
Age-related comparisons: Gender identity disclosure
When we separated disclosure to healthcare providers by age, we found that younger adolescents (13- and 14-year olds) had disclosed their gender identities to fewer healthcare providers than their older gender expansive peers. These findings may indicate that an increased level of maturity, confidence, and/or positive life experiences relative to gender expansive age are necessary for increased disclosure to healthcare providers. Our findings suggested that older gender expansive youth disclosed more to healthcare providers than their younger-aged peers. One caveat within these findings was among transgender girls’ disclosure to healthcare providers compared to other gender expansive subgroups. While transgender girls exhibit the highest levels of disclosure to healthcare providers, they are the only subgroup to display decreasing rates of full disclosure when disclosure is isolated by age. This suggests that transgender girls are disclosing less to healthcare providers as they get older. This evidence is supported by previous research that suggests that transgender youth, particularly transgender girls, experience increased anxiety and distress as they age (Edwards-Leeper et al., 2017), and thus may be less apt to disclose their gender identity. Further research is needed to explore the possibility of increased negative life experiences among transgender girls as they get older.
As we examined gender identity disclosure to healthcare providers and symptoms of depression among gender expansive youth, we found that symptoms of depression were highest for mixed disclosure (out to some, but not all), whereas symptoms of depression were lowest for disclosure to all healthcare providers. This suggests a negative relationship between disclosure and symptoms of depression. Similarly, self-esteem was highest for gender expansive youth who disclosed to all, and was lowest for those who had only disclosed their gender identity to a mixed number of healthcare providers. Thus, gender identity disclosure and levels of self-esteem exhibited a positive relationship.
These findings are noteworthy on two fronts: First, while gender identity disclosure among sexual and gender expansive youth has been suggested to contribute to negative mental health outcomes due to stigmatization and discrimination, the management of multiple gender identities for the purpose of selective concealment (GMSR model, Testa et al., 2015) may be compounding gender expansive-related stress (Riggle et al., 2017; Skidmore et al., 2006). Second, the highest symptoms of depression are found among mixed disclosure of gender identity (out to some, but not all) when compared to lower symptoms for non-disclosure and lowest symptoms for disclosure to all healthcare providers. These findings highlight the need for research that examines gender expansive-related stress due to mixed disclosure to healthcare providers.
Previous research and theory (GMSR model) suggests that factors related to gender identity concealment may compound negative mental health outcomes (Breslow, 2015; Hendricks, & Testa, 2012; Mizock & Mueser, 2014; Riggle et al., 2017; Testa et al., 2017; Testa et al., 2015). The findings reported here suggest that mixed disclosure to healthcare providers is specifically related to higher symptoms of depression and lower levels of self-esteem; future research should more fully explore gender expansive identity disclosure and its relationship to gender expansive stress.
Gender identity disclosure amongst gender expansive youth is a process that has no clearly defined protocol to protect against victimization, harassment, or discrimination. It seems however that there are positive attributes to understanding disclosure to healthcare providers. For transgender girls, who exhibit the highest rates of disclosure, sharing their gender identity to healthcare providers may be a successful means of coping with the inherent stress of social pressures on gender expansive youth; whereas for non-binary youth (particularly non-binary AMAB) the prevalence of non-disclosure is the highest among gender subgroups. For those non-binary youth, non-disclosure may be a logical strategy to avoiding increased stigmatization and victimization within a binary gender society. Transgender boys however, whom are exhibiting the highest symptoms of depression and the lowest levels of self-esteem seem to be faring the worst with mixed disclosure to healthcare providers. Our findings suggest that being out to some, but not to all can be problematic for gender expansive youth.
Rossman and colleagues (2017) suggested that anticipated stigma is implicit in the disclosure process and may impact how patients interpret providers’ reactions. Levitt and Ippolito (2014) found that due to environmental limitations (i.e, discrimination, risk of harm), gender expansive individuals significantly compromise their life choices to maintain their friendships, safety, and social standing within their communities. This scholarship is an important exploration into the lived experiences of gender expansive youth, who may eventually seek the services of a healthcare provider for therapy, puberty suppression, or hormone treatments and may benefit from understanding the mental health outcomes associated with gender identity disclosure.
Implications
Over fifteen years ago, the Substance Abuse and Mental Health Services Administration (SAMHSA) released a policy with the aim to make healthcare providers aware of the LGBTQ-specific issues in substance use and mental health treatment (Craft & Mulvey, 2001). This policy underscored the need for healthcare providers to understand the within-group differences, as well as the theoretically-driven mechanisms and moderators of gender expansive mental health outcomes (Stevens, 2012). Our work was conducted in the spirit of better informing recommendations for clinical training and practice towards improved gender expansive healthcare models.
