Abstract
Background/Aim: This study aimed to assess the association of the modified albumin-bilirubin (mALBI) grade with the endoscopic findings of gastroesophageal varices (GEVs). Patients and Methods: A total of 141 patients with histologically proven cirrhosis who underwent a liver biopsy and esophagogastroduodenoscopy were enrolled. The relationships between the mALBI grade and endoscopic findings were evaluated. Results: The incidence of GEVs and high-risk GEVs differed among mALBI grades. Patients with mALBI grades of 2b-3 had higher rates of GEVs and high-risk GEVs in comparison to those with mALBI grades of 1-2a (p<0.0001). In addition, patients with mALBI grade 2b or grade 3, but not those with mALBI grade 2a, had significantly higher rates of complicated GEVs and high-risk GEVs in comparison to those with mALBI grade 1. Conclusion: The mALBI grade may be useful in predicting the presence of GEVs and for stratifying their bleeding risk.
Keywords: Liver cirrhosis, gastroesophageal varices, ALBI score
Gastroesophageal varices (GEVs) are an important complication in patients with liver cirrhosis (1-3). Esophagogastroduodenoscopy (EGD) is the most reliable method for evaluating GEVs; however, from the viewpoint of the burden on patients, a non-invasive method for predicting the presence of varices, particularly those with a risk of hemorrhage, is desired (4,5). Currently, a combination of liver stiffness data with transient elastography (Fibroscan®) and the platelet count is widely used as the established criteria (Baveno VI criteria) to determine the indication for EGD (6). However, the institutions that are able to perform transient elastography are limited; thus, the evaluation of varices based on blood test parameters is still clinically relevant. In particular, an accurate method of evaluation based on daily clinical data would be ideal.
The albumin-bilirubin (ALBI) grade is a newly reported classification that can be used to classify the liver reserve function into three grades (ALBI grades 1-3: i.e. from better to poorer function) using two commonly measured variables: The serum values of albumin and total bilirubin (7). However, ALBI grade 2 includes a wide-range of patients in whom the liver function is relatively heterogeneous, and a scoring system that combines the ALBI grade and platelet count (ALBI-PLT score) was reported to be useful for predicting the presence of high-risk GEVs in patients with hepatocellular carcinoma and compensated cirrhosis (8).
In order to alleviate the heterogeneity of patients with ALBI grade 2, a modified classification that divides ALBI grade 2 into two categories (a and b) was recently proposed as the ‘modified ALBI grade’ (mALBI grade) (9). However, the relationship between mALBI grade and the endoscopic findings of GEVs has not been clarified. In the present study, we assessed the mALBI grade, and evaluated their association with the endoscopic findings of GEVs.
Patients and Methods
We retrospectively studied a total of 141 patients who underwent a percutaneous liver biopsy at our Institution from October 2008 to December 2015 and who were pathologically confirmed to have liver cirrhosis. The etiologies of liver cirrhosis were determined and classified as described previously (10). Liver biopsy studies were conducted using standard techniques (11,12). All blood data were obtained on the same day as the liver biopsies. The albumin level, total bilirubin level, and platelet count were measured in routine blood tests. The ALBI score (7), ALBI grade (7), ALBI-PLT score (8) and mALBI grade (9) were determined as follows:
ALBI score: [log10 bilirubin (μmol/l)×0.66]−[albumin (g/l)×0.085]
ALBI grade by ALBI score: Grade 1: ≤−2.60; 2: >−2.60 to −1.39; 3: >−1.39
ALBI-PLT score: Sum of points for ALBI grade (1-3 points) and platelet count (1 point: >150×103/mm3; 2 points: ≤150×103/mm3). ALBI-PLT score ranged from 2 to 5.
mALBI grade: Grade 1: ≤−2.60; 2a: >−2.60 to <−2.27; 2b: ≥−2.27 to −1.39; 3: >−1.39
GEVs were evaluated by EGD according to the current Japanese guidelines for the management of liver cirrhosis, as previously described (3,13). Endoscopically detected GEVs were classified into three grades (F1, F2, or F3), and the presence of red signs on the varices was also investigated. Patients with F2 varices with red signs, and those with F3 varices were considered to have high-risk varices (13). Evaluation by EGD was conducted within 6 months of the liver biopsy. Patients who had previously received endoscopic treatment for varices were considered to have varices with a high-risk of bleeding.
