Abstract
INTRODUCTION
Low back pain is the most common type of global disability and annually costs the United States over two billion dollars. Opioids have been used to reduce low back pain, although current evidence concerning efficacy is lacking. Sacroiliac joint dysfunction (SIJD) is estimated to be a primary pain source of low back pain in between 10 and 25% of affected patients. The primary objective of this study was to evaluate the rate of SIJD identified through osteopathic techniques in a convenience sample of patients seeking low back pain treatment. The secondary objective was to assess prevalence of low back pain and SIJD among different age groups, and genders.
METHODS
Retrospective chart reviews were completed the adult patients who had received osteopathic manipulative treatment for low back pain at Family Health and Wellness Center in Essexville, MI from January 2018 through June 2019. The prevalence of patients with SIJD was identified during reviews of osteopathic procedural documentation for patients seeking low back pain treatment. Data regarding patients’ age, sex, and treatment modalities were also extracted. Descriptive statistics consisting of frequencies and percentages were calculated.
RESULTS
A total of 84 patient records were reviewed. A total of 51 (60.7%) patients seeking low back pain treatment were diagnosed with SIJD identified by osteopathic providers. This included patients with both lumbar and sacral diagnoses simultaneously. SIJD alone accounted for 26 (31%) of patients seeking treatment. Female patients were more likely to have SIJD involvement than males. Forty one (48.8%) treated patients were between 45-64 years old. Muscle Energy Technique was documented to be the most used for 68 (81%) patients. In addition, techniques tended to move from direct to indirect for older patients.
DISCUSSION
Our study demonstrated that SIJD appeared to contribute to low back pain in 51 (60.7%) of low back pain cases identified using osteopathic techniques. This is much greater than the previously reported percentages of 10 to 25%. One possible confounding influence included varied resident screening and reporting of sacral dysfunction. Since multiple areas of the body can be treated at one time, our current procedure notes did not allow for distinguishing between which types of modalities were used on each region or capture residents’ preferred treatments.
CONCLUSIONS
Although further studies are needed, our results suggest that knowledge of SIJD’s impact on low back pain could lead to improved patient outcomes such as decreased medical costs and opioid use.
Keywords: osteopathic manipulative treatment, sacroiliac joint dysfunction, low back pain
INTRODUCTION
Low back pain is the fifth most common chief complaint in the primary care setting, affecting more than 26 million Americans.1 It has also been estimated that 65-80% of adults will have low back pain during their lifetime.1,2 In 2015, a systematic review demonstrated that lower back and neck pain was the single largest cause of US and global disability from musculoskeletal disorders.3 Globally, it was the most common reason for disability for persons aged 25 to 64 and the second most common cause in adults between 20 to 24 and 65 to 79 years old.3
In addition to the physical toll of low back pain in the US, this high rate of this condition results in a substantial financial impact.4 A recent article analyzing health care utilization in an opiate-naive patient population found a 12-month post-diagnosis cost of over $2.5 billion. Non-surgical patients accounted for 70.8%, costing the healthcare system $1.8 billion (i.e., approximately $795 per patient).4 Current guidelines recommend against obtaining imaging of the spine within 30 days of a low back pain diagnosis or without a trial of physical therapy.4 One-third of patients with low back pain who were treated non-surgically received imaging within 30 days of diagnosis. These patients expended two times greater healthcare dollars than those who followed guidelines and did not receive early imaging.4
In contrast, surgical patients in this same study comprised 29.3%, spending $784 million (i.e., approx. $25,613 per patient).4 When providers consider surgical low back pain patients, it is important to consider postoperative failure risks. Patients may experience post-lumbar laminectomy syndrome, or failed back surgery syndrome (FBSS) with persistent pain and functional compromise. Unfortunately, as many as 80,000 surgical patients, or roughly 20-40% of the low back surgery population, result in FBSS.5,6
Although evidence appears to be lacking in regard to opioids providing short-term low back pain relief, adherence to an opioid regimen has been shown to provide some functional improvement.5,7 However, there is an increasing problem with opioid use and dependence in the US. In 2010, 20% of 164 million pain visits were treated with an opioid; meaning, approximately one in five noncancerous pain patients had been prescribed an opioid.2,8 This ratio has only been increasing. By 2016, there were 67 opioid prescriptions filled for every 100 Americans with noncancerous pain.2 Of more concern, one in four patients receiving long-term opioid treatment for chronic pain have been shown to struggle with opioid use disorder and approximately 130 Americans die every day from an opioid overdose.8
One modality with the potential to mitigate opioid use by decreasing low back pain is osteopathic manipulative treatment (OMT). Manipulation is known for its noninvasive, low-risk benefits, and has been demonstrated as a first-line treatment for chronic low back pain.9–11 OMT has been defined as, "the therapeutic application of manually guided forces by an osteopathic physician to improve physiologic function and/or support homeostasis that has been altered by somatic dysfunction."12 Somatic dysfunction is a malfunction of the body system, which may involve muscles, skeleton, nervous system, and/or lymphatics that leads to overall dysfunction manifesting as pain or impairment. Somatic dysfunction has been shown to be treatable using OMT.9,12,13
Osteopathic physicians are trained to look at structure and function as a whole; they connect somatic dysfunctions to patients' symptoms.14 Osteopathic physicians have also been specifically taught that there are six main dysfunctions that can be associated with low back pain. One of those dysfunctions is found in the sacroiliac joint (SIJ), seen as restriction of movement at the sacral base.14 Previous research has estimated that 10 to 25% of chronic low back pain has a SIJ pain source.11,15–17 Interestingly, there is a higher rate (i.e., up to 40%) of SIJD being the source of low back pain in patients with FBSS with the rate in some studies noted as high as 63%.16–18
When SIJ is included in the differential diagnosis for chronic low back pain, there is a decrease in not only pain, but in health care expenditures.10,14,18 The diagnosis of SIJD can be formulated in several different ways. There are many provocative tests that aid in diagnosis; Flexion Abduction External Rotation (FABER), a stress maneuver that detects hip and sacroiliac joint pathology.15 FABER is found to be the most reliable as well as most prevalent in studies examining SIJ pain.15,19 The current “gold standard” for SIJ diagnosis and treatment is performing injections with a corticosteroid or anesthetic drug under fluoroscopic guidance to obtain between 50 to 75% pain relief.10,15,16,18
Research is currently lacking in osteopathic manipulative diagnosis of low back pain, and SIJD. Recent studies have shown that manipulative treatments have a positive effect on decreasing patients' pain with some improvement on functional status.9 By incorporating osteopathic manipulation into patients' treatment plans, there could be fewer costly surgeries and FBSS risks. Improving patients’ function and level of pain could also result in fewer opioid prescriptions for chronic low back pain.
Study Purpose
The primary purpose of this retrospective descriptive correlational study was to evaluate the relationship between low back pain and sacroiliac joint dysfunction as identified using OMT within the primary care population. Secondarily, this study sought to assess the prevalence of low back pain and sacroiliac dysfunction by age and gender. Before the study, the authors hypothesized that sacroiliac joint dysfunction would be more common than previously found.
METHODS
The authors’ institutional review board approved the study protocol prior to any data collection. This study was conducted at an outpatient family medicine residency clinic in Essexville, Michigan. Charts were identified and evaluated of patients who were: 18 years and older and had received OMT for low back pain between January 1, 2018 and June 30, 2019.
The McLaren Medical Group’s Business Info Specialist and Physician Biller generated a report based on office billing codes of patients who had a diagnosis of low back pain along with OMT procedure codes. This report listed the patient's name, date of birth and date of service, identifying which charts would be utilized. A report of eligible charts was shredded after use, and all necessary research data was kept on a spreadsheet containing only a unique patient identifier with all study information.
All data were solely recorded on the encrypted McLaren Cloud information system. Specifically, charts were evaluated for the percentage rates of patients with sacroiliac joint dysfunction, as documented note for patients who had received OMT for low back pain. As part of routine OMT procedures for the treatment of low back pain, providers had completed notes of any sacroiliac joint dysfunction diagnosed as based on Osteopathic Manipulative Medicine (OMM) principles.14
Patients’ charts were excluded if they were found to be non-English speaking without an interpreter present during treatments, pregnant, or have known mental and/or physical disabilities. There were no vulnerable populations identified for recruitment in this retrospective chart review.
STATISTICAL ANALYSIS
Before proceeding with statistical analyses, data were examined for data outliers, out of range values, and the need for data cleaning and editing before performing a series of frequencies, proportions, descriptive statistics (e.g., mean, median, and standard deviation) and figures (e.g., histograms and box and whisker plots). After this process was performed, any needed data editing for simplification and clarity was conducted. Descriptive statistics such as percentages were presented from this study. The last author CFR-B performed all statistical analysis using the Stata statistical software package (Stata Corporation, College Station, TX).
RESULTS
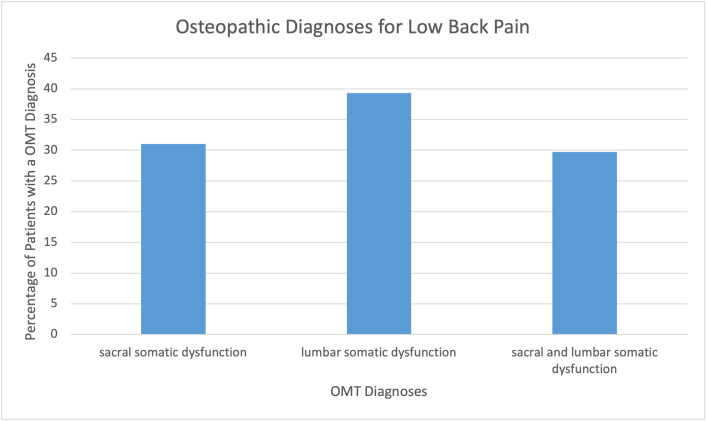
A total of 84 unique patients were identified and reviewed during this study, including 58 (69.0%) females and 26 (31.0%) males. Forty one (48.8%) sample patients who received treatment were between the ages of 45-64 years old. (Table 1) A total of 51 (60.7%) patients who were seeking low back pain treatment were diagnosed with SIJD identified using osteopathic techniques. This number included patients with both lumbar and sacral diagnoses. Sacral diagnoses alone accounted for 26 (31.0%) of patients seeking treatment for low back pain. (Figure 1)
Table 1: Patient Characteristics.
| Individuals | Percentage | |
|---|---|---|
| Total | 84 | 100.0% |
| Gender | ||
| Female | 58 | 69.0% |
| Males | 26 | 31.0% |
| Age | ||
| 18-24 years | 7 | 8.3% |
| 25-44 years | 33 | 39.3% |
| 45-64 years | 41 | 48.8% |
| 65+ years | 3 | 3.8% |
Figure 1: Osteopathic Diagnoses for Low Back Pain.
The prevalence of somatic dysfunctions were identified overall for patients with a chief complaint of back pain. Lumbar somatic dysfunction alone was most common at 33 (39.3%), followed by only sacral somatic dysfunction 26 (31.0%), then combined sacral and lumbar somatic dysfunction 25 (29.7%). (Figure 1)
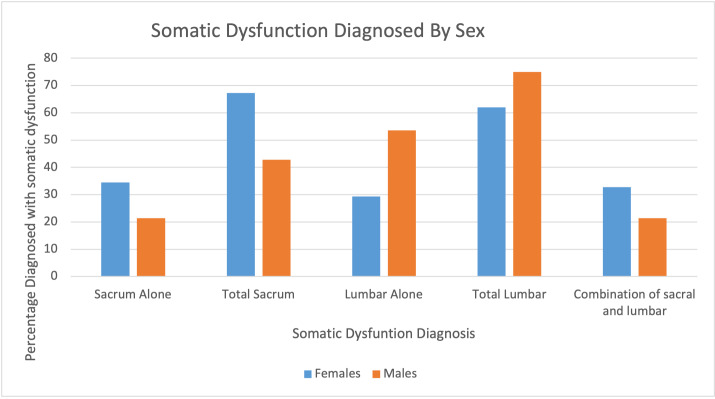
Our secondary objective was to examine the prevalence of low back pain by gender and explore different treatment modalities used for low back pain. Generally, females were more likely to have SIJD involvement than males. Females had 39 (67.2%) of overall sacral involvement, with 20 (34.5%) females accounting for SIJD alone. While males accounted for 12 (46.2%) sacral or sacral and lumbar involvement and six (23.1%) of sacral alone. (Figure 2)
Figure 2: Somatic Dysfunction Diagnosis by Sex.
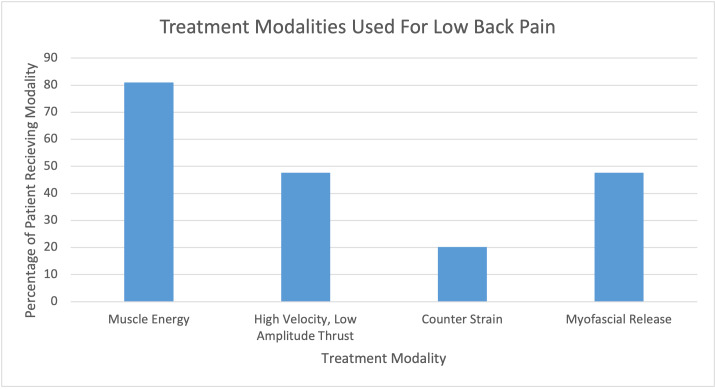
Although multiple modalities can be individually or simultaneously used to treat low back pain, Muscle Energy Technique (MET) was found to be the most commonly used 68 (81.0%) treatment. Following MET, High Velocity Low Amplitude (HVLA) and Myofascial Release (MFR) were both next at 40 (47.6%). Counterstrain (CS) was used least frequently at 17 (20.2%). (Figure 3)
Figure 3: Low Back Pain Treatment Modalities.
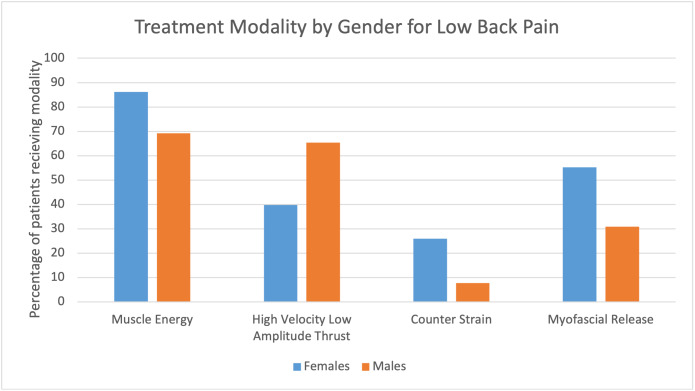
When examining which modalities were most commonly used for each gender, MET was still the most common for in both female 50 (86.2%) and male 18 (69.2%) patients. Overall, females were more likely to receive treatment multiple modalities. Specifically, females were more likely to receive all types of treatment except for HVLA. For females, MET was most used for 50 (86.2%), followed by MFR 32 (55.2%), HVLA 23 (39.7%), and finally CS 15 (25.9%). For males, MET was most used for 18 (69.2%), followed by HVLA 17 (65.4%), MFR eight (30.8%), and CS two (7.7%). (Figure 4)
Figure 4: Treatment Modalities by Gender.
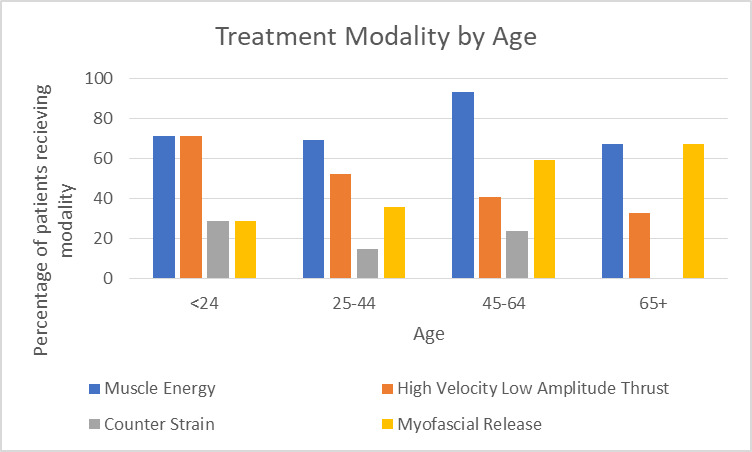
When examining modalities by age subgroup, techniques were seen to change from direct to indirect for older patients. For patients under 24 years old, HVLA and MET were equally used, both being used in five (71.4%) patients in this age subgroup. For ages 25-44, MET was most common (n = 23 (69.7%) with HVLA being second most common at 17 (51.5%). For ages 45-64, MET was again most common (n = 38 (92.7%) with MFR being second most likely at 24 (58.5%) respectively. For patients aged 65 and older, MET and MFR were seen to be equally as common, with both being used in two (66.7%) patients in this age range. (Figure 5)
Figure 5: Treatment Modalites by Patient Age.
DISCUSSION
It is evident from these results that SIJD involvement in low back pain is possibly being overlooked. Our study demonstrated more than double the rate of SIJD than was found in previous studies.11,15–17 There are a several possible explanations to explain this finding.
First, our sample size was a small section of the overall low back pain population. Rates of SIJD could potentially be different in a larger sample. Also, many sample patients may have come in for routine treatments of their chronic ailments and may have not always received the same OMT diagnoses during each visit. Incorporating data from each visit may have increased our total sample size. Another explanation for this finding is that osteopathic physicians are trained to seek out other diagnoses which cause low back pain. This could have potentially led to surveillance bias.
There were several confounding influences that may have affected our final results, the largest involving screening and documentation. As our data collection used chart reviews, there was no standardized process for screening patients’ somatic dysfunctions or documentation. Although osteopathic providers are taught systematic ways to screen and document osteopathic findings, these practice patterns are always utilized in practice.
Physicians may not screen for dysfunctions outside of the immediate area, such as in the sacrum, when they are examining a patient for low back pain.14 Although it is anatomically related to the back, many patients may not experience, or be able to articulate, pain within in the sacrum, encouraging osteopathic physicians to focus directly on the back or on the patient's expressed area of pain or discomfort.
In 2016, the American Osteopathic Association provided guidelines for OMT to assist osteopaths with regards to low back pain in the proper utilization of OMT rather than guidelines for screening.9 Currently, there is no best practice guidelines for screening the lumbar spine using OMT. Furthermore, current healthcare documentation systems do not generally distinguish which OMT techniques are used on which areas. Many OMT modalities can be used on just one area of the body, and similarly multiple areas of the body are often treated at one office visit for OMT.
For example, our documentation system only enables osteopaths to denote that MET, HVLA, MFR and CS were used and that lumbar, sacral, and cervical regions were treated. As a result, we were unable to tell which treatments were used on each region of the body and to what affect. This is likely a nationwide issue and has major room for growth in the osteopathic community.
Unlike our retrospective chart review project, larger-sample prospective studies comparing groups given SIJ injections to those receiving osteopathic manipulation, a less invasive technique, could contribute a new gold standard for diagnosing sacroiliac joint dysfunction. Additionally, longitudinal studies could examine how osteopathic treatments over time impact the severity of low back pain, concurrent analgesic and/or opioid use frequency, and subsequent surgical procedure rates. Another prospective study design would be to record pain scales prior to, and following, treatment of patients’ SIJD to further identify how dysfunctions might impact low back pain.
Finally, it will be important to consider the holistic osteopathic tenants when developing projects in this area of research. Non-invasive osteopathic medicine treatment style improve patients’ quality of life from improved structural and functional self-regulating and self-healing has a significant potential to become a mainstay treatment for SIJD.
CONCLUSION
Previous research indicates that 10 to 25% of chronic low back pain has a SIJ pain source.11,15–17 The current gold standard for diagnosis & treatment is performing SIJ injections using a corticosteroid or anesthetic drug under fluoroscopic guidance to obtain 50 to 75% pain relief.10,15,16,18 Utilizing osteopathic techniques for diagnosis and treatment, the authors found that SIJD was present in the majority of patients when examined for low back pain. Based on these results, increased medical knowledge concerning SIJD’s impact on low back pain could lead to decreased medical costs and opioid use.
Disclosures
The overall results of this study were presented as a poster presentation at the Statewide Campus System Poster Day, May 2020.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The authors report no external funding source for this study.
References
- Urits Ivan, Burshtein Aaron, Sharma Medha, Testa Lauren, Gold Peter A., Orhurhu Vwaire, Viswanath Omar, Jones Mark R., Sidransky Moises A., Spektor Boris, Kaye Alan D. Current Pain and Headache Reports. 3. Vol. 23. Springer Science and Business Media LLC; Low back pain, a comprehensive review: Pathophysiology, diagnosis, and treatment. [DOI] [PubMed] [Google Scholar]
- Introduction to the opioid epidemic: The economic burden on the healthcare system and impact on quality of life. Hagemeier N.E. 2018Am J Manag Care. 24(10):S200–S206. [PubMed] [Google Scholar]
- Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Vos Theo, Allen Christine, Arora Megha, Barber Ryan M, Bhutta Zulfiqar A, Brown Alexandria, Carter Austin, Casey Daniel C, Charlson Fiona J, Chen Alan Z, Coggeshall Megan, Cornaby Leslie, Dandona Lalit, Dicker Daniel J, Dilegge Tina, Erskine Holly E, Ferrari Alize J, Fitzmaurice Christina, Fleming Tom, Forouzanfar Mohammad H, Fullman Nancy, Gething Peter W, Goldberg Ellen M, Graetz Nicholas, Haagsma Juanita A, Hay Simon I, Johnson Catherine O, Kassebaum Nicholas J, Kawashima Toana, Kemmer Laura, Khalil Ibrahim A, Kinfu Yohannes, Kyu Hmwe H, Leung Janni, Liang Xiaofeng, Lim Stephen S, Lopez Alan D, Lozano Rafael, Marczak Laurie, Mensah George A, Mokdad Ali H, Naghavi Mohsen, Nguyen Grant, Nsoesie Elaine, Olsen Helen, Pigott David M, Pinho Christine, Rankin Zane, Reinig Nikolas, Salomon Joshua A, Sandar Logan, Smith Alison, Stanaway Jeffrey, Steiner Caitlyn, Teeple Stephanie, Thomas Bernadette A, Troeger Christopher, Wagner Joseph A, Wang Haidong, Wanga Valentine, Whiteford Harvey A, Zoeckler Leo, Abajobir Amanuel Alemu, Abate Kalkidan Hassen, Abbafati Cristiana, Abbas Kaja M, Abd-Allah Foad, Abraham Biju, Abubakar Ibrahim, Abu-Raddad Laith J, Abu-Rmeileh Niveen M E, Ackerman Ilana N, Adebiyi Akindele Olupelumi, Ademi Zanfina, Adou Arsène Kouablan, Afanvi Kossivi Agbelenko, Agardh Emilie Elisabet, Agarwal Arnav, Kiadaliri Aliasghar Ahmad, Ahmadieh Hamid, Ajala Oluremi N, Akinyemi Rufus Olusola, Akseer Nadia, Al-Aly Ziyad, Alam Khurshid, Alam Noore K M, Aldhahri Saleh Fahed, Alegretti Miguel Angel, Alemu Zewdie Aderaw, Alexander Lily T, Alhabib Samia, Ali Raghib, Alkerwi Ala'a, Alla François, Allebeck Peter, Al-Raddadi Rajaa, Alsharif Ubai, Altirkawi Khalid A, Alvis-Guzman Nelson, Amare Azmeraw T, Amberbir Alemayehu, Amini Heresh, Ammar Walid, Amrock Stephen Marc, Andersen Hjalte H, Anderson Gregory M, Anderson Benjamin O, Antonio Carl Abelardo T, Aregay Atsede Fantahun, Ärnlöv Johan, Artaman Al, Asayesh Hamid, Assadi Reza, Atique Suleman, Avokpaho Euripide Frinel G Arthur, Awasthi Ashish, Quintanilla Beatriz Paulina Ayala, Azzopardi Peter, Bacha Umar, Badawi Alaa, Balakrishnan Kalpana, Banerjee Amitava, Barac Aleksandra, Barker-Collo Suzanne L, Bärnighausen Till, Barregard Lars, Barrero Lope H, Basu Arindam, Bazargan-Hejazi Shahrzad, Beghi Ettore, Bell Brent, Bell Michelle L, Bennett Derrick A, Bensenor Isabela M, Benzian Habib, Berhane Adugnaw, Bernabé Eduardo, Betsu Balem Demtsu, Beyene Addisu Shunu, Bhala Neeraj, Bhatt Samir, Biadgilign Sibhatu, Bienhoff Kelly, Bikbov Boris, Biryukov Stan, Bisanzio Donal, Bjertness Espen, Blore Jed, Borschmann Rohan, Boufous Soufiane, Brainin Michael, Brazinova Alexandra, Breitborde Nicholas J K, Brown Jonathan, Buchbinder Rachelle, Buckle Geoffrey Colin, Butt Zahid A, Calabria Bianca, Campos-Nonato Ismael Ricardo, Campuzano Julio Cesar, Carabin Hélène, Cárdenas Rosario, Carpenter David O, Carrero Juan Jesus, Castañeda-Orjuela Carlos A, Rivas Jacqueline Castillo, Catalá-López Ferrán, Chang Jung-Chen, Chiang Peggy Pei-Chia, Chibueze Chioma Ezinne, Chisumpa Vesper Hichilombwe, Choi Jee-Young Jasmine, Chowdhury Rajiv, Christensen Hanne, Christopher Devasahayam Jesudas, Ciobanu Liliana G, Cirillo Massimo, Coates Matthew M, Colquhoun Samantha M, Cooper Cyrus, Cortinovis Monica, Crump John A, Damtew Solomon Abrha, Dandona Rakhi, Daoud Farah, Dargan Paul I, das Neves José, Davey Gail, Davis Adrian C, Leo Diego De, Degenhardt Louisa, Gobbo Liana C Del, Dellavalle Robert P, Deribe Kebede, Deribew Amare, Derrett Sarah, Jarlais Don C Des, Dharmaratne Samath D, Dhillon Preet K, Diaz-Torné Cesar, Ding Eric L, Driscoll Tim R, Duan Leilei, Dubey Manisha, Duncan Bruce Bartholow, Ebrahimi Hedyeh, Ellenbogen Richard G, Elyazar Iqbal, Endres Matthias, Endries Aman Yesuf, Ermakov Sergey Petrovich, Eshrati Babak, Estep Kara, Farid Talha A, Farinha Carla Sofia e Sa, Faro André, Farvid Maryam S, Farzadfar Farshad, Feigin Valery L, Felson David T, Fereshtehnejad Seyed-Mohammad, Fernandes Jefferson G, Fernandes Joao C, Fischer Florian, Fitchett Joseph R A, Foreman Kyle, Fowkes F Gerry R, Fox Jordan, Franklin Richard C, Friedman Joseph, Frostad Joseph, Fürst Thomas, Futran Neal D, Gabbe Belinda, Ganguly Parthasarathi, Gankpé Fortuné Gbètoho, Gebre Teshome, Gebrehiwot Tsegaye Tewelde, Gebremedhin Amanuel Tesfay, Geleijnse Johanna M, Gessner Bradford D, Gibney Katherine B, Ginawi Ibrahim Abdelmageem Mohamed, Giref Ababi Zergaw, Giroud Maurice, Gishu Melkamu Dedefo, Giussani Giorgia, Glaser Elizabeth, Godwin William W, Gomez-Dantes Hector, Gona Philimon, Goodridge Amador, Gopalani Sameer Vali, Gotay Carolyn C, Goto Atsushi, Gouda Hebe N, Grainger Rebecca, Greaves Felix, Guillemin Francis, Guo Yuming, Gupta Rahul, Gupta Rajeev, Gupta Vipin, Gutiérrez Reyna A, Haile Demewoz, Hailu Alemayehu Desalegne, Hailu Gessessew Bugssa, Halasa Yara A, Hamadeh Randah Ribhi, Hamidi Samer, Hammami Mouhanad, Hancock Jamie, Handal Alexis J, Hankey Graeme J, Hao Yuantao, Harb Hilda L, Harikrishnan Sivadasanpillai, Haro Josep Maria, Havmoeller Rasmus, Hay Roderick J, Heredia-Pi Ileana Beatriz, Heydarpour Pouria, Hoek Hans W, Horino Masako, Horita Nobuyuki, Hosgood H Dean, Hoy Damian G, Htet Aung Soe, Huang Hsiang, Huang John J, Huynh Chantal, Iannarone Marissa, Iburg Kim Moesgaard, Innos Kaire, Inoue Manami, Iyer Veena J, Jacobsen Kathryn H, Jahanmehr Nader, Jakovljevic Mihajlo B, Javanbakht Mehdi, Jayaraman Sudha P, Jayatilleke Achala Upendra, Jee Sun Ha, Jeemon Panniyammakal, Jensen Paul N, Jiang Ying, Jibat Tariku, Jimenez-Corona Aida, Jin Ye, Jonas Jost B, Kabir Zubair, Kalkonde Yogeshwar, Kamal Ritul, Kan Haidong, Karch André, Karema Corine Kakizi, Karimkhani Chante, Kasaeian Amir, Kaul Anil, Kawakami Norito, Keiyoro Peter Njenga, Kemp Andrew Haddon, Keren Andre, Kesavachandran Chandrasekharan Nair, Khader Yousef Saleh, Khan Abdur Rahman, Khan Ejaz Ahmad, Khang Young-Ho, Khera Sahil, Khoja Tawfik Ahmed Muthafer, Khubchandani Jagdish, Kieling Christian, Kim Pauline, Kim Cho-il, Kim Daniel, Kim Yun Jin, Kissoon Niranjan, Knibbs Luke D, Knudsen Ann Kristin, Kokubo Yoshihiro, Kolte Dhaval, Kopec Jacek A, Kosen Soewarta, Kotsakis Georgios A, Koul Parvaiz A, Koyanagi Ai, Kravchenko Michael, Defo Barthelemy Kuate, Bicer Burcu Kucuk, Kudom Andreas A, Kuipers Ernst J, Kumar G Anil, Kutz Michael, Kwan Gene F, Lal Aparna, Lalloo Ratilal, Lallukka Tea, Lam Hilton, Lam Jennifer O, Langan Sinead M, Larsson Anders, Lavados Pablo M, Leasher Janet L, Leigh James, Leung Ricky, Levi Miriam, Li Yichong, Li Yongmei, Liang Juan, Liu Shiwei, Liu Yang, Lloyd Belinda K, Lo Warren D, Logroscino Giancarlo, Looker Katharine J, Lotufo Paulo A, Lunevicius Raimundas, Lyons Ronan A, Mackay Mark T, Magdy Mohammed, Razek Abd El, Mahdavi Mahdi, Majdan Marek, Majeed Azeem, Malekzadeh Reza, Marcenes Wagner, Margolis David Joel, Martinez-Raga Jose, Masiye Felix, Massano João, McGarvey Stephen Theodore, McGrath John J, McKee Martin, McMahon Brian J, Meaney Peter A, Mehari Alem, Mejia-Rodriguez Fabiola, Mekonnen Alemayehu B, Melaku Yohannes Adama, Memiah Peter, Memish Ziad A, Mendoza Walter, Meretoja Atte, Meretoja Tuomo J, Mhimbira Francis Apolinary, Millear Anoushka, Miller Ted R, Mills Edward J, Mirarefin Mojde, Mitchell Philip B, Mock Charles N, Mohammadi Alireza, Mohammed Shafiu, Monasta Lorenzo, Hernandez Julio Cesar Montañez, Montico Marcella, Mooney Meghan D, Moradi-Lakeh Maziar, Morawska Lidia, Mueller Ulrich O, Mullany Erin, Mumford John Everett, Murdoch Michele E, Nachega Jean B, Nagel Gabriele, Naheed Aliya, Naldi