Abstract
Background/Aim: The aim of this study is to report a case series of three patients who developed postoperative severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) infection, although the initial tests were negative. Patients and Methods: Between April and September 2020, three patients submitted to pancreatoduodenectomy developed SARS-CoV-2 infection; their outcomes were compared to those of a similar group in which the postoperative outcomes were uneventful. Results: There were no significant differences between the two groups in terms of pre- and intraoperative outcomes; however, all of the three cases who developed SARS-CoV-2 infection postoperatively required re-admission in the intensive care unit and a longer hospital in stay. The overall mortality rate was null. Conclusion: Patients submitted to pancreatoduodenectomy for pancreatic head cancer who develop SARS-COV-2 infection postoperatively need a more appropriate supportive care; however, the overall mortality does not appear to increase, justifying, in this way, the continuation of programmed oncological of surgeries.
Keywords: COVID, pancreatic cancer, postoperative outcome, pandemic
Initially described as a new coronavirus subtype first detected to affect a significant number of Wuhan’s inhabitants, severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) became a true serial killer affecting all group ages globally in 2020 (1). Four months after describing the presence of the virus in the Chinese city the World Health Organization declared SARS-CoV-2 as an international pandemic on 11th of March 2020, with more than 10,000 new cases reported per day in Europe (2). At that moment the spread of the virus was far from being under control in Europe, so that at the end of April 2020 almost 80,000 new cases per day were being reported (2). In this context, and due to the increasing number of cases and their critical condition an large number of hospitals decided to concentrate all their resources for this subgroup of patients. Therefore, a significant number of patients diagnosed with oncological issues were forced to postpone their surgical procedures during this period, while places in the intensive care units were spared for corona virus disease-19 (COVID-19)-positive patients. Due to the fact that hepato-bilio-pancreatic cancer is recognized as one of the most aggressive tumors with a very high rate of progression (3-5), its surgical treatment is rather considered an emergency. For this reason, high attention was paid so that programmed hepato-bilio-pancreatic surgeries take place, even during the COVID-19 pandemic. In a significant number of oncology centers in Europe, it was decided to test all cases with this kind of neoplastic diseases, and following a negative result from a COVID-19 test, to submit the patient for pancreatic surgery. Although initially this protocol seemed to be very efficient, in certain cases there were complications with the postoperative outcome and, upon re-testing of these patients, some appeared to be COVID-19 -positive (6-9). The aim of this current paper is to report a case series of three patients who were negative for COVID-10 pre-operatively, however, they became positive in the early postoperative period.
Patients and Methods
After obtaining the Ethical Committee approval no 288/2020, patient data submitted to pancreatoduodenectomy between June and August 2020 were retrospectively reviewed. During this period, we identified three cases submitted to surgery for pancreatic head cancer who presented preoperative negative testing for COVID-19 and who developed a postoperative infection (group A). Their postoperative outcomes were compared to the outcomes of three patients diagnosed with similar pathologies in terms of the extent of the disease, associated comorbidities and age, who, however, tested negative for COVID-19 infection pre- and post-operatively (group B). Concerning the type of testing, in all six cases deep nasal swab samples were used for the detection of the viral RNA using protein chain reaction (PCR) in association with chest computed tomography.
Results
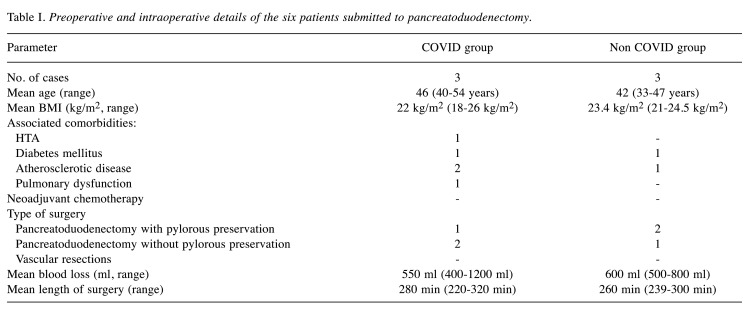
The mean age of the patients who developed postoperative SARS-CoV-2 infection (group A) was 46 years (range=40-54 years), similar to the age of group B (42 years). The mean body mass index was 22 kg/m2 in group A, similar to the one reported in group B (23.4 kg/m2). In all six cases the surgery intended was pancreatoduodenectomy, with the mean duration of it as well as the mean blood loss being similar between the two groups. Preoperative and intraoperative details are shown in Table I.
