Abstract
Background/Aim: Postoperative complications have a tremendous impact on in-hospital costs. The novel Comprehensive Complication Index® (CCI®) summarizes all complications together and is more sensitive than existing morbidity endpoints. The purpose of this study was to assess the correlation of CCI® with in-hospital costs and externally validate a novel cost prediction calculator. Patients and Methods: This was a prospective study including consecutive patients undergoing elective major hepatopancreaticobiliary (HPB) surgery for malignancy at a London tertiary referral hospital. A priori sample size and post-hoc power calculations were performed. Results: Thirty patients were included in the analysis, 14 were female, and the median age was 67 [interquartile range (IQR)=54-74] years. The median Charlson Comorbidity Index was 6 (IQR=5-8). Eighteen patients underwent liver, 9 pancreatic surgery and three a palliative bypass; 11 patients had a major complication (≥grade 3a) according to the Clavien–Dindo classification. The median CCI® was 30.2 (IQR=12.18-39.5). The mean cost per case was 13,908 (SD=4,600) GBP. There was no correlation between the Charlson Comorbidity Index or age with actual cost. However, there was very good correlation of actual cost with the CCI® (r=0.77, 95% confidence interval=0.57-0.89, p<0.001) as well as with the predicted cost (Clavien Cost Prediction Calculator) (r=0.70, 95% confidence interval=0.44-0.85, p<0.001). Conclusion: These findings support the hypothesis that complications are the most important predictor of overall cost in the setting of elective major HPB surgery for malignancy. Furthermore, CCI® and the novel Cost Prediction Calculator can be used in this setting to accurately predict costs using no additional resources.
Keywords: Liver, pancreas, surgery, complications, cost
Over the coming decades, health spending in the UK National Health Service (NHS) is forecast to rise significantly as a proportion of gross domestic product, partly as a result of increasing demand and also due to the increased complexity of treatments (1). In line with this overall trend, demand for and complexity of major elective hepatopancreaticobiliary (HPB) surgery is increasing. Outcomes following major elective HPB surgery have improved significantly following centralisation of services but complication rates remain high compared with other types of surgery and have a massive impact on in-hospital costs worldwide (2). In 2001, Vonlanthen et al. demonstrated that complications were the strongest indicator of in-hospital cost and that complications following pancreatic surgery were significantly more costly than equivalent complications in other specialities (3). Thus, complications in major elective HPB surgery represent a disproportionate financial burden when compared to other specialities. In the context of the finite resources of the NHS, new approaches to cost containment in major elective HPB surgery are therefore required.
Thus far, approaches to such cost containment have been hampered by a dearth of data and significant heterogeneity in how complications following major elective HPB surgery are measured and costed (4). Although HPB has greater consistency in measuring and reporting complications than other specialities, several issues remain (4). The Clavien–Dindo classification (CDC) is the most widely used grading system for reporting postoperative complications (5). The CDC grades complications according to how they are treated, selecting only the most severe complication and omitting numerous complications of lesser severity. To overcome this limitation, Slankamenac et al. developed the novel Comprehensive Complication Index® (CCI®), which is based upon the CDC but summarizes all postoperative complications, yielding a metric value between 0-100 (6). To date the CCI® has been shown to be a sensitive indicator of morbidity following surgery for gastric cancer (7) and major hepatectomy for biliary cancer (8) amongst others. The Clavien Group in Zurich developed the CCI® further with the addition of a novel Cost Prediction Calculator. This calculator requires only three variables, Age, CCI® and type of surgery, to estimate the total in-hospital cost. Both the CCI® and Cost Prediction Calculator are welcome developments which could form the basis for much needed cost calculation and containment initiatives but still require validation in specific clinical settings.
The purpose of this prospective study was to assess the correlation of the CCI® with in-hospital costs, establish the cost per unit of CCI®, externally validate the Clavien Cost Prediction Calculator and assess the economic burden they represent in patients undergoing elective major HPB surgery for malignancy at a London tertiary referral hospital.
Patients and Methods
Study design. This was a prospective, observational, longitudinal, cohort cost-analysis study. This study received approval by the local Audit Committee of the Royal Free Hospital (08-01-2018/RF13) and all patients provided written signed consent for participation. The protocol was published prior to the conduction of the study at CoCoS.surgery.