Additionally, there is a noticeable lack of quantitative data exploring gender expansive experiences prior to 2010, due to most large-scale survey measures pursuing specific male-female binary parameters for gender identification (Westbrook & Saperstein, 2015). The limited studies that test gender-identity disparities note important differences. In a recent analysis of gender expansive health-related behaviors, researchers found that gender expansive individuals are at an elevated risk for negative mental health outcomes, with a threefold risk of symptoms of depression and psychiatric disorders (Day et al., 2017; Reisner et al., 2015).
Gender affirmative healthcare relationships within the lives of gender expansive youth may significantly benefit those who are struggling with symptoms of depression and low self-esteem, and who are attempting to manage the stress of gender identity disclosure. Recent studies have demonstrated that positive role models (i.e., teachers, school counselors) may benefit gender expansive youth (Dessell et al., 2017; Heck et al., 2013; Heck et al., 2014; Snapp et al., 2015), so why too couldn’t doctors and clinicians be considered as proponents for positively impacting the lives of gender expansive youth? Gender affirmative support by doctors and therapists may help to ensure a protective effect between gender expansive stress and negative mental health outcomes (i.e., symptoms of depression, low self-esteem).
The framework within which gender expansive youth mental health disparities exist requires vigilance and understanding. Rossman and colleagues (2017) stated that a significant barrier to patient disclosure was healthcare providers simply not asking about their gender identity. The modification of healthcare paperwork to include questions about gender identity status has been underscored as a clear and present need by the Institute of Medicine (Cahill & Makadon, 2014; Graham et al., 2011; Rossman, et al., 2017) and the World Provider Association for Transgender Health (Deutsch et al., 2013; Rossman, et al., 2017) as a means to bridge the gap between clinical knowledge and practice. Additionally, considering the effectiveness of family-based treatment for adolescent symptoms of depression (Wills, Vaccaro, & McNamara, 1992), it is important to understand and account for the ways in which family support can influence the modification of gender affirmative healthcare. The question of how a gender affirmative healthcare system can protect against the negative effects of victimization and internalized transphobia on gender expansive youth has yet to be answered. Based on the non-disclosure rates of gender expansive youth with healthcare providers, stakeholders can continue to invest in fostering an environment inclusive of gender affirmative care.
Limitations
There are multiple factors that make accurate sampling a challenging endeavor when studying gender expansive youth populations. Population-level research within the United States oftentimes lacks reliable data on gender identity. This survey sought to include as many gender expansive respondents as possible. However, due to the recruitment of participants using social media means for a web-based survey, gender expansive individuals with specific characteristics (e.g., internet access, stable housing, and time) may have disproportionally participated in this survey. Thus, our survey measures and means may not reach homeless or transient populations of gender expansive youth—this sample may not completely represent the full-lived experiences of gender expansive youth within the US. Additionally, by utilizing methods of online advertising to gain survey participants, we may have disproportionately attracted responses from specific ethno-racial backgrounds.
There are many variables that may impact gender expansive mental health, and it is important to consider the possibility that certain aspects of self-esteem and depressive symptoms may not be completely due to gender expansive identity. Specifically, gender expansive youth who exhibit high self-esteem may not be exhibiting these symptoms solely due to being out to their healthcare providers. It is certainly possible that gender expansive youth who have supportive relationships with family and friends have the protective factors to ensure higher levels of self-esteem. Conversely, if gender expansive youth have been taught positive coping mechanisms, then they may be more apt to be able to manage gender minority stress and negative life experiences that can contribute to symptoms of depression. A gender expansive young person’s depressive symptoms may not be as a result of the degree to which they are out to their healthcare provider.
Our measure of disclosure to health providers did not specify the type of health care provider or ask whether or not youth have multiple healthcare providers. Though we utilized a question from a validated and widely used scale on disclosure, the wording of this question is a limitation (e.g., an inability to assess whether youth have providers and how many) and should be explored further in subsequent research. Last, youth may have different reasons for disclosure to certain types of health care providers (e.g., primary care physician, mental health counselor, nurse)—future research should disentangle the specific types health care providers to which gender expansive youth may disclose their identities. Last, we found some small effect sizes in our ANOVA and MANCOVA analyses. Specifically, some effect sizes between disclosure to healthcare providers and symptoms of depression and self-esteem among gender expansive youth were weak. Though this indicates there are other factors explaining mental health among gender expansive youth, it is still a contribution that this study is the first analysis on disclosure to healthcare providers and negative mental health outcomes.