Table I. Preoperative and intraoperative details of the six patients submitted to pancreatoduodenectomy.
One patient from each group developed postoperative pancreatic fistula. The patient from group A necessitated early reintervention while the patient from group B was successfully treated in a conservative manner. In detail, the latter patient developed a febrile syndrome and was diagnosed with a 2/2 cm fluid accumulation in the proximity of the pancreatic anastomosis, but due to the fact that the overall condition was satisfactory the patient was treated with antibiotics and antisecretory therapy. The overall evolution of the patient’s condition was a favorable one at one week follow up, with the fluid accumulation reduced and the febrile syndrome remitted. Concerning respiratory-associated symptomatology, this was present in all three patients from group A and became clinically visible on the seventh, ninth and thirteenth days following pancreatic resection, respectively. All these cases presented oxygen desaturation up to 76%, followed by infection-associated hematological signs, such as lymphopenia. Due to the presence of these characteristics, nasal sampling was repeated for PCR testing and demonstrated the presence of COVID-19. All three cases were further admitted in the intensive care unit in order to be submitted to a specific supportive treatment; however, oro-tracheal intubation was needed in a single case, the one in which pancreatic fistula had been also diagnosed. The mean hospital in-stay in the intensive care unit for group A patients was 18 days (range=9-25 days), while following readmission, their mean length of hospital in-stay was 28 days (range=17-32 days). The mean postoperative hospital in-stay of group B patients was 14 days (range=8-19 days), and none of them was re-admitted in the intensive care unit. The overall mortality was null.
Discussion
During the SARS-CoV-2 pandemic, the most important listed reasons for temporization of pancreatic surgery for neoplastic disease were represented by the national directives for stopping surgeries for non-life-threatening pathologies, followed by the lack of available beds in the intensive care units and concern among patients of contracting SARS-CoV-2 infection during the postoperative period (6,7). Moreover, infection of medical stuff imposed taking the decision of self-isolation of the direct contacts increasing even more the service pressure due to a lower number of available healthcare workers (10,11).
Therefore, further challenge of the therapeutic protocols in cancer patients were needed; initially it has been considered that neoadjuvant therapy should be routinely administrated; However, it should not be omitted the fact that there was no evidence-based data which might demonstrate the effectiveness of such a modification of the therapeutic guidelines (6,12).
However, further studies came to demonstrate that cancer diagnosis in association with medical oncologic treatment might increase both the risk and the severity of COVID-19 infection (13-17). Therefore, it seems that administration of systemic chemotherapeutic agents might predispose to the diminishing of the patients’ immunity, increasing in this way the chances to contract the virus and moreover, to develop severe, fulminant forms of the disease (8). Therefore, it is well known the fact that administration of FOLFIRINOX regimen, one of the most widely recommended chemotherapeutical protocols in pancreatic cancer patients is associated with a significant risk of grade 3 and 4 neutropenia and lymphopenia (18,19). Meanwhile, cases diagnosed with COVID infection present a higher risk of lymphopenia, infection itself being responsible for the weakening of the immune system (20).
An interesting consensus which was published on this issue in 2020 came to demonstrate that pancreatic surgery should not be temporized in patients presenting malignant diseases; moreover the same consensus established the fact that in such cases informed consents which will underline the additional perioperative risks as well as special protection equipment should be mandatory in order to allow to continue performing pancreatic surgery for malignant pathologies irrespective of the levels of contamination with COVID in the next period (21).
Meanwhile a systematic review conducted by the Italian Surgeons at the University of Padova stated that all potential curable pancreatic lesions (including those who ended the neoadjuvant chemotherapy) as well as cases presenting high grade dysplastic lesions should undergo resection; meanwhile the same study group stated that pancreatic surgery should be postponed only in particular situations, if pandemic escalates; therefore in this condition the authors recommend only performing lifesaving procedures such as biliary drainage in case of cholangitis or alimentary derivative procedures for upper digestive stenosis (22).