This study was considered as a health economics and clinical audit by the Audit Committee and the Caldicott Guardian for data management of the Royal Free Hospital, NHS Foundation Trust and the need for a formal RIB ethics approval was waived. Being a prospective audit, the Audit Committee of our institution did request a formal patient information sheet and consent form to be obtained by each participating patient. The CoCoS.surgery Patient Information Sheet is available for download at: https://cocos-surgery.com/sites/default/files/CoCos_Patient_Information_v1.1.pdf. The CoCoS.surgery Patient Consent Form is available for download at: https://cocos-surgery.com/sites/default/files/CoCos_consent_form_v1.1.pdf
Setting. The study took place at the Royal Free Hospital in London, UK. The recruitment start date was 1st February 2018 until 18th of March 2018. The data collection team consisted of three doctors (TH, TO, DD). Complete data collection was finalized on the 18th of June 2018 after all patients were discharged from the hospital. Data collection was conducted through a secure platform that uses an electronic Case Report Form through a specially designed Data Entry Management System to meet international standards for electronic databases including fully anonymized data, as previously described (9). This article adheres to the Standard Protocol Items: Recommendations for Interventional Trials guidelines.
Participants. The study population consisted of consecutive adult patients with malignant lesions undergoing major elective HPB open as well as laparoscopic surgery. Patients under the age of 18 years, or those undergoing surgery other than major elective HPB were not considered eligible for participation in this study.
Variables and data sources. To establish the dataset required for the study, several sources were examined. All studies included in a recent systematic review examining the economic burden of complications following major surgical procedures for both liver and pancreatic resections were reviewed and their datasets amalgamated (3). Both the CCI® and CDC of surgical complications were consulted for scope of data collection on complications. The Charlson co-morbidity index is a widely used measure of co-morbidity and was therefore also included in the data collection (10). Basic demographics, preoperative, intraoperative and postoperative characteristics were included as listed in Tables I to III. The Finance Department of the Royal Free Hospital provided the exact in-hospital cost data related to each patient. Additionally, the Clavien cost calculator was used to obtain the predicted cost for each patient converting euros (EUR) to British pounds (GBP) with a factor of 0.88, the conversion spot rate on the 25th of May 2018. The investigators received permission to use the Clavien Cost Prediction Calculator available at www.assessurgery.com/cost-prediction during personal communication.
Bias. Selection bias was avoided by including all consecutive cases who met the pre-specified inclusion and exclusion criteria. No patients were lost to follow-up and there were no missing data. Data extraction was independently performed by three investigators, always in pairs. The investigators did not identify any confounding factors whilst measuring and associating complications with costs. Information bias, including measurement bias was minimized by the fact that the electronic Case Report Form within the specially designed Data Entry Management System included predefined datasets with obligatory options and was designed to identify inaccuracies.
Study size. In the pilot phase of this study, a sample size calculation using the standard bivariate model, with a two-sided alpha of 0.05 and power of 0.80, was conducted after having included 30 cases to estimate the correlation coefficient of the CCI® with the total in-hospital costs. The sample size calculation indicated that at least 10 cases should be analysed to ensure statistically significant correlation of r=0.77 between the CCI® and cost. An additional sample size calculation was conducted using the lower 95% confidence interval of the aforementioned (r=0.54) correlation and showed that at least 23 patients had to be included to ensure statistical significance.
Quantitative variables. All quantitative variables were included in the analysis without any grouping, with the exception of the Clavien Cost Prediction Calculator that groups patient ages into three groups. As a separate analysis, the CCI® was grouped into 10-point groups to assess the cost increase.
Statistical methods. Data are reported as mean (±SD), median (interquartile range, IQR) and frequencies, where appropriate. The Pearson correlation coefficient (r2) was used to assess the correlation of continuous variables. As a high correlation does not necessarily imply that there is good agreement between two methods, the Bland–Altman test was used to assess agreement between continuous variables. All p-values were two-sided and considered statistically significant when 0.05 or less. For better interpretation of the different correlation results, an arbitrary scale was used with a value of >0.80 representing excellent, 0.61-0.80 very good, 0.41-0.60 good, 0.21-0.40 moderate, and 0.01-0.20 poor correlation. Statistical analysis was performed using R version 3.3.2 (R Core Team, GNU GPL v2 License), R Studio version 1.0.44 (RStudio, Inc. GNU Affero General Public License v3, Boston, MA, 2016) with the graphical user interface rBiostatistics.com alpha version (rBiostatistics.com, London, UK, 2017). The analysis was performed on an intension to treat basis. There were no missing data in this study and no patients were lost to follow-up. There was no sensitivity analysis required for this study.