Conclusion
While gender expansive youth face high levels of discrimination, stigmatization, and victimization (Boza & Nicholson Perry, 2014; Goldblum et al., 2012), and are at an increased risk for symptoms of depression (Reisner et al., 2015), anxiety (Reisner et al., 2015), and suicidal ideation (Testa et al., 2017) relative to their cisgender peers (Nuttbrock et al., 2014), it is important to consider the protective and exposure factors that are created by gender expansive identity disclosure to healthcare providers. In addressing these concerns, Glynn & van den Berg (2017) called for the modification of the healthcare system to include gender expansive-specific needs. It behooves the clinical and research community to explore the contributing factors (negative and positive) that may influence mental health outcomes of gender expansive youth. It is therefore prudent for healthcare providers to work towards an understanding of gender affirmative treatment to ensure positive outcomes for these youth. Gender expansive youth systematically vary by multiple psychosocial factors (e.g., gender identity, disclosure, and mental health) and should thus be understood by their unique lived experiences, with greater consideration paid to the quality of gender affirming support from healthcare providers.
Public Significance:
In our study, most transgender and non-binary youth had not disclosed their gender identity to healthcare providers. Mixed levels of disclosure to healthcare providers was associated with more depression and lower self-esteem. These findings inform clinicians and policy makers of the need to improve gender-based clinical practices for transgender and non-binary youth.
Acknowledgements:
This research uses data from the LGBTQ National Teen Study, designed by Ryan J. Watson and Rebecca M. Puhl in collaboration with the Human Rights Campaign, and supported by the Office for Vice President of Research at the University of Connecticut. The authors acknowledge the intensive efforts of Ellen Kahn, Gabe Murchison, and Liam Miranda in their support, conceptualization, and management related to the LGBTQ National Teen Study. This work was funded in part by the National Institutes of Drug Abuse grant K01DA047918.
Additional thanks expressed to the Center for the Study of Culture, Health, and Human Development at the University of Connecticut. Particularly, Dr. Charles Super and Dr. Sara Harkness for their guidance with data analysis on this paper.
Contributor Information
Timothy McKay, University of Connecticut.
Ryan J. Watson, University of Connecticut.
References
- Benotsch EG, Zimmerman R, Cathers L, McNulty S, Pierce J, Heck T, Snipes D (2013). Non-medical use of prescription drugs, polysubstance use, and mental health in transgender adults. Drug & Alcohol Dependence, 132(1), 391–394. doi: 10.1016/j.drugalcdep.2013.02.027. [DOI] [PubMed] [Google Scholar]
- Bethea M, & Mccollum E (2013). The disclosure experiences of male-to-female transgender individuals: A systems theory perspective. Journal of Couple & Relationship Therapy. 12(2), 89–112. doi: 10.1080/15332691.2013.779094. [DOI] [Google Scholar]
- Bouman WP, Claes L, Brewin N, Crawford JR, Millet N, Fernandez-Aranda F, & Arcelus J (2017). Transgender and anxiety: A comparative study between transgender people and the general population. International Journal of Transgenderism, 18(1), 16–26. doi: 10.1080/15532739.2016.1258352. [DOI] [Google Scholar]
- Bouman WP, Claes L, Brewin N, Crawford JR, Millet N, Fernandez-Aranda F, & Arcelus J (2017). Transgender and anxiety: A comparative study between transgender people and the general population. International Journal of Transgenderism, 18(1), 16–26. doi: 10.1080/15532739.2016.1258352. [DOI] [Google Scholar]
- Bouman WP, Davey A, Meyer C, Witcomb GL, & Arcelus J (2016). Predictors of psychological well-being among treatment seeking transgender individuals. Sexual and Relationship Therapy, 31(3), 359–375. doi: 10.1080/14681994.2016.1184754. [DOI] [Google Scholar]
- Bowen M (1978). Family therapy in clinical practice. New York: J. Aronson. [Google Scholar]
- Boza C, & Nicholson Perry K (2014). Gender-related victimization, perceived social support, and predictors of depression among transgender Australians. International Journal of Transgenderism, 15(1), 35–52. doi: 10.1080/15532739.2014.890558. [DOI] [Google Scholar]
- Breslow AS, Brewster ME, Velez BL, Wong S, Geiger E, & Soderstrom B (2015). Resilience and collective action: Exploring buffers against minority stress for transgender individuals. Psychology of Sexual Orientation and Gender Diversity, 2(3), 253. doi: 10.1037/sgd0000117. [DOI] [Google Scholar]
