Abstract
Background
Transportation barriers limit access to cancer care services and contribute to suboptimal clinical outcomes. Our objectives were to describe the frequency of Veterans reporting and the factors associated with transportation barriers to or from colorectal cancer (CRC) care visits.
Methods
Between November 2015 and September 2016, Veterans with incident stage I, II, or III CRC completed a mailed survey to assess perceived barriers to recommended care. Participants who reported difficulty with transportation to or from CRC care appointments were categorized as experiencing transportation barriers. We assessed pairwise correlations between transportation barriers, transportation-related factors (e.g., mode of travel), and chaotic lifestyle (e.g., predictability of schedules), and used logistic regression to examine the association between the reporting of transportation difficulties, distance traveled to the nearest Veterans Affairs (VA) facility, and life chaos.
Results
Of the 115 Veterans included in this analysis, 18% reported experiencing transportation barriers. Distance to the VA was not strongly correlated with the reporting of transportation barriers (Spearman’s ρ = 0.12, p = 0.19), but chaotic lifestyle was both positively and significantly correlated with experiencing transportation barriers (Spearman’s ρ = 0.22, p = 0.02). Results from the logistic regression model modestly supported the findings from the pairwise correlations, but were not statistically significant.
Conclusions
Transportation is an important barrier to or from CRC care visits, especially among Veterans who experience greater life chaos. Identifying Veterans who experience chaotic lifestyles would allow for timely engagement in behavioral interventions (e.g., organizational skills training) and with support services (e.g., patient navigation).
Keywords: Access to care, Colorectal cancer, Life chaos, Transportation, Travel distance, Veterans Affairs
Background
Transportation barriers, including availability and cost of transportation and distance and time traveled to care [1], limit access to necessary healthcare services and contribute to suboptimal clinical outcomes across the cancer care continuum [2, 3]. For patients with colorectal cancer (CRC), transportation barriers have been associated with diagnoses of advanced disease [2–4] and also resulted in the decreased likelihood of receiving or adhering with recommended treatment and specialist care [2, 3, 5, 6]. In turn, non-adherence with CRC care plans – treatment, surveillance, and survivorship – has contributed to shortened survival and impaired quality of life [7, 8].
Transportation barriers and subsequent health consequences disproportionately affect older adults [6–11], patients living in rural areas [2, 4, 5, 9–11], persons of color [8, 11, 12], those of lower socioeconomic status [5–7, 10, 11], and individuals with limited social support [6, 10, 12]. U.S. Veterans are more likely to be older when diagnosed with CRC [11, 13, 14], more often to reside in rural counties [11], and have lower rates of employment [15, 16], college education [16], and income [11, 15, 16] than the general population. Despite the increased risk for experiencing transportation difficulties to or from care, only a few studies have evaluated the relationship between known patient-level factors and transportation barriers among Veterans.
Veterans Health Administration (VHA) research has supported findings related to the demographic (e.g., older age, persons of color) [17, 18], geographic (e.g., rurality) [18, 19], and lifestyle characteristics (e.g., inadequate social support) [11] associated with transportation barriers, reduced access to care, and unmet medical need among privately and publicly insured individuals [11, 17–20]. However, a majority of these studies did not focus on Veterans with CRC [17–20] or were not designed to or inconsistently measured difficulties with transportation [11, 17, 20]. Questions regarding the frequency of and which transportation-related factors (e.g., distance to care, mode of travel) are associated with self-reported transportation barriers among Veterans with CRC remain.
To address these gaps in knowledge, the objectives of this study were to determine how widespread transportation barriers were among Veterans with CRC and to assess the patient-level and transportation-related factors associated with the reporting of transportation difficulties.
