Abstract
Background
Special care units are a well-utilized approach in the long-term care for persons with dementia. A therapeutic goal of such settings is to provide meaningful engagement and a sense of community that is crucial for the overall quality of life. In recent years, several studies followed this notion by investigating residents’ social interactions and the influence of the environment on these interactions.
Aims
This review aims to synthesize the literature on the social interactions of persons with dementia living in special care units.
Design
A mixed-methods systematic review was conducted.
Methods
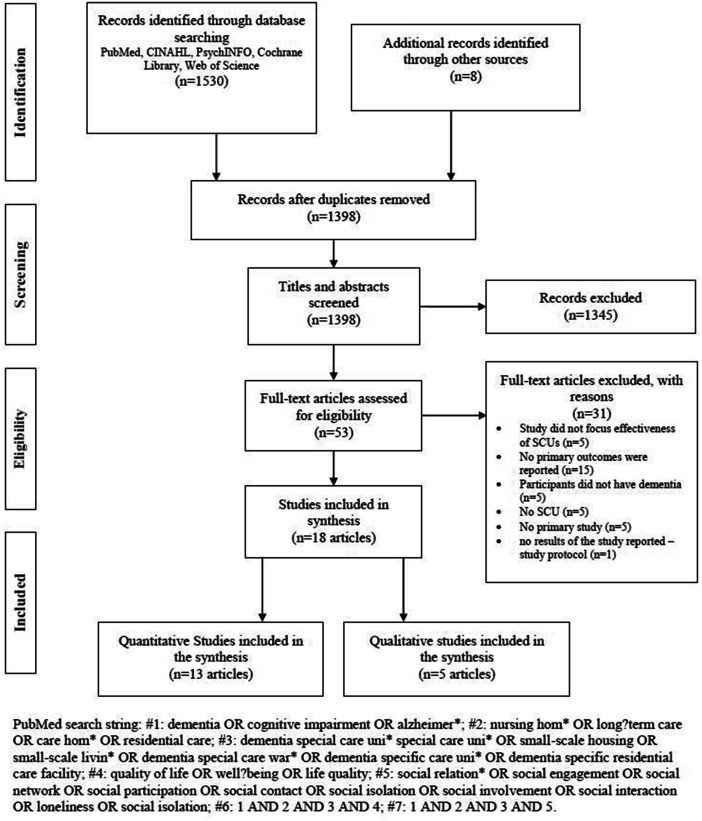
Literature was searched in PubMed, CINAHL, PsycINFO, the Cochrane Library and Web of Science databases. Additionally, reference lists of relevant articles were searched. Studies were screened, data were extracted and the quality was appraised. Separate syntheses were conducted for qualitative and quantitative studies, which were subsequently merged in the final mixed-methods synthesis.
Results
In total, 18 articles were included, investigating large-scale, small-scale and homelike special care units and green care farms. Residents in special care units experience few social interactions but more than those in the comparative groups. Opportunities to interact are only marginally seized. Interactions typically occur in small groups and are facilitated by familiarity and the organizational environment. Residents mainly rely on staff members to create social interaction, for example initiating or facilitating resident-to-resident interaction.
Conclusion
Although the evidence base is increasing, it is still fragmented and built on different concepts, interventions, control groups and measurements. Nevertheless, the first conclusions suggest a positive impact of special care units on residents’ social interactions. Although the review yielded a more comprehensive picture of residents’ social life, further high-quality research built on a sound theoretical background is needed.
Keywords: dementia, social interaction, special care unit, long-term care, systematic review
Introduction
Over half of all nursing home residents in Western countries are persons with dementia, a population with complex physical and psychosocial care needs (Harris-Kojetin et al., 2016; Hoffmann et al., 2014). In long-term care settings, they often experience a loss of abilities and freedom (Forsund et al., 2018), as well as a lower quality of life and less social connectedness (Nikmat et al., 2015). However, evidence is mounting that residential facilities can not only have a debilitating impact but can also have a therapeutic impact on persons with dementia (Calkins, 2018). Environmental characteristics, such as unit size, spatial layout, homelike character, sensory stimulation and characteristics of social spaces significantly influence residents’ behaviour and well-being (Chaudhury et al., 2017).
One approach, used by many healthcare providers worldwide to improve the quality of care for persons with dementia using environmental characteristics, is the establishment of special care units for persons with dementia (Joyce et al., 2018). Although there is no concrete definition of special care units, the shared understanding is that they refer to units for persons with dementia who experience difficult or distressed behaviours. The structural design, specifically trained staff and activities are adopted to residents’ needs to offer a supportive environment for residents (Joyce et al., 2018; Kok et al., 2013; Palm & Bartholomeyczik, 2018). Since there is no common definition for special care units, their designs vary (Brandenburg, 2013). Some special care units are large wards with a special group-living structure or homelike community areas (Morgan-Brown et al., 2013; Nakanishi et al., 2012). Others implement small-scale, homelike wards for five to eight residents, sometimes separated from the main facility and built as stand-alone houses (De Rooij et al., 2012; Verbeek et al., 2010) or designed as farms (De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a).
In recent years, there has been a considerable increase in studies investigating special care units where quality of life was regarded as the primary outcome and was found to be better in special care unit residents compared to residents of traditional nursing homes (De Boer, Hamers, Zwakhalen, Tan, & Verbeek, 2017b; Kok et al., 2013). These findings are reinforced by the notion that the therapeutic goals of settings designed for persons with dementia, comprising the enhancement of well-being and dignity, provision of opportunities for choice and meaningful engagement, as well as the creation of a sense of community, are reflected in major realms of quality of life, including autonomy, social relations, feeling at home and having something to do (Ettema et al., 2007).
An increasing number of studies have explored social interactions, relationships, integration and networks of special care unit residents as a domain of quality of life (Abbott et al., 2017; De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a). Social relations and interactions, together with being in company and connected to others, are an essential part of the overall quality of life (O’Rourke et al., 2015) and contributors to physical and mental health (Smith & Christakis, 2008). Research on social interactions dates back to the microsociology of Goffman (1959)who studied the dynamic sequences of social actions between individuals or groups modified in reaction to the action of the interaction partner(s). Social interactions are the roots of social structures and cultures. For residents with dementia, social interactions may be a challenge because the cognitive-communicative impairments associated with dementia, such as recalling names and phrases, are enhanced by the circumstance of living in an environment consisting of unfamiliar persons and settings (O'Rourke et al., 2015). In long-term care settings, contacts with family, friends and significant others often decrease, creating a feeling of social isolation for some residents. Others conversely describe an expansion of social contacts as the setting provides spaces for persons to meet and opportunities to participate in social activities (Forsund et al., 2018). Consequently, the nursing home is not merely a physical location but also a social community where meaningful reciprocal relationships can be formed (Brown Wilson, 2009).