- Buxton AP (2006). When a spouse comes out: Impact on the heterosexual partner. Sexual Addiction & Compulsivity, 13(2–3), 317–332. doi: 10.1080/10720160600897599. [DOI] [Google Scholar]
- Cahill S, & Makadon H (2014). Sexual orientation and gender identity data collection in clinical settings and in electronic health records: A key to ending LGBT health disparities. LGBT Health, 1(1), 34–41. doi: 10.1089/lgbt.2013.0001. [DOI] [PubMed] [Google Scholar]
- Carroll L, Gilroy PJ, & Ryan J (2002). Counseling transgendered, transsexual, and gender‐variant clients. Journal of Counseling & Development, 80(2), 131–139. doi: 10.1002/j.1556-6678.2002.tb00175.x. [DOI] [Google Scholar]
- Chen P, & Jacobson KC (2012). Developmental trajectories of substance use from early Adolescence to Young Adulthood: Gender and racial/ethnic differences. Journal of adolescent health, 50(2), 154–163. doi: 10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran BN, & Cauce AM (2006). Characteristics of lesbian, gay, bisexual, and transgender individuals entering substance abuse treatment. Journal of Substance Abuse Treatment, 30(2), 135–146. doi: 10.1016/j.jsat.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Coulter RW, Bersamin M, Russell ST, & Mair C (2017). The effects of gender-and sexuality-based harassment on lesbian, gay, bisexual, and transgender substance use disparities. Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2017.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craft E, Mulvey K (2001). Addressing lesbian, gay, bisexual, and transgender issues from the inside: one federal agency’s approach. American Journal of Public Health, 91, 889–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuadros O, & Berger C (2016). The protective role of friendship quality on the wellbeing of adolescents victimized by peers. Journal of Youth and Adolescence, 45(9), 1877–1888. doi: 10.1007/s10964-016-0504-4. [DOI] [PubMed] [Google Scholar]
- D’Augelli A, Grossman A, Starks M (2008). Gender atypicality and sexual orientation development among lesbian, gay, and bisexual youth: Prevalence, sex differences, and parental responses. Journal of Gay Lesbian Mental Health, 12(1/2), 121–143. doi: 10.1300/J529v12n01_08 [DOI] [Google Scholar]
- Dank M, Lachman P, Zweig JM, & Yahner J (2014). Dating violence experiences of lesbian, gay, bisexual, and transgender youth. Journal of youth and Adolescence, 43(5), 846–857. doi: 10.1007/s10964-013-9975-8. [DOI] [PubMed] [Google Scholar]
- Day JK, Fish JN, Perez-Brumer A, Hatzenbuehler ML, & Russell ST (2017). Transgender youth substance use disparities: results from a population-based sample. Journal of Adolescent Health, 61(6), 729–735. doi: 10.1016/j.jadohealth.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demant D, Hides L, White KM, & Kavanagh DJ (2018). Effects of participation in and connectedness to the LGBT community on substance use involvement of sexual minority young people. Addictive behaviors, 81, 167–174. doi: 10.1016/j.addbeh.2018.01.028. [DOI] [PubMed] [Google Scholar]
- Demant D, Oviedo-Trespalacios O, Carroll JA, Ferris JA, Maier L, Barratt MJ, & Winstock AR (2018). Do people with intersecting identities report more high-risk alcohol use and lifetime substance use?. International Journal of Public Health, 63(5), 621–630. doi: 10.1007/s00038-018-1095-5. [DOI] [PubMed] [Google Scholar]
- De Pedro KT, & Shim-Pelayo H (2018). Prevalence of Substance Use among Lesbian, Gay, Bisexual, and Transgender Youth in Military Families: Findings from the California Healthy Kids Survey. Substance Use & Misuse, 1–5. doi: 10.1080/10826084.2017.1409241. [DOI] [PubMed] [Google Scholar]
- De Pedro KT, Gilreath TD, Jackson C, & Esqueda MC (2017). Substance use among transgender students in California public middle and high schools. Journal of School Health, 87(5), 303–309. doi: 10.1111/josh.12499. [DOI] [PubMed] [Google Scholar]
- Dessel AB, Kulick A, Wernick LJ, & Sullivan D (2017). The importance of teacher support: Differential impacts by gender and sexuality. Journal of Adolescence, 56, 136–144. doi: 10.1016/j.adolescence.2017.02.002. [DOI] [PubMed] [Google Scholar]
- Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, Hall AM, … & Blumer O (2013). Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. Journal of the American Medical Informatics Association, 20(4), 700–703. doi: 10.1136/amiajnl-2012-001472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards-Leeper L, Feldman HA, Lash BR, Shumer DE, & Tishelman AC (2017). Psychological profile of the first sample of transgender youth presenting for medical intervention in a US pediatric gender center. Psychology of Sexual Orientation and Gender Diversity, 4(3), 374. doi: 10.1037/sgd0000239. [DOI] [Google Scholar]
