Abstract
Purpose
To describe in detail the technique used and results of disruption of ingrown epithelium via Nd:YAG laser (DIEYAG) after LASIK treatment and enhancement.
Observations
Epithelial ingrowth following laser in situ keratomileusis (LASIK) enhancement has the potential to cause significant refractive error and discomfort when allowed to progress. This retrospective case series following seven eyes after LASIK enhancement and one eye with flap trauma, assessed the effectiveness and safety of the disruption of ingrown epithelium via Nd:YAG laser. In all cases, we found that the progression of ingrown epithelium was eliminated. Using best spectacle corrected visual acuity and topography as our main outcome measures, we found that refractive error and visual disturbance caused by ingrowth stabilized or improved, with no subsequent complications identified.
Conclusion and Importance
The disruption of ingrown epithelium via Nd:YAG laser offers a safe and effective alternative to other treatments for epithelial ingrowth after LASIK treatment and enhancement.
Keywords: Epithelial ingrowth, LASIK, LASIK enhancement, Corneal flap, YAG laser
Introduction
Epithelial ingrowth following laser in situ keratomileusis (LASIK) enhancement has the potential to cause significant refractive error and discomfort when allowed to progress. There are a number of techniques currently utilized for the management of epithelial ingrowth. We and others have had documented success in disruption of ingrown epithelium via Nd:YAG laser which we refer to as, and for which we propose the acronym, DIEYAG.1, 2, 3
The most common complication of LASIK is undercorrection, which may be managed by lifting the flap and performing additional laser ablation.4 However, lifting the flap has the disadvantage of nonuniform trauma to the flap edge which can be sufficient to introduce epithelial cells beneath the flap or increase edema at the edge, coinciding with a higher incidence of epithelial ingrowth after enhancement compared to after initial LASIK.4, 5, 6, 7 Epithelial ingrowth can be defined as the proliferation of epithelial cells in the space between the stromal bed and flap.8 It can be further categorized as clinically significant ingrowth (if central, progressing, and/or causing reduced visual acuity or increased visual symptoms) or non-clinically significant (at the flap border, stable, and/or causing no change in visual acuity). The incidence of epithelial ingrowth following primary LASIK varies from 0.2 to 12%; following enhancement, it may increase up to 32%.1 Multiple methods of managing ingrowth have been described in the literature which have shown varying rates of success. These methods include: lifting and scraping ingrowth with or without adjuvant alcohol or mitomycin-C (MMC); use of fibrin adhesive or suturing of the flap edge following lift and scrape; and Nd:YAG laser disruption of the ingrowth.
This refractive practice has had experience with a variety of these techniques with varying success. However, Nd:YAG laser treatment appears to show significant promise as a noninvasive and effective treatment for primary or recurrent epithelial ingrowth. A small case series is presented here that shows significant improvement in eyes treated with this technique. This further supports data presented by Ayala et al. and others (Table 1) which showed Nd:YAG laser treatment of epithelial ingrowth to be safe and effective.1, 2, 3
Table 1.
Study comparisons.
| Ayala et al.1 | Mohammed et al.2 | Lindfield et al.3 | |
|---|---|---|---|
| Country | Spain | Egypt | United Kingdom |
| Year | 2018 | 2019 | 2012 |
| Sample Size | 38 Eyes | 41 Eyes | 2 Eyes |
| Definition of Treatment Success | Corneal topographic and visual symptomatic improvement (100%); complete disappearance of ingrowth opacities occurred in 80% | Complete regression and resolution of ingrowth (100%) | Symptomatic relief and microscopic improvement of ingrowth (100%) |
Case 1
A 52-year-old Caucasian female initially had LASIK performed bilaterally in 2007. The Hansatome (Bausch & Lomb, Rochester, NY) was used. Both eyes were correctable to 20/20 before and after initial LASIK treatment. In 2010, her uncorrected distance visual acuity (UCDVA) had improved from 20/60+ OD and 20/50- OS to 20/25- OD and 20/20- OS. Her manifest refraction was plano-0.75 × 175 20/20 OD and plano-0.50 × 135 20/20- OS. At this time she showed early signs of epithelial ingrowth around the flap edge of both eyes. Several weeks later she began to develop significant epithelial ingrowth and her UCDVA had decreased to 20/30 and 20/25 OD and OS, respectively. That day the flaps were lifted and the epithelium was debrided from the flap edge, the underside of the flap, the stromal bed, and 1–2mm around the outer margin of the flap. Improvement was noted on the first postoperative day. Ingrowth recurred one month later, however UCDVA remained 20/20 OU. Two weeks following this exam her UCDVA had declined OD to 20/30 with a manifest refraction of −0.75-0.25 × 127 and she was scheduled for disruption of ingrown epithelium via Nd:YAG laser one week later.
Technique
Two drops of proparacaine were instilled into each eye. An Abraham Peripheral Iridotomy (PI) lens (Accutome, Malvern, PA) was placed on the eye to be treated. Hypromellose 2.5% (Goniovisc, Accutome, Malvern, PA) was used as a coupling agent. The laser, 7970 Nd:YAG (Coherent, Inc. Palo Alto, CA) was set at the lowest setting (per pulse energy 0.5mJ–0.7mJ depending on the tissue response) and the HeNe beams were focused on the area of ingrowth. Shots were distributed in an effort to create cavitation bubbles adjacent to one another in the area of ingrowth. If a pulse was placed too deep, a starburst pattern would appear in the corneal stroma. If a pulse was placed too shallow, a cavitation bubble would appear in the goniosol and float harmlessly away. Therefore, pulses were aimed slightly shallow so that a suboptimal pulse location would be more likely to fall in the goniovisc rather than in the stroma of the cornea. This resulted in a high percentage of pulses falling in the goniovisc. However, the procedure was continued until satisfactory cavitation bubbles were seen in the area of the epithelial ingrowth. 203 pulses were applied to the right eye with a total energy of 123.3mJ. The left eye received 121 pulses with a total energy of 65.4mJ. The patient tolerated the procedure well and was placed on fluorometholone (FML) QID for 14 days following the procedure.
Upon subsequent visits the ingrowth appeared quiescent with none of the typical amoeboid pattern or interface bubbles common with active ingrowth. Three weeks post-DIEYAG, UCDVA OS had improved to 20/20; however, despite the quiescent appearance of ingrowth in both eyes, UCDVA OD and BSCDVA OD decreased with a concomitant increase in astigmatism. Manifest refraction OD was +0.25–1.25 × 151 20/25. Therefore, a second lift and scrape procedure and application of TISSEEL (Baxter Pharmaceuticals, Deerfield, IL) was scheduled for OD two weeks later. Fortunately, the ingrowth continued to appear quiescent by this time with no increase in astigmatism or decrease in UCDVA or BSCDVA. Manifest refraction OD was essentially unchanged. The patient was content to postpone any further intervention, and one month later her UCDVA OD had improved to 20/25 and BSCDVA OD had also improved to 20/20 with a manifest refraction of +0.25–0.25 × 135. Slit lamp examination of both eyes showed corneal patterns consistent with resolved ingrowth in the affected areas.
Case 2
A 39-year-old female initially had custom LASIK performed bilaterally in 2007 as described above. Both eyes were correctable to 20/20 before and after initial LASIK treatment. She subsequently underwent flap lift enhancement OU three years later. Her treatment refraction was −1.00-0.50 × 139 OD and −0.50-0.75 × 056 OS. A 6.5mm optical zone was used. Several months following enhancement her UCDVA had improved to 20/15 OU. At this time she showed early signs of epithelial ingrowth temporally along the flap edge OD, as well as nasally and temporally around the flap edge OS. Ingrowth progressed over the next few weeks and while her UCDVA remained at 20/15 OD, it had decreased to 20/20 OS. That day she underwent the DIEYAG procedure (see Technique above).
68 pulses were applied to the right eye with a total energy of 45.3mJ. 251 pulses were applied to the left eye with a total energy of 167.9mJ. The patient tolerated the procedure well and was placed on prednisolone acetate 1.0% QID for 14 days following the procedure.
Three months post-DIEYAG UCDVA had improved to 20/15- OS. There were no signs of progression of ingrowth. Of note, on slit lamp examination there were a few small vacuoles (<0.1mm diameter) in the stroma of the cornea deep to the area of treated epithelial ingrowth. These vacuoles may represent areas of the stroma that had inadvertently received Nd:YAG laser treatment during DIEYAG.
Case 3
A 46-year-old Caucasian male initially had LASIK performed bilaterally in 2006. Both eyes were correctable to 20/20 before and after initial LASIK treatment. The patient desired monovision with the OD target at near. Three years later manifest refraction OD was −0.75 sphere 20/20. The patient complained of difficulty reading with his near eye which had uncorrected near visual acuity (UCNVA) of J3 and subsequently underwent flap lift enhancement OD. Four months post-DIEYAG UCNVA had improved to J1 OD and the patient was delighted with the result. At this time, however, he showed early signs of epithelial ingrowth around the flap edge OD. The ingrowth remained stable but showed some signs of progression two months later, with UCNVA remaining at the J1 level. After an additional two months, ingrowth had progressed enough that the patient underwent the DIEYAG procedure (see Technique above). By this time UCNVA had decreased to J2 and manifest refraction was −0.25-1.75 × 003 20/20.
For his right eye, 266 pulses were applied to the temporal area of ingrowth and 97 pulses to the nasal area with total energies of 259.4mJ and 61.5mJ respectively. The patient tolerated the procedure well and was placed on FML QID for 14 days following the procedure. One month post-DIEYAG his UCNVA had improved to J1 OD. There were no signs of progression of ingrowth. Manifest refraction was plano-1.50 × 180 20/20.
Case 4
A 47-year-old male initially had LASIK performed OD in 2013. Both eyes were correctable to 20/20 before and after initial LASIK treatment. He underwent flap lift enhancement OD one year later. Seven months after enhancement, his UCDVA OD was 20/40. No epithelial ingrowth was noted at this time, and he underwent a second flap lift enhancement several months later. His UCDVA OD improved to 20/20 one month following enhancement, but epithelial ingrowth was visualized at this time along the inferotemporal area (Fig. 1). He subsequently underwent the DIEYAG procedure (technique was the same as described above, however a different laser was used–the Tango™ Nd:YAG Laser, Ellex Medical Pty Ltd, USA). 411 pulses were applied in the right eye with a total energy of 304.8mJ and successful treatment was affirmed by the presence of bubbles at the flap interface (Fig. 2). The patient tolerated the procedure well. Two weeks post-DIEYAG, UCDVA OD remained 20/20 and regressed ingrowth was confirmed. Regression was again confirmed approximately one month post-DIEYAG on both slit lamp examination (Fig. 3) and Pentacam (Fig. 4).
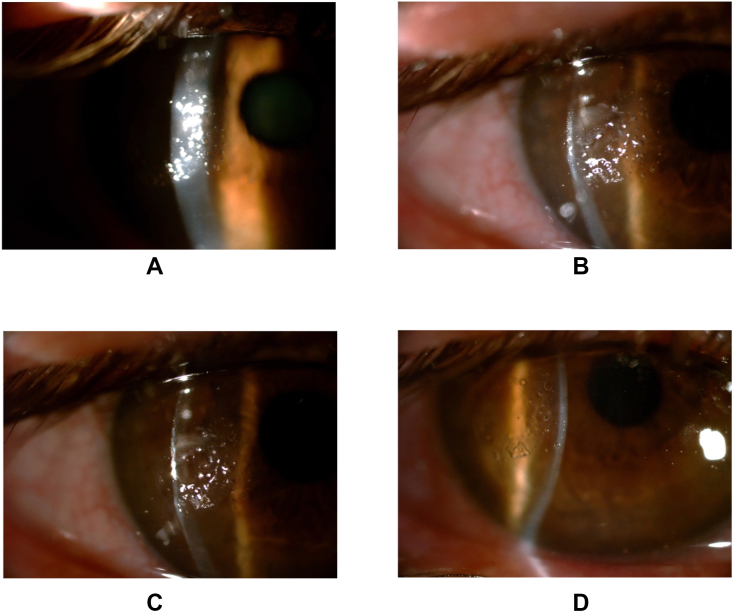
Fig. 1.
A-B. Pre-YAG: Pictures taken one month after flap lift enhancement. Epithelial ingrowth can be seen in a pseudopodial configuration.
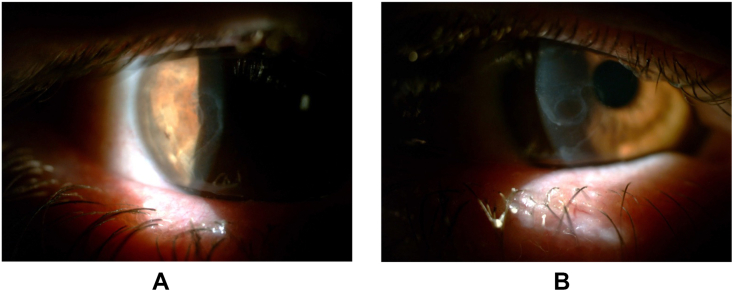
Fig. 2.
A-D. Two Minutes Post-YAG: Bubbles in the interface between the flap and the stromal bed indicate success of treatment. These arise when laser energy is applied directly to areas of ingrowth.
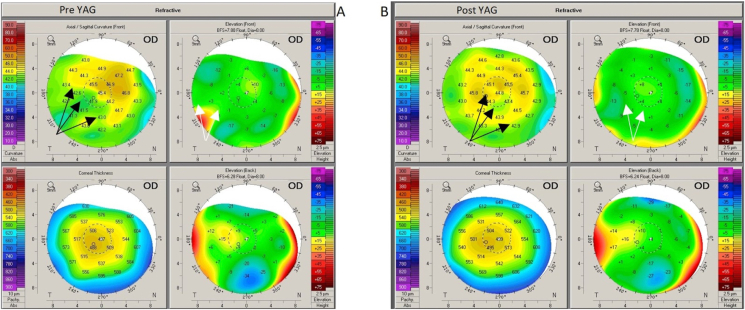
Fig. 3.
A-B. Regressed ingrowth approximately one month after treatment with DIEYAG.
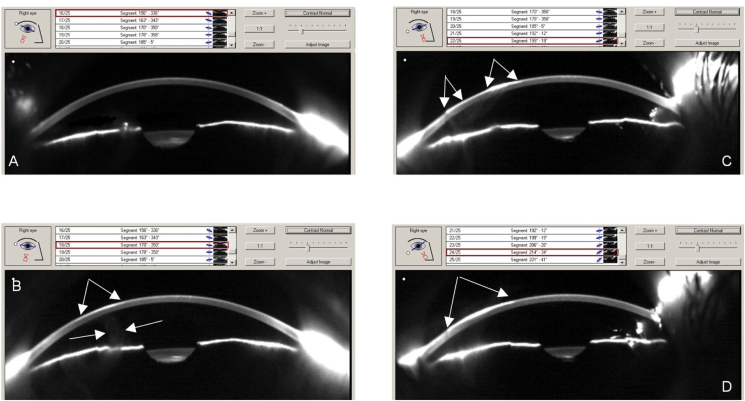
Fig. 4.
The Pentacam (Oculus, Inc, Arlington, WA) labeled “Pre YAG” was captured immediately before DIEYAG was performed. The Pentacam labeled “Post YAG” was captured approximately one month after DIEYAG. Black arrows correspond to areas of flattening on the axial map, and white arrows correspond to areas of elevation above the best fit sphere on the elevation map. Both normalize following YAG laser treatment.
Case 5
A 55-year-old male initially had LASIK performed bilaterally circa 2005 outside of our LASIK center. In 2015, he experienced a corneal abrasion OS from a falling metal rod. In addition, the rod caused the temporal flap edge to fold under the flap. Therefore, it was necessary to refloat the flap in that area. As a result he developed epithelial ingrowth OS in this same area.
He was scheduled to undergo DIEYAG one month after the inciting trauma. Before the DIEYAG procedure, UCDVA OS was 20/25. He tolerated the procedure well and was placed on prednisolone acetate 1.0% QID for 14 days and ciprofloxacin drops QID for 7 days following the procedure. The next day, UCDVA was 20/30. By one month post-DIEYAG, UCDVA had improved to 20/20. Four months later UCDVA remained 20/20, but with some clouding and glare at night. He was considering additional DIEYAG at this time.
Case 6
A 63-year-old male initially had LASIK performed bilaterally in 2015. Both eyes were correctable to 20/20 before and after initial LASIK treatment. Postoperative UCDVA was 20/20 OU. By one month post-DIEYAG, UCDVA remained 20/20 OU yet the patient expressed disappointment due to poor night vision and some ocular pruritus OU. Epithelial ingrowth was noted at this time, and DIEYAG was performed with the technique and laser as noted in Case 4.
223 pulses were applied to the left eye with a total energy of 164.1mJ, and the patient tolerated the procedure well. Two weeks post-DIEYAG, UCDVA was 20/20 OS. On slit lamp examination, the cornea of the left eye showed resolving epithelial ingrowth inferiorly with slight haze present.
Discussion
Epithelial ingrowth is a well-documented complication of both LASIK and LASIK enhancement. There have been two proposed hypotheses for the mechanism of epithelial ingrowth. One theory is that implantation of epithelial cells under the flap occurs during the surgery; the other theory is that there is a postoperative invasion of surface epithelial cells under the edge of the corneal flap.9, 10, 11 Deposited epithelial cells appear to have limited ability to proliferate due to poor nutrient supply, supporting the postoperative migration theory.10 Thus, ingrowth is proposed to stem from poor adherence of the flap edge allowing epithelial cells to invade the lamellar surface.5,12,13
Only a small percentage of patients with epithelial ingrowth require surgical treatment, as epithelial growth in the corneal interface following LASIK is in most cases self-limiting.9,10,14, 15, 16, 17 Surgical intervention is aimed at removing the existing cells in the interface and sealing the interface surface and resection edge to prevent further ingrowth.17 While there are currently a number of techniques available for the management of epithelial ingrowth, there has not been a definitive conclusion regarding which treatment is the most efficacious. Currently the most common technique for removing epithelial ingrowth is to lift the flap and mechanically debride the flap undersurface and stromal bed to remove the invasive tissue.7,15,18 In most cases of ingrowth this method is adequate; other treatment options include flap suturing, flap removal, ethanol use, fibrin glue surgical adhesive, or adjuvant phototherapeutic keratectomy.18, 19, 20, 21, 22, 23, 24, 25
The authors feel that it is imperative to define a more standardized approach to managing ingrowth that is not only efficacious, but also takes into consideration the psychological and lifestyle impact of additional surgery on an otherwise healthy eye. We believe that techniques involving multiple trips to the operating room, multiple episodes of recovery, additional risk of infection, placement of corneal sutures, application of tissue sealant or antimetabolites, or higher risk of recurrence of ingrowth should be employed as infrequently as possible.
YAG laser treatment of epithelial ingrowth has the advantages of being noninvasive, quick and effective. It can be done with little discomfort and repeated if necessary without subjecting the patient to the risks mentioned previously. Psychologically, patients have already accepted the idea of laser treatment for their refractive error and thus are more likely to accept additional laser to manage their ingrowth. For these reasons the authors feel that this technique should be considered as a first line of treatment for progressive ingrowth causing discomfort or change in refractive error.