Thus far, various concepts and phenomena have been studied from different perspectives. To enable a more comprehensive understanding of social interactions in special care units, the fragmented body of qualitative and quantitative evidence must be brought together and interlinked. An emerging approach to integrate diverse types of research in one review is mixed-mixed methods systematic reviews. By synthesizing results of qualitative and quantitative studies, mixed-methods systematic reviews maximize the evidence-base and benefit for research, practice and policy. Therefore, the objective of this study is a mixed-methods systematic review to synthesize the existing literature on social interactions of persons with dementia living in special care units in long-term care by addressing the following question:
How can the social interactions of persons with dementia living in special care units be described?
Materials and methods
A systematic literature review (Grant & Booth, 2009; Higgins & Green, 2011) with a mixed-methods synthesis was conducted on the social interactions of persons with dementia living in special care units. This approach is defined by the integration and synthesis of qualitative and quantitative studies, and therefore allowed the inclusion of sound qualitative research investigating the meaning and composition of constructs in a specific context, as well as rigorous quantitative research assessing the magnitude, frequency and correlations of constructs (Pearson et al., 2015) to explain possible heterogeneity between studies. The result is aimed at a synthesis with diverse studies complementing and thus expanding each other.
This literature review is exempt from the approval of an ethics committee as it is based on data from former qualitative and quantitative studies for which the authors of the original studies obtained ethics approval and informed consent from participants.
Data sources and search strategy
A comprehensive literature search was conducted in PubMed, CINAHL, PsycINFO, Cochrane library and Web of Science in July and August 2018. The database search was undertaken with controlled vocabulary and free terms in combination with Boolean operators, truncations, wildcards and no time restrictions. The search strategy was developed for PubMed and adapted for the other databases. The search string for PubMed is provided in Figure 1. Additionally, the reference lists of relevant articles were searched for potential related articles.
Figure 1.
Flow diagram of study selection (PRISMA flow diagram) and PubMed search string.
SCU: special care unit.
Study selection
Studies were included in this review if they were peer-reviewed and published in English or German (a), reporting the results of a primary study (b) of residential special care units or small-scale living facilities for persons with dementia (c) in long-term care (d) examining social interactions (e) of the residents. Relevant review articles were scanned for studies meeting the criteria (a) to (e), and these were included in this review.
After duplicates were removed, two researchers (LA and TN) independently screened titles, abstracts and, subsequently, the remaining full texts for eligibility based on the above-described inclusion criteria. Disagreement between the two researchers about exclusion or inclusion mostly concerned criteria (b) and (c) and was discussed until consensus was reached.
Assessment of study quality
The methodological quality of the included studies was appraised independently by two researchers (LA and CH). Criteria for the appraisal were based on the Joanna Briggs Institute’s Checklists for Quasi-Experimental Studies, for Cohort Studies, for Analytical Cross-Sectional Studiesand for Qualitative Research(Aromataris & Munn, 2017). For the purpose of the study, the checklists were adjusted by extending them to the criteria of Joanna Briggs Institute’s checklists for other designs. This made it possible to assess sampling strategies and descriptions of study subjects and interventions, as well as possible confounding factors in quantitative experimental and cohort studies in all relevant designs. Differences in opinions between the two researchers regarding the assessment of study quality emerged mainly on the assessment of the appropriateness of sampling strategies, inclusion criteria, similarity of groups and the comprehensiveness of the description of study subjects. Concerns were discussed until consensus was reached.
Data extraction
The data extraction form was developed by the first author and reviewed by the second and third authors. The following data were extracted from the studies: reference, study design, objective, setting, type of residential care model under study, sample size and sample characteristics. For quantitative studies, additionally, outcome variables, their measurements, time points and control of confounding factors were extracted. Group by time effects were described for studies with repeated measures analyses; for all other quantitative studies, overall group comparisons were analysed. The results controlled for confounding factors were presented when reported in the primary studies. Data extraction for qualitative studies further included data collection and analysis methods, as well as the main themes and categories of the results. Extraction was performed by LA.
Method of results synthesis
The social interactions of special care unit residents were reported in qualitative and quantitative studies; therefore, a mixed-methods synthesis was conducted. For this purpose, a segregated approach was chosen that required individual syntheses of qualitative and quantitative studies to maintain a clear distinction between the methodologies before they are synthesised in the final mixed-methods synthesis (Pearson et al., 2015; Sandelowski et al., 2006).
The synthesis was conducted in three steps. First (1), all studies were separately summarized in a narrative textual description and were illustrated in tables depicting the data described in the section data extraction (see supplementary material – characteristics and results of the included qualitative and quantitative studies). Qualitative and quantitative studies investigated mostly different aspects of social interaction.
Second (2), the qualitative and quantitative data were synthesised separately. Qualitative studies (2a) were analysed by applying thematic synthesis (Thomas & Harden, 2008). This analysis process consisted of the following steps: (i) relevant findings of the included studies were coded line-by-line. All lines of the result-sections of the included studies, that in some way dealt with social interaction, were coded according to their meaning and content. The line-by-line coding was not only a process of data extraction but also of translating the studies into one another. An example of a code was ‘interactions often initiated by staff’. (ii) Descriptive themes were developed by looking at differences and similarities of the codes and grouping them in a hierarchical structure. Descriptive themes are close to the original results and reflect them in diverse levels of abstraction. For example, the code above is displayed by the descriptive themes ‘staff roles’ and ‘social interactions promoting factors’. (iii) In the next step, analytical themes were constructed. These themes ideally go beyond the original findings and provide new insights into the topic regarding the research question. In the example, the analytical theme was ‘creation of interaction by special care unit staff members’.
Quantitative studies (2b) were categorized according to their intervention and control groups, and the findings were classified as significantly positive, positive, neither positive nor negative, negative or significantly negative. In the context of the respective outcomes, the heterogeneity of study designs, interventions and comparators, a meta-analysis could not be performed; therefore, a narrative synthesis of the results was performed (Popay et al., 2006). The similarities and differences of the tabulated findings were analysed and narratively described.