- Eisenberg ME, Gower AL, McMorris BJ, Rider GN, Shea G, & Coleman E (2017). Risk and protective factors in the lives of transgender/gender nonconforming adolescents. Journal of Adolescent Health, 61(4), 521–526. doi: 10.1016/j.jadohealth.2017.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyler AE (2007). Primary medical care of the gender-variant patient. In Ettner R, Monstrey S, & Eyler E (Eds.) Principles of Transgender Medicine and Surgery. Binghamton, NY: Haworth Press, pp. 15–32. [Google Scholar]
- Gage NL (1978). The scientific basis of the art of teaching. New York: Teachers College Press. [Google Scholar]
- Galupo MP, Krum TE, Hagen DB, Gonzalez KA, & Bauerband LA (2014). Disclosure of transgender identity and status in the context of friendship. Journal of LGBT Issues in Counseling, 8(1), 25–42. doi: 10.1080/15538605.2014.853638. [DOI] [Google Scholar]
- Glynn TR, & van den Berg JJ (2017). A Systematic Review of Interventions to Reduce Problematic Substance Use Among Transgender Individuals: A Call to Action. Transgender Health, 2(1), 45–59. doi: 10.1089/trgh.2016.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn TR, Gamarel KE, Kahler CW, Iwamoto M, Operario D, & Nemoto T (2016). The role of gender affirmation in psychological well-being among transgender women. Psychology of Sexual Orientation and Gender Diversity, 3(3), 336. doi: 10.1037/sgd0000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldblum P, Testa RJ, Pflum S, Hendricks ML, Bradford J, & Bongar B (2012). The relationship between gender-based victimization and suicide attempts in transgender people. Provider Psychology: Research and Practice, 43(5), 468. doi: 10.1037/a0029605. [DOI] [Google Scholar]
- Goldblum P, & Espelage DL (Eds.). (2014). Youth Suicide and Bullying: Challenges and strategies for prevention and intervention. Oxford University Press, USA. [Google Scholar]
- Graham R, Berkowitz B, Blum R, Bockting W, Bradford J, de Vries B, & Makadon H (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: Institute of Medicine. [Google Scholar]
- Hackimer L, & Proctor SL (2015). Considering the community influence for lesbian, gay, bisexual, and transgender youth. Journal of Youth Studies, 18(3), 277–290. doi: 10.1080/13676261.2014.944114. [DOI] [Google Scholar]
- Hatzenbuehler ML, Jun HJ, Corliss HL, & Austin SB (2015). Structural stigma and sexual orientation disparities in adolescent drug use. Addictive Behaviors, 46, 14–18. doi: 10.1016/j.addbeh.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck NC, Livingston NA, Flentje A, Oost K, Stewart BT, & Cochran BN (2014). Reducing risk for illicit drug use and prescription drug misuse: High school gay-straight alliances and lesbian, gay, bisexual, and transgender youth. Addictive Behaviors, 39(4), 824–828. doi: 10.1016/j.addbeh.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck NC, Flentje A, & Cochran BN (2013). Offsetting risks: High school gay-straight alliances and lesbian, gay, bisexual, and transgender (LGBT) youth. Psychology of Sexual Orientation and Diversity, 1(S), 81–90. doi: 10.1037/2329-0382.1.S.81. [DOI] [Google Scholar]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Provider Psychology: Research and Practice, 43(5), 460. doi: 10.1037/a0029597. [DOI] [Google Scholar]
- Hill DB, Menvielle E, Sica KM, & Johnson A (2010). An affirmative intervention for families with gender variant children: Parental ratings of child mental health and gender. Journal of Sex & Marital Therapy, 36(1), 6–23. doi: 10.1080/00926230903375560. [DOI] [PubMed] [Google Scholar]
- Hines S (2006). Intimate transitions: Transgender practices of partnering and parenting. Sociology, 40(2), 353–371. doi: 10.1177/0038038506062037. [DOI] [Google Scholar]
- Hughes TL, & Eliason M (2002). Substance use and abuse in lesbian, gay, bisexual and transgender populations. Journal of Primary Prevention, 22(3), 263–298. doi: 10.1023/A:1013669705086. [DOI] [Google Scholar]
- Hines S (2006). What’s the difference? Bringing particularity to queer studies of transgender. Journal of Gender Studies, 15(1), 49–66. Doi: 10.1080/09589230500486918. [DOI] [Google Scholar]
- Klein K, Holtby A, Cook K, & Travers R (2015). Complicating the coming out narrative: Becoming oneself in a heterosexist and cissexist world. Journal of Homosexuality. 62(3), 297–326. doi: 10.1080/00918369.2014.970829. [DOI] [PubMed] [Google Scholar]
