Abstract
Purpose. It is currently still common practice to obtain conventional radiographs in the follow-up of surgically treated displaced intra-articular calcaneal fractures at regular intervals. There is, however, insufficient evidence that these radiographs can be used to predict functional outcome. The aim of the current study was to evaluate the correlation between the most commonly used angles on lateral radiographs and disease-specific patient-reported outcome measures (PROMs). Methods. Two available databases, containing a total of 233 patients, were used in this study. Eleven angles on the lateral images of the preoperative and at 1-year follow-up radiographs were measured. The 6 most commonly used angles were also measured immediately postoperatively. These 6 most commonly used angles were correlated with PROMs (American Orthopaedic Foot and Ankle Society hindfoot score, Foot Function Index) by a Spearman’s rho analysis. After a Bonferroni correction was applied, a P value of <.0042 was considered to be statistically significant. Results. After exclusion of bilateral fractures, primary arthrodesis, open fractures, wound infections, other wound complications, nonavailable radiographs, and nonresponders, 86 patients remained. No significant correlations were found between the measured angles on the preoperative and at 1-year follow-up radiographs and the PROMs. Conclusion. No apparent correlation between lateral radiograph morphology and outcome was detected. Therefore, long-term follow-up radiographs after confirmed healing may be restricted to patients with persistent complaints on indication.
Levels of Evidence: Prognostic, Level IV: Retrospective
Keywords: calcaneal fractures, radiographic, angles, functional outcome
“There is, however, insufficient evidence that the morphology of the calcaneus as depicted by lateral radiographs is correlated with functional outcome.”
Obtaining conventional radiographs at regular intervals during the follow-up of surgically treated displaced intra-articular calcaneal fractures is common practice. In these radiographs, several angles are often measured, such as the Böhler’s and Gissane’s angles, as a representation of overall calcaneal morphology. There is, however, insufficient evidence that the morphology of the calcaneus as depicted by lateral radiographs is correlated with functional outcome. Several studies have studied the role of conventional radiographs in assessing postoperative outcome.1-10 However, these studies are hampered by low number of included patients,2-4 by small numbers of used angles,3-7,9 or by not using disease-specific patient-reported outcome measures (PROMs).1,4,5,10 Traditionally, the evaluation of outcome of displaced intra-articular calcaneal fractures consists of 3 aspects: the PROMs; physical examination, including range of motion (ROM); and routine conventional radiographs. Various different angles that can be measured on the lateral radiograph to characterize calcaneal morphology have been described. The angles of Böhler11 and Gissane12 are the most commonly used. In addition, several other angles have been described in the literature (eg, calcaneal compression angle [CCA], DeLangre angle, facet inclination angle, tuber plantar angle). These angles have, however, been studied less often.
The aim of the current study was to evaluate the correlation between the most commonly used angles on lateral radiographs (preoperatively and at 1-year follow-up) and disease-specific PROMs. This in order to predict functional outcome and determine the need for routine radiographs during follow-up in displaced intra-articular calcaneal fractures.
The hypothesis was that when the angles are closer to the reported normal range studies, the outcome would be significantly better.
Patients and Methods
Patients
Two databases of previous publications13,14 were used for this study. The 233 patients included in these databases were all surgically treated for a displaced intra-articular calcaneal fracture. The inclusion criteria of these previous studies were for the study of Dingemans et al,13 operated calcaneal fractures from January 1, 2012 until July 1, 2015 and for the study of Backes et al,14 all patients operated on a calcaneal fracture between 2000 and 2011 with open reduction and internal fixation through an extended lateral approach. The first study contained a total of 139 patients who were surgically treated using either the extensile lateral approach (ELA) or the sinus tarsi approach (STA).13 The second study contained a total of 94 patients who were surgically treated, using the ELA.14 Patients were included in the current study if functional outcome scores were available and when at least the preoperative radiographs or the radiographs at follow-up were available. The exclusion criteria were bilateral fractured patients (n = 14), angles were not measurable due to primary arthrodesis (n = 27), or when the outcome was negatively influenced by concommitant ipsilateral foot fractures, open fractures or postoperative woundcomplications (n = 72). We also excluded patients who did not respond to the send questionnaires (n = 33) and 1 patient who did not have any available radiographs.
A total of 86 patients were included for analysis. Informed consent was obtained from all included patients according to the Declaration of Helsinki. All patients were operated at a single level-1 trauma center between May 2000 and August 2015.