In a third step (3), the results of the two syntheses were brought together by conversion of data and were, in a third synthesis, subsequently analysed together (Dai & Livesley, 2018; Möhler & Meyer, 2014). The qualitative and quantitative studies investigated mainly different aspects; thus, they complemented each other and provided explanations for possible heterogeneity between studies. The themes and narratives were entered into a matrix. Therefore, related, opposing and complementing aspects were identified and depicted in higher-level themes. Synthesis was performed by LA and discussed several times with the other authors.
Results
Study selection and characteristics
The systematic literature search yielded 1397 non-redundant articles, among which 18 were included in the review. Figure 1shows the selection process and reasons for exclusion. The articles included five quasi experimental studies (De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; De Rooij et al., 2012; Kok et al., 2018; Verbeek et al., 2010; Wolf-Ostermann et al., 2012), one prospective cohort study (Van der Zon et al., 2018), seven cross-sectional studies (Abbott & Pachucki, 2017; Abbott et al., 2017; Abrahamson et al., 2012; De Boer, Hamers, Zwakhalen, Tan, & Verbeek, 2017a; Morgan-Brown et al., 2013; Weyerer et al., 2010; Wood et al., 2005) and five qualitative studies (Aasgaard et al., 2017; Campo & Chaudhury, 2012; Doyle et al., 2012; Moore, 1999; Moore & Verhoef, 1999).
Description of the studied special care units
The features of the investigated special care units are barely described in most articles, impeding the comparison between studies (see supplementary material – characteristics and results of the included studies). The reported descriptions mainly focus on architectural features, suggesting differences in unit size and spatial layout of the special care units and not detailing other features of the special care units. Four articles report on large-scale special care units for more than 20 residents (Campo & Chaudhury, 2012; Doyle et al., 2012; Moore, 1999; Moore & Verhoef, 1999). Special care units for 15–20 residents are analysed in another three articles (Abbott & Pachucki, 2017; Abbott et al., 2017; Morgan-Brown et al., 2013), among which one describes so-called household model units (Morgan-Brown et al., 2013). Three articles report findings on small-scale special care units, referring to units for at most nine residents (Kok et al., 2018; Verbeek et al., 2010; Wood et al., 2005). Two articles describe green care farms, a special type of a small-scale facility in the Netherlands (De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; De Boer, Hamers, Zwakhalen, Tan, & Verbeek, 2017b). The authors of six studies do not describe the features of the special care units at all (Aasgaard et al., 2017; Abrahamson et al., 2012; De Rooij et al., 2012; Van der Zon et al., 2018; Weyerer et al., 2010; Wolf-Ostermann et al., 2012).
Among the quantitative studies, seven define residents with dementia living in traditional nursing homes as the control group (Abbott et al., 2017; Abrahamson et al., 2012; De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; De Boer, Hamers, Zwakhalen, Tan, & Verbeek, 2017; De Rooij et al., 2012; Verbeek et al., 2010; Weyerer et al., 2010). One study uses a large-scale special care unit as a control group (Kok et al., 2018), and another (Morgan-Brown et al., 2013) investigates the same special care unit before and after implementing household environments. A further study compares special care unit to shared housing arrangements (Wolf-Ostermann et al., 2012), and flats in normal apartment buildings in which persons with dementia live together and are cared for by community services. Three studies have no control group (Abbott & Pachucki, 2017; Van der Zon et al., 2018; Wood et al., 2005), and two of them investigate the residents of the special care unit in longitudinal research designs (Abbott & Pachucki, 2017; Van der Zon et al., 2018).
Resident characteristics including cognitive and functional status are reported in all included studies, except in Aasgaard et al. (2017), who investigated health care professionals’ perspective, Campo & Chaudhury (2012)and Moore (1999). The use of different instruments and measurements limits comparability of the information. Further aspects of the studied settings, such as staffing features, were barely reported (see supplementary material – characteristics and results of the included studies).
Description of the concepts examined in relation to social interactions
Research on social interactions of persons with dementia living in special care units is fragmented as demonstrated by the multiple concepts investigated by the included studies. Whereas some articles focus on the microlevel and social interactions (or contacts themselves, others examine concepts requesting recurrent interactions and emotional involvement, such as social relationships social engagement, social groups, social networks), social communities and social life. Additionally, studies investigating primarily quality of life are considered if they report separately findings on domains in relation to social interactions. Table 1provides a brief overview of the concepts examined in the studies. A table detailing the applied definitions of the concepts in the included studies is available from the corresponding author on request.
Table 1.
Overview of the concepts examined in the included studies.
Quality appraisal of the included studies
Quality appraisal (see supplementary material – critical appraisal of included studies) yields moderate (Aasgaard et al., 2017; Abbott & Pachucki, 2017; Abbott et al., 2017; Doyle et al., 2012; Moore & Verhoef, 1999; Van der Zon et al., 2018) to high quality for most studies (Abrahamson et al., 2012; Campo & Chaudhury, 2012; De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; De Boer, Hamers, Zwakhalen, Tan, & Verbeek, 2017b; De Rooij et al., 2012; Kok et al., 2018; Verbeek et al., 2010; Weyerer et al., 2010; Wolf-Ostermann et al., 2012). Three studies show low quality (Moore, 1999; Morgan-Brown et al., 2013; Wood et al., 2005). Table 2depicts a short summary of the main issues arisen in the quality appraisal. The detailed quality appraisal of the included studies is attached in the supplementary material ‘critical appraisal of included studies’. Apart from the criteria of the quantitative appraisal tools, the small sample size in the study of Wood et al. (2005)raises concerns about the appropriateness of the study design in general, the statistical analysis and the external validity of the results. Only two studies (Kok et al., 2018; Wolf-Ostermann et al., 2012) took baseline measurements of residents who were not exposed to the special care unit before the first measurement. The other longitudinal studies followed participants over a defined time, not differentiating regarding their length of stay before the first measurement (De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; De Rooij et al., 2012; Van der Zon et al., 2018; Verbeek et al., 2010; Wolf-Ostermann et al., 2012). The assessment of qualitative studies focuses on the congruity between methodological aspects and results. In some studies, methodological aspects are described in insufficient detail, impairing the quality assessment.
Table 2.