- Legal L. (2010). When health care isn’t caring: Lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York, NY: Lambda Legal. [Google Scholar]
- Lev A (2004). Transgender emergence therapeutic guidelines for working with gender-variant people and their families (Haworth marriage and the family). New York: Haworth Clinical Practice Press: Routledge. [Google Scholar]
- Levitt H, & Ippolito MR (2014). Being transgender: The experience of transgender identity development. Journal of Homosexuality. 61(12), 1727–1758. doi: 10.1080/00918369.2014.951262. [DOI] [PubMed] [Google Scholar]
- Lombardi E (2010). Transgender health: A review and guidance for future research—Proceedings from the Summer Institute at the Center for Research on Health and Sexual Orientation, University of Pittsburgh. International Journal of Transgenderism, 12(4), 211–229. doi: 10.1080/15532739.2010.544232. [DOI] [Google Scholar]
- Maguen S, Shipherd JC, Harris HN, & Welch LP (2007). Prevalence and predictors of disclosure of transgender identity. International Journal of Sexual Health, 19(1), 3–13. doi: 10.1300/j514v19n01_02. [DOI] [Google Scholar]
- Meyer IH (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36, 38–56. doi: 10.2307/2137286. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129(5), 674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills‐Koonce WR, Rehder PD, & McCurdy AL (2018). The significance of parenting and parent–child relationships for sexual and gender minority adolescents. Journal of Research on Adolescence, 28(3), 637–649. doi: 10.1111/jora.12404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizock L, Hopwood R, Brown Ronald T., & Borden Kathi A. (2018). Economic Challenges Associated With Transphobia and Implications for Practice With Transgender and Gender Diverse Individuals. Provider Psychology: Research and Practice. 49(1), 65–74. doi: 10.1037/pro0000161. [DOI] [Google Scholar]
- Mizock L, & Mueser KT (2014). Employment, mental health, internalized stigma, and coping with transphobia among transgender individuals. Psychology of Sexual Orientation and Gender Diversity, 1(2), 146. doi: 10.1037/sgd0000029. [DOI] [Google Scholar]
- Mohr J, Fassinger R. (2000). Measuring dimensions of lesbian and gay male experience. Measurement and Evaluation in Counseling and Development, 33(2), 66–90. doi: 10.1037/t07099-000. [DOI] [Google Scholar]
- Nemoto T, Operario D, Keatley J, Han L, & Soma T (2004). HIV risk behaviors among male-to-female transgender persons of color in San Francisco. American Journal of Public Health, 94(7), 1193–1199. doi: 10.2105/AJPH.94.7.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Birkett M, Corliss HL, & Mustanski B (2014). Sexual orientation, gender, and racial differences in illicit drug use in a sample of US high school students. American Journal of Public Health, 104(2), 304–310. doi: 10.2105/AJPH.2013.301702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, & Becker J (2014). Gender abuse, depressive symptoms, and substance use among transgender women: a 3-year prospective study. American Journal of Public Health, 104(11), 2199–2206. doi: 10.2105/AJPH.2014.302106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson-Kennedy J, Cohen-Kettenis PT, Kreukels BP, Meyer-Bahlburg HF, Garofalo R, Meyer W, & Rosenthal SM (2016). Research priorities for gender nonconforming/transgender youth: gender identity development and biopsychosocial outcomes. Current Opinion in Endocrinology, Diabetes, and Obesity, 23(2), 172. doi: 10.1097/MED.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson KR, Durwood L, DeMeules M, & McLaughlin KA (2016). Mental health of transgender children who are supported in their identities. Pediatrics, 137(3), 1–8. doi: 10.1542/peds.2015-4358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott-Holland CJ, Huang JL, Ryan AM, Elizondo F, & Wadlington PL (2013). Culture and vocational interests: The moderating role of collectivism and gender egalitarianism. Journal of Counseling Psychology, 60(4), 569. doi: 10.1037/a0033587. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Cochran SD, & Mays V, & Nezu AM (2015). The mental health of sexual minority adults in and out of the closet: A population-based study. Journal of Consulting and Clinical Psychology, 83(5), 890–901. doi: 10.1037/ccp0000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock E, Andrinopoulos K, & Hembling J (2015). Binge drinking among men who have sex with men and transgender women in San Salvador: correlates and sexual health implications. Journal of Urban Health, 92(4), 701–716. doi: 10.1007/s11524-014-9930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pflum SR, Testa RJ, Balsam KF, Goldblum PB, & Bongar B (2015). Social support, trans community connectedness, and mental health symptoms among transgender and gender nonconforming adults. Psychology of Sexual Orientation and Gender Diversity, 2(3), 281. doi: 10.1037/sgd0000122. [DOI] [Google Scholar]