Patients who had undergone splenectomy or partial splenic arterial embolization were excluded from the study, as such methods influenced the ALBI-PLT score. The study conformed to the ethical guidelines of the Helsinki declaration. The current study was approved by the Ethics Committee of the Institutional Review Board (No. 3431).
Statistical analysis. Frequencies were compared among the groups by the chi-squared test. Odds ratios between groups were determined with a logistic regression model (14). p-Values of less than 0.05 were considered to indicate statistical significance.
Results
Basic characteristics of patients with cirrhosis. A total of 141 patients with cirrhosis who were diagnosed by liver biopsy were enrolled; their basic characteristics are shown in Table I. The median age of the patients was 63 years. The study population included 73 men and 68 women. The distribution of the ALBI-PLT scores was as follows: score 2 in 10, 3 in 31, 4 in 95, and 5 in five. The distribution of the ALBI grades was as follows: Grade 1 in 25, grade 2 in 109, and grade 3 in seven. The 109 patients classified as grade 2 were further subdivided by the mALBI grade system into grade 2a in 40 and grade 2b in 69 (Table I).
Table I. Characteristics of the enrolled patients with liver cirrhosis (N=141).
AIH: Autoimmune hepatitis; ALBI: albumin-bilirubin; ALBI-PLT: ALBI-platelet; ALD: alcoholic-related liver disease; ALP: alkaline phosphatase; ALT: alanine aminotransferase; AST: aspartate aminotransferase; γ-GTP: γ-glutamyl transpeptidase; HBV: hepatitis B virus; HCV: hepatitis C virus; IQR: interquartile range mALBI: modified ALBI; NASH: nonalcoholic steatohepatitis; PBC: primary biliary cholangitis.
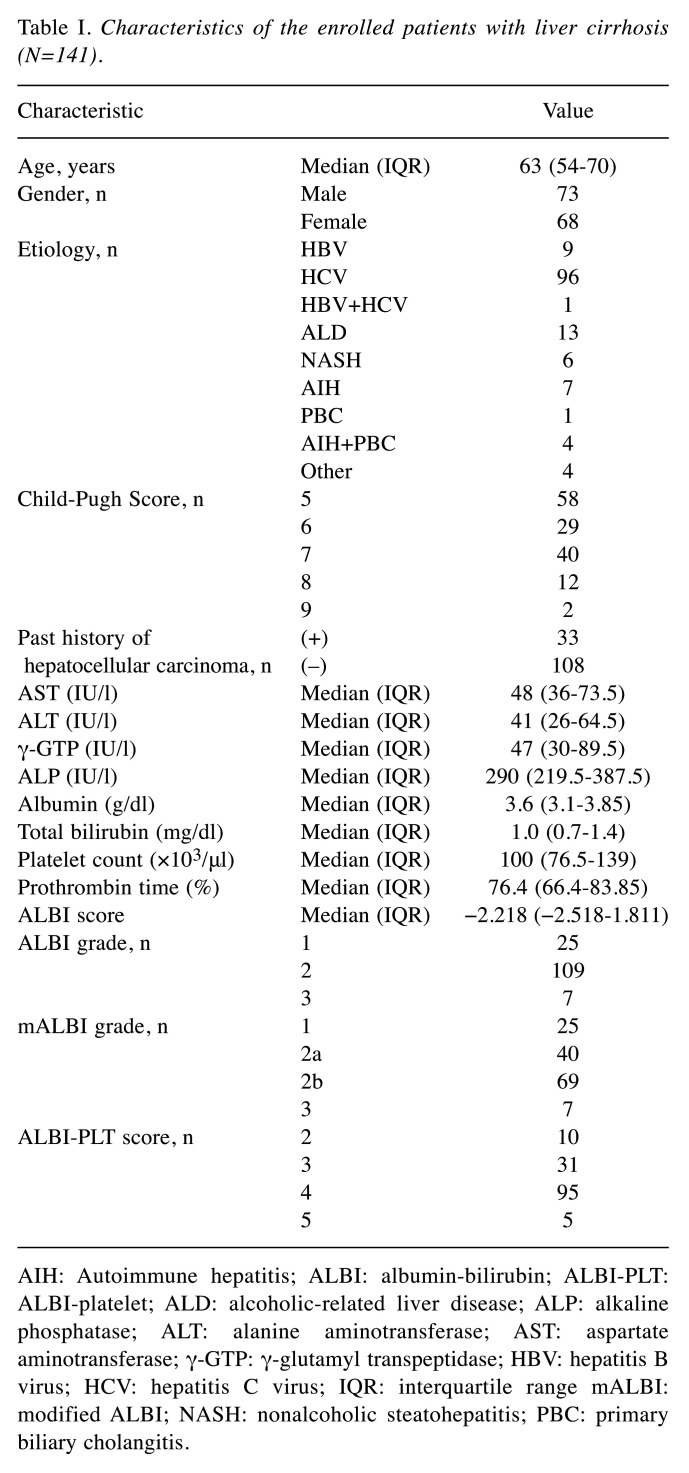
Association of the ALBI-PLT score with the endoscopic findings of GEVs. The incidence of GEVs increased as the ALBI-PLT score increased (overall: p<0.01) (Figure 1A). The incidence of high-risk varices also increased as the score increased, and among the patients with ALBI-PLT score 2, only one patient had high-risk varices; however, the differences among the groups (score 2-5) did not reach statistical significance (overall: p=0.222) (Figure 1B).
Figure 1. Association of the albumin-bilirubin (ALBI)-platelet (PLT) score with the endoscopic findings of gastroesophageal varices (GEVs). A: The incidence of GEVs increased as the score increased (overall: p<0.01). B: The incidence of high-risk varices also increased as the score increased; however, the differences among the groups (score 2-5) did not reach statistical significance (overall: p=0.222).
