Abstract
Background:
Traumatic abdominal wall hernia (TAWH) in children is an uncommon injury and most commonly occurs following blunt abdominal trauma. There is no consensus on the management of these rare cases. We performed a systematic review of the literature to describe injuries, management, and outcomes.
Materials and Methods:
Following PRISMA guidelines, a systematic literature search of PubMed, Web of Science, Embase, and Google Scholar was performed to identify English-language publications of blunt TAWH in patients <18 years old. Conflicts were resolved by consensus. Data were collected on demographics, associated injuries, management, and outcomes.
Results:
A total of 71 articles were reviewed with 100 cases of TAWH. 82.5% of patients were male and the median age was 9 (range 2–15). Injury by bicycle handlebar was most common (72%) followed by motor vehicle collision (MVC, 14%). Forty patients had intraabdominal injuries, most commonly bowel (70%) or mesentery (37.5%). Rate of intraabdominal injury was significantly higher in patients with injuries due to non-bicycle handlebar injuries when compared to bicycle handlebar injuries (60.7% vs. 33.3%, p=0.02). Most patients were managed operatively (85%), most commonly via laparotomy (68/85, 80%), with six laparoscopic repairs and five laparoscopic converted to open repairs. There were three reported complications and no recurrences over a median of follow up of 5 months in patients who underwent repair.
Conclusions:
Pediatric traumatic abdominal wall hernia is a rare injury with a high rate of intraabdominal injuries, particularly when due to high-impact mechanisms such as MVC. Although open repair is more commonly performed, laparoscopic repair has been described with success. Recurrence rates appear low but follow up has been short-term.
Keywords: pediatric trauma, abdominal wall hernia, traumatic hernia, TAWH, systematic review
Introduction
Traumatic abdominal wall hernia (TAWH) most commonly occurs following blunt abdominal wall trauma. The injury consists of disruption of the layers of the abdominal wall with overlying skin remaining intact. Intraabdominal contents, such as small bowel, may herniate through the defect1. The first TAWH described in the literature occurred in an adult injured by a wheelbarrow handle in 19062, but the first pediatric TAWH was not described until 19563, in a 14-year old boy who was hit in the abdomen by the handles of a motorbike. TAWH in children is a rare injury4, and most commonly is reported after direct abdominal wall trauma by bicycle handlebar impact5,6 but has also been seen following motor vehicle collision (MVC) with lap belt restraints7. In one large retrospective review of nearly 10,000 pediatric trauma patients who sustained blunt abdominal trauma, the incidence of TAWH was only 0.1%4, which is similar to that found in adult trauma patients8.
Due to its rarity, reports of pediatric TAWH are found only in case reports and small case series, the largest of which described only eleven cases over an eleven-year period. Prior literature reviews have focused primarily on TAWH due to bicycle handlebar injuries, but there have been several cases of TAWH due to higher energy mechanisms such as MVCs4,9. The management of pediatric blunt TAWH, including methods of abdominal access and hernia repair, is not standardized owing to its rarity. In addition, post-operative outcomes, including complications and hernia recurrence are not well known. Although TAWH is uncommon in pediatric patients, as trauma is the leading cause of morbidity and mortality in children and adolescents10, a better understanding of this injury will aid in its timely detection and management.
We performed a systematic review of the literature to identify cases of pediatric blunt traumatic abdominal wall hernia and to characterize demographics, associated injuries, management, and post-operative outcomes.
Material and Methods
Literature Search
With the assistance of a reference librarian, a systematic literature search of PubMed, Web of Science, Embase, and Google Scholar was performed by two authors to identify English-language publications of traumatic abdominal wall hernia in patients < 18 years old published through November 2020. The key words used as search terms included “traumatic abdominal wall hernia,” “abdominal wall hernia,” and “handlebar hernia.” No other filters, including publication date range, were applied. No attempt was made to obtain information about unpublished studies. The protocol is based on the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) checklist for the reporting of systematic reviews. For a full description of the search terms used please see Supplemental Digital Content 1: Systematic Review Search Strategy.
Publications of any type, including case reports, case series, prospective observational studies, and randomized controlled trials evaluating children with traumatic abdominal wall hernias were included. The abstracts of all studies were reviewed and screened independently by two investigators using the Covidence software tool (Covidence, Veritas Health Innovation, Melbourne, Australia). Conflicts were resolved by consensus. Article full texts were then independently screened by two reviewers, and conflicts were resolved by consensus to generate the final list of included studies. Inclusion criteria were English-language publications describing blunt traumatic abdominal wall hernias in patients < 18 years old. Exclusion criteria were ≥ 18 years old, non-English language publications, non-traumatic abdominal wall hernias (i.e. congenital or acquired ventral hernias), or injuries from penetrating trauma. Additionally, if pediatric patients were not described separately from adult patients the study was excluded.
Data Extraction
Data extracted included study design, number of patients reported, demographics, mechanism of injury, diagnostic evaluations, associated intraabdominal injuries, operative or non-operative management of the TAWH, details of operative repair, post-operative complications, and hernia recurrence. Additional details on patient management from Hafezi et al were obtained by correspondence with the authors4.
Statistical Analysis
Descriptive statistics were performed. Continuous data are presented as median and interquartile range (IQR) and categorical data are presented as number and percentage. Rates of intraabdominal injuries were compared by mechanism of injury using Fisher’s exact test. Statistical significance was set at p < 0.05. Analyses were performed using statistical software (Prism for Mac, version 9.00; GraphPad software, San Diego, California).
Results
Article Selection
A total of 254 articles were analyzed for inclusion by systematic database searching. After removing duplicates (n = 60), 194 articles underwent title and abstract screening. One hundred seventeen articles were excluded, and 77 full-text articles were assessed for eligibility. Twelve studies were excluded, and six additional articles were included from manual search of references. Thus, 71 articles reporting 100 cases of blunt pediatric TAWH were included in this systematic review (Figure 1). The full list of included citations is available in Supplemental Table 1.
Figure 1: Systematic Review flowsheet of article inclusion and exclusion.