- Poteat T, German D, & Kerrigan D (2013). Managing uncertainty: A grounded theory of stigma in transgender health care encounters. Social Science & Medicine, 84, 22–29. doi: 10.1016/j.socscimed.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Ramirez MH, & Sterzing PR (2017). Coming out in camouflage: A queer theory perspective on the strength, resilience, and resistance of lesbian, gay, bisexual, and transgender service members and veterans. Journal of Gay & Lesbian Social Services, 29(1), 68–86. doi: 10.1080/10538720.2016.1263983. [DOI] [Google Scholar]
- Reisner SL, Gamarel KE, Nemoto T, & Operario D (2014). Dyadic effects of gender minority stressors in substance use behaviors among transgender women and their non-transgender male partners. Psychology of sexual Orientation and Gender Diversity, 1(1), 63. doi: 10.1037/0000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, & Austin SB (2014). Monitoring the health of transgender and other gender minority populations: validity of natal sex and gender identity survey items in a US national cohort of young adults. BMC Public Health, 14(1), 1224. doi: 10.1186/1471-2458-14-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, & Murchison GR (2016). A global research synthesis of HIV and STI biobehavioural risks in female-to-male transgender adults. Global Public Health, 11(7–8), 866–887. doi: 10.1080/17441692.2015.1134613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, & Mimiaga MJ (2015). Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. Journal of Adolescent Health, 56(3), 274–279. doi: 10.1016/j.jadohealth.2014.10.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S, Pardo S, Gamarel K, Hughto J, Pardee D, Keo-Meier C (2015). Substance use to cope with stigma in healthcare among U.S. female-to-male trans masculine adults. LGBT Health, 2(4), 324–332. doi: 10.1089/lgbt.2015.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggle ED, Rostosky SS, McCants LE, & Pascale-Hague D (2011). The positive aspects of a transgender self-identification. Psychology & Sexuality, 2(2), 147–158. doi: 10.1080/19419899.2010.534490 [DOI] [Google Scholar]
- Riggle ED, Rostosky SS, Black WW, & Rosenkrantz DE (2017). Outness, concealment, and authenticity: Associations with LGB individuals’ psychological distress and well-being. Psychology of Sexual Orientation and Gender Diversity, 4(1), 54. doi: 10.1037/sgd0000202. [DOI] [Google Scholar]
- Rosenberg M (2015). Society and the adolescent self-image. Princeton University Press. [Google Scholar]
- Rosenberg M (1989). Society and the adolescent self-image (rev. ed.). Middletown, CT: Wesleyan University Press. Retrieved from EBSCOhost. [Google Scholar]
- Rossman K, Salamanca P, & Macapagal K (2017). A qualitative study examining young adults’ experiences of disclosure and nondisclosure of LGBTQ identity to health care providers. Journal of Homosexuality, 64(10), 1390–1410. doi: 10.1080/00918369.2017.1321379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell S, Toomey R, Ryan C, Diaz R (2014). Being out at school: The implications for school victimization and young adult adjustment. American Journal of Orthopsychiatry, 84(6), 635–643. doi: 10.1037/ort0000037. [DOI] [PubMed] [Google Scholar]
- Ryan C, Russell ST, Huebner D, Diaz R, & Sanchez J (2010). Family acceptance in adolescence and the health of LGBT young adults. Journal of Child and Adolescent Psychiatric Nursing, 23(4), 205–213. doi: 10.1111/j.1744-6171.2010.00246.x. [DOI] [PubMed] [Google Scholar]
- Saeed A, Mughal U, & Farooq S (2017). It’s Complicated: Sociocultural factors and the Disclosure Decision of Transgender Individuals in Pakistan. Journal of Homosexuality, 1–20. doi: 10.1080/00918369.2017.1368766. [DOI] [PubMed] [Google Scholar]
- Santos GM, Rapues J, Wilson EC, Macias O, Packer T, Colfax G, & Raymond HF (2014). Alcohol and substance use among transgender women in San Francisco: prevalence and association with human immunodeficiency virus infection. Drug and Alcohol Review. 33(3), 287–295. doi: 10.1111/dar.12116. [DOI] [PubMed] [Google Scholar]
- Savin-Williams RC, & Dubé EM (1998). Parental reactions to their child’s disclosure of a gay/lesbian identity. Family Relations, 47. 7–13. doi: 10.2307/584845 [DOI] [Google Scholar]
