Abstract
Breaking bad news is a key component of the physicians’ work. Traditionally, breaking bad news has been encouraged to be performed in person whenever possible (Monden et al. Proc (Bayl Univ Med Cent) 29(1):101–102, 2016; Nickson 2019). The common practice prior to the pandemic can be summarized by “The first rule of breaking bad news is: do not do it over the phone.” It is important to be present with the family and provide support through compassion and empathy. Until recently, virtual communication technology for serious medical discussions was rare and primarily used when compelled by circumstances such as distance. The COVID-19 pandemic has transformed our ability to deliver news in person and has required the medical community to increase the utilization of telephone and video conferencing to communicate with patients and their family members. Breaking bad news through virtual media is a new skill in need of further guidance and education regarding how to set up the conversation, provide empathy, and lend support (Wolf et al., Oncologist 25(6):e879–e880, 2020). Therefore, we have created a teaching toolbox to help educate healthcare providers on how to deliver bad news by phone or video.
Keywords: Bad news, Simulation, Education, Virtual technology, Telehealth
Breaking Bad News Training
There are various frameworks that provide guidance and steps for delivering bad news. One is the SPIKES framework, which includes setting, immediate concerns, knowledge, empathy, and summary/second touch [4]. It has been demonstrated in prior studies that physicians’ confidence and skills in delivering bad news can be improved using the SPIKES framework along with scenarios conducted in a simulated environment [5–7].
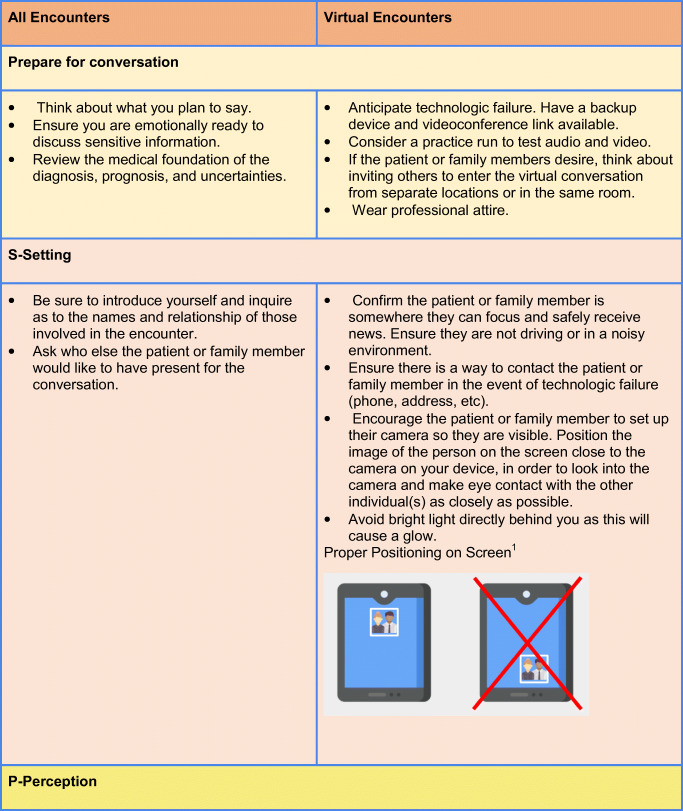
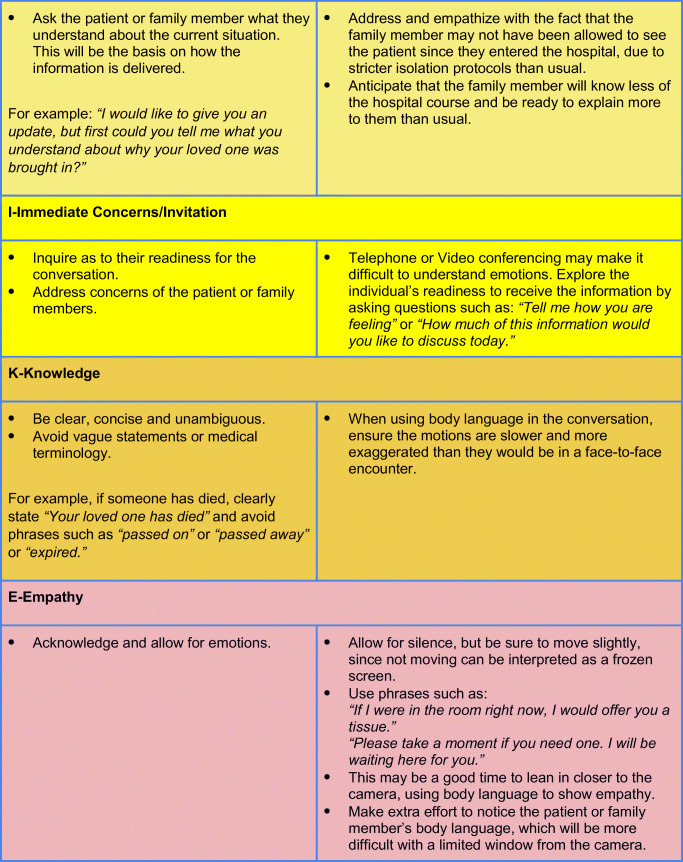
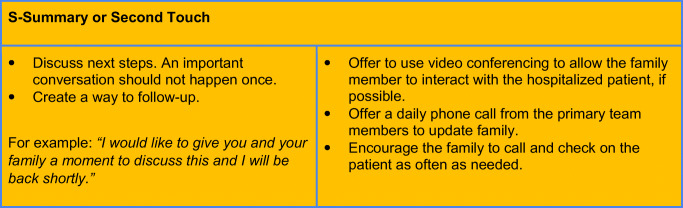
Given the increasing need to deliver bad news over virtual media platforms, we have created a teaching toolbox to adapt the traditional SPIKES model for use during virtual encounters (Table 1). In addition, our institution has added the “prep” portion to emphasize the importance of preparing for the conversation. Breaking bad news in-person is already difficult for providers to empathetically deliver and for patients to emotionally receive, and the current pandemic poses additional challenges. Virtual technologies are increasingly being used to deliver care through telemedicine and can be extended to support breaking bad news virtually. These strategies should only be employed when a face-to-face meeting is unable to be scheduled due to transportation barriers or social distancing recommendations. Some educators may choose to allow trainees to practice using standardized patients, case-based discussions, and role plays. By creating high fidelity simulations, it will help to both reinforce the key concepts of delivering bad news and will help improve provider communication skills.
