Abstract
Background
Miliary tuberculosis (TB) is a form of extrapulmonary tuberculosis due to hematogenous dissemination and occurs more frequently in immunocompromised patients. Clinical manifestations are non-specific and varied with the related organ, including central nervous system involvement. We report the first case of encephalitis associated with miliary TB in human immunodeficiency virus (HIV)-the infected patient.
Case presentation
A 39-year-old male presented with severe headache, numbness in the left side of the body, and partial seizure for two weeks. Previously, the patient complaining of several weeks of cough with generalized weakness. Physical examination showed progressive left-sided weakness and numbness. Chest radiograph showed uniform-sized small nodules randomly distributed diffusely throughout the lungs. Plain computer tomography (CT) brain imaging showed hypodensity in the right parietal region. Laboratory findings showed positive for the HIV antibody test, CD4 counts were 84 cells/μL and acid-fast bacilli from sputum. He was administered empirical anti-TB treatment and was discharged without any complications on day 10.
Conclusion
This is a rare cause of encephalitis due to miliary TB infection in HIV patients. Even though central nervous system involvement is rare in miliary TB infection, physicians should be aware of atypical features of the disease and comorbidity that may predispose this infection.
Keywords: Miliary tuberculosis, Encephalitis, Human immunodeficiency virus
1. Introduction
Tuberculosis (TB) is one of the commonest and important opportunistic infections in patients with human immunodeficiency virus (HIV) infection [1], [2]. The data showed as much as 13% of TB cases occurring among patients with HIV infection [3], [4]. From the total number of occurrence, data showed that 1% of the TB patients had central nervous system (CNS) involvement that related to a high mortality rate and permanent neurological sequelae [5], [6].
Encephalitis is one of the rarest CNS involvement of miliary tuberculosis, particularly in immunocompromised patients [7]. To this day, only a few references have reported the involvement of miliary tuberculosis in the CNS, even though the early treatment of CNS infection by TB can tremendously improve the patient condition [8]. Thus we reported a case of encephalitis as a result of miliary tuberculosis infection in a patient with HIV.
2. Case presentation
A 39-year-old male was referred to our hospital's neurology department because of severe headache and numbness in the left side of his body with a partial seizure that lasts 1–2 min for 3–4 times a day. The complaint started two weeks before hospital admission and progressively worsened. He had been healthy until two months before. Recently, the patient presents complaining of several weeks of cough with generalized weakness and poor oral intake. He was a non-smoker and denied using illicit drugs or another relevant medical history. He had no family history of TB and denied contact with a person with a TB infection.
On admission, he appeared well: bodyweight, 52 kg; height, 162 cm; temperature, 36.5 °C; blood pressure, 120/80 mmHg; pulse, 72 beats/min; respirations rate, 24/min; oxygen saturation, 98% while breathing ambient air. The neurology examination showed a hemisensory syndrome and 4/5 as the muscle strength score on the upper and lower extremity, respectively, in the left side of the body. All of the cranial nerve examination results were normal.
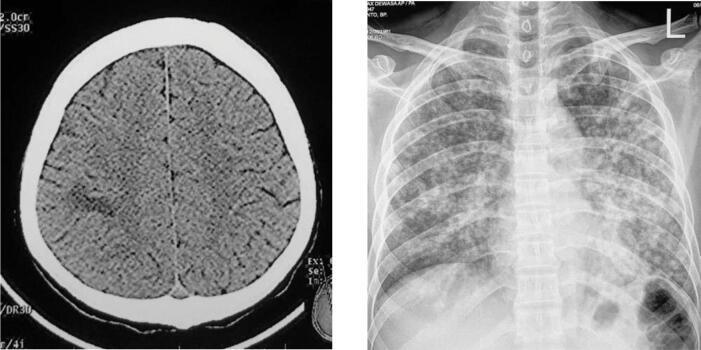
A computed tomography (CT) scan of the head showed a hypodense lesion in the right parietal lobe. Chest radiograph showed uniform-sized small nodules randomly distributed diffusely throughout the lungs (Fig. 1). Laboratory results found HIV antibody test was positive using ELISA (enzyme-linked immunosorbent assay), and acid-fast bacilli from sputum produced positive results. His CD4 count was 84 cells/μL. We, therefore, diagnosed the patient with miliary TB.
Fig. 1.
The CT Scan with hypodense lesion and the chest X-ray showed multiple uniform nodule in both lungs.
The patient was treated daily with three tablets of a fixed-dose combination of antituberculous treatment consisted of isoniazid (225 mg), rifampicin (450 mg), ethambutol (825 mg), and pyrazinamide (1200 mg), and also streptomycin injection 15 mg/kg. He also received intravenous dexamethasone 0.4 mg/kg per day and mannitol and then tapered-off. Valproic acid was also given for his focal seizure. The symptoms began to improve within three days after he received the anti-TB agents, and he was discharged without any complications on day 10. We postponed the ARV (antiretroviral) therapy within two weeks after starting the Anti-TB medication.
3. Discussion and conclusion
It is estimated that miliary TB presents for about less than 2% of total TB cases in immunocompetent patients such as HIV co-infection [7] There is a similar case about a miliary TB patient with headache and cognitive disturbance due to brain tuberculomas reported by Akriditis et al. [9] Another report from Portugal found persistent headache and sleep disturbance that associated with cerebral involvement of miliary TB [10].