Methods
Participants
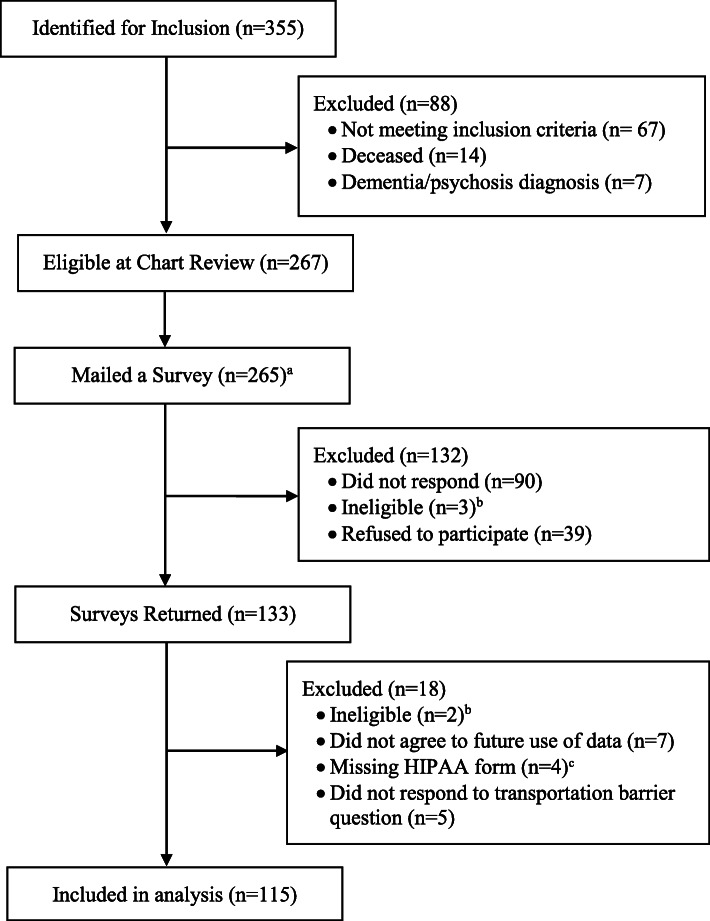
We used the Veterans Affairs (VA) Cancer Cube, which contains diagnostic, clinical, and treatment information about suspected cancer cases [21, 22], to identify eligible participants. We included Veterans who (1) had incident stage I, II, or III colorectal cancer, (2) were diagnosed between October 2007 and December 2015 at VA Medical Centers (VAMCs) in North Carolina or Virginia, and (3) had a valid home mailing address and telephone number. Following initial identification of 355 Veterans, we reviewed electronic health record (EHR) data to confirm eligibility criteria and vital status (Fig. 1).
Fig. 1.
Study Participant Identification. Abbreviations: HIPAA, Health Insurance Portability and Accountability Act. a Two surveys were not mailed to Veterans because at the time of mailing these individuals were deemed ineligible since they did not meet inclusion criteria, had a dementia or psychosis diagnosis, or were deceased. b Patients were deemed ineligible because they did not meet inclusion criteria, had a dementia or psychosis diagnosis, or were deceased. c Study participants were required to complete and sign a HIPAA authorization form. Participants whose forms were not returned, incomplete, and/or lacked a signature were excluded from analysis
Data collection
The Colorectal Cancer Patient Adherence to Survivorship Treatment (COAST) survey assessed perceived barriers to, and adherence with, recommended care [21]. Between October 2015 and September 2016, information regarding informed consent, self-administered surveys, and non-monetary incentives (cancer survivorship pins) were mailed to 265 eligible Veterans. Approximately 2 weeks after the initial mailing, Veterans were called if surveys were not returned (to verify mailing addresses) or if information was incomplete (to collect missing survey responses). A total of 133 Veterans returned surveys, yielding an overall response rate of 50.2%.
Ethical considerations
This study was approved by the Durham VA Health Care System Institutional Review Board. All participants included in this analysis provided implied consent by returning a completed survey and completed a Health Insurance Portability and Accountability Act (HIPAA) authorization form.
Measures
Transportation barriers
The primary outcome was reporting difficulty with transportation to or from CRC treatment or a related appointment. Veterans who responded “Sometimes”, “Often”, or “Always” were categorized as having experienced transportation barriers, while those that selected “Never” were classified as having no transportation barriers [11]. Consistent with prior studies that have assessed transportation barriers [11] and cross-sectional surveys [23–25], Veterans who did not respond or reported “Don’t know” were excluded from analysis (n = 5).