Results
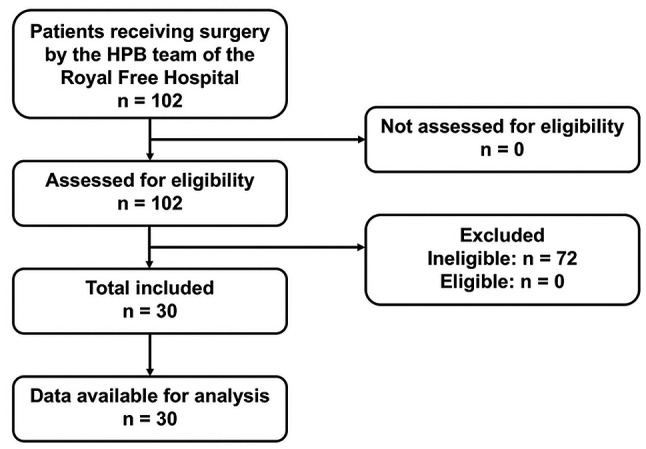
Participants. Within the study period, a total of 102 patients underwent surgery by the HPB team of the Royal Free Hospital in London, UK. All patients were assessed for eligibility by the study investigators. Of those patients, 72 were excluded as they did not meet the inclusion criteria (underwent minor surgery or a type other than pancreatic or hepato-biliary). Finally, a total of 30 consecutive patients were included in this study after the completion of the pilot study (Figure 1). A sample size calculation indicated no need for additional patient recruitment.
Figure 1. Flow diagram of the patient inclusion process. HPB: Hepatopancreaticobiliary surgery.
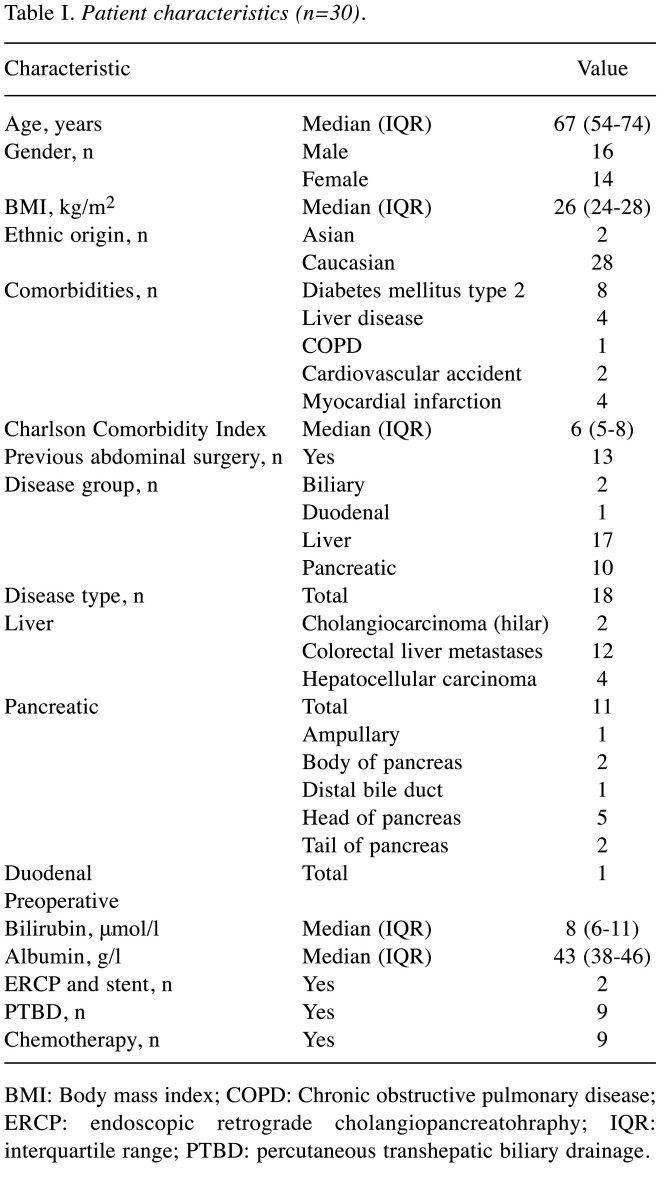
Patient characteristics. Of the 30 patients included in the analysis, 14 were female and the median age was 67 (IQR=54-74) years. The median Charlson Comorbidity Index score was 6 (IQR=5-8) (maximum possible 33 points) (Figure 2A). Two patients had biliary, one duodenal, 17 liver and 10 pancreatic disease. The detailed patient characteristics are listed in Table I.
