Abstract
Objectives
Technology-based prompting has the potential to support people with dementia to complete multistep tasks in the home. However, these devices can be complex to use. This paper reports a feasibility trial of a personalised touchscreen digital prompter designed for home use.
Methodology: A tablet-based prompter suitable for people living with dementia was developed, along with a detailed guidance manual. Carers loaded instructions for completing the task onto the prompter, and the person with dementia then used the tablet independently to complete a task. Eleven couples used the prompter ‘out-of-the-box’ with no support other than a guidance manual.
Results
The majority of participants with dementia could follow the steps on the prompter, and carers were able to breakdown and load tasks onto the prompter. Eight couples used the prompter successfully to complete goals that they had identified in advance. These included preparing simple snacks and using a TV remote control. Successfully achieving goals was associated with more frequent use of the prompting screen on more days, but not higher levels of editing or previewing of tasks.
Conclusion
The study provides the preliminary evidence that family caregivers can use a touchscreen tablet, software and manual package to identify specific tasks and break these down into steps and that people living with dementia can then follow the prompts to complete the tasks. This potentially represents an important advance in dementia care. Further testing is required to establish efficacy and to identify any factors that impact on outcomes.
Keywords: Alzheimer’s disease, dementia, audiovisual aids, reminder systems, activities of daily living, technology
Introduction
Over the course of their illness, people with dementia find performing simple tasks such as food preparation and household chores increasingly challenging (Marshall et al., 2012). Supporting people who are living with dementia to perform these activities of daily living (or ADLs) can enhance their self-esteem and well-being (Orpwood et al., 2007). In addition, increasing a person’s activity levels may also help to improve their autonomy and quality of life (Graff, 2009; Graff et al., 2007). Consequently, many health care workers view supporting clients with dementia and their carers in maintaining multistep ADLs as an important aspect of their work (Andersen et al., 2004). However, developing effective, individualised rehabilitation programmes can be challenging, especially in a period of restricted budgets and increasing demand. It is important, then, to consider whether assistive technology can provide a cost-effective intervention that will enable people with early dementia to complete ADLs. For instance, prospective memory aids (or personal digital assistants) can help with task initiation and completion in the home by providing appropriate cues to guide behaviour.
Developing effective methods of utilising technology to prompt people living with dementia within the community can be challenging. For instance, multistep activities need to be deconstructed into a series of simple tasks or steps. While this technique is commonly used by professionals (Small et al., 2003; Wilson et al., 2013) and has been incorporated into most electronic prompting systems that support multistep activities (Dishman & Carrillo, 2007; Hoey et al., 2012; Lancioni et al., 2010), it can present problems, especially for family caregivers. Similarly, prompts can be provided in different mediums each of which presents opportunities and challenges. Audio prompts have been successfully used to support task performance in individuals with a variety of cognitive difficulties (Adlam et al., 2006; Evans et al., 2007; Lines & Hone, 2006; O’Neill & Gillespie, 2008). Short verbal instructions seem to be preferable as these constrain the number of possible options available, reducing the demand on the person’s cognitive abilities. However, audio prompts are transient and therefore if used in isolation may be of limited support for individuals who have difficulties with short-term memory and verbal retention. A recent systematic review concluded that text and audio-based prompting technology are effective interventions and highlighted the need for more technology for people with memory impairments (Jamieson et al., 2014).
Visual prompts are also a widely accepted means of conveying information. Pictorial instructions can be effective for people with learning disabilities or brain injury whilst learning or undertaking multistep tasks (Cihak et al., 2006; Mechling & Gustafson, 2009). Lancioni et al. (2012) used technology-aided pictorial cues to support people with moderate Alzheimer’s disease in carrying out ADLs and found that pictorial prompts were as effective as verbal audio prompts, or combinations of both. However, Orpwood et al. (2010) found that picture and video prompts tended to encourage copying rather than a genuine understanding of the nature of the task. In addition, video systems cannot easily be used to capture ADL performance in a person’s home and tend to require more time and expertise to use than simpler formats. A comparison of four types of prompts (text, audio, picture and video) to help people with early-stage dementia complete a three-step task indicated that audio and text prompts were generally the most effective method of prompting successful performance, although a combination of pictures with verbal prompting was more successful for some participants (Boyd et al., 2017).
Taken together, then, for any prompting device to be used successfully, four conditions need to be satisfied: firstly, the person with dementia and their carer need to be able to identify a meaningful and suitable task; secondly, this task must then be deconstructed into a sequence of suitable short steps or prompts that the person with dementia can follow; thirdly, the carer then needs to load this prompt sequence onto the tablet; before finally, the prompting device needs to be correctly positioned and appropriately activated to enable the person with dementia to follow the prompts independently and to complete the task without needing any further support.