Demographics
Self-reported demographics included age, sex, race, education, employment, and marital status. Veterans were categorized as either 40 to 65 years of age or 66 years or older at time of survey completion based on their year of birth and date of survey completion. Due to a limited number of racial and ethnic minority respondents (n = 38), we classified race as white or persons of color (American Indian or Alaska Native, Asian, black or African American, Native Hawaiian or Pacific Islander, multiracial). In addition, Veterans who reported full- or part-time employment were categorized as working. Veterans’ marital status was classified as married (married or living together), divorced or separated, widowed, or single (single or never married).
Transportation-related factors
We measured location of CRC care services, distance to the nearest VA hospital or clinic, convenience of the nearest VA location, and the most common mode of travel to the VA. The VA was considered the primary treatment location for Veterans who reported receiving “All”, “More than half”, or “About half” of their CRC care in VA hospitals or clinics, whereas a non-VA facility was deemed the major source of services for those receiving “Less than half” of their CRC care at the VA. Since travel distances exceeding 20 miles have been associated with delays in and/or reduced receipt of cancer care [26, 27], we categorized distance to the nearest VA as either less than or equal to 20 miles (respondents selected “0 to 20 miles”) or greater than 20 miles (Veterans selected “21 to 40 miles”, “41 to 60 miles”, “61 to 80 miles”, “81 to 100 miles” or “101 miles or more”).
Chaotic lifestyle
Chaotic lifestyle and environment (also referred to as life chaos) encompasses individuals’ ability to organize and anticipate future events, as well as the consistency and predictability of their daily schedules [28, 29]. Chaotic lifestyle has been associated with reduced engagement with the healthcare system [30] and non-adherence with treatment plans [28, 29], and thus, may also affect a patient’s ability to adequately plan for transportation to or from CRC care appointments. To assess Veterans’ perceived life chaos, we used the six validated measures of the Confusion, Hubbub, and Order Scale (CHAOS): “My life is organized” (reverse coded); “My life is unstable”; “My routine is the same from week to week” (reverse coded); “My daily activities from week to week are unpredictable”; “Keeping a schedule is difficult for me”; and “I do not like to make appointments too far in advance because I do not know what might come up” [30]. The CHAOS scale was scored by summing 5-point Likert scale responses ranging from “Definitely true” to “Definitely false”, with higher scores signifying a chaotic lifestyle (scores range from 6 to 30) [28–30]. We considered a CHAOS score of 16 or higher as an indication of a more chaotic lifestyle [31].
Statistical analysis
We conducted statistical analysis in SAS version 9.4 (SAS Institute, Cary, NC). We examined differences in demographic, lifestyle, and transportation-related characteristics between Veterans who did and did not report transportation barriers using chi-square or Fisher’s exact tests. We also assessed pairwise correlations between transportation barriers, transportation-related factors, and chaotic lifestyle. Lastly, we used logistic regression to evaluate the association between the reporting of transportation barriers, distance traveled to the VA, and chaotic lifestyle.
Results
COAST respondent characteristics
Of the 115 survey respondents that were included in this analysis (Fig. 1), a majority were aged 66 years or older (72%), were married (59%), and had a high school diploma or higher education (87%) (Table 1). In addition, most Veterans reported primarily receiving CRC care at a VA hospital or clinic (94%), living more than 20 miles from the nearest VA (71%), and driving themselves to and from the VA for care (58%). A majority of Veterans experienced a less chaotic lifestyle (57%).
Table 1.