Figure 2. Distribution of the Charlson Comorbidity Index (A), Comprehensive Complication Index® (CCI®) (B) and actual cost (British pounds, GBP) of the surgical healthcare (C) of the 30 study patients.
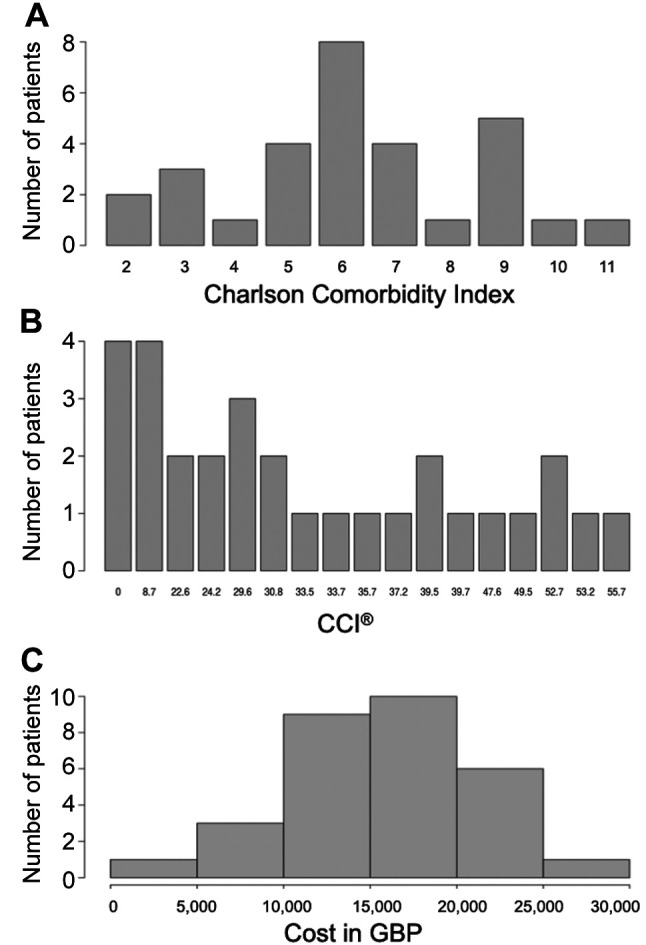
Table I. Patient characteristics (n=30).
BMI: Body mass index; COPD: Chronic obstructive pulmonary disease; ERCP: endoscopic retrograde cholangiopancreatohraphy; IQR: interquartile range; PTBD: percutaneous transhepatic biliary drainage.
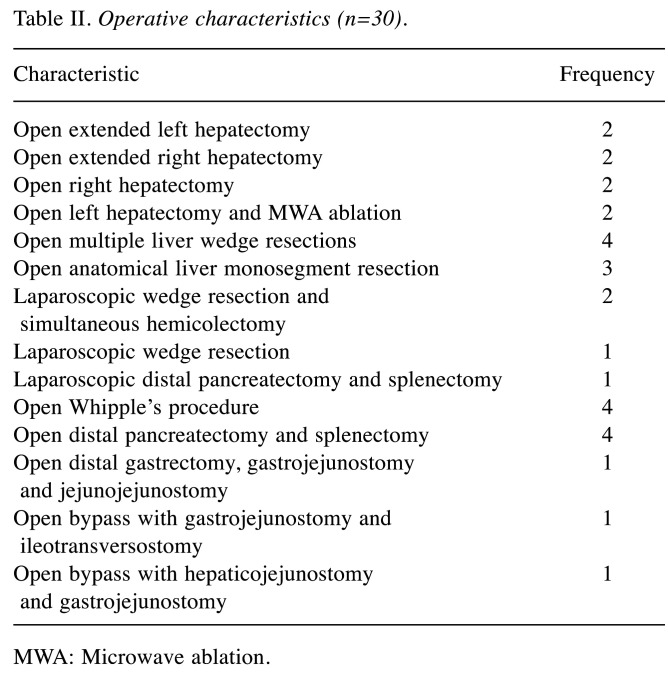
Operation characteristics. Out of the 30 patients, 16 underwent liver surgery, 11 pancreatic surgery and three a palliative bypass. The median duration of operation was 375 (IQR=320-420) minutes. All patients received preoperative prophylactic antibiotics and all 11 pancreatic cases received intraoperative somatostatin analogues. The operation characteristics are listed in Table II.
Table II. Operative characteristics (n=30).
MWA: Microwave ablation.
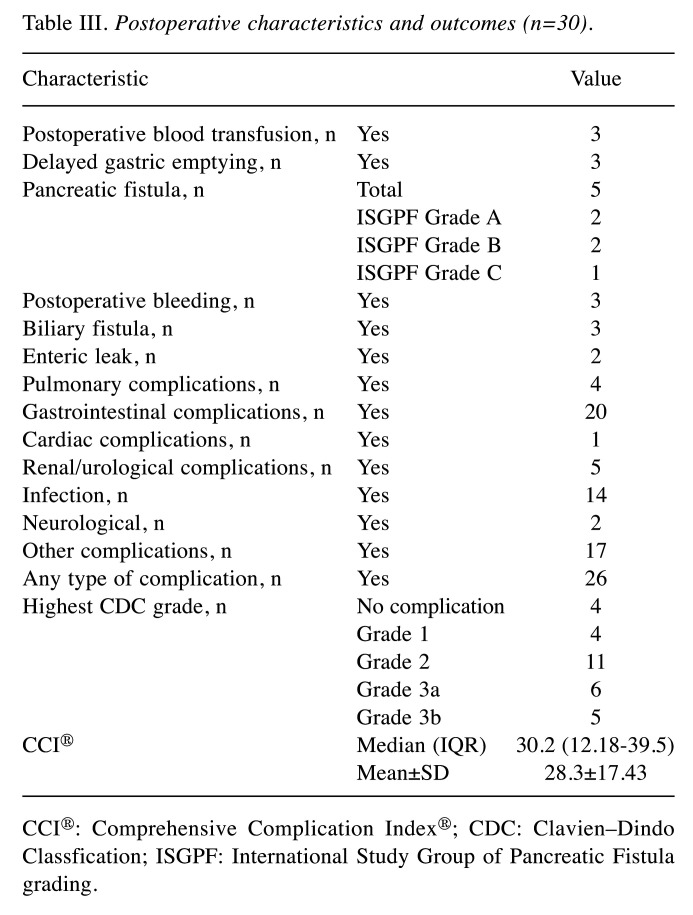
Postoperative characteristics and outcomes. Only four patients did not experience any postoperative complications, while 11 patients had a major complication (≥grade 3a) according to the CDC, of whom five underwent an emergency re-operation. Of the 11 patients that underwent pancreatic resection, five developed a pancreatic fistula (two grade B and one grade C based on the International Study Group of Pancreatic Fistula). The most frequent complications were gastrointestinal (n=20, including postoperative ileus) followed by infections (n=14, including wound, chest and intra-abdominal infections). The median postoperative length of Intensive Therapy Unit stay was 2 (IQR=1-3) days and hospital stay 11 (IQR=6-17) days (Figure 2B). The median CCI® was 30.2 (IQR=12.18-39.5). All postoperative outcomes are listed in Table III.
Table III. Postoperative characteristics and outcomes (n=30).
CCI®: Comprehensive Complication Index®; CDC: Clavien–Dindo Classfication; ISGPF: International Study Group of Pancreatic Fistula grading.
Cost analysis. The 30 cases included in this study cost a total of 481,179 GBP, corresponding to 531,074 EUR (620,348 USD or 607,715 CHF). The lowest cost was 4,932 and the highest 26,734 GBP. The mean cost per case was 13,908±4,600 GBP) and the median 13,210 (IQR=12,319-19,837) GBP. Figure 2C illustrates the distribution of cost.
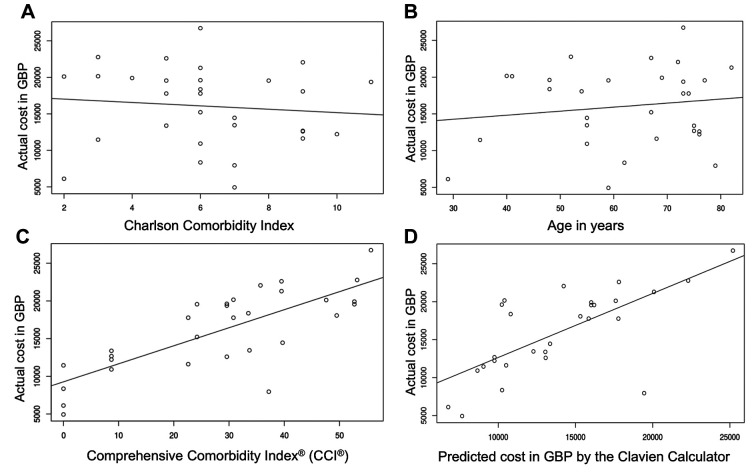
There was no correlation between the Charlson Comorbidity Index and the actual cost, with a Pearson correlation coefficient (PCC) r of −0.10 [95% confidence interval (CI)=−0.44-0.27; p=0.599] (Figure 3A). There was a weak but not significant (p=0.447) correlation between the patient age and actual cost, with PCC r of 0.14 (95% CI=−0.22-0.48) (Figure 3B). However, there was a very good correlation between the CCI® and the actual cost with PCC r of 0.77 (95% CI=0.57-0.89) (p<0.001) (Figure 3C).
Figure 3. Correlation of the actual cost (in British pounds, GBP) with the Charlson Comorbidity Index (A), patient age (B), Comprehensive Complication Index® (CCI®) (C) and cost predicted by the Clavien Cost Prediction Calculator (D).
In order to externally validate the Clavien cost prediction calculator, the calculator-predicted costs were correlated with actual costs provided by the Finance Department of our Institution. We found a very good correlation between predicted and actual cost with PCC r of 0.70 (95% CI=0.44-0.85) (p<0.001) (Figure 3D). The actual cost in GBP for each 10 units of the CCI® is illustrated in Figure 4A.
Figure 4. A: Actual cost in GBP for each 10 units of Comprehensive Complication Index® (CCI®). B: Bland–Altman plot of the agreement between the actual cost and cost predicted by the Clavien Cost Prediction Calculator (in British pounds, GBP). Overall underestimation of the cost by the Clavien Cost Prediction Calculator by only −2,041 GBP (95% CI. Level of Agreement=5,981 to -9,974 GBP).
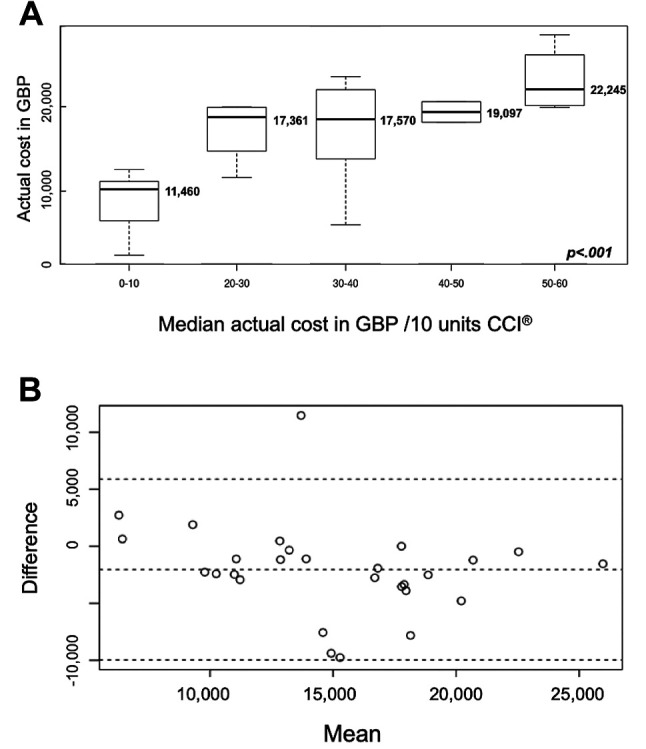
The agreement, as measured by the Bland–Altman analysis, between the predicted by the Clavien Calculator and the actual cost provided by the Finance Department of our Institution is illustrated in Figure 4B. The overall bias was only −2,041 (95% CI=−472 - −3.611) GBP, indicating minimal underestimation of the actual cost.
Discussion
The main finding of this study is that only the CCI® showed signification correlation with hospital costs in the setting of elective major HPB surgery, whereas age and Charlson co-morbidity index alone did not. These findings support the hypothesis that complications are the most important predictor of overall cost and should therefore be the main focus of efforts to contain escalating healthcare costs.
Contrary to our results, Vonlanthen et al. found that a Charlson Comorbidity Index of 3 or higher contributed significantly to greater costs (2). The study population in that instance included a wide spectrum of surgical specialties with a median Charlson Comorbidity Index of 2 (IQR=0-13) whereas the present study was limited to major HPB surgery with patients who had a much higher median Charlson Comorbidity Index of 6 (IQR=5-8). This difference in median Charlson Comorbidity Index may account for the loss of cost predicting ability of the index. In addition, age was not found to be a significant predictor of costs and this might be explained by a rigorous pre-operative assessment process undertaken at our Institution prior to performance of major elective HPB surgery. It is conceivable that a higher level of fitness is required from elderly patients than from younger patients undergoing an equivalent HPB surgical procedure to compensate for a perceived age-related reduction of physiological reserve, neutralizing any effect age might have on cost. This finding is also reported in a multivariate analysis by Vonlanthen et al. which found age per se was not a significant predictor of costs (2). Further research is required to determine exactly to what extent age as an independent factor relates to cost.
Apart from optimal preoperative patient selection and optimization, another approach towards reducing both the quantity and severity of complications is to prospectively audit institution-specific data on complications and their costs. One of the important findings of this study is the validation of the CCI® and the related Cost Prediction Calculator as a means to achieve this. Here we present a detailed analysis of the cost break-down for 30 consecutive patients. In practice, it is not feasible to expect already stretched finance departments to divert resources to provide such comprehensive cost analysis for all patients in real time. NHS-based finance departments and surgical departments rarely share such detailed information on a case-by-case basis.
The Cost Prediction Calculator (www.assessurgery.com/cost-prediction) is an online tool, which aims to provide such real-time estimates of the costs of surgery and associated complications to clinicians so they may measure and manage finances more appropriately. The online calculator requires just three, readily available parameters: Age, CCI® and type of surgery. In this study, we tested the Cost Prediction Calculator against the formal cost calculation from the Finance Department at our Institution and found a very good correlation. The Cost Prediction Calculator has the potential to allow hospitals providing major HPB services to easily identify discrepancies between costs incurred and reimbursement. Greater transparency in this respect may facilitate improved and more sustainable reimbursement models. Furthermore, a simple and not time-consuming prediction of cost may be included in morbidity and mortality meetings in order to add the cost dimension to postoperative surgical complications.
This study has demonstrated that it is possible to accurately predict the costs of major elective HPB surgery in real time, without diversion of vast resources. The use of both the CCI® and Cost Prediction Calculator are generalizable to other major HPB tertiary centres in the UK. Indeed, the comparison of CCI® and predicted costs between HPB centres in the UK offers a unique opportunity to raise awareness and better understand the economic burden on the NHS from HPB complications.
This study’s strengths are its prospective nature and completeness of data collection, which reduce bias to a minimum. The strong correlation between the CCI® and total in-hospital costs allowed significance to be reached with only 10 patients, as also confirmed by a post-hoc power calculation: The 30 patients in this study were more than enough for this purpose but did not allow further sub-group analysis to be performed. The limitations of the study are the absence of long-term follow-up after discharge. The Authors appreciate that vast costs are incurred by complications after discharge from the index admission. The measurement and calculation of these costs, however, are extremely challenging and beyond the scope of this study.