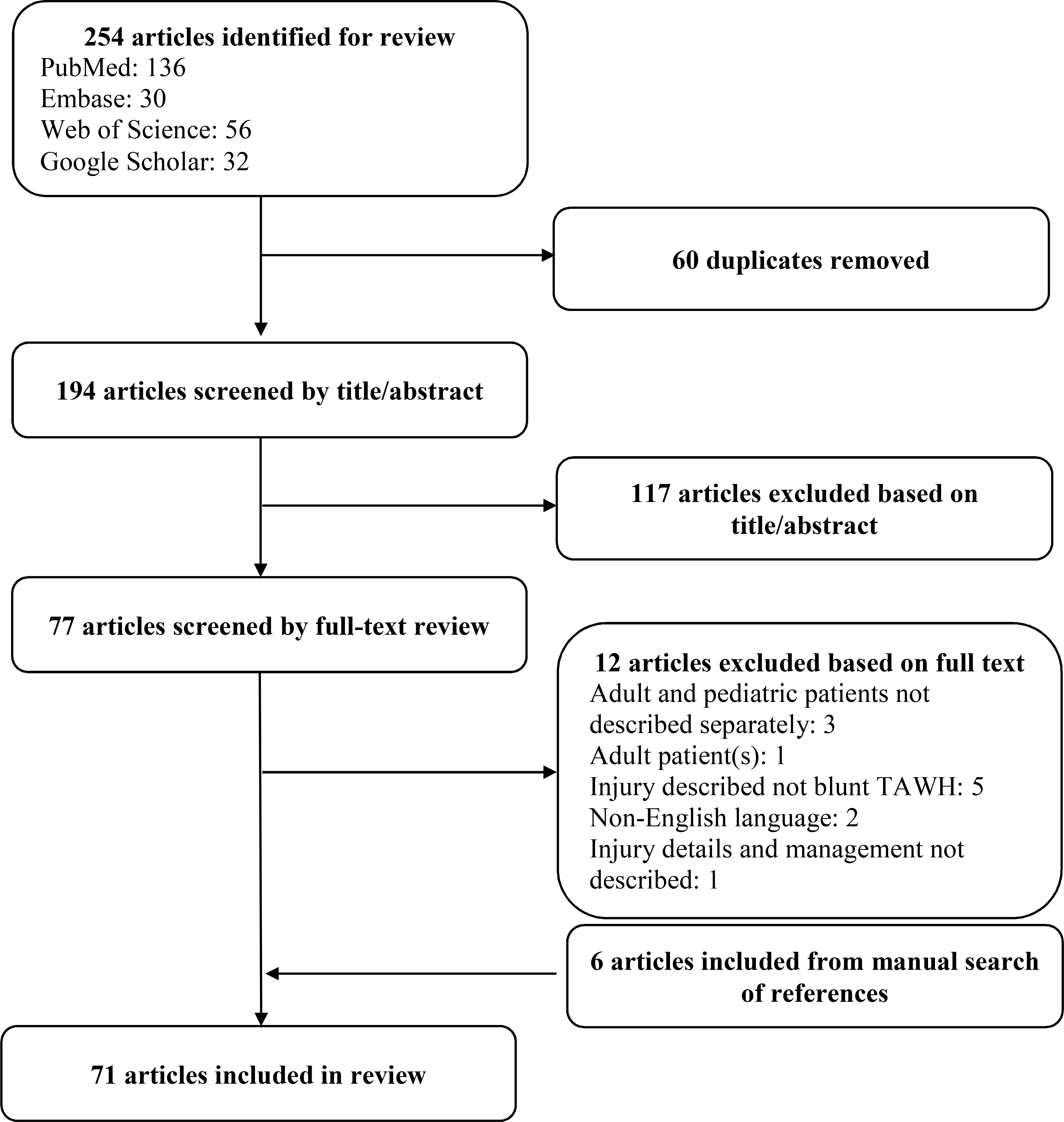
TAWH: traumatic abdominal wall hernia.
Article Characteristics
Although the first report of a blunt pediatric trauma abdominal wall hernia was published in 19563, the majority of included articles were published within the past ten years (2010–2020, n = 41, 57.7%), followed by 2000–2009 (n = 15, 21.1%) (Figure 2). The most common country represented was the United States, with 22 publications (31.0%), followed by the United Kingdom (n = 8, 11.3%), India (n = 6, 8.5%), Turkey and Italy (n = 5, 7.0% each). Most countries had only one article published (n = 14, 19.7%). The articles included were case reports (n = 58, 81.7%) and case series (n = 13, 18.3%).
Figure 2: Publications on Pediatric TAWH Over Time by Decade.