Main issues arisen from the quality appraisal of the included studies.
| Issue | References |
|---|---|
| Quantitative studies | |
| Study subject and setting not described in sufficient detail | Abbott & Pachucki, 2017; Abbott et al., 2017; De Rooij et al., 2012; Kok et al., 2018; Wolf-Ostermann et. al., 2012; Weyerer et al., 2010 |
| Small sample size | Wood et al., 2005 |
| No strategies to deal with (possible) confounding factors stated | Abbott & Pachucki, 2017; Abbott et al., 2017; Morgan-Brown et al., 2013; Wood et al., 2005 |
| Outcomes not measured before the intervention was introduced | De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; De Rooij et al., 2012; Verbeek et al., 2010 |
| Qualitative studies | |
| Congruity between research methodology and data collection is not made explicit | Doyle et al., 2012; Moore, 1999; Moore & Verhoef, 1999 |
| Agreement between research methodology and data analysis is not made distinct | Aasgaard et al., 2017 |
| Connection between research methodology and the interpretation of results is not clear | Aasgaard et al., 2017; Moore, 1999; Moore & Verhoef, 1999 |
Social interactions of persons with dementia in special care units
The synthesis yielded the following five categories addressing the two research questions. Although special care unit residents have more social interactions than residents with dementia in the control groups, their level of social interaction is low and they only seize few opportunities for social interaction and interact in small networks. In special care units, staff members, as well as characteristics of the built environment, promote social interactions.
Low level of social interaction in special care units
A social community is desired by residents and nurses (Aasgaard et al., 2017). However, residents do not interact socially for most of the day (Moore & Verhoef, 1999). For example, residents of a small-scale special care unit in the USA spend 10.5 hours of a 12-hour observation frame not interacting (Wood et al., 2005).
Residents of special care units (Abbott et al., 2017) and green care farms (De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a) have more social interactions than those of traditional nursing homes. Interactions are more likely to occur in the afternoons in special care units. Yet, no differences are reported in the length of interactions and time spent interacting (Abbott et al., 2017). Special care unit residents have more social interactions with staff members (Weyerer et al., 2010), although they report that they do not interact socially with residents as much and in ways they approve as adequate to meet the residents’ psychosocial needs (Aasgaard et al., 2017).
The course of social interactions over time in special care unit residents remains unclear. One study (Van der Zon et al., 2018) finds reduced social relations but also reduced social isolation over a two-year period, whereas another study (Wolf-Ostermann et al., 2012) finds a non-significant increase in social relations and stable scores in social isolation in a 12-month period. Studies comparing special care units to traditional nursing homes and analysing social interactions in the subscales of quality of life report inconsistent results, indicating that residents of special care units still have little but probably slightly more social relations than traditional nursing home residents (Abrahamson et al., 2012; De Boer, Hamers, Zwakhalen, Tan, & Verbeek, 2017b; De Rooij et al., 2012; Morgan-Brown et al., 2013; Verbeek et al., 2010).
Emergence of small networks among special care unit residents
Residents’ social networks are typically small, and several residents are virtually isolated and do not interact with others (Abbott & Pachucki, 2017). Some residents do engage in the social community (Moore, 1999), but preferably in small groups with four to six residents (Campo & Chaudhury, 2012; Doyle et al., 2012). Residents in groups with less or more than four to six members tend to have fewer social interactions (Campo & Chaudhury, 2012). The groups are mainly formed in the dining room and sustain in other spaces, such as group activities in other communal areas (Doyle et al., 2012). Normally, residents stick to their groups and interact little outside these clusters (Doyle et al., 2012). When they build their networks, they tend to be more tied to residents with a higher quality of life and opposed by those with a similar or lower quality of life (Abbott & Pachucki, 2017). Residents also engage more with staff members who are familiar to them; additionally, for staff members, it is easier to interact socially with residents with whom they already have a relationship (Aasgaard et al., 2017). Staff members emphasise they need to know the residents, their preferences and history to understand their expressions, to be familiar to them and to reassure them when they feel lost (Aasgaard et al., 2017). Hence, social interactions between staff members and residents increase when they are familiar to each other; consequently, staff members establish emotional connections with several residents and vice versa.
The number of social contacts with other residents do not differ between special care units and traditional nursing homes (Weyerer et al., 2010).
Low level of seized opportunities for social interactions in special care units
Occasions for interactions arise in places where residents spend time with other residents or staff members. Therefore, most occasions for interaction emerge in communal areas, where residents also spend most of the day (Moore, 1999; Moore & Verhoef, 1999; Morgan-Brown et al., 2013). However, residents seem to seize these opportunities only marginally – e.g. residents do not tend to interact with other residents during group activities (Wood et al., 2005). Inconsistent results are reported on social interaction during meal times. One study reports that most interactions happen around mealtimes and only occur sporadically outside these times (Campo & Chaudhury, 2012). Another study finds little resident-to-resident interaction and little social interaction with staff members, which is mostly limited to assistance with eating and drinking and occasionally included encouragement to eat (Wood et al., 2005). However, most conversations take place during downtimes, when no activities take place (Wood et al., 2005). Outside communal areas, interactions are mainly observed during support in activities of daily living (Wood et al., 2005). Situations related to activities of daily living are seen as the best opportunities for one-on-one conversations between staff members and residents and for the establishment of emotional connections because these conversations usually take place in private rooms and involve intimate situations such as body care (Aasgaard et al., 2017).
Most of the interactions are initiated by staff members, and staff members in special care units are more likely to initiate interactions than staff members in traditional nursing homes (Abbott et al., 2017).
Creation of social interactions by staff
The caring philosophy of an organization has a strong influence on the way staff members interact with residents. A strong caring philosophy in special care units asserts that staff members see social interactions as an important aspect of well-being and acknowledge that the social life of residents with dementia often relies on them (Campo & Chaudhury, 2012; Doyle et al., 2012). Therefore, they try to create opportunities for social engagement by routinely initiating interactions and facilitating informal interactions between residents such as having a snack of their own while sitting with the residents and chatting (Campo & Chaudhury, 2012). However, they interact with residents in different modes, not always promoting social engagement: interacting socially and establishing emotional connections, engaging socially but with a hidden agenda (to get the residents to do something) and interacting with residents only to fulfil physical caring tasks (Aasgaard et al., 2017; Moore, 1999).
Furthermore, staff members describe a dilemma because they state that they do not interact socially with residents as much and in ways they approve as adequate to meet residents’ psychosocial needs. The reasons are a lack of physical presence when tasks in other rooms must be performed and a lack of emotional closeness to some residents because they cannot establish the same relationship with all residents (Aasgaard et al., 2017).
Facilitation of social interactions by the built environment of a special care unit
The built environment defines the frame wherein social interactions take place and thereby shapes opportunities for these to occur. Particularly, homelike facilities, characterized by the presence of familiar objects of their past life and the arrangement of these objects, promote social engagement between residents and between residents and staff members (Campo & Chaudhury, 2012; Morgan-Brown et al., 2013). However, contradictory results are reported on the influence of the unit size (Campo & Chaudhury, 2012; Kok et al., 2018). It appears that, independent of the overall unit size, residents experience more social interaction in facilities that provide spaces to form small social groups (Campo & Chaudhury, 2012). In small-scale, homelike facilities, spaces to promote small social groups are mainly inherent, but they can also exist in large-scale units, such as corners with cosy seating options or small-scale dining areas.
Predominantly, social interactions take place in common areas, such as dining rooms and lounge areas because these are also the areas where residents spend most of the day (Abbott et al., 2017; Campo & Chaudhury, 2012; Doyle et al., 2012; Moore, 1999; Moore & Verhoef, 1999; Morgan-Brown et al., 2013). This aspect is increased by the presence of household-like environments, in which residents spend their time preferably in communal spaces and not in their own room (Morgan-Brown et al., 2013). However, residents are sparsely exposed to stimuli and activities in these areas; consequently, they are engaged in solo activities or passively or not at all for almost half of the time they spend in common areas (Moore, 1999; Moore & Verhoef, 1999). One reason for this may lie in the climate of being a place created for efficient mealtimes, impairing the natural state of the dining room as a place for intimate conversations (Moore, 1999).
Discussion
The current systematic review included 18 studies analysing social interactions of persons with dementia living in special care units differing in the underlying concepts and phenomena studied, as well as in intervention and control groups and measurements. Despite presenting a fragmented database, some conclusions can be drawn. The residents of special care units experience little social interaction, which can engender loneliness characterized by an absence of emotional attachment and an absence of engaging in social networks (Cahill & Diaz-Ponce, 2011; Moyle et al., 2011). The low level of interaction may be to some extent explained by the disease progress (Aasgaard et al., 2017), which affects persons’ conceptual frames to organize experiences and the perception of society. However, researchers on quality of life (O’Rourke et al., 2015) and person-centred care argue that social interaction is a basic human need (Fazio et al., 2018; Harnett, 2014; Kitwood & Bredin, 1992; O’Rourke et al., 2015). The uncertainties arising from an unfamiliar setting and expectations connected to it reinforce problems with social interactions and the community (Örulv, 2010). This notion is supported by Wood et al. (2005)who found little interactions in organized group activities and more interaction in more familiar one-on-one situations such as during the support in activities of daily living. In general, people adapt their acting and interacting to the setting. Specifically, persons with dementia adjust their behaviour to the ritualized, social order and framework of the institution based on a shared interpretation and definition of the situation (Goffman, 1959; Harnett, 2014).
Major therapeutic goals of settings designed for persons with dementia, as proposed by Calkins (2018), are the creation of a sense of community and meaningful engagement. Considering the low level of social interactions and little opportunities for it, the interpretation of the results questions that the actual everyday life and care in special care units do automatically fulfil these therapeutic goals. However, special care unit residents show more social interaction and better social functioning than non-special care unit residents (De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; Kutner et al., 1999; Morgan-Brown et al., 2013). Although the designs of the studied special care units differed, the results suggest that common features of the special care units have a positive impact on residents’ social interactions. On the one hand, certain architectural characteristics of special care units, especially those of the common places, facilitate social community (Lee et al., 2016). Common places of dementia special care units support the interpretation of the place as a private or semi-private space, in contrast to public spaces, where persons tend to display un-availability for interaction (Goffman, 1963). Furthermore, social interactions occur in small groups (Casey et al., 2016), which are inherent in many special care units, such as small-scale homelike units (De Boer, Hamers, Zwakhalen, Tan, Beerens, & Verbeek, 2017a; Verbeek et al., 2010). On the other hand, the staffing features of the special care units have a crucial influence on residents’ social life. Staff members are mainly responsible for initiating interactions and creating opportunities for resident-to-resident interactions. Resident’s interpretation of the social framework of staff members being in charge of the common room and of themselves being expected to sit calmly and minding their own business reinforces this notion (Andersen et al., 2019). Subsequently, residents’ social interactions depend mostly on staff members. The built environment represents the frame for these interactions and has little impact by themselves when not complemented with adequate personnel policy. In line with this finding, Garcia et al. (2012)stated that human environments are perceived as more important than the physical environment; subsequently, the behaviour, competencies and attitude of the staff members seem to have the highest influence on residents’ social interactions.
Because social interactions facilitate the domains of quality of life such as participation in activities and engagement, they are significantly related to positive effects, higher interest and pleasure (Cahill & Diaz-Ponce, 2011; Jao et al., 2018). Additionally, residents with larger social networks tend to have a higher quality of life, whereas mainly isolated residents show a poor quality of life (Aasgaard et al., 2017). It can be deduced that social interactions are major contributors to the overall quality of life in persons with dementia (Martyr et al., 2018). However, the results of one study (Van der Zon et al., 2018) indicating less social isolation but also negative developments in social relations raise the questions regarding how the subscales of the QUALIDEM (Ettema et al., 2007) depicting social interactions and relationships are connected and how they contribute to the overall quality of life.
A considerable proportion of the included studies lacked detailed information about the intervention components of the special care unit (Abrahamson et al., 2012; De Rooij et al., 2012; Kok et al., 2018; Van der Zon et al., 2018; Weyerer et al., 2010; Wolf-Ostermann et al., 2012). Interesting aspects, for example, would be architectural and staffing features and implemented care concepts, as they have a considerable impact on residents’ feeling of connectedness and well-being (Power, 2014). This is a problem that seems to be widely spread in the development but also the evaluation of special care units (Palm & Bartholomeyczik, 2018). Furthermore, except for a some studies (Aasgaard et al., 2017; Abbott & Pachucki, 2017; Abbott et al., 2017; Campo & Chaudhury, 2012; Doyle et al., 2012; Moore & Verhoef, 1999; Morgan-Brown et al., 2013; Weyerer et al., 2010), the analysed concepts are not clearly defined. Thus, it is unclear what behaviours and actions are examined, even though this would be of special interest, as non-verbal forms of interactions, such as micro movements or exchange of glances, are often neglected to be included in the analysis of social interactions.
The rationale for the chosen concepts and outcomes, giving information on why and how the outcomes are affected by the special care units, is not reported in most studies and limits the understanding of the positive and negative effects of the special care units. The outlined uncertainty of the intervention–outcome relation emphasizes the importance of a sound theoretical background and its reporting in publications by, for example, stating the programme theory or logic model of the intervention that addresses the question regarding what intervention components affect what outcomes in what way (Adlbrecht et al., 2018; Ausserhofer et al., 2016; Funnel & Rodgers, 2011).
Strengths and limitations
This study is the first mixed-methods systematic review that synthesises the existing literature of social interactions of persons with dementia living in special care units. A major strength of this review is that it is not merely based on a summary of the aggregated data of single studies but takes another step by synthesizing the results of the primary studies. By doing so, the synthesis shows a deeper understanding of the social interactions of persons with dementia living in special care units. Additionally, it incorporates the findings of quantitative and qualitative studies, allowing a more comprehensive picture of social interactions. The review was constructed following the reporting guideline Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Liberati et al., 2009).
The review focuses on one of the major therapeutic goals of dementia special care units – social interactions – therefore, this paper does not provide a comprehensive overview of social interactions of persons with dementia in general. The search was performed in five major databases in the fields of healthcare and social sciences, omitting articles not written in English or German, listed in other databases, not listed in databases or grey literature. Hence, some valuable information might have been missed. The included studies investigated the social interactions of special care unit residents from different viewpoints, applying various concepts as well as methodologies, studied heterogeneous special care units and control groups and analysed relatively small sample sizes from dissimilar populations. The insufficient description of the special care units and analysed concepts limits the interpretation of results in the synthesis. Their comparability remains questionable because it is not clear whether they originated from comparable or completely different environmental conditions. Besides, the samples of the studies differ in cognitive and functional status – aspects that may considerably influence residents’ social interactions (Power, 2014). As participants’ characteristics are assessed with varying instruments and measurements, the samples’ comparability remains limited.
Conclusion
The current review yielded fragmented evidence based on special care unit residents’ social interactions, highlighting the need for more profound research to make comprehensive recommendations for healthcare providers. Furthermore, persons with dementia living in special care units experience little, but more, social interaction than those not living in special care units. Social interaction mainly occurs in small clusters and is influenced by the organizational environment, care philosophy and built environment that shapes the opportunities for interactions. Nevertheless, the results are inconclusive regarding the influence of unit size and homelike characteristics on social interactions. More research is needed to better understand the relationships between special care unit’s concepts and the intended and actual outcomes. A special effort must be made to report detailed descriptions of the special care units and their theoretical foundation. Such research contributes to a collective understanding of special care units and their impact.
Supplemental Material
Supplemental material, sj-pdf-1-dem-10.1177_1471301220919937 for Social interactions of persons with dementia living in special care units in long-term care: A mixed-methods systematic review by Laura Adlbrecht, Sabine Bartholomeyczik, Christiane Hildebrandt and Hanna Mayer in Dementia
Supplemental material, sj-pdf-2-dem-10.1177_1471301220919937 for Social interactions of persons with dementia living in special care units in long-term care: A mixed-methods systematic review by Laura Adlbrecht, Sabine Bartholomeyczik, Christiane Hildebrandt and Hanna Mayer in Dementia
Acknowledgements
The authors thank Tamara Nemeth (TN), who assisted with the process of study selection.
Biography
Laura Adlbrechtis research associate at the Center of Dementia Care at the Institute of Applied Nursing Science, FHS St. Gallen University of Applied Sciences and a PhD student at the Faculty of Social Sciences, University of Vienna. Her research areas are gerontological nursing and theory-driven evaluation.
Sabine Bartholomeyczikis professor (em.) at the School of Nursing Science, Witten/Herdecke University. Her research focusses dementia care, nursing diagnostics, concepts of care dependency and the development of nursing science in middle Europe.
Christiane Hildebrandtis a research associate and a PhD student at the Department of Nursing Science, University of Vienna. Her research areas are gerontological and oncological nursing as well as theory-driven evaluation.
Hanna Mayeris a professor and head of the Department of Nursing Science, University of Vienna. Her research focuses on gerontological and oncological nursing and the development of nursing science in middle Europe.
Authors’ note: Laura Adlbrecht is also affiliated with Center for Dementia Care, Institute of Applied Nursing Sciences, Department of Health, FHS St. Gallen, University of Applied Sciences, Switzerland.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Senecura Kliniken- und HeimebetriebsgmbH.
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Laura Adlbrecht, Department of Nursing Science, University of Vienna, Austria.
Sabine Bartholomeyczik, School of Nursing Science, Witten/Herdecke University, Germany.
ORCID iD
Laura Adlbrecht https://orcid.org/0000-0002-7042-7523
References
- Aasgaard H. S. Landmark B. T., Öresland S.(2017). Healthcare personnel’s experiences of enhancing social community for people living in dementia special care units. Nordic Journal of Nursing Research, 37(4), 186–193. [Google Scholar]
- Abbott K. M., Pachucki M. C.(2017). Associations between social network characteristics, cognitive function, and quality of life among residents in a dementia special care unit: A pilot study. Dementia, 16(8), 1004–1019. [DOI] [PubMed] [Google Scholar]
- Abbott K. M. Sefcik J. S., van Haitsma K.(2017). Measuring social integration among residents in a dementia special care unit versus traditional nursing home: A pilot study. Dementia, 16(3), 388–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrahamson K. Clark D. Perkins A., Arling G.(2012). Does cognitive impairment influence quality of life among nursing home residents? The Gerontologist, 52(5), 632–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adlbrecht L. Bartholomeyczik S., Mayer H.(2018). Development of a program theory as a basis for the evaluation of a dementia special care unit. Pflege, 31(3), 125–134. [DOI] [PubMed] [Google Scholar]