COAST Respondent Characteristics
| Characteristic | All Respondents (n = 115) |
Reported Transportation Barriers (n = 21) | Reported No Transportation Barriers (n = 94) | P-value |
|---|---|---|---|---|
| Demographics (N, %) | ||||
| Age at survey completion | ||||
| 40–65 | 32 (28) | 11 (52) | 21 (22) | 0.006 |
| ≥ 66 | 83 (72) | 10 (48) | 73 (78) | |
| Sex | ||||
| Male | 109 (95) | 19 (90) | 90 (96) | 0.301 |
| Female | 6 (5) | 2 (10) | 4 (4) | |
| Racea | ||||
| White | 74 (64) | 13 (62) | 61 (65) | 0.700 |
| Persons of color | 38 (33) | 7 (33) | 31 (33) | |
| Employmenta | ||||
| Working | 28 (24) | 1 (5) | 27 (29) | 0.060 |
| Not working | 85 (74) | 20 (95) | 65 (69) | |
| Educationa | ||||
| Less than high school | 14 (12) | 1 (5) | 13 (14) | 0.559 |
| High school graduate or higher education | 100 (87) | 20 (95) | 80 (85) | |
| Marital status | ||||
| Married | 68 (59) | 8 (38) | 60 (64) | 0.005 |
| Divorced/separated | 29 (25) | 12 (57) | 17 (18) | |
| Widowed | 13 (11) | 1 (5) | 12 (13) | |
| Single | 5 (4) | 0 (0) | 5 (5) | |
| Transportation-related Factors (N, %) | ||||
| CRC care locationa | ||||
| VA hospital/clinic | 108 (94) | 19 (90) | 89 (95) | 0.488 |
| Non-VA health center | 5 (4) | 2 (10) | 3 (3) | |
| Distance to the VA | ||||
| ≤ 20 miles | 33 (29) | 4 (19) | 29 (31) | 0.280 |
| > 20 miles | 82 (71) | 17 (81) | 65 (69) | |
| Convenience of the VAa | ||||
| Convenient | 96 (83) | 15 (71) | 81 (86) | 0.143 |
| Not convenient | 17 (15) | 6 (29) | 11 (12) | |
| Mode of travel | ||||
| Drive self | 67 (58) | 8 (38) | 59 (63) | 0.098 |
| Rely on friends/family | 44 (38) | 12 (57) | 32 (34) | |
| Public transportation | 2 (2) | 1 (5) | 1 (1) | |
| Other method | 2 (2) | 0 (0) | 2 (2) | |
| Lifestyle Factors (N,%) | ||||
| Chaotic lifestylea | ||||
| Less chaotic | 65 (57) | 9 (43) | 56 (60) | 0.245 |
| More chaotic | 47 (41) | 12 (57) | 35 (37) | |
Abbreviations: COAST Colorectal Cancer Patient Adherence to Survivorship Treatment, CRC colorectal cancer, VA Veterans Affairs
aParticipants with missing data, which is defined as not responding or selecting “Prefer not to answer” or “Don’t know”, are not included in the table. Race was missing for 1 participant reporting barriers and for 2 participants reporting no barriers; employment was missing for 2 participants reporting no barriers; education was missing for 1 participant reporting no barriers; location of cancer care was missing for 2 participants reporting no barriers; convenience of VA location was missing for 2 participants reporting no barriers; and chaotic lifestyle was missing for 3 participants reporting no barriers
Approximately 18% (n = 21) of Veterans reported experiencing transportation barriers to or from CRC care appointments. Demographics, transportation-related factors, and lifestyle characteristics were similar between Veterans who did and did not report transportation barriers, although Veterans experiencing difficulties with transportation were more likely to be younger (52% vs. 22%, p = 0.006) and less likely to be married (38% vs. 64%, p = 0.005) than those without barriers.
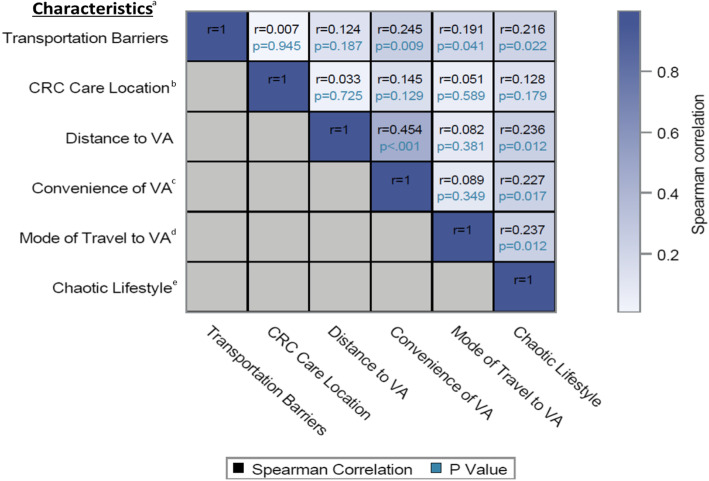
Correlation between transportation barriers, transportation-related factors, and life chaos
Distance to the VA was not strongly correlated with reporting transportation barriers to or from CRC care visits (Spearman’s ρ = 0.124, p = 0.187), but mode of travel was significantly correlated with reporting transