Abstract
Introduction
Few studies have assessed the perception of teledermatologists about the utility and limitations of teledermatology, especially to diagnose a broad range of skin diseases. This study aimed to evaluate dermatologists’ confidence in teledermatology, its utility and limitations for dermatological conditions in primary care.
Methods
An analytical study that used a survey for dermatologists who diagnosed 30,916 patients with 55,012 lesions through teledermatology during a 1-year project in São Paulo, Brazil.
Results
Dermatologists found teledermatology useful for triage and diagnosis, especially for xerotic eczema, pigmentary disorders and superficial infections. Their confidence in teledermatology was statistically higher by the end of the project (p = 0.0012). Limitations included some technical issues and the impossibility to suggest how soon the patient should be assisted face-to-face by a dermatologist. The most treatable group of diseases by teledermatology was superficial infections (92%). The use of dermoscopy images would significantly increase the confidence to treat atypical naevi and malignant tumours (p < 0.0001 and p = 0.0003 respectively). Follow-ups by teledermatology or feedback from primary-care physicians would be desirable, according to the dermatologists.
Discussion
We found it interesting that dermatologists became increasingly confident in teledermatology after the project and how they classified teledermatology as useful for triage, diagnosis and even treatment of most types of skin conditions followed at primary care. Dermoscopy should definitely be added to the photographs, especially for malignant tumours and atypical naevi. Most of the technical limitations found could be solved with a few improvements in the software/platform.
Keywords: Teledermatology, survey, dermatologist, utility, limitations
Introduction
Teledermatology (TD) deals with delivering dermatologic care from a distance using technology. The two most frequently used models of the service are store-and-forward (SF) of shared digital photographs and real-time or live-interactive synchronous video conferencing TD.1–4 In a previous study, the use of TD shortened the wait times of in-person dermatology consultations and was considered reliable and accurate.5 The diagnostic accuracy of SF-TD is 80–90%6 and an average of 75% agreement between SF-TD and face-to-face consultation is observed.1 It is the most commonly used technology with a better cost-benefit ratio.7 Many studies have established the diagnostic precision and concordance of TD with dermoscopy, face-to-face evaluation and histopathologic findings.5,8–10
The use of TD has become widely accepted, especially for communication between general practitioners and dermatologists. In addition to making dermatology services accessible in remote areas, which is the initial purpose of TD,11,12 it also makes the referral process more efficient, safer and more convenient for patients,1,13,14 especially when there is a shortage of a dermatology workforce.15 There is a high prevalence of chronic dermatologic conditions and often limited access to dermatologists due to insurance scarcity in urban underserved communities.16
This was the case in São Paulo, Brazil, where from July 2017 to August 2018, 57,832 patients had been waiting for an appointment with a dermatologist through the public health system supported by the City Hall Municipality. This means patients waited almost a year for a face-to-face evaluation. As a result, the City Hall decided to create a programme in conjunction with Hospital Israelita Albert Einstein (HIAE), a private hospital, to assist those patients using TD. They were called by phone and, based on where they lived, were directed to three different public hospitals in the city to be photographed by trained nurse technicians. Using a smartphone, each referred lesion was photographed from three different standard angles and distances. Additionally, short clinical histories and information were collected, such as sex, age, self-declared race, history of bleeding or pruritus in the lesion, time of onset and location, which were input into a software application developed by HIAE, installed on smartphones used for this purpose. The data and pictures were uploaded to a secure platform, accessible only to the dermatologists from HIAE who took part in the project and had a login and password. The primary objective of the project was to give a diagnosis using an International Code of Disease 10 (ICD-10), treatment and/or orientation and referral for each lesion. When the webpage opened, dermatologists had to analyse the lesion photograph and mark a box ‘bad photograph’ if the quality was not sufficient to make a diagnosis. In those cases, the patient was directed to an in-person visit with a dermatologist. If the photograph was good-enough quality to be used, the dermatologist had to make the diagnosis according to the ICD-10 list. If needed, they could pick one or more treatments from a list of medications, provide instructions on how to use them and, finally, complete the consultation with comments, such as recommendations for patients (for example, avoid sun exposure, wear a hat, dry well between the toes, avoid hot water in the bath) and/or suggestions for exams to be requested by the physicians before, during, or after the treatment. After doing so, they had to choose one of three options for the referral of the patient: (a) back to a general physician; (b) face-to-face appointment with a dermatologist; (c) proceed directly to biopsy procedure and, after that, a face-to-face meeting with a dermatologist.
The number of patients participating in the project was 30,916, summing up to 55,012 lesions photographed, resulting in nearly 165,000 images to be evaluated by 13 dermatologists over 12 months.
There are very few studies evaluating the perception of teledermatologists about their confidence in TD and its utility and limitations, especially using the tool for diagnosing a broad range of diseases, such as in this project. For this reason, using such a large number of images examined by the dermatologists, we conducted an analytical study to evaluate their perceptions about TD while keeping the following objectives in mind:
How confident were the dermatologists about TD before and after the project?
Which limitations of TD have they encountered in the project as physicians or working online using this platform?
What is the utility of TD for triage, diagnosis and treatment of common dermatological complaints in primary care?
If they had access to dermoscopy for melanocytic naevi and malignant tumours, would they be more confident in their diagnosis?
Methods
Both the Ethics Committees of Hospital Israelita Albert Einstein and the Health Department of São Paulo County (CAAE: 97126618.6.30001.0086) approved this work and the study was conducted in accordance with the ethical standards on human experimentation and the Declaration of Helsinki. It was an analytical study that used a survey emailed to dermatologists who participated in the project. Our inclusion criterion was any dermatologist that has reported more than 1000 lesions in the project described above. Only one of 13 did not meet the criteria, so we questioned 12 dermatologists. All of them signed the consent form for this research. After this step, we emailed them a questionnaire (supplemental file 1) and the answers were anonymously collated in another computer file. Some survey questions just had ‘yes’ or ‘no’ answers, whereas in others, such as the dermatologists’ confidence and the limitations encountered in the project, a five-category rating scale (none, low, medium, high and maximum) was used. For the possibility of treating by TD, the five-category scale was never, almost never, half of the time, most of the time and several times. Questions about confidence in diagnosing and treating diseases or groups of diseases by TD were based on the most frequent ICD-10 disorders observed in this project. To analyse results in the five-category rating scale, we considered the first three (none, low and medium) as ‘low’ and the last two (high and maximum) as ‘high’. Then, we compared the groups ‘low’ versus ‘high’ pre- and post-TD use, utilizing the Graph Prism 6 software to calculate Fischer’s exact test and p values. A p value < 0.05 was considered statistically significant.
Results
A total of 12 dermatologists responded to the questionnaire. They used the TD tool for diagnosing 30,916 patients with 55,012 lesions. Each lesion was photographed in three positions, resulting in a total of 165,036 images for evaluation and one report per lesion. Table 1 lists the profiles of dermatologists who participated in this project. There were eight female dermatologists and four male dermatologists (two female: one male). The age range was 30 to 56 years old (mean: 42.3); time spent after board-certification varied for each dermatologist from 3 to 26 years (mean: 13). Three of the 12 (25%) also had a PhD. Only 2/12 (17%) had previous experience in TD for a short period or sporadically. The most common subspecialty among them was dermoscopy (50%), followed by skin cancer (33%). The number of lesion reports per physician ranged from 1161 to 11,173 (mean: 4570) and the period working on the project went from 2 to 12 months. There was a unanimous desire to continue working with TD by the end of the project.
Table 1.
Participant profiles.
| Dermatologist | Gender | Age (years) | Time as a specialist (years) | Degrees | Previous experience in TD/time | Subspecialty | Number of total reports | Willing to keep working with TD |
|---|---|---|---|---|---|---|---|---|
| T1 | F | 40 | 12 | MD; PhD | No | Dermoscopy | 4720 | Yes |
| T2 | F | 56 | 18 | MD | No | Skin cancer | 5024 | Yes |
| T3 | F | 39 | 9 | MD | No | Dermoscopy, psoriasis | 3735 | Yes |
| T4 | F | 48 | 20 | MD | No | Dermoscopy | 6709 | Yes |
| T5 | F | 30 | 3 | MD | Yes/1 year | Teledermatology | 3008 | Yes |
| T6 | M | 36 | 7 | MD | No | Skin cancer | 4233 | Yes |
| T7 | M | 33 | 5 | MD | Yes/sporadic | Dermoscopy | 3213 | Yes |
| T8 | M | 55 | 26 | MD, PhD | No | Skin cancer, STD | 1161 | Yes |
| T9 | F | 49 | 21 | MD, PhD | No | Skin cancer | 11,173 | Yes |
| T10 | M | 32 | 5 | MD | No | Dermoscopy, ADR | 5599 | Yes |
| T11 | F | 39 | 9 | MD | No | Dermoscopy | 4999 | Yes |
| T12 | F | 51 | 21 | MD | No | Dermatologic surgery;cosmetic dermatology | 1268 | Yes |
MD: medical doctor; PhD: doctor of philosophy; TD: teledermatology; STD: sexually transmitted diseases; ADR: adverse drug reactions; F: female; M: male.
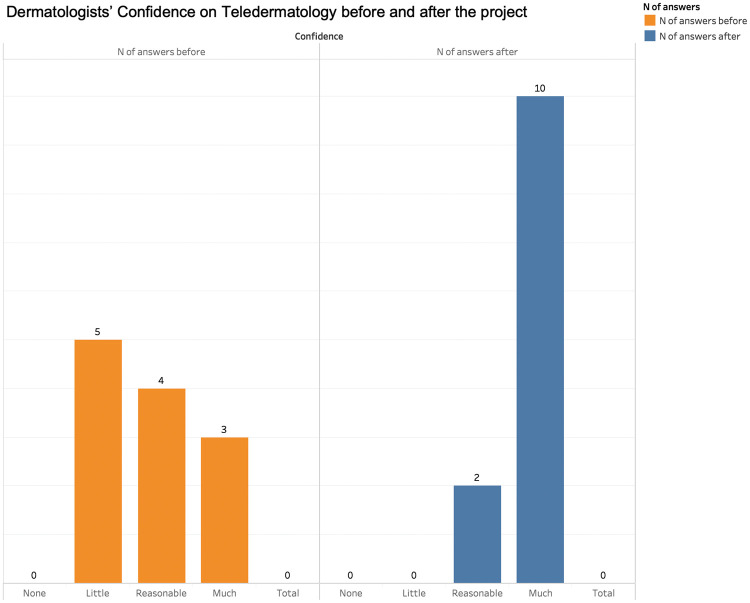
When asked to compare how confident the dermatologists felt about using TD as a tool before starting work on this project and after it, most had little or reasonable confidence before (9/12) and only 3/13 had a lot of confidence. By the end of the project, there was an inversion: 10/12 stated they were very confident and only 2/12 felt reasonably sure. No one felt little confidence by that point (Figure 1; p = 0.0012).
Figure 1.
Dermatologists’ confidence in teledermatology before and after the project.
The subjects were also asked about the utility of TD (Figure 2). Most of them (8/12) pointed that TD was useful for triage and diagnosis whereas 3/12 said it was useful for triage, diagnosis and treatment. Only one dermatologist answered TD was only useful for triage.
Figure 2.
Utility of teledermatology (n = 12).
Note. Please refer to the online version to see this figure in colour.