The aim of this programme of work (of which this paper is one part) was to develop just such a prompting device that could be used independently by a person with dementia and their carer in a home environment with little or no training. Our initial work developed a prototype package (a touchscreen tablet computer with a user-friendly interface, bespoke software and an accompanying manual) that could potentially support carers and the person living with dementia across all four steps. An initial evaluation with 12 dyads made up of person who was living with dementia and a carer indicated that this was an acceptable and potentially effective means of delivering audio, text and visual prompts (Boyd et al., 2017). However, during this initial testing of this prompter, carers were first trained in using the prompter and were then provided with regular support by the project team. In order to test whether the prompter can be used independently in more naturalistic settings, we therefore needed to repeat this evaluation, but without providing carers with either training or support. This study reports the results of a preliminary evaluation of the prompter package (i.e. tablet and manual) being used ‘out of the box’ by carers and people living with dementia who had no previous experience of the package and who received no support from the project team. The objectives of this evaluation were to provide preliminary evidence relating to four key questions:
Were participants (both those living with dementia and their carers) able to use the prompter successfully?
Were couples able to achieve the goals they set?
Were any background factors associated with use of the prompter?
Was use of the prompter associated with outcome?
Methodology
National Health Service (NHS) Health Research Authority and Ethics approval was received.1 All participants living with dementia were independently assessed as having capacity to consent to study participation and provided written consent to the inclusion of their data in dissemination of the results.
Participants
Pairs of participants (individuals with dementia and their primary carers) were recruited from an NHS Memory Clinic using the following criteria. Potential participants with dementia were eligible for entry into the study if they had:
A confirmed clinical diagnosis of Alzheimer’s disease, vascular dementia, or mixed Alzheimer’s disease with vascular dementia;
Mild to moderate cognitive impairment due to dementia as judged by an Addenbrooke’s Cognitive Examination (ACE)-III (Hsieh et al., 2013) score of 50 or over;
Reduced ability to perform ADLs, as indicated, for instance, by a score of 5 or more on the Bristol Activities of Daily Living Scale or BADLS (Bucks et al., 1996);
Capacity to give informed consent; and
A primary carer who is willing and able to take part in the study and who has contact with the individual with dementia on at least three separate occasions per week.
People living with dementia were not eligible to take part in the study if they had:
A severe sensory disability, including profound loss of hearing or vision that would prevent them from engaging with the prompting technology;
A significant impairment of mobility or dexterity such that the prompting technology could not be safely or meaningfully used;
Experienced a large cerebrovascular lesion in the last nine months; or
Were living in residential care.
Procedure
Participant pairs were provided with the prompting toolkit (touchscreen tablet with software loaded and a manual) as an ‘out-of-the-box’ experience that is without setting up the package or showing participants how to use it. They were asked to use the toolkit over a period of four weeks and to choose an activity, break this down into a series of steps, load these steps onto the tablet and then use the toolkit to carry out the activity. Carers were able to choose how to present each step, using verbal, text (see Figure 1) or photographs (see Figure 2). Guidance around choosing which modality to use and how to create each step was provided in the manual.
Figure 1.
Example of a text step using text and audio prompts.
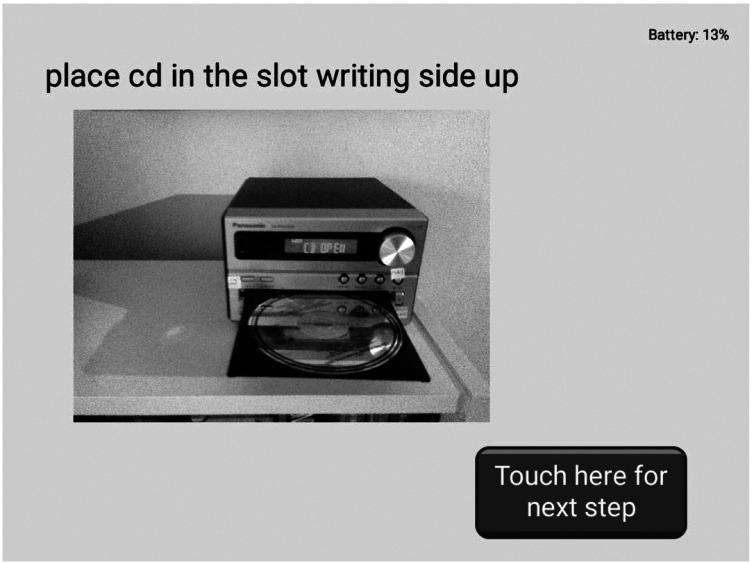
Figure 2.
Example of a task step using text, audio and image prompts.
During the goal setting discussions with NE, some participating dyads were quickly able to identify the specific activity (e.g. ‘prepare a simple snack’ and ‘switch on music/TV’) that they would use the prompter for. Other dyads identified the tasks they would work on after the goal setting discussion and instead chose more general benefits as research goals such as being ‘more engaged in activity’ or not needing ‘to give step by step guidance’. The manual provided guidance on how to choose a task and break it down into steps as well as practical instructions on how to use the tablet. Carers and people living with dementia were able to choose from three alternative prompting mediums in the form of text, pictures or audio recordings (as an audio prompt carers could record their own voice or use an automated electronic voice). Participating dyads received weekly research phone calls (these did not discuss practical issues around the use of the toolkit) and were offered a help line number that they could use if they had questions or got into difficulty using the prompter and needed support to work out how to resolve problems in using it.
