Abstract
Hepatocellular carcinoma (HCC) is the second leading cause of death due to cancer. Although there are different treatment options, these strategies are not efficient in terms of restricting the tumor cell’s proliferation and metastasis. The liver tumor microenvironment contains the non-parenchymal cells with supportive or inhibitory effects on the cancerous phenotype of HCC. Several signaling pathways are dis-regulated in HCC and cause uncontrolled cell propagation, metastasis, and recurrence of liver carcinoma cells. Recent studies have established new approaches for the prevention and treatment of HCC using small molecules. Small molecules are compounds with a low molecular weight that usually inhibit the specific targets in signal transduction pathways. These components can induce cell cycle arrest, apoptosis, block metastasis, and tumor growth. Devising strategies for simultaneously targeting HCC and the non-parenchymal population of the tumor could lead to more relevant research outcomes. These strategies may open new avenues for the treatment of HCC with minimal cytotoxic effects on healthy cells. This study provides the latest findings on critical signaling pathways governing HCC behavior and using small molecules in the control of HCC both in vitro and in vivo models.
Keywords: Hepatocellular carcinoma, Cancer, Signaling pathways, Small molecules, Carcinoma
Background
Hepatocellular carcinoma (HCC) or hepatoma is the most type of cancer in the tissues of the liver and the second leading cause of cancer-related death around the world [1, 2]. Hepatitis B/C virus and alcohol consumption are two important and independent risk factors that increase the risk of HCC [3–5]. Liver transplantation or surgical liver resection are two main options for the treatment of HCC [6, 7]. In addition to other surgical treatment options, some non-surgical methods such as chemotherapy or radiotherapy are effective treatments for HCC [8, 9]. However, these methods are not able to restrict the growth, progression, and metastasis of HCC [10]. On the other hand, these treatments cause side effects on the surrounding healthy cells [11]. Several signaling pathways are dis-regulated in HCC and lead to uncontrolled cell division and metastasis [12, 13]. Targeting specific signaling pathways that are involved in HCC phenotypes such as non-stopped cell proliferation, migration, and metastasis may control the progress of the disease [14, 15]. Recent studies have established a new approach for the prevention and treatment of HCC using small molecules [16]. Small molecules are compounds with a low molecular weight that usually inhibit the specific targets in signal transduction pathways [14, 17]. Targeting cancer-specific signaling pathways using small molecules can be novel therapeutic strategies against HCC (Table 1). Inhibition of these signaling pathways or common downstream effectors by different anti-cancer agents leads to increase apoptosis and autophagy along with a decrease in the survival, metastasis, EMT, proliferation, and colony formation of HCC cell lines and animal models [18, 19]. This study provides the latest findings on using small molecules in the control of HCC both in vitro and in vivo models.
Table 1.
The effects of small molecules on signaling pathways related to HCC
| Pathway | Small molecule | Target | Cell line | Animal model | Result | Ref. | |
|---|---|---|---|---|---|---|---|
| TGF-B | Galunisertib (LY2157299) |
Phase II/III in HCC |
Receptor | SK-HEP1, HepG2, Hep3B, Huh7 | – |
Decrease proliferation, increase apoptosis In combination with Sorafenib, the anti-cancer effects was increased in concentration dependent manner |
[42] |
| PD98059 | – | ERK | HepG2 | 7 × 105 HepG2 intraperitoneal into nude mice |
Inhibit proliferation, migration, invasion, and tumor growth – |
[45] | |
| Wnt | IC-2 | – | TCF/β-catenin | Huh7, HepG2, HLF | Huh7 spheres to flank of NOD/SCID mice |
Decrease the CSC subpopulation – |
[63] |
| CGP049090/ PKF115-854 |
-/ PMID: 23,626,717 |
TCF/β-catenin | Huh7, HepG2, | 1 × 107 HepG2 subcutaneously to Nude mice |
Induce apoptosis, cell cycle arrest, inhibit tumor growth – |
[191] | |
| Hh | Cyclopamine |
Phase III |
SMO receptor | Huh7, PLC, SM-7721, | 5 × 106 Mistheton Lectin-1 into the left liver of mice |
Induce apoptosis, inhibit tumor growth -/- |
[74, 192] |
| GANT61 | – | Gli | Huh7, Hep3B, HepG2 | 1 × 107 Huh7 cells to flank of SCID mice |
Induce the autophagy and apoptosis, Inhibit the HCC tumor growth Similar to Sorafenib, increase the apoptosis |
[71] | |
| GDC-0449 |
Phase II |
SMO receptor | Huh7, MHCC97 | 5 × 106 MHCC97subcutaneously to syngeneic rat |
Decrease the angiogenesis Combined with Sorafenib can modulate the VEGF expression |
[69] | |
| Notch | PF-4014 |
Phase II https://clinicaltrials.gov/ct2/show/NCT02299635?cond=PF-03084014&draw=2&rank=1 |
γ-secretase | MHCC97, Huh7 | 1 × 106 MHCC97-H or 4 × 105 CSC subcutaneously to nude or SCID mice then tumor cubes were then implanted into nude mice liver lobes |
Inhibited the proliferation of HCC and CSC self-renewal, decrease the tumor volume, and suppress the liver tumor metastasis PF-03084014 in combination with cisplatin or doxorubicin increase the anti-cancer effects |
[80] |
| GSI |
Phase II |
γ-secretase | Bel7404, HepG2 | – |
Decrease the HCC proliferation and colony formation – |
[81] | |
| EGF | Brivanib |
Phase II |
Tyrosine kinase receptor | Hep3B, HepG2, Huh7 | DEN to rat |
HCC apoptosis, cell cycle arrest, inhibit the liver tumor growth – |
[193] |
| U0126 | – | Erk | HCCLM3, HepG2 | – |
Decrease proliferation – |
[87] | |
| BEZ-235/ SHBM1009 | PhaseII, https://clinicaltrials.gov/ct2/show/NCT01288092/- | PI3K | |||||
| HGF | PHA665752 | – | c-met | MHCC97l Huh7, Hep3B | 3 × 105 MHCC97 subcutaneously to nude mice |
Inhibit proliferation, tumor growth, and CSC, increase apoptosis – |
[93] |
| AMG 337 | Phase I/II, https://clinicaltrials.gov/ct2/show/NCT02096666 | c-met | MHCC97, HCCLM3, Hep3B, SNU, JHH5 | human primary HCC tumor tissues Subcutaneously injecting nude mice |
Decrease proliferation, tumor growth – |
[95] | |
| Indo5 | – | c-met |
HepG2, A549, SMMC-7721 MHCC97H |
2 × 106 HepG2, 4 × 106 MHCC 97H, 4 × 106 MHCC 97 L, 2 × 106 A549 cells, or 5 × 106 SMMC-7721 subcutaneously to flank of SCID mouse MHCC97H subcutaneously to flank of SCID mouse then insert tumor into liver |
Inhibit proliferation, migration, and metastasis Similar or better result in animal model recovery compared with Sorafenib In contrast to Sorafenib without body weight lost |
[94] | |
| VEGF | Bufalin | – | VEGFR/EGFR | SMMC-7721, PLC | 5 × 106 SMMC-7721 subcutaneously to flank of nude mice |
Inhibit angiogenesis, HCC migration, and proliferation The anti-cancer effects of Bufalin improved in combination with Sorafenib |
[194] |
| Stat3 | Jaki | – | Jak | Huh7, Hep3B, HepG2 | – |
Increase apoptosis Sensitize the HCC to anti-cancer effects of Sorafenib |
[112] |
| C188-9 | – | Stat3 | PLC, HepG2, Huh7 | HepPten- mice Non-alcoholic steatohepatitis (NASH) |
Decrease the survival of HCC, reduce the HCC proliferation, decrease the secretion of inflammatory factors – |
[113] | |
| S3i-201 | – | Stat3 | Huh7, Hep3B, HepG2 | – |
Induce HCC apoptosis and enhance the Sorafenib effects Increase the anti-cancer effects of Sorafenib |
[112] | |
| UA | – | Stat3 | Huh7, HepG2, SM-7721, Hep3B | 1 × 107 HepG2 subcutaneously into flank of nude mice |
Increase the HCC apoptosis, inhibit the tumor growth – |
[114] | |
| 2-Ethoxystypandrone | Stat3 | HepG2 | – |
Induce apoptosis and cell cycle arrest, inhibit the CSC self-renewal – |
[115] | ||
| YAP/TAZ | verteporfin | – | YAP/TEAD | Huh7, MLP29 | IP injection of DENA to Rats |
Decrease the colony formation, survival, and tumor colony – |
[125] |
| HIF | PT2385 | Phase I, https://clinicaltrials.gov/ct2/show/NCT02293980 | HIF-2a | HepG2, Sk-hep1 | of 1 × 106 SK-Hep1 intrahepatic injections to nude mice |
Increase the efficiency of Sorafenib treatment, decrease invasion and survival Increase the anti-cancer effects of Sorafenib |
[136] |
| Cell cycle | Dinaciclib | Phase I https://clinicaltrials.gov/ct2/show/NCT01711528?cond=Dinaciclib&draw=2&rank=2 | Cdk1,2,5,9 | Hep3B, HLE | 1 × 106 Huh7 cells or 2 × 106 PLC BALB/c subcutaneously to nude mice |
Decrease the colony formation, survival, induce cell cycle arrest, decrease the tumor size Similar results with Sorafenib |
[143] |
| Ribociclib | – | CylinD/cdk4,6 | Huh7, HepG2, Hep3B, PLC | – |
Decrease cell proliferation Synergist effects with Sorafenib and anti-cancer effects on Sorafenib resistance-HCC lines |
[144] | |
| Apoptosis | Tumstatin | – | Akt/mTOR | Huh7, Hep3B | 5 × 106 Hep3B cells subcutaneously to armpit of nude mice |
Induce apoptosis, cell cycle arrest, autophagy, decrease the tumor growth, increase the apoptotic proteins – |
[171] |
| Brivanib | – |
FGF, VEGF, P53 |
Huh7, HepG2, Hep3B, | Rat with DENA |
Induce cell cycle arrest and apoptosis – |
[82] | |
| Nutlin | – | MDM | Huh7, SM-7721, | – |
Inhibit proliferation and survival – |
[161] | |
| Rubone | – | miR-34a, Bcl2, cyclinD | HepG2, HuH7, Hep3B | 5 × 106 HepG2 to dorsal flanks of nude mice |
Activate the miR34 and inhibit the TGF-B pathway and tumor growth Stronger than Sorafenib |
[162] | |
| Autophagy | Verteporfin | lysosom | HepG2, HuH7 | 2 × 106 HepG2 to dorsal flanks of nude mice |
Induce autophagy Increase the anti-cancer effects with Sorafenib |
[173] | |
| NVP-BGT226 | – | mTOR | Hep3B, HepG2, SNU475, Mahlavu | – |
Induce autophagy More sensitive to Sorafenib |
[174] | |
| Mitoxantrone | – | mTOR | HepG2, HuH7 | – |
Induce autophagy – |
[170] | |
| ROS | Propyl gallate | – | ROS formation | HepJ5, Hep3B, Mahlava | 200 HepJ5 or Hep3B injected to yolk of zebrafish embryos |
Decrease proliferation, increase apoptosis and autophagy – |
[186] |
| Auranofin | – | TXNRD | Hep3B | – |
Increase apoptosis – |
[184] |
Characterization of HCC
Hepatocytes as the most functionally liver cells have been reported to participate in HCC [20, 21].