- Andersen E. M. Kristiansen E. D., Rasmussen G.(2019). Routines of “sitting” and “enjoying ourselves” in the common room of a dementia unit. Logopedics Phoniatrics Vocology, 44(1), 23–30. [DOI] [PubMed] [Google Scholar]
- Aromataris E., Munn Z.(Eds.) (2017). Joanna Briggs Institute Reviewer’s Manual. https://reviewersmanual.joannabriggs.org/
- Ausserhofer D. Deschodt M. De Geest S. van Achterberg T. Meyer G. Verbeek H., Engberg S.(2016). “There’s No Place Like Home”: A scoping review on the impact of homelike residential care models on resident-, family-, and staff-related outcomes. Journal of the American Medical Directors Association, 17(8), 685–693. [DOI] [PubMed] [Google Scholar]
- Brandenburg H.(2013). Quality of life of people with severe dementia in nursing oases: Empirical results and methodological implications. Zeitschrift Für Gerontologie Und Geriatrie, 46(5), 417–424. [DOI] [PubMed] [Google Scholar]
- Brown Wilson C.(2009). Developing community in care homes through a relationship-centred approach. Health & Social Care in the Community, 17(2), 177–186. [DOI] [PubMed] [Google Scholar]
- Cahill S., Diaz-Ponce A. M.(2011). I hate having nobody here. I’d like to know where they all are’: Can qualitative research detect differences in quality of life among nursing home residents with different levels of cognitive impairment? Aging & Mental Health, 15(5), 562–572. [DOI] [PubMed] [Google Scholar]
- Calkins M. P.(2018). From research to application: Supportive and therapeutic environments for people living with dementia. The Gerontologist, 58, S114–S128. [DOI] [PubMed] [Google Scholar]
- Campo M., Chaudhury H.(2012). Informal social interaction among residents with dementia in special care units: Exploring the role of the physical and social environments. Dementia, 11(3), 401–423. [Google Scholar]
- Casey A. N. Low L. F. Jeon Y. H., Brodaty H.(2016). Residents perceptions of friendship and positive social networks within a nursing home. The Gerontologist, 56(5), 855–867. [DOI] [PubMed] [Google Scholar]
- Chaudhury H. Cooke H. A. Cowie H., Razaghi L.(2017). The influence of the physical environment on residents with dementia in long-term care settings: A review of the empirical literature. The Gerontologist, 58(5), e325–e337. [DOI] [PubMed] [Google Scholar]
- Dai Y., Livesley J.(2018). A mixed-method systematic review of the effectiveness and acceptability of preoperative psychological preparation programmes to reduce paediatric preoperative anxiety in elective surgery. Journal of Advanced Nursing. Advance online publication. 10.1111/jan.13713 [DOI] [PubMed]
- De Boer B. Hamers J. P. H. Zwakhalen S. M. G. Tan F. E. S. Beerens H. C., Verbeek H.(2017. a). Green care farms as innovative nursing homes, promoting activities and social interaction for people with dementia. Journal of the American Medical Directors Association, 18(1), 40–46. [DOI] [PubMed] [Google Scholar]
- De Boer B. Hamers J. P. H. Zwakhalen S. M. G. Tan F. E. S., Verbeek H.(2017. b). Quality of care and quality of life of people with dementia living at green care farms: A cross-sectional study. BMC Geriatrics, 17(1), 155. 10.1186/s12877-017-0550-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Rooij A. Luijkx K. G. Schaafsma J. Declercq A. G. Emmerink P. M. J., Schols J.(2012). Quality of life of residents with dementia in traditional versus small-scale long-term care settings: A quasi-experimental study. International Journal of Nursing Studies, 49(8), 931–940. [DOI] [PubMed] [Google Scholar]
- Doyle P. J. De Medeiros K., Saunders P. A.(2012). Nested social groups within the social environment of a dementia care assisted living setting. Dementia, 11(3), 383–399. [Google Scholar]
- Ettema T. P. Droes R. M. De Lange J. Mellenbergh G. J., Ribbe M. W.(2007). QUALIDEM: Development and evaluation of a dementia specific quality of life instrument. Scalability, reliability and internal structure. International Journal of Geriatric Psychiatry, 22(6), 549–556. [DOI] [PubMed] [Google Scholar]
- Fazio S. Pace D. Flinner J., Kallmyer B.(2018). The fundamentals of person-centered care for individuals with dementia. Gerontologist, 58(S1), S10–S19. [DOI] [PubMed] [Google Scholar]
- Forsund L. H. Grov E. K. Helvik A. S. Juvet L. K. Skovdahl K., Eriksen S.(2018). The experience of lived space in persons with dementia: A systematic meta-synthesis. BMC Geriatrics, 18(1), 33. 10.1186/s12877-018-0728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funnel S. C., Rodgers P. J.(2011). Purposeful program theory. Effective use of theories of change and logic models. Jossey-Bass. [Google Scholar]
- Garcia L. J. Hebert M. Kozak J. Senecal I. Slaughter S. E. Aminzadeh F., Eliasziw M.(2012). Perceptions of family and staff on the role of the environment in long-term care homes for people with dementia. International Psychogeriatrics, 24(5), 753–765. [DOI] [PubMed] [Google Scholar]
- Goffman E.(1959). The presentation of self in everyday life. Anchor Books. [Google Scholar]
- Goffman E.(1963). Behaviour in public places: Notes on the social order of gatherings. The Free Press. [Google Scholar]
- Grant M. J., Booth A.(2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information & Library Journal, 26(2), 91–108. [DOI] [PubMed] [Google Scholar]
- Harnett T.(2014). Framing spaces in places: Creating “respite spaces” in dementia care settings. Dementia, 13(3), 396–411. [DOI] [PubMed] [Google Scholar]
- Harris-Kojetin L. Sengupta M. Park-Lee E. Valverde R. Caffrey C. Rome V., Lendon J.(2016). Long-term care providers and services users in the United States: Data from the National Study of Long-Term Care Providers, 2013–2014. Vital and Health Statistics, 3(38), 1–105; x–xii. [PubMed] [Google Scholar]
- Higgins J. P. T., Green S.(Eds.) (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. http://handbook.cochrane.org/
- Hoffmann F. Kaduszkiewicz H. Glaeske G. Van den Bussche H., Koller D.(2014). Prevalence of dementia in nursing home and community-dwelling older adults in Germany. Aging Clinical and Experimental Research, 26(5), 555–559. [DOI] [PubMed] [Google Scholar]
- Jao Y.-L. Loken E. MacAndrew M. van Haitsma K., Kolanowski A.(2018). Association between social interaction and affect in nursing home residents with dementia. Aging & Mental Health, 22(6), 778–783. [DOI] [PubMed] [Google Scholar]
- Joyce N. R. McGuire T. G. Bartels S. J. Mitchell S. L., Grabowski D. C.(2018). The impact of dementia special care units on quality of care: An instrumental variables analysis. Health Services Research, 53(5), 3657–3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitwood T., Bredin K.(1992). Towards a theory of dementia care: Personhood and well-being. Ageing and Society, 12, 269–287. [DOI] [PubMed] [Google Scholar]