Another multicentric study which has just been published and which also comes from the Northern Italy recommends performing upfront surgery in all cases presenting resectable lesions followed by FOLFIRINOX adjuvant chemotherapy only in cases presenting a good general status (defined as ECOG PS=0 and age under 70 years); even in these cases the authors recommend that this treatment should be performed at 12 weeks after resection; meanwhile in cases presenting locally advanced or metastatic lesions the same study group recommends choosing gemcitabine and nab-paclitaxel instead of FOLFIRINOX in order to diminish the adverse outcomes. In cases in which this change cannot be performed, decreasing the doses of irinotecan and omission of 5 fluorouracil has been proposed in order to increase the tolerability (23).
Surprisingly, the study conducted at the MD Anderson Cancer Center, Houston, United States of America concluded that neoadjuvant chemotherapy should be considered the option of choice even in cases presenting localized disease due to the fact that pancreatic surgery is otherwise associated with increased risks of postoperative complications; in this respect, for pancreatic cancer patients, the American scientists proposed administration of neoadjuvant chemotherapy alone or in association with radiation therapy, and proposed that these treatments should be performed in hospitals as close as possible to patients’ residence in order to avoid traveling (24).
One of the most relevant studies which came to demonstrate the catastrophic effect of postponing the treatment in pancreatic cancer patients comes from Sud et al. and demonstrates that a three months delay to diagnostic is associated with a reduction of the 10-year survival rate with more than 10% in most age groups (25).
According to a recently published consensus which revealed the United Kingdom's position, the interviewed experts stated that systemic therapy should be administrated in locally advanced and metastatic disease while cases presenting limited disease should be further treated by surgery (10); meanwhile the same study group underlined the necessity of dose modification and administration of antibioprophilaxy and of prophylactic growth factors in order to avoid the development of any synchronous infections which might supplementary affect the immune status of pancreatic cancer patients. In the meantime, the same study group underlined the fact that patients should be encouraged to respect the measures of social distancing as well as to use telephone consultations in order to minimize the contact with other potential COVID positive patients or even health care workers. When it comes to resectable lesions, the authors underlined once again the need of careful selection of cases submitted to surgery (according to their general status and comorbidities), the necessity of performing such procedures in well defined, clean zones or even in selected hospitals which are found in areas with a lower number of COVID infections as well as the recommendation of decreasing the number of robotic procedures in order to minimize the costs (10). However, a recent study conducted by the Chinese authors came to demonstrate that both oncological patients submitted to surgery or to chemotherapy presented a significantly higher risk of developing severe episodes of COVID 19 infection after completing their treatment (14).
As for the risks of postoperative complications, it is widely understood the fact that performing such complicated surgical procedures might be associated with increased risks of postoperative complications related both to surgical procedure and to pulmonary diseases. As demonstrated in our study, patients diagnosed with COVID infection necessitated a more supportive respiratory treatment including oro-tracheal intubation; although these complications necessitated a longer intensive care in stay the overall mortality was null, demonstrating in this way the effectiveness and safety of the method.
In conclusion, during the pandemic period, multiple therapeutic strategies have been proposed in pancreatic cancer patients (26). However, it should not be omitted the fact that this is a very aggressive malignancy and each postponement of any therapeutic gesture might significantly decrease the overall survival. Therefore, we suggest that resection should be taken in consideration whenever is feasible; meanwhile, attention should be focused on early identification of any clinical signs which might preclude COVID infection; in this way, an early recognition of the viral infection might provide the chance for best supportive care and in the meantime might decrease the risk of postoperative mortality. In our study group none of the three cases deceased during the postoperative period although an increased length of intensive care unit and overall hospital in stay was observed.
Conflicts of Interest
The Authors have no conflicts of interest to declare regarding this study.
