Abstract
Objective:
Four decades ago the “controlled drinking” controversy roiled the alcohol field. Data have subsequently accumulated indicating that non-abstinent alcohol use disorder (AUD) recovery is achievable, but questions remain whether it is sustainable long-term. This study examined whether non-abstinent recovery at three years following AUD treatment is associated with better functioning at 10 years following treatment.
Methods:
Data were from the 10-year follow-up of Project MATCH (New Mexico site only, n=146; 30.1% female, 58.6% non-White). Recovery was defined by latent profile analyses based on psychosocial functioning and alcohol consumption three years following treatment. Drinking practices and consequences, depression, purpose in life, and anger were assessed 10 years following treatment. Distal outcome analyses examined differences in drinking and functional outcomes at 10 years as a function of the 3-year latent profiles. Analyses were pre-registered at https://osf.io/3hbxr.
Results:
Four latent profiles identified at three years following treatment (i.e., low functioning frequent heavy drinkers, low functioning infrequent heavy drinkers, high functioning heavy drinkers, and high functioning infrequent non-heavy drinkers) were significantly associated with outcomes ten years following treatment. The two high functioning profiles at three years had the highest level of psychological functioning at ten years post-treatment, regardless of alcohol consumption level. Abstinence at three years did not predict better psychological functioning at ten years.
Conclusions:
Non-abstinent AUD recovery is possible and is sustainable for up to 10 years following treatment. The current findings align with recent proposals to move beyond relying on alcohol consumption as a central defining feature of AUD recovery.
Keywords: alcohol use disorder, alcohol treatment, recovery, mixture models, Project MATCH
Introduction
Abstinence from alcohol remains a primary target in many treatment programs for alcohol use disorder (AUD)1–3 and in mutual help organizations such as Alcoholics Anonymous (AA). Achieving abstinence is associated with improvements in psychosocial functioning4,5 and lower risk of physical health problems6–8. However, some individuals also attempt to recover from AUD by reducing their alcohol use (i.e., moderation or controlled drinking), and a number of empirical studies demonstrate that reducing alcohol consumption is also associated with improvements in functioning and health9–12.
Recent conceptualizations of the term ‘recovery’ have shifted to emphasize the broader biopsychosocial process of improvement that is related to, but not solely determined by, alcohol consumption. As noted by Ashford and colleagues13, stakeholder institutions, including the American Society of Addiction Medicine (ASAM), have updated and modified their operational definitions of recovery over the past two decades. In 2005, ASAM’s public policy statement on recovery highlighted a state of psychological and physical health in which an individual’s abstinence from substance use was “complete and comfortable”14. A 2013 update to ASAM’s definition still mentions “an individual’s consistent pursuit of abstinence,” but does so in the context of “a process of sustained action that addresses biological, psychological, social, and spiritual disturbances,” including improvements in interpersonal relationships, behavioral control, and emotional responding15. Empirical support for a broader conceptualization of recovery has been reviewed in recent work16–18 and also expressed by individuals who self-identify as being in recovery19–21.
Consistent with expanding definitions of recovery, we recently conducted empirical investigations seeking to identify “recovery profiles” (i.e., subgroups) characterized by a range of both alcohol-related and psychosocial functioning measures. Using data from the outpatient arm of Project MATCH22, we found four profiles at three years following AUD treatment: (1) low functioning frequent heavy drinkers (15.8% of the sample), (2) low functioning infrequent heavy drinkers (16.1%), (3) high functioning heavy drinkers (16.9%), and (4) high functioning, infrequent, non-heavy drinkers (51.2%)23. These results suggest that abstinence may be a necessary recovery element for some individuals with AUD, but is not essential for all, and positive changes in functioning and well-being often are more fundamental elements.
Although this research adds to growing evidence that distinct longer term recovery profiles can be identified based on both alcohol-related outcomes and functioning indicators, important questions remain about whether these profiles forecast sustained positive outcomes over longer intervals. For example, do the individuals in the high functioning profiles—including those engaging in heavy drinking—maintain this level of functioning in subsequent years? A limited number of studies with follow-up intervals longer than three years suggest this is the case. For example, using follow-up data from the COMBINE Study24, we found that individuals who were high functioning at three years post-treatment, regardless of level of alcohol consumption, had the best self-reported health and fewer hospitalizations at 7–9 years post-treatment25. An observational study of individuals with AUD surveyed participants about their drinking practices, psychosocial functioning, and life contexts at baseline and 1, 3, 8, and 16 years later. Regardless of whether they had recently sought help or achieved abstinence, many participants showed improvement in alcohol-related functioning, life contexts, and coping26. Taken together, these studies may inform a longstanding debate in the field concerning the risks and stability of non-abstinent recovery9 and the utility of broader conceptualizations of recovery that emphasize improvements in biopsychosocial functioning16,17.
Current Study
The present study attempts to replicate and extend our recent work with the COMBINE Study24 by investigating the relationships between recovery profiles identified at three years following treatment and alcohol consumption and psychological functioning outcomes at ten years following treatment among a site-specific subset of participants involved in Project MATCH22. Importantly, this is an extension of our analyses with COMBINE25 to include a broader set of psychosocial functioning indicators, for a longer time period, and the analyses are conducted in a more diverse sample of participants. We hypothesized the recovery typologies characterized by high functioning heavy drinking and high functioning infrequent non-heavy drinking at three years following treatment23 would be associated with less drinking and higher psychological functioning at ten years following treatment when compared to recovery typologies characterized by low functioning frequent or infrequent heavy drinkers at three years following treatment.