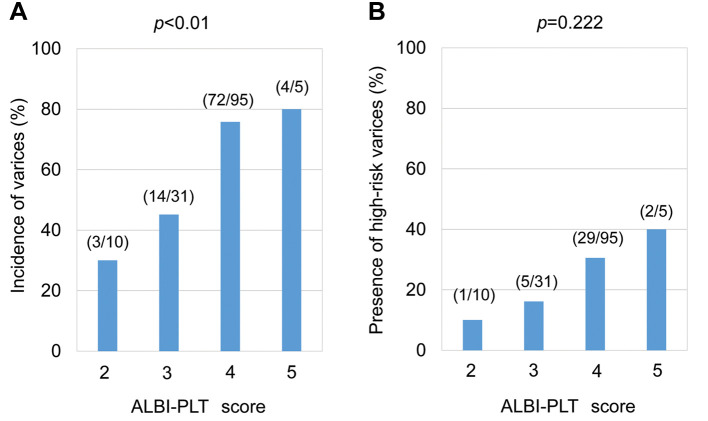
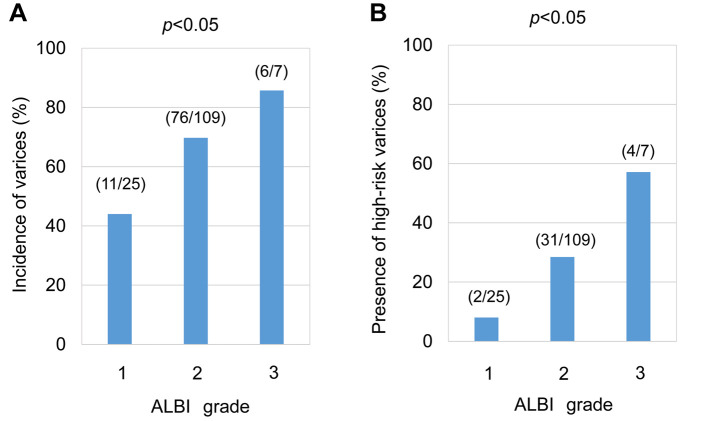
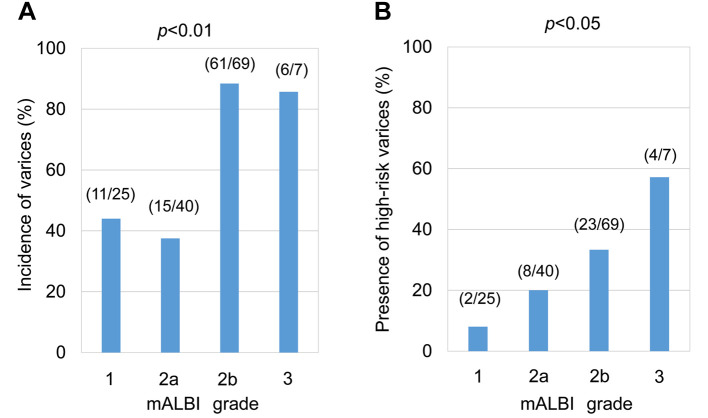
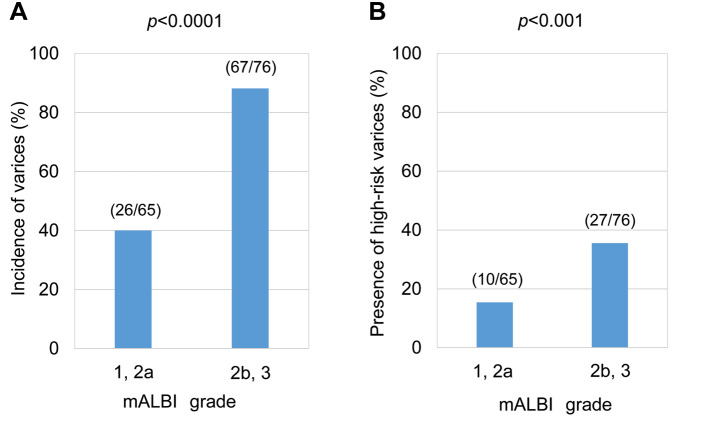
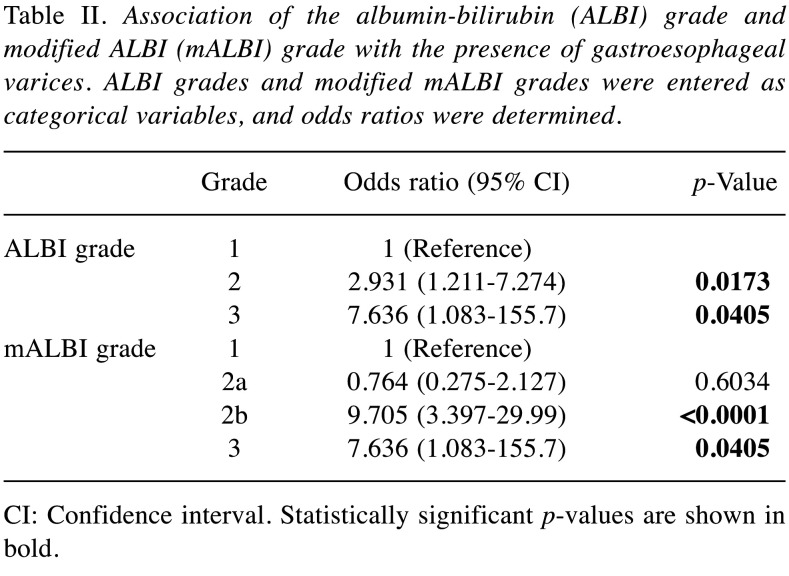
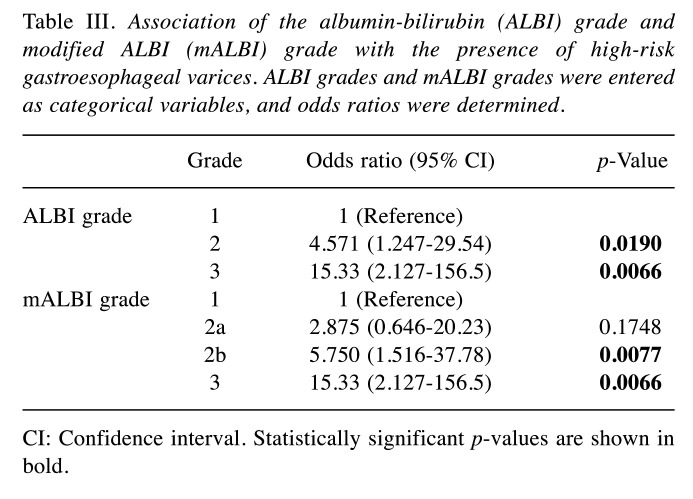
Association of the ALBI and mALBI grades with the endoscopic findings of GEVs. In the evaluation of ALBI grade alone, the incidence of GEVs statistically significantly differed among the groups, increasing with increasing grade (overall: p<0.05) (Figure 2A). The incidence of high-risk varices also statistically significantly increased as the grade increased (overall: p<0.05) (Figure 2B). When the mALBI grade was used, statistically significant differences were observed among the groups in the incidence of GEVs (overall: p<0.01) (Figure 3A) and the incidence of high-risk varices (overall: p<0.05) (Figure 3B). We further evaluated the relevance of the sub-classification of ALBI grade 2 to the endoscopic findings. The incidence of GEVs in patients with grade 2b or 3 was significantly higher in comparison to those with grades 1 or 2a (p<0.0001) (Figure 4A). Similar results were observed regarding the incidence of high-risk GEVs (p<0.001) (Figure 4B).