Measures
Data across several domains were collected:
Cognitive functioning. Participants living with dementia completed three cognitive assessments: (i) the ACE-III, a brief cognitive screening assessment; (ii) the California Verbal Learning Task (CVLT-II), a test of verbal learning and memory (Delis et al., 2000); and (iii) the Trail Making Component of the Delis Kaplan Executive Functions System Test Battery (D-KEFS-TM), a brief test of visual scanning, attentional abilities, motor speed and cognitive flexibility (Delis et al., 2001). Carers also completed the BADLS, which assesses the ability of a person with dementia to perform daily tasks.
Care knowledge and attitudes. Primary caregiver participants completed: the Alzheimer’s Disease Knowledge Scale (ADKS) to assess their knowledge about Alzheimer’s disease (Carpenter et al., 2009); and the Sense of Competence Questionnaire (SCQ), which measures a caregiver’s satisfaction and worry in their role as a carer (Vernooij‐Dassen et al., 1999).
Log of prompter use. The software used in the prompter automatically recorded every occasion in which the component steps of the task were edited or a task was run.
The Goal Attainment Scale (GAS). The GAS is a widely used instrument for measuring change within rehabilitation research (Kiresuk & Sherman, 1968; Rockwood et al., 1993; Stolee et al., 1992). A modified version of the GAS was used, which omitted any requirement to weight the relative importance of different goals, that could be completed by people with moderate levels of dementia (Evans et al., 2015). At the initial (pre-intervention) assessment, the occupational therapy researcher (NE) agreed three priority goals with participants (two that were important for the person with dementia and one that the carer wanted to achieve) as well as the outcome criteria that would be used to evaluate success or failure for each goal. These were reviewed at the final (post intervention) interview and three possible levels of success identified by the OT researcher together with both participants in each dyad: the goal being completely achieved (a score of 2); partially achieved (1) or not achieved, and no change (0).
Ratings of success. At the end of the four-week trial, carers were asked to make two ratings of their level of success: firstly, whether or not they were able to access and use the prompt screen to load the steps; and secondly, whether the person with dementia had been able to complete at least one step on their own
Results
A total of 14 dyads were recruited to the study. Three pairs (E, G and M) subsequently withdrew after giving consent but before starting the study (one due to personal circumstances, another had concerns about compliance and the third pair decided on reflection that they would not be able to use the prompter). All couples were white British with an average age of 81 (SD = 5.87) and a mean ACE III score of 67.86 (SD = 9.98). Table 1 outlines the demographic details of participating couples and caregiver participants’ scores on the Alzheimer’s Disease Knowledge Scale and Sense of Competence scale, while Table 2 provides levels of the cognitive functioning of participants living with dementia.
Table 1.
Demographic and other background details of participants (n = 14).
|
Person living with dementia details |
Carer details |
Goal attainment total scorec | ||||||
|---|---|---|---|---|---|---|---|---|
| ID | Age | Sex | Diagnosis | More than 12 years of education | Alzheimer’s disease knowledge scorea | Relationship | Sense of competenceb | |
| A | 79 | Male | DAT | No | 27 | Wife | 16 | 2 |
| B | 88 | Male | VD | Yes | 26 | Daughter | 15 | 6 |
| C | 80 | Male | VD | Not known | 27 | Wife | 16 | 4 |
| D | 86 | Female | DAT | Yes | 21 | Husband | 25 | 6 |
| E | 75 | Male | Mixed | Yes | 22 | Wife | 11 | Withdrew |
| F | 79 | Female | DAT | Yes | 29 | Daughter | 20 | 2 |
| G | 76 | Male | Mixed | Not known | 24 | Wife | 10 | Withdrew |
| H | 81 | Female | DAT | Yes | 28 | Husband | 20 | 0 |
| I | 78 | Female | DAT | Yes | 20 | Husband | 26 | 6 |
| J | 78 | Male | Mixed | No | 17 | Wife | 26 | 6 |
| K | 87 | Female | VD | Yes | 24 | Sister | 13 | 4 |
| L | 94 | Female | Mixed | Yes | 25 | Daughter | 15 | 6 |
| M | 72 | Female | DAT | No | 22 | Husband | 15 | Withdrew |
| N | 81 | Female | DAT | Yes | 28 | Husband | 18 | 5 |
| Average | 81.00 | 24.29 | 17.57 | |||||
DAT: dementia of the Alzheimer’s type; VD: vascular dementia; mixed: mixed Alzheimer’s and vascular dementia.
aMaximum score is 30 (higher scores represent greater knowledge).
bMaximum score is 27 (a higher score represents a greater sense of competence).
cMaximum score is 6 (higher scores represent greater completion of more goals).
Table 2.