Overall, these findings support the hypothesis that complications are the most important predictor of overall cost in the setting of elective major HPB surgery. Furthermore, CCI® and the novel Cost Prediction Calculator can be used in this setting to accurately predict costs using no additional resources. It is anticipated that HPB centres would be able to use the data generated from their department as a baseline from which to benchmark future cost savings. A national prospective registry for major elective HPB using the CCI® and the novel Cost Prediction Calculator would be a feasible and valuable project.
Conflicts of Interest
The Authors declare that they have no competing interests.
Authors’ Contributions
The authorship of this article was established according to the “Authorships.org Software for Objective Qualification and Order of Academic Authorship in Medical and Science Journals” (Authorships.org, Zurich, Switzerland, 2016)(11).
Conception and design: DAR, TH, KF; Acquisition of data: TH, TO, DD; Analysis and interpretation: DAR, TH, NM. Drafting the article: DAR, TH, NM, TO. Revision of the article: DAR, NM, KF. Final approval for submission: All Authors.
Acknowledgements
The Authors express special thanks to Ms. Laura Fenlon for providing the cost data generated by the Finance Department of the Royal Free London NHS Foundation Trust. The CoCoS.surgery data collection management system was supported by the Fiorina Royal Free Charity https://www.royalfreecharity.org/charities/fiorina. The Fiorina Royal Free Charity Members had no influence on the design, the analysis or interpretation of the results of this study.
References
- 1.Fiscal sustainability report 2017. Office for Budget Responsibility. Available at: http://cdn.obr.uk/FSR_Jan17.pdf.
- 2.Shah R, Diaz A, Tripepi M, Bagante F, Tsilimigras DI, Machairas N, Sigala F, Moris D, Barreto SG, Pawlik TM. Quality versus costs related to gastrointestinal surgery: Disentangling the value proposition. J Gastrointest Surg. 2020;24:2874–2883. doi: 10.1007/s11605-020-04748-7. [DOI] [PubMed] [Google Scholar]
- 3.Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Muller MK, Hahnloser D, Hauri D, Graf R, Clavien PA. The impact of complications on costs of major surgical procedures: A cost-analysis of 1200 patients. Ann Surg. 2011;254:907–913. doi: 10.1097/SLA.0b013e31821d4a43. [DOI] [PubMed] [Google Scholar]
- 4.Patel AS, Bergman A, Moore BW, Haglund U. The economic burden of complications occurring in major surgical procedures: A systematic review. Appl Health Econ Health Policy. 2013;11:577–592. doi: 10.1007/s40258-013-0060-y. [DOI] [PubMed] [Google Scholar]
- 5.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 6.Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The Comprehensive Complication Index: A novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258:1–7. doi: 10.1097/SLA.0b013e318296c732. [DOI] [PubMed] [Google Scholar]
- 7.Kim TH, Suh YS, Huh YJ, Son YG, Park JH, Yang JY, Kong SH, Ahn HS, Lee HJ, Slankamenac K, Clavien PA, Yang HK. The Comprehensive Complication Index (CCI) is a more sensitive complication index than the conventional Clavien-Dindo classification in radical gastric cancer surgery. Gastric Cancer. 2018;21:171–181. doi: 10.1007/s10120-017-0728-3. [DOI] [PubMed] [Google Scholar]
- 8.Nakanishi Y, Tsuchikawa T, Okamura K, Nakamura T, Tamoto E, Noji T, Asano T, Amano T, Shichinohe T, Hirano S. Risk factors for a high Comprehensive Complication Index score after major hepatectomy for biliary cancer: A study of 229 patients at a single institution. HPB. 2016;18:735–741. doi: 10.1016/j.hpb.2016.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raptis DA, Mettler T, Fischer MA, Patak M, Lesurtel M, Eshmuminov D, de Rougemont O, Graf R, Clavien PA, Breitenstein S. Managing multicentre clinical trials with open source. Inform Health Soc Care. 2014;39:67–80. doi: 10.3109/17538157.2013.812647. [DOI] [PubMed] [Google Scholar]
- 10.Chang CM, Yin WY, Wei CK, Wu CC, Su YC, Yu CH, Lee CC. Adjusted age-adjusted Charlson Comorbidity Index score as a risk measure of perioperative mortality before cancer surgery. PLoS One. 2016;11:e0148076. doi: 10.1371/journal.pone.0148076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raptis D, Raptis A. Authorships.org. Available at: http://authorships.org.