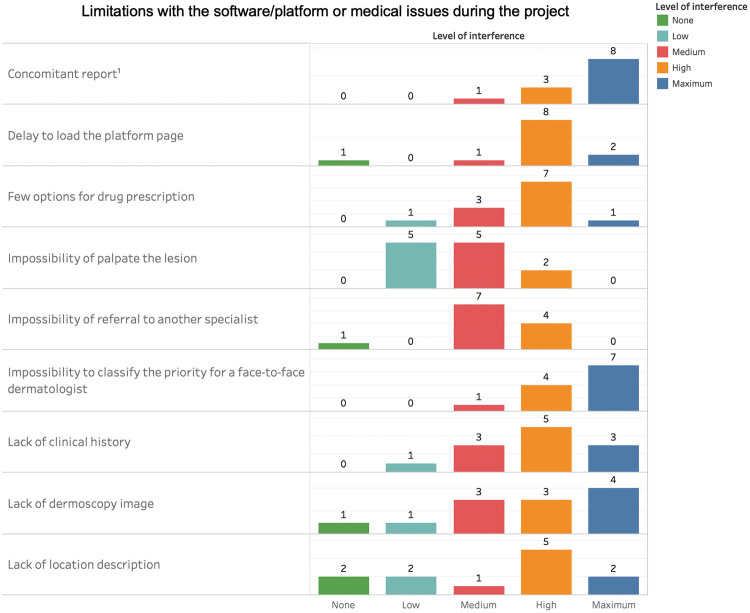
We came up with some questions about problems with the platform the physicians used to see the images and report on the questionnaire. As a project provided by the public health system, dermatologists faced some challenges as physicians (Figure 3). For example, the list of drug prescriptions had limited options (topical and oral drugs) and the procedure for referring a patient through the public health system had to follow a determined flow, as described in the Methods section. Those limitations interfered with physicians’ work and they were asked to grade how intense this interference was in a five-category scale (none, low, medium, high and maximum). For the analysis, we summed answers with the high and maximum levels of interference and compared it with the total number of responses on any given item.
Figure 3.
Limitations with the software/platform or as a physician during the project. 1When two or more teledermatologists were reporting lesions from the same patient, concomitantly, without knowing it. The first one to click the ‘done’ box saved the work. The other(s) lost their work.
Note. Please refer to the online version to see this figure in colour.
Regarding the limitations of the platform, the worst interference faced was that more than one dermatologist could report the same patient’s lesions at the same time without knowing it and one of them subsequently lost their work (11/12). The second largest problem was the delay in loading the next page after clicking ‘done’ (10/12). A lack of clinical history and stated location in the clinical data received 8 votes for high or maximum interference out of 12 voters.
For physicians’ limitations, such as physical examination, complementary exams, prescriptions and forwarding patients, they used the same scale and we compared them in the same way as mentioned above.
The worst medical issue the physicians faced was the impossibility of suggesting how soon the patient should be assisted face-to-face by a dermatologist (11/12). The protocol used in this project did not involve asking teledermatologists to suggest the time frame for in-presence consultation (days, weeks or months). The lack of options for drug prescriptions was the second worse situation involving work (8/12), followed by the lack of dermoscopy images (7/12). Some teledermatologists also wanted to directly refer the patient to another specialist, such as orthopedist and vascular surgeon. Only 2/12 dermatologists voted that the impossibility to palpate the lesion or feel its texture were issues of high or maximum interference in their work.
At the end of the project we also tested how confident dermatologists were about their diagnosis of certain common diseases using TD (Figure 4). Two hypothetical questions were used to search if the use of dermoscopy would change teledermatologists’ confidence in diagnosing malignant tumours and atypical or melanocytic naevi. We continued using the same procedure, adding those answers with a level of confidence that was high or maximum. The three groups of diseases with the highest confidence in diagnosing were xerotic eczema (12/12), pigmentary disorders and superficial infections (11/12 each), followed by scars (10/12), inflammatory lesions (9/12), benign tumours (7/12), alopecia/effluvium (6/12), benign subcutaneous nodules (4/12), malignant tumours without dermoscopy (3/12) and atypical naevi without dermoscopy (2/12). If physicians had access to dermoscopic images, the confidence on diagnosing typical or atypical naevi and malignant tumours would be high in 100% of the subjects. Analysing the confidence results from atypical naevi and malignant tumours with or without dermoscopy, we verified that adding dermoscopy images significantly increased teledermatogists’ confidence (p < 0.0001 and p = 0.0003 respectively).