Cognitive functioning scores for participants living with dementia (n = 14).
| Participant ID | ACE-III (total score)a | CVLT learning phaseb | CVLT-II short-delay free recallb | CVLT-II long-delay free recallb | D-KEFS visual scanningb | D-KEFS letter sequencingb | D-KEFS number–letter switchingb | D-KEFS motor speedb | Activities of daily living (BADLS)c |
|---|---|---|---|---|---|---|---|---|---|
| A | 83 | 3.0 | 0.1 | 7.0 | 50.0 | 9.0 | 9.0 | 63.0 | 11 |
| B | 56 | 1.0 | 1.0 | 1.0 | 9.0 | 0.1 | 1.0 | 0.4 | 21 |
| C | 64 | 5.0 | 2.0 | 7.0 | 25.0 | 63.0 | 1.0 | 63.0 | 10 |
| D | 77 | 0.1 | 1.0 | 0.1 | 84.0 | 91.0 | 1.0 | 50.0 | 8 |
| E | 71 | 0.2 | 0.1 | 1.0 | 0.1 | 50.0 | 0.1 | 37.0 | 15 |
| F | 53 | 0.1 | 2.0 | 1.0 | 16.0 | 16.0 | 0.4 | 9.0 | 17 |
| G | 72 | 0.2 | 0.1 | 1.0 | 50.0 | 37.0 | 37.0 | 84.0 | 13 |
| H | 78 | 5.0 | 1.0 | 0.1 | 25.0 | 25.0 | 50.0 | 75.0 | 8 |
| I | 64 | 3.0 | 2.0 | 1.0 | 25.0 | 37.0 | 9.0 | 2.0 | 1 |
| J | 70 | 0.1 | 0.1 | 7.0 | 16.0 | 0.1 | 0.4 | 16.0 | 6 |
| K | 76 | 5.0 | 1.0 | 0.1 | 25.0 | 1.0 | 1.0 | 9.0 | 22 |
| L | 62 | 1.0 | 2.0 | 1.0 | 0.1 | 0.1 | 1.0 | 0.1 | 17 |
| M | 50 | 1.0 | 1.0 | 1.0 | 75.0 | 5.0 | 0.4 | 0.1 | 18 |
| N | 74 | 1.0 | 1.0 | 0.1 | 37.0 | 16.0 | 1.0 | 0.1 | 11 |
| Average | 67.86 | 1.89 | 1.16 | 2.03 | 31.23 | 25.02 | 8.04 | 29.19 | 12.71 |
ACE-III: Addenbrooke’s Cognitive Examination; CVLT: California Verbal Learning Task; D-KEFS: Delis Kaplan Executive Functions System Test Battery; BADLS: Bristol Activities of Daily Living Scale.
aMaximum score is 100 (higher scores represent better cognitive functioning).
bAge-matched percentile scores.
cMaximum score is 60 (higher scores indicate greater impairment in performing ADLs).
Participants’ familiarity with technology
Elsewhere we have set out how participants’ prior use of technology and their confidence in doing so impacted on their experience of using the prompter (reference removed to preserve anonymity). While some participating dyads had little experience with digital technology, others regularly used mobile phones and laptops and were familiar with apps, including Twitter and Facebook. Nevertheless, almost all of the participants (both people living with dementia and their carers) expressed concerns about using the prompter not just before doing so, but also after the trial, even if they had completed the tasks successfully.
Tasks for which the prompter was used
Participating dyads used the prompter to complete a range of different tasks, the most common of which were using household appliances (e.g. a TV remote control or a camera); as a prompt to remember keys or a mobile phone before leaving the house; and in the kitchen, for instance, laying the table or making a sandwich.
Goals set by participant dyads
Typically, participants with dementia set goals of using the prompter to complete a household task successfully (6), but goals were also related to becoming more confident in performing these tasks (6). Details of the goals that dyads set are provided in Table 3. Given how little confidence participants living with dementia now had in using even basic appliances in the home, many of the goals concerned wanting to be reassured about either using the prompter itself successfully (6) or finding it worthwhile to use (4). Similarly, the goals that carers set related both to what difference using the prompter might make in their lives and their own concerns about their ability to use it. Thus, four carers wanted the person with dementia to ask fewer questions, and to need less guidance, while two hoped that the person with dementia would become more independent. For three carers, their goal was to be able to identify tasks to use on the prompter, while two set a goal of breaking this down and installing it on the prompter successfully.
Table 3.
Participants dyad goals and total GAS (n = 11).a
| Participant ID | Participant with dementia goal 1 | Participant with dementia goal 2 | Carer participant goal (in their own words) | GAS score |
|---|---|---|---|---|
| A | To be more engaged in activity | Increased confidence in using technology | To have tasks and activities done | 2 |
| B | To prepare a simple snack | Use a familiar piece of home electronic technology | Not to need to give step by step guidance | 6 |
| C | To take photographs | To use the technology | To complete a task without additional prompts | 4 |
| D | To help carer to do things around the house | To use the technology | Being able to load a task successfully | 6 |
| F | To switch on music/TV | To see a purpose in using the tablet | Able to programme the tablet | 2 |
| H | To complete a task | To use the technology | Asks less questions when doing task | 0 |
| I | To complete a task | To find the step by step helpful | Identified some tasks | 6 |
| J | To complete a task | To increase confidence in doing tasks | Able to complete a task on their own | 6 |
| K | To complete a task | To be confident about using technology | Identified some tasks | 4 |
| L | To put on music | To be more independent and asking for less help | To use the tablet on their own | 6 |
| N | To use kitchen appliances | Able to use the instructions to complete a task | To identify and set up a task | 5 |
GAS: goal attainment scale.
aAll goals use the participants’ own words.