Luigi, Nangia Vinay, Newton John N, Ng Marie, Ngalesoni Frida Namnyak, Nguyen Quyen Le, Nisar Muhammad Imran, Pete Patrick Martial Nkamedjie, Nolla Joan M, Norheim Ole F, Norman Rosana E, Norrving Bo, Nunes Bruno P, Ogbo Felix Akpojene, Oh In-Hwan, Ohkubo Takayoshi, Olivares Pedro R, Olusanya Bolajoko Olubukunola, Olusanya Jacob Olusegun, Ortiz Alberto, Osman Majdi, Ota Erika, PA Mahesh, Park Eun-Kee, Parsaeian Mahboubeh, de Azeredo Passos Valéria Maria, Caicedo Angel J Paternina, Patten Scott B, Patton George C, Pereira David M, Perez-Padilla Rogelio, Perico Norberto, Pesudovs Konrad, Petzold Max, Phillips Michael Robert, Piel Frédéric B, Pillay Julian David, Pishgar Farhad, Plass Dietrich, Platts-Mills James A, Polinder Suzanne, Pond Constance D, Popova Svetlana, Poulton Richie G, Pourmalek Farshad, Prabhakaran Dorairaj, Prasad Noela M, Qorbani Mostafa, Rabiee Rynaz H S, Radfar Amir, Rafay Anwar, Rahimi Kazem, Rahimi-Movaghar Vafa, Rahman Mahfuzar, Rahman Mohammad Hifz Ur, Rahman Sajjad Ur, Rai Rajesh Kumar, Rajsic Sasa, Ram Usha, Rao Puja, Refaat Amany H, Reitsma Marissa B, Remuzzi Giuseppe, Resnikoff Serge, Reynolds Alex, Ribeiro Antonio L, Blancas Maria Jesus Rios, Roba Hirbo Shore, Rojas-Rueda David, Ronfani Luca, Roshandel Gholamreza, Roth Gregory A, Rothenbacher Dietrich, Roy Ambuj, Sagar Rajesh, Sahathevan Ramesh, Sanabria Juan R, Sanchez-Niño Maria Dolores, Santos Itamar S, Santos João Vasco, Sarmiento-Suarez Rodrigo, Sartorius Benn, Satpathy Maheswar, Savic Miloje, Sawhney Monika, Schaub Michael P, Schmidt Maria Inês, Schneider Ione J C, Schöttker Ben, Schwebel David C, Scott James G, Seedat Soraya, Sepanlou Sadaf G, Servan-Mori Edson E, Shackelford Katya A, Shaheen Amira, Shaikh Masood Ali, Sharma Rajesh, Sharma Upasana, Shen Jiabin, Shepard Donald S, Sheth Kevin N, Shibuya Kenji, Shin Min-Jeong, Shiri Rahman, Shiue Ivy, Shrime Mark G, Sigfusdottir Inga Dora, Silva Diego Augusto Santos, Silveira Dayane Gabriele Alves, Singh Abhishek, Singh Jasvinder A, Singh Om Prakash, Singh Prashant Kumar, Sivonda Anna, Skirbekk Vegard, Skogen Jens Christoffer, Sligar Amber, Sliwa Karen, Soljak Michael, Søreide Kjetil, Sorensen Reed J D, Soriano Joan B, Sposato Luciano A, Sreeramareddy Chandrashekhar T, Stathopoulou Vasiliki, Steel Nicholas, Stein Dan J, Steiner Timothy J, Steinke Sabine, Stovner Lars, Stroumpoulis Konstantinos, Sunguya Bruno F, Sur Patrick, Swaminathan Soumya, Sykes Bryan L, Szoeke Cassandra E I, Tabarés-Seisdedos Rafael, Takala Jukka S, Tandon Nikhil, Tanne David, Tavakkoli Mohammad, Taye Bineyam, Taylor Hugh R, Ao Braden J Te, Tedla Bemnet Amare, Terkawi Abdullah Sulieman, Thomson Alan J, Thorne-Lyman Andrew L, Thrift Amanda G, Thurston George D, Tobe-Gai Ruoyan, Tonelli Marcello, Topor-Madry Roman, Topouzis Fotis, Tran Bach Xuan, Truelsen Thomas, Dimbuene Zacharie Tsala, Tsilimbaris Miltiadis, Tura Abera Kenay, Tuzcu Emin Murat, Tyrovolas Stefanos, Ukwaja Kingsley N, Undurraga Eduardo A, Uneke Chigozie Jesse, Uthman Olalekan A, van Gool Coen H, Varakin Yuri Y, Vasankari Tommi, Venketasubramanian Narayanaswamy, Verma Raj Kumar, Violante Francesco S, Vladimirov Sergey K, Vlassov Vasiliy Victorovich, Vollset Stein Emil, Wagner Gregory R, Waller Stephen G, Wang Linhong, Watkins David A, Weichenthal Scott, Weiderpass Elisabete, Weintraub Robert G, Werdecker Andrea, Westerman Ronny, White Richard A, Williams Hywel C, Wiysonge Charles Shey, Wolfe Charles D A, Won Sungho, Woodbrook Rachel, Wubshet Mamo, Xavier Denis, Xu Gelin, Yadav Ajit Kumar, Yan Lijing L, Yano Yuichiro, Yaseri Mehdi, Ye Pengpeng, Yebyo Henock Gebremedhin, Yip Paul, Yonemoto Naohiro, Yoon Seok-Jun, Younis Mustafa Z, Yu Chuanhua, Zaidi Zoubida, Zaki Maysaa El Sayed, Zeeb Hajo, Zhou Maigeng, Zodpey Sanjay, Zuhlke Liesl Joanna, Murray Christopher J L. Oct;2016 The Lancet. 388(10053):1545–1602. doi: 10.1016/s0140-6736(16)31678-6. doi: 10.1016/s0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Lily H., Vail Daniel, Azad Tej D., Bentley Jason P., Zhang Yi, Ho Allen L., Fatemi Paras, Feng Austin, Varshneya Kunal, Desai Manisha, Veeravagu Anand, Ratliff John K. JAMA Network Open. 5. Vol. 2. American Medical Association (AMA); Expenditures and health care utilization among adults with newly diagnosed low back and lower extremity pain; p. e193676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirdelfan Kasra, Webster Lynn, Poree Lawrence, Sukul Vishad, McRoberts Porter. Spine. 14. Vol. 42. Ovid Technologies (Wolters Kluwer Health); Treatment options for failed back surgery syndrome patients with refractory chronic pain: An evidence based approach; pp. S41–S52. [DOI] [PubMed] [Google Scholar]