Figure 4.
Dermatologists’ confidence in diagnosing diseases using teledermatology: 1vitiligo, melasma, solar lentigo, solar leukoderma, postinflammatory hyperpigmentation; 2melanocytic nevus, seborrheic keratosis, dermatofibroma, soft fibromas, acrochordon, warts; 3basal cell carcinoma, squamous cell carcinoma, melanoma; 4acne, psoriasis, atopic dermatitis, nummular eczema, stasis dermatitis, lichen simplex chronicus, seborrheic dermatitis, pityriasis alba; 5epidermoid cyst, trichilemmal cyst, lipoma; 6molluscum contagiosum, impetigo, folliculitis, tineas, candidiasis, scabies, onychomycosis, pityriasis versicolor; 7hypertrophic scar, keloid, stretch marks, acne scars; 8androgenic alopecia, alopecia areata, telogen effluvium.
Note. Please refer to the online version to see this figure in colour.
From the diseases in Figure 4, we excluded all conditions that needed surgical treatment, for obvious reasons, then asked the subjects to opine how frequently they could treat patients presented with the remaining dermatological disorders using TD. The five-category scale in this case was never, almost never, half of the time, most of the time and several times. Figure 5 below lists the number of answers in each category. Similar to the previous results, we added the first three grades (never, almost never and half of the time) as ‘low’ and the last two grades (most of the time and several times) as ‘high’ to analyse them.
Figure 5.
Possibility of treatment the following diseases using teledermatology.
1Vitiligo, melasma, solar lentigo, solar leukoderma, postinflammatory hyperpigmentation.
2Acne, psoriasis, atopic dermatitis, nummular eczema, stasis dermatitis, lichen simplex chronicus, seborrheic dermatitis, pityriasis alba.
3Molluscum contagiosum, impetigo, folliculitis, tineas, candidiasis, scabies, onychomycosis, pityriasis versicolor.
4Androgenic alopecia, alopecia areata, telogen effluvium.
From the dermatologists’ point of view, superficial infection was the condition that could most frequently be treated using TD (11/12), followed by xerotic eczema (10/12), inflammatory disease and alopecia/effluvium (9/12) then pigmentary disorders (8/12). Conditions whose primary choice of treatment demands face-to-face intervention, such as malignant or benign tumours, subcutaneous nodules, atypical naevi and scars were not enquired about.
Most of the spontaneous comments the subjects made at the end of the survey emphasized the need to have dermoscopy images along with the current photographs and the desire to have follow-ups of the patients by TD or feedbacks from the primary care physician of the treated patients.
Discussion
Our participants in this survey had different profiles and ranged from a young dermatologist who was just out of residency and only had a few years’ experience after obtaining his board certification as a specialist, to experienced professionals with more than 25 years of experience who held PhDs. Experience is an essential factor, as we wanted to see how ‘old-fashioned’ physicians could adapt to new tools such as TD. The 2:1 female: male dermatologist predominance reflects actual presence of women in dermatology in Brazil (78%) according to a recent study. Additionally, the mean age in our study (42.3 years) is compatible with the median age of dermatologists in Brazil (43 years).17 The vast majority had no experience in TD and for the two subjects that did, the timeframe was very short, which reflects that, in Brazil, TD is still in its infancy. Interestingly, even with such different profiles, all participants stated the desire to keep working and utilizing TD at the end of the project, which is very promising. The number of patients and lesions analysed by our subjects was impressive – nearly 31,000 and 55,000 respectively – which led to 165,000 different images, giving us a robust base to run the survey.