Could participants use the prompter successfully?
At the end of the four-week trial of the prompter, participants were asked to rate their success in using it. All 11 dyads reported that they had been able to break down at least one activity into steps and then load these onto the prompter. In addition, 8 of the 11 dyads reported that the person living with dementia had been able to read the instructions on the prompter and to follow these to complete at least one step in a task successfully. Finally, 10 of the 11 carers said that they felt confident in accessing the carer set up screen, with the other carer able to do so with the help of a member of their family.
Were couples able to use the prompter to achieve the goals they set?
Only one of the 11 dyads that completed the study did not rate themselves as having either fully or partially met at least one of the goals that they had set. Successful completion of a goal was scored as 2 points, partial completion as 1 and not completing as 0. Combining points for each of the three goals resulted in a scale from 0 to 6 (see Table 3). Of the 22 goals set by participants living with dementia, 14 were fully met, 1 partially met and 7 not met. The majority of goals that were met (8) related to becoming more independent. For carers, eight goals were fully met and two partially met with one carer reporting that the prompter did not meet their goal.
Were any background factors associated with use of the prompter?
We operationally defined successful use of the prompter by combining the goals set by both participants living with dementia and carers using a GAS score of 4 or above as a cut off. Thus, participating dyads that scored at least 4 had either wholly or at least partially completed two of the three goals that were set. Using this cut off, we assessed eight dyads as having successfully used the prompter, with six dyads not doing so (either because they fell below the threshold or because they withdrew from the study before attempting to do so).
We used independent samples t-tests to compare cognitive functioning scores and carer knowledge about dementia and strain for the eight dyads who scored at least 4 out of 6 on the GAS, and the six dyads who either fell below this cut-off or who withdrew from the study (see Tables 2 and 3). There were no significant differences in cognitive functioning, BADLS scores, Alzheimer’s disease knowledge or caregiver competence between the groups. However, participants living with dementia who had more success with the prompter were significantly older (M = 84.00, SD = 5.68) than were those who had less success (M = 77.00, SD = 3.29) (t(12) = 2.69, p = 0.02). Using a chi-squared test, the two groups did not differ significantly in terms of their gender, relationship to care or diagnosis.
Was use of the prompter associated with outcome?
The data collected from the tablet enabled us to establish whether there were differences in how successful and unsuccessful dyads used the tablet (see Table 4). Again, we analysed the data using independent samples t-tests, this time comparing the eight dyads who were successful with the three dyads who used the prompter unsuccessfully. There were no differences between successful and unsuccessful dyads in the frequency with which they edited or previewed tasks (measured by either the number of days or occasions in which they accessed the edit or carer screens). However, the two groups did differ significantly in how often they ran a task: dyads who were successful ran the task more often (t(9) = −2.31, p = 0.046) and on more days (t(9) = −2.29, p = 0.048) than did dyads who did not meet their goals.
Table 4.
Use of prompter by carers and participants living with dementia for successful (GAS ≥ 4) and unsuccessful (GAS < 4) dyads.
| GAS ≥ 4Mean (SD), n = 8 | GAS < 4Mean (SD), n = 3 | |
|---|---|---|
| Running the task | ||
| • Number of days | 10.88 (3.40) | 5.67 (3.21) |
| • Number of occasions | 49.25 (36.11) | 16.00 (11.53) |
| Accessing carer screens (to potentially add, edit, preview or delete a task) | ||
| • Number of days | 5.63 (2.50) | 5.67 (3.21) |
| • Number of occasions | 39.88 (31.07) | 25.67 (11.02) |
| Accessing the edit screens (to potentially edit or preview a task) | ||
| • Number of days | 3.75 (1.58) | 3.00 (1.00) |
| • Number of occasions | 42.50 (45.54) | 42.67 (32.19) |
GAS: goal attainment scale; SD: standard deviation.
Discussion
People living with dementia experience increasing difficulties in completing everyday tasks. This increases their dependency, causes frustration and undermines their self-confidence. While the development of ‘simple to use’ touchscreen tablets has the potential to support people living with dementia to complete everyday tasks, this still requires tasks to be broken down into a series of steps and then loaded onto the tablet so that they then provide a combination of verbal and visual prompts that the person living with dementia can use. This project explored whether it was possible for carers and people living with dementia to work together to use a touchscreen tablet, and its associated software to complete everyday tasks that they saw as important.
In a previous study, we have shown that with training and support, people living with dementia and their carers could use the prompter to help them to complete multistep activities of daily living (Boyd et al., 2017). In this study, we wanted to see whether a different group of participating dyads could have success in using the prompter package ‘out-of-the-box’ – that is to say without any training or support. Our initial results suggest that the majority of the couples in this small trial were indeed able to use the prompter in this way: all 11 carers were able to deconstruct a task that their partner experienced difficulties with, breaking it down into a series of steps and then loading this onto the prompter. Eight of the 11 carers also felt that their partner who was living with dementia was able to use the prompter independently, and all eight of these participants were able to achieve all of their goals, either fully or partially. As the reasons for success or failure are often likely to be complex and relate not to both cognitive functioning and also to participants’ expectations and prior experiences with technology, we will explore this area further in a separate paper (Evans et al., 2020).