The purpose of this paper was to describe in detail the technique used and results of disruption of ingrown epithelium via Nd:YAG laser (DIEYAG), further summarized in Table 2 and Table 3. Following patients through their progression of LASIK, enhancement, and management of epithelial ingrowth, we tracked visual acuity throughout their treatment course and found improvement in all patients treated with DIEYAG.
Table 2.
Case totals.
| Eye | Case 1 |
Case 2 |
Case 3 |
Case 4 |
Case 6 |
||
|---|---|---|---|---|---|---|---|
| OD | OS | OD | OS | OD | OD | OS | |
| Laser Model | Coherent 7970 | Coherent 7970 | Coherent 7970 | Coherent 7970 | Coherent 7970 | Tango | Tango |
| Pulses | 203 | 121 | 68 | 251 | 363 | 411 | 223 |
| Total Energy (mJ) | 123.3 | 65.4 | 45.3 | 167.9 | 320.9 | 304.8 | 164.1 |
Table 3.
DIEYAG Instructions.
| Utilization: | When ingrowth is clinically significant (central, progressing, and/or causing reduced visual acuity or increased visual symptoms), and when patient prefers laser treatment over more invasive surgical options |
| Settings: |
|
| Assessment: | Before DIEYAG: Define extent of the ingrowth observed on biomicroscopy; approximate borders are also seen as hyperreflective areas on corneal cross section with Pentacam |
| Successful treatment: Bubbles at interface between the flap and stromal bed appear when laser energy is applied directly to areas of ingrowth | |
| Follow up: Halting of progression and gradual dissolution of ingrowth are observed on biomicroscopy and Pentacam corneal cross section |
One can gauge successful treatment during the DIEYAG procedure as indicated by bubbles seen in the interface between the flap and stromal bed, arising when laser energy is applied directly to areas of ingrowth (Fig. 2). In assessment of epithelial ingrowth, approximate borders of these areas can be seen as hyperreflective areas on corneal cross section with Pentacam Scheimpflug images (Fig. 5, Video 1). In all cases, prevention of progression with gradual dissolution of epithelial ingrowth was confirmed on slit lamp examination (Fig. 3), and no sight-threatening complications were noted.
Fig. 5.
Pentacam Scheimpflug images before YAG treatment. A: No ingrowth observed in corneal cross section. B,C,D: Hyperreflective areas with epithelial ingrowth. White arrows indicate approximate borders of areas of ingrowth.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.ajoc.2021.101071
The following is the supplementary data related to this article:
Scrolling images of Fig. 5. Hyperreflective areas with epithelial ingrowth can be seen in the corneal cross section around the 9 o'clock position. (Video credit to John VanDoorne).1
Conclusion
This small series involving eight eyes of six patients shows that this procedure offers what appears to be a safe and effective alternative to other established treatments for this condition. Following patients through their progression of LASIK, enhancement, and management of epithelial ingrowth, we tracked visual acuity throughout their treatment course and found improvement in all patients treated with DIEYAG. Small sample size is the most significant limitation of this retrospective series. Additionally, a longer follow up time course of one year or greater would be beneficial.
Finally, since ingrowth is far more common after flap lift LASIK enhancement, we do not feel that the LASIK flap should be routinely lifted when treating patients who are post-LASIK and beyond the one-year recovery period for the procedure. Enhancements with photorefractive keratectomy have multiple advantages which have been elucidated elsewhere.26
Patient consent
Consent to publish the case series was not obtained. This report does not contain any personal information that could lead to the identification of the patients.
Funding
None.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Declaration of competing interest
The authors have no financial disclosures.
Acknowledgements
None.