Figure 2. Association of the albumin-bilirubin (ALBI) grade with the endoscopic findings of gastroesophageal varices (GEVs). A: The incidence of GEVs among the ALBI grade groups differed statistically significantly (overall: p<0.05). B: The incidence of high-risk varices was statistically significantly increased as the grade increased (overall: p<0.05).
Figure 3. Association of the modified albumin-bilirubin (mALBI) grade with the endoscopic findings of gastroesophageal varices (GEVs). A: The incidence of GEVs among the mALBI grade groups was statistically significantly different (overall: p<0.01). B: Similarly, the incidence of highrisk varices among the groups differed statistically significantly (overall: p<0.05).
Figure 4. Comparison of the endoscopic findings of gastroesophageal varices (GEVs) between patients with albumin-bilirubin (ALBI) grade 1-2a and those with ALBI grade 2b-3. A: The incidence of GEVs in patients with grades 2b and 3 was significantly higher than that in those with grades 1 and 2a (p<0.0001). B: Similar results were observed regarding the incidence of high-risk GEVs (p<0.001).
The incidence rates of GEVs in patients with ALBI grades 2 or 3 were significantly higher in comparison to those with ALBI grade 1 (Table II); however, when the enrolled patients were classified according to the mALBI grade, the incidence rates in patients with mALBI grade 2b or grade 3, but not those with mALBI grade 2a, were significantly higher in comparison to that of patients with grade 1. Similar results were also observed regarding the incidence of high-risk GEVs (Table III).
Table II. Association of the albumin-bilirubin (ALBI) grade and modified ALBI (mALBI) grade with the presence of gastroesophageal varices. ALBI grades and modified mALBI grades were entered as categorical variables, and odds ratios were determined.
CI: Confidence interval. Statistically significant p-values are shown in bold
Table III. Association of the albumin-bilirubin (ALBI) grade and modified ALBI (mALBI) grade with the presence of high-risk gastroesophageal varices. ALBI grades and mALBI grades were entered as categorical variables, and odds ratios were determined.
CI: Confidence interval. Statistically significant p-values are shown in bold
Discussion
Variceal bleeding is a serious complication in patients with liver cirrhosis. However, EGD is relatively burdensome, and the ability to predict GEVs using noninvasive biomarkers would be useful. The ALBI score is suggested to be a more useful evaluation than the Child-Pugh classification, especially in patients with compensated cirrhosis (7,9). On the other hand, the ALBI score alone seems to have a limitation in that a large number of patients are classified into ALBI grade 2, and therefore the mALBI grade was proposed as a more detailed classification for patients with cirrhosis (9).
In 2018, a score that combined ALBI with the platelet count was proposed, and it was found that GEVs with a bleeding risk were rarely detected in patients with an ALBI-PLT score of 2 points (8). This suggested that the ALBI-PLT score can be used for the risk stratification of patients with ALBI grade 2, which includes a wide range of patients. The report focused on compensated cirrhosis with liver cancer; however, consistent results were obtained in the current cohort of patients without liver cancer (Figure 1). We herein used the mALBI classification to avoid the problem that a large number of patients were classified into ALBI grade 2. To our knowledge, this is the first report to study the association of endoscopic findings with mALBI grades. The endoscopic findings of GEVs were considered to differ between patients with mALBI grade 2a and those with grade 2b (Figure 4). The differences between the patients with mALBI grade 1 and those with grade 2a did not reach statistical significance (Tables II and III). Our findings suggest that the mALBI grade, in which grade 2 is divided into grade 2a and grade 2b, may be useful in predicting the presence of GEVs and for stratifying the bleeding risk of GEVs.