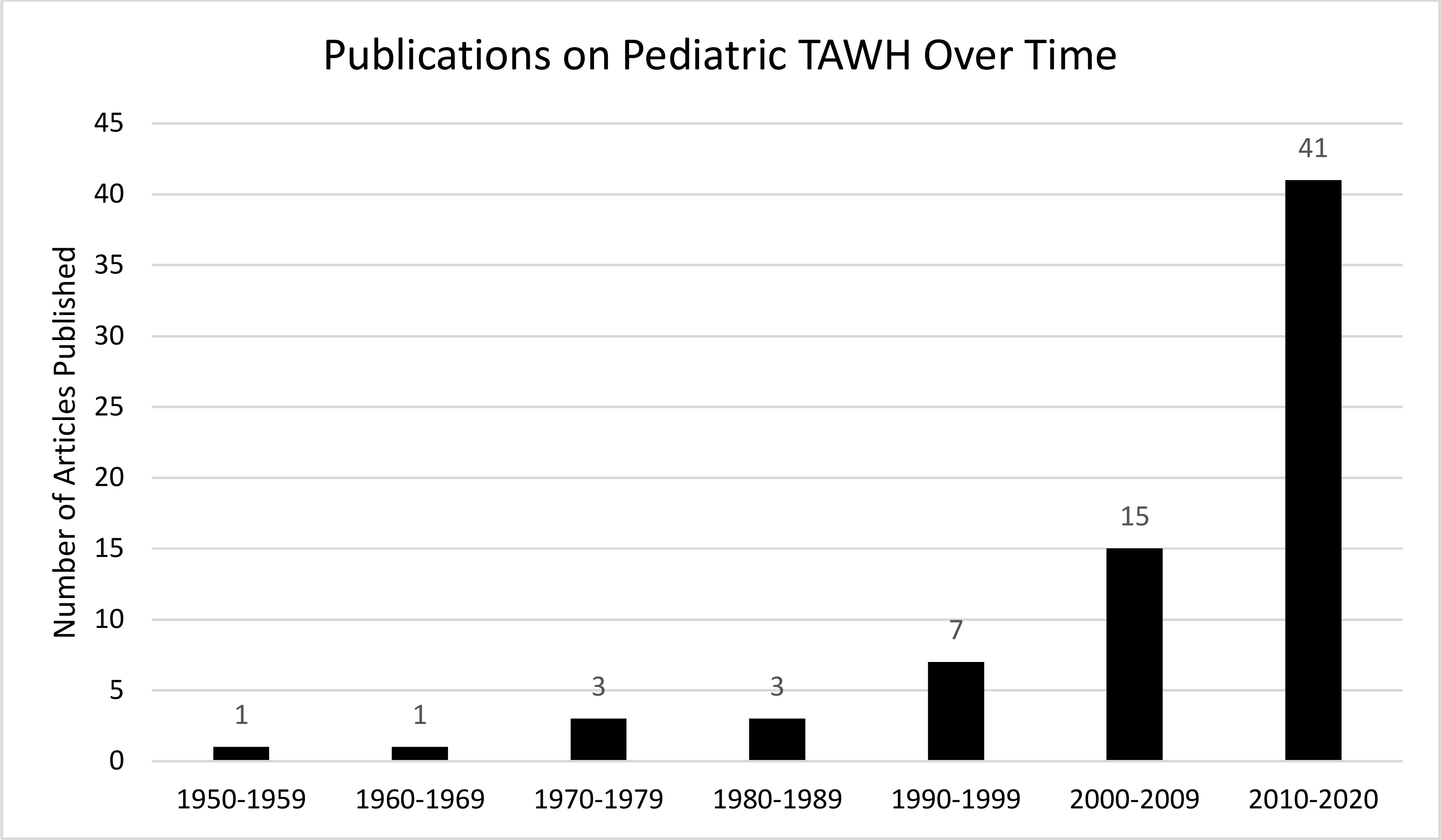
TAWH: Traumatic abdominal wall hernia.
Patient Demographics and Injury Characteristics
Most patients were male (n = 81/100) and the median age was 9 years old (IQR 7–12; range 2–15). The most common mechanism of injury was injury by bicycle or motorbike handlebars (n = 72/100), followed by injury in a motor vehicle collision (MVC, n = 14/100) and being hit by a vehicle (Ped vs. auto, n = 8/100) (Table 1). Less common injury mechanisms included impalement by a pole4,11 or animal horn12 without breaking the skin (n = 3), crush injuries13,14 (n = 2), and one all-terrain vehicle (ATV) accident14.
Table 1:
Mechanisms of injury
| Mechanism | Number of patients |
|---|---|
| Bicycle or motorbike handlebar | 72 |
| Motor vehicle collision | 14 |
| Pedestrian or bicyclist struck by vehicle | 8 |
| Impalement (without breaking skin) | 3 |
| Crush injury | 2 |
| All-terrain vehicle accident | 1 |
Presenting symptoms were reported for 90 patients. The most common reported symptom was abdominal wall ecchymosis or abrasions (62/90, 68.9%). An abdominal wall bulge or swelling was present in 55 patients (55/90, 61.1%). Of these, four were non-reducible. Sixteen patients had a palpable fascial defect on exam (16/90, 17.8%).
Diagnostic work-up
Patients most commonly underwent computed tomography scans (CT, n = 59) and ultrasound examinations (US, n = 30). Fourteen patients had both CT and US imaging performed. Nineteen patients were reported to have abdominal radiographs performed, and of these, six also had CT or US performed. One patient had magnetic resonance imaging performed14 and one patient underwent a barium enema1. Seventeen patients were reported to have no imaging performed4,12,15–21. Nine patients did not have information available on imaging performed.
Of the 19 patients who had abdominal radiographs performed, ten were reported to be normal. Seven displayed findings concerning for TAWH such as pockets of air or abnormal gas shadows in the subcutaneous tissues22–26, or air-filled loops of bowel anterior to the sternum1,13. Two did not show TAWH but had abnormal findings such as dilated loops or bowel or gastric dilation. Of the 30 patients who had US performed, eight were read as normal, including one patient who had a repeat study 24 hours later that showed a TAWH6. Eighteen ultrasounds showed evidence of definite or likely TAWH, resulting in a sensitivity of 60.0% (18/30). Four of the 30 US were abnormal but did not show TAWH; instead, they reported free fluid (n = 2), abdominal wall hematoma (n = 1), or abdominal wall mass (n = 1). The vast majority of CT scans performed showed TAWH (55/59), resulting in a sensitivity of 93.2%. In two cases, TAWH was not reported on two CT scans but was evident on retrospective review of the images4, which would increase the sensitivity to 96.6%. In one case, CT was obtained to evaluate for associated intraabdominal injury following an ultrasound which showed TAWH, and interestingly the CT did not show evidence of TAWH27.
The modality which ultimately resulted in diagnosis was evident in 95 cases. Diagnosis was made by CT in 46 patients, on physical exam in 25 patients, on ultrasound in 12 patients, and intraoperatively in 8 patients. Abdominal radiographs revealed the diagnosis in two patients, and MRI and barium enema in one patient each. Of the 25 patients who had a TAWH diagnosed on exam, 16 (16/25, 64%) had subsequent imaging performed, seven underwent operative repair without imaging, and two were managed non-operatively.