Method
Participants and Procedure
The current study was a secondary data analysis of Project MATCH22, a randomized clinical trial comparing three psychosocial treatments for AUD: Cognitive Behavioral Therapy (CBT)27, Motivational Enhancement Therapy (MET)28, and Twelve-Step Facilitation (TSF)29. Participants who sought outpatient treatment from nine research centers in the United States (N=952) and provided drinking data at the 3-year follow-up assessment (n=806; 84.7% retention) were included in the latent profile analysis. Additionally, participants in the outpatient arm at the Albuquerque, New Mexico site (n=226) were invited to complete a 10-year follow-up assessment30. Of this subset, 149 provided data at the 10-year follow-up (66.4%) and 146 (64.6%) completed both the 3- and 10-year follow-up and were included in the present study. Table 1 provides descriptive statistics for the subset of participants who provided 3-year and 10-year follow-up data.
Table 1.
Descriptive Statistics for 10-Year Sample by 3-Year Latent Profile Membership (Analysis N=146)
| 10-Year Outcomes | Total Sample (N=146) |
Profile 1: Low Functioning Frequent Heavy Drinking (n=16) |
Profile 2: Low Functioning Infrequent Heavy Drinking (n=23) |
Profile 3: High Functioning Heavy Drinking (n=22) |
Profile 4: High Functioning Infrequent Drinking (n=85) |
|---|---|---|---|---|---|
| M (SD)/N (%) | M (SD) /N (%) | M (SD) /N (%) | M (SD) /N (%) | M (SD) /N (%) | |
| Percent drinking days | 24.83 (33.98) | 23.33 (36.64) | 25.07 (31.62) | 50.95 (42.51) | 18.45 (28.76) |
| Percent heavy drinking days | 14.85 (27.81) | 22.71 (36.23) | 17.25 (28.33) | 25.71 (35.31) | 9.60 (22.37) |
| Drinks per drinking day | 5.04 (7.81) | 5.33 (10.55) | 6.71 (8.13) | 7.66 (8.00) | 3.86 (6.89) |
| DrInC Total Score | 24.21 (30.07) | 36.69 (37.77) | 41.67 (38.80) | 29.52 (25.65) | 16.96 (24.57) |
| Beck Depression Inventory | 7.92 (8.02) | 10.81 (7.61) | 13.81 (8.32) | 9.43 (9.00) | 5.54 (6.80) |
| Purpose in Life | 103.82 (16.67) | 98.75 (15.17) | 91.24 (15.47) | 106.10 (16.50) | 106.71 (15.47) |
| State-Trait Anger Expression Inventory | 80.46 (13.30) | 79.25 (13.40) | 91.86 (18.64) | 84.67 (14.42) | 77.08 (9.43) |
| Demographics | |||||
| Age (Baseline) | 42.83 (8.59) | 43.38 (7.66) | 43.23 (7.41) | 44.00 (9.71) | 42.32 (8.83) |
| Sex (N, % Male) | 103(71.0%) | 11 (68.8%) | 12 (57.1%) | 14 (66.7%) | 63 (75.0%) |
| Marital status (N, % Married) | 45 (31.0%) | 4 (25.0%) | 6 (28.6%) | 7 (33.3%) | 28 (33.3%) |
| Race (N, % White) | 60 (41.4%) | 7 (43.8%) | 9 (42.9%) | 11 (52.4%) | 31 (36.9%) |
| 3-Year Latent Profile Indicators | |||||
| Percent drinking days | 27.80 (32.19) | 82.22 (14.34) | 27.72 (19.85) | 66.88 (25.30) | 7.69 (10.34) |
| Percent heavy drinking days | 16.23 (24.78) | 73.61 (19.10) | 15.82 (13.86) | 24.02 (16.52) | 3.45 (6.39) |
| Drinks per drinking day | 4.85 (5.70) | 12.72 (9.57) | 5.57 (4.75) | 5.49 (3.39) | 3.00 (3.80) |
| DrInC Total Score | 31.79 (27.26) | 62.50 (32.25) | 47.84 (24.89) | 34.10 (19.45) | 15.60 (14.75) |
| PFI social behavior subscale score | 3.39 (0.54) | 2.95 (0.63) | 2.84 (0.70) | 3.46 (0.31) | 3.60 (0.35) |
| Unemployed (N, % unemployed) | 21 (14.4%) | 2 (12.5%) | 5 (21.7%) | 2 (9.1%) | 12 (14.1%) |
| Depressed (N, % depressed) | 19 (13.0%) | 5 (31.3%) | 10 (43.5%) | 0 (0.0%) | 4 (4.7%) |
| Difficulty concentrating (N, % with difficulty) | 19 (13.0%) | 4 (25.0%) | 6 (26.1%) | 0 (0.0%) | 9 (10.6%) |
| Tension (N, % with tension) | 35 (24.0%) | 6 (37.5%) | 10 (43.5%) | 2 (9.1%) | 17 (20.0%) |
| Unhappy with living situation (N, % unhappy) | 26 (17.8%) | 8 (50.0%) | 13 (56.5%) | 3 (13.6%) | 2 (2.4%) |
| Unhappy with life (N, % unhappy) | 25 (17.1%) | 11 (68.8%) | 12 (52.2%) | 1 (4.5%) | 1 (1.2%) |
| Unhappy with relationships (N, % unhappy) | 30 (20.5%) | 12 (75.0%) | 12 (52.2%) | 1 (4.5%) | 5 (5.9%) |
| Unhappy with leisure activities (N, % unhappy) | 30 (20.5%) | 9 (56.3%) | 14 (60.9%) | 1 (4.5%) | 6 (7.1%) |
| Cannabis use (N, % with cannabis use) | 47 (32.2%) | 10 (62.5%) | 8 (34.8%) | 8 (36.4%) | 21 (24.7%) |
| Other drug use (N, % with other drug use) | 37 (25.3%) | 11 (68.8%) | 9 (39.1%) | 7 (31.8%) | 10 (11.8%) |
Note. DrInC=Drinker Inventory of Consequences; PFI=Psychosocial Functioning Inventory. Sample size (n) for each profile is based on the most likely class membership.
Measures
Measures were assessed at multiple time points including baseline, three years following treatment (39-months post-baseline), and ten years following treatment.
Three-Year Follow-Up Latent Profile Indicators
Alcohol and drug use were assessed with the Form-9031, a calendar-based tool determining alcohol and drug use in the previous 90 days. Summary alcohol use variables included percent drinking days (PDD), percent heavy drinking days (PHDD, i.e., 4+ drinks/day for women, 5+ drinks/day for men), and drinks per drinking day (DDD). Marijuana and other illicit drug use responses were summarized as binary (0=no use, 1=any use).
The Drinker Inventory of Consequences (DrInC)32 was utilized to assess negative alcohol-related consequences. Participants reported the regularity of 45 consequences on a 4-point scale (1=never, 4=daily or almost daily). Internal consistency of the DrInC for this sample was α=0.97.
The Psychosocial Functioning Inventory (PFI)33 was used to evaluate social functioning. The 10-item social behavior subscale from the PFI included items assessing the prevalence of problem social interactions and behaviors in the past 30 days (e.g., “Demanded others do things your way”); higher scores indicated better psychosocial functioning. Sample internal consistency of the PFI social behavior subscale was α=0.83. Additionally, we selected four items to measure life satisfaction and social functioning over the past 30 days with binary responses (0=satisfied/happy; 1=dissatisfied/unhappy). The internal consistency of these four items was α=0.79.
The Addiction Severity Index (ASI)34 was used to measure employment and experiences with affective or cognitive symptoms (e.g., “severe depression”) in the past 30 days with responses coded as binary (0=employed or symptom not present, 1=unemployed or symptom present). We examined four individual items given prior evidence of poor measurement properties of the ASI composites35. The internal consistency of the four items was α=0.63.
10-Year Follow-Up Outcomes
Different measures from the original Project MATCH study were assessed at the 10-year follow-up assessment, and only the Form-90 and DrInC were administered at both 3-year and 10-year follow-ups. The PFI and ASI were not administered at the 10-year follow-up.
The Form-9036 was utilized at the 10-year follow-up to assess alcohol use, including PDD, PHDD, and DDD. These variables represent alcohol use over the 30 days prior to the 10-year assessment.
The DrInC32 was also used to measure the frequency of 45 alcohol-related negative consequences over the three months prior to the 10-year follow-up assessment. At this assessment, internal consistency of the DrInC was α=0.98.
The Beck Depression Inventory (BDI)37 was utilized to assess 21 depression symptoms (rated from 0 to 3, representing the severity of each symptom) in the previous week. At the 10-year follow-up, the BDI demonstrated internal consistency of α=0.91.
The Purpose in Life (PIL) test38 was used to measure individuals’ sense of meaning or purpose in life, including items assessing life meaning, satisfaction, freedom, fear of death, suicidal ideation, and how worthwhile one’s life is. This 20-item questionnaire had an internal consistency of α=0.92 at the 10-year assessment.
The State-Trait Anger Expression Inventory (STAXI) assessed the expression of anger in situational contexts (state anger) and a predisposition toward anger (trait anger)39. The total score from the 44-item questionnaire was utilized in the present analysis, and the internal consistency was α=0.87.
Analytic Approach
Analyses for the current study were preregistered. Project documents and preregistration details can be found at https://osf.io/3hbxr (last accessed 6/16/2020). Latent profiles of drinking and functioning at the 3-year follow-up were derived using latent profile analysis in Mplus version 840. The latent profile models were estimated based on the entire Project MATCH outpatient sample who completed the 3-year follow-up assessment (n=806; 84.6% of the MATCH outpatient sample). As detailed by Witkiewitz et al.23, we used a weighted maximum likelihood function and estimated variance-covariance matrix for all available 3-year data (n=806). Model fit was examined using the Lo Mendell Rubin Likelihood Ratio test (LRT), Bayesian Information Criterion (BIC), and sample-size–adjusted BIC (aBIC). Classification precision was defined using relative entropy, where entropy greater than .80 indicated good classification precision41.
Distal Outcomes at 10-Year Follow-Up
To examine differences in latent profiles on functioning at 10 years following treatment, we conducted latent profile analyses with the manual 3-step Bolck, Croons, and Hagenaars (BCH) approach42–44 to assess whether the latent profiles at the 3-year follow-up were associated with distal outcomes of alcohol consumption, alcohol consequences, and psychosocial functioning at the 10-year follow-up. Of the Albuquerque outpatient sample that was consented to the 10-year follow-up (n=193), 149 had data at the 10-year follow-up (66.4%) and 146 (64.6%) completed both the 3- and 10-year follow-up, and were included in the distal outcomes analysis. Latent profile models at the 3-year follow-up were estimated in this subsample and differences in distal outcomes at 10 years as a function of latent profile membership at 3 years were evaluated using a Wald χ2 test with paired t-tests for pairwise profile comparisons. Cohen’s d statistic, which reflects standardized mean differences in outcomes (i.e., differences between groups in standard deviation units), was also calculated. A priori power analyses, using a Monte Carlo simulation, indicated power to detect distal outcome effects (i.e., mean differences in 10-year outcomes) by profile membership at 10 years was greater than 0.63 to detect medium effect sizes and we had power greater than 0.97 to detect large effect sizes.
Sensitivity Analyses.
Attrition analyses (t-tests for continuous measures and χ2 tests for categorical measures) were used to explore differences in the baseline and 3-year follow-up assessments among those with complete data at the 10-year follow-up (n=149) versus those who did not complete the 10-year follow-up (n=43). We also examined whether there were differences in latent profiles at the 3-year assessment and completion of the 10-year follow-up assessment. Additional analyses were conducted, which were not preregistered, to examine differences in 10-year outcomes among those who were or were not abstinent at the 3-year follow-up. Mean differences were examined using Wald χ2 tests with t-tests for individual outcome comparisons. Cohen’s d statistics were also calculated comparing abstainers to non-abstainers.
Results
Latent Profiles at the 3-Year Follow-Up
As reported previously23, the four-profile model at the three-year follow-up was selected based on BIC, aBIC, and LRT statistics, and the model classification precision was excellent in the total sample23 (entropy=0.92) and among those with 10 year follow-up data (entropy=0.97). The profiles were substantively meaningful and were labeled “low functioning frequent heavy drinking” (profile 1; 15.8% of the sample), “low functioning infrequent heavy drinking” (profile 2; 16.1%, “high functioning heavy drinking” (profile 3; 16.9%), and “high functioning infrequent non-heavy drinking” (profile 4; 51.2%). None of the individuals with expected classification in profile 1 or profile 3 were abstinent. Of those with expected classification in profile 4, 48.9% were abstinent from alcohol; and of those with expected classification in profile 2, 26.9% were abstinent from alcohol.
Distal Outcomes at the 10-Year Follow-Up
Table 1 provides descriptive statistics for distal outcomes by latent profile membership, which differed significantly at the 10-year follow-up (Wald χ2 (24)=133.85, p < 0.001). Figure 1 depicts alcohol consumption and alcohol-related consequences at the 10-year follow-up among individuals with expected classification in profiles 1–4, respectively. Pairwise comparisons indicated that those in profile 4 (high functioning infrequent non-heavy drinking) had significantly fewer consequences on the DrInC, as compared to all other profiles (all p<0.04), and significantly fewer drinks per drinking day (t(1)=−4.25, p=0.04), percent drinking days (t(1)=−36.37, p=0.001), and percent heavy drinking days (t(1)=−17.82, p= 0.04), as compared to profile 3 (high functioning heavy drinking). Profile 3 also reported significantly greater percent drinking days, as compared to profile 1 (t(1)=31.76, p=0.02) and profile 2 (t(1)=29.19, p=0.02). We also examined abstinence status at the 10-year follow-up by latent profile membership at 3 years and found that 62.5% of individuals in profile 1, 39.1% of individuals in profile 2, 19.0% of individuals in profile 3, and 50.0% of individuals in profile 4 were abstinent in the month preceding the 10-year follow-up assessment.
Figure 1. Drinking outcomes ten years following treatment as a function of latent profile membership three years following treatment.
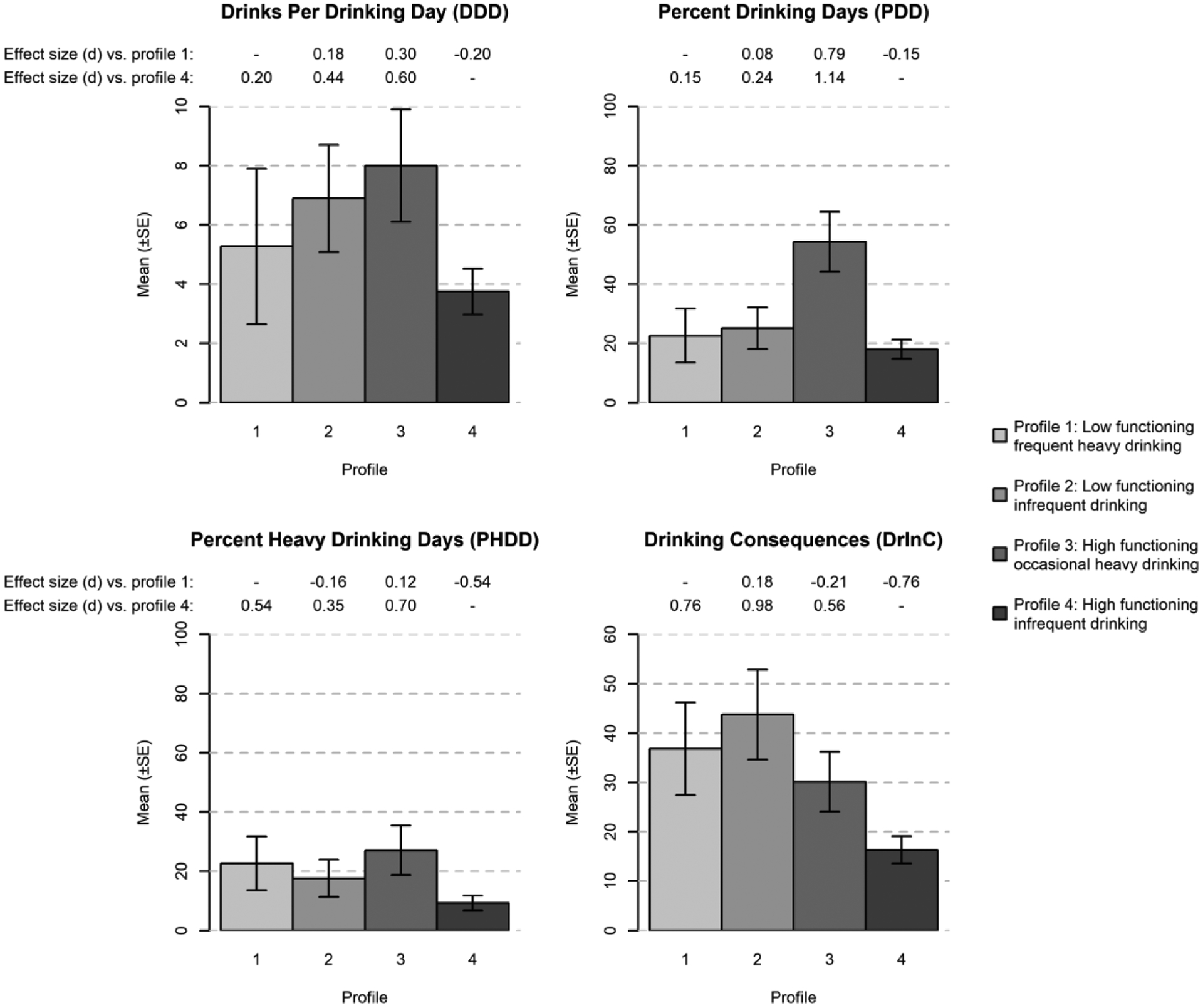
Note. Standard errors indicated by error bars. Cohen’s d standardized mean differences shown between profiles using profile 1 (low functioning frequent heavy drinking) and profile 4 (high functioning infrequent drinking) as reference groups.
At 10-year follow-up (Figure 2), profiles 3 and 4 had significantly greater purpose in life, as compared to profile 2 (all ps < .002). Profile 4 had significantly lower depression than profile 1 (t(1)=−5.53, p=0.007) and profile 2 (t(1)=−9.22, p < 0.001), but did not significantly differ from profile 3 (t(1)=−4.31, p=0.06). Profile 4 also had significantly less anger than profile 3 (t(1)=−8.62, p=0.02) and profile 2 (t(1)=−16.69, p < 0.001), and profile 2 had significantly more anger than profile 1 (t(1)=14.21, p= 0.01).
Figure 2. Functioning outcomes ten years following treatment as a function of latent profile membership three years following treatment.
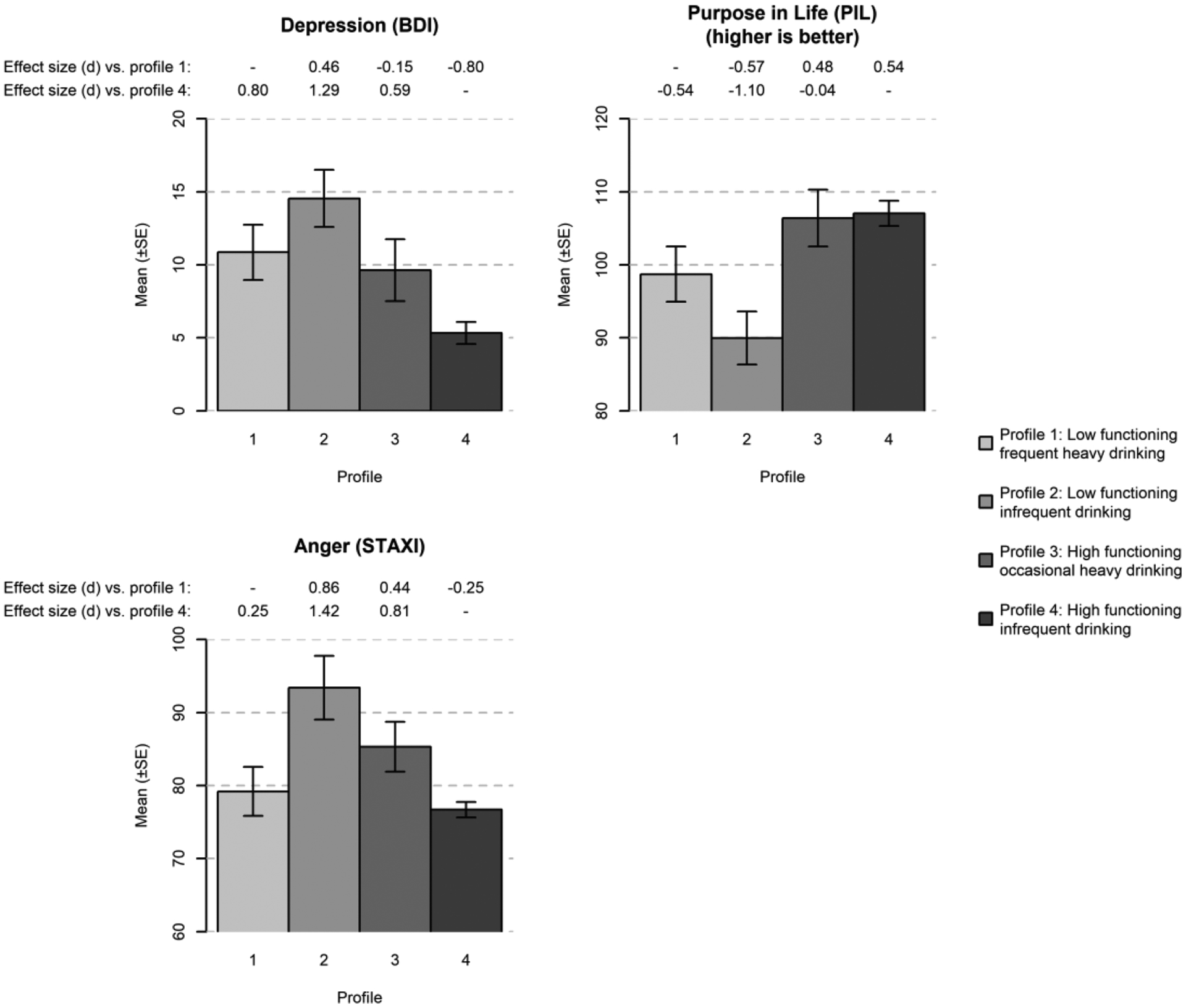
Note. Standard errors indicated by error bars. Cohen’s d standardized mean differences shown between profiles using profile 1 (low functioning frequent heavy drinking) and profile 4 (high functioning infrequent drinking) as reference groups.
Sensitivity Analyses
Attrition analyses indicated no significant differences on any study variables (alcohol consumption, consequences, or psychosocial functioning) at baseline or at the 3-year follow-up between those who did (n=149) and did not complete (n=43) the 10-year follow-up. There were also no differences in 3-year latent profile membership among the Albuquerque subsample who were eligible for, but did not complete, the 10-year follow-up (n=47; χ2(3)=1.554, p=.670).
Additional analyses were conducted to examine mean outcome differences at the 10-year follow-up among those who were (n=33) and were not abstinent (n=113) at the 3-year follow-up. Significant differences in distal outcomes were found between groups at the 10-year follow-up (Wald χ2 (7)=20.79, p=0.004). Supplementary Figures 1 and 2 illustrate the differences in mean outcomes (with standard errors indicated by error bars) and Cohen’s d standardized mean differences between abstainers and drinkers. Abstainers at the 3-year follow-up reported significantly lower percent heavy drinking days (t (1)=−11.04, p=0.01), percent drinking days (t (1)=−19.02, p < 0.001), and drinking consequences (t (1)=−12.68, p=0.02) at the 10-year follow-up, but did not differ on any of the other psychological functioning outcomes (all ps > .13).
Discussion
As hypothesized, the two highest functioning profiles at three years following treatment (profile 3 and 4) generally had the best psychological functioning outcomes, including greater purpose in life and lower levels of depression, at ten years following treatment. These findings support the clinical validity of the recovery profiles and reaffirm the importance of considering indicators of psychological functioning, and not simply alcohol consumption levels, when defining long-term recovery from AUD. Indeed, our findings revealed a lack of a one-to-one correspondence between drinking behavior and psychological functioning during the process of recovery over time. Abstinence three years following treatment did not predict better functioning ten years following treatment. Rather, functioning at three years following treatment (profiles 3 and 4) predicted better psychological functioning at ten years following treatment. As recently proposed, focusing on functioning rather than drinking practices per se may be more useful when defining successful AUD recovery and forecasting how an individual will fare over the long run4,13,16,17,45. Our quantitative findings using a clinical treatment sample also are aligned with research indicating that functional outcomes, including quality of life and well-being, are highly valued among persons who self-identify as being in recovery20,21.
An important finding was that profile 3, which was characterized by occasional heavy drinking three years following treatment, generally showed favorable psychological functioning at both the three-year and ten-year follow-ups. For example, compared to low functioning profiles 1 and 2, membership in profile 3 was associated with significantly higher purpose in life at year 10, whereas depression symptoms and purpose in life were similar in high functioning profiles 3 and 4. These findings are consistent with our prior work demonstrating that heavy drinking itself may not predict psychological functioning among individuals with AUD4,45–47. Overall, study findings support and extend a growing body of literature that suggests that abstinence is not the only path to achieve and/or sustain a high level of psychosocial functioning in the years following alcohol treatment. Rather, there appear to be multiple paths to recovery that can include moderate or heavy alcohol consumption post-treatment for some individuals16,23,25,48.
It is also important to note that profile 4 (high functioning, infrequent non-heavy drinking at year 3) had the best overall outcomes at year 10, despite the fact that some individuals in profile 4 had returned to some heavy drinking (average percent heavy drinking days of 10%) at year 10. Profile 4 had significantly lower anger, depression, and alcohol-related consequences, and greater purpose in life than profiles 1 and 2 and did not differ significantly from profile 3 on two important functioning outcomes at year 10 (i.e., depression and purpose in life). While individuals who achieved both high functioning and abstinence/non-heavy drinking (profile 4) at three years had optimal long-term outcomes as a whole, individuals who have a combination of high functioning and more frequent heavy drinking (profile 3) also showed favorable long-term outcomes in psychosocial functioning.
Some differences in ten-year drinking outcomes among recovery profiles at three years following treatment were somewhat unexpected. For instance, rates of abstinence at year 10 for profiles 1, 2, 3, and 4 were 62.5%, 39.1%, 19.0%, and 50.0%, respectively. It is quite possible that individuals in profile 1 (low functioning frequent heavy drinking at year 3) were not able to sustain frequent heavy drinking without significant negative consequences and thus were more likely to abstain at 10 years. Additionally, those in high functioning profile 3 reported the highest levels of drinks per drinking day, percent drinking days, and percent heavy drinking days at year 10 – but lower levels of drinking consequences at year 10 – relative to the two low functioning profiles (profiles 1 and 2). The high level of drinking in profile 3 at year 10 was also unexpected and the level of drinking among individuals in profile 3 could be associated with increased risk of serious alcohol-related health problems, alcohol toxicity, and accidental injury49.
Limitations and Future Directions
Several limitations should be considered when interpreting the present results. First, the current study examined profiles of recovery and long-term outcomes among an outpatient sample collected at one site over a decade ago, and findings may not generalize to inpatient or more contemporary samples. Replication in larger samples of individuals who received inpatient and outpatient treatment is warranted. Second, recovery is likely best conceptualized as a dynamic process of change17, and the present study only examined outcomes in a three-month timeframe ten years following AUD treatment. It did not assess behavior patterns and outcomes or capture other treatment that may have occurred during the 10 years following the Project MATCH treatment episode, and the extent of additional help-seeking across time is unknown. Third, all measures included in the study were self-reported, and collateral information from providers or family were not available. We also did not measure physical health, or medical outcomes at year 10, and we were not able to evaluate whether individuals who continued drinking heavily were at increased risk for physical health-related diseases6,49. Future studies should include additional indicators and outcomes, such as cognitive functioning, social functioning, employment and housing issues, chronic pain, medical comorbidities, and other substance use to advance our understanding of functioning following AUD treatment. Fourth, only a small subset of original participants in the outpatient arm of Project MATCH at the Albuquerque site were followed successfully over 10 years, and the extent to which the sample may be biased cannot be thoroughly ascertained. Nevertheless, alcohol consumption, consequences, and psychosocial functioning at baseline and at the 3-year follow-up did not differ significantly between participants who did (n=149) and did not complete (n=43) the 10-year follow-up.
With these qualifications, the present study adds to evidence that non-abstinent AUD recovery is possible and can be maintained for up to 10 years following treatment. The findings support recent proposals to move beyond viewing abstinence as a central defining feature of AUD recovery and relying heavily on quantity-frequency measures of drinking practices as the primary outcome indicator. Future research that expands the scope of outcome indicators to include measures of biopsychosocial functioning and AUD diagnostic criteria50 is important for advancing understanding of the multiple pathways to recovery from AUD. Additional research should examine whether remission from AUD diagnostic symptoms, which were not examined in the current study, are useful in defining recovery or whether focusing on well-being and psychological functioning is sufficient to characterize recovery from AUD.