Authors’ Contributions
NB performed surgical procedures; CD, CoS, CaS and OS preoperatively investigated the patients and postoperatively treated SARS-CoV-2 infection; IB did the literature review; NB, IB, OS, and CaS analyzed data; CD, CoS, OS and IB – prepared the draft; NB finally revised the draft of the manuscript. All Authors read and approved the final version of the manuscript.
References
- 1.Deng X, Yang J, Wang W, Wang X, Zhou J, Chen Z, Li J, Chen Y, Yan H, Zhang J, Zhang Y, Wang Y, Qiu Q, Gong H, Wei X, Wang L, Sun K, Wu P, Ajelli M, Cowling BJ, Viboud C, Yu H. Case fatality risk of the first pandemic wave of novel coronavirus disease 2019 (COVID-19) in China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Statement on the COVID-19 situation in Europe. Available at:euro.who.int/en/health-topics/health-emergencies/coronaviruscovid-19/statements/statement-on-the-covid-19-situation-ineurope.
- 3.Brasoveanu V, Anghel C, Barbu I, Pautov M, Ionescu MI, Motthor M, Balescu I, Dima S, Bacalbasa N. Pancreatoduodenectomy en bloc with portal and superior mesenteric artery resection – a case report and literature review. Anticancer Res. 2015;35(3):1613–1618. [PubMed] [Google Scholar]
- 4.Brasoveanu V, Dumitrascu T, Bacalbasa N, Zamfir R. Splenic artery used for replaced common hepatic artery reconstruction during pancreatoduodenectomy – a case report. Chirurgia (Bucur) 2009;104(4):499–504. [PubMed] [Google Scholar]
- 5.Bacalbasa N, Balescu I, Tanase A, Pautov M, Brezean I, Vilcu M, Brasoveanu V. Spleno-pancreatectomy en bloc with parcelar gastrectomy for splenic artery aneurysm - a case report and literature review. In Vivo. 2018;32(4):915–919. doi: 10.21873/invivo.11329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balakrishnan A, Lesurtel M, Siriwardena AK, Heinrich S, Serrablo A, Besselink MGH, Erkan M, Andersson B, Polak WG, Laurenzi A, Olde Damink SWM, Berrevoet F, Frigerio I, Ramia JM, Gallagher TK, Warner S, Shrikhande SV, Adam R, Smith MD, Conlon KC. Delivery of hepato-pancreato-biliary surgery during the COVID-19 pandemic: A European-African Hepato-Pancreato-Biliary Association (E-AHPBA) cross-sectional survey. HPB (Oxford) 2020;22(8):1128–1134. doi: 10.1093/cid/ciaa578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, Zhan LY, Jia Y, Zhang L, Liu D, Xia ZY, Xia Z. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aminian A, Safari S, Razeghian-Jahromi A, Ghorbani M, Delaney CP. COVID-19 outbreak and surgical practice: Unexpected fatality in perioperative period. Ann Surg. 2020;272(1):e27–e29. doi: 10.1097/SLA.0000000000003925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Society of Surgical Oncology (SSO). Resource for management options of GI and HPB cancers. . Available at: https://www.surgonc.org/wp-content/uploads/2020/03/GI-and-HPB-Resource-during-COVID-19-3.23.20.pdf.