Disruption of intracellular regulators or extracellular signals in the tumor microenvironment (TME) leads to inappropriate activation of certain signaling pathways [22–24]. Thus, aberrant molecular signaling increases levels of abnormal epigenetic modification and gene expression in the cancerous hepatocytes [25]. The outcome of these events is the loss of mature or differentiated hepatocytes (a phenomenon termed cellular dedifferentiation) [26, 27]. Under these conditions, the expression of E-cadherin (an epithelial marker) is downregulated and the cytoskeleton is reorganized [28]. The expression of Snail, Twist, and ZEB as the major transcription factors associated with mesenchymal cellular phenotype are up-regulated and induce an epithelial-to-mesenchymal transition (EMT) state in HCC [29]. Matrix metalloproteinases (MMPs) are also expressed at a high level in HCC and promote cellular migration and angiogenesis [30]. In HCC, the telomerase activity increases by up to 90%, checkpoints of the cell cycle are inactivated, and apoptosis is suppressed [31, 32]. All of these events cause uncontrolled cell proliferation, prolonged cell viability, and metastasis in HCC [33]. In HCC, several growth factors are released from non-parenchymal cells around the hepatocytes [14]. This event triggers cancerous phenotypes include EMT, metastasis, checkpoints aberration, uncontrolled proliferation, immortalization, and neovascularization in hepatocytes [34]. Other stimulators of hepatocyte malignancy come from microenvironmental cues such as hypoxia [35].
Critical signaling pathways in HCC
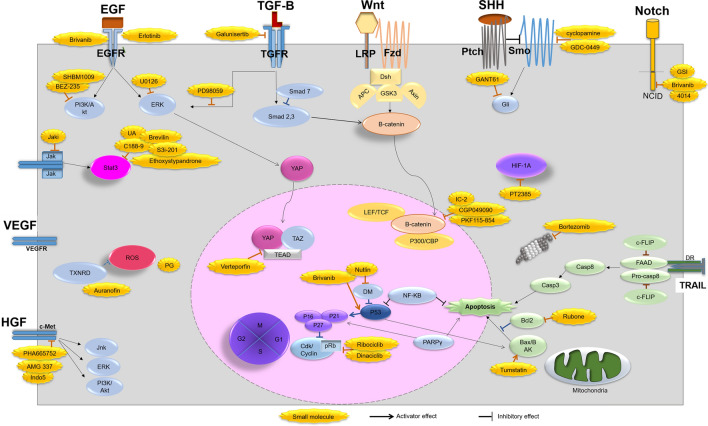
Several signaling pathways, including TGF-β, Wnt/B-catenin, Hh, Notch, EGF, HGF, VEFG, JAK/STAT, Hippo, and HIF are dis-regulated in HCC and lead to uncontrolled cell division and metastasis (Fig. 1).
Fig. 1.
Critical signaling pathways governing HCC behavior and using small molecules in the control of HCC
Transforming growth factor-β (TGF-β) signaling
Cancer-associated fibroblast (CAF), derived from either stromal cells or hepatocytes is the main source of TGF-β secretion in the liver tumor [36]. TGF-β binds to the heterodimer of receptors, TβRII and TβRI, phosphorylates and activates Smad2/3 that further translocate to the nucleus in association with Smad4 [37]. TGF-β upregulates the expression of Snail, downregulates E-cadherin in the polarized hepatocytes, and promotes EMT and metastasis [38]. The role of the TGF-β signaling pathway is also the preservation of CSC subpopulation and the promotion of HCC proliferation [39]. This pathway has been shown to induce VEGF expression in HCC and recruit endothelial cells at the tumor site [40]. TGF-β with the EGF, Wnt, and SHH pathways can promote the mesenchymal features of HCC cell lines [41]. TGF-β converts tumor-associated macrophages (TAM) to M2-like macrophages and improves proliferation, metastasis, and neoangiogenesis of HCC [38], suppresses MHC-I and II expression on HCC and modulates the immune cell defense in HCC [39]. Accumulating evidence shows that HCC cell lines represent different levels of TGF-β activity (Sk-Hep1 cells with low expression and HepG2 cells with high expression of TGF-β) [42]. Suppression of TGF-β receptors by LY2109761 or SB431542 increases E-cadherin expression, decreases migration, and invasion of HCC [43]. Recently, LY2157299 (Galunisertib) was shown to decrease both the canonical and non-canonical TGF-β pathway in HCC [42]. Galunisertib with Sorafenib has entered into the phase II clinical trial [44]. FGFR or MAPK/ERK inhibitors (such as PD98059) can also be used for inhibition of TGF-β and metastasis in HCC [45]. A combination of TGF-β inhibitor and atezolizumab (a programmed cell death ligand 1 (PD-L1) inhibitor) can overcome the immune escape of HCC [46].
Wnt/B-catenin signaling
In the liver tumor, HCC cells, and macrophages are emerging sources of Wnt ligand [47]. Besides, some of the environmental risk factors cause mutations in different components of the Wnt pathway, leading to overactivation of Wnt signaling in HCC [48, 49]. Binding of Wnt ligand to the Frizzled (Fzd) and low-density lipoprotein receptor-related protein (LRP) receptors causes phosphorylation of the Disheveled [50]. Activated receptors and Disheveled inhibit the destruction of complex proteins (glycogen synthase kinase 3β (GSK3β), axis inhibition protein (Axin), and adenomatous polyposis coli (APC)), thereby causing the release of β-catenin [51, 52]. Activated β-catenin further translocates to the nucleus, binds with other co-activators (like lymphoid enhancer factor (LEF)/ T-cell factor (TCF) proteins or histone acetyltransferase CREB-binding protein (CBP)/p300), and activates the transcription of several target genes [53]. These genes are involved in CSC maintenance (CD44, EpCAM), proliferation (cyclin D1, c-Myc), and EMT [54]. Leucine-rich repeat-containing G (LGR5) is a receptor related to the Wnt/B-catenin pathway and metastasis of HCC [55, 56]. High expression of LGR5 has been found in the PLC and HepG2 lines [57]. Wnt/β-catenin also regulates angiogenesis in the liver tumor [58]. TGF-β, HGF, and environmental cues (such as hypoxia condition) can activate β-catenin [59, 60]. Targeting this pathway at the receptors-ligand level or downstream effectors modulate its activation in HCC [61, 62]. It has been reported that CGP049090 and PKF115-854 can block TCF/LEF/β-catenin interactions [58]. A recent study reported that IC-2 can decrease CSC subpopulation by sphere formation assay [63]. Some of the inhibitors of β-catenin-CBP interaction can induce the differentiation of CSCs [58].
Hedgehog (Hh) signaling
In the liver, hepatocytes and kupffer cells are able to secrete SHH ligands after injury [64, 65]. Hepatitis B virus also activates the SHH pathway [66]. SHH interacts with Patched (Ptch) receptor and triggers Smoothened (Smo) receptor, initiates the signaling cascade, and subsequent nuclear translocation of the transcription factor, and the glioma protein (Gli) [67, 68]. SHH causes the expression of cell cycle-related genes (cyclin D, c-Myc), invasion-related genes (especially MMPs), and CSC-specific genes (like CD133) in HCC [65]. Gli enhances the expression of VEGF in HCC and tumor angiogenesis [69]. SHH can bind to the TGF-β, Wnt, or Notch pathways to promote EMT and metastasis in HCC [65]. Smo and Gli can be increased in several HCC cell lines such as Hep3B, Huh7, Sk-Hep1, and HepG2 [70]. Cyclopamine is a small molecule that inhibits SMO and GANT61 [70–72].
Notch signaling
Activation of the Notch pathway is regulated via the interaction of two receptors on adjacent cells, wherein one of them acts as a ligand (majorly from macrophages) and the other as a receptor, known as the Notch receptor (on hepatocytes) [73, 74]. The intracellular domain (NICD) of the Notch receptor is then cleaved by γ-secretase, which further translocates to the nucleus and binds to the DNA binding transcription factors [75]. The main target genes of the Notch pathway such as Hes1, P53, cyclin-D, and c-Myc control the expression of cancer cell proliferation, invasion, and apoptosis markers [76, 77]. However, it is notable that the Notch pathway has controversial effects on HCC [75]. This pathway crosstalks with the Wnt and SHH pathways for CSC maintenance, the PI3K and mTOR pathways for HCC proliferation, and the VEGF pathway for angiogenesis [78]. The level of the Notch pathway activity in various HCC cell lines depends on their invasion character [79]. For instance, activation of Notch signaling in an invasive MHCC97 cell line is more than the HepG2 cell line [79]. Small molecules like GSI or PF-03084014 (4014) are known to suppress γ-secretase activity [80, 81]. Brivanib is a tyrosine kinase and a Notch3 inhibitor that promotes the intracellular accumulation of P53 protein and enhances HCC apoptosis [82].
Epidermal growth factor (EGF) signaling
The EGF pathway can be abnormally activated in HCC via autocrine or paracrine secretion, which promotes cell proliferation and migration [83]. EGF binds to the EGF receptors and activates PI3K/Akt, MAPK/ERK, P38/MAPK, or NF-kB proteins via a series of downstream signal transduction events [84, 85]. Overexpression and overactivation of EGFR are often observed in HCC [86]. EGF pathway is involved in the recruitment of the inflammatory cells for the secretion of interleukins (IL-1, 6, 8) and tumor progression [87]. U0126 is a small molecule inhibitor of ERK; while BEZ-235 and SHBM1009 are the antagonists of PI3K [87]. EGCG can suppress the EGFR, PI3K/Akt, and MAPK/ERK pathways [88].
Hepatocyte growth factor (HGF) signaling
HGF was found to regulate HCC proliferation, survival, and metastasis [89, 90]. HGF binds to the c-met receptor and activates PI3K, ERK, and Jnk/Stat3 pathways [91]. c-Met inhibitors such as capmatinib and tepotinib have been assessed in liver tumor clinical trials [89, 92]. c-Met is overexpressed in the MHCC97 and HCCLM3 cell lines [89]. It has been confirmed that 3-(1H-benzimidazole-2-methylene)-5-(2-methylphenylaminosulfo)-2-indolone (Indo5), PHA665752, and AMG 337 as selective c-MET inhibitors decrease HCC proliferation, migration, and tumor growth [93–96].
Vascular endothelial growth factor (VEGF) signaling
In order to ensure efficient nutrient and oxygen supply in the solid tumors, the liver tumor cells secrete growth factors that promote angiogenesis [97]. Angiogenic signals can be triggered via several pathways like HGF, PDGF, FGF, and VEGF [98]. VEGF, as the main angiogenic factor, not only induces angiogenesis, but also interacts with RTK in an autocrine manner, and activates PI3K/Akt pathway in HCC [99, 100]. Sorafenib is known to inhibit the VEGF, PDGF, and FGF pathways, thereby suppressing neovasculogeneis in HCC [101, 102]. LY2109761 (TGF-β inhibitor) can suppress VEGF secretion and neovascularization in HCC [103].
Targeting common downstream proteins in HCC
Several growth factors or environmental signaling pathways can activate the common targets in HCC [104, 105]. Signal transducer and activator of transcription 3 (Stat3), Hippo, and HIF are the main downstream proteins that are activated in HCC [106]. Inhibition of these proteins can suppress or weaken the activated signal pathway, thereby modulating the tumorigenicity of HCC [107, 108].
Janus kinases (Jak)/Stat3 signaling
The Jak/Stat3 pathway can be stimulated by inflammatory cytokines (such as interleukins, tumor necrosis factor (TNF), HGF, TGF-β, and EGF) [109, 110]. Stat3 as a transcription factor can promote HCC proliferation, metastasis, tumor survival, and angiogenesis [111]. The Jak inhibitors such as Jaki and S3i-201, or Stat3 inhibitor-related small molecules such as C188-9, ursolic acid (UA), and 2-Ethoxystypandrone can induce apoptosis, cell cycle arrest, and block CSC self-renewal in HCC [112–115].
Hippo signaling
Several growth factors such as Wnt, Notch, EGF, and SHH can activate the YAP (Yes-associated protein) pathway [116, 117]. Activated YAP translocates to the nucleus and interacts with a transcriptional coactivator, PDZ-binding motif (TAZ), and transcriptional enhanced associate domain (TEAD) to promote proliferation, metastasis, and inhibition of apoptosis and autophagy in HCC [118]. YAP or TAZ are highly expressed in HCC cell lines such as HLF and HepG2 and also primary liver tumor samples [119, 120]. Hippo protein activates several kinases and negatively regulates the expression of oncoprotein YAP [121]. Inhibition of YAP/TAZ/TEAD transcriptional activity is often used for anti-cancer treatment [122–124]. Verteporfin is a small molecule that inhibits YAP/TEAD complex interaction [125].
Hypoxia signaling
It has been confirmed that HCC cells rapidly use environmental oxygen [126]. In the center of the liver tumor, hypoxic conditions activate major transcription factors and inducing factors such as HIF-1A, HIF-2A [127]. HIF induces the expression of TGF-β and Snail and enhances EMT in tumor cells [126]. HIF via MMP expression helps in ECM remodeling and tumor cell invasion [128]. It also increases c-Myc expression, HCC proliferation, and escape of HCC from the immune destruction [129]. HIF also inhibits P53 (a tumor suppressor gene), enhances the activity of anti-apoptotic proteins (like Bcl-2, caspases), and prevents HCC apoptosis [126]. HIF-1A promotes CSCs maintenance in liver tumors [130]. HSP90, a general oncogene protein, stabilizes HIF-1A and positively modulates the survival, growth, and metastasis of the tumor cells [131]. Under hypoxia conditions, the cells transition from aerobic to anaerobic metabolism [132]. HIF-1A promotes glycolysis metabolism and increases lactate production in HCC [133]. The components of this pathway also interact with other pathways to promote tumorigenicity [134]. HIF-1A impacts on downstream signal transduction and increases VEGF expression and angiogenesis in HCC [98]. HIF-1A also stimulates TGF-β interaction with its receptors, enhances HCC survival, and proliferation [128]. Hypoxia activates the expression of Notch downstream genes and recruits HIF-1A for HCC metastasis [130]. Recent studies have suggested that hypoxia can regulate the Hh pathway [130]. The Wnt pathway also increases the expression of HIF-1A in HCC [130]. YAP interacts and stabilizes HIF-1A in HCC [135]. HIF-1A regulates the metabolism of HCC, increases the expression of glycolysis enzymes and glucose uptake receptors for adaptation to the hypoxic condition [130]. Besides, HIF-1A changes the activity of the macrophages and hepatic stellate cells (HSC) to promote HCC survival, growth, and angiogenesis [130]. PT2385 as a small molecule can suppress HIF-activated proteins such as Stat3, VEGF, PDGF, and ERK [136].
Cell division signaling
Uncontrolled cell cycle program and telomerase activity in the hepatocytes increase carcinogenesis [137]. The cell cycle is regulated by cyclin-dependent kinases (CDK)/Cyclin complex at different stages [138]. Downstream of signaling pathways such as EGF, TGF-β, TNF, and IL6 can stimulate CDK/CyclinD complex and phosphorylated retinoblastoma (pRb) to promote HCC proliferation [139]. P53, an anti-proliferation protein, activates P16, P21, and P27 tumor suppressor proteins at the G1 phase, thereby hindering the pRb and CDK/Cyclin proteins [140]. Notably, P21 via inhibition of procaspase 3 has contradictory effects in cancers [141]. Normal hepatocytes have a cell cycle arrest in the G0 phase; however, in the case of HCC, P21, and P27 are usually degraded [142]. Mutations of β-catenin or P53 lead to sustain expression of c-Myc, misregulation of PI3K and ERK pathways, and uncontrolled cell cycle progression in HCC [138].
In this regard, Dinaciclib and Ribociclib are CDK/pRb inhibitors that upregulate P53 to control HCC proliferation [143, 144].
Apoptosis signaling
Targeted activation of the apoptosis pathway in cancer cells is another crucial way in cancer therapy [145, 146]. In normal cells, apoptosis may initiate via the extrinsic (owing to the attachment of external ligands to the receptors) or intrinsic (owing to mitochondrial factors) pathways [147]. Cellular FlICE/caspase-8-inhibitory protein (cFLIP) and Bcl-2 are negative regulators of the apoptosis pathway, while PPARγ acts as an apoptosis inducer [148, 149].
The extrinsic pathway is activated when immune cells secrete TNF-related apoptosis-inducing ligand (TRAIL) that binds to death receptors (DR) on the cell surface [150]. This cascade causes the recruitment of a complex of FAAD-procaspase 8 (DISC complex), and subsequent activation of caspase 8 (an endonuclease and protease), leading to apoptosis [148]. The proteasome complex causes the degradation of tumor suppressor proteins and activation of NF-kB and c-FLIP, thereby promoting the survival and proliferation of HCC [148]. Additionally, NF-kB regulates MMP9 expression and HCC metastasis [151]. On the other hand, in the intrinsic apoptosis pathway, DNA damage in the cells activates P53 protein, triggers the activation of Bax, and mitochondria-mediated caspase activity [152]. P53 is crucial for cell cycle arrest, cell senescence, and cell autophagy [153, 154]. In HCC, mutations or deletion in the P53 gene or increase of its inhibitors such as a ubiquitin ligase DM2 (Double Minute 2) obligate the apoptosis pathway [155]. Snail inhibits the TRAIL pathway and P53 in cancer cells [156] HCC cell lines express P53 at different levels. For instance, Hep3B, HepG2, and Huh7 have no, normal, and high levels of P53, respectively [157]. PPARγ also positively modulates the components of these pathways and inhibits HCC survival [158]. The strategies that upregulate TRAIL receptors or ligands (via recombinant protein or agonist receptor antibodies) were shown to cause selective apoptosis in HCC cell lines [159, 160]. Co-treatment of HCC cell lines with recombinant TRAIL and Bortezomib (as proteasome inhibitors) increased the apoptosis induction in the Huh7 cells, compared to the primary hepatocytes [159]. Nutlin, an inhibitor of DM, was reported to stabilize P53 and decrease Bcl-2 expression [161]. Rubone can downregulate the expression of Notch, cyclin D1, Bcl-2, while increase P53 level in HCC [162].
Autophagy signaling
Autophagy, a type II cell death, is lysosome-dependent and initiated by surrounding the intracellular organelle with a double membrane (autophagosome) and self-degradation of cells [163]. ATG7, LC3, and beclin are the major proteins involved in this process [164]. Depends on the stage of cancer, autophagy either negatively or positively regulates cancer progression [165, 166]. In HCC late stages, autophagy promotes survival, metastasis, and EMT via activation of the TGFβ pathway, P53 degradation, and chemotherapy resistance of HCC [167]. Inhibitors of main signaling pathways such as PI3K/Akt, MAPK/ERK, and JAK/Stat3 can induce autophagy and cell death in HCC [168, 169]. Small molecules like rapamycin, Mitoxantrone (PI3K/mTOR inhibitors), and Erlotinib/Cetuximab (EGFR inhibitors) are thought to activate cellular autophagy and apoptosis in various HCC cell lines [167, 170]. Tumstatin was previously shown to increase the expression of Bax, Fas, and Fasl to induce apoptosis and autophagy in HCC [171]. However, some studies have found that the suppression of autophagy via 3-MA leads to inhibit HCC growth [167, 172]. Verteporfin, mitoxantrone, and NVP-BGT226 are small molecules that trigger autophagy in HCC [170, 173, 174].
Oxidative stress signaling
Both the intrinsic and extrinsic apoptotic pathways affect the mitochondrial respiratory chain and cause the generation of reactive oxygen species (ROS) in the cells [152, 175]. In cancer cells, ROS may play as a double-edged sword in the induction or suppression of tumor growth in a concentration-dependent manner [176]. A low level of ROS is normal in all the cell types, while its moderate level leads to promote cancer development [176]. ROS, via activation of the TGF-β pathway along with an increase in MMP expression, causes EMT, metastasis, and invasion of cancer cells [176]. ROS can stimulate VEGF or the hypoxia pathway to promote angiogenesis in HCC [177, 178] and mediates cell cycle activation and CSC maintenance in cancer [179]. ROS-mediated signaling events mediate chemoresistance to the cancer cells [180]. Though, excessive ROS can disrupt the proteins in mitochondria and promote the DNA mutations, causing the release of pro-apoptotic factors into the cytoplasm of the cancer cells [178]. Accordingly, agents that restore the intracellular REDOX balance or elevate the ROS content cannot be useful in cancer treatment [181, 182]. In this regard, vitamin C as a natural antioxidant can increase ROS production in HCC and stimulate apoptosis, cell cycle arrest, and suppress CSC self-renewal [183]. Auranofin, a thioredoxin reductase (TXNRD) inhibitor, increases ROS in HCC and suppresses both the extrinsic and intrinsic apoptotic pathways [184]. Morin, a flavonoid from Ficus carica, in combination with Auranofin caused apoptosis in HCC [185]. Propyl gallate (PG), a synthetic antioxidant, activates superoxidase and ROS formation in HCC, thereby causing autophagy and apoptosis [186]. N-acetylcysteine (NAC) acts as a potent ROS inhibitor [187]. ART, a YAP inhibitor, promotes ROS formation in HCC [188].
Conclusion and perspective
Several important signaling pathways such as TGF-β, Wnt, SHH, Notch, and RTK are misregulated in HCC, compared to the normal hepatocytes. These pathways initiate differential networks that consequently result in HCC cell cycle promotion, EMT, metastasis, vasculogenesis, and anti-apoptotic mechanisms. Suppression of these pathways with small molecules, herbal drugs, and miRNA stimulates cell cycle arrest, apoptosis, and inhibits the invasion of HCC [189, 190]. Simultaneously targeting different signaling pathways or common downstream proteins would facilitate control over malignant HCC. Induction of differentiation in transformed mesenchymal HCC to the epithelial state would also help in regulating the tumorigenesis of HCC. Smart delivery of anti-cancer agents to the liver tumor could facilitate the targeted therapy in this solid tumor.
Acknowledgements
Not applicable.
Abbreviations
- APC
Adenomatous polyposis coli
- CAF
Cancer-associated fibroblast
- CBP
CREB-binding protein
- CDK
Cyclin-dependent kinases
- Cflip
Cellular FlICE/caspase-8-inhibitory protein
- DM2
Double Minute 2
- DR
Death receptors
- HSC
Hepatic stellate cells
- ROS
Reactive oxygen species
- EGF
Epidermal growth factor
- EMT
Epithelial-to-mesenchymal transition
- Fzd
Frizzled
- Gli
Glioma protein
- GSK3β
Glycogen synthase kinase 3β
- HGF
Hepatocyte growth factor
- HCC
Hepatocellular carcinoma
- Hh
Hedgehog
- Indo5
3-(1H-benzimidazole-2-methylene)-5 (2methylphenylaminosulfo)-2-indolone
- Jak
Janus kinases
- LEF
Lymphoid enhancer factor
- LGR5
Leucine-rich repeat-containing G
- LRP
Lipoprotein receptor-related protein
- MMPs
Matrix metalloproteinases
- PD-L1
Programmed cell death ligand 1
- PRb
Phosphorylated retinoblastoma
- Ptch
Patched
- Smo
Smoothened
- TAM
Tumor-associated macrophages
- TCF
T-cell factor
- TEAD
Transcriptional enhanced associate domain
- TGF-β
Transforming growth factor-β
- TME
Tumor microenvironment
- TRAIL
TNF-related apoptosis-inducing ligand
- TXNRD
Thioredoxin reductase
- UA
Ursolic acid
- VEGF
Vascular endothelial growth factor
- YAP
Yes-associated protein
Authors’ contributions
ZF has been involved in drafting the manuscript. MV and TA have made substantial contributions to the revising of the manuscript. MF has made a substantial contribution to the writing and revising of the manuscript and the design of the Figures. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zahra Farzaneh, Email: zahrafarzaneh@royaninstitute.org.
Maryam Farzaneh, Email: Khoshnam.e@ajums.ac.ir.
References
- 1.Chen S, Cao Q, Wen W, Wang H. Targeted therapy for hepatocellular carcinoma: Challenges and opportunities. Cancer Lett. 2019;460:1–9. doi: 10.1016/j.canlet.2019.114428. [DOI] [PubMed] [Google Scholar]
- 2.Balogh J, Victor D, 3rd, Asham EH, Burroughs SG, Boktour M, Saharia A, Li X, Ghobrial RM, Monsour HP., Jr Hepatocellular carcinoma: a review. J Hepatocell Carcinoma. 2016;3:41–53. doi: 10.2147/JHC.S61146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iida-Ueno A, Enomoto M, Tamori A, Kawada N. Hepatitis B virus infection and alcohol consumption. World J Gastroenterol. 2017;23:2651–2659. doi: 10.3748/wjg.v23.i15.2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Midorikawa Y, Takayama T, Nakayama H, Higaki T, Moriguchi M, Moriya K, Kanda T, Matsuoka S, Moriyama M. Prior hepatitis B virus infection as a co-factor of chronic hepatitis C patient survival after resection of hepatocellular carcinoma. BMC Gastroenterol. 2019;19:147. doi: 10.1186/s12876-019-1069-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li W, Deng R, Liu S, Wang K, Sun J. Hepatitis B virus-related hepatocellular carcinoma in the era of antiviral therapy: The emerging role of non-viral risk factors. Liver Int. 2020;40:2316–2325. doi: 10.1111/liv.14607. [DOI] [PubMed] [Google Scholar]
- 6.Kumari R, Sahu MK, Tripathy A, Uthansingh K, Behera M. Hepatocellular carcinoma treatment: hurdles, advances and prospects. Hepat Oncol. 2018;5:HEP08. doi: 10.2217/hep-2018-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raza A, Sood GK. Hepatocellular carcinoma review: current treatment, and evidence-based medicine. World J Gastroenterol. 2014;20:4115–4127. doi: 10.3748/wjg.v20.i15.4115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen CP. Role of radiotherapy in the treatment of hepatocellular carcinoma. J Clin Transl Hepatol. 2019;7:183–190. doi: 10.14218/JCTH.2018.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gallicchio R, Nardelli A, Mainenti P, Nappi A, Capacchione D, Simeon V, Sirignano C, Abbruzzi F, Barbato F, Landriscina M, Storto G. Therapeutic strategies in HCC: radiation modalities. Biomed Res Int. 2016;2016:1295329. doi: 10.1155/2016/1295329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin Y-L, Li Y. Study on the hepatocellular carcinoma model with metastasis. Genes Dis. 2020;7:336–350. doi: 10.1016/j.gendis.2019.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daher S, Massarwa M, Benson AA, Khoury T. Current and future treatment of hepatocellular carcinoma: an updated comprehensive review. J Clin Transl Hepatol. 2018;6:69–78. doi: 10.14218/JCTH.2017.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swamy SG, Kameshwar VH, Shubha PB, Looi CY, Shanmugam MK, Arfuso F, Dharmarajan A, Sethi G, Shivananju NS, Bishayee A. Targeting multiple oncogenic pathways for the treatment of hepatocellular carcinoma. Target Oncol. 2017;12:1–10. doi: 10.1007/s11523-016-0452-7. [DOI] [PubMed] [Google Scholar]
- 13.Alqahtani A, Khan Z, Alloghbi A, Said Ahmed TS, Ashraf M, Hammouda DM. Hepatocellular carcinoma: molecular mechanisms and targeted therapies. Medicina (Kaunas) 2019;55:526. doi: 10.3390/medicina55090526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lachenmayer A, Alsinet C, Chang CY, Llovet JM. Molecular approaches to treatment of hepatocellular carcinoma. Dig Liver Dis. 2010;42(Suppl 3):S264–272. doi: 10.1016/S1590-8658(10)60515-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dimri M, Satyanarayana A. Molecular signaling pathways and therapeutic targets in hepatocellular carcinoma. Cancers (Basel) 2020;12:491. doi: 10.3390/cancers12020491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma Y-S, Liu J-B, Wu T-M, Fu D. New therapeutic options for advanced hepatocellular carcinoma. Cancer Control. 2020;27:1073274820945975. doi: 10.1177/1073274820945975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xie J, Zhang A, Wang X. Metabolomic applications in hepatocellular carcinoma: toward the exploration of therapeutics and diagnosis through small molecules. RSC Adv. 2017;7:17217–17226. doi: 10.1039/C7RA00698E. [DOI] [Google Scholar]
- 18.Wei Q, Qian Y, Yu J, Wong CC. Metabolic rewiring in the promotion of cancer metastasis: mechanisms and therapeutic implications. Oncogene. 2020;39:6139–6156. doi: 10.1038/s41388-020-01432-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ren T, Zhu L, Cheng M. CXCL10 accelerates EMT and metastasis by MMP-2 in hepatocellular carcinoma. Am J Transl Res. 2017;9(6):2824–2837. [PMC free article] [PubMed] [Google Scholar]
- 20.Tummala KS, Brandt M, Teijeiro A, Graña O, Schwabe RF, Perna C, Djouder N. Hepatocellular carcinomas originate predominantly from hepatocytes and benign lesions from hepatic progenitor cells. Cell Rep. 2017;19:584–600. doi: 10.1016/j.celrep.2017.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mu X, Español-Suñer R, Mederacke I, Affò S, Manco R, Sempoux C, Lemaigre FP, Adili A, Yuan D, Weber A, Unger K, Heikenwälder M, Leclercq IA, Schwabe RF. Hepatocellular carcinoma originates from hepatocytes and not from the progenitor/biliary compartment. J Clin Invest. 2015;125:3891–3903. doi: 10.1172/JCI77995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Villanueva A, Newell P, Chiang DY, Friedman SL, Llovet JM. Genomics and signaling pathways in hepatocellular carcinoma. Semin Liver Dis. 2007;27:55–76. doi: 10.1055/s-2006-960171. [DOI] [PubMed] [Google Scholar]
- 23.Yu L-X, Ling Y, Wang H-Y. Role of nonresolving inflammation in hepatocellular carcinoma development and progression. NPJ Precis Oncol. 2018;2(1):1–10. doi: 10.1038/s41698-017-0044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hernandez-Gea V, Toffanin S, Friedman SL, Llovet JM. Role of the microenvironment in the pathogenesis and treatment of hepatocellular carcinoma. Gastroenterology. 2013;144:512–527. doi: 10.1053/j.gastro.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Toh TB, Lim JJ, Chow EK-H. Epigenetics of hepatocellular carcinoma. Clin Transl Med. 2019;8:13–13. doi: 10.1186/s40169-019-0230-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chao J, Zhao S, Sun H. Dedifferentiation of hepatocellular carcinoma: molecular mechanisms and therapeutic implications. Am J Transl Res. 2020;12:2099–2109. [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwal T, Subramanian B, Maiti TK. Liver tissue engineering: challenges and opportunities. ACS Biomater Sci Eng. 2019;5:4167–4182. doi: 10.1021/acsbiomaterials.9b00745. [DOI] [PubMed] [Google Scholar]
- 28.Loh C-Y, Chai JY, Tang TF, Wong WF, Sethi G, Shanmugam MK, Chong PP, Looi CY. The E-cadherin and N-cadherin switch in epithelial-to-mesenchymal transition: signaling, therapeutic implications, and challenges. Cells. 2019;8:1118. doi: 10.3390/cells8101118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giannelli G, Koudelkova P, Dituri F, Mikulits W. Role of epithelial to mesenchymal transition in hepatocellular carcinoma. J Hepatol. 2016;65:798–808. doi: 10.1016/j.jhep.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Scheau C, Badarau IA, Costache R, Caruntu C, Mihai GL, Didilescu AC, Constantin C, Neagu M. The role of matrix metalloproteinases in the epithelial-mesenchymal transition of hepatocellular carcinoma. Anal Cell Pathol (Amst) 2019;2019:9423907. doi: 10.1155/2019/9423907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nault J-C, Ningarhari M, Rebouissou S, Zucman-Rossi J. The role of telomeres and telomerase in cirrhosis and liver cancer. Nat Rev Gastroenterol Hepatol. 2019;16:544–558. doi: 10.1038/s41575-019-0165-3. [DOI] [PubMed] [Google Scholar]
- 32.Hong M, Almutairi MM, Li S, Li J. Wogonin inhibits cell cycle progression by activating the glycogen synthase kinase-3 beta in hepatocellular carcinoma. Phytomedicine. 2020;68:153174. doi: 10.1016/j.phymed.2020.153174. [DOI] [PubMed] [Google Scholar]
- 33.Llovet JM, Bruix J. Molecular targeted therapies in hepatocellular carcinoma. Hepatology. 2008;48:1312–1327. doi: 10.1002/hep.22506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cicchini C, Amicone L, Alonzi T, Marchetti A, Mancone C, Tripodi M. Molecular mechanisms controlling the phenotype and the EMT/MET dynamics of hepatocyte. Liver Int. 2015;35:302–310. doi: 10.1111/liv.12577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonzalez DM, Medici D. Signaling mechanisms of the epithelial-mesenchymal transition. Sci Signal. 2014;7:re8. doi: 10.1126/scisignal.2005189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang J, Gu C, Song Q, Zhu M, Xu Y, Xiao M, Zheng W. Identifying cancer-associated fibroblasts as emerging targets for hepatocellular carcinoma. Cell Biosci. 2020;10:127. doi: 10.1186/s13578-020-00488-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hata A, Chen Y-G. TGF-β signaling from receptors to Smads. Cold Spring Harb Perspect Biol. 2016;8:a022061. doi: 10.1101/cshperspect.a022061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fabregat I, Caballero-Diaz D. Transforming growth factor-beta-induced cell plasticity in liver fibrosis and hepatocarcinogenesis. Front Oncol. 2018;8:357. doi: 10.3389/fonc.2018.00357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krstic J, Trivanovic D, Mojsilovic S, Santibanez JF. Transforming growth factor-beta and oxidative stress interplay: implications in tumorigenesis and cancer progression. Oxid Med Cell Longev. 2015;2015:654594. doi: 10.1155/2015/654594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mancarella S, Krol S, Crovace A, Leporatti S, Dituri F, Frusciante M, Giannelli G. Validation of hepatocellular carcinoma experimental models for TGF-β promoting tumor progression. Cancers (Basel) 2019;11:1510. doi: 10.3390/cancers11101510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Steinway SN, Zanudo JG, Ding W, Rountree CB, Feith DJ, Loughran Albert TPR., Jr Network modeling of TGFbeta signaling in hepatocellular carcinoma epithelial-to-mesenchymal transition reveals joint sonic hedgehog and Wnt pathway activation. Cancer Res. 2014;74:5963–5977. doi: 10.1158/0008-5472.CAN-14-0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Serova M, Tijeras-Raballand A, Dos Santos C, Albuquerque M, Paradis V, Neuzillet C, Benhadji KA, Raymond E, Faivre S, de Gramont A. Effects of TGF-beta signalling inhibition with galunisertib (LY2157299) in hepatocellular carcinoma models and in ex vivo whole tumor tissue samples from patients. Oncotarget. 2015;6:21614–21627. doi: 10.18632/oncotarget.4308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fransvea E, Angelotti U, Antonaci S, Giannelli G. Blocking transforming growth factor-beta up-regulates E-cadherin and reduces migration and invasion of hepatocellular carcinoma cells. Hepatology. 2008;47:1557–1566. doi: 10.1002/hep.22201. [DOI] [PubMed] [Google Scholar]
- 44.Kelley RK, Gane E, Assenat E, Siebler J, Galle PR, Merle P, Hourmand IO, Cleverly A, Zhao Y, Gueorguieva I, Lahn M, Faivre S, Benhadji KA, Giannelli G. A phase 2 study of galunisertib (TGF-beta1 receptor type I inhibitor) and sorafenib in patients with advanced hepatocellular carcinoma. Clin Transl Gastroenterol. 2019;10:e00056. doi: 10.14309/ctg.0000000000000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang J, Qiu M, Wan L, Wang G, Huang T, Chen Z, Jiang S, Li X, Xie L, Cai L. TGF-beta1 promotes hepatocellular carcinoma invasion and metastasis via ERK pathway-mediated FGFR4 expression. Cell Physiol Biochem. 2018;45:1690–1699. doi: 10.1159/000487737. [DOI] [PubMed] [Google Scholar]
- 46.Chen J, Gingold JA, Su X. Immunomodulatory TGF-beta signaling in hepatocellular carcinoma. Trends Mol Med. 2019;25:1010–1023. doi: 10.1016/j.molmed.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 47.Yang Y, Ye Y-C, Chen Y, Zhao J-L, Gao C-C, Han H, Liu W-C, Qin H-Y. Crosstalk between hepatic tumor cells and macrophages via Wnt/β-catenin signaling promotes M2-like macrophage polarization and reinforces tumor malignant behaviors. Cell Death Dis. 2018;9:793–793. doi: 10.1038/s41419-018-0818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang W, Smits R, Hao H, He C. Wnt/beta-catenin signaling in liver cancers. Cancers (Basel) 2019;11:926. doi: 10.3390/cancers11070926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu W, Zhou W, Cheng M, Wang J, Liu Z, He S, Luo X, Huang W, Chen T, Yan W, Xiao J. Hypoxia activates Wnt/beta-catenin signaling by regulating the expression of BCL9 in human hepatocellular carcinoma. Sci Rep. 2017;7:40446. doi: 10.1038/srep40446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jung Y-S, Park J-I. Wnt signaling in cancer: therapeutic targeting of Wnt signaling beyond β-catenin and the destruction complex. Exp Mol Med. 2020;52(2):183–191. doi: 10.1038/s12276-020-0380-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stamos JL, Weis WI. The β-catenin destruction complex. Cold Spring Harb Perspect Biol. 2013;5:a007898–a007898. doi: 10.1101/cshperspect.a007898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu C, Takada K, Zhu D. Targeting Wnt/β-catenin pathway for drug therapy. Med Drug Discov. 2020;8:100066. doi: 10.1016/j.medidd.2020.100066. [DOI] [Google Scholar]
- 53.Wang W, Smits R, Hao H, He C. Wnt/β-catenin signaling in liver cancers. Cancers. 2019;11:926. doi: 10.3390/cancers11070926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhan T, Rindtorff N, Boutros M. Wnt signaling in cancer. Oncogene. 2017;36:1461–1473. doi: 10.1038/onc.2016.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma Z, Guo D, Wang Q, Liu P, Xiao Y, Wu P, Wang Y, Chen B, Liu Z, Liu Q. Lgr5-mediated p53 Repression through PDCD5 leads to doxorubicin resistance in Hepatocellular Carcinoma. Theranostics. 2019;9:2967. doi: 10.7150/thno.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Koni M, Pinnarò V, Brizzi MF. The Wnt signalling pathway: a tailored target in cancer. Int J Mol Sci. 2020;21:7697. doi: 10.3390/ijms21207697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Effendi K, Yamazaki K, Fukuma M, Sakamoto M. Overexpression of leucine-rich repeat-containing G protein-coupled receptor 5 (LGR5) represents a typical Wnt/beta-catenin pathway-activated hepatocellular carcinoma. Liver Cancer. 2014;3:451–457. doi: 10.1159/000343873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vilchez V, Turcios L, Marti F, Gedaly R. Targeting Wnt/beta-catenin pathway in hepatocellular carcinoma treatment. World J Gastroenterol. 2016;22:823–832. doi: 10.3748/wjg.v22.i2.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zheng J-J, Que Q-Y, Xu H-T. Hypoxia activates SOX5/Wnt/β-catenin signaling by suppressing MiR-338–3p in gastric cancer. Technol Cancer Res Treat. 2020;19:1533033820905825. doi: 10.1177/1533033820905825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Han Z, Li Y, Yang B, Tan R, Wang M, Zhang B, Dai C, Wei L, Chen D, Chen Z. Agmatine attenuates liver ischemia reperfusion injury by activating Wnt/β-catenin signaling in mice. Transplantation. 2020;104(9):1906–1916. doi: 10.1097/TP.0000000000003161. [DOI] [PubMed] [Google Scholar]
- 61.Yuan K, Xie K, Lan T, Xu L, Chen X, Li X, Liao M, Li J, Huang J, Zeng Y. TXNDC12 promotes EMT and metastasis of hepatocellular carcinoma cells via activation of β-catenin. Cell Death Differ. 2020;27:1355–1368. doi: 10.1038/s41418-019-0421-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hou J, Zhao N, Zhu P, Chang J, Du Y, Shen W. Irradiated mesenchymal stem cells support stemness maintenance of hepatocellular carcinoma stem cells through Wnt/β-catenin signaling pathway. Cell Biosci. 2020;10:1–7. doi: 10.1186/s13578-020-00449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Seto K, Sakabe T, Itaba N, Azumi J, Oka H, Morimoto M, Umekita Y, Shiota G. A novel small-molecule WNT inhibitor, IC-2, has the potential to suppress liver cancer stem cells. Anticancer Res. 2017;37:3569–3579. doi: 10.21873/anticanres.11727. [DOI] [PubMed] [Google Scholar]
- 64.Shen X, Peng Y, Li H. The injury-related activation of hedgehog signaling pathway modulates the repair-associated inflammation in liver fibrosis. Front Immunol. 2017;8:1450–1450. doi: 10.3389/fimmu.2017.01450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jeng KS, Jeng CJ, Jeng WJ, Sheen I, Li SY, Leu CM, Tsay YG, Chang CF. Sonic Hedgehog signaling pathway as a potential target to inhibit the progression of hepatocellular carcinoma. Oncol Lett. 2019;18:4377–4384. doi: 10.3892/ol.2019.10826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li Y, Jiang M, Li M, Chen Y, Wei C, Peng L, Liu X, Liu Z, Tong G, Zhou D, He J. Compound phyllanthus urinaria L inhibits HBV-related HCC through HBx-SHH pathway axis inactivation. Evid Based Complement Alternat Med. 2019;2019:1635837. doi: 10.1155/2019/1635837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Skoda AM, Simovic D, Karin V, Kardum V, Vranic S, Serman L. The role of the Hedgehog signaling pathway in cancer: a comprehensive review. Bosn J Basic Med Sci. 2018;18:8–20. doi: 10.17305/bjbms.2018.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Quijada L, Callejo A, Torroja C, Guerrero I. The patched receptor: Switching on/off the Hedgehog signaling pathway. Hedgehog-Gli signaling in human disease. 2013;23:12–33.
- 69.Pinter M, Sieghart W, Schmid M, Dauser B, Prager G, Dienes HP, Trauner M, Peck-Radosavljevic M. Hedgehog inhibition reduces angiogenesis by downregulation of tumoral VEGF-A expression in hepatocellular carcinoma. United European Gastroenterol J. 2013;1:265–275. doi: 10.1177/2050640613496605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Patil MA, Zhang J, Ho C, Cheung ST, Fan ST, Chen X. Hedgehog signaling in human hepatocellular carcinoma. Cancer Biol Ther. 2006;5:111–117. doi: 10.4161/cbt.5.1.2379. [DOI] [PubMed] [Google Scholar]
- 71.Wang Y, Han C, Lu L, Magliato S, Wu T. Hedgehog signaling pathway regulates autophagy in human hepatocellular carcinoma cells. Hepatology. 2013;58:995–1010. doi: 10.1002/hep.26394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen XL, Cheng QY, She MR, Wang Q, Huang XH, Cao LQ, Fu XH, Chen JS. Expression of sonic hedgehog signaling components in hepatocellular carcinoma and cyclopamine-induced apoptosis through Bcl-2 downregulation in vitro. Arch Med Res. 2010;41:315–323. doi: 10.1016/j.arcmed.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 73.Steinbuck MP, Winandy S. A review of notch processing with new insights into ligand-independent notch signaling in T-cells. Front Immunol. 2018;9:1230–1230. doi: 10.3389/fimmu.2018.01230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Anna B, Lluis E. Notch Signaling in Cell-Cell Communication Pathways. Current Stem Cell Reports. 2016;2:349–355. doi: 10.1007/s40778-016-0065-1. [DOI] [Google Scholar]
- 75.Huang Q, Li J, Zheng J, Wei A. The carcinogenic role of the notch signaling pathway in the development of hepatocellular carcinoma. J Cancer. 2019;10:1570–1579. doi: 10.7150/jca.26847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dotto GP. Crosstalk of notch with p53 and p63 in cancer growth control. Nat Rev Cancer. 2009;9:587–595. doi: 10.1038/nrc2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dai M-Y, Fang F, Zou Y, Yi X, Ding Y-J, Chen C, Tao Z-Z, Chen S-M. Downregulation of Notch1 induces apoptosis and inhibits cell proliferation and metastasis in laryngeal squamous cell carcinoma. Oncol Rep. 2015;34:3111–3119. doi: 10.3892/or.2015.4274. [DOI] [PubMed] [Google Scholar]
- 78.Giovannini C, Bolondi L, Gramantieri L. Targeting notch3 in hepatocellular carcinoma: molecular mechanisms and therapeutic perspectives. Int J Mol Sci. 2016;18:56. doi: 10.3390/ijms18010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhou L, Wang DS, Li QJ, Sun W, Zhang Y, Dou KF. Downregulation of the Notch signaling pathway inhibits hepatocellular carcinoma cell invasion by inactivation of matrix metalloproteinase-2 and -9 and vascular endothelial growth factor. Oncol Rep. 2012;28:874–882. doi: 10.3892/or.2012.1880. [DOI] [PubMed] [Google Scholar]
- 80.Wu CX, Xu A, Zhang CC, Olson P, Chen L, Lee TK, Cheung TT, Lo CM, Wang XQ. Notch inhibitor PF-03084014 inhibits hepatocellular carcinoma growth and metastasis via suppression of cancer stemness due to reduced activation of Notch1-Stat3. Mol Cancer Ther. 2017;16:1531–1543. doi: 10.1158/1535-7163.MCT-17-0001. [DOI] [PubMed] [Google Scholar]
- 81.Shen Y, Yin Y, Peng Y, Lv D, Miao F, Dou F, Zhang J. Modulation of the gamma-secretase activity as a therapy against human hepatocellular carcinoma. J Cancer Res Ther. 2018;14:S473–S479. doi: 10.4103/0973-1482.174542. [DOI] [PubMed] [Google Scholar]
- 82.Giovannini C, Salzano AM, Baglioni M, Vitale M, Scaloni A, Zambrano N, Giannone FA, Vasuri F, D'Errico A, Svegliati Baroni G, Bolondi L, Gramantieri L. Brivanib in combination with Notch3 silencing shows potent activity in tumour models. Br J Cancer. 2019;120:601–611. doi: 10.1038/s41416-018-0375-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liu Z, Chen D, Ning F, Du J, Wang H. EGF is highly expressed in hepatocellular carcinoma (HCC) and promotes motility of HCC cells via fibronectin. J Cell Biochem. 2018;119:4170–4183. doi: 10.1002/jcb.26625. [DOI] [PubMed] [Google Scholar]
- 84.Peng Q, Deng Z, Pan H, Gu L, Liu O, Tang Z. Mitogen-activated protein kinase signaling pathway in oral cancer. Oncol Lett. 2018;15:1379–1388. doi: 10.3892/ol.2017.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cargnello M, Roux PP. Activation and function of the MAPKs and their substrates, the MAPK-activated protein kinases. Microbiol Mol Biol Rev. 2011;75:50–83. doi: 10.1128/MMBR.00031-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Komposch K, Sibilia M. EGFR signaling in liver diseases. Int J Mol Sci. 2015;17:30. doi: 10.3390/ijms17010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang P, Xu X, Wang L, Zhu B, Wang X, Xia J. The role of EGF-EGFR signalling pathway in hepatocellular carcinoma inflammatory microenvironment. J Cell Mol Med. 2014;18:218–230. doi: 10.1111/jcmm.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen J, Chen L, Lu T, Xie Y, Li C, Jia Z, Cao J. ERalpha36 is an effective target of epigallocatechin-3-gallate in hepatocellular carcinoma. Int J Clin Exp Pathol. 2019;12:3222–3234. [PMC free article] [PubMed] [Google Scholar]
- 89.Wang H, Rao B, Lou J, Li J, Liu Z, Li A, Cui G, Ren Z, Yu Z. The Function of the HGF/c-met axis in hepatocellular carcinoma. Front Cell Dev Biol. 2020;8:55–55. doi: 10.3389/fcell.2020.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.García-Vilas JA, Medina MÁ. Updates on the hepatocyte growth factor/c-Met axis in hepatocellular carcinoma and its therapeutic implications. World J Gastroenterol. 2018;24:3695–3708. doi: 10.3748/wjg.v24.i33.3695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang Y, Xia M, Jin K, Wang S, Wei H, Fan C, Wu Y, Li X, Li X, Li G, Zeng Z, Xiong W. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol Cancer. 2018;17:45–45. doi: 10.1186/s12943-018-0796-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bouattour M, Raymond E, Qin S, Cheng AL, Stammberger U, Locatelli G, Faivre S. Recent developments of c-Met as a therapeutic target in hepatocellular carcinoma. Hepatology. 2018;67:1132–1149. doi: 10.1002/hep.29496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.You H, Ding W, Dang H, Jiang Y, Rountree CB. c-Met represents a potential therapeutic target for personalized treatment in hepatocellular carcinoma. Hepatology. 2011;54:879–889. doi: 10.1002/hep.24450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Luo T, Zhang SG, Zhu LF, Zhang FX, Li W, Zhao K, Wen XX, Yu M, Zhan YQ, Chen H, Ge CH, Gao HY, Wang L, Yang XM, Li CY. A selective c-Met and Trks inhibitor Indo5 suppresses hepatocellular carcinoma growth. J Exp Clin Cancer Res. 2019;38:130. doi: 10.1186/s13046-019-1104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Du Z, Caenepeel S, Shen Y, Rex K, Zhang Y, He Y, Tang ET, Wang O, Zhong W, Zhou H, Huang J, Huang E, Hu L, Coxon A, Zhang M. Preclinical Evaluation of AMG 337, a highly selective small molecule MET inhibitor, in hepatocellular carcinoma. Mol Cancer Ther. 2016;15:1227–1237. doi: 10.1158/1535-7163.MCT-15-0745. [DOI] [PubMed] [Google Scholar]
- 96.Korhan P, Erdal E, Atabey N. miR-181a-5p is downregulated in hepatocellular carcinoma and suppresses motility, invasion and branching-morphogenesis by directly targeting c-Me. Biochem Biophys Res Commun. 2014;450:1304–1312. doi: 10.1016/j.bbrc.2014.06.142. [DOI] [PubMed] [Google Scholar]
- 97.Lugano R, Ramachandran M, Dimberg A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell Mol Life Sci. 2020;77:1745–1770. doi: 10.1007/s00018-019-03351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Semela D, Dufour JF. Angiogenesis and hepatocellular carcinoma. J Hepatol. 2004;41:864–880. doi: 10.1016/j.jhep.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 99.Mathonnet M, Descottes B, Valleix D, Labrousse F, Denizot Y. VEGF in hepatocellular carcinoma and surrounding cirrhotic liver tissues. World J Gastroenterol. 2006;12:830–831. doi: 10.3748/wjg.v12.i5.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hamdy M, Shaheen K, Awad MA, Barakat EM, Shalaby S, Gupta N, Gupta V. Vascular endothelial growth factor (VEGF) as a biochemical marker for the diagnosis of hepatocellular carcinoma (HCC) Clin Pract. 2020;17:1441–1453. [Google Scholar]
- 101.Morse MA, Sun W, Kim R, He AR, Abada PB, Mynderse M, Finn RS. The role of angiogenesis in hepatocellular carcinoma. Clin Cancer Res. 2019;25:912–920. doi: 10.1158/1078-0432.CCR-18-1254. [DOI] [PubMed] [Google Scholar]
- 102.Tang W, Chen Z, Zhang W, Cheng Y, Zhang B, Wu F, Wang Q, Wang S, Rong D, Reiter FP, De Toni EN, Wang X. The mechanisms of sorafenib resistance in hepatocellular carcinoma: theoretical basis and therapeutic aspects. Signal Transduct Target Ther. 2020;5:87–87. doi: 10.1038/s41392-020-0187-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mazzocca A, Fransvea E, Lavezzari G, Antonaci S, Giannelli G. Inhibition of transforming growth factor beta receptor I kinase blocks hepatocellular carcinoma growth through neo-angiogenesis regulation. Hepatology. 2009;50:1140–1151. doi: 10.1002/hep.23118. [DOI] [PubMed] [Google Scholar]
- 104.Kudo M. Signaling pathway/molecular targets and new targeted agents under development in hepatocellular carcinoma. World J Gastroenterol. 2012;18:6005–6017. doi: 10.3748/wjg.v18.i42.6005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Moeini A, Cornellà H, Villanueva A. Emerging signaling pathways in hepatocellular carcinoma. Liver Cancer. 2012;1:83–93. doi: 10.1159/000342405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu Y, Wang X, Yang Y. Hepatic Hippo signaling inhibits development of hepatocellular carcinoma. Clin Mol Hepatol. 2020;26(4):742–750. doi: 10.3350/cmh.2020.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Luo D, Wang Z, Wu J, Jiang C, Wu J. The role of hypoxia inducible factor-1 in hepatocellular carcinoma. Biomed Res Int. 2014;2014:409272. doi: 10.1155/2014/409272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jia J, Qiao Y, Pilo MG, Cigliano A, Liu X, Shao Z, Calvisi DF, Chen X. Tankyrase inhibitors suppress hepatocellular carcinoma cell growth via modulating the Hippo cascade. PLoS ONE. 2017;12:e0184068. doi: 10.1371/journal.pone.0184068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Seif F, Khoshmirsafa M, Aazami H, Mohsenzadegan M, Sedighi G, Bahar M. The role of JAK-STAT signaling pathway and its regulators in the fate of T helper cells. Cell Commun Signal. 2017;15:23–23. doi: 10.1186/s12964-017-0177-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Banerjee S, Biehl A, Gadina M, Hasni S, Schwartz DM. JAK-STAT signaling as a target for inflammatory and autoimmune diseases: current and future prospects. Drugs. 2017;77:521–546. doi: 10.1007/s40265-017-0701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Svinka J, Mikulits W, Eferl R. STAT3 in hepatocellular carcinoma: new perspectives. Hepat Oncol. 2014;1:107–120. doi: 10.2217/hep.13.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Xie L, Zeng Y, Dai Z, He W, Ke H, Lin Q, Chen Y, Bu J, Lin D, Zheng M. Chemical and genetic inhibition of STAT3 sensitizes hepatocellular carcinoma cells to sorafenib induced cell death. Int J Biol Sci. 2018;14:577–585. doi: 10.7150/ijbs.22220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Jung KH, Yoo W, Stevenson HL, Deshpande D, Shen H, Gagea M, Yoo SY, Wang J, Eckols TK, Bharadwaj U, Tweardy DJ, Beretta L. Multifunctional effects of a small-molecule STAT3 inhibitor on NASH and hepatocellular carcinoma in mice. Clin Cancer Res. 2017;23:5537–5546. doi: 10.1158/1078-0432.CCR-16-2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Liu T, Ma H, Shi W, Duan J, Wang Y, Zhang C, Li C, Lin J, Li S, Lv J, Lin L. Inhibition of STAT3 signaling pathway by ursolic acid suppresses growth of hepatocellular carcinoma. Int J Oncol. 2017;51:555–562. doi: 10.3892/ijo.2017.4035. [DOI] [PubMed] [Google Scholar]
- 115.Li W, Zhang Q, Chen K, Sima Z, Liu J, Yu Q. 2-Ethoxystypandrone, a novel small-molecule STAT3 signaling inhibitor from Polygonum cuspidatum, inhibits cell growth and induces apoptosis of HCC cells and HCC Cancer stem cells. BMC Complement Altern Med. 2019;19:38. doi: 10.1186/s12906-019-2440-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Shan L, Jiang H, Ma L, Yu Y. Yes-associated protein: a novel molecular target for the diagnosis, treatment and prognosis of hepatocellular carcinoma. Oncol Lett. 2017;14:3291–3296. doi: 10.3892/ol.2017.6622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Xia H, Dai X, Yu H, Zhou S, Fan Z, Wei G, Tang Q, Gong Q, Bi F. EGFR-PI3K-PDK1 pathway regulates YAP signaling in hepatocellular carcinoma: the mechanism and its implications in targeted therapy. Cell Death Dis. 2018;9:269. doi: 10.1038/s41419-018-0302-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Valero V, 3rd, Pawlik TM, Anders RA. Emerging role of Hpo signaling and YAP in hepatocellular carcinoma. J Hepatocell Carcinoma. 2015;2:69–78. doi: 10.2147/JHC.S48505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shan L, Li Y, Jiang H, Tao Y, Qian Z, Li L, Cai F, Ma L, Yu Y. Huaier restrains proliferative and migratory potential of hepatocellular carcinoma cells partially through decreased yes-associated protein 1. J Cancer. 2017;8:4087–4097. doi: 10.7150/jca.21018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hayashi H, Higashi T, Yokoyama N, Kaida T, Sakamoto K, Fukushima Y, Ishimoto T, Kuroki H, Nitta H, Hashimoto D, Chikamoto A, Oki E, Beppu T, Baba H. An imbalance in TAZ and YAP expression in hepatocellular carcinoma confers cancer stem cell–like behaviors contributing to disease progression. Can Res. 2015;75:4985–4997. doi: 10.1158/0008-5472.CAN-15-0291. [DOI] [PubMed] [Google Scholar]
- 121.Shi J, Farzaneh M, Khoshnam SE. Yes-associated protein and PDZ binding motif: a critical signaling pathway in the control of human pluripotent stem cells self-renewal and differentiation. Cell Reprogram. 2020;22:55–61. doi: 10.1089/cell.2019.0084. [DOI] [PubMed] [Google Scholar]
- 122.Warren JSA, Xiao Y, Lamar JM. YAP/TAZ Activation as a Target for Treating Metastatic Cancer. Cancers (Basel) 2018;10:115. doi: 10.3390/cancers10040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pobbati AV, Hong W. A combat with the YAP/TAZ-TEAD oncoproteins for cancer therapy. Theranostics. 2020;10:3622–3635. doi: 10.7150/thno.40889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Liu Y, Wang X, Yang Y. Hepatic Hippo signaling inhibits development of hepatocellular carcinoma. Clin Mol Hepatol. 2020;26:742–750. doi: 10.3350/cmh.2020.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Perra A, Kowalik MA, Ghiso E, Ledda-Columbano GM, Di Tommaso L, Angioni MM, Raschioni C, Testore E, Roncalli M, Giordano S, Columbano A. YAP activation is an early event and a potential therapeutic target in liver cancer development. J Hepatol. 2014;61:1088–1096. doi: 10.1016/j.jhep.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 126.Chen C, Lou T. Hypoxia inducible factors in hepatocellular carcinoma. Oncotarget. 2017;8:46691–46703. doi: 10.18632/oncotarget.17358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lee JW, Ko J, Ju C, Eltzschig HK. Hypoxia signaling in human diseases and therapeutic targets. Exp Mol Med. 2019;51:1–13. doi: 10.1038/s12276-019-0235-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lin D, Wu J. Hypoxia inducible factor in hepatocellular carcinoma: a therapeutic target. World J Gastroenterol. 2015;21:12171–12178. doi: 10.3748/wjg.v21.i42.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mu H, Yu G, Li H, Wang M, Cui Y, Zhang T, Song T, Liu C. Mild chronic hypoxia-induced HIF-2α interacts with c-MYC through competition with HIF-1α in hepatocellular carcinoma proliferation. 2020;33:1–13. [DOI] [PubMed]
- 130.Guo Y, Xiao Z, Yang L, Gao Y, Zhu Q, Hu L, Huang D, Xu Q. Hypoxiainducible factors in hepatocellular carcinoma (Review) Oncol Rep. 2019;8(28):46691. doi: 10.3892/or.2019.7397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Liu X, Chen S, Tu J, Cai W, Xu Q. HSP90 inhibits apoptosis and promotes growth by regulating HIF-1alpha abundance in hepatocellular carcinoma. Int J Mol Med. 2016;37:825–835. doi: 10.3892/ijmm.2016.2482. [DOI] [PubMed] [Google Scholar]
- 132.Koziel A, Jarmuszkiewicz W. Hypoxia and aerobic metabolism adaptations of human endothelial cells. Pflugers Arch. 2017;469:815–827. doi: 10.1007/s00424-017-1935-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Jia YY, Zhao JY, Li BL, Gao K, Song Y, Liu MY, Yang XJ, Xue Y, Wen AD, Shi L. miR-592/WSB1/HIF-1alpha axis inhibits glycolytic metabolism to decrease hepatocellular carcinoma growth. Oncotarget. 2016;7:35257–35269. doi: 10.18632/oncotarget.9135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Masoud GN, Li W. HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharm Sin B. 2015;5:378–389. doi: 10.1016/j.apsb.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang X, Li Y, Ma Y, Yang L, Wang T, Meng X, Zong Z, Sun X, Hua X, Li H. Yes-associated protein (YAP) binds to HIF-1alpha and sustains HIF-1alpha protein stability to promote hepatocellular carcinoma cell glycolysis under hypoxic stress. J Exp Clin Cancer Res. 2018;37:216. doi: 10.1186/s13046-018-0892-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Xu J, Zheng L, Chen J, Sun Y, Lin H, Jin RA, Tang M, Liang X, Cai X. Increasing AR by HIF-2alpha inhibitor (PT-2385) overcomes the side-effects of sorafenib by suppressing hepatocellular carcinoma invasion via alteration of pSTAT3, pAKT and pERK signals. Cell Death Dis. 2017;8:e3095. doi: 10.1038/cddis.2017.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nault J-C, Ningarhari M, Rebouissou S, Zucman-Rossi J. The role of telomeres and telomerase in cirrhosis and liver cancer. Nat Rev Gastroenterol Hepatol. 2019;16(9):544–558. doi: 10.1038/s41575-019-0165-3. [DOI] [PubMed] [Google Scholar]
- 138.Bisteau X, Caldez MJ, Kaldis P. The complex relationship between liver cancer and the cell cycle: a story of multiple regulations. Cancers (Basel) 2014;6:79–111. doi: 10.3390/cancers6010079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sonntag R, Giebeler N, Nevzorova YA, Bangen J-M, Fahrenkamp D, Lambertz D, Haas U, Hu W, Gassler N, Cubero FJ, Müller-Newen G, Abdallah AT, Weiskirchen R, Ticconi F, Costa IG, Barbacid M, Trautwein C, Liedtke C. Cyclin E1 and cyclin-dependent kinase 2 are critical for initiation, but not for progression of hepatocellular carcinoma. Proc Natl Acad Sci U S A. 2018;115:9282–9287. doi: 10.1073/pnas.1807155115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wang TJ, Huang MS, Hong CY, Tse V, Silverberg GD, Hsiao M. Comparisons of tumor suppressor p53, p21, and p16 gene therapy effects on glioblastoma tumorigenicity in situ. Biochem Biophys Res Commun. 2001;287:173–180. doi: 10.1006/bbrc.2001.5565. [DOI] [PubMed] [Google Scholar]
- 141.Shamloo B, Usluer S. p21 in cancer research. Cancers (Basel) 2019;11(8):1178. doi: 10.3390/cancers11081178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yang Z, Zhang J, Lin X, Wu D, Li G, Zhong C, Fang L, Jiang P, Yin L, Zhang L. Inhibition of neddylation modification by MLN4924 sensitizes hepatocellular carcinoma cells to sorafenib. Oncol Rep. 2019;41:3257–3269. doi: 10.3892/or.2019.7098. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 143.Shao YY, Li YS, Hsu HW, Lin H, Wang HY, Wo RR, Cheng AL, Hsu CH. Potent activity of composite cyclin dependent kinase inhibition against hepatocellular carcinoma. Cancers (Basel) 2019;11:1433. doi: 10.3390/cancers11101433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Reiter FP, Denk G, Ziesch A, Ofner A, Wimmer R, Hohenester S, Schiergens TS, Spampatti M, Ye L, Itzel T, Munker S, Teufel A, Gerbes AL, Mayerle J, De Toni EN. Predictors of ribociclib-mediated antitumour effects in native and sorafenib-resistant human hepatocellular carcinoma cells. Cell Oncol (Dordr) 2019;42:705–715. doi: 10.1007/s13402-019-00458-8. [DOI] [PubMed] [Google Scholar]
- 145.Pfeffer CM, Singh ATK. Apoptosis: a target for anticancer therapy. Int J Mol Sci. 2018;19:448. doi: 10.3390/ijms19020448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhu X, Qiu J, Zhang T, Yang Y, Guo S, Li T, Jiang K, Zahoor A, Deng G, Qiu C. MicroRNA-188-5p promotes apoptosis and inhibits cell proliferation of breast cancer cells via the MAPK signaling pathway by targeting Rap2c. J Cell Physiol. 2020;235:2389–2402. doi: 10.1002/jcp.29144. [DOI] [PubMed] [Google Scholar]
- 147.Jan R, Chaudhry G-ES. Understanding apoptosis and apoptotic pathways targeted cancer therapeutics. Adv Pharm Bull. 2019;9:205–218. doi: 10.15171/apb.2019.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Fayyaz S, Yaylim I, Turan S, Kanwal S, Farooqi AA. Hepatocellular carcinoma: targeting of oncogenic signaling networks in TRAIL resistant cancer cells. Mol Biol Rep. 2014;41:6909–6917. doi: 10.1007/s11033-014-3577-8. [DOI] [PubMed] [Google Scholar]
- 149.Bai J, Gao Y, Du Y, Yang X, Zhang X. MicroRNA-300 inhibits the growth of hepatocellular carcinoma cells by downregulating CREPT/Wnt/beta-catenin signaling. Oncol Lett. 2019;18:3743–3753. doi: 10.3892/ol.2019.10712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Dai X, Zhang J, Arfuso F, Chinnathambi A, Zayed ME, Alharbi SA, Kumar AP, Ahn KS, Sethi G. Targeting TNF-related apoptosis-inducing ligand (TRAIL) receptor by natural products as a potential therapeutic approach for cancer therapy. Exp Biol Med (Maywood) 2015;240:760–773. doi: 10.1177/1535370215579167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wang H, Ma D, Wang C, Zhao S, Liu C. triptolide inhibits invasion and tumorigenesis of hepatocellular carcinoma MHCC-97H cells through NF-kappaB signaling. Med Sci Monit. 2016;22:1827–1836. doi: 10.12659/MSM.898801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Redza-Dutordoir M, Averill-Bates DA. Activation of apoptosis signalling pathways by reactive oxygen species. Biochim et Biophys Acta (BBA) Mol Cell Res 2016; 1863: 2977–2992. [DOI] [PubMed]
- 153.Gupta S, Silveira DA, Mombach JCM. Towards DNA-damage induced autophagy: a Boolean model of p53-induced cell fate mechanisms. DNA Repair. 2020;96:102971. doi: 10.1016/j.dnarep.2020.102971. [DOI] [PubMed] [Google Scholar]
- 154.Mijit M, Caracciolo V, Melillo A, Amicarelli F, Giordano A. Role of p53 in the regulation of cellular senescence. Biomolecules. 2020;10:420. doi: 10.3390/biom10030420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Azer SA. MDM2-p53 interactions in human hepatocellular carcinoma: what is the role of nutlins and new therapeutic options? J Clin Med. 2018;7(4):64. doi: 10.3390/jcm7040064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wan Z, Pan H, Liu S, Zhu J, Qi W, Fu K, Zhao T, Liang J. Downregulation of SNAIL sensitizes hepatocellular carcinoma cells to TRAIL-induced apoptosis by regulating the NF-kappaB pathway. Oncol Rep. 2015;33:1560–1566. doi: 10.3892/or.2015.3743. [DOI] [PubMed] [Google Scholar]