References
- 1.Ayala M.J., Alio J.L., Mulet M.E., De La Hoz F. Treatment of laser in situ keratomileusis interface epithelial ingrowth with neodymium:yttrium-aluminum-garnet laser. Am J Ophthalmol. 2008;145(4):630–634. doi: 10.1016/j.ajo.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 2.Mohammed O.A., Mounir A., Hassan A.A., Alsmman A.H., Mostafa E.M. Nd:YAG laser for epithelial ingrowth after laser in situ keratomileusis. Int Ophthalmol. 2019;39(6):1225–1230. doi: 10.1007/s10792-018-0923-1. [DOI] [PubMed] [Google Scholar]
- 3.Lindfield D., Ansari G., Poole T. Nd:YAG laser treatment for epithelial ingrowth after laser refractive surgery. Ophthalmic Surg Laser Imag. 2012;43(3):247–249. doi: 10.3928/15428877-20120102-02. [DOI] [PubMed] [Google Scholar]
- 4.Perez-Santonja J.J., Ayala M.J., Sakla H.F., Ruíz-Moreno J.M., Alio J.L. Retreatment after laser in situ keratomileusis. Ophthalmology. 1999;106(1):21–28. doi: 10.1016/S0161-6420(99)90001-5. [DOI] [PubMed] [Google Scholar]
- 5.Wang M.Y., Maloney R.K. Epithelial ingrowth after laser in situ keratomileusis. Am J Ophthalmol. 2000;129(6):746–751. doi: 10.1016/s0002-9394(00)00357-3. [DOI] [PubMed] [Google Scholar]
- 6.Bragheeth M.A., Fares U., Dua H.S. Re-treatment after laser in situ keratomileusis for correction of myopia and myopic astigmatism. Br J Ophthalmol. 2008;92(11):1506–1510. doi: 10.1136/bjo.2008.143636. [DOI] [PubMed] [Google Scholar]
- 7.Chan C.C.K., Boxer Wachler B.S. Comparison of the effects of LASIK retreatment techniques on epithelial ingrowth rates. Ophthalmology. 2007;114(4):640–642. doi: 10.1016/j.ophtha.2006.06.062. [DOI] [PubMed] [Google Scholar]
- 8.Bromley J.G., Albright T.D., Kharod-Dholakia B., Kim J.K. Intraoperative and postoperative complications of laser in situ keratomileusis. Expert Rev Opthalmol. 2012;7(1):25–31. [Google Scholar]
- 9.Asano-Kato N., Toda I., Hori-Komai Y., Takano Y., Tsubota K. Epithelial ingrowth after laser in situ keratomileusis: clinical features and possible mechanisms. Am J Ophthalmol. 2002;134:801–807. doi: 10.1016/s0002-9394(02)01757-9. [DOI] [PubMed] [Google Scholar]
- 10.Caster A.I., Friess D.W., Schwendeman F.J. Incidence of epithelial ingrowth in primary and retreatment laser in situ keratomileusis. J Cataract Refract Surg. 2010;36(1):97–101. doi: 10.1016/j.jcrs.2009.07.039. [DOI] [PubMed] [Google Scholar]
- 11.Wang M.Y., Maloney R.K. Epithelial ingrowth after laser in situ keratomileusis. Am J Ophthalmol. 2000;129(6):746–751. doi: 10.1016/s0002-9394(00)00357-3. [DOI] [PubMed] [Google Scholar]
- 12.Karabela Y., Muftuoglu O., Gulkilik I.G., Kocabora M.S., Ozsutcu M. Intraoperative and early postoperative flap-related complications of laser in situ keratomileusis using two types of Moria microkeratomes. Int Ophthalmol. 2014;34(5):1107–1114. doi: 10.1007/s10792-014-9919-7. [DOI] [PubMed] [Google Scholar]
- 13.He L., Manche E.E. Fibrin glue for prevention of recurrent epithelial ingrowth under a LASIK flap with a central buttonhole defect. J Cataract Refract Surg. 2012;38:1857–1860. doi: 10.1016/j.jcrs.2012.08.031. [DOI] [PubMed] [Google Scholar]
- 14.Pérez-Santonja J.J., Bellot J., Claramonte P. Laser in situ keratomileusis to correct high myopia. J Cataract Refract Surg. 1997;23(3):372–385. doi: 10.1016/s0886-3350(97)80182-4. [DOI] [PubMed] [Google Scholar]