Clinical Outcome Assessments
The PROMs used were the American Orthopaedic Foot and Ankle Society hindfoot score (AOFAS)15 and the Foot Function Index (FFI).16 Both the clinical outcome assessments were obtained at least 1.5 year after the surgery via postal questionnaires. Although the AOFAS score is not specific for calcaneal fractures it is the most frequently used outcome score in calcaneal fracture literature. The AOFAS score is usually divided into 4 categories. A score between 90 and 100 points is classified as excellent, between 80 and 89 points as good, between 70 and 79 points as fair, and <70 points as poor.15 In the FFI, lower scores reflect in better outcome, with zero points being the best possible score.17
Radiographic Measurements
The radiographs were obtained from the institutions PACS (picture archiving and communication system). Permission to perform this study was obtained from our institution’s Internal Reviewing Board. All measurements were done by LN. TS, a specialized foot-ankle trauma surgeon, verified a sample of the measurements. In case of discrepancies of more than 5°, measurements were repeated.
Conventional lateral radiographic images were obtained preoperatively, immediately postoperatively, and at 1-year follow-up according to the hospital protocol. Lateral radiographs are made with the central beam perpendicular to the detector with the usage of 50 kV and 6 mA·s parameter. The fluoroscopy during surgery was used for the measurements of the immediate postoperative angles. The angles were measured using the measuring tool in the radiologic program XERO Viewer.
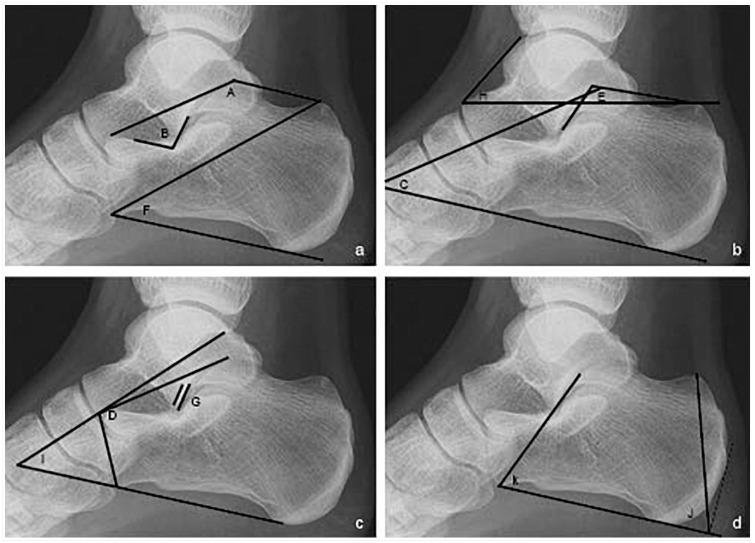
A total of 11 angles were found in the literature and measured on the preoperative, immediate postoperative, and at the 1-year follow-up radiographs. These angles were the Böhler’s angle (A),11, the angle of Gissane (B),12 CCA (C),18 DeLangre angle (D),19 facet inclination angle (E),20 front angle (F),21 Posterior Facet angle (G),22 talo-tuber angle (H),23 the talocalcaneal angle (TCA; I),24 tuber plantar angle (J),21 and the anterior-front angle (K). All individual angles are shown in Figure 1.
Figure 1.
Angles. (a) Böhler’s angle (A), the angle of Gissane (B), and front angle (F); (b) calcaneal compression angle (CCA) (C), facet inclination angle (E), talo-tuber angle (H); (c) DeLangre angle (D), Posterior Facet angle (G), the talocalcaneal angle (TCA) (I); and (d) tuber plantar angle (J), anterior-front angle (K).
Statistical Analysis
The data of the 11 preoperative and 1-year follow-up angles were analyzed using the Statistical Package for the Social Sciences (released 2016, SPSS for Macintosh, Version 24.0, IBM Corp, Armonk, NY). A Spearman’s rho analysis was performed on the data of the 6 most described angles (A, B, C, D, E, J). An analysis to find a correlation between the PROMs and the preoperative, immediate postoperative, and at 1-year follow-up for the 6 most commonly described angles (A, B, C, D, E, J) was performed. After a Bonferroni correction was applied, a P value of <.0042 was considered to be statistically significant.
Results
Demographics
A total of 86 patients were included. All measurements (preoperative, immediate postoperative and 1-year follow-up) were performed in 56% (n = 48) of the patients. In 17 patients, the preoperative radiographs were not available, or the quality of the images was insufficient to allow for accurate measurement. This left 69 patients available for analysis of the preoperative radiographs. For 5 patients, the immediate postoperative photographs were not available. This left 81 patients available for analysis of these immediate postoperative photographs. The 1-year follow-up radiographs were available for 77 patients. Demographics are shown in Table 1. The majority of patients were males (64%), the median age was 49 years (interquartile range [IQR] 38-58.3 years). The most common calcaneal fracture diagnosed was a Sanders type II. Median AOFAS and FFI were 84 (IQR 70-90.8) and 7.4 (IQR 1.2-15.7), respectively.
Table 1.
Demographics of Surgically Treated Intra-Articular Calcaneal Fractures (N = 86).
| Demographic | |
|---|---|
| Gender, n (%) | |
| Male | 55 (64) |
| Female | 31 (36) |
| Age, y, median [IQR] | 49 [38-58.3] |
| Sanders classification, % | |
| I | 8.1 |
| II | 62.8 |
| III | 22.1 |
| IV (%) | 1.2 |
| N/A | 5.9 |
| Surgical approach | |
| ELA, n (%) | 56 (65) |
| STA, n (%) | 30 (35) |
| IR, % | 34.9 |
| AOFAS score, median [IQR] | 84 [70.0-90.8] |
| FFI, median [IQR] | 7.4 [1.2-15.7] |
Abbreviations: N/A, not available; ELA, extensile lateral approach; STA, sinus tarsi approach; IR, implant removal.
Radiographic Data
The median and IQR of the 6 most commonly described angles preoperative, immediate postoperative, and at 1-year follow up are shown in Table 2. The median and IQR preoperative and at 1-year follow-up of the other 5 described angles are shown in the appendix. The results of the correlation between the PROMs and the preoperative, immediate postoperative, and at 1-year follow-up for the 6 most commonly described angles (A, B, C, D, E, and J) are displayed in Table 3. None of the 6 most commonly used angles were associated with either the AOFAS or the FFI.
Table 2.
Descriptive Data of the 6 Most Commonly Measured Angles.
| Angle | n, Preoperative | Median [IQR], Degree | n, Immediate Postoperative | Median [IQR], Degree | n, 1-Year Follow-up | Median [IQR], Degree |
|---|---|---|---|---|---|---|
| Böhler | 69 | 9.9 [1.6-19.4] | 81 | 30.4 [23.6-36.3] | 77 | 25.4 [18.6-31.0] |
| Gissane | 69 | 112.5 [100.9-122.4] | 81 | 113.0 [106.6-119.7] | 76 | 111.9 [110.7-120.5] |
| CCA | 69 | 24.1 [19.5-29.6] | 81 | 32.7 [27.6-37.0]] | 77 | 30.2 [24.2-33.3] |
| DeLangre | 69 | 83.9 [75.6-93.1] | 81 | 88.4 [80.0-93.95] | 77 | 85.9 [80.05-91.7] |
| Facet inclination | 69 | 47.5 [ 36.3-55.8] | 81 | 59.6 [52.6-67.1] | 76 | 56.7 [50.9-63.63] |
| Tuberplantar | 69 | 71.4 [ 68.9-74.0] | 81 | 73.2 [70.7-95.0] | 77 | 73.2 [71.0-75.4] |
Abbreviations: IQR, interquartile range; CCA, calcaneal compression angle.
Table 3.
Correlations Between the 6 Most Described Angles and the AOFAS/FFI PROMs.
| AOFAS | FFI | |||||
|---|---|---|---|---|---|---|
| Spearmans’s rho: | Correlation Coefficient | Significance | n | Correlation Coefficient | Significance | n |
| Böhler Preop | −0.013 | 0.915 | 69 | 0.004 | 0.972 | 69 |
| Böhler Di-post | −0.065 | 0.562 | 82 | 0.003 | 0.978 | 81 |
| Böhler 1-year FU | −0.028 | 0.811 | 77 | 0.016 | 0.888 | 76 |
| Δ pre - FU Böhler | −0.082 | 0.515 | 65 | 0.060 | 0.637 | 65 |
| ΔDi-post - FU Böhler | 0.007 | 0.955 | 74 | −0.053 | 0.658 | 73 |
| Gissane Pre-op | −0.047 | 0.704 | 69 | 0.032 | 0.794 | 69 |
| Gissane Di-post | 0.021 | 0.851 | 82 | 0.043 | 0.703 | 81 |
| Gissane 1-year FU | 0.005 | 0.967 | 76 | 0.085 | 0.468 | 75 |
| CCA Pre-op | −0.011 | 0.932 | 69 | 0.040 | 0.746 | 69 |
| CCA Di-post | −0.077 | 0.492 | 82 | 0.043 | 0.702 | 81 |
| CCA 1-year FU | −0.003 | 0.982 | 77 | 0.019 | 0.873 | 76 |
| DeLangre Pre-op | 0.051 | 0.680 | 69 | 0.023 | 0.852 | 69 |
| DeLangre Di-post | 0.172 | 0.123 | 82 | −0.088 | 0.435 | 81 |
| DeLangre 1-year FU | 0.089 | 0.440 | 77 | −0.112 | 0.335 | 76 |
| Facet inclination Pre-op | −0.038 | 0.758 | 69 | 0.045 | 0.713 | 69 |
| Facet inclination Di-post | −0.050 | 0.655 | 82 | 0.056 | 0.623 | 81 |
| Facet inclination 1-year FU | −0.095 | 0.413 | 76 | 0.058 | 0.618 | 75 |
| Tuberplantar Pre-op | 0.052 | 0.670 | 69 | −0.079 | 0.520 | 69 |
| Tuberplantar Di-post | −0.059 | −0.598 | 82 | 0.002 | 0.988 | 81 |
| Tuberplantar 1-year FU | 0.117 | 0.309 | 77 | −0.197 | 0.088 | 76 |
Abbreviations: AOFAS, American Orthopaedic Foot and Ankle Society hindfoot score; FFI, Foot Function Index; PROM, patient-reported outcome measure; Pre-op, preoperatively; Di-post, immediately postoperatively; FU, follow-up.
Discussion
In this study, no correlation was found between preoperative, immediate postoperative, and 1-year follow-up radiographs and the functional outcome following surgically treated displaced intra-articular calcaneal fractures. The 6 most commonly described angles (Böhler, Gissane, CCA, DeLangre, facet inclination, and tuber plantar) showed no statistically significant correlation with the AOFAS and FFI scores.
The angles of Böhler and Gissane are the most commonly used angles in the evaluation of the calcaneal fractures. Böhler mentioned his “tuber joint angle” for the first time in 1931.11 The angle has a normal range of 30° to 35°, which becomes sharper, straighter, or reversed with a calcaneal fracture. In our study, the injured preoperative angle had a median [IQR] of 9.9° [1.6-19.4]. The immediate postoperative angle had a median [IQR] of 30.5° [23.6-36.2]. At 1-year follow-up, the angle had a median [IQR] of 25.4° [18.6-31.0] degrees. In the current study, the normal 1-year follow-up range of 20° to 45°, as described in earlier studies,11,25,26 has not been achieved in all cases. In a systematic review by Van Hoeve et al,27 which included a total of 46 studies with a total of 2018 calcaneal fractures in 1776 patients, the preoperative median angle was 5° and postoperative 24°, values similar to our results. Van Hoeve et al27 furthermore described that a failure to restore the angle of Böhler has frequently been mentioned as an important predictor of outcome after operative treatment of calcaneal fractures. Agren et al4 argued that better restoration of the angle of Böhler has a significant better foot-ankle visual analogue score. However, this study did not correlate Böhler’s angle with calcaneal specific PROMs.
The crucial angle of Gissane was first described by Gissane in 1947.12 The angle has a normal range of 100° to 130°.12 In our study, the preoperative angle had a median [IQR] of 112.5° [100.9-122.4]. The immediate postoperative angle had a median [IQR] of 113.5° [106.7-119.7]. At 1-year follow-up, the angle had a median [IQR] of 111.9° [110.7-120.5]. In the literature, a reduction in Gissane’s angle is often shown, with a restoration following surgery. In our cohort these differences were small. This compares favorably with the absence of increase in the angle of Gissane pre- and postoperatively by Van Hoeve et al.27 In the literature, a relationship between the angle of Gissane and the outcome has, however, never been described.2
The CCA was first mentioned by Saxena et al18 in 1989. This angle is described for assessing the destruction and reduction of intra-articular calcaneal fractures involving the posterior subtalar joint. Saxena et al18 found a mean value of the preoperative CCA of 15°. After surgery, they found a mean CCA of 24.5°. The difference between the degrees are similar to our results (Δ8.6 immediate postoperative – preoperative) but the angles found in our study are larger (preoperative: median [IQR] of 24.1°, 19.5 - 29.6, immediate postoperative: median [IQR] 32.7°, 27.6 - 37.0, 1-year follow-up: median [IQR] 30.2°, 24.2 - 33.3).
The DeLangre angle was first used in calcaneal fractures by Massari et al19 in 2002. This angle is introduced to determine the outcome after surgical treatment with open reduction and internal fixation of intra-articular fractures (Sanders type II/III). The average (preoperative 89.7°, postoperative 90.3°) found in their study is comparable to the median found in the current study (preoperative: median [IQR] of 83.9°, 75.6 - 93.1, immediate post-operative: median [IQR] 88.4°, 80.0 - 93.95, 1-year follow up: [IQR] 85.9°, 80.05 - 91.7).
Sarrafian et al20 first described the facet inclination angle in 1983. This angle has an average of 65° with a minimum of 55° and a maximum of 75°. A larger inclination angle provides more flexion in the motion of the subtalar joint complex. We found a median (preoperative: median [IQR] of 47.5°, 36.3 - 55.8, immediate postoperative: median [IQR] 59.6°, 52.6 - 67.1, 1-year follow-up: [IQR] 56.7°, 50.9 - 63.63) are smaller than the average degrees mentioned by Sarrafian et al.20 What may indicate a decrease in flexion of the subtalar joint complex.
The tuber plantar angle was first described by Riepert et al21 in 1996. They used the tuber plantar angle, to determine the gender of patients. They found a mean of 73.0° and 72.0°, respectively, for female and male patients. In our study we also found similar average degrees for this angle (preoperative: median [IQR] of 71.4°, 68.9 - 74.0, immediate postoperative: median [IQR] 73.2°, 70.7 - 95.0, 1-year follow up: [IQR] 73.2°, 71.0 - 75.4). The similar median for immediate postoperative and 1-year follow-up indicates that this angle does not decline over time. We were unable to find any studies regarding this angle in combination with calcaneal fractures.
The findings of the present study, however, partly contradict earlier studies. Su et al9 showed a weak correlation between the postoperative Böhler’s angle and the AOFAS score. They showed, however, that there was no correlation between the preoperative angle of Böhler and the AOFAS score. Qiang et al6 found a statistically significant correlation between the difference between the Böhler’s angle and the reference value of the Böhler’s angle with the AOFAS measure. They found a correlation between Gissane’s angle, the reference value of the Gissane’s angle, and the AOFAS score as well. However, the reference values used in the study of Qiang et al6 are both based on a single study and the angles are all measured on a 3-dimensional model instead of lateral radiographs. Loucks and Buckley1 and Buckley at al10 found correlations between Böhler’s angle and PROMs when Böhler’s angle was divided into 3 groups. These studies, however, used the Short Form 36 (SF-36) and visual analogue scale instead of disease-specific PROMs.1,10 In accordance with our study Schepers et al2 described in 2013 that usage of plain radiographs is not useful in determining outcome after percutaneous reduction and fixation of intra articular calcaneal fractures. Based on the aforementioned findings of Qiang et al,6 the usage of 3-dimensional models might have additional value when correlating angles with PROMs.
We also measured the 6 most commonly described angles immediate postoperatively. It is a common finding that during follow-up the angle of Böhler decreases over time.26 In our study, the angle of Böhler decreased in 70.4% of the cases (n = 57 of total n = 81). The hypothesis for the angle of Gissane is that the angle increases with time. In our study, the angle of Gissane increased in 48.8% of the cases (n = 80). Overall, there is no correlation between the decrease in angles and the PROMs. The problem of the measurement of the immediate postoperative angles is the usage of intraoperative fluoroscopy and the lack of protocolled imaging. Backes et al26 described that collapse was correlated with the occurrence of postoperative wound infections and substance abuse. Gonzalez et al. found a reduction in Böhlers angle of 8 degrees over time independent of treatment modality.28 Johal et al29 even found a reduction of more than 10° for the angle of Böhler at final follow-up. However, no correlations between the collapse and the outcome were observed in their study as well.
A limitation of our study is the absence of an intra- and interobserver variability to increase the reliability of the measured angles, although the measured angles were saved and controlled by an independent observer. Knight et al25 researched the inter- and intraobserver variability of Böhler’s and Gissane’s angles. In their study, the interrater reliability for the angle of Böhler was 0.84 (excellent) and for the angle of Gissane 0.52 (poor).25 Veltman et al30 researched the inter- and intraobserver variability of 3 classification systems and the variability of Böhler’s and Gissane’s angles as well. In their study, the interobserver agreement for the angle of Böhler was moderate (0.57), which decreased with the use of 3-dimensional images (0.19). The intraobserver agreement found for Böhler’s angle was moderate (0.45). The interobserver agreement for the angle of Gissane was 0.11 (poor) and increased to 0.22 (slight) with the use of 2-dimensional images. The intraobserver agreement for the angle of Gissane was fair (0.35).30 As already described in the literature, our study found that the relative variation for the angle of Gissane is bigger than for the angle of Böhler.
Another weakness of our study is the number of excluded patients. Several patients were excluded when additional injuries or post operative wound complications may have influenced outcome negatively. For example open fractures and post-operative wound infection are known to cause lower outcome scores. It is uncertain if this is linked to a worse reduction as well. Shuler et al31 tried to find an answer to the question if drastic correction in Böhler’s angle resulted in increased incidence of wound-healing complications. They recommended avoidance of overcorrection because of the wound complications.31 More research needs to be done between restoring the anatomy and wound complications.
What often hindered accurate measurements was the lack of the unambiguous landmarks on the radiographs and the overprojection of the other bones or joints. Gonzalez et al. also described a measurement error for Böhlers angle of six degrees, which increased with radiographes that were more chephalad oblique.32 This made the PF angle (G) by far the most difficult angle to measure. Therefore, the [IQR] is large (pre: 4.1°-22.8° degrees, 1-year: 1.4°-12.9°) and the number of measurements lower than expected (pre: 60/69, 1-year: 74/77). There was an extra difficulty in the measurement of the tuber plantar angle because of the inability of the computer program to measure an angle with an extra 90° angle (J, Figure 1). To overcome this, measurements were performed by hand.
An advantage of this study is the number of angles identified and measured. A total of 11 angles were measured in 86 patients. We tried to correlate the 6 most described angles with the PROMs. In the most recent studies, Böhler’s angle, Gissane’s angle, the length and height of the posterior facet of the calcaneal bone, and the calcaneal width are the most commonly researched parameters.27,33 They are sometimes compared with the AOFAS PROM but most of the time not with the FFI and not with this many angles. Because of the usage of the Bonferroni correction, the results are more reliable.
In conclusion, no significant correlations between the 6 most commonly described preoperative, immediate postoperative, and 1-year follow-up angles with the outcome as measured using commonly used PROMs (AOFAS/FFI) in patients treated for displaced intra-articular calcaneal fractures could be identified. Thus, there appears to be a limited role for follow-up radiographs in surgically treated displaced intra-articular calcaneal fractures after healing of the fracture. Especially for long-term follow-up (eg, more than 1 year), the added value of radiographs might be less than previously assumed. Postoperative radiographs might only be reserved for patients with persisting complaints who might suffer from implant failure or for other indications such as medico-legal purposes. Future research should look for measurable predictors of outcome, for example, 3-dimensional imaging.
Appendix
Appendix.
Descriptive Statics of the 5 Less Used Angles.
| Angle | n, Preoperative | Median [IQR], Degrees | n, 1-Year Follow-up | Median [IQR], Degrees |
|---|---|---|---|---|
| Front | 69 | 42.2 [38.0-44.7] | 77 | 40.60 [37.7-43.3] |
| PF | 60 | 12.05 [4.1-22.8] | 74 | 5.85 [1.4-12.9] |
| Talotuber | 67 | 37.9 [34.1-43.7] | 73 | 39.5 [35.4-43.4] |
| TCA | 69 | 41.6 [35.5-45.7] | 75 | 44.1 [39.1-48.8] |
| Anterior front | 69 | 61.8 [56.0-66.8] | 77 | 63.4 [60.3-67.2] |
Abbreviations: IQR, interquartile range; PF, Posterior Facet; TCA, talocalcaneal angle.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Permission to perform this study was obtained from our institution’s Internal Reviewing Board.