- Kok J. S. Berg I. J., Scherder E. J.(2013). Special care units and traditional care in dementia: Relationship with behavior, cognition, functional status and quality of life – A review. Dementia and Geriatric Cognitive Disorders Extra, 3(1), 360–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok J. S. Nielen M. M., Scherder E. J.(2018). Quality of life in small-scaled homelike nursing homes: An 8-month controlled trial. Health & Quality of Life Outcomes, 16(1), 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutner N. G. Mistretta E. F. Barnhart H. X., Belodoff B. F.(1999). Family members’ perceptions of quality of life change in dementia SCU residents. Journal of Applied Gerontology, 18(4), 423–439. [Google Scholar]
- Lee S. Y. Chaudhury H., Hung L.(2016). Effects of physical environment on health and behaviors of residents with dementia in long-term care facilities: A longitudinal study. Research in Gerontological Nursing, 9(2), 81–91. [DOI] [PubMed] [Google Scholar]
- Liberati A. Altman D. G. Tetzlaff J. Mulrow C. Gotzsche P. C. Ioannidis J. P., Moher D.(2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. The BMJ, 339, b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martyr A. Nelis S. M. Quinn C. Wu Y. T. Lamont R. A. Henderson C., Clare L.(2018). Living well with dementia: A systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychological Medicine, 48(13), 2130–2139. [DOI] [PubMed] [Google Scholar]
- Möhler R., Meyer G.(2014). Attitudes of nurses towards the use of physical restraints in geriatric care: A systematic review of qualitative and quantitative studies. International Journal of Nursing Studies, 51(2), 274–288. [DOI] [PubMed] [Google Scholar]
- Moore K. D.(1999). Dissonance in the dining room: A study of social interaction in a special care unit. Qualitative Health Research, 9(1), 133–155. [DOI] [PubMed] [Google Scholar]
- Moore K. D., Verhoef R.(1999). Special care units as places for social interaction: Evaluating an SCU’s social affordance. American Journal of Alzheimer’s Disease and Other Dementias, 14(4), 217–229. [Google Scholar]
- Morgan-Brown M. Newton R., Ormerod M.(2013). Engaging life in two Irish nursing home units for people with dementia: Quantitative comparisons before and after implementing household environments. Aging & Mental Health, 17(1), 57–65. [DOI] [PubMed] [Google Scholar]
- Moyle W. Kellett U. Ballantyne A., Gracia N.(2011). Dementia and loneliness: An Australian perspective. Journal of Clinical Nursing, 20(9/10), 1445–1453. [DOI] [PubMed] [Google Scholar]
- Nakanishi M. Nakashima T., Sawamura K.(2012). Quality of life of residents with dementia in a group-living situation: An approach to creating small, homelike environments in traditional nursing homes in Japan. Nihon Koshu Eisei Zasshi, 59(1), 3–10. [DOI] [PubMed] [Google Scholar]
- Nikmat A. W. Hawthorne G., Al-Mashoor S. H.(2015). The comparison of quality of life among people with mild dementia in nursing home and home care—A preliminary report. Dementia, 14(1), 114–125. [DOI] [PubMed] [Google Scholar]
- O’Rourke H. M. Duggleby W. Fraser K. D., Jerke L.(2015). Factors that affect quality of life from the perspective of people with dementia: A metasynthesis. Journal of the American Geriatrics Society, 63(1), 24–38. 10.1111/jgs.13178 [DOI] [PubMed] [Google Scholar]
- Örulv L.(2010). Placing the place, and placing oneself within it: (Dis)orientation and (dis)continuity in dementia. Dementia, 9(1), 21–44. [Google Scholar]
- Palm R., Bartholomeyczik S.(2018). Specialist dementia care units. In Michel J. P. Beattie L. Finbarr M., Watson J.(Eds.), Oxford textbook of geriatric medicine, third edition(pp. 281–285). Oxford University Press. [Google Scholar]
- Pearson A. White H. Bath-Hextall F. Salmond S. Apostolo J., Kirkpatrick P.(2015). A mixed-methods approach to systematic reviews. International Journal of Evidence-Based Healthcare, 13(3), 121–131. [DOI] [PubMed] [Google Scholar]
- Popay J. Roberts H. Sowden A. Petticrew M. Arai L. Rodgers M., Duffy S.(2006). Guidance on the conduct of narrative synthesis in systematic reviews: A product from the ESRC Methods Programme. http://lancs.ac.uk/shm/research/nssr/research/dissemination/publications.php/ 10.13140/2.1.1018.4643 [DOI]
- Power G. A.(2014). Dementia beyond disease. Enhancing well-being. Revised edition. Health Professions Press. [Google Scholar]
- Sandelowski M. Voils C. I., Barroso J.(2006). Defining and designing mixed research synthesis studies. Research in the Schools, 13(1), 29. [PMC free article] [PubMed] [Google Scholar]
- Smith K. P., Christakis N. A.(2008). Social networks and health. Annual Review of Sociology, 34(1), 405–429. [Google Scholar]
- Thomas J., Harden A.(2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8, 45. 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Zon A. Wetzels R. B. Bor H. Zuidema S. U. Koopmans R., Gerritsen D. L.(2018). Two-year course of quality of life in nursing home residents with dementia. American Journal of the Geriatric Psychiatry, 26(7), 754–764. [DOI] [PubMed] [Google Scholar]
- Verbeek H. Zwakhalen S. M. van Rossum E. Ambergen T. Kempen G. I., Hamers J. P.(2010). Dementia care redesigned: Effects of small-scale living facilities on residents, their family caregivers, and staff. Journal of the American Medical Directors Association, 11(9), 662–670. [DOI] [PubMed] [Google Scholar]
- Weyerer S. Schaufele M., Hendlmeier I.(2010). Evaluation of special and traditional dementia care in nursing homes: Results from a cross-sectional study in Germany. International Journal of Geriatric Psychiatry, 25(11), 1159–1167. [DOI] [PubMed] [Google Scholar]
- Wolf-Ostermann K. Worch A. Fischer T. Wulff I., Graske J.(2012). Health outcomes and quality of life of residents of shared-housing arrangements compared to residents of special care units-Results of the Berlin DeWeGE-study. Journal of Clinical Nursing, 21(21–22), 3047–3060. [DOI] [PubMed] [Google Scholar]
- Wood W. Harris S. Snider M., Patchel S. A.(2005). Activity situations on an Alzheimer’s disease special care unit and resident environmental interactions, time use, and affect. American Journal of Alzheimer’s Disease and Other Dementias, 20(2), 105–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-dem-10.1177_1471301220919937 for Social interactions of persons with dementia living in special care units in long-term care: A mixed-methods systematic review by Laura Adlbrecht, Sabine Bartholomeyczik, Christiane Hildebrandt and Hanna Mayer in Dementia
Supplemental material, sj-pdf-2-dem-10.1177_1471301220919937 for Social interactions of persons with dementia living in special care units in long-term care: A mixed-methods systematic review by Laura Adlbrecht, Sabine Bartholomeyczik, Christiane Hildebrandt and Hanna Mayer in Dementia