Abstract
Mental and substance use disorders have been identified as the leading cause of global disability, and the global burden of mental illness is concentrated among those experiencing disability due to serious mental illness (SMI). Music has been studied as a support for SMIs for decades, with promising results; however, a lack of synthesized evidence has precluded increased uptake of and access to music-based approaches. The purpose of this scoping review was to identify the types and quantity of research at intersections of music and SMIs, document evidentiary gaps and opportunities, and generate recommendations for improving research and practice. Studies were included if they reported on music's utilization in treating or mitigating symptoms related to five SMIs: schizophrenia, bipolar disorder, generalized anxiety disorder, major depressive disorder, or post-traumatic stress disorder. Eight databases were searched; screening resulted in 349 included studies for data extraction. Schizophrenia was the most studied SMI, with bipolar disorder studied the least. Demographics, settings, and activity details were found to be inconsistently and insufficiently reported; however, listening to recorded music emerged as the most common musical activity, and activity details appeared to have been affected by the conditions under study. RCTs were the predominant study design, and 271 unique measures were utilized across 289 primary studies. Over two-thirds of primary studies (68.5%) reported positive results, with 2.8% reporting worse results than the comparator, and 12% producing indeterminate results. A key finding is that evidence synthesis is precluded by insufficient reporting, widely varied outcomes and measures, and intervention complexity; as a result, widespread changes are necessary to reduce heterogeneity (as feasible), increase replicability and transferability, and improve understandings of mechanisms and causal pathways. To that end, five detailed recommendations are offered to support the sharing and development of information across disciplines.
Keywords: mental health, scoping review, music, psychiatric illness, innovative treatment, music therapy, complex intervention, evidence synthesis
Introduction
Mental and substance use disorders have been identified as “the leading cause of disability globally” (Whiteford et al., 2016, n.p.), affecting one in every three to five individuals throughout their lives (see Steel et al., 2014; Vigo et al., 2016). Despite the high prevalence of these disorders, resources and effective treatment remain inconsistently available, with funders and policy makers “fail[ing] to prioritize treatment and care of people with mental illness” (Vigo et al., 2016). Indeed, according to Steel et al. (2014), “substantial evidence indicates the majority of people with mental disorder do not receive specialized services and that global resources allocated to the management of mental disorders is substantially lower than for other chronic health conditions” (p. 490)1. In response, health researchers and practitioners have increasingly called for policy changes and additional research to improve treatment, noting that the burden of mental illness will not be reduced without the identification of “more effective ways to provide sustainable mental health services, especially in resource constrained environments” (Whiteford et al., 2013).
In 2020, the need for improved treatment and access skyrocketed as a result of the COVID-19 pandemic. Psychological well-being was undermined by diagnoses and fear of infection (Duan and Zhu, 2020), the necessity of social isolation (Armitage and Nellums, 2020; Brooks et al., 2020), and job loss and subsequent economic hardship (Murthy et al., 2020; Panchal et al., 2020). Health care workers have experienced increased post-traumatic stress disorder (PTSD), stress, insomnia, and depressive symptoms as a result of their work and lack of adequate support (Choudhury et al., 2020; Greenberg, 2020; Spoorthy, 2020). In addition, COVID-19 has disproportionately affected low-income communities and communities of color (Farquharson and Thornton, 2020; Laurencin and McClinton, 2020), exacerbated by the fact that such communities have historically been excluded from access to—and the benefits of—adequate health resources. When combined with the disproportionate prevalence of mental health concerns in these same communities (Coleman et al., 2016, Kilbourne et al., 2018), the current crises make clear that the provision of quality mental health care—as well as policy changes, funding, and innovation to increase access and effectiveness—is an urgent priority for health and health equity.
Given this increasing urgency, it is imperative that mental health researchers and funders prioritize the study of innovative strategies that show promise not only of reducing or eliminating symptoms of mental illness, but also of preventing illness and supporting thriving and resilience. Notably, research and innovation in mental health should be targeted toward SMIs (serious mental illnesses), as “the burden of mental illness is…concentrated among those who experience disability due to SMI” (National Institute of Mental Health, 2019, n.p.). SMIs are defined as “mental, behavioral, or emotional disorder[s] resulting in serious functional impairment, which substantially interferes with or limits one or more major life activities” (National Institute of Mental Health, 2019, n.p.).
To support efforts toward improved and expanded options for addressing SMIs, this scoping review gathers and maps evidence regarding uses of music to treat or mitigate symptoms related to SMI. In doing so, it maps the current research landscape, answering the questions: What has been researched? How, and with what results? And what barriers and opportunities exist moving forward?
Music and Mental Health
For many decades, music has been utilized and studied as a support for mental health—with applications ranging from general mood elevation and stress reduction to clinical interventions designed to treat SMIs. Research indicates that music-based approaches to mental health care can increase patients' likelihood of accessing care2 (Schroeder, 2018; Fancourt and Finn, 2019) while reducing its costs (Aalbers et al., 2017). Studies also suggest that mental health treatments that incorporate music may advance health by delivering benefits long associated with arts exposure and participation, such as increased social connectivity (Kreutz, 2014; Welch et al., 2014; Fancourt et al., 2016), additional health-enhancing behaviors (Theorell and Kreutz, 2012; Løkken et al., 2018), and the promotion of identity and resilience (Boggan et al., 2017; Zarobe and Bungay, 2017). Taking place in both clinical and community settings, studies of music's effects on mental health have been conducted within disciplines including psychology (McFerran et al., 2018; Pezzin et al., 2018); neurology (Ventouras et al., 2015; Tan et al., 2016); music therapy (Moe, 2002; Gold et al., 2006); nursing (McCaffrey and Locsin, 2002; Pölkki et al., 2012), dance therapy (Meekums et al., 2015; Campbell, 2020); and psychiatry (Grocke et al., 2008; Grasser et al., 2019), among others.
As one might expect, the many disciplines involved in this work vary widely in how they describe, conduct, and report their studies and practices. As a result, mental health researchers and practitioners have found it difficult to coordinate and synthesize relevant evidence; this has hindered efforts to establish best practices and clinical practice guidelines, develop standardized prescription and treatment models, and promote responsive policies. These limitations have posed ongoing barriers to the testing and scaling of promising strategies that could improve outcomes and access to mental health care.
Scoping Review
To address these barriers, a scoping review was conducted of the literature regarding uses of music in treatment and symptom mitigation related to SMIs3. The purpose of the review was threefold:
to outline the many practices, interventions, and research processes being undertaken at the intersection(s) of music and SMIs, from all published works;
to identify evidentiary gaps and opportunities; and
to offer initial recommendations to support evidence synthesis, improve research practices, and ultimately increase treatment effectiveness and access over time.
Methods
Design
This review was conducted utilizing the methodological framework detailed by the Joanna Briggs Institute's (JBI) Methodology for JBI Scoping Reviews (Peters et al., 2020). According to the The Joanna Briggs Institute (2015), the purpose of a scoping review is “to map the key concepts underpinning a research area as well as to clarify working definitions, and/or the conceptual boundaries of a topic” (p. 6). Scoping reviews involve a systematic process of literature searching, screening, and data analysis; the result is a detailed overview of the topic—including who and what have been studied, when and how frequently, research strategies utilized, and preliminary findings. Unlike systematic reviews, scoping reviews do not include a quality assessment of included studies, nor do they generate meta-analyses. Instead, scoping reviews are undertaken regarding emerging topics or knowledge areas, when it is not yet clear what particular questions could or should be addressed via future systematic reviews. Their purpose is to provide a sense of the field's landscape, identifying existing gaps and densities in the evidence.
Over the past decade, heightened interest in researching the mechanistic features of music's effects on mental health has led to an increase in studies; as a result, a scoping review at this point in time advances understanding of the uptake and dissemination of music across disciplines addressing SMIs. Thus, in December 2019, this review's research team searched for similar reviews or protocols using PROSPERO: International Prospective Register of Systematic Reviews, Cochrane Database of Systematic Reviews, BioMed Central Systematic Reviews, and JBI Database of Systematic Reviews and Implementation Reports. None of the resulting reviews had examined ways in which music—including but not limited to “music therapy”—was being utilized in interventions for multiple SMIs.
Protocol Registration and Reporting
A protocol for this review was developed following the JBI scoping review protocol guidelines (Peters et al., 2020); it was registered in January 2020 with both JBI and the Open Science Foundation (OSF) under the title, “Uses of music in the treatment of serious mental illness: A scoping review.” Reporting of this scoping review was completed in accordance with the PRISMA-ScR Reporting Guidelines.
Definitions and Classifications
In categorizing music-based interventions represented in included studies, researchers extracted details regarding the musical elements of each intervention—referring to these as the interventions' music-based “activities.” Throughout this article, the term “activities” refers specifically to the music-based elements of the intervention of which they are a part.
Activities were further characterized as “passive,” “active,” or “both.” While levels of felt engagement are likely to vary from participant to participant, these terms allowed the research team to calculate how many activities involved direct/active engagement such as singing or playing an instrument, vs. comparatively passive experiences such as listening to music or watching a performance. This distinction is important, as previous studies have indicated that passive and active engagement in music and other alternative therapies generate varied changes via differing mechanisms (Cosio and Lin, 2018; McPherson et al., 2019; Prakash, 2019).
Activities were additionally categorized as “individual” (involving a single participant either on their own or one-on-one with a facilitator), “group” (involving multiple participants), or “both”—the latter indicating interventions that, for example, alternated between individual and group sessions. Studies regarding the health benefits of social connection suggest that group activities may moderate or mediate effects of music engagement (Holt-Lunstad et al., 2010; Umberson and Karas Montez, 2010; Eisenberger and Cole, 2012), rendering this distinction important.
Finally, most activities involved a therapist, researcher, or other leader who directed or facilitated music-based activities; throughout this article, these individuals are referred to as “facilitator(s).”
Inclusion and Exclusion Criteria
Because its goal was to illuminate all published research at intersections of music and SMIs, this review did not limit results by date or geographic location. Inclusion criteria were identified using the following PICOS framework:
Population (P): Humans of all ages being treated for—or assisted in the alleviation of symptoms related to—serious mental illness (SMI), as defined for the purposes of this review by: (1) a diagnosis or suspected diagnosis (verified or self-reported) of schizophrenia, bipolar disorder, MDD, GAD, or PTSD; or (2) inclusion in the experimental group in a study of interventions designed to treat or mitigate symptoms related to these illnesses4.
Intervention (I): Any uses of music when incorporated specifically in the context of a SMI for the purpose of treating or mitigating symptoms related to the SMI. To accomplish the task of mapping all uses of music in this context, the current review drew upon an intentionally broad conceptualization of music-based activities, as differentially conceptualized by varying fields and practitioners. Thus, interventions may involve (but were not limited to) listening to music, playing musical instruments, singing, attending a music-based performance, performing music, dancing5, songwriting, or analyzing songs or song lyrics. Uses of music for the promotion of general mental well-being were not included, as these were not pertinent to the SMI classification.
Comparator (C): Studies comparing music interventions to standard treatments (or treatment as usual (TAU)), studies comparing music interventions to no treatment, and studies comparing music interventions to other non-standard treatments. Studies without a comparator were also eligible for inclusion.
Outcome (O): All outcomes related to the treatment of SMIs were eligible, such as changes in symptoms, affect, quality of life, functional assessments, academic achievement, social or emotional functioning, delivery of care, and more. Because this review focused on treatment or symptom mitigation related to SMIs, uses of music to research SMIs (i.e., outcomes not directly related to changes in symptoms, function, etc.) were excluded.
Study design (S). All study designs were eligible, including RCTs, pre/post-test designs, qualitative studies, case reports, systematic reviews with and without meta-analyses, etc.