Informed Consent: Informed consent was obtained from all included patients according to the Declaration of Helsinki.
Trial Registration: Not applicable.
ORCID iDs: Lynn E. Nooijen  https://orcid.org/0000-0002-5404-4637
https://orcid.org/0000-0002-5404-4637
Fay R.K. Sanders  https://orcid.org/0000-0002-5479-418X
https://orcid.org/0000-0002-5479-418X
References
- 1. Loucks C, Buckley R. Bohler’s angle: correlation with outcome in displaced intra-articular calcaneal fractures. J Orthop Trauma. 1999;13:554-558. [DOI] [PubMed] [Google Scholar]
- 2. Schepers T, Ginai AZ, Mulder PG, Patka P. Radiographic evaluation of calcaneal fractures: to measure or not to measure. Skeletal Radiol. 2007;36:847-852. [DOI] [PubMed] [Google Scholar]
- 3. De Groot R, Frima AJ, Schepers T, Roerdink WH. Complications following the extended lateral approach for calcaneal fractures do not influence mid- to long-term outcome. Injury. 2013;44:1596-1600. [DOI] [PubMed] [Google Scholar]
- 4. Agren PH, Mukka S, Tullberg T, Wretenberg P, Sayed-Noor AS. Factors affecting long-term treatment results of displaced intraarticular calcaneal fractures: a post hoc analysis of a prospective, randomized, controlled multicenter trial. J Orthop Trauma. 2014;28:564-568. [DOI] [PubMed] [Google Scholar]
- 5. Baptista M, Pinto R, Torres J. Radiological predictive factors for the outcome of surgically treated calcaneus fractures. Acta Orthop Belg. 2015;81:218-224. [PubMed] [Google Scholar]
- 6. Qiang M, Chen Y, Jia X, et al. Post-operative radiological predictors of satisfying outcomes occurring after intra-articular calcaneal fractures: a three dimensional CT quantitative evaluation. Int Orthop. 2017;41:1945-1951. [DOI] [PubMed] [Google Scholar]
- 7. Chan SWCN, Ng WK, Ip SKN, Chu PY, Wong WY, Yuen K. The clinical significance of common radiographic parameters of intraarticular calcaneal fractures in terms of pain duration after non-operative management. Poster presented at: European Cogress of Radiology: ECR 2015; March 4-8, 2015; Vienna, Austria. [Google Scholar]
- 8. Persson J, Peters S, Haddadin S, O’Loughlin PF, Krettek C, Gaulke R. The prognostic value of radiologic parameters for long-term outcome assessment after an isolated unilateral calcaneus fracture. Technol Health Care. 2015;23:285-298. [DOI] [PubMed] [Google Scholar]
- 9. Su Y, Chen W, Zhang T, Wu X, Wu Z, Zhang Y. Bohler’s angle’s role in assessing the injury severity and functional outcome of internal fixation for displaced intra-articular calcaneal fractures: a retrospective study. BMC Surg. 2013;13:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Buckley R, Tough S, McCormack R, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84:1733-1744. [DOI] [PubMed] [Google Scholar]
- 11. Böhler L. Diagnosis, pathology and treatment of fractures of the os calcis. J Bone Joint Surg. 1931;13:75-89. [Google Scholar]
- 12. Gissane W. Fractures of the os calcis. J Bone Joint Surg. 1947;29:254-255. [Google Scholar]
- 13. Dingemans SA, Meijer ST, Backes M, de Jong VM, Luitse JSK, Schepers T. Outcome following osteosynthesis or primary arthrodesis of calcaneal fractures: a cross-sectional cohort study. Injury. 2017;48:2336-2341. [DOI] [PubMed] [Google Scholar]
- 14. Backes M, Schep NW, Luitse JS, Goslings JC, Schepers T. The effect of postoperative wound infections on functional outcome following intra-articular calcaneal fractures. Arch Orthop Trauma Surg. 2015;135:1045-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [DOI] [PubMed] [Google Scholar]
- 16. Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44:561-570. [DOI] [PubMed] [Google Scholar]