The timing of TAWH diagnosis was reported in 92 cases. In 81 cases (81/92, 88.0%), the diagnosis was made immediately upon presentation. However, this included four cases in which patients presented to the healthcare system in a delayed manner, ranging from 1–4 days post-injury28–31. Eleven cases had delays in diagnosis, ranging from 2 hours to 5 weeks after injury (Table 2). Two patients had delayed diagnoses at 2 and 3.5 hours post-presentation respectively, and both developed worsening abdominal pain resulting in repeat imaging which diagnosed isolated TAWH in one case32 and TAWH with pneumoperitoneum in the other33. Three patients had diagnoses delayed by 24 hours, in all cases the diagnosis was made due to worsening abdominal pain resulting in repeat imaging: two had TAWH diagnosed on repeat imaging6,23, while one had negative repeat imaging and underwent laparoscopy which identified the TAWH34. In one case, the TAWH was missed during laparotomy for management of concurrent IAI, and was not diagnosed until 13 days after injury when a subcutaneous swelling developed, which was thought to be a post-operative abscess until incision and drainage revealed fecal matter due to herniated bowel through a missed abdominal wall defect35.
Table 2: Patients with Delayed TAWH Diagnosis.
US: ultrasound; TAWH: traumatic abdominal wall hernia; CT: computed tomography; Ped vs Auto: pedestrian struck by vehicle; I&D: incision and drainage.
| Article | Age | Mechanism | Presentation | Initial Imaging | Diagnostic Delay | Findings prompting diagnosis |
|---|---|---|---|---|---|---|
| Atiemo12 | 6 | Cow horn | Abdominal wall bulge, small fascial defect | None | 48 hours | Increasing size of bulge |
| Bosemani33 | 11 | Handlebar | Abdominal bruise | US: possible TAWH | 2 hours | Worsening pain prompted CT which showed free air |
| Everett35 | 5 | Ped vs Auto | Polytrauma | X-Ray, laparotomy for other injuries | 13 days | I&D of flank swelling revealed fecal matter |
| Fraser23 | 11 | Handlebar | Abdominal abrasions | None | 24 hours | Abdominal bulge developed, X-ray and US showed TAWH |
| Iinuma34 | 8 | Handlebar | Abdominal ecchymosis | None | 24 hours | Worsening pain, CT without TAWH. Diagnosed on laparoscopy |
| Iuchtman36 | 7 | Handlebar | Abdominal ecchymosis | Normal US | 48 hours | Abdominal bulge developed, which prompted surgical intervention |
| Persano37 | 6 | Handlebar | No abdominal symptoms | None | 8 days | Developed abdominal bulge, US showed TAWH |
| Prada Arias6 | 6 | Handlebar | Abdominal bulge without fascial defect palpated | Normal US | 10 days | Planned follow-up exam revealed fascial defect; US showed TAWH |
| 10 | Handlebar | Abdominal ecchymosis | Normal US | 24 hours | Abdominal bulge developed, US showed TAWH | |
| Rinaldi32 | 12 | Handlebar | Abdominal pain | Normal US | 3.5 hours | Worsening of abdominal pain prompted CT which showed TAWH |
| Thakur38 | 9 | Handlebar | Initially developed abdominal bulge and ecchymosis but was not diagnosed with TAWH by local physician | None | 5 weeks | Presented again to new hospital 5 weeks after injury with reducible abdominal bulge, US showed TAWH |
Management
The vast majority of patients (n = 85) underwent operative repair of the TAWH. Thirteen patients underwent non-operative management, including one patient who underwent laparotomy for repair of associated injuries but did not have their TAWH repaired due to difficulty in identifying it without additional dissection7 (Table 3). One patient underwent attempted elective TAWH repair at 4 months post-injury but the procedure was aborted due to significant scar tissue4. Two patients did not have management method reported.
Table 3: Patients with TAWH Managed Non-Operatively.
TAWH: traumatic abdominal wall hernia; MRI: magnetic resonance imaging; US: ultrasound; CT: computed tomography; MVC: motor vehicle collision; NS: not stated; IAI: intraabdominal injury. Additional details on patient management obtained from Hafezi et al4 to complete this table.
| Article | Age | Mechanism | Presenting Details | Outcome |
|---|---|---|---|---|
| Aggelidou39 | 6 | Handlebar | 3 days after injury presented with reducible hernia | Repeat MRI and US at 2 weeks and 6 weeks showed <2 mm hernia. |
| Hafezi4 | 11 | MVC | Presented as transfer 2 weeks post injury, planned elective repair | Unable to repair hernia at 4 month planned repair due to scar tissue. Asymptomatic at 8 months without hernia on exam. |
| 9 | MVC | Hypotensive with peritonitis, diagnosed on CT after damage control laparotomy. | Hernia persists on imaging at 3 months but asymptomatic. | |
| 7 | Handlebar | Diagnosed on CT, went to OR after worsened abdominal exam. Had TAWH with amputated appendix, hernia left unrepaired due to contamination. | Asymptomatic at 1 month, US at 3 months showed no hernia. | |
| Karaman5 | NS | Handlebar | Reducible hernia with 4×2 cm fascial defect | Defect resolved by 1.5 months, no recurrence at 3 months. |
| Litton40 | 13 | Handlebar | Reducible hernia | Planned elective repair but hernia reduced at 1 month, not present on CT 4 months later |
| Matsuo41 | 9 | Handlebar | Reducible hernia with 3cm fascial defect | Treated with abdominal binder. Bulge disappeared by 3 weeks, CT 3 months later without hernia |
| Moremen7 | 13 | MVC | TAWH with bowel herniation. | Underwent laparotomy for IAI; peritoneal opening of TAWH unable to be easily identified so not repaired. Resolved on exam 3 months later. |
| Talutis14 | 4 | Crush | TAWH without IAI | MRI 1 month later with no hernia. Asymptomatic at 1 year. |
| Bar-Maor42 | 5 | MVC | Reducible hernia with 4 cm fascial defect | Planned repair 3 weeks later but resolved without intervention. No recurrence at 2 months. |
| Upasani43 | 12 | Handlebar | TAWH on CT | Resolved by 5 months, US with defect <5 mm. |
| Volpe44 | 8 | Handlebar | TAWH on US with 15 mm defect | Decrease in size at 1, 6, and 12 months to 3 mm defect. |
| 12 | Handlebar | TAWH on exam with 1 cm fascial defect | No defect palpable 2 months later, US showed 3 mm defect without herniation. |
Of the 85 patients who had operative repair of the TAWH, most were repaired via laparotomy (n = 68/85, 80.0%), five underwent laparoscopy converted to laparotomy14,34,45 (5/85, 5.9%), and six underwent laparoscopic repair27,32,46–49 (6/86, 7.1%). Six did not have the operative approach reported (6/85, 7.1%). All laparoscopic or laparoscopic converted to open repairs were published in 2005 or later. Most patients underwent primary suture repair of the hernia (n = 69/85, 81.2%). Mesh was utilized in four cases7,28,50,51 (4/85, 4.7%), including one case in which biologic mesh was used due to concurrent bowel resection7. Method of hernia repair was not reported in twelve cases (13/85, 15.3%).
