Rarely appropriate cardiac stress tests remain prevalent in the range of 10% to 20% (1) and unnecessarily prolong wait times. To address this ongoing problem, we designed the EPIQ-Stress workflow, which includes a structured electronic consult (“e-consult”) with all outpatient stress test orders. The e-consult was designed to provide real-time decision support guiding appropriate test selection, individualized feedback to primary care clinicians (PCCs) regarding ordered test appropriateness, and the patient-specific rationale for any changes or cancellations of test orders. In this study, we assessed whether EPIQ-Stress implementation was associated with a reduction in rarely appropriate testing and in order-to-report wait times.
The pre-implementation cohort included consecutive veteran patients aged 40 to 75 years without a history of coronary artery disease referred by PCCs for exercise treadmill testing, stress single-photon emission computed tomography myocardial perfusion imaging, or stress echocardiography between March 1, 2017 and August 30, 2017. In these veterans, we determined the Appropriate Use Criteria (AUC) indication under which stress test referral occurred (2) and calculated “order-to-report” wait time as the number of days between order entry and test report generation. The EPIQ-Stress workflow (Figure 1A) was implemented at the Providence Veterans Affairs (VA) Medical Center on April 1, 2018. The e-consult was a checkbox-based hierarchical questionnaire structured to efficiently define the most appropriate AUC indication and then guide PCC ordering of an appropriate test (or no test). E-consult responses were required within 48 h and were templated (Figure 1B). The post-intervention cohort consisted of consecutive veterans meeting the pre-intervention cohort criteria who were referred for stress testing between April 1, 2018 and March 31, 2019. Between-cohort differences in the proportion of rarely appropriate tests were assessed using a chi-square test. Differences in order-to-report wait times were assessed using a 2-sample Wilcoxon rank-sum test. The Providence VA Medical Center granted institutional review board approval.
FIGURE 1. EPIQ-Stress.
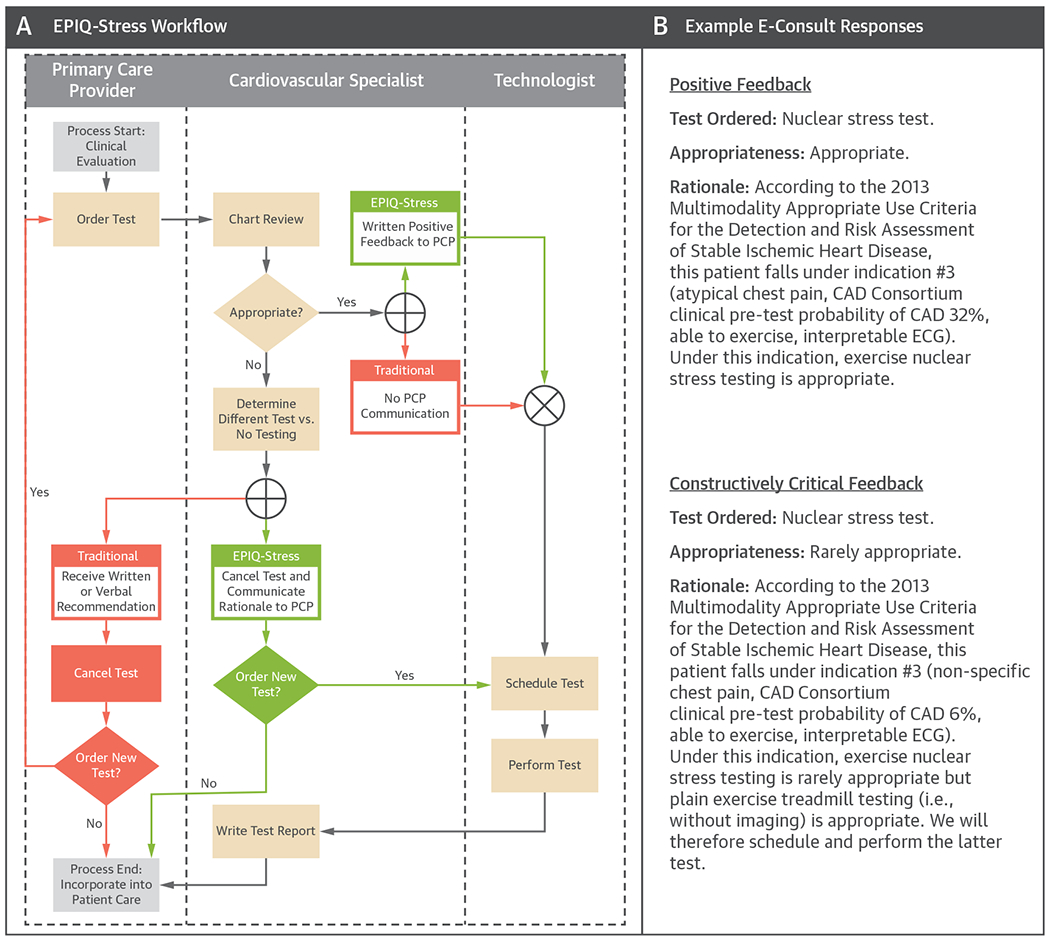
(A) EPIQ-Stress Workflow. Swimlane diagram showing key differences between EPIQ-Stress and traditional workflows. (B) Example E-Consult Responses. CAD = coronary artery disease; ECG = electrocardiogram; PCP = primary care provider.