At the same time, some participating dyads struggled to use the prompter successfully: three dyads withdrew from the study without using it, while another dyad used the prompter but were not able to meet any of their goals. Two other dyads achieved only partial success. Importantly, while there was no difference in the way that successful and unsuccessful dyads used the prompter to set up tasks, problems for these three couples seemed to emerge when the person living with dementia came to use the prompter. Where the prompter was unsuccessful, couples used the prompter less often and on fewer days.
In this study, carers rather than people living with dementia typically initiated use of the prompter. Follow on work is needed to explore adaptations to the prompter to support task initiation that will enable it to be used more independently by the person living with dementia. We will report elsewhere on whether there is a relationship between the type of goals that were set and outcomes.
Study limitations
A secondary aim of the study was to identify any obvious background factors associated with cognitive functioning or knowledge about dementia that might contribute to successful (or unsuccessful) use of the prompter. Encouragingly, while increased age was associated with outcome, none of the measures of cognitive functioning were. This suggests that within the parameters of this study at least, successful use of the prompter does not rely on cognitive ability. However, clearly more work is required to identify both whether cognitive or social factors impact on use of the prompter and also whether successful use of the prompter translates into greater functional independence and increased life satisfaction. In addition, we excluded prospective participants who were living with dementia but who while they might have been able to use the prompter, either lacked the dexterity (e.g. from arthritis) or had sensory disabilities that might have prevented them from doing so. This, taken together with the exclusion of people with forms of dementia other than Alzheimer’s disease, vascular dementia or mixed forms of these, would act to restrict the wider applicability of our findings.
Moreover, given the progressive nature of dementia, it is likely that where someone living with dementia initially succeeds in using the prompter to engage with a task, they may later either be unable to do so or need to use the prompter in a different way. While we are encouraged by the fact that people of differing cognitive abilities were able to make use of the prompter, further work will be needed to understand how deterioration impacts upon its use.
Conclusion
This study provides preliminary evidence that people living with dementia and their carers can successfully use a touchscreen tablet and prompting software to complete tasks without additional support. This potentially represents an important advance in dementia care. The majority of carers in this study were able to select tasks and to set up multistep prompts, while the majority of participants living with dementia were able to use the prompter to follow the steps and complete the task. At the same time, some dyads experienced problems and either did not start to use the prompter or did so but without finding it helpful. While the results of this small study are promising, a larger trial of the prompter is required before we can conclude either that the prompter will be of help to people living with dementia and their carers, or whether cognitive or other background factors are associated with its successful use.
Acknowledgement
The authors would like to thank everyone who participated in their studies. We would also like to acknowledge the support of The Dunhill Medical Trust, the Dowager Eleanor Peel Trust, the Pixel Fund, the Edith Lilian Harrison 2000 Foundation and the McLay Dementia Trust.
Biography
Nigel Harris is the director of Innovation and Growth with the West of England Academic Health Network and visiting professor in the Department of Health at the University of Bath. He was previously a chief executive of Designability, a design and development charity working to develop assistive and enabling technologies. Nigel is a clinical scientist and has over 30 years’ experience of clinical research, specialising in physiological measurement and rehabilitation. Recent research projects include the use of digital technologies to support individuals with cognitive impairments and use of robotics and autonomous systems in the home.
Hazel Boyd is a user interface engineer at Designability, a design and development charity specialising in the design of assistive technology for people with a range of physical and cognitive conditions. After graduating from the University of Bath with a degree in Mechanical Engineering, she completed a PhD in the measurement of functional wrist motion in the University’s Centre for Orthopaedic Biomechanics working alongside academics and clinicians. Hazel’s work now focuses primarily on user-led design of assistive technology, including user engagement with a wide range of stakeholders to inform design decisions. She has contributed to the design of several consumer products for people with dementia, including a day clock and a simple music player.
Nina Evans is currently an occupational therapist/researcher in the charity Designability. She has worked extensively as a clinical therapist in the 80s and 90s but since 2001 has been involved in a broad range of research and product development activities for people living with dementia. Her work includes a contribution to early smart house technology, the Memory Technology Library and the Day Clock.
Richard Cheston spent 25 years working as a clinical psychologist in the NHS and is now a professor of dementia research at the University of the West of England. In both roles, he has been involved in developing and evaluating psychological interventions for people affected by dementia.
Krist Noonan is currently the research operations manager for Avon & Wiltshire Mental Health Partnership NHS Trust, where he oversees their dementia research programme, including studies which investigate new potential drug treatments for dementia and related disorders at the Kingshill Research Centre. He has previously worked as an academic neuropsychologist/research fellow at the Research Institute for the Care of Older People (RICE) centre, where he was involved in a number of grants which explored cognitive and language rehabilitation approaches for dementia, as well as additional work investigating the validity of cognitive screening tools for detecting dementia in the community at the earliest stage of presentation.
Thomas Ingram is presently a PhD candidate in the Department for Health, University of Bath, and a researcher at the Royal National Hospital for Rheumatic Diseases, Bath. He has formerly worked in the fields of dementia, neurodegenerative diseases and ageing, with five years’ experience at the Research Institute for the Care of Older People (RICE) and the National Institute for Health Research: Clinical Research Network.