Intraabdominal Injury
Overall, 57 patients had an isolated TAWH with no associated intraabdominal injury (IAI). Forty patients had associated IAI. Three patients did not have enough information provided to determine if IAI was present. The most common type of IAI was injury to the small bowel or colon (n = 28/40, 70.0%), followed by injuries to the mesentery and omentum (n = 15/40, 37.5%) (Table 4). Taken together, injuries to the bowel, mesentery, or omentum occurred in 32 patients (32%). Many patients had multiple injuries.
Table 4: Types of intraabdominal injuries sustained.
Note that multiple patients had multiple intraabdominal injuries.
| Intraabdominal injury | Number of patients |
|---|---|
| Small bowel or colon | 28 |
| Mesentery or omentum | 15 |
| Solid organ injury (liver, spleen, or kidney) | 3 |
| Genitourinary injury (bladder, ureter, or urethra) | 3 |
| Pancreas | 2 |
| Rectum | 1 |
| Traumatic diaphragmatic hernia | 1 |
Intraabdominal injury was most common in children who were injured in MVCs (9/14, 64.3%) or pedestrian vs. automobile accidents (4/8, 50%). When comparing rates of IAI in patients for whom presence of absence of IAI was reported (excluding those without sufficient information to determine both mechanism and presence of IAI, n = 6), children with TAWH from handlebar injuries had a lower rate of IAI (23/69, 33.3%) when compared to all other mechanisms grouped together (MVC, pedestrian vs. automobile, impalement, crush injury, and ATV injury: 17/28, 60.7%, p = 0.02).
Complications and Recurrences
There were three reported post-operative complications. One patient developed a superficial surgical site incision requiring bedside incision and drainage and intravenous antibiotics52. One patient presented one month after TAWH repair with a small bowel obstruction which resolved non-operatively53. One patient developed an incisional seroma which resolved without intervention30. There were no reported hernia recurrences in the included cases. The median duration of follow-up was five months; follow-up duration was reported for 38 patients.
Discussion
In this systematic review of 71 articles describing 100 pediatric patients with blunt traumatic abdominal wall hernia, we found that most (72%) were injured by direct impact of bicycle or motorbike handlebars. Despite the likely lower energy mechanism of bicycle handlebar impacts, one-third of these patients had a concurrent intraabdominal injury. Patients injured by higher energy mechanisms had a much higher rate of IAI, 68.0%. Thus, in patients who are diagnosed with TAWH due to blunt trauma, physicians must have a high degree of suspicion for IAI. As most (70%) of the IAI were bowel injuries, pediatric trauma providers should have a low threshold for surgical exploration to rule out IAI in patients with concerning clinical presentations. In patients not undergoing immediate surgery, serial abdominal exams should be performed to evaluate for the development of peritonitis. Although TAWH in the literature were most commonly managed via laparotomy, laparoscopic repair has become more prevalent in recent years, and may allow for accurate diagnosis of IAI, with the potential for minimally invasive TAWH repair while avoiding the morbidity of a laparotomy. Although non-operative management was reported in a minority of cases, the length of follow-up was short, and long-term outcomes are not known.
Overall, TAWH is a rare diagnosis. Abdominal wall injuries (AWI) in general, which range from contusions to frank evisceration, have been reported to occur in 3.6% of blunt trauma patients8. Grade V AWI, defined as complete abdominal wall disruption with resulting herniation of intraabdominal contents, was even less common, found in 0.07% - 0.24% of blunt trauma patients8,54. In children, blunt TAWH are most frequently due to abdominal trauma from bicycle handlebar impact. This is in contrast to adults, where TAWH most frequently occurs following MVC54. In a large series of 80 adolescents and adults from a single center, bowel and mesentery injuries occurred in 36% of patients, which is similar to the rate in the literature of 32% of pediatric TAWH cases included in this review. The rate of TAWH repair in the adolescent and adult series was much lower (23/80, 28.8%) than in the pediatric literature presented here (85%). However, this may be due to publication bias toward case reports of patients with TAWH requiring operative repair.
Pediatric providers caring for these patients have several decisions to make. In the pediatric patient with blunt abdominal trauma, a palpable hernia with fascial defect may be detected on physical exam. Although the diagnosis was evident in 25 patients on exam in this review, 16 patients had subsequent imaging performed to confirm the diagnosis prior to operative intervention. Thus, only seven patients in the literature underwent operative intervention based on physical exam findings alone. Although in some cases, abdominal radiography revealed subcutaneous bowel herniation13,26, X-rays were frequently non-diagnostic. Ultrasound and CT scans were more commonly obtained, with many showing fascial disruption and TAWH. The sensitivity of CT scans was much higher than that of ultrasounds (93.2% vs. 53.3%). Thus, in the pediatric patient with blunt abdominal trauma and symptoms concerning for TAWH, a negative US cannot be used to reliably rule out the diagnosis of TAWH. This is highlighted by the fact that nearly half of the patients with delayed diagnoses in the literature had initial normal abdominal US imaging. Cross-sectional imaging has the additional advantage of being able to identify concurrent IAI which may guide management of the patient but may miss injuries such as bowel injury4. In patients with high suspicion for TAWH, abdominal ultrasound by a skilled sonographer is reasonable first step, but if negative, we recommend that patients be observed for signs of IAI or undergo CT scan for more definitive diagnosis.