Studies that were not available in English (n = 24) were excluded from this scoping review. In addition, library closures caused by the COVID-19 pandemic resulted in lack of access to some texts. Great effort was taken by multiple research team members to access all missing texts, using InterLibrary Loan (ILL) requests at multiple research institutions and extensive hand-searches online. Dozens of texts were ultimately located using this strategy; however, 88 studies remained inaccessible, and were ultimately excluded.
Literature Search
Comprehensive literature searches were conducted by an experienced health sciences librarian in PubMed, the Cochrane Library, PsychINFO, CINAHL, Embase, SCOPUS, RILM, and The Music Periodicals Database. The search strategy was peer-reviewed by an external expert advisor; after recommended modifications were made, it was again peer-reviewed by a second health sciences librarian using the PRESS (Peer Review of Electronic Search Strategies) Checklist (McGowan et al., 2016). Once searches were conducted, librarians exported results from each database into EndNote, de-duplicated them, and uploaded them into the Covidence platform (https://www.covidence.org/home) for screening by the research team.
Data Collection and Analysis
Title and abstract screening was conducted in Covidence by blinded pairs of research team members. Full-text screening was conducted by the research team, with data extraction completed in a shared Google Sheets file.
Critical Appraisal
As noted above, scoping reviews differ from systematic reviews in that their objective is to provide “an overview of existing evidence regardless of methodological quality or risk of bias” (Tricco et al., 2018). In keeping with the aims of this scoping review, included sources were not critically appraised.
Results
Numerical Summary
This scoping review's literature search identified 11,967 studies for potential inclusion. Following title/abstract screening and full-text screening, 349 articles were found to meet the inclusion criteria; they have been included in the following analysis. See Data Sheet 1 for a complete list of articles.
Analysis
Data were analyzed by diagnosis, population, musical activity, study design, variables or outcomes measured, and findings. Studies indicated considerable variations in purposes, intervention strategies, populations, settings, facilitator identities/roles, measurements, outcomes, and reported details. Because secondary studies incorporated multiple primary studies, some of which appeared separately in this scoping review, secondary studies were excluded from analyses that sought frequency counts of factors such as demographics, setting, facilitator details, etc. This prevented duplicative reporting.
Sample Size and Populations
Of the 289 primary studies, 10 (3.4%) did not record a study sample size. Among the remaining studies, sample size ranged from one to 1,000 participants, with a mean sample size of 48.8 and a median of 20.
Demographic reporting varied widely. Of the 289 primary studies, 19 (6.6%) did not report on gender. Of the remaining studies, 50 (17.3%) involved female participants, and 40 (13.8%) involved male participants. One hundred seventy-nine studies (61.9%) were “mixed group,” meaning that multiple genders were included (breakdown was not consistently reported).
Race and ethnicity were inconsistently reported, with 221 primary studies (76.5%) failing to report race or ethnicity at all. Of those reporting this variable, the majority included multiple races, although the breakdown was inconsistently reported.
Age was also inconsistently reported, with 124 primary studies (42.9%) failing to report minimum participant age, and 131 (45.3%) failing to report maximum age. Thirty-one primary studies (10.7%) reported the numeric age of a single participant. Across all studies, a range in age from 3 to 100 is represented, with apparent density between the ages of 18 and 60.
Apart from demographics, data extraction included populations/groups under study, such as “veterans” (Wilbur et al., 2015), “inpatients with schizophrenia” (He et al., 2018), and survivors of domestic violence (Hernández-Ruiz, 2005). Such groups were initially documented verbatim, and later coded by researchers according to the list in Table 1, selecting the most specific population group discernible from the full text6. Given the complexity of research at the intersections of music and SMIs, it is likely that targeted interventions (for particular groups, settings) would support the development and synthesis of evidence and best practices.
Table 1.
Population.
| Population | N | % |
|---|---|---|
| Inpatients (general) | 65 | 22.5 |
| Person(s) with SMI(s) | 62 | 21.4 |
| Patients (location unspecified) | 52 | 18.0 |
| Other | 18 | 6.2 |
| Veterans and/or Military Personnel | 18 | 6.2 |
| Outpatients (general) | 15 | 5.2 |
| Adolescent(s) | 14 | 4.8 |
| Elderly Individual(s) | 10 | 3.5 |
| Child(ren) | 11 | 3.8 |
| Refugees | 9 | 3.1 |
| Survivor(s) (general) | 6 | 2.1 |
| Child(ren) and Adolescents | 4 | 3.8 |
| Prisoners | 3 | 1.0 |
| IPV/DV Survivors | 2 | 0.7 |
| Total | 289 | 100.0 |
Studies Over Time
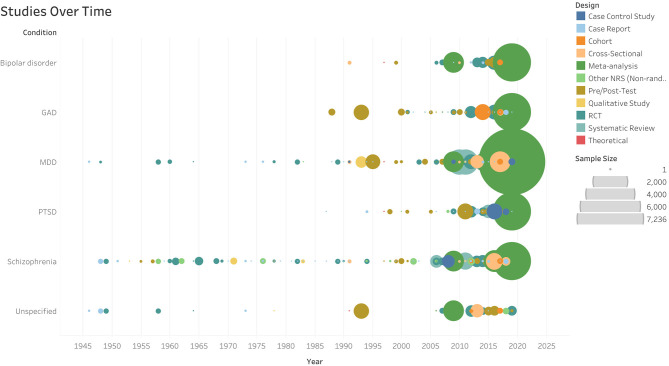
Data extraction for this scoping review dated each study according to publication date. The earliest study identified in this literature search was published in 1946 (Rubin and Katz, 1946); studies began increasing in frequency in 2005, and this trend continues. Study frequency over time can be seen in Figure 1 (interactive version available at https://www.aerodatalab.org/livingreviews/onemind).
Figure 1.
Studies Over Time.
Study Locations
Study locations were documented by country. When the study country could not be determined, locations were documented according to the corresponding author's country. Results are recorded in Table 2.
Table 2.
Location.
| Location | N | % | Location | N | % |
|---|---|---|---|---|---|
| USA | 137 | 39.5 | South Korea | 3 | 0.9 |
| UK | 33 | 9.5 | Sweden | 3 | 0.9 |
| Canada | 16 | 4.6 | France | 3 | 0.9 |
| Germany | 16 | 4.6 | Singapore | 4 | 1.2 |
| Taiwan | 14 | 4.0 | Iran | 3 | 0.9 |
| Australia | 13 | 3.7 | Austria | 2 | 0.6 |
| Norway | 12 | 3.5 | Hong Kong | 2 | 0.6 |
| China | 8 | 2.3 | Russia | 1 | 0.3 |
| Israel | 8 | 2.3 | Luxembourg | 1 | 0.3 |
| Various | 8 | 2.3 | Pakistan | 1 | 0.3 |
| Denmark | 7 | 2.0 | Argentina | 1 | 0.3 |
| Finland | 7 | 2.0 | Korea | 1 | 0.3 |
| Italy | 5 | 1.4 | Bosnia and Herzegovina | 1 | 0.3 |
| India | 5 | 1.4 | Mexico | 1 | 0.3 |
| Not Reported | 5 | 1.4 | Uganda | 1 | 0.3 |
| Japan | 4 | 1.2 | Zealand | 1 | 0.3 |
| Ireland | 4 | 1.2 | Nigeria | 1 | 0.3 |
| Turkey | 4 | 1.2 | Hungary | 1 | 0.3 |
| Greece | 3 | 0.9 | Thailand | 1 | 0.3 |
| Netherlands | 3 | 0.9 | Poland | 1 | 0.3 |
| South Africa | 3 | 0.9 | Portugal | 1 | 0.3 |
| Total | 349 | 100.0 |
In addition to geographic area, the settings of included studies varied widely. The majority (247, 85.4%) were conducted in clinical settings; other settings are documented in Table 3.
Table 3.
Settings.
| Setting | N | % |
|---|---|---|
| Community center | 4 | 9.5 |
| Homes | 4 | 9.5 |
| School (s) | 4 | 9.5 |
| nursing homes | 4 | 9.5 |
| Laboratory/Research | 4 | 7.1 |
| Online | 3 | 4.8 |
| Hospital library | 2 | 4.8 |
| VA | 2 | 4.8 |
| Music therapy clinic | 2 | 4.8 |
| Residential treatment | 2 | 4.8 |
| Not-reported | 1 | 2.4 |
| Dance studio | 1 | 2.4 |
| Arts center | 1 | 2.4 |
| Correctional facility | 1 | 2.4 |
| Halfway house | 1 | 2.4 |
| Activity room | 1 | 2.4 |
| Day center | 1 | 2.4 |
| Day care unit | 1 | 2.4 |
| Trauma center | 1 | 2.4 |
| Meditation studio | 1 | 2.4 |
| Drug rehabilitation | 1 | 2.4 |
| Total | 42 | 100 |
Study Designs
This scoping review collected data from 349 studies, inclusive of all study designs as well as secondary studies—including systematic reviews with or without meta-analyses (n = 60). When documenting study designs, the research team utilized the study design terminology identified by the study authors. If the study design was not identified by the authors, the research team assigned a design type based on their reading.
The study design for each study was coded according to the list in Table 4. Randomized Controlled Trials (RCTs) comprised the largest percentage of studies (23.2%), followed by Pre/Post Tests (21.8%) and Case Reports (18.3%).
Table 4.
Design type.
| Design | N | % |
|---|---|---|
| RCT | 81 | 23.2 |
| Pre/Post test | 76 | 21.8 |
| Case report | 64 | 18.3 |
| Systematic review | 30 | 8.6 |
| Other non-randomized controlled study | 26 | 7.5 |
| Qualitative study | 24 | 6.9 |
| Meta-analysis | 15 | 4.3 |
| Theoreticala | 15 | 4.3 |
| Cross sectional | 9 | 2.6 |
| Case control | 6 | 1.7 |
| Cohort | 3 | 0.9 |
| Total | 349 | 100.0 |
SMIs Studied
Of the five SMIs included in this scoping review, schizophrenia was the most studied, followed by MDD and PTSD. The majority of included studies (69.2%) addressed only one SMI. Ninty studies (30.7%) addressed multiple diagnoses; notably, only one study focused strictly on bipolar disorder. Frequency counts by SMIs are documented in Table 5.
Table 5.
Frequency counts by SMI.
| SMI | N of all studies | N of studies including only this dx | N of primary studies | N of primary studies including only this dx |
|---|---|---|---|---|
| Schizophrenia | 165 | 98 | 141 | 87 |
| MDD | 145 | 72 | 116 | 55 |
| PTSD | 145 | 55 | 112 | 43 |
| GAD | 59 | 17 | 50 | 14 |
| Unspecified | 34 | 0 | 30 | 0 |
| Bipolar disorder | 36 | 1 | 29 | 1 |
Interventions
Music Activities
The music-based activities engaged by each study were documented verbatim for the first 210 studies. Researchers utilized this data to generate a standard list, with which activities in all 349 studies were ultimately coded. Activity types for all primary studies are documented in Table 6.
Table 6.