Aron Jarvis is a research psychologist with five years’ experience working with people with a diagnosis of dementia. He currently works in a clinical and research capacity at the Research Institute for the Care of Older People (RICE) memory clinic in Bath, UK.
Jessica Ridgers is a passionate human-centred designer who works with people to understand real user needs. Jess is an industrial designer and researcher at Designability, where her work focuses on user engagement and design for disability. Jess was responsible for designing the interface aesthetic and user–interface interactions for the prompting device.
Note
The study received ethics permission on 16 April 2016, from the South-West Central Bristol Research ethics committee (ref: 16/SW/0038). Amendment number 01/11/2017 was approved on the 8 January 2018. IRAS project reference 188515.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by The Dunhill Medical Trust [grant number R399/0215], the Dowager Eleanor Peel Trust, the Pixel Fund, the Edith Lilian Harrison 2000 Foundation and the McLay Dementia Trust. The authors would like to acknowledge the support of the National Institute for Health Research Clinical Research Network (NIHR CRN), the National Institute for Health Research Masters programme and Designability Charitable funding.
Contributor Information
Nigel Harris, Department for Health, University of Bath, Bath, UK.
Nina Evans, Designability, Wolfson Centre, Royal United Hospital, Bath, UK.
Richard Cheston, Health and Social Sciences, University of the West of England, Bristol, UK.
Krist Noonan, School of Social and Community Medicine, University of Bristol, Bristol, UK.
Thomas Ingram, Department for Health, University of Bath, Bath, UK.
Aron Jarvis, Research Institute for the Care of Older People, The RICE Centre, Royal United Hospital, Bath, UK.
ORCID iD
Richard Cheston https://orcid.org/0000-0002-7466-3777
References
- Adlam T. D., Evans N. M., Gibbs C., Orpwood R. D. (2006). User evaluation of smart flats for people with dementia. In 2006 pervasive health: Conference and workshops (pp. 1–4). IEEE.
- Andersen C. K., Wittrup-Jensen K. U., Lolk A., Andersen K., Kragh-Sørensen P. (2004). Ability to perform activities of daily living is the main factor affecting quality of life in patients with dementia. Health and Quality of Life Outcomes, 2(1), 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd, H. C., Evans, N. E., Cheston, R., Noonan, K., & Harris, N. (2017). Home testing of a digital prompter for people with dementia. Studies in Health Technology and Informatics, 242, 27--30. [PubMed] [Google Scholar]
- Boyd H. C., Evans N. M., Orpwood R. D., Harris N. D. (2017). Using simple technology to prompt multistep tasks in the home for people with dementia: An exploratory study comparing prompting formats. Dementia: The International Journal of Social Research and Policy, 16(4), 424–442. 10.1177/1471301215602417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucks R. S., Ashworth D. L., Wilcock G. K., Siegfried K. (1996). Assessment of activities of daily living in dementia: Development of the Bristol activities of daily living scale. Age and Ageing, 25, 113–120. [DOI] [PubMed] [Google Scholar]
- Carpenter B. D., Balsis S., Otilingam P. G., Hanson P. K., Gatz M. (2009). The Alzheimer’s disease knowledge scale: Development and psychometric properties. The Gerontologist, 49(2), 236–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cihak D., Alberto P. A., Taber-Doughty T., Gama R. I. (2006). A comparison of static picture prompting and video prompting simulation strategies using group instructional procedures. Focus Autism Other Developmental Disabilities, 21(2), 89–99. [Google Scholar]
- Delis D. C., Kaplan E., Kramer J. H. (2001). Delis-Kaplan executive function system. Technical manual. Psychological Corporation. [Google Scholar]
- Delis D. C., Kramer J. H., Kaplan E., Ober B. A. (2000). California verbal learning test (2nd ed.). Adult Version. Manual. Psychological Corporation.