- 15.Azar D.T., Scally A., Hannush S.B., Soukiasian S., Terry M. Epithelial-defect masquerade syndrome after laser in situ keratomileusis; characteristic clinical findings and visual outcomes. J Cataract Refract Surg. 2003;29:2358–2365. doi: 10.1016/s0886-3350(03)00333-x. [DOI] [PubMed] [Google Scholar]
- 16.Stulting R.D., Carr J.D., Thompson K.P., Waring G.O., III, Wiley W.M., Walker J.G. Complications of laser in situ keratomileusis for the correction of myopia. Ophthalmology. 1999;106(1):13–20. doi: 10.1016/S0161-6420(99)90000-3. [DOI] [PubMed] [Google Scholar]
- 17.Fagerholm P., Molander N., Podskochy A., Sundelin S. Epithelial ingrowth after LASIK treatment with scraping and phototherapeutic keratectomy. Acta Ophthalmol Scand. 2004;82(6):707–713. doi: 10.1111/j.1600-0420.2004.00375.x. http://onlinelibrary.wiley.com/doi/10.1111/j.1600-0420.2004.00375.x/pdf Available at. [DOI] [PubMed] [Google Scholar]
- 18.Rojas M.C., Lumba J.D., Manche E.E. Treatment of epithelial ingrowth after laser in situ keratomileusis with mechanical debridement and flap suturing. Arch Ophthalmol. 2004;122(7):997–1001. doi: 10.1001/archopht.122.7.997. http://archopht.jamanetwork.com/data/Journals/OPHTH/9926/ECS30159.pdf Available at. [DOI] [PubMed] [Google Scholar]
- 19.Haw W., Manche E. Treatment of progressive or recurrent epithelial ingrowth with ethanol following laser in situ keratomileusis. J Refract Surg. 2001;17(1):63–68. doi: 10.3928/1081-597X-20010101-08. [DOI] [PubMed] [Google Scholar]
- 20.Yeh D.L., Bushley D.M., Kim T. Treatment of traumatic LASIK flap dislocation and epithelial ingrowth with fibrin glue. Am J Ophthalmol. 2006;141(5):960–962. doi: 10.1016/j.ajo.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Yeung A.M., Faraj L.A., McIntosh O.D., Dhillon V.K., Dua H.S. Fibrin glue inhibits migration of ocular surface epithelial cells. Eye. 2016;30(10):1389–1394. doi: 10.1038/eye.2016.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilde C., Messina M., Dua H. Management of recurrent epithelial ingrowth following laser in situ keratomileusis with mechanical debridement, alcohol, mitomycin-C, and fibrin glue. J Cataract Refract Surg. 2017;43(7):980–984. doi: 10.1016/j.jcrs.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Samimi D.B., Hamilton D.R. Recalcitrant epithelial ingrowth in patients with compromised eyelid function. J Refract Surg. 2008;24:544–546. doi: 10.3928/1081597X-20080501-14. [DOI] [PubMed] [Google Scholar]
- 24.Narváez J., Chakrabarty A., Chang K. Treatment of epithelial ingrowth after LASIK enhancement with a combined technique of mechanical debridement, flap suturing, and fibrin glue application. Cornea. 2006;25(9):1115–1117. doi: 10.1097/01.ico.0000240086.56522.69. [DOI] [PubMed] [Google Scholar]
- 25.Anderson N.J., Hardten D.R. Fibrin glue for the prevention of epithelial ingrowth after laser in situ keratomileusis. J Cataract Refract Surg. 2003;29(7):1425–1429. doi: 10.1016/s0886-3350(02)01989-2. [DOI] [PubMed] [Google Scholar]
- 26.Shaikh N.M., Wee C.E., Kaufman S.C. The safety and efficacy of photorefractive keratectomy after laser in situ keratomileusis. J Refract Surg. 2005;21(4):353–358. doi: 10.3928/1081-597X-20050701-09. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Scrolling images of Fig. 5. Hyperreflective areas with epithelial ingrowth can be seen in the corneal cross section around the 9 o'clock position. (Video credit to John VanDoorne).1