The management of pediatric TAWH is not standardized, as it is a rare injury. However, we found that most cases reported repairing the hernia, as opposed to conservative management. Although we found that TAWH is most commonly repaired via laparotomy, laparoscopic repair is becoming increasingly more common, and was reported in 11% of TAWHs in the literature. There were no complications reported with laparoscopic repair. Pediatric surgeons are more likely than adult trauma surgeons to choose laparoscopy rather than laparotomy in the injured child55 and approximately one-third of pediatric trauma patients requiring surgical intervention undergo laparoscopy56,57. In the stable patient, we recommend diagnostic and potentially therapeutic laparoscopy, with the option to convert to an open approach if needed. When possible, primary repair is the most commonly used method for hernia repair. If the defect requires bridging, mesh may be used, with the choice of synthetic or biologic mesh dictated by the presence or absence of concurrent IAI. Although there were no recurrences noted in the literature, this may be due to publication bias. It should be noted that in a series of 23 adolescent and adult trauma patients undergoing TAWH repair (n = 16 via primary repair, n = 7 via mesh repair), the recurrence rate was 26% (n = 6), and all were in patients who had a mesh repair54. Non-operative management of the TAWH was chosen for 13% of patients in the literature reported here, and all but one had no evidence of concurrent IAI. In the one patient with IAI, although laparotomy was required to address the other injuries, the hernia was not able to be repaired at the time of this index surgery and resolved on follow-up. In all cases, the patients were followed by serial exams or imaging, with the hernias either resolving or remaining asymptomatic. Thus, in select patients with asymptomatic reducible TAWH and without intraabdominal injury, non-operative management may be pursued, but close follow-up is required.
This systematic review of the literature has several limitations. There is likely publication bias, with cases with favorable outcomes more likely to be published, which is potentially responsible for the low rate of post-operative complications and the lack of reported recurrences. The duration of follow up was short term, and long-term outcomes of pediatric TAWH are unknown. Additionally, all included cases were either case reports or case series, and there have been no randomized clinical trials on the management of pediatric TAWH, nor are there likely to be in the future. Due to this heterogeneity, not all included variables were available in each article. We have been transparent when the denominator of a given finding is less than the total number of cases reported. By summarizing the available literature on pediatric blunt TAWH we have provided a knowledge base which may be used to guide surgical decision making in these rare cases.
Conclusion
Pediatric blunt traumatic abdominal wall hernia is a rare diagnosis, with high rates of intraabdominal injury (IAI). One-third of patients injured by bicycle handlebars had IAI compared to 68% of patients injured by other, higher energy mechanisms. CT is the most common diagnostic modality, with a sensitivity of 93.2% in the literature. Repair may be done via laparotomy or laparoscopy, and the hernia is most commonly repaired primarily. Non-operative management may be an option in select cases.
Supplementary Material
Acknowledgements:
The authors would like to acknowledge Nicole Capdarest-Arest for assistance with literature searches for this review.
Funding Information:
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 for author C.M.T. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Declarations of Interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Ciftci AO, Salman B, Turken A, Senocak ME. Acute Blunt Traumatic Abdominal Hernia. J Pediatr Surg. 1997;32(12):1732–1734. [DOI] [PubMed] [Google Scholar]
- 2.Selby CD. Direct Abdominal Hernia of Traumatic Origin. JAMA. 1906;XLVII(18):1485–1486. [Google Scholar]
- 3.Landry RM. Traumatic Hernia. Am J Surg. 1956;91:301–302. [DOI] [PubMed] [Google Scholar]
- 4.Hafezi N, Raymond JL, Mayo ED, Rouse TM, Billmire DF, Gray BW. Traumatic abdominal wall hernias in children: A case for early exploration. J Pediatr Surg. 2020. doi: 10.1016/j.jpedsurg.2020.06.046 [DOI] [PubMed] [Google Scholar]
- 5.Karaman I, Karaman A, Aslan MK, Erdoǧan D, Çavuşoǧlu YH, Tütün Ö. A hidden danger of childhood trauma: Bicycle handlebar injuries. Surg Today. 2009;39(7):572–574. doi: 10.1007/s00595-008-3931-3 [DOI] [PubMed] [Google Scholar]
- 6.Prada Arias M, Dargallo Carbonell T, Estévez Martínez E, Bautista Casasnovas A, Varela Cives R. Handlebar hernia in children: Two cases and review of the literature. Eur J Pediatr Surg. 2004;14(2):133–136. doi: 10.1055/s-2004-815863 [DOI] [PubMed] [Google Scholar]
- 7.Moremen JR, Nakayama DK, Ashley DW, Astin M, Nolan TL. Traumatic disruption of the abdominal wall: Lap-belt injuries in children. J Pediatr Surg. 2013;48(4):e21–e24. doi: 10.1016/j.jpedsurg.2013.02.039 [DOI] [PubMed] [Google Scholar]