Table 1.
Prep-SPIKES adaptation to virtual format
1“tablet” icon made by Freepik from www.flaticon.com. <div>Icons made by <a href=“https://www.flaticon.com/authors/freepik” title=“Freepik”>Freepik</a> from <a href=“https://www.flaticon.com/” title=“Flaticon”>
Conclusion
The COVID-19 pandemic has presented challenges in our ability to deliver bad news. However, we have the ability to utilize virtual technology to help us deliver high value care to our patients and their loved ones. We have focused on ways to maintain empathy when having difficult conversations with patients and their family members. We believe these adaptations to the traditional SPIKES model can be easily implemented by others to provide virtual training in delivering bad news.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Monden KR, Gentry L, Cox TR. Delivering bad news to patients. Proc (Bayl Univ Med Cent). 2016;29(1):101–102. doi: 10.1080/08998280.2016.11929380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nickson DC. Breaking bad news to patients and relatives • LITFL • CCC Clinical Governance. Life in the Fast Lane • LITFL • Medical Blog. Published January 7, 2019. https://litfl.com/breaking-bad-news-to-patients-and-relatives/. Accessed 24 May 2020
- 3.Wolf I, Waissengrin B, Pelles S. Breaking bad news via telemedicine: a new challenge at times of an epidemic. Oncologist. 2020;25(6):e879–e880. doi: 10.1634/theoncologist.2020-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 5.Park I, Gupta A, Mandani K, Haubner L, Peckler B. Breaking bad news education for emergency medicine residents: a novel training module using simulation with the SPIKES protocol. J Emerg Trauma Shock. 2010;3(4):385. doi: 10.4103/0974-2700.70760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papadakos CT, Stringer T, Papadakos J, Croke J, Embleton A, Gillan C, Miller K, Weiss A, Wentlandt K, Giuliani M (2020 Mar 5) Effectiveness of a multiprofessional, online and simulation-based difficult conversations training program on self-perceived competence of oncology healthcare provider trainees. J Cancer Educ. 10.1007/s13187-020-01729-x [DOI] [PubMed]
- 7.von Blanckenburg P, Hofmann M, Rief W, Seifart U, Seifart C (2020) Assessing patients’ preferences for breaking bad news according to the SPIKES-protocol: the MABBAN scale. Patient Educ Couns:S0738-3991(20)30110-5. 10.1016/j.pec.2020.02.036 [DOI] [PubMed]