The manifestations such as hemiparesis, numbness, focal seizure were atypical features of encephalitis that may have confounded early diagnosis. In the later stage of the disease, encephalitis may be associated with findings such as altered mental status, confusion, or severe headache [8]. In this patient, the CD4 counts less than normal. This immunocompetent state may precipitate the bacterial spread to other organs. The clinical presentation of miliary TB in early HIV infection (CD4 cell counts >200 cells/μL) is similar to that observed in immunocompetent individuals. With the progression of immunosuppression in late, advanced HIV infection (CD4 cell counts <200 cells/μL), disseminated and miliary TB are seen more often [11], [12], [13].
During the progression of the disease, M. tuberculosis may disseminate from the lungs to local lymph nodes and bloodstream, spread throughout the systemic circulatory system. The CNS is protected from the systemic circulatory system by the blood–brain barrier (BBB). However, there are several microorganism pathogens capable of passing the BBB and causing subsequent inflammation in brain parenchyma. The well-known theory is rich postulated, termed as “Rich foci,” develop around bacteria deposited in the brain layer and parenchyma during the initial bacteremic phase. Later on, the rupture of these foci led to the dissemination of the bacilli into the subarachnoid space and spread, causing diffuse or focal inflammation in the brain meninges or extensively to its parenchyma [14].
In conclusion, physicians should be aware of comorbidities, particularly infection by HIV is responsible for the etiology of this disease. Early recognition and management of this disorder are important to prevent patient worsening and jeopardize the outcome. Early treatment with antituberculosis therapy (ATT) has been proven to avoid unwanted complications in extrapulmonary miliary TB [7]. Therefore, the reporting of this patient is essential to highlight the atypical features of miliary brain tuberculosis and initiate appropriate care.
Ethical statement
This study requires no approval from the ethical committee due to the nature of this case report. However, this study has obtained permission from the Bethesda Hospital Research and Development Department. In accordance to Declaration of Helsinki, patient identity was hidden.
Acknowledgments
Acknowledgment
The authors declare no conflict of interest to disclose.
Authors contribution
RP involved in writing the initial manuscript, collection of the data, and supervision. VOW was involved in the preparation and editing of the manuscript. DP prepared the imaging report and editing of the manuscript.
Consent for Publication
Written informed consent was retrieved from the patient for publication of this case report.
References
- 1.Getahun H., Gunneberg C., Granich R., Nunn P. HIV infection–associated tuberculosis: the epidemiology and the response. Clin Infect Dis. 2010;50(s3):S201–S207. doi: 10.1086/651492. [DOI] [PubMed] [Google Scholar]
- 2.Phypers M., Harris T., Power C. CNS tuberculosis: a longitudinal analysis of epidemiological and clinical features. Int J Tuberc Lung Dis. 2006;10:99–103. [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Organization; Geneva: 2011. WHO report: global tuberculosis control. [Google Scholar]
- 4.WHO Global tuberculosis program. Switzerland: WHO Press; 2010.
- 5.Rock R.B., Olin M., Baker C.A., Molitor T.W., Peterson P.K. Central nervous system tuberculosis: pathogenesis and clinical aspects. Clin Microbiol Rev. 2008;21(2):243–261. doi: 10.1128/CMR.00042-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma S.K., Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004;120:316–353. [PubMed] [Google Scholar]
- 7.Ray S, Talukdar A, Kundu S, Khanra D, Sonthalia N. Diagnosis and management of miliary tuberculosis: current state and future perspectives [retracted in Ther Clin Risk Manag. 2015 Sep 28;11:1457]. Ther Clin Risk Manag. 2013;9:9‐26. doi:10.2147/TCRM.S29179. [DOI] [PMC free article] [PubMed] [Retracted]
- 8.Christie L.J., Loeffler A.M., Honarmand S., Flood J.M., Baxter R., Jacobson S., Alexander R., Glaser C.A. Diagnostic challenges of central nervous system tuberculosis. Emerging Infectious Diseases. 2008;14(9):1473–1475. doi: 10.3201/eid1409.070264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akritidis N., Galiatsou E., Kakadellis J., Dimas K., Paparounas K. Brain tuberculomas due to miliary tuberculosis. South Med J. 2005;98(1):111–113. doi: 10.1097/01.SMJ.0000149409.38256.14. [DOI] [PubMed] [Google Scholar]
- 10.Goncalves R., Lopes P., Mendes P., Trepa J., Rua J., Sa R. Miliary tuberculosis with cerebral, liver, prostate, and retro esophageal involvement. ID Cases. 2017;9:25–27. doi: 10.1016/j.idcr.2017.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee M.P., Chan J.W., Ng K.K., Li P.C. Clinical manifestations of tuberculosis in HIV‐infected patients. Respirology. 2000;5(4):423–426. doi: 10.1111/j.1440-1843.2000.00287.x. [DOI] [PubMed] [Google Scholar]
- 12.Vinyard C., Macgregor R.R. Tuberculous meningitis in HIV-infected individuals. Curr HIV/AIDS Rep. 2009;6(3):139–145. doi: 10.1007/s11904-009-0019-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shao C., Qu J., He L. A comparative study of clinical manifestations caused by tuberculosis in immunocompromised and non-immunocompromised patients. Chin Med J. 2003;116:1717–1722. [PubMed] [Google Scholar]
- 14.Be N.A., Kim K.S., Bishai W.R., Jain S.K. Pathogenesis of central nervous system tuberculosis. Curr Mol Med. 2009;9(2):94–99. doi: 10.2174/156652409787581655. [DOI] [PMC free article] [PubMed] [Google Scholar]