- 8.Dennis RW, Marshall A, Deshmukh H, et al. Abdominal wall injuries occurring after blunt trauma: incidence and grading system. Am J Surg. 2009;197(3):413–417. doi: 10.1016/j.amjsurg.2008.11.015 [DOI] [PubMed] [Google Scholar]
- 9.Theodorou CM, Galganski LA, Stark RA. Traumatic posterolateral abdominal wall hernia in a pediatric patient. J Pediatr Surg Case Reports. 2019;43:23–25. doi: 10.1016/j.epsc.2019.01.013 [DOI] [Google Scholar]
- 10.Mclaughlin C, Zagory JA, Fenlon M, et al. Timing of Mortality in Pediatric Trauma Patients: A National Trauma Databank Analysis. J Pediatr Surg. 2019;53(2):344–351. doi: 10.1016/j.jpedsurg.2017.10.006.Timing [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmed LS. Traumatic abdominal wall hernia (TAWH): A case report and literature review. AAJMS. 2020;3(2):91–99. [Google Scholar]
- 12.Atiemo EA, Goswami G. Traumatic Ventral Hernia. J Trauma. 1974;14(2):181–182. [DOI] [PubMed] [Google Scholar]
- 13.Kiliç N, Balkan E, Kiriştioǧlu I, Güney N, Doǧruyol H. Abdominal wall ruptured by blunt trauma in a child. Eur J Surg. 2000;166(3):265–266. doi: 10.1080/110241500750009393 [DOI] [PubMed] [Google Scholar]
- 14.Talutis SD, Muensterer OJ, Pandya S, McBride W, Stringel G. Laparoscopic-assisted management of traumatic abdominal wall hernias in children: Case series and a review of the literature. J Pediatr Surg. 2015;50(3):456–461. doi: 10.1016/j.jpedsurg.2014.10.020 [DOI] [PubMed] [Google Scholar]
- 15.Dreyfuss DC, Flancbaum L, Krasna IH, Tell B, Trooskin SZ. Acute trans-rectus Traumatic Hernia. J Trauma. 1986;26(12):1134–1136. [DOI] [PubMed] [Google Scholar]
- 16.Kubalak G Handlebar Hernia: A Case Report and Review of the Literature. J Trauma. 1994;36(3):438–439. [PubMed] [Google Scholar]
- 17.Mitchell PJ, Green M, Ramesh AN. Handlebar hernia in children. Emerg Med J. 2011;28(5):439–440. doi: 10.1136/emj.2009.089870 [DOI] [PubMed] [Google Scholar]
- 18.Perez VM, McDonald AD, Ghani A, Bleacher JHO. Handlebar hernia: A rare traumatic abdominal wall hernia. J Trauma,Injury, Infect Crit Care. 1998;44(3). [DOI] [PubMed] [Google Scholar]
- 19.Roberts GR. Traumatic Abdominal Wall Rupture. Br J Surgery1. 1964;51:153–154. [DOI] [PubMed] [Google Scholar]
- 20.Tianyi FL, Agbor VN, Njim T. Motorbike-handlebar hernia - A rare traumatic abdominal wall hernia: A case report and review of the literature. J Med Case Rep. 2017;11(1):3–6. doi: 10.1186/s13256-017-1245-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Bemmel AJM, Van Marle AGJ, Schlejen PM, Schmitz RF. Handlebar hernia: A case report and literature review on traumatic abdominal wall hernia in children. Hernia. 2011;15(4):439–442. doi: 10.1007/s10029-010-0665-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chowdhury TK, Alam A, Rahman M, Khastagir R, Khan R. Traumatic Abdominal Wall Hernia. J Pediatr Surg Case Reports. 2020;59. [Google Scholar]
- 23.Fraser N, Milligan S, Arthur R, Crabbe D. Handlebar hernia masquerading as an inguinal haematoma. Hernia. 2002;6(1):39–41. doi: 10.1007/s10029-002-0051-7 [DOI] [PubMed] [Google Scholar]
- 24.Klimek PM, Lutz T, Stranzinger E, Zachariou Z, Kessler U, Berger S. Handlebar injuries in children. Pediatr Surg Int. 2013;29(3):269–273. doi: 10.1007/s00383-012-3227-y [DOI] [PubMed] [Google Scholar]
- 25.Quinn R, Jehangir S, Collin M, Soundappan SVS. Traumatic Abdominal Wall Hernias Following High-Velocity Trauma in Children. J Indian Assoc Pediatr Surg. 2020;25(3):169–171. doi: 10.4103/jiaps.JIAPS [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grover SB, Ratan SK. Simultaneous Dual Posttraumatic Diaphragmatic and Abdominal Wall Hernias. J Trauma. 2001;51(3):583–586. doi: 10.1097/00005373-200109000-00031 [DOI] [PubMed] [Google Scholar]
- 27.Bjork LB, Bellew SD, Kummer T. Point-of-care ultrasound diagnosis of traumatic abdominal wall hernia. Pediatr Emerg Care. 2017;33(5):367–369. doi: 10.1097/PEC.0000000000001126 [DOI] [PubMed] [Google Scholar]
- 28.Dhakre VW, Kadam SB, Gowda A, Iyer S. Handlebar sign: A bruise with underlying visceral injury. BMJ Case Rep. 2019;12(11):10–12. doi: 10.1136/bcr-2019-231835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hatti RB, Basarkod SI, Vishwanath G, Patil V. Handlebar hernias: Case reports of rare traumatic abdominal wall hernias. J Clin Diagnostic Res. 2011;5(4):826–827. [Google Scholar]
- 30.Mahmoud MEA. Traumatic Ventral Hypogastric Hernia: A Case Report and Review of Literature in Pediatrics. Acta Sci Paediatr. 2020;3(4):43–50. doi: 10.31080/aspe.2020.03.0239 [DOI] [Google Scholar]
- 31.Yaylaci S, Ercelik H, Seyit M, Kocyigit A, Serinken M. Handlebar trauma causing small bowel hernia with jejunal perforation. West J Emerg Med. 2014;15(4):367–368. doi: 10.5811/westjem.2014.4.22096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rinaldi VE, Bertozzi M, Magrini E, Riccioni S, Di Cara G, Appignani A. Traumatic Abdominal Wall Hernia in Children by Handlebar Injury: When to Suspect, Scan, and Call the Surgeon. Pediatr Emerg Care. 2017;00(00):1–4. doi: 10.1097/PEC.0000000000001153 [DOI] [PubMed] [Google Scholar]
- 33.Bosemani T, Huiseman T, Benson J, Tekes A. “Handlebar hernia”- CT findings and associated visceral injuries. Pediatr Radiol. 2011;41(Supplement 1):S342–343. [Google Scholar]