The present study was associated with several limitations. Firstly, the study population was limited to patients who underwent a liver biopsy and who had histologically proven cirrhosis. Thus, the study population was relatively small. In addition, we did not conduct liver biopsies for patients with highly advanced cirrhosis with signs of hepatic failure, such as ascites, and the study population only included a relatively small number of patients with ALBI grade 3. Secondly, all chronic liver diseases were included, and the difference due to etiology was not evaluated. Finally, in general, no single biomarker was able to completely predict the endoscopic findings of GEVs (15-17), and a combination of mALBI with other variable/parameter(s) should be considered.
In summary, we evaluated the association of the mALBI score with the endoscopic findings of GEVs. The endoscopic findings of GEVs were considered to differ between patients with mALBI grade 2a and those with grade 2b. The incidence of GEVs predicted by the mALBI score, with the sub-classifications of grade 2a and 2b, may differ from that predicted by ALBI grade 2.
Conflicts of Interest
The Authors declare no conflicts of interest in association with the present study.
Authors’ Contributions
YM collected and analyzed the data; HE designed the study, analyzed the data and wrote the article. NH, TN, and YI collected the data; SN and HI collected the data and supervised the study. All Authors reviewed and edited the article, and approved the final version of the article.
Acknowledgements
This work was partially funded by a grant from the Hyogo Innovative Challenge, Hyogo College of Medicine, Japan.
The Authors are grateful to Inui S, Higuchi Y, Kanazawa N, Matsushita Y, Fujii S, Kido H and Minemoto K (Hyogo College of Medicine) for their technical and secretarial assistance.
References
- 1.Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 Practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2017;65(1):310–335. doi: 10.1002/hep.28906. [DOI] [PubMed] [Google Scholar]
- 2.European Association for the Study of the Liver EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406–460. doi: 10.1016/j.jhep.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 3.Fukui H, Saito H, Ueno Y, Uto H, Obara K, Sakaida I, Shibuya A, Seike M, Nagoshi S, Segawa M, Tsubouchi H, Moriwaki H, Kato A, Hashimoto E, Michitaka K, Murawaki T, Sugano K, Watanabe M, Shimosegawa T. Evidence-based clinical practice guidelines for liver cirrhosis 2015. J Gastroenterol. 2016;51(7):629–650. doi: 10.1007/s00535-016-1216-y. [DOI] [PubMed] [Google Scholar]
- 4.Lee HA, Kim SU, Seo YS, Lee YS, Kang SH, Jung YK, Kim MY, Kim JH, Kim SG, Suk KT, Jung SW, Jang JY, An H, Yim HJ, Um SH. Prediction of the varices needing treatment with non-invasive tests in patients with compensated advanced chronic liver disease. Liver Int. 2019;39(6):1071–1079. doi: 10.1111/liv.14036. [DOI] [PubMed] [Google Scholar]
- 5.Kim NJ, Su F, Biggins SW. CON: Noninvasive modalities are preferred to screen for the diagnosis of esophageal and gastric varices when the diagnosis of cirrhosis is made. Clin Liver Dis. 2020;16(2):48–52. doi: 10.1002/cld.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Franchis R, Baveno VI Faculty Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–752. doi: 10.1016/j.jhep.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O’Beirne J, Fox R, Skowronska A, Palmer D, Yeo W, Mo F, Lai P, Iñarrairaegui M, Chan SL, Sangro B, Miksad R, Tada T, Kumada T, Toyoda H. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach – the ALBI grade. J Clin Oncol. 2015;33(6):550–558. doi: 10.1200/JCO.2014.57.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen PH, Hsieh WY, Su CW, Hou MC, Wang YP, Hsin IF, Yang TC, Liao WC, Lin HC, Lee FY, Wu JC. Combination of albumin-bilirubin grade and platelets to predict a compensated patient with hepatocellular carcinoma who does not require endoscopic screening for esophageal varices. Gastrointest Endosc. 2018;88(2):230–239.e2. doi: 10.1016/j.gie.2017.12.023. [DOI] [PubMed] [Google Scholar]