- 17. Kuyvenhoven MM, Gorter KJ, Zuithoff P, Budiman-Mak E, Conrad KJ, Post MW. The foot function index with verbal rating scales (FFI-5pt): A clinimetric evaluation and comparison with the original FFI. J Rheumatol. 2002;29:1023-1028. [PubMed] [Google Scholar]
- 18. Saxena A, Weddington J. New radiographic angle to assess intra-articular calcaneal fractures. J Foot Surg. 1989;28:200-203. [PubMed] [Google Scholar]
- 19. Massari L, Ferrante R, Massini G, Artioli A. A new technique for treatment of calcaneal fractures with a multihole plate: indications and results. Foot Ankle Surg. 2002;5:39-45. [Google Scholar]
- 20. Sarrafian SK. Biomechanics of the subtalar joint complex. Clin Orthop Relat Res. 1993;(290):17-26. [PubMed] [Google Scholar]
- 21. Riepert T, Drechsler T, Schild H, Nafe B, Mattern R. Estimation of sex on the basis of radiographs of the calcaneus. Forensic Sci Int. 1996;77:133-140. [DOI] [PubMed] [Google Scholar]
- 22. Gardner MJ, Nork SE, Barei DP, Kramer PA, Sangeorzan BJ, Benirschke SK. Secondary soft tissue compromise in tongue-type calcaneus fractures. J Orthop Trauma. 2008;22:439-445. [DOI] [PubMed] [Google Scholar]
- 23. Ghorbanhoseini M, Ghaheri A, Walley KC, Kwon JY. Superior tuber displacement in intra-articular calcaneus fractures. Foot Ankle Int. 2016;37:1076-1083. [DOI] [PubMed] [Google Scholar]
- 24. Heywood AW. The mechanics of the hind foot in club foot as demonstrated radiographically. J Bone Joint Surg Br. 1964;46:102-107. [PubMed] [Google Scholar]
- 25. Knight JR, Gross EA, Bradley GH, Bay C, LoVecchio F. Boehler’s angle and the critical angle of Gissane are of limited use in diagnosing calcaneus fractures in the ED. Am J Emerg Med. 2006;24:423-427. [DOI] [PubMed] [Google Scholar]
- 26. Backes M, Dorr MC, Luitse JS, Goslings JC, Schepers T. Predicting loss of height in surgically treated displaced intra-articular fractures of the calcaneus. Int Orthop. 2016;40:513-518. [DOI] [PubMed] [Google Scholar]
- 27. van Hoeve S, Poeze M. Outcome of minimally invasive open and percutaneous techniques for repair of calcaneal fractures: a systematic review. J Foot Ankle Surg. 2016;55:1256-1263. [DOI] [PubMed] [Google Scholar]
- 28. Gonzalez TA, Lucas RC, Miller TJ, Gitajn IL, Zurakowski D, Kwon JY. Posterior Facet Settling and Changes in Bohler’s Angle in Operatively and Nonoperatively Treated Calcaneus Fractures. Foot Ankle Int. 2015;36(11):1297-309. [DOI] [PubMed] [Google Scholar]
- 29. Johal HS, Buckley RE, Le IL, Leighton RK. A prospective randomized controlled trial of a bioresorbable calcium phosphate paste (alpha-BSM) in treatment of displaced intra-articular calcaneal fractures. J Trauma. 2009;67:875-882. [DOI] [PubMed] [Google Scholar]
- 30. Veltman ES, van den Bekerom MP, Doornberg JN, et al. Three-dimensional computed tomography is not indicated for the classification and characterization of calcaneal fractures. Injury. 2014;45:1117-1120. [DOI] [PubMed] [Google Scholar]
- 31. Shuler FD, Conti SF, Gruen GS, Abidi NA. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures: does correction of Bohler’s angle alter outcomes? Orthop Clin North Am. 2001;32:187-192. [DOI] [PubMed] [Google Scholar]
- 32. Gonzalez TA, Ehrlichman LK, Macaulay AA, Gitajn IL, Toussaint RJ, Zurakowski D, Kwon JY. Determining Measurement Error for Bohler’s Angle and the Effect of X-Ray Obliquity on Accuracy. Foot Ankle Spec. 2016;9(5):409-16. [DOI] [PubMed] [Google Scholar]
- 33. Zhang T, Chen W, Su Y, Wang H, Zhang Y. Does axial view still play an important role in dealing with calcaneal fractures? BMC Surg. 2015;15:19. [DOI] [PMC free article] [PubMed] [Google Scholar]