- 157.Gomes AR, Abrantes AM, Brito AF, Laranjo M, Casalta-Lopes JE, Goncalves AC, Sarmento-Ribeiro AB, Botelho MF, Tralhao JG. Influence of P53 on the radiotherapy response of hepatocellular carcinoma. Clin Mol Hepatol. 2015;21:257–267. doi: 10.3350/cmh.2015.21.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hsu HT, Chi CW. Emerging role of the peroxisome proliferator-activated receptor-gamma in hepatocellular carcinoma. J Hepatocell Carcinoma. 2014;1:127–135. doi: 10.2147/JHC.S48512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wahl K, Siegemund M, Lehner F, Vondran F, Nussler A, Langer F, Krech T, Kontermann R, Manns MP, Schulze-Osthoff K, Pfizenmaier K, Bantel H. Increased apoptosis induction in hepatocellular carcinoma by a novel tumor-targeted TRAIL fusion protein combined with bortezomib. Hepatology. 2013;57:625–636. doi: 10.1002/hep.26082. [DOI] [PubMed] [Google Scholar]
- 160.Yuan X, Gajan A, Chu Q, Xiong H, Wu K, Wu GS. Developing TRAIL/TRAIL death receptor-based cancer therapies. Cancer Metastasis Rev. 2018;37:733–748. doi: 10.1007/s10555-018-9728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Shi X, Liu J, Ren L, Mao N, Tan F, Ding N, Yang J, Li M. Nutlin-3 downregulates p53 phosphorylation on serine392 and induces apoptosis in hepatocellular carcinoma cells. BMB Rep. 2014;47:221–226. doi: 10.5483/BMBRep.2014.47.4.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Xiao Z, Li CH, Chan SL, Xu F, Feng L, Wang Y, Jiang JD, Sung JJ, Cheng CH, Chen Y. A small-molecule modulator of the tumor-suppressor miR34a inhibits the growth of hepatocellular carcinoma. Cancer Res. 2014;74:6236–6247. doi: 10.1158/0008-5472.CAN-14-0855. [DOI] [PubMed] [Google Scholar]
- 163.Yu L, Chen Y, Tooze SA. Autophagy pathway: cellular and molecular mechanisms. Autophagy. 2018;14:207–215. doi: 10.1080/15548627.2017.1378838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Li X, He S, Ma B. Autophagy and autophagy-related proteins in cancer. Mol Cancer. 2020;19:12. doi: 10.1186/s12943-020-1138-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Yun CW, Lee SH. The roles of autophagy in cancer. Int J Mol Sci. 2018;19:3466. doi: 10.3390/ijms19113466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wang B-S, Liu Y-Z, Yang Y, Zhang Y, Hao J-J, Yang H, Wang X-M, Zhang Z-Q, Zhan Q-M, Wang M-R. Autophagy negatively regulates cancer cell proliferation via selectively targeting VPRBP. Clin Sci. 2013;124:203–214. doi: 10.1042/CS20120270. [DOI] [PubMed] [Google Scholar]
- 167.Yazdani HO, Huang H, Tsung A. Autophagy: dual response in the development of hepatocellular carcinoma. Cells. 2019;8(2):91. doi: 10.3390/cells8020091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Duan Y, Li J, Jing X, Ding X, Yu Y, Zhao Q. Fucoidan induces apoptosis and inhibits proliferation of hepatocellular carcinoma via the p38 MAPK/ERK and PI3K/Akt signal pathways. Cancer Manag Res. 2020;12:1713–1723. doi: 10.2147/CMAR.S243495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Yang S, Yang L, Li X, Li B, Li Y, Zhang X, Ma Y, Peng X, Jin H, Li H. New insights into autophagy in hepatocellular carcinoma: mechanisms and therapeutic strategies. Am J Cancer Res. 2019;9:1329–1353. [PMC free article] [PubMed] [Google Scholar]
- 170.Xie B, He X, Guo G, Zhang X, Li J, Liu J, Lin Y. High-throughput screening identified mitoxantrone to induce death of hepatocellular carcinoma cells with autophagy involvement. Biochem Biophys Res Commun. 2020;521:232–237. doi: 10.1016/j.bbrc.2019.10.114. [DOI] [PubMed] [Google Scholar]
- 171.Liu F, Wang F, Dong X, Xiu P, Sun P, Li Z, Shi X, Zhong J. T7 peptide cytotoxicity in human hepatocellular carcinoma cells is mediated by suppression of autophagy. Int J Mol Med. 2019;44:523–534. doi: 10.3892/ijmm.2019.4231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Stiuso P, Potenza N, Lombardi A, Ferrandino I, Monaco A, Zappavigna S, Vanacore D, Mosca N, Castiello F, Porto S, Addeo R, Prete SD, De Vita F, Russo A, Caraglia M. MicroRNA-423-5p promotes autophagy in cancer cells and is increased in serum from hepatocarcinoma patients treated with sorafenib. Mol Ther Nucleic Acids. 2015;4:e233. doi: 10.1038/mtna.2015.8. [DOI] [PubMed] [Google Scholar]
- 173.Gavini J, Dommann N, Jakob MO, Keogh A, Bouchez LC, Karkampouna S, Julio MK, Medova M, Zimmer Y, Schlafli AM, Tschan MP, Candinas D, Stroka D, Banz V. Verteporfin-induced lysosomal compartment dysregulation potentiates the effect of sorafenib in hepatocellular carcinoma. Cell Death Dis. 2019;10:749. doi: 10.1038/s41419-019-1989-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Simioni C, Cani A, Martelli AM, Zauli G, Alameen AA, Ultimo S, Tabellini G, McCubrey JA, Capitani S, Neri LM. The novel dual PI3K/mTOR inhibitor NVP-BGT226 displays cytotoxic activity in both normoxic and hypoxic hepatocarcinoma cells. Oncotarget. 2015;6:17147–17160. doi: 10.18632/oncotarget.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Soltan MY, Sumarni U, Assaf C, Langer P, Reidel U, Eberle J. Key Role of Reactive Oxygen Species (ROS) in indirubin derivative-induced cell death in cutaneous t-cell lymphoma cells. Int J Mol Sci. 2019;20:1158. doi: 10.3390/ijms20051158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Aggarwal V, Tuli HS, Varol A, Thakral F, Yerer MB, Sak K, Varol M, Jain A, Khan MA, Sethi G. Role of reactive oxygen species in cancer progression: molecular mechanisms and recent advancements. Biomolecules. 2019;9(11):735. doi: 10.3390/biom9110735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Takaki A, Yamamoto K. Control of oxidative stress in hepatocellular carcinoma: helpful or harmful? World J Hepatol. 2015;7:968–979. doi: 10.4254/wjh.v7.i7.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cardin R, Piciocchi M, Bortolami M, Kotsafti A, Barzon L, Lavezzo E, Sinigaglia A, Rodriguez-Castro KI, Rugge M, Farinati F. Oxidative damage in the progression of chronic liver disease to hepatocellular carcinoma: an intricate pathway. World J Gastroenterol. 2014;20:3078–3086. doi: 10.3748/wjg.v20.i12.3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kim EK, Jang M, Song MJ, Kim D, Kim Y, Jang HH. Redox-mediated mechanism of chemoresistance in cancer cells. Antioxidants (Basel) 2019;8(10):471. doi: 10.3390/antiox8100471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Huang G, Pan S-T. ROS-mediated therapeutic strategy in chemo-/radiotherapy of head and neck cancer. Oxid Med Cell Longev. 2020;2020:5047987. doi: 10.1155/2020/5047987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Perillo B, Di Donato M, Pezone A, Di Zazzo E, Giovannelli P, Galasso G, Castoria G, Migliaccio A. ROS in cancer therapy: the bright side of the moon. Exp Mol Med. 2020;52:192–203. doi: 10.1038/s12276-020-0384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Liou G-Y, Storz P. Reactive oxygen species in cancer. Free Radic Res. 2010;44:479–496. doi: 10.3109/10715761003667554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lv H, Wang C, Fang T, Li T, Lv G, Han Q, Yang W, Wang H. Vitamin C preferentially kills cancer stem cells in hepatocellular carcinoma via SVCT-2. NPJ Precis Oncol. 2018;2:1. doi: 10.1038/s41698-017-0044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Hwang-Bo H, Jeong JW, Han MH, Park C, Hong SH, Kim GY, Moon SK, Cheong J, Kim WJ, Yoo YH, Choi YH. Auranofin, an inhibitor of thioredoxin reductase, induces apoptosis in hepatocellular carcinoma Hep3B cells by generation of reactive oxygen species. Gen Physiol Biophys. 2017;36:117–128. doi: 10.4149/gpb_2016043. [DOI] [PubMed] [Google Scholar]
- 185.Hwang-Bo H, Lee WS, Nagappan A, Kim HJ, Panchanathan R, Park C, Chang SH, Kim ND, Leem SH, Chang YC, Kwon TK, Cheong JH, Kim GS, Jung JM, Shin SC, Hong SC, Choi YH. Morin enhances auranofin anticancer activity by up-regulation of DR4 and DR5 and modulation of Bcl-2 through reactive oxygen species generation in Hep3B human hepatocellular carcinoma cells. Phytother Res. 2019;33:1384–1393. doi: 10.1002/ptr.6329. [DOI] [PubMed] [Google Scholar]
- 186.Wei PL, Huang CY, Chang YJ. Propyl gallate inhibits hepatocellular carcinoma cell growth through the induction of ROS and the activation of autophagy. PLoS ONE. 2019;14:e0210513. doi: 10.1371/journal.pone.0210513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yuan Z, Liang Z, Yi J, Chen X, Li R, Wu J, Sun Z. Koumine promotes ROS production to suppress hepatocellular carcinoma cell proliferation via NF-kappaB and ERK/p38 MAPK signaling. Biomolecules. 2019;9(10):559. doi: 10.3390/biom9100559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Li Y, Lu J, Chen Q, Han S, Shao H, Chen P, Jin Q, Yang M, Shangguan F, Fei M, Wang L, Liu Y, Liu N, Lu B. Artemisinin suppresses hepatocellular carcinoma cell growth, migration and invasion by targeting cellular bioenergetics and Hippo-YAP signaling. Arch Toxicol. 2019;93:3367–3383. doi: 10.1007/s00204-019-02579-3. [DOI] [PubMed] [Google Scholar]
- 189.Liu C, Yang S, Wang K, Bao X, Liu Y, Zhou S, Liu H, Qiu Y, Wang T, Yu H. Alkaloids from Traditional Chinese Medicine against hepatocellular carcinoma. Biomed Pharmacother. 2019;120:109543. doi: 10.1016/j.biopha.2019.109543. [DOI] [PubMed] [Google Scholar]
- 190.Singh A, Shafi S, Upadhyay T, Najmi AK, Kohli K, Pottoo FH. Insights into nanotherapeutic strategies as an impending approach to liver cancer treatment. Curr Top Med Chem. 2020;20:1839–1854. doi: 10.2174/1568026620666200624161801. [DOI] [PubMed] [Google Scholar]
- 191.Wei W, Chua MS, Grepper S, So S. Small molecule antagonists of Tcf4/beta-catenin complex inhibit the growth of HCC cells in vitro and in vivo. Int J Cancer. 2010;126:2426–2436. doi: 10.1002/ijc.24810. [DOI] [PubMed] [Google Scholar]
- 192.Jeng KS, Sheen IS, Jeng WJ, Yu MC, Tsai HH, Chang FY, Su JC. Blockade of the sonic hedgehog pathway effectively inhibits the growth of hepatoma in mice: An in vivo study. Oncol Lett. 2012;4:1158–1162. doi: 10.3892/ol.2012.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Tsang CM, Cheung KC, Cheung YC, Man K, Lui VW, Tsao SW, Feng Y. Berberine suppresses Id-1 expression and inhibits the growth and development of lung metastases in hepatocellular carcinoma. Biochim Biophys Acta. 2015;1852:541–551. doi: 10.1016/j.bbadis.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 194.Wang H, Zhang C, Chi H, Meng Z. Synergistic anti-hepatoma effect of bufalin combined with sorafenib via mediating the tumor vascular microenvironment by targeting mTOR/VEGF signaling. Int J Oncol. 2018;52:2051–2060. doi: 10.3892/ijo.2018.4351. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.