Confidence in TD was statistically greater by the end of the project. More than 40% of subjects jumped two grades in confidence after the study, 25% jumped one grade of confidence and the two who had high confidence at the beginning of the project remained high. One subject answered that they experienced a downgrading of one point in confidence between the start and the end of the project. Based on the project as it was, most of the dermatologists (91%) felt TD was useful for triage and diagnosis; 25% thought it would be suitable for treatment too. If the project permitted follow-ups, more dermatologists would possibly choose this second response.
SF-TD has many apparent advantages for patients and physicians, but it also has some inconveniences. Regarding the online platform, the fact that a person can experience some delay in loading pages, sending reports, or losing their work for technical reasons is an unpleasant situation and useful information technology support is essential. A lack of proper clinical history and information on the location can be avoided if a well-trained person collects the data. The impossibility of palpating and feeling the texture of lesions was surprisingly not overrated by teledermatologists as a limitation for TD, which would be hard to solve using today’s technology. In our project, there was no possibility to refer the patient to a different specialist (other than the three options available) or to grade the urgency with which we advise consultation with a face-to-face dermatologist appointment (days, weeks, or months). This could also be solved with future projects and is one of the many spontaneous suggestions dermatologists made, such as that follow-ups by TD would be very welcome.
Regarding teledermoscopy, it was found that adding dermoscopy images to conventional photographs of atypical or melanocytic naevi and malignant tumours significantly increased teledermatogists’ confidence (p < 0.0001 and p = 0.0003 respectively). Another study showed the addition of dermoscopic images substantially improves the diagnostic performance, efficacy and cost effectiveness of an SF-TD-based screening system for skin cancer, based exclusively on clinical images.18
Among common dermatological disorders, TD was useful to diagnose xerotic eczema, pigmentary disorders, superficial infections, scars, inflammatory lesions, benign tumours and hair disorders with a high grade of confidence. TD was not as efficient for subcutaneous nodules, as palpation and image exams are important steps to support the diagnosis. A study from India highlighted the utility of TD for leprosy, infectious dermatosis, contact dermatitis, urticaria, vitiligo, pigmented lesions and leg ulcers.7 Dermatologists stated that TD could most frequently be used to treat some prevalent diseases, such as superficial infections, xerotic eczema, inflammatory, hair and pigmentary disorders, especially if the follow-ups by TD or feedback from the primary care doctor were available.
In conclusion, the confidence of the dermatologists on TD was statistically greater by the end of the project (p = 0.0012). Most were of the opinion that TD was suitable for triage and diagnosis (91%). The most difficult problem they faced with the online platform was working on the reports concomitantly with another dermatologist without being aware of it (92%). The worst limitation as a physician was the impossibility of classifying the urgency for a face-to-face dermatologist appointment when referring the patient (92%). The highest confidence in diagnosing common dermatological diseases by TD was for xerotic eczema, pigmentary disorders and superficial infections. The use of dermoscopy images, besides clinical images, would significantly increase the confidence in TD for treating atypical naevi and malignant tumours (p<0.0001 and p = 0.0003 respectively). The most treatable group of diseases by TD was superficial infections (92%) and follow-ups by TD or through feedback from primary care physicians were desirable.
Supplemental Material
Supplemental Material for Dermatologists’ perceptions on the utility and limitations of teledermatology after examining 55,000 lesions by Mara Giavina Bianchi, Andre Santos and Eduardo Cordioli in Journal of Telemedicine and Telecare
Acknowledgements
The authors would like to thank Fabricio de Almeida Rodrigues Gonçalves for his survey assistance and Raquel Machado de Sousa for graphic design.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Supplemental material: Supplemental material for this article is available online.