Activity types.
| Activity | All studies N | % | Primary studies N | % |
|---|---|---|---|---|
| Listening to music (Recorded) | 89 | 15.3 | 82 | 17 |
| Playing an instrument | 68 | 11.7 | 57 | 11.8 |
| Dancing/Movement to music | 68 | 11.7 | 54 | 11.2 |
| Listening to music (Unspecified) | 68 | 11.7 | 53 | 11 |
| Improvising | 48 | 8.3 | 41 | 8.5 |
| Not reported/specified | 47 | 8.1 | 37 | 7.7 |
| Singing in a group | 37 | 6.4 | 29 | 6 |
| Discussing or analyzing music | 31 | 5.3 | 28 | 5.8 |
| Songwriting | 26 | 4.5 | 25 | 5.2 |
| Listening to music (Live) | 16 | 2.8 | 12 | 2.5 |
| Singing | 16 | 2.8 | 10 | 2.1 |
| Drumming/Percussion | 14 | 2.4 | 11 | 2.3 |
| Other | 13 | 2.2 | 13 | 2.7 |
| Composing music | 9 | 1.6 | 7 | 1.5 |
| Recording music | 7 | 1.2 | 7 | 1.5 |
| Not applicable | 7 | 1.2 | 2 | 0.4 |
| Performing for an audience | 6 | 1.0 | 6 | 1.2 |
| Auditory stimuli | 5 | 0.9 | 5 | 1 |
| Singing alone | 5 | 0.9 | 3 | 0.6 |
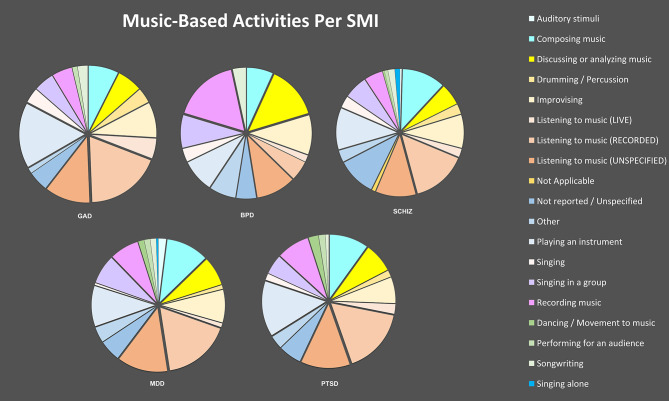
Activities were later disaggregated by SMIs to illuminate whether condition/diagnosis appears to have had a bearing on choice of activity. Results are shown in Figure 2.
Figure 2.
Music-Based Activities Per SMI.
Activity Details
As noted earlier, each music activity was categorized as passive, active, or both. One hundred thirty-five primary studies (46.7%) involved active elements, while 79 (27.2%) involved passive elements; 52 studies (18%) involved both. The remaining 23 studies (8%) did not provide enough information to allow categorization.
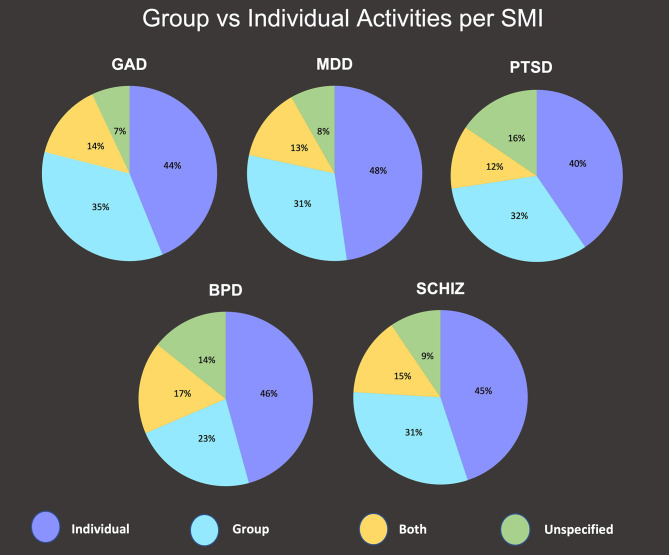
The music activities in each study were also categorized as individual, group, or both. One hundred and nine primary studies (37.7%) involved individual interventions; 139 (48.1%) involved group interventions and 21 (7.3%) involved both. Participation categories were disaggregated by SMIs to illuminate disparities among SMIs. Results are shown in Figure 3.
Figure 3.
Group vs. Individual Activities Per SMI.
Facilitators
Two hundred and thirty-five primary studies (81.3%) reported information regarding the identities of those facilitating the interventions. Of these, Music Therapists working alone was the most represented identity or credential (29.4%), followed by Researcher/Investigator (10.4%). Remaining facilitator identities are documented in Table 7.
Table 7.
Facilitators of music-based activities.
| Facilitator | N | % |
|---|---|---|
| Music therapist | 85 | 29.4 |
| Not reported/Unspecified | 47 | 16.3 |
| Researcher/Investigator | 30 | 10.4 |
| Therapist | 22 | 7.6 |
| Researcher/Investigator, therapist | 20 | 6.9 |
| Other (Not listed here) | 12 | 4.2 |
| Dance/Movement therapist | 11 | 3.8 |
| Healthcare professional (Other than listed) | 9 | 4.1 |
| Music therapist + Psychologist | 8 | 2.8 |
| Psychiatrist | 8 | 2.8 |
| Not applicable | 7 | 2.4 |
| Self-administered (No facilitator) | 6 | 2.1 |
| Dance/Movement therapist + Psychologist | 4 | 1.4 |
| Music therapist + Psychiatrist + Healthcare professional (Other than listed) | 4 | 1.4 |
| Creative arts therapist | 3 | 1.0 |
| Music therapist + Other (Not listed here) | 3 | 1.0 |
| Dance instructor | 2 | 0.7 |
| Dance/Movement therapist + Music therapist | 2 | 0.7 |
| Music instructor | 2 | 0.7 |
| Music therapist + Healthcare professional (Other than listed) | 2 | 0.7 |
| Dance therapist + Psychiatrist + Healthcare professional (Other than listed) | 1 | 0.4 |
| Researcher/Investigator + Dance/Movement therapist | 1 | 0.4 |
| Total | 289 | 100.0 |
Outcomes
Outcomes in each of the included studies varied widely. To allow for analysis, outcomes were first documented verbatim, then later coded by researchers utilizing Dodd et al.' (2018) taxonomy of outcome domains. As expected given a focus on SMIs, the majority of studies (199, 57.0%) measured psychiatric outcomes—which “relate to mental health conditions and associated behaviors (e.g., addictions and behavioral problems)” (Dodd et al., 2018). For example, Zarate (2016) and Gutiérrez and Camarena (2015) examined whether music therapy reduced anxiety symptoms, and Pylvänäinen et al. (2015) investigated effects of dance movement therapy (DMT) on symptoms of depression. Other studies examined effects of music engagement on PTSD symptoms (e.g., Esparza, 2016; Macfarlane et al., 2019), symptoms of schizophrenia (e.g., He et al., 2018), stress levels (Wilbur et al., 2015; Steinberg-Oren et al., 2016), and similar.
Emotional Functioning/Well-Being was the second most prominent outcome domain (n = 130, 37.3%), addressing such factors as “impact of disease/condition on emotions or overall well-being (e.g., ability to cope, worry, frustration, confidence, perceptions regarding body image and appearance, psychological status, stigma, life satisfaction, meaning and purpose, positive affect, self-esteem, self-perception and self-efficacy” (Dodd et al., 2018). For example, Hovey (2013) and Silverman (2019) conducted studies of the effects of music therapy on self-efficacy among acute care mental health inpatients and patients with schizophrenia, respectively. Papadopoulos and Röhricht (2014) and Pylvänäinen and Lappalainen (2018) investigated effects of dance movement therapy on body image.
Social Functioning followed (n = 91, 26.1%); this domain encompasses ways in which one's condition affects “ability to socialize, behavior within society, communication, companionship, psychosocial development, aggression, recidivism, participation” (Dodd et al., 2018). For example, Solli and Rolvsjord (2015) studied whether making music in a group could improve participants' ability to take “an important first social step” (p. 76). Much earlier, Lehrer-Carle (1971) studied how group music therapy affected the ability of adolescents with schizophrenia to communicate with others and generate socially-valuable skills.
Physical functioning was the fourth most prominent domain (n = 30, 8.6%), with studies examining effects of music interventions on pain (e.g., Gosselin et al., 2019) and sleep (e.g., Guétin et al., 2009; Blanaru et al., 2012). Global Quality of Life followed (n = 35, 10.0%), often included as a second or third outcome. This domain “includes only implicit composite outcomes measuring global quality of life;” e.g., Zidani et al. (2017) utilized the Quality of Life Systematic Inquiry (QLSI) in their study of the effects of music listening on anxiety, and Deatrich et al. (2016) measured effects of group music therapy on the quality of life among inpatients at a psychiatric hospital. Role Functioning (n = 12, 3.4%) was also typically included as a second or third outcome, and involved such factors as ability to care for one's children (Tornek et al., 2003) or ability to follow therapy instructions (Strauss et al., 2016).
Cognitive Functioning outcomes (n = 22, 6.3%) involved such factors as cognition/memory testing (e.g., Glicksohn and Cohen, 2000; Tan et al., 2016) and attention/concentration (e.g., Shagan et al., 2018; Macfarlane et al., 2019). Delivery of Care7 was addressed by 12 studies (3.44%); e.g., Trimmer et al. (2018) examined whether integrating music with CBT group therapy increased effectiveness and retention. Preyde et al. (2017) investigated the feasibility and acceptability of group music therapy among youth in a hospital's Child and Adolescent Mental Health unit. All outcome domains identified by this scoping review are documented with frequency counts in Table 8.
Table 8.
Count of outcome subdomains.
| Outcome subdomain | All Studies N | % | Primary studies N | % |
|---|---|---|---|---|
| Psychiatric outcomes | 199 | 57.0 | 157 | 54.3 |
| Emotional functioning | 130 | 37.2 | 113 | 39.1 |
| Social functioning | 91 | 26.1 | 72 | 24.9 |
| Global quality of life | 35 | 10.0 | 21 | 7.3 |
| Physical functioning | 30 | 8.6 | 26 | 9.0 |
| Cognitive functioning | 22 | 6.3 | 17 | 5.9 |
| Delivery of care | 12 | 3.4 | 11 | 3.8 |
| Role functioning | 12 | 3.4 | 12 | 4.2 |
| None reported | 11 | 3.2 | 8 | 2.8 |
| Not applicable | 7 | 2.0 | 3 | 1.0 |
| Perceived health status | 3 | 0.9 | 3 | 1.0 |
| Need for further intervention | 2 | 0.6 | 2 | 0.7 |
| Adverse events/effects | 1 | 0.3 | 0 | 0.0 |
| Total | 349 | 100.0 | 289 | 100.0 |
Comparators
Like outcomes, the comparators in included studies varied widely; see Table 9. Note that while most study designs involve varying comparators, Pre/Post tests—which accounted for over a quarter of all study designs—always utilize the same comparator: a participant's status previous to the intervention. As a result, this “comparator” (documented as “Before/After”) was the most common across studies (n = 128, 44.3%). The second most prominent comparator was treatment as usual (TAU), utilized by 26 studies (9%).
Table 9.