- Dishman E., Carrillo M. C. (2007). Perspective on everyday technologies for Alzheimer’s care: Research findings, directions, and challenges. Alzheimer’s and Dementia, 3(3), 227–234. [DOI] [PubMed] [Google Scholar]
- Evans, N., Boyd, H., Cheston, R., Harris, N., & Noonan, K. (2020). The experience of using prompting technology from the perspective of people with dementia and their primary carers. Aging and Mental Health. Advance online publication. doi: 10.1080/13607863.2020.1745145. [DOI] [PubMed] [Google Scholar]
- Evans N., Cheston R., Harris N. (2015). Personal message cards: An evaluation of an alternative method of delivering simulated presence therapy. Dementia: The International Journal of Social Research and Policy, 15(6), 1703–1715. 10.1177/1471301215574363 [DOI] [PubMed] [Google Scholar]
- Evans N., Orpwood R., Adlam T., Chadd J., Self D. (2007). Evaluation of an enabling smart flat for people with dementia. Journal of Dementia Care, 15(6), 33–36. [Google Scholar]
- Graff M. (2009). Teaching and supporting clients with dementia and their caregivers in daily functioning. In International handbook of occupational therapy (pp. 433–449). Springer. [Google Scholar]
- Graff M., Vernooij-Dassen M., Thijssen M., Dekker J., Hoefnagels W., OldeRikkert M. (2007). Effects of community occupational therapy on quality of life, mood, and health status in dementia patients and their caregivers: A randomized controlled trial. The Journal of Gerontology Series A: Biological and Medical Sciences, 62(9), 1002–1009. [DOI] [PubMed] [Google Scholar]
- Hoey J., Boutilier C., Poupart P., Olivier P., Monk A., Mihailidis A. (2012). People, sensors, decisions: Customizable and adaptive technologies for assistance in healthcare. ACM Transactions on Interactive Intelligent Systems, 2(4), 20. [Google Scholar]
- Hsieh S., Schubert S., Hoon C., Mioshi E., Hodges J. (2013). Validation of the Addenbrooke’s Cognitive Examination III in frontotemporal dementia and Alzheimer’s disease. Dementia and Geriatric Cognitive Disorder, 36(3–4), 242–250. [DOI] [PubMed] [Google Scholar]
- Jamieson M., Cullen B., McGee-Lennon M., Brewster S., Evans J. (2014). The efficacy of cognitive prosthetic technology for people with memory impairments: A systematic review and meta-analysis. Neuropsychological Rehabilitation, 24(3–4), 419–444. [DOI] [PubMed] [Google Scholar]
- Kiresuk T., Sherman R. (1968). Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Mental Health Journal, 4(6), 443–453. [DOI] [PubMed] [Google Scholar]
- Lancioni G., Perilli V., Singh N., O’Reilly M., Sigafoos J., Cassano G., Pinto K., Minervini M. G., Oliva D. (2012). Technology-aided pictorial cues to support the performance of daily activities by persons with moderate Alzheimer’s disease. Research in Developmental Disabilities, 33(1), 265–273. [DOI] [PubMed] [Google Scholar]
- Lancioni G., Singh N., O’Reilly M., Sigafoos J., Tatulli E., Rigante V., Zonno N., Perilli V., Pinto K., Minervini M. (2010). Technology-aided verbal instructions to help persons with mild or moderate Alzheimer’s disease perform daily activities. Research in Developmental Disabilities, 31(6), 1240–1250. [DOI] [PubMed] [Google Scholar]
- Lines L., Hone K. (2006). Multiple voices, multiple choices: Older adults’ evaluation of speech output to support independent living. Gerontechnology, 5(2), 78–91. [Google Scholar]
- Marshall G., Amariglio R., Sperling R., Rentz D. (2012). Activities of daily living: Where do they fit in the diagnosis of Alzheimer’s disease? Neurodegenerative Disease Management, 2(5), 483–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechling L., Gustafson M. (2009). Comparison of the effects of static picture and video prompting on completion of cooking related tasks by students with moderate intellectual disabilities. Exceptionality, 17(2), 103–116. [Google Scholar]
- O’Neill B., Gillespie A. (2008). Simulating naturalistic instruction: The case for a voice mediated interface for assistive technology for cognition. Journal of Assistive Technology, 2(2), 22–31. [Google Scholar]
- Orpwood R., Chadd J., Howcroft D., Sixsmith A., Torrington J., Gibson G., Chalfont G. (2010). Designing technology to improve quality of life for people with dementia: User-led approaches. Universal Access in the Information Society, 9(3), 249–259. [Google Scholar]
- Orpwood R., Sixsmith A., Torrington J., Chadd J., Gibson G., Chalfont G. (2007). Designing technology to support quality of life of people with dementia. Technology and Disability, 19, 103–112. [Google Scholar]
- Rockwood K., Stolee P., Fox R. (1993). Use of goal attainment scaling in measuring clinically important change in the frail elderly. Journal of Clinical Epidemiology, 46, 1113–1118. [DOI] [PubMed] [Google Scholar]
- Small J. A., Gutman G., Makela S., Hillhouse B. (2003). Effectiveness of communication strategies used by caregivers of persons with Alzheimer’s disease during activities of daily living. Journal of Speech and Language Hearing Research, 46(2), 353–367. [DOI] [PubMed] [Google Scholar]
- Stolee P., Rockwood K., Fox R. A., Streiner D. L. (1992). The use of goal attainment scaling in a geriatric care setting. Journal of the American Geriatrics Society, 40, 574–578. [DOI] [PubMed] [Google Scholar]
- Vernooij-Dassen M. J., Felling A. J., Brummelkamp E., Dauzenberg M. G., van den Bos G. A., Grol R. (1999). Assessment of caregiver’s competence in dealing with the burden of caregiving for a dementia patient: A Short Sense of Competence Questionnaire (SSCQ) suitable for clinical practice. Journal of the American Geriatrics Society, 47(2), 256–257. [DOI] [PubMed] [Google Scholar]
- Wilson R., Rochon E., Mihailidis A., Leonard C. (2013). Quantitative analysis of formal caregivers’ use of communication strategies while assisting individuals with moderate and severe Alzheimer’s disease during oral care. Journal of Communication Disorders, 46(3), 249–263. [DOI] [PubMed] [Google Scholar]