- Schimmel-Bristow A, Haley SG, Crouch JM, Evans YN, Ahrens KR, McCarty CA, & Inwards-Breland DJ (2018). Youth and caregiver experiences of gender identity transition: A qualitative study. Psychology of Sexual Orientation and Gender Diversity. doi: 10.1037/sgd0000269. [DOI] [Google Scholar]
- Simons L, Schrager SM, Clark LF, Belzer M, & Olson J (2013). Parental support and mental health among transgender adolescents. Journal of Adolescent Health, 53(6), 791–793. doi: 10.1016/j.jadohealth.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skidmore W, Linsenmeier C, & Bailey J (2006). Gender Nonconformity and Psychological Distress in Lesbians and Gay Men. Archives of Sexual Behavior. 35(6), 685–697. doi: 10.1007/s10508-006-9108-5. [DOI] [PubMed] [Google Scholar]
- Snapp SD, Watson RJ, Russell ST, Diaz RM, & Ryan C (2015). Social support networks for LGBT young adults: Low cost strategies for positive adjustment. Family Relations, 64(3), 420–430. doi: 10.111/fare.12124. [DOI] [Google Scholar]
- Sterzing PR, Ratliff GA, Gartner RE, McGeough BL, & Johnson KC (2017). Social ecological correlates of polyvictimization among a national sample of transgender, genderqueer, and cisgender sexual minority adolescents. Child Abuse & Neglect, 67, 1–12. doi: 10.1016/j.chiabu.2017.02.017. [DOI] [PubMed] [Google Scholar]
- Stevens S (2012). Meeting the substance abuse treatment needs of lesbian, bisexual and transgender women: implications from research to practice. Substance Abuse Rehabilitation, 3(Suppl 1), 27–36. doi: 10.2147/SAR.S26430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strain JD, & Shuff IM (2010). Psychological well-being and level of outness in a population of male-to-female transsexual women attending a national transgender conference. International Journal of Transgenderism, 12(4), 230–240. doi: 10.1080/15532739.2010.544231. [DOI] [Google Scholar]
- Testa R, Sciacca L, Wang F, Hendricks M, Goldblum P, Bradford J, Roberts Michael C. (2012). Effects of Violence on Transgender People. Provider Psychology: Research and Practice. 43(5), 452–459. doi: 10.1037/a0029604. [DOI] [Google Scholar]
- Testa R, Habarth J, Peta J, Balsam K, Bockting W, & Gonsiorek John C. (2015). Development of the Gender Minority Stress and Resilience Measure. Psychology of Sexual Orientation and Gender Diversity. 2(1), 65–77. doi: 10.1037/sgd0000081. [DOI] [Google Scholar]
- Testa RJ, Michaels MS, Bliss W, Rogers ML, Balsam KF, & Joiner T (2017). Suicidal ideation in transgender people: Gender minority stress and interpersonal theory factors. Journal of Abnormal Psychology, 126(1), 125–136. doi: 10.1037/abn0000234. [DOI] [PubMed] [Google Scholar]
- Trusty J, Thompson B, & Petrocelli JV (2004). Practical guide for reporting effect size in quantitative research in the Journal of Counseling & Development. Journal of Counseling & Development, 82(1), 107–110. doi: 10.1002/j.1556-6678.2004.tb00291.x. [DOI] [Google Scholar]
- Tucker JS, Ellickson PL, Orlando M, Martino SC, & Klein DJ (2005). Substance use trajectories from early adolescence to emerging adulthood: A comparison of smoking, binge drinking, and marijuana use. Journal of Drug Issues, 35(2), 307–332. doi: 10.1177/002204260503500205. [DOI] [Google Scholar]
- Veale JF, Watson RJ, Peter T, Saewyc EM (2017). Mental health disparities among Canadian transgender youth, Journal of Adolescent Health. 60, 44–49. doi: 10.1016/j.jadohealth.2016.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson RJ, Wheldon C, & Puhl RM (2019). Evidence of diverse identities in a large national sample of sexual and gender minority adolescents. Journal of Research on Adolescence, Online Early View, 1–12. doi: 10.1111/jora.12488 [DOI] [PubMed] [Google Scholar]
- Westbrook L, & Saperstein A (2015). New categories are not enough: Rethinking the measurement of sex and gender in social surveys. Gender & Society, 29(4), 534–560. doi: 10.1177/0891243215584758. [DOI] [Google Scholar]
- Wills TA, Vaccaro D, & McNamara G (1992). The role of life events, family support, and competence in adolescent substance use: A test of vulnerability and protective factors. American Journal of Community Psychology, 20(3), 349–374. doi: 10.1007/BF00937914. [DOI] [PubMed] [Google Scholar]
- Wolf EC, & Dew BJ (2012). Understanding risk factors contributing to substance use among MTF transgender persons. Journal of LGBT Issues in Counseling, 6(4), 237–256. doi: 10.1080/15538605.2012.727743. [DOI] [Google Scholar]
- Wren B (2002). ‘I can accept my child is transsexual but if I ever see him in a dress I’ll hit him’: Dilemmas in parenting a transgendered adolescent. Clinical Child Psychology and Psychiatry, 7(3), 377–397. doi: 10.1177/1359104502007003006. [DOI] [Google Scholar]