- 10.Jones CM, Radhakrishna G, Aitken K, Bridgewater J, Corrie P, Eatock M, Goody R, Ghaneh P, Good J, Grose D, Holyoake D, Hunt A, Jamieson NB, Palmer DH, Soonawalla Z, Valle JW, Hawkins MA, Mukherjee S. Considerations for the treatment of pancreatic cancer during the COVID-19 pandemic: the UK consensus position. Br J Cancer. 2020;123(5):709–713. doi: 10.1038/s41416-020-0980-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Philouze P, Cortet M, Quattrone D, Ceruse P, Aubrun F, Dubernard G, Mabrut JY, Delignette MC, Mohkam K. Surgical activity during the Covid-19 pandemic: Results for 112 patients in a French tertiary care center, a quality improvement study. Int J Surg. 2020;80:194–201. doi: 10.1016/j.ijsu.2020.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barcellini A, Vitolo V, Cobianchi L, Valvo F, Vischioni B, Bonora M, Fiore MR, Iannalfi A, Riva G, Ronchi S, Tornari E, Orlandi E. Pancreatic cancer: Does a short course of carbon ion radiotherapy worth during COVID-19 outbreak. Pancreatology. 2020;20(5):1004–1005. doi: 10.1016/j.pan.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6(7):1108–1110. doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xia Y, Jin R, Zhao J, Li W, Shen H. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21(4):e180. doi: 10.1016/S1470-2045(20)30150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, Liu XQ, Chen RC, Tang CL, Wang T, Ou CQ, Li L, Chen PY, Sang L, Wang W, Li JF, Li CC, Ou LM, Cheng B, Xiong S, Ni ZY, Xiang J, Hu Y, Liu L, Shan H, Lei CL, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Cheng LL, Ye F, Li SY, Zheng JP, Zhang NF, Zhong NS, He JX. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miyashita H, Mikami T, Chopra N, Yamada T, Chernyavsky S, Rizk D, Cruz C. Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann Oncol. 2020;31(8):1088–1089. doi: 10.1016/j.annonc.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la FC, Bennouna J, Bachet JB, Khemissa-Akouz F, Pere-Verge D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817–1825. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 19.Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel R, Saif MW. Management of pancreatic cancer during COVID-19 pandemic: To treat or not to treat. JOP. 2020;21(2):27–28. [PMC free article] [PubMed] [Google Scholar]
- 21.Soreide K, Hallet J, Matthews JB, Schnitzbauer AA, Line PD, Lai PBS, Otero J, Callegaro D, Warner SG, Baxter NN, Teh CSC, Ng-Kamstra J, Meara JG, Hagander L, Lorenzon L. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020;107(10):1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moletta L, Pierobon ES, Capovilla G, Costantini M, Salvador R, Merigliano S, Valmasoni M. International guidelines and recommendations for surgery during Covid-19 pandemic: A systematic review. Int J Surg. 2020;79:180–188. doi: 10.1016/j.ijsu.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pietrantonio F, Morano F, Niger M, Corallo S, Antista M, Raimondi A, Prisciandaro M, Pagani F, Prinzi N, Nichetti F, Randon G, Torchio M, Corti F, Ambrosini M, Palermo F, Palazzo M, Biamonte L, Platania M, Sposito C, Cosimelli M, Mazzaferro V, Pusceddu S, Cremolini C, de Braud F, Di Bartolomeo M. Systemic treatment of patients with gastrointestinal cancers during the COVID-19 outbreak: COVID-19-adapted recommendations of the National Cancer Institute of Milan. Clin Colorectal Cancer. 2020;19(3):156–164. doi: 10.1016/j.clcc.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tzeng CD, Tran Cao HS, Roland CL, Teshome M, Bednarski BK, Ikoma N, Graham PH, Keung EZ, Scally CP, Katz MHG, Gershenwald JE, Lee JE, Vauthey JN. Surgical decision-making and prioritization for cancer patients at the onset of the COVID-19 pandemic: A multidisciplinary approach. Surg Oncol. 2020;34:182–185. doi: 10.1016/j.suronc.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sud A, Torr B, Jones ME, Broggio J, Scott S, Loveday C, Garrett A, Gronthoud F, Nicol DL, Jhanji S, Boyce SA, Williams M, Riboli E, Muller DC, Kipps E, Larkin J, Navani N, Swanton C, Lyratzopoulos G, McFerran E, Lawler M, Houlston R, Turnbull C. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21(8):1035–1044. doi: 10.1016/S1470-2045(20)30392-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vanni G, Legramante JM, Pellicciaro M, de Carolis G, Cotesta M, Materazzo M, Buonomo C, Farinaccio A, Santori F, Saraceno F, Ielpo B, Aiello F, Paganelli C, Grande M, de Andreis G, Chiocchi M, Palombi L, Buonom OC. Effect of lockdown in surgical emergency accesses: Experience of a COVID-19 hospital. In Vivo. 2020;34(5):3033–3038. doi: 10.21873/invivo.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]