- Prevalence, characteristics, and burden of failed back surgery syndrome: The influence of various residual symptoms on patient satisfaction and quality of life as assessed by a nationwide Internet survey in Japan. Inoue Shinsuke, Kamiya Mitsuhiro, Nishihara Makoto, Arai Young-Chang P., Ikemoto Tatsunori, Ushida Takahiro. Apr;2017 Journal of Pain Research. 10:811–823. doi: 10.2147/jpr.s129295. doi: 10.2147/jpr.s129295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuijpers T., van Middelkoop M., Rubinstein S. M., Ostelo R., Verhagen A., Koes B. W., van Tulder M. W. European Spine Journal. 1. Vol. 20. Springer Science and Business Media LLC; A systematic review on the effectiveness of pharmacological interventions for chronic non-specific low-back pain; pp. 40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opioid Overdose. Centers for Disease Control and Prevention; https://www.cdc.gov/drugoverdose/index.html [Google Scholar]
- American osteopathic association guidelines for osteopathic manipulative treatment (OMT) for patients with low back pain. Snow R J, Seffinger M A, Hensel K L, Wiseman R. Aug 1;2016 The Journal of the American Osteopathic Association. 116(8):536. doi: 10.7556/jaoa.2016.107. doi: 10.7556/jaoa.2016.107. [DOI] [PubMed] [Google Scholar]
- Diagnosis and management of sacroiliac joint dysfunction. Ou-Yang David C., York Philip J., Kleck Christopher J., Patel Vikas V. Dec 6;2017 Journal of Bone and Joint Surgery. 99(23):2027–2036. doi: 10.2106/jbjs.17.00245. doi: 10.2106/jbjs.17.00245. [DOI] [PubMed] [Google Scholar]
- Coats T., Dong X. SI Joint Pain. PM Knowledge Now. AAPMR; https://now.aapmr.org/si-joint-pain/ [Google Scholar]
- Seffinger M. Foundations of Osteopathic Medicine. Wolters Kluwer; [Google Scholar]
- Somatic dysfunction: An osteopathic conundrum. Fryer Gary. Dec;2016 International Journal of Osteopathic Medicine. 22:52–63. doi: 10.1016/j.ijosm.2016.02.002. doi: 10.1016/j.ijosm.2016.02.002. [DOI] [Google Scholar]
- DeStefano L.A. Greenman's principles of manual medicine. In: Greenman's Principles of Manual Medicine. Wolters Kluwer; Philadelphia: pp. 472–473. [Google Scholar]
- Diagnosing sacroiliac joint pain. Thawrani Dinesh P., Agabegi Steven S., Asghar Ferhan. Feb;2019 Journal of the American Academy of Orthopaedic Surgeons. 27(3):85–93. doi: 10.5435/jaaos-d-17-00132. doi: 10.5435/jaaos-d-17-00132. [DOI] [PubMed] [Google Scholar]
- Sacroiliac joint pain: Burden of disease. Cher Daniel, Polly David, Berven Sigurd. Apr;2014 Medical Devices: Evidence and Research. 7:73. doi: 10.2147/mder.s59437. doi: 10.2147/mder.s59437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignoring the sacroiliac joint in chronic low back pain is costly. Polly David, Cher Daniel. Jan;2016 ClinicoEconomics and Outcomes Research. 8:23. doi: 10.2147/ceor.s97345. doi: 10.2147/ceor.s97345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The impact of sacro-iliac joint dysfunction in the management of low back pain and failed back surgery syndrome. Landi Alessandro, Grasso Giovanni, Mancarella C, Delfini R. 2016Journal of Spine. 5(4) doi: 10.4172/2165-7939.1000321. doi: 10.4172/2165-7939.1000321. [DOI] [Google Scholar]
- Prevalence of sacroiliac joint dysfunction and sacroiliac pain provocation tests in people with low back pain. Ramírez C., Sanchez L., Oliveira B. Jul;2018 Annals of Physical and Rehabilitation Medicine. 61:e152. doi: 10.1016/j.rehab.2018.05.343. doi: 10.1016/j.rehab.2018.05.343. [DOI] [Google Scholar]