References
- 1.Wurm EM, Hofmann-Wellenhof R, Wurm R, et al. Telemedicine and teledermatology: Past, present and future. J Dtsch Dermatol Ges 2008; 6: 106–112. [DOI] [PubMed] [Google Scholar]
- 2.Pathipati AS, Lee L, Armstrong AW. Health-care delivery methods in teledermatology: Consultative, triage and direct-care models. J Telemed Telecare 2011; 17: 214–216. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong AW, Kwong MW, Ledo L, et al. Practice models and challenges in teledermatology: A study of collective experiences from teledermatologists. PLoS One 2011; 6: e28687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loane MA, Gore HE, Bloomer SE, et al. Preliminary results from the Northern Ireland arms of the UK Multicentre Teledermatology Trial: Is clinical management by realtime teledermatology possible? J Telemed Telecare 1998; 4 Suppl 1: 3–5. [DOI] [PubMed] [Google Scholar]
- 5.Ferrándiz L, Ruiz-de-Casas A, Martin-Gutierrez FJ, et al. Effect of teledermatology on the prognosis of patients with cutaneous melanoma. Arch Dermatol 2012; 148: 1025–1028. [DOI] [PubMed] [Google Scholar]
- 6.Heinzelmann PJ, Williams CM, Lugn NE, et al. Clinical outcomes associated with telemedicine/telehealth. Telemed J E Health 2005; 11: 329–347. [DOI] [PubMed] [Google Scholar]
- 7.Kanthraj GR. Classification and design of teledermatology practice: What dermatoses? Which technology to apply? J Eur Acad Dermatol Venereol 2009; 23: 865–875. [DOI] [PubMed] [Google Scholar]
- 8.Kroemer S, Frühauf J, Campbell TM, et al. Mobile teledermatology for skin tumour screening: diagnostic accuracy of clinical and dermoscopic image tele-evaluation using cellular phones. Br J Dermatol 2011; 164: 973–979. [DOI] [PubMed] [Google Scholar]
- 9.Massone C, Brunasso AM, Hofmann-Wellenhof R, et al. Teledermoscopy: Education, discussion forums, teleconsulting and mobile teledermoscopy. G Ital Dermatol Venereol 2010; 145: 127–132. [PubMed] [Google Scholar]
- 10.Lamel SA, Haldeman KM, Ely H, et al. Application of mobile teledermatology for skin cancer screening. J Am Acad Dermatol 2012; 67: 576–581. [DOI] [PubMed] [Google Scholar]
- 11.Klaz I, Wohl Y, Nathansohn N, et al. Teledermatology: quality assessment by user satisfaction and clinical efficiency. Isr Med Assoc J 2005; 7: 487–490. [PubMed] [Google Scholar]
- 12.Lopez AM, Avery D, Krupinski E, et al. Increasing access to care via tele-health: The Arizona experience. J Ambul Care Manage 2005; 28: 16–23. [DOI] [PubMed] [Google Scholar]
- 13.Eminović N, de Keizer NF, Wyatt JC, et al. Teledermatologic consultation and reduction in referrals to dermatologists: A cluster randomized controlled trial. Arch Dermatol 2009; 145: 558–564. [DOI] [PubMed] [Google Scholar]
- 14.Massone C, Wurm EM, Hofmann-Wellenhof R, et al. Teledermatology: An update. Semin Cutan Med Surg 2008; 27: 101–105. [DOI] [PubMed] [Google Scholar]
- 15.Burdick AE. Teledermatology: Extending specialty care beyond borders. Arch Dermatol 2007; 143: 1581–1582. [DOI] [PubMed] [Google Scholar]
- 16.Resneck JS, Isenstein A, Kimball AB. Few Medicaid and uninsured patients are accessing dermatologists. J Am Acad Dermatol 2006; 55: 1084–1088. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt SM, Miot HA, Luz FB, et al. Demographics and spatial distribution of the Brazilian dermatologists. An Bras Dermatol 2018; 93: 99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferrándiz L, Ojeda-Vila T, Corrales A, et al. Internet-based skin cancer screening using clinical images alone or in conjunction with dermoscopic images: A randomized teledermoscopy trial. J Am Acad Dermatol 2017; 76: 676–682. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Dermatologists’ perceptions on the utility and limitations of teledermatology after examining 55,000 lesions by Mara Giavina Bianchi, Andre Santos and Eduardo Cordioli in Journal of Telemedicine and Telecare