- 9.Hiraoka A, Kumada T, Tsuji K, Takaguchi K, Itobayashi E, Kariyama K, Ochi H, Tajiri K, Hirooka M, Shimada N, Ishikawa T, Tachi Y, Tada T, Toyoda H, Nouso K, Joko K, Hiasa Y, Michitaka K, Kudo M. Validation of modified ALBI grade for more detailed assessment of hepatic function in hepatocellular carcinoma patients: A multicenter analysis. Liver Cancer. 2019;8(2):121–129. doi: 10.1159/000488778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Enomoto H, Ueno Y, Hiasa Y, Nishikawa H, Hige S, Takikawa Y, Taniai M, Ishikawa T, Yasui K, Takaki A, Takaguchi K, Ido A, Kurosaki M, Kanto T, Nishiguchi S, Japan Etiology of Liver Cirrhosis Study Group in the 54th Annual Meeting of JSH Transition in the etiology of liver cirrhosis in Japan: A nationwide survey. J Gastroenterol. 2020;55(3):353–362. doi: 10.1007/s00535-019-01645-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shimono Y, Enomoto H, Kishino K, Moriwaki EI, Nishikawa H, Nishimura T, Iwata Y, Iijima H, Nishiguchi S. Arm skeletal muscle mass is associated with the prognosis of patients with cirrhosis. In Vivo. 2020;34(3):1165–1171. doi: 10.21873/invivo.11889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moriwaki EI, Enomoto H, Saito M, Hara N, Nishikawa H, Nishimura T, Iwata Y, Iijima H, Nishiguchi S. The anthropometric assessment with the bioimpedance method is associated with the prognosis of cirrhotic patients. In Vivo. 2020;34(2):687–693. doi: 10.21873/invivo.11825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yuri Y, Nishikawa H, Enomoto H, Yoh K, Iwata Y, Sakai Y, Kishino K, Ikeda N, Takashima T, Aizawa N, Takata R, Hasegawa K, Ishii N, Nishimura T, Iijima H, Nishiguchi S. Impact of sustained virological response for gastroesophageal varices in hepatitis-C-virus-related liver cirrhosis. J Clin Med. 2019;9(1):95. doi: 10.3390/jcm9010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nishikawa H, Yoh K, Enomoto H, Iwata Y, Sakai Y, Kishino K, Shimono Y, Ikeda N, Takashima T, Aizawa N, Takata R, Hasegawa K, Koriyama T, Yuri Y, Nishimura T, Nishiguchi S, Iijima H. Sarcopenia and frailty in chronic liver damage: Common and different points. In Vivo. 2020;34(5):2549–2559. doi: 10.21873/invivo.12072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lesmana CRA, Raharjo M, Gani RA. Managing liver cirrhotic complications: Overview of esophageal and gastric varices. Clin Mol Hepatol. 2020;26(4):444–460. doi: 10.3350/cmh.2020.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pateu E, Oberti F, Calès P. The noninvasive diagnosis of esophageal varices and its application in clinical practice. Clin Res Hepatol Gastroenterol. 2018;42(1):6–16. doi: 10.1016/j.clinre.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Calvaruso V, Cacciola I, Licata A, Madonia S, Benigno R, Petta S, Bronte F, Conte E, Malizia G, Bertino G, Distefano M, Montineri A, Digiacomo A, Alaimo G, Cacopardo B, Davì A, Guarneri L, Scalisi I, Colletti P, Cartabellotta F, Portelli V, Prestileo T, Averna A, Iacobello C, Mondello L, Scifo G, Russello M, Squadrito G, Raimondo G, Cammà C, Craxì A, Di Marco V, RESIST-HCV (Rete Sicilia Selezione Terapia-HCV) Is transient elastography needed for noninvasive assessment of high-risk varices? The REAL experience. Am J Gastroenterol. 2019;114(8):1275–1282. doi: 10.14309/ajg.0000000000000266. [DOI] [PubMed] [Google Scholar]