The pre- and post-intervention cohorts included 90 and 255 veterans, respectively, and both were predominantly composed of middle-aged non-Hispanic white males. AUC indications 1 to 6, representing tests requested for detection of coronary artery disease in symptomatic patients (2), accounted for ~85% of PCC referrals in both cohorts. Comparing the pre- and post-intervention cohorts, there was a nonsignificant reduction in the prevalence of rarely appropriate tests ordered (8% to 5%; chi-square test = 0.87; p = 0.35), but there was a significant reduction in the prevalence of rarely appropriate tests performed (8% to 2%; v = 8.31; p = 0.004). The median order-to-report wait time decreased from 26 days (interquartile interval: 18 to 32 days) in the pre-intervention cohort (n = 89) to 21 days (interquartile interval: 17 to 27 days) in the post-intervention cohort (n = 195), a statistically significant reduction (2-sample Wilcoxon rank-sum test p = 0.0433).
This study showed that EPIQ-Stress implementation was associated with a significant reduction in the prevalence of rarely appropriate cardiac stress tests performed and in order-to-report wait times. Our results suggest real-time clinical decision support may help PCCs order more appropriate tests but must be paired with structured auditing (including test changes or cancellations as appropriate) and feedback after order entry to achieve significant reduction in the prevalence of rarely appropriate tests. Moreover, full capture of feedback within the health record is a unique feature of EPIQ-Stress compared with prior clinical decision support tools (3) and simplifies retrospective audits of stress test appropriateness. We believe the improvement in order-to-report wait time was largely driven by the novel EPIQ-Stress mandate to answer e-consults (i.e., complete pre-test protocoling) within 48 h. Lastly, we believe EPIQ-Stress represents a viable policy alternative to the Centers for Medicare and Medicaid AUC Program, which shifts the burden of pre-test protocoling to nonspecialist referring providers. In contrast, EPIQ-Stress encourages appropriate testing through ground-level collaboration between referring providers and specialists.
Given the encouraging results at a single clinical site, there may be value in expanding EPIQ-Stress to other VA and non-VA clinical sites to determine if similar gains in quality care delivery can be achieved.
Acknowledgments
This work was supported by the Agency for Healthcare Research and Quality award 5K12HS022998 (Dr. Shah), the National Institute of General Medical Sciences award U54GM115677 (Dr. Shah and Dr. Sarkar), the Department of Veterans Affairs Health Service Research & Development Service award CDA0-020-16W (Dr. Winchester), the Research Project Grant from the National Institutes of Health (NIH) National Heart, Lung, and Blood Institute R01HL139795 (Dr. Morrison), and the Institutional Development Award (IDeA) from the NIH NIGMS P20GM103652 (Dr. Morrison). The opinions expressed reflect those of the authors and not necessarily those of the National Institutes of Health, the Department of Veterans Affairs, or the US government. All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
REFERENCES
- 1.Ladapo JA, Blecker S, O’Donnell M, Jumkhawala SA, Douglas PS. Appropriate use of cardiac stress testing with imaging: a systematic review and meta-analysis. PloS One 2016;11:e0161153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolk MJ, Bailey SR, Doherty JU, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014; 63:380–406. [DOI] [PubMed] [Google Scholar]
- 3.Lin FY, Dunning AM, Narula J, et al. Impact of an automated multimodality point-of-order decision support tool on rates of appropriate testing and clinical decision making for individuals with suspected coronary artery disease: a prospective multicenter study. J Am Coll Cardiol 2013;62: 308–16. [DOI] [PubMed] [Google Scholar]