- 34.Iinuma Y, Yamazaki Y, Hirose Y, et al. A case of a traumatic abdominal wall hernia that could not be identified until exploratory laparoscopy was performed. Pediatr Surg Int. 2005;21(1):54–57. doi: 10.1007/s00383-004-1264-x [DOI] [PubMed] [Google Scholar]
- 35.Everett WG. Traumatic lumbar hernia. Injury. 1964;4(4):354–356. [DOI] [PubMed] [Google Scholar]
- 36.Iuchtman M, Kessel B, Kirshon M. Trauma-related acute spigelian hernia in a child. Pediatr Emerg Care. 1997;13(6):404–405. doi: 10.1097/00006565-199712000-00013 [DOI] [PubMed] [Google Scholar]
- 37.Persano G, Pinzauti E, Lo Piccolo R, Messineo A, Ghionzoli M. Traumatic Abdominal Wall Hernia. Indian J Pediatr. 2014;81(12):1409–1410. doi: 10.1007/s12098-014-1440-5 [DOI] [PubMed] [Google Scholar]
- 38.Thakur SK, Gupta S, Goel S. Traumatic Spigelian hernia due to handlebar injury in a child: A case report and review of literature. Indian J Surg. 2013;75(1 SUPPL.):404–406. doi: 10.1007/s12262-012-0734-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aggelidou M, Deftereos S, Foutzitzi S, Oikonomou P, Kambouri K. Handlebar hernia in children: a conservative approach. Case report and literature review. J Surg Case Reports. 2018:1–3. doi: 10.1093/jscr/rjy075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Litton K, Izzidien AY, Hussien O, Vali A. Conservative management of a traumatic abdominal wall hernia after a bicycle handlebar injury (case report and literature review). J Pediatr Surg. 2008;43(4):31–32. doi: 10.1016/j.jpedsurg.2007.12.059 [DOI] [PubMed] [Google Scholar]
- 41.Matsuo S, Okada S, Matsumata T. Successful conservative treatment of a bicycle-handlebar hernia: Report of a case. Surg Today. 2007;37(4):349–351. doi: 10.1007/s00595-006-3375-6 [DOI] [PubMed] [Google Scholar]
- 42.Bar-Maor JA, Sweed Y. Spigelian hernia in children, two cases of unusual etiology. Pediatr Surg Int. 1989;4(5):357–359. doi: 10.1007/BF00183407 [DOI] [Google Scholar]
- 43.Upasani A, Bouhadiba N. Paediatric abdominal wall hernia following handlebar injury: should we diagnose more and operate less? BMJ Case Rep. 2013:1–4. doi: 10.1136/bcr-2012-008501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Volpe A, Virgone C, Gamba P. Successful conservative management of handlebar hernia in children. Pediatr Int. 2017;59(1):105–106. doi: 10.1111/ped.13110 [DOI] [PubMed] [Google Scholar]
- 45.Picket D, Geiger J. Lap-Belt-Induced Pediatric Blunt Traumatic Abdominal Wall Hernia. Am Surg. 2017;83:189–191. [PubMed] [Google Scholar]
- 46.Lopez R, King S, Maoate K, Beasley S. Laparoscopic repair of paediatric traumatic Spigelian hernia avoids the need for mesh. ANZ J Surg. 2011;81(5):397–397. doi: 10.1111/j.1445-2197.2011.05719.x [DOI] [PubMed] [Google Scholar]
- 47.Pimpalwar A, Joseph J. Immediate laparoscopic repair of a traumatic abdominal wall hernia in a 2-year-old child. J Laparoendosc Adv Surg Tech. 2011;21(9):881–883. doi: 10.1089/lap.2011.0265 [DOI] [PubMed] [Google Scholar]
- 48.So HF, Nabi H. Handlebar hernia - A rare complication from blunt trauma. Int J Surg Case Rep. 2018;49:118–120. doi: 10.1016/j.ijscr.2018.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rowell EE, Chin AC. Laparoscopic repair of traumatic abdominal wall hernia from handlebar injury. J Pediatr Surg. 2011;46(5):e9–e12. doi: 10.1016/j.jpedsurg.2011.01.031 [DOI] [PubMed] [Google Scholar]
- 50.Mancel B, Aslam A. Traumatic abdominal wall hernia: An unusual bicycle handlebar injury. Pediatr Surg Int. 2003;19(11):746–747. doi: 10.1007/s00383-003-1064-8 [DOI] [PubMed] [Google Scholar]
- 51.Mezhir JJ, Glynn L, Lui DC, Statter MB. Handlebar Injuries in Children: Should We Raise the Bar of Suspicion? Am Surg. 2007;73:807–810. [PubMed] [Google Scholar]
- 52.Deepak J, Aravind KL, Shankar G, Narendrababu M. Bicycle Handlebar Injuries in Children: Is Ring Sign an Indicator of Intra-Abdominal Injuries? Indian J Child Heal. 2013;126(2009):834–838. doi: 10.3760/cma.j.issn.0366-6999.20122801 [DOI] [Google Scholar]
- 53.Theodorou CM, Galganski LA, Stark RA. Traumatic posterolateral abdominal wall hernia in a pediatric patient. J Pediatr Surg Case Reports. 2019;43. doi: 10.1016/j.epsc.2019.01.013 [DOI] [Google Scholar]
- 54.Coleman JJ, Fitz EK, Zarzaur BL, et al. Traumatic abdominal wall hernias: Location matters. J Trauma Acute Care Surg. 2016;80(3):390–397. doi: 10.1097/TA.0000000000000946 [DOI] [PubMed] [Google Scholar]
- 55.Butler EK, Groner JI, Vavilala MS, Bulger EM, Rivara FP. Surgeon choice in management of pediatric abdominal trauma. J Pediatr Surg. 2020;(xxxx). doi: 10.1016/j.jpedsurg.2020.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Train AT, Naseem HUR, Chen Z, et al. Predictors and outcomes of laparoscopy in pediatric trauma patients: A retrospective cohort study. J Laparoendosc Adv Surg Tech. 2019;29(12):1598–1604. doi: 10.1089/lap.2019.0322 [DOI] [PubMed] [Google Scholar]
- 57.Butler EK, Mills BM, Arbabi S, Groner JI, Vavilala MS, Rivara FP. Laparoscopy Compared With Laparotomy for the Management of Pediatric Blunt Abdominal Trauma. J Surg Res. 2020;251:303–310. doi: 10.1016/j.jss.2020.01.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