Count of comparator types.
| Comparator type | All studies N | % | Primary studies N | % |
|---|---|---|---|---|
| Before/After | 133 | 38.1 | 128 | 44.3 |
| Not applicable | 83 | 23.8 | 36 | 12.5 |
| TAU | 31 | 8.9 | 26 | 9.0 |
| Without music | 17 | 4.9 | 17 | 5.9 |
| No treatment | 12 | 3.4 | 11 | 3.8 |
| Different kind of music | 9 | 2.6 | 9 | 3.1 |
| Different kind of music, Other (Not listed) | 9 | 2.6 | 9 | 3.1 |
| Delayed treatment | 7 | 2.0 | 7 | 2.4 |
| Other (Not listed) | 7 | 2.0 | 7 | 2.4 |
| Different art therapy (Drama, Vis art, Creative Play) | 5 | 1.4 | 5 | 1.7 |
| Group without SMI/Healthy volunteers | 5 | 1.4 | 5 | 1.7 |
| Passive listening | 4 | 1.1 | 4 | 1.4 |
| Silence | 4 | 1.1 | 4 | 1.4 |
| Different art therapy (Drama, Vis art, Creative Play) + Other CAM | 3 | 0.9 | 2 | 0.7 |
| Not recorded/Unspecified | 3 | 0.9 | 2 | 0.7 |
| Without music, Different kind of music | 3 | 0.9 | 3 | 1.0 |
| Group therapy | 2 | 0.6 | 2 | 0.7 |
| Other CAM | 2 | 0.6 | 2 | 0.7 |
| Self-administered vs. facilitator | 2 | 0.6 | 2 | 0.7 |
| Talk therapy | 2 | 0.6 | 2 | 0.7 |
| Cognitive therapy | 1 | 0.3 | 1 | 0.3 |
| Delayed treatment + Different kind of music | 1 | 0.3 | 1 | 0.3 |
| No treatment + Self-administered vs. facilitator | 1 | 0.3 | 1 | 0.3 |
| Other CAM + Delayed treatment | 1 | 0.3 | 1 | 0.3 |
| White/Pink noise | 1 | 0.3 | 1 | 0.3 |
| Without music + Other (Not listed) | 1 | 0.3 | 1 | 0.3 |
| Total | 349 | 100.0 | 289 | 100.0 |
Measures
Across the 289 included primary studies in this review, 271 distinct measures were reported (Data Sheet 2). Most studies utilized more than one measure, and reporting regarding their use varied considerably. To determine measures used, all measures were documented verbatim during data extraction. Then, to accommodate their scope and variety, verbatim measures were standardized8 and subsequently coded as Biomarkers, Custom Questionnaires, Physical/Performance Tests/Tasks, Qualitative Measures, or Standardized Questionnaires. These categories are documented in Table 10. All included measures are listed in Data Sheet 2.
Table 10.
Measures/Instruments.
| Category | # of instruments in this category | % | # of times instrument in this category was used, across all primary studies |
|---|---|---|---|
| Standardized questionnaires/Scales | 201 | 74 | 378 |
| Qualitative methods (Interviews, focus groups, etc.) | 35 | 13 | 132 |
| Custom questionnaires/Scales | 13 | 5 | 27 |
| Biomarkers | 11 | 4 | 32 |
| Physical/Performance tests/tasks | 11 | 4 | 12 |
| Total | 271 | 100% | 581 |
Study Findings
Due to the wide variety of outcomes and measures included, findings for each primary study were coded simplistically according to whether the music intervention had performed better, worse, or equal to the comparator, or whether results had been indeterminable (Table 11).
Table 11.
Study results.
| Results | N | % |
|---|---|---|
| Music > Comparator | 198 | 68.51 |
| Not Applicable | 39 | 13.49 |
| Undetermined | 35 | 12.11 |
| Music = Comparator | 9 | 3.11 |
| Music < Comparator | 8 | 2.77 |
| Total | 289 | 100.00 |
Discussion
This scoping review found that hundreds of studies related to music-based interventions for SMIs have been conducted worldwide over several decades, with significant increases in study frequency since 2005. Studies have primarily involved mixed-gender groups with more than one race or ethnicity represented; however, demographic reporting was inconsistent and routinely inadequate. This limits researchers' and practitioners' ability to note disparities in results, and to ascertain who may be most helped by music-based activities and experiences.
As noted, schizophrenia was the most studied SMI, followed by MDD, PTSD, GAD, and bipolar disorder. While bipolar disorder was included in 30 studies, only one study focused singularly on this illness; similarly, only 14 studies addressed GAD alone9. Further research is warranted to determine causes for frequency disparities among the included SMIs; e.g., do theories of change indicate less potential for music-based interventions for bipolar disorder and GAD patients, or have studies regarding these illnesses simply been limited by lack of funding, researcher interest, and other concerns?
Many systematic reviews related to music and health have been unable to aggregate and synthesize evidence from studies; as a result, they have often recommended further study and greater rigor (see van Westrhenen and Fritz, 2014; Petrovsky et al., 2015; Williams et al., 2018). This need for rigor is often interpreted as a need for greater utilization of RCTs; however, this scoping review yields that RCTs emerged as the predominant study design. In other words, a lack of rigor—along with other obstacles to evidence synthesis—should not be simplistically linked to a failure to utilize a particular study design. Indeed, while some systematic review authors do highlight the value of randomized controlled trials (Yang et al., 2019), others note that rigor would be improved by longer-term studies (Veerman et al., 2017), as well as improved use of rigorous qualitative strategies such as data triangulation, structured clinical observations, and far more detailed descriptions of study participants, their behaviors, and musical activities (van Westrhenen and Fritz, 2014).
Of course, although RCTs were the predominant study design in this scoping review, it should be noted that controls varied widely—including treatment as usual (TAU), delayed treatment, other genres of music, other forms of art therapy, and more. As a result, the findings of the included RCTs had quite disparate applications. In addition, given that scoping reviews are not designed to assess data quality, the authors cannot speak to the rigor and quality of the studies included, regardless of design. In the absence of quality assessments, it can be tempting to use study design as a proxy for study quality (e.g., assuming that an RCT is of higher evidential quality than a case study); however, such assumptions are inadvisable, as quality varies widely across study designs (see Ryan et al., 2013; Chambers, 2017; Higgins and Thomas, 2020).
Activities
A wide range of activities were represented in this scoping review, with the most prominent being listening to recorded music (15.3%). Notably, 47 studies (8.1%) did not report the type of musical activity experienced by study participants. Active engagement in music-based interventions was considerably more common in the review's findings than passive engagement (46.7 vs. 27.2%), and group interventions were more common than individual (48.1 vs. 37.7%). Notably, the SMI being addressed appears to have affected activity facets. For example, bipolar disorder studies involved more “recording music” activities than other SMIs, while GAD and PTSD studies involved more playing of instruments. Group interventions were utilized for MDD more often than for PTSD (48 vs. 40%).
Just as the details of activities themselves were inconsistently reported, the rationale behind detail selection is inconsistently provided. As a result, it is often unclear to what extent activity facets—such as passive vs. active engagement, group-based vs. individual approaches, genres, etc.—were selected based upon factors such as availability, convenience, or facilitator expertise, vs. factors such as prior research or formalized theories of change related to particular participant groups or conditions. Considering that outcomes are highly likely to be affected by activity details, further research is needed to determine which types of engagement reliably generate particular results—and for whom. This would allow selection of activity details based on diagnoses, symptoms, participant factors, outcomes, and more. To this end, it is critical that future researchers document the rationale behind each decision related to interventions and their many facets (see Recommendation I).
Facilitators
Facilitators ranged in discipline and background; while music therapists comprised the largest percentage (29.4%), those identified simply as a researcher/investigator (often including an author of the study) made up over 16% of the facilitators. The frequency with which researchers facilitated music interventions raises two questions: First, did researchers receive musical (or music-facilitation) training before initiating programs or studies; and second, was their training decision based on science/evidence? (For example if researchers did not receive training, was this based on evidence that such training was not essential/beneficial?).
One in six primary studies (16.6%) involved multidisciplinary teams as facilitators, or facilitators who had multidisciplinary backgrounds—underscoring the interdisciplinary nature of the music and SMI intersection. Unfortunately, almost as many (16.3%) failed to report or specify facilitator details at all. This prevents assessment regarding the role of facilitators—including their discipline, training, relationship with study participants, etc.—in an intervention and its outcomes. Inconsistencies in reporting, combined with the variety of facilitators involved, highlight the need for continued research regarding whether and to what extent facilitator characteristics and backgrounds affect results. In the future, evidence synthesis will be supported by the careful reporting of facilitator details including credentials, training (or lack thereof), and relationships with study participants (see Recommendation I).
Reported Findings
Over two-thirds of all primary studies (68.5%) reported positive findings (“music > comp”), while 12 percent (n = 35) produced indeterminate results. Only eight studies (2.8%) indicated that the music-based intervention had produced worse results than the comparator. A scoping review does not offer assessments of study quality or risk of bias; as a result, practice and policy guidelines cannot be generated based on existing data. However, these data indicate the potential promise of music-based activities in treatment or symptom management of SMIs, and they underscore the value of continued research—with the implementation of robust study and reporting protocols.
Evidence Synthesis
Overall, the findings in this scoping review suggest that inconsistent reporting practices, a lack of core outcomes or outcome measures, and the sheer complexity of interventions combine to render difficult the synthesis of existing evidence for the purposes of further developing or scaling music-based interventions. Reporting practices and core outcome sets are discussed under Recommendation IV, below. Regarding intervention complexity, the many variables involved in each musical activity generate the potential for effects on studied outcomes. For example, “listening to music,” though often documented as a straightforward activity, can take place while participants lay down or while they move about; it can also take place via the use of headphones, small speakers, large speakers, or the presence of a live musician. The music to which participants listen may be selected by study participants themselves, or by facilitators; it could be of high quality and played at an ideal volume; it could also be of low quality, or too quiet/loud for a given participant. Activity complexity expands significantly when one adds the potential effects of: setting (e.g., clinic vs. home vs. community center vs. prison); facilitators' relationships with participants; group interactions (including how well group members know one another); how long a given participant has lived with an SMI; how many other treatments or options a study participant has previously tried; levels of autonomy in the activity (who selects music, volume, instruments, dose/duration, etc.); and more.
Unfortunately, this scoping review found that such variables were insufficiently and inconsistently reported—precluding readers' ability to discern precisely what type of activity/component delivered (or failed to deliver) results. For example, it was impossible in some cases to ascertain the identity of the activity facilitator at all, let alone the nature of the facilitator's relationship with study participants. Similarly, basic demographic data were inconsistently available, let alone details regarding participants' diagnoses (were these volunteered/self-reported?) or participants' prior experience(s) with mental health treatments.
Meticulous documentation is necessary for identifying mechanisms, causal patterns, and replicable strategies. Replicability is critical to the development of robust evidence bases and practice guidelines for integrating music into intervention and treatment plans. When researchers or health practitioners read a peer-reviewed article and cannot identify precisely what was done in the reported study or intervention, it becomes impossible for them to replicate the process with other populations, in other settings, or with larger sample sizes.
Of course, studies that cannot produce generalizable results (due to study designs or small sample sizes) may yet generate valuable, transferable findings; however, a lack of detail impedes this benefit as well. In other words, although scalability is not an aim of every music-based intervention for SMIs, improved reporting is nevertheless critical for enhancing understanding of the music-SMI intersection across disciplines. Consistent, rigorous detail in reporting will support the sharing of information among mental health practitioners, individuals with lived experience with SMIs, artists and arts-program facilitators, and others, while also improving research and scalability when appropriate.
Music's complex, wide-ranging nature—as observed in this review—should be understood as a promising asset; it suggests that music-based strategies offer adaptability, flexibility, and customize-ability as SMI interventions. Nevertheless, the sheer breadth of activities falling under the heading of “music”—and the extent to which each of these can vary from setting to setting—present impediments to synthesizing evidence and advancing the field. To navigate these difficulties, five recommendations are offered below.
Recommendations
While existing systematic reviews have demonstrated the potential for music interventions to support mental health (e.g., music therapy for depression; Aalbers et al., 2017), many have also asserted that there are issues with the quality of evidence and relevance of outcome measures (Aalbers et al., 2017; Geretsegger et al., 2017; Clift, 2020). Results of the current scoping review comport with these assertions. As noted, scoping reviews are not designed to analyze existing research for the purpose of making practice recommendations; however, they are designed to document the state of the science and identify gaps and future directions for research. The below recommendations are intended to support ongoing and future research to improve the evidence base and promote translation of evidence into practice.
Recommendation I: Standardize Reporting Practices by Adopting Existing Reporting Guidelines to Clearly and Consistently Document Studies
A limitation to the current body of research—and a hindrance to translating existing evidence into practice—is a lack of consistent and sufficient documentation with regard to key study information necessary to understand: (1) the populations and conditions studied; (2) specific details of each intervention studied; and (3) the specificity and relevance of outcomes measured, along with details required for an assessment of the quality of the research.
Underreporting of key information in research is not a phenomenon unique to music-based studies. An analysis of completeness of the intervention description in trials and reviews found that studies of non-pharmacological interventions provided adequate documentation of the intervention only 29% of the time, as compared to 67% for pharmacological interventions (Glasziou et al., 2008). In addition, a comprehensive study of adherence to reporting guidelines over a 20-years span (January 1996 to September 2016) for clinical trials, systematic reviews, observational studies, meta-analysis, diagnostic accuracy, economic evaluations, and preclinical animal studies demonstrated that 87.9% of the included studies reported suboptimal adherence to reporting guidelines (Jin et al., 2018). Inadequate reporting of intervention studies limits opportunities for clinicians and patients to utilize research studies to support medical decision making and precludes future researchers from building on existing research. By contrast, standardizing reporting practices for all studies—including those involving music-based interventions for SMIs—will support translation into policy and practice and improve future research.
Sharp et al. (2019) observed that across disciplines, “[r]eporting guideline endorsement rates are low; information is vague and scattered” (n.p); similarly, Jin et al. (2018) confirmed “the need for further emphasis in the scientific community to encourage the use of reporting guidelines” (n.p.). Building on their findings, we recommend that future research incorporate and promote the use of reporting guidelines. Reporting guidelines inform researchers which elements of a study must be documented in order to support the transparency, interpretation, synthesis, replication, and reproducibility of research. A number of reporting guidelines are available to researchers working at the nexus of music and mental health, and they help document each key aspect of a study, including:
Conditions/populations of interest; e.g., PTSD (Kaloupek et al., 2010);
Study designs employed; e.g., CONSORT for RCTs, STROBE for observational studies;
Types of data collected; e.g., eMOOD (Faurholt-Jepsen et al., 2019), fMRI (Poldrack et al., 2008); and
Intervention details; e.g., TIDieR (Hoffmann et al., 2014) and CReDECI 2 (Möhler et al., 2015).
Notably, while reporting guidelines focus on optimizing the translation of research findings into practice, much of the valuable work regarding art's impacts on health is not necessarily occurring in the context of formal academic research. Therefore, the authors suggest that artists, practitioners, and facilitators also utilize these reporting guidelines when evaluating and documenting arts-based programming and activities—regardless of the level of researcher involvement. This enables consistency in communicating the work across the spectrum of disciplines and audiences.
Recommendation II: Utilize the Current Scoping Review as a Basis on Which to Investigate the Utility of a Reporting Guideline or Reporting Guideline Extension for Music Interventions
Studies of music interventions in mental health may be sufficiently unique as to warrant a new guideline for reporting these studies. Indeed, a 2017 workshop about “music and the brain,” hosted by the National Institutes of Health (NIH), generated recommendations to promote “more rigorous reporting of interventions, methodologies and results” at the intersection of music and brain health, and to “establish standardized and/or personalized outcome measures” (Ambler et al., 2020). A proposal for a reporting guideline for music and health was suggested by Robb and colleagues (2011); however, this guideline does not appear to have been formalized or taken up by the field.
A first step toward the development of any reporting guideline is an evidence synthesis of the body of evidence in the relevant field, such as the current scoping review. The data in this review, combined with existing guidelines, suggests an opportunity to generate a new tool for researchers working at the nexus of music and mental health. If taken up by researchers in the field, a reporting guideline specific to music in mental health research could facilitate better documentation—ultimately improving evidence synthesis and the translation of research into practice. Such a guideline could also support the design of new music-based interventions, and support funding agencies in structuring their grant reporting and calls for proposals (CFPs).
If undertaken, the development of a new reporting guideline should take a comprehensive, stakeholder-engaged approach that yields insights into how clinicians, artists, content experts, patients, caregivers, researchers, and other key stakeholders imagine the research process. Diverse perspectives and iterative development processes help ensure the guideline accounts for the many ways in which music impacts on mental health. The guideline should additionally support transparent documentation for all who will be looking to evidence to inform their decision making.
Meanwhile, the authors of the current scoping review have identified key elements for reporting, which may be considered in any guideline for music interventions in mental health research. These are offered in Data Sheets 3 and 4.
Recommendation III: Accommodate the Complexity of Music Interventions
Simple interventions typically feature a linear pathway whereby outcomes and interventions are linked; by contrast, complex interventions include non-linear causal pathways and multiple, interacting components (Petticrew, 2011). In fact, even “simple” interventions are often influenced by complex interplays of individual characteristics, social determinants, the health care delivery system, and the interventions themselves (Guise et al., 2017). Like most non-pharmacological interventions, music interventions are complex, consisting of several components that work independently or interdependently of each other and can be tailored to fit a specific setting (Craig et al., 2008). This non-standardization of music interventions complicates how we study them.
For example, the fact that music could be delivered through headphones to patients in a therapist's private office, vs. delivered through speakers to patients in clinical waiting rooms, generates so-called intervention complexity (Guise et al., 2017). In addition, music has unique neurobiological and psychological impacts (Boso et al., 2006) that can interact with other clinically important outcomes in healthcare—generating so-called pathway complexity (Guise et al., 2017)10. In short, music-based approaches to SMI care must be understood and studied as complex interventions.
Working with complex interventions requires solid theoretical understanding of how a given intervention causes change. Theories of change undergird the development of intervention protocols; they also allow weak links in the causal chain to be identified and strengthened. Of course, researchers should balance the need for protocol fidelity with the utility of adaptation when important for the local setting; however, departures from protocols should be documented with care and transparency (see “Modifications,” Data Sheet 4). In addition, when studying complex interventions, researchers should be cautious about interpreting findings—as a lack of impact may not signal a lack of efficacy, but rather a failure of implementation. Lastly, research teams working with music and SMIs should consider study designs capable of yielding better evidence for complex interventions; e.g., cluster-randomized trials, N-of-1 designs, and step-wedge designs (Craig et al., 2008).
As stated, transparent reporting of study elements is critical; to that end, the Criteria for Reporting the Development and Evaluation of Complex Interventions in Healthcare: Revised Guideline (CReDECI 2) provides specific guidance on documenting the components of complex interventions (Möhler et al., 2015). It emphasizes the importance of documenting:
Theoretical underpinnings of an intervention.
Selection of outcomes and modes of evaluation.
All intervention components, including reasons for their selection, their essential functions, and any intended interaction between components.
Strategy for delivering the intervention within the study context.
All materials and tools used in the delivery of the intervention.
Fidelity of the delivery process compared to the study protocol.
Recommendation IV: Consider Developing Core Outcome Sets and Core Measures for Studies of Music's Use in Supporting Mental Health
This scoping review demonstrates broad uptake of music as an intervention to support those with SMI and their caregivers across a continuum of outcomes—including clinical, humanistic, and economic outcomes that matter to patients, providers, and policy-makers. Nevertheless, it remains a rare occurrence for systematic reviews of music-based interventions to yield a strong recommendation for clinical translation into practice. As stated above, this is not necessarily a result of insufficiently rigorous study methods (e.g., RCTs), but rather of clinical heterogeneity—defined as a “…variation in study population characteristics, coexisting conditions, cointerventions, and outcomes evaluated across studies included in an SR [systematic review] or CER [comparative effectiveness research] that may influence or modify the magnitude of the intervention measure of effect” (West et al., 2010). In other words, the selection of unique, often incomparable, heterogenous outcomes—in terms of outcome domains (what is measured) and selection of measurement tools/instruments (how the outcome is measured)—often limits the combination and comparison of results of individual studies. An additional consequence of inconsistent outcome selection is the risk that outcomes are being selected without having determined their importance or relevance to patients and caregivers living with the studied conditions.
This issue of outcome heterogeneity is not specific to research related to music and mental health; it actually affects the conclusion of a substantial proportion of Cochrane Collaborative systematic reviews (Kirkham et al., 2010), and outcome reporting bias is an important problem in randomized trials (Dwan et al., 2008). Of relevance to the current scoping review, these issues also occur in a great deal of general SMI research. A meta-analysis of 198 trials of psychotherapeutic interventions for MDD identified 33 unique outcome measurement tools (Barth et al., 2013). The current scoping review confirms this trend with regard to music and SMIs, demonstrating extensive heterogeneity in outcomes and outcome measures (see Tables 8, 10).
One approach to mitigating the effects of outcome heterogeneity is the adoption of core outcome sets. A core outcome set (COS) establishes a minimum standardized collection of outcomes, identified by key stakeholders through robust consensus methods11. Utilizing a minimum COS would improve comparative effectiveness of interventions and ensure that the outcomes that are important to communities requiring evidence for decision-making (e.g., patients, caregivers) are represented in the study design process, even if not directly engaged by the study team.
Implementing a COS does not restrict researchers to only those minimum outcomes; rather, it sets an expectation that COS will always be collected while researchers continue to explore additional outcomes. If it is decided that a measure within a COS should be excluded from a given study, the research team is expected to explain the exclusion, as well as the relevance and importance of other (additional) selected outcomes (Williamson et al., 2012).
Notably, the process of engaging stakeholders to identify a COS can itself yield important findings that advance health. For example, a recent study to identify outcome domains and outcome measures of importance to people living with MDD identified 80 outcome domains related to the benefits of treatments, derived from the lived experience of depression (Chevance et al., 2020). The study revealed that several outcome domains frequently mentioned by participants were not measured by the seven most-used depression scales in MDD research. It also identified 57 additional outcome domains that were unrelated to the direct benefits of treatment (e.g., treatment safety, health-care organization, social representation of depression), and which at present remain understudied (Chevance et al., 2020).
For the above reasons, the authors recommend the uptake and implementation of existing COS for each SMI. Teams studying music-based interventions for SMIs should first identify whether a COS exists for the population and condition of interest, and (if so) implement that COS by reviewing the literature and consulting the COMET Database. In addition, the development and implementation of a specific COS for the study of music-based interventions for SMIs may be an important step in this field, to promote the translation of evidence into practice.
Recommendation V: Consider Developing a Taxonomy to Better Organize and Define “Music” and “Music Engagement”
Distinct activities included under the general umbrella-term of “music” are likely to affect health via multiple, distinct mechanisms. For example, vigorous group drumming outdoors can be expected to generate different physiological and psychological effects than listening to music on headphones while lying in a hospital bed. While both are music-based activities, the expectation that they share outcomes or measures may strain the definition or category of music beyond its utility in health research and practice. To be clear, improved reporting of all music-based interventions is both urgent and fully feasible, as is the increased standardization of many research aspects and processes. However, expecting distinct activities to utilize similar outcomes or measures merely because they can both be described as “music(al)” may actually minimize the effects of music-inclusive interventions by obscuring or eliding their scope and variety.
The general category of “music” is highly useful in terms of developing research and practice networks, supporting advocacy, raising funds, and advancing patient and public awareness of the value of music as an aspect of health and well-being. However, grouping disparate activities together in research, particularly apart from specific protocols, may perpetuate the heterogeneity that has precluded adequate synthesis to date. Notably, this scoping review was able to identify the difficulties of this heterogeneity in part because it too was broadly inclusive. To meet its goal of illuminating all uses of music in the treatment or mitigation of symptoms related to SMIs, this review was required to include studies involving myriad activities that, while related to music, are likely to effect change in disparate ways.
As researchers and practitioners consider developing formal reporting guidelines and core outcome sets, they might also consider developing taxonomies of music-based or music-inclusive activities—perhaps grouping them iteratively (e.g., by types of movement involved, potential mechanisms, where they range from prescriptive to improvisational/expressive, etc.). Such taxonomies would help generate shared vocabularies for use by practitioners, artists, and the research community, and support development of best practices related to specific forms of music engagement. Taxonomies may be operationalized by journals and research databases to index studies—enabling better identification of similar studies, in turn supporting meaningful aggregation and synthesis of studies for the purposes of systematic review.
Limitations
The extraction and coding of data across this collection of studies involved adapting studies to the extraction tool, typically in collaboration with multiple research team members. It is possible that, provided with the same data, other research teams may have made alternative selections. However, these would be highly unlikely to result in changes to the review's overarching findings or recommendations.
Interruptions to library access caused by the COVID-19 pandemic limited the research team's access to studies that may otherwise have been available. While many of these would likely have been excluded regardless, it is possible that current findings exclude data from applicable studies. That said, the sample size of the review generates a high level of confidence regarding its findings; again, it is unlikely that the addition of inaccessible texts would result in changes to overarching findings or recommendations.
Finally, the large number of studies included in this scoping review resulted in a focus on frequency counts and standardized coding practices, with the aim of illuminating a general landscape and identifying research densities and gaps. Future researchers may wish to disaggregate studies by various factors, allowing more in-depth looks into particular practices, populations, or study designs.
Conclusion
This scoping review sought to support the improvement and expansion of options for addressing SMIs by gathering and coordinating evidence regarding music-based interventions for MDD, PTSD, bipolar disorder, GAD, and schizophrenia. To our knowledge, it is the first scoping review to examine intersections of music and SMIs at this scale. Having documented details regarding 349 studies, this review illuminates the volume and variety of research occurring at intersections of music and SMIs. It additionally underlines the promise of music in supporting mental health, as most studies indicated positive results. Findings indicate that music-based interventions are currently constrained not by a lack of research, but by an ongoing inability to synthesize the extensive research being generated. Despite accumulating studies since 1946, synthesis continues to be precluded by a wide variety of outcomes and outcome measures, a lack of quality reporting, and the inherent complexity of music-based interventions. Findings suggest that the extensive time, funds, and expertise being invested in this field will continue to see limited returns until widespread changes occur to reduce heterogeneity (as feasible), increase replicability and transferability, and improve understandings of mechanisms and causal pathways.
To support these efforts, this review offered five key recommendations, with an emphasis on the immediate action step of improving reporting practices. While the review's illumination of extensive heterogeneity and complexity have indicated urgent obstacles, the creativity, innovation, and attentiveness to patient experience that are apparent in included studies also figure as assets to the mental health field's overarching efforts to advance care, access, and equity over the long term.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
TG led the scoping review study as well as the writing of this article. SS co-authored the discussion and recommendations, and contributed multiple revisions throughout. HK, SG, AT, and CS contributed data analyses. SG contributed to the manuscript's introduction. SM helped conceive of the project and oversees IAM Lab's research output. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1See also Vigo et al. (2019), who indicated that a “striking imbalance exists between government spending on mental health and the related disease burden in the Americas” (n.p.).
2For example, by reducing stigma associated with care, or by rendering care less intimidating or more culturally responsive.
3This scoping review was part of a larger initiative which included a transdisciplinary gathering of thought leaders, who were asked to review and respond to early scoping-review findings. This group then generated recommendations to advance opportunities at the intersection of music and SMIs. Their responses, informed by professional expertise as well as lived experience with SMIs, will be published separately.
4This scoping review excluded (a) studies that were inexplicit regarding the type of mental illness treated (such as the five diagnoses here named); and (b) studies that examined effects of relevant interventions on one or more of the five diagnoses here listed, but included these among other illnesses or diagnoses while failing to disaggregate outcomes.
5The authors acknowledge that the inclusion of dance will be seen by some disciplines as problematic; however, many cultures, disciplines, patients, and practitioners do not formally separate these activities (Besson and Schön, 2001; Thompson, 2014; Leman and Maes, 2015; Levitin et al., 2018). Because dance interventions utilize music (with rare exceptions), excluding dance would have resulted in the exclusion of many interventions in which music played a role—thereby compromising the scoping review's goal of generating of a broad, inclusive landscape of all uses of music in SMI interventions.
6For example, if a study indicated that study participants had been veterans and clinical patients, the “Veterans and/or Military Personnel” category would be selected over “patients,” due to increased specificity.
7According to Dodd et al. (2018), this outcome domain refers to outcomes related to “adherence/compliance; patient preference; tolerability/acceptability of intervention; withdrawal from intervention (e.g., time to treatment failure, reason for stopping therapy); appropriateness of intervention; accessibility, quality and adequacy of intervention; patient/career satisfaction (emotional rather than financial burden); process, implementation, and service outcomes (e.g., overall health system performance and the impact of service provision on the users of services)”.
8For example, “heart rate” and “pulse” were combined, “EEG” and “electroencephalogram” were combined, etc.
9By comparison, 43 studies addressed PTSD alone, 55 addressed MDD alone, and 87 addressed schizophrenia alone.
10Recognizing that complex interventions require deeper consideration and different tools to design, implement, replicate, and critically review associated studies, the Medical Research Council updated their guidance in 2019. Their document articulates key implications for the study of complex interventions, and provides recommendations for researchers studying complex interventions (Craig, 2019).
11These consensus methods should themselves be measured and consistently reported in all trials for a specific clinical area (Williamson et al., 2012).
Funding. Partial funding for this study was provided by One Mind.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.649840/full#supplementary-material
References
- Aalbers S., Fusar-Poli L., Freeman R. E., Spreen M., Ket J. C., Vink A. C., et al. (2017). Music therapy for depression. Cochrane Database Syst. Rev. 11:Cd004517. 10.1002/14651858.CD004517.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambler M., Springs S., Garcia D., Born C. (2020, August 19). “Heterogeneity of Outcomes for Intraoperative Music Interventions: A Scoping Review and Evidence Map,” in BMJ Evidence-Based Medicine (BMJ Publishing Group). 10.1136/bmjebm-2020-111382 [DOI] [PubMed] [Google Scholar]
- Armitage R., Nellums L. B. (2020). COVID-19 and the consequences of isolating the elderly. Lancet Public Health 5:e256. 10.1016/S2468-2667(20)30061-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth J., Munder T., Gerger H., Nüesch E., Trelle S., Znoj H., Jüni P., Cuijpers P. (2013). Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis. PLoS Med. 10:e1001454. 10.1371/journal.pmed.1001454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besson M., Schön D. (2001). Comparison between language and music. Ann. N. Y. Acad. Sci. 930, 232–258. 10.1111/j.1749-6632.2001.tb05736.x [DOI] [PubMed] [Google Scholar]
- Blanaru M., Bloch B., Vadas L., Arnon Z., Ziv N., Kremer I., Haimov I. (2012). The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Mental Illness. 4, 59–65. 10.4081/mi.2012.e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggan C. E., Grzanka P. R., Bain C. L. (2017). Perspectives on queer music therapy: a qualitative analysis of music therapists' reactions to radically inclusive practice, in Journal of Music Therapy (Vol. 54) (American Music Therapy Association; ), 375–404. 10.1093/jmt/thx016 [DOI] [PubMed] [Google Scholar]
- Boso P., Barale F., Enzo E., Politi M. (2006). Neurophysiology and neurobiology of the musical experience. Funct. Neurol. 21, 187–191. [PubMed] [Google Scholar]
- Brooks S. K., Webster R. K., Smith L. E., Woodland L., Wessely S., Greenberg N., Rubin G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence, in The Lancet (Vol. 395) (Lancet Publishing Group; ), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell B. (2020). Correction to: past, present, future: a program development project exploring post traumatic slave syndrome (PTSS) using experiential education and dance/movement therapy informed approaches, in American Journal of Dance Therapy (Vol. 42) (Springer; ), 145–146. 10.1007/s10465-020-09330-x [DOI] [Google Scholar]
- Chambers C. (2017). The Seven Deadly Sins of Psychology: A Manifesto for Reforming the Culture of Scientific Practice by Chris Chambers. Princeton, NJ: Princeton University Press. Retrieved from: https://www.goodreads.com/book/show/32025411-the-seven-deadly-sins-of-psychology [Google Scholar]
- Chevance A., Ravaud P., Tomlinson A., Le Berre C., Teufer B., Touboul S., et al. (2020). Identifying outcomes for depression that matter to patients, informal caregivers, and health-care professionals: qualitative content analysis of a large international online survey. Lancet Psychiatry 7, 692–702. 10.1016/S2215-0366(20)30191-7 [DOI] [PubMed] [Google Scholar]
- Choudhury T., Debski M., Wiper A., Abdelrahman A., Wild S., Chalil S., et al. (2020). COVID-19 pandemic: looking after the mental health of our healthcare workers. J. Occupat. Environ. Med. 62, e373–e376. 10.1097/JOM.0000000000001907 [DOI] [PubMed] [Google Scholar]
- Clift S. (2020). Fancourt, D. and Finn, S. (2019). What is the evidence on the role of the arts in improving health and well-being? A scoping review. Nordic J. Arts Cult. Health 2, 77–83. 10.18261/issn.2535-7913-2020-01-08 [DOI] [PubMed] [Google Scholar]
- Coleman K. J., Stewart C., Waitzfelder B. E., Zeber J. E., Morales L. S., Ahmed A. T., et al. (2016). Racial-ethnic differences in psychiatric diagnoses and treatment across 11 health care systems in the mental health research network. Psychiatr. Serv. 67, 749–757. 10.1176/appi.ps.201500217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosio D., Lin E. (2018). Role of active vs. passive complementary and integrative health approaches in pain management. Global Adv. Health Med. 7:216495611876849. 10.1177/2164956118768492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig P. (2019). Developing and Evaluating Complex Interventions. London. Retrieved from: www.mrc.ac.uk/complexinterventionsguidance [Google Scholar]
- Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I., Petticrew M. (2008). Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 337:1–39. 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deatrich K. G., Prout M. F., Boyer B. A., Yoder S. E. (2016). Effectiveness of group music therapy in a psychiatric hospital: a randomized pilot study of treatment outcome. Int. J. Group Psychother. 66, 592–617. 10.1080/00207284.2016.1190239 [DOI] [PubMed] [Google Scholar]
- Dodd S., Clarke M., Becker L., Mavergames C., Fish R., Williamson P. R. (2018). A taxonomy has been developed for outcomes in medical research to help improve knowledge discovery. J. Clin. Epidemiol. 96, 84–92. 10.1016/j.jclinepi.2017.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Zhu G. (2020). Psychological interventions for people affected by the COVID-19 epidemic, in The Lancet Psychiatry (Vol. 7) (Elsevier Ltd; ), 300–302. 10.1016/S2215-0366(20)30073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwan K., Altman D. G., Arnaiz J. A., Bloom J., Chan A. W., Cronin E., et al. (2008). Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS ONE 3:e3081. 10.1371/journal.pone.0003081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger N., Cole S. W. (2012). Social neuroscience and health: neurophysiological mechanisms linking social ties with physical health. Nat. Neurosci. 15:6690674. 10.1038/nn.3086 [DOI] [PubMed] [Google Scholar]
- Esparza J. (2016). Using Person-Centered Expressive Arts Group Therapy With Combat-Related PTSD Veterans. ProQuest Information & Learning. Retrieved from: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2016-31155-090&site=ehost-live&scope=siteNS~-
- Fancourt D., Finn S. (2019). What is the evidence on the role of the arts in improving health and well-being? A scoping review. WHO Regional Office Europe. Available onlien at: http://www.euro.who.int/en/publications/abstracts/what-is-the-evidence-on-the-role-of-the-arts-in-improving-health-and-well-being-a-scoping-review-2019 [PubMed]
- Fancourt D., Perkins R., Ascenso S., Carvalho L. A., Steptoe A., Williamon A. (2016). Effects of group drumming interventions on anxiety, depression, social resilience and inflammatory immune response among mental health service users. PLoS ONE. 11:e0151136. 10.1371/journal.pone.0151136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquharson W. H., Thornton C. J. (2020). Debate: Exposing the most serious infirmity – racism's impact on health in the era of COVID-19. Child Adolesc. Ment. Health. 25, 182–183. 10.1111/camh.12407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faurholt-Jepsen M., Geddes J. R., Goodwin G. M., Bauer M., Duffy A., Vedel Kessing L., Saunders K. (2019). Reporting guidelines on remotely collected electronic mood data in mood disorder (eMOOD)—recommendations. Transl. Psychiatry. 9:162. 10.1038/s41398-019-0484-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geretsegger M., Mössler K. A., Bieleninik Ł., Chen X.-J., Heldal T. O., Gold C. (2017). Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochr. Database System. Rev. 5:CD004025. 10.1002/14651858.CD004025.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasziou P., Meats E., Heneghan C., Shepperd S. (2008). What is missing from descriptions of treatment in trials and reviews? BMJ 336, 1472–1474. 10.1136/bmj.39590.732037.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glicksohn J., Cohen Y. (2000). Can music alleviate cognitive dysfunction in schizophrenia? Psychopathology 33, 43–47. 10.1159/000029118 [DOI] [PubMed] [Google Scholar]
- Gold C., Wigram T., Elefant C. (2006). Music therapy for autistic spectrum disorder, in Cochrane Database of Systematic Reviews (John Wiley & Sons, Ltd; ). 10.1002/14651858.CD004381.pub2 [DOI] [PubMed] [Google Scholar]
- Gosselin E., Gélinas C., Bourgault P., Lavoie S. (2019). Intervention for Patients Intubated and Conscious to decrease Peritraumatic Distress (IPIC-PTD) – Acceptability and Feasibility. 10.31770/2561-7516.1019 [DOI] [Google Scholar]
- Grasser L. R., Al-Saghir H., Wanna C., Spinei J., Javanbakht A. (2019). Moving through the trauma: dance/movement therapy as a somatic-based intervention for addressing trauma and stress among syrian refugee children, in Journal of the American Academy of Child and Adolescent Psychiatry (Vol. 58) (Elsevier Inc.), 1124–1126. 10.1016/j.jaac.2019.07.007 [DOI] [PubMed] [Google Scholar]
- Greenberg N. (2020, August 1). Mental Health of Health-Care Workers in the COVID-19 Era. Nature Reviews Nephrology. Nature Research. 10.1038/s41581-020-0314-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grocke D., Bloch S., Castle D. (2008). Is there a role for music therapy in the care of the severely mentally ill? Austral. Psychiatry 16, 442–445. 10.1080/10398560802366171 [DOI] [PubMed] [Google Scholar]
- Guétin S., Soua B., Voiriot G., Picot M. C., Hérisson C. (2009). The effect of music therapy on mood and anxiety-depression: an observational study in institutionalised patients with traumatic brain injury. Ann. Phys. Rehabil. Med. 52, 30–40. 10.1016/j.annrmp.2008.08.009 [DOI] [PubMed] [Google Scholar]
- Guise J.-M., Chang C., Butler M., Viswanathan M., Tugwell P. (2017). AHRQ series on complex intervention systematic reviews—paper 1: an introduction to a series of articles that provide guidance and tools for reviews of complex interventions. J. Clin. Epidemiol. 90, 6–10. 10.1016/j.jclinepi.2017.06.011 [DOI] [PubMed] [Google Scholar]
- Gutiérrez E. O. F., Camarena V. A. T. (2015). Music therapy in generalized anxiety disorder. Arts Psychother. 44, 19–24. 10.1016/j.aip.2015.02.003 [DOI] [Google Scholar]
- He H., Yang M., Duan M., Chen X., Lai Y., Xia Y., et al. (2018). Music intervention leads to increased insular connectivity and improved clinical symptoms in schizophrenia. Front. Neurosci. 11:744. 10.3389/fnins.2017.00744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Ruiz E. (2005). Effect of music therapy on the anxiety levels and sleep patterns of abused women in shelters, in Journal of Music Therapy (Vol. 42) (American Music Therapy Association; ), 140–158. 10.1093/jmt/42.2.140 [DOI] [PubMed] [Google Scholar]
- Higgins J., Thomas J. (2020). Cochrane Handbook for Systematic Reviews of Interventions | Cochrane Training. Available online at: https://training.cochrane.org/handbook/current (accessed November 25, 2020).
- Hoffmann T. C., Glasziou P. P., Boutron I., Milne R., Perera R., Moher D., et al. (2014). Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 348, 348–1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T. B., Layton J. B. (2010). Social relationships and mortality risk: a meta-analytic review. PLoS Med. 7:e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovey S. A. (2013). The effects of musical activity on the self-esteem and self-efficacy of patients with schizophrenia: a cultural study in west bengal, india. Music Med. 5, NP1–NP4. 10.1177/1943862112467465 [DOI] [Google Scholar]
- Jin Y., Sanger N., Shams I., Luo C., Shahid H., Li G., et al. (2018). Does the medical literature remain inadequately described despite having reporting guidelines for 21 years? – A systematic review of reviews: an update. J. Multidiscip. Healthc. 11, 495–510. 10.2147/JMDH.S155103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaloupek D. G., Chard K. M., Freed M. C., Peterson A. L., Riggs D. S., Stein M. B., et al. (2010). Common data elements for posttraumatic stress disorder research. Kamioka Am. Congress Rehabil. Med. 91, 1684–1691. 10.1016/j.apmr.2010.06.032 [DOI] [PubMed] [Google Scholar]
- Kilbourne A. M., Beck K., Spaeth-Rublee B., Ramanuj P., O'Brien R. W., Tomoyasu N., Pincus H. A. (2018). Measuring and improving the quality of mental health care: a global perspective. World Psychiatry. 17, 30–38. 10.1002/wps.20482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham J. J., Dwan K. M., Altman D. G., Gamble C., Dodd S., Smyth R., et al. (2010). The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ 340, 637–640. 10.1136/bmj.c365 [DOI] [PubMed] [Google Scholar]
- Kreutz G. (2014). Does singing facilitate social bonding? Music Med. 6:51. 10.47513/mmd.v6i2.180 [DOI] [Google Scholar]
- Laurencin C. T., McClinton A. (2020). The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J. Rac. Ethnic Health Dispar. 7, 398–402. 10.1007/s40615-020-00756-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehrer-Carle I. (1971). Group dynamics as applied to the use of music with schizophrenic adolescents. J. Contemp. Psychother. 3, 111–116. 10.1007/BF02110244 [DOI] [Google Scholar]
- Leman M., Maes P. J. (2015). The role of embodiment in the perception of music. Empir. Music. Rev. 9, 236–246. 10.18061/emr.v9i3-4.4498 [DOI] [Google Scholar]
- Levitin D. J., Grahn J. A., London J. (2018). The psychology of music: rhythm and movement. Annu. Rev. Psychol. 69, 51–75. 10.1146/annurev-psych-122216-011740 [DOI] [PubMed] [Google Scholar]
- Løkken B. I., Rangul V., Merom D., Ekholm O., Krokstad S., Sund E. R. (2018). Are playing instruments, singing or participating in theatre good for population health? Associations with self-rated health and all-cause mortality in the HUNT3 study (2006-2008), Norway, in Music and Public Health: A Nordic Perspective (Springer International Publishing; ), 33–54. 10.1007/978-3-319-76240-1_3 [DOI] [Google Scholar]
- Macfarlane C., Masthoff E., Hakvoort L. (2019). Short-Term music therapy attention and arousal regulation treatment (SMAART) for prisoners with posttraumatic stress disorder: a feasibility study. J. Foren. Psychol. Res. Practice 19, 376–392. 10.1080/24732850.2019.1670023 [DOI] [Google Scholar]
- McCaffrey R., Locsin R. C. (2002). Music listening as a nursing intervention: a symphony of practice. Holistic Nurs. Pract. 16, 70–77. 10.1097/00004650-200204000-00012 [DOI] [PubMed] [Google Scholar]
- McFerran K. S., Hense C., Koike A., Rickwood D. (2018). Intentional music use to reduce psychological distress in adolescents accessing primary mental health care. Clin. Child Psychol. Psychiatry 23, 567–581. 10.1177/1359104518767231 [DOI] [PubMed] [Google Scholar]
- McGowan J., Sampson M., Salzwedel D. M., Cogo E., Foerster V., Lefebvre C. (2016). PRESS Peer review of electronic search strategies: 2015 guideline statement. J. Clin. Epidemiol. 75, 40–46. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- McPherson T., Berger D., Alagapan S., Fröhlich F. (2019). Active and passive rhythmic music therapy interventions differentially modulate sympathetic autonomic nervous system activity. J. Music Ther. 56, 240–264. 10.1093/jmt/thz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meekums B., Karkou V., Nelson E. A. (2015). Dance movement therapy for depression, in Cochrane Database of Systematic Reviews (Vol. 2015) (John Wiley and Sons Ltd; ). 10.1002/14651858.CD009895.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moe T. (2002). Restitutional factors in receptive group music therapy inspired by GIM. Nord. J. Music Ther. 11, 152–166. 10.1080/08098130209478057 [DOI] [Google Scholar]
- Möhler R., Köpke S., Meyer G. (2015). Criteria for reporting the development and evaluation of complex interventions in healthcare: revised guideline (CReDECI 2). Trials 16:204. 10.1186/s13063-015-0709-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy S., Gomersall C. D., Fowler R. A. (2020). Care for “Critically Ill Patients with COVID-19, in JAMA - Journal of the American Medical Association (Vol. 323) (American Medical Association; ), 1499–1500. 10.1001/jama.2020.3633 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2019). Mental Illness. Available online at: https://www.nimh.nih.gov/health/statistics/mental-illness.shtml (accessed August 31, 2020).
- Osborne N. (2012). Neuroscience and “real world” practice: Music as a therapeutic resource for children in zones of conflict. Annals N. Y. Acad. Sci. 1252, 69–76. 10.1111/j.1749-6632.2012.06473.x [DOI] [PubMed] [Google Scholar]
- Panchal N., Kamal R., Orgera K., Cox C., Garfield R., Hamel L., et al. (2020, August 21). The Implications of COVID-19 for Mental Health and Substance Use | KFF. Retrieved from: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ (accessed August 31, 2020).
- Papadopoulos N. L. R., Röhricht F. (2014). An investigation into the application and processes of manualised group body psychotherapy for depressive disorder in a clinical trial. Body Mov. Dance Psychother. 9, 167–180. 10.1080/17432979.2013.847499 [DOI] [Google Scholar]
- Peters M., Godfrey C., McInerney P., Munn Z., Trico A., Khalil H. (2020). Chapter 11: scoping reviews, in JBI Manual for Evidence Synthesis (JBI; ). 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- Petrovsky D., Cacchione P. Z., George M. (2015). Review of the effect of music interventions on symptoms of anxiety and depression in older adults with mild dementia, in International Psychogeriatrics (Vol. 27) (Cambridge University Press; ), 1661–1670. 10.1017/S1041610215000393 [DOI] [PubMed] [Google Scholar]
- Petticrew M. (2011). When are complex interventions “complex”? When are simple interventions “simple”? Europ. J. Public Health 21, 397–398. 10.1093/eurpub/ckr084 [DOI] [PubMed] [Google Scholar]
- Pezzin L. E., Larson E. R., Lorber W., McGinley E. L., Dillingham T. R. (2018). Music-instruction intervention for treatment of post-traumatic stress disorder: A randomized pilot study. BMC Psychol. 6:60. 10.1186/s40359-018-0274-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poldrack R. A., Fletcher P. C., Henson R. N., Worsley K. J., Brett M., Nichols T. E. (2008). Guidelines for reporting an fMRI study. NeuroImage 40, 409–414. 10.1016/j.neuroimage.2007.11.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pölkki T., Korhonen A., Laukkala H. (2012). Nurses' expectations of using music for premature infants in neonatal intensive care unit. J. Pediatr. Nurs. 27, e29–e37. 10.1016/j.pedn.2011.06.001 [DOI] [PubMed] [Google Scholar]
- Prakash R. (2019). Passive and Active Music Therapy. Retrieved from: https://sites.duke.edu/voicestogether/series-the-potential-power-of-music-therapy-within-the-autism-community/passive-and-active-music-therapy/ (accessed November 19, 2020)
- Preyde M., Berends A., Parehk S., Heintzman J. (2017). Adolescents' evaluation of music therapy in an inpatient psychiatric unit: a quality improvement project. Music Ther. Persp. 35, 58–62. 10.1093/mtp/miv008 [DOI] [Google Scholar]
- Pylvänäinen P., Lappalainen R. (2018). Change in body image among depressed adult outpatients after a dance movement therapy group treatment. Arts Psychother. 59, 34–45. 10.1016/j.aip.2017.10.006 [DOI] [Google Scholar]
- Pylvänäinen P. M., Muotka J. S., Lappalainen R. (2015). A dance movement therapy group for depressed adult patients in a psychiatric outpatient clinic: effects of the treatment. Front. Psychol. 6:980. 10.3389/fpsyg.2015.00980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robb S. L., Carpenter J. S., Burns D. S. (2011). Reporting guidelines for music-based interventions, in Journal of Health Psychology (SAGE Publications Ltd.) 10.1177/1359105310374781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin H. E., Katz E. (1946). Auroratone films for the treatment of psychotic depressions in an army general hospital. J. Clin. Psychol. 2, 333–340. [DOI] [PubMed] [Google Scholar]
- Ryan R., Hill S., Prictor M., McKenzie Last J. (2013). Cochrane Study Quality Guide. Retrieved from: https://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/StudyQualityGuide_May%202013.pdf
- Schroeder M. O. (2018, May). Accessing the Mental Health Benefits of Music Therapy. U.S. News & World Report. [Google Scholar]
- Shagan S., Shagan D., Shagan B., Fiszdon J. M., Thime W., Haber L. C., Pearlson G. D., Choi J. (2018). How music impacts visual attention training in schizophrenia: a pilot study. J. Nerv. Mental Dis. 206, 968–970. 10.1097/NMD.0000000000000911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp M. K., Bertizzolo L., Rius R., Wager E., Gómez G., Hren D. (2019). Using the STROBE statement: survey findings emphasized the role of journals in enforcing reporting guidelines. J. Clin. Epidemiol. 116, 26–35. 10.1016/j.jclinepi.2019.07.019 [DOI] [PubMed] [Google Scholar]
- Silverman M. J. (2019). Music therapy for coping self-efficacy in an acute mental health setting: a randomized pilot study. Commun. Ment. Health J. 55, 615–623. 10.1007/s10597-018-0319-8 [DOI] [PubMed] [Google Scholar]
- Solli H. P., Rolvsjord R. (2015). The Opposite of Treatment”: a qualitative study of how patients diagnosed with psychosis experience music therapy. Nord. J. Music Ther. 24, 67–92. 10.1080/08098131.2014.890639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoorthy M. S. (2020). Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review, in Asian Journal of Psychiatry (Vol. 51) (Elsevier B.V; ), 102119. 10.1016/j.ajp.2020.102119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel Z., Marnane C., Iranpour C., Chey T., Jackson J. W., Patel V., et al. (2014). The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int. J. Epidemiol. 43, 476–493. 10.1093/ije/dyu038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg-Oren S. L., Krasnova M., Krasnov I. S., Baker M. R., Ames D. (2016). Let's dance: a holistic approach to treating veterans with posttraumatic stress disorder, in Federal Practitioner (Vol. 33) (Frontline Medical Communications; ). Available online at: www.fedprac.comProgramProfile [PMC free article] [PubMed] [Google Scholar]
- Strauss M., van Heerden S. M., Joubert G. (2016). Occupational therapy and the use of music tempo in the treatment of the mental health care user with psychosis. South Afric. J. Occup. Ther. 46, 21–26. 10.17159/2310-3833/2016/v46n1a6 [DOI] [Google Scholar]
- Tan S., Zou Y., Wykes T., Reeder C., Zhu X., Yang F., et al. (2016). Group cognitive remediation therapy for chronic schizophrenia: a randomized controlled trial. Neurosci. Lett. 626, 106–111. 10.1016/j.neulet.2015.08.036 [DOI] [PubMed] [Google Scholar]
- The Joanna Briggs Institute. (2015). The Joanna Briggs Institute Reviewers' Manual 2015: Methodology for JBI Scoping Reviews. Retrieved from: https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Scoping-.pdf
- Theorell T., Kreutz G. (2012). Epidemiological studies of the relationship between musical experiences and public health, in Music, Health, and Wellbeing (Oxford University Press; ). 10.1093/acprof:oso/9780199586974.003.0028 [DOI] [Google Scholar]
- Thompson W. (2014). Music in the social and behavioral sciences: an encyclopedia, in Music in the Social and Behavioral Sciences: An Encyclopedia. 10.4135/9781452283012 [DOI] [Google Scholar]
- Tornek A., Field T., Hernandez-Reif M., Diego M., Jones N. (2003). Music Effects on EEG in intrusive and withdrawn mothers with depressive symptoms. Psychiatry 66, 234–243. 10.1521/psyc.66.3.234.25157 [DOI] [PubMed] [Google Scholar]
- Tricco A. C., Lillie E., Zarin W., O'Brien K. K., Colquhoun H., Levac D., et al. (2018, October 2). PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine. American College of Physicians. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Trimmer C., Tyo R., Pikard J., McKenna C., Naeem F. (2018). Low-intensity cognitive behavioural therapy-based music group (CBT-music) for the treatment of symptoms of anxiety and depression: a feasibility study. Behav. Cogn. Psychother. 46, 168–181. 10.1017/S1352465817000480 [DOI] [PubMed] [Google Scholar]
- Umberson D., Karas Montez J. (2010). Social relationships and health: a flashpoint for health policy. J. Health Soc. Behav. 51, S54–S66. 10.1177/0022146510383501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Westrhenen N., Fritz E. (2014). Creative Arts Therapy as treatment for child trauma: an overview. Arts Psychothe. 41, 527–534. 10.1016/j.aip.2014.10.004 [DOI] [Google Scholar]
- Veerman S. R. T., Schulte P. F. J., de Haan L. (2017). Treatment for negative symptoms in schizophrenia: a comprehensive review, in Drugs (Vol. 77) (Springer International Publishing; ), 1423–1459. 10.1007/s40265-017-0789-y [DOI] [PubMed] [Google Scholar]
- Ventouras E. C., Margariti A., Chondraki P., Kalatzis I., Economou N. T., Tsekou H., et al. (2015). EEG-based investigation of brain connectivity changes in psychotic patients undergoing the primitive expression form of dance therapy: a methodological pilot study. Cogn. Neurodyn. 9, 231–248. 10.1007/s11571-014-9319-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigo D., Thornicroft G., Atun R. (2016, February 1). Estimating the true global burden of mental illness, in The Lancet Psychiatry (Elsevier Ltd; ). 10.1016/S2215-0366(15)00505-2 [DOI] [PubMed] [Google Scholar]
- Vigo D. V., Kestel D., Pendakur K., Thornicroft G., Atun R. (2019). Disease burden and government spending on mental, neurological, and substance use disorders, and self-harm: cross-sectional, ecological study of health system response in the Americas. Lancet Public Health. 4, e89–e96. 10.1016/S2468-2667(18)30203-2 [DOI] [PubMed] [Google Scholar]
- Wang S., Agius M. (2018). The use of music therapy in the treatment of mental illness and the enhancement of societal wellbeing, in Psychiatria Danubina (Vol. 30) (Medicinska Naklada Zagreb; ), S595–S600. [PubMed] [Google Scholar]
- Welch G. F., Himonides E., Saunders J., Papageorgi I., Sarazin M. (2014). Singing and social inclusion. Front. Psychol. 5:803. 10.3389/fpsyg.2014.00803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- West S. L., Gartlehner G., Mansfield A. J., Poole C., Tant E., Lenfestey N., et al. (2010). Comparative Effectiveness Review Methods: Clinical Heterogeneity. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK53310/ [PubMed]
- Whiteford H., Ferrari A., Degenhardt L. (2016). Global burden of disease studies: Implications for mental and substance use disorders. Health Aff. 35, 1114–1120. 10.1377/hlthaff.2016.0082 [DOI] [PubMed] [Google Scholar]
- Whiteford H. A., Degenhardt L., Rehm J., Baxter A. J., Ferrari A. J., Erskine H. E., et al. (2013). Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet 382, 1575–1586. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- Wilbur S., Meyer H. B., Baker M. R., Smiarowski K., Suarez C. A., Ames D., Rubin R. T. (2015). Dance for veterans: a complementary health program for veterans with serious mental illness. Arts and Health. 7, 96–108. 10.1080/17533015.2015.1019701 [DOI] [Google Scholar]
- Williams E., Dingle G. A., Clift S. (2018). A systematic review of mental health and wellbeing outcomes of group singing for adults with a mental health condition. Eur. J. Public Health. 28, 1035–1042. 10.1093/eurpub/cky115 [DOI] [PubMed] [Google Scholar]
- Williamson P. R., Altman D. G., Blazeby J. M., Devane D., Gargon E., Tugwell P. (2012). Developing core outcome sets for clinical trials: issues to consider. Trials 13:132. 10.1186/1745-6215-13-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., jiao Bai Y., mei Qin L., Xu X., lan Bao K., fang Xiao J., et al. (2019). The effectiveness of music therapy for postpartum depression: a systematic review and meta-analysis, in Complementary Therapies in Clinical Practice (Vol. 37) (Churchill Livingstone; ), 93–101. 10.1016/j.ctcp.2019.09.002 [DOI] [PubMed] [Google Scholar]
- Zarate R. (2016). Clinical Improvisation and its effect on anxiety: a multiple single subject design. Arts Psychother. 48, 46–53. 10.1016/j.aip.2015.11.005 [DOI] [Google Scholar]
- Zarobe L., Bungay H. (2017, November 1). The role of arts activities in developing resilience and mental wellbeing in children and young people a rapid review of the literature, in Perspectives in Public Health (SAGE Publications Ltd; ). 10.1177/1757913917712283 [DOI] [PubMed] [Google Scholar]
- Zidani M., Audet J. S., Borgeat F., Aardema F., O'Connor K. P., Khazaal Y. (2017). Augmentation of psychotherapy through alternative preconscious priming: a case series exploring effects on residual symptoms. Front. Psychiatry 8:8. 10.3389/fpsyt.2017.00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.