Supplementary Material
Acknowledgments
Preparation of this manuscript was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism (R01 AA022328, 2K05 AA016928, K01 AA024796, K01 AA023233, and T32 AA018108).
Footnotes
The authors declare no conflicts of interest.
Contributor Information
Adam D. Wilson, University of New Mexico.
Corey R. Roos, Yale University.
J. Scott Tonigan, University of New Mexico.
Kevin A. Hallgren, University of Washington.
Kevin S. Montes, California State University Dominquez Hills.
Stephen A. Maisto, Syracuse University.
Jalie A. Tucker, University of Florida.
References
- 1.Davis AK, Rosenberg H, Rosansky JA. American counselors’ acceptance of non-abstinence outcome goals for clients diagnosed with co-occurring substance use and other psychiatric disorders. J Subst Abuse Treat. 2017;82:29–33. doi: 10.1016/j.jsat.2017.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenberg H, Davis LA. Acceptance of moderate drinking by alcohol treatment services in the United States. J Stud Alcohol. 1994;55(2):167–172. http://www.ncbi.nlm.nih.gov/pubmed/8189737.AccessedJuly 5, 2013. [DOI] [PubMed] [Google Scholar]
- 3.Davis AK, Rosenberg H. Acceptance of non-abstinence goals by addiction professionals in the United States.: Bulletin of the society of psychologists in addictive behaviors: Bulletin of the society of psychologists in substance abuse. Psychol Addict Behav. 2013;27(4):1102–1109. doi: 10.1037/a0030563 [DOI] [PubMed] [Google Scholar]
- 4.Wilson AD, Bravo AJ, Pearson MR, Witkiewitz K. Finding success in failure: using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction. 2016;111(12):2145–2154. doi: 10.1111/add.13518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maisto SA, Clifford P r., Longabauch R, Beattie M. The relationship between abstinence for one year following pretreatment assessment and alcohol use and other functioning at two years in individuals presenting for alcohol treatment. J Stud Alcohol. 2002;July:397–403. [DOI] [PubMed] [Google Scholar]
- 6.GBD 2016 Alcohol Collaborators MG, Fullman N, Hawley C, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10152):1015–1035. doi: 10.1016/S0140-6736(18)31310-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zemore SE, Lui C, Mericle A, Hemberg J, Kaskutas LA. A longitudinal study of the comparative efficacy of Women for Sobriety, LifeRing, SMART Recovery, and 12-step groups for those with AUD. J Subst Abuse Treat. 2018;88:18–26. doi: 10.1016/j.jsat.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Visser RO, Piper R. Short- and Longer-Term Benefits of Temporary Alcohol Abstinence During ‘Dry January’ Are Not Also Observed Among Adult Drinkers in the General Population: Prospective Cohort Study. Alcohol Alcohol. 2020. doi: 10.1093/alcalc/agaa025 [DOI] [PubMed] [Google Scholar]
- 9.Sobell MB, Sobell LC. The aftermath of heresy: A response to Pendery et al.’s (1982) critique of “Individualized behavior therapy for alcoholics.” Behav Res Ther. 1984;22(4):413–440. doi: 10.1016/0005-7967(84)90084-6 [DOI] [PubMed] [Google Scholar]
- 10.Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: Prevalence in two population surveys. Am J Public Health. 1996;86(7):966–972. doi: 10.2105/AJPH.86.7.966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheong JW, Lindstrom K, Chandler SD, Tucker JA. Utility of different dimensional properties of drinking practices to predict stable low-risk drinking outcomes of natural recovery attempts. Addict Behav. 2020;106:106387. doi: 10.1016/j.addbeh.2020.106387 [DOI] [PubMed] [Google Scholar]
- 12.Fan AZ, Chou SP, Zhang H, Jung J, Grant BF. Prevalence and correlates of past year recovery from DSM-5 alcohol use disorder: Results from National Epidemiologic Survey on Alcohol and Related Conditions-III. Alcohol Clin Exp Res. 2019;43(11):2406–2420. [DOI] [PubMed] [Google Scholar]
- 13.Ashford RD, Brown A, Brown T, et al. Defining and operationalizing the phenomena of recovery: a working definition from the recovery science research collaborative. Addict Res Theory. 2019;27(3):179–188. doi: 10.1080/16066359.2018.1515352 [DOI] [Google Scholar]
- 14.American Society of Addiction Medicine. Public Policy Statement on the State of Recovery. Chevy Chase, MD, USA; 2005. [Google Scholar]
- 15.American Society of Addiction Medicine. Terminology Related to Addiction, Treatment, and Recovery. Chevy Chase, MD, USA; 2013. [Google Scholar]
- 16.Witkiewitz K, Montes KS, Schwebel FJ, Tucker JA. What is recovery? A narrative review of definitions of recovery from alcohol use disorder. Alcohol Res Curr Rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Witkiewitz K, Tucker JA. Abstinence not required: Expanding the definition of recovery from alcohol use disorder. Alcohol Clin Exp Res. 2020;44(1):36–40. doi: 10.1111/acer.14235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neale J, Finch E, Marsden J, et al. How should we measure addiction recovery? Analysis of service provider perspectives using online Delphi groups. Drugs Educ Prev Policy. 2014;21(4):310–323. doi: 10.3109/09687637.2014.918089 [DOI] [Google Scholar]
- 19.Kaskutas LA, Borkman TJ, Laudet A, et al. Elements that define recovery: the experiential perspective. J Stud Alcohol Drugs. 2014;75(6):999–1010. doi: 10.15288/jsad.2014.75.999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kelly JF, Greene MC, Bergman BG. Beyond abstinence: Changes in indices of quality of life with time in recovery in a nationally representative sample of U.S. adults. Alcohol Clin Exp Res. 2018;42(4):770–780. doi: 10.1111/acer.13604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neale J, Vitoratou S, Finch E, et al. Development and validation of SURE: A patient reported outcome measure for recovery from drug and alcohol dependence. Drug Alcohol Depend. 2016;165:159–167. doi: 10.1016/j.drugalcdep.2016.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58(1):7–29. http://www.ncbi.nlm.nih.gov/pubmed/8979210.AccessedSeptember 27, 2013. [PubMed] [Google Scholar]
- 23.Witkiewitz K, Wilson AD, Pearson MR, et al. Profiles of recovery from alcohol use disorder at three years following treatment: Can the definition of recovery be extended to include high functioning heavy drinkers? Addiction. 2019;114(1):69–80. doi: 10.1111/add.14403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anton RF, O’Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–2017. doi: 10.1001/jama.295.17.2003 [DOI] [PubMed] [Google Scholar]
- 25.Witkiewitz K, Pearson MR, Wilson AD, et al. Can alcohol use disorder recovery include some heavy drinking? A replication and extension up to nine years following treatment. Alcohol Clin Exp Res. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moos RH, Moos BS. Sixteen-year changes and stable remission among treated and untreated individuals with alcohol use disorders. Drug Alcohol Depend. 2005;80(3):337–347. doi: 10.1016/j.drugalcdep.2005.05.001 [DOI] [PubMed] [Google Scholar]
- 27.Kadden RM, Carroll KM, Donovan DM, et al. Cognitive-Behavioral Coping Skills Therapy Manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. https://pubs.niaaa.nih.gov/publications/MATCHSeries3/ProjectMATCHVol_3.pdf. [Google Scholar]
- 28.Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivation Enhancement Therapy Manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1994. [Google Scholar]
- 29.Nowinski J, Baker S, Carroll KM. Twelve Step Facilitation Therapy Manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 30.Pagano ME, White WL, Kelly JF, Stout RL, Tonigan JS. The 10-year course of Alcoholics Anonymous participation and long-term outcomes: a follow-up study of outpatient subjects in Project MATCH. Subst Abus. 2013;34(1):51–59. doi: 10.1080/08897077.2012.691450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller WR, National Institute on Alcohol Abuse and Alcoholism. Form 90: A Structured Assessment Interview for Drinking and Related Behaviors (Test Manual), NIAAA Project MATCH Monograph Series, Vol. 5.; 1996. [Google Scholar]
- 32.Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC). An Instrument for Assessing Adverse Consequences of Alcohol Abuse. Test Manual. … MATCH Monogr Ser. 1995. [Google Scholar]
- 33.Feragne MA, Longabaugh R, Stevenson JF. The psychosocial functioning inventory. Eval Health Prof. 1983;6(1):25–48. doi: 10.1177/016327878300600102 [DOI] [PubMed] [Google Scholar]
- 34.McLellan AT, Kushner H, Metzger D, et al. The fifth edition of the addiction severity index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-S [DOI] [PubMed] [Google Scholar]
- 35.Mäkelä K Studies of the reliability and validity of the Addiction Seventy Index. Addiction. 2004;99(4):398–410. doi: 10.1111/j.1360-0443.2003.00665.x [DOI] [PubMed] [Google Scholar]
- 36.Miller WR. Form 90: A Structured Assessment Interview for Drinking and Related Behaviors. Project MA. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1996. [Google Scholar]
- 37.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77–100. doi: 10.1016/0272-7358(88)90050-5 [DOI] [Google Scholar]
- 38.Crumbaugh JC, Maholick LT. An experimental study in existentialism: The psychometric approach to Frankl’s concept of noogenic neurosis. J Clin Psychol. 1964;20(2):200–207. doi: [DOI] [PubMed] [Google Scholar]
- 39.Spielberger CD, Sydeman SJ. State-trait anxiety inventory and state-trait anger expression inventory. In: The Use of Psychological Testing for Treatment Planning and Outcome Assessment. ; 1994. [Google Scholar]
- 40.Muthén LK, Muthén BO. Mplus users guide (Version 8). 2019. [Google Scholar]
- 41.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Model. 2007;14(4):535–569. [Google Scholar]
- 42.Bolck A, Croon M, Hagenaars JA. Estimating latent structure models with categorical variables: One-step versus three-step estimators. Polit Anal. 2004;12(1):3–27. doi: 10.1093/pan/mph001 [DOI] [Google Scholar]
- 43.Nylund-Gibson K, Grimm RP, Masyn KE. Prediction from latent classes: A demonstration of different approaches to include distal outcomes in mixture models. Struct Equ Model A Multidiscip J. 2019;26(6):967–985. doi: 10.1080/10705511.2019.1590146 [DOI] [Google Scholar]
- 44.Yeo RA, Phillips JP, Jung RE, Brown AJ, Campbell RC, Brooks WM. Magnetic resonance spectroscopy detects brain injury and predicts cognitive functioning in children with brain injuries. J Neurotrauma. 2006;23(10):1427–1435. doi: 10.1089/neu.2006.23.1427 [DOI] [PubMed] [Google Scholar]
- 45.Maisto SA, Hallgren KA, Roos CR, Witkiewitz K. Course of remission from and relapse to heavy drinking following outpatient treatment of alcohol use disorder. Drug Alcohol Depend. 2018;187:319–326. doi: 10.1016/j.drugalcdep.2018.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tucker JA, Cheong J, James T, Jung S, Chandler SD. Pre-resolution drinking problem severity profiles associated with stable moderation outcomes of natural recovery attempts. Alcohol Clin Exp Res. 2020;44(3):738–748. doi: 10.1111/acer.14287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Witkiewitz K, Kirouac M, Roos CR, et al. Abstinence and low risk drinking during treatment: Association with psychosocial functioning, alcohol use, and alcohol problems 3 years following treatment. Psychol Addict Behav. 2018;32(6):639–646. doi: 10.1037/adb0000381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tucker JA, Chandler SD, Witkiewitz K. Epidemiology of recovery from alcohol use disorder. Alcohol Res Curr Rev. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rehm J, Gmel GE, Gmel G, et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction. 2017;112(6):968–1001. doi: 10.1111/add.13757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC, US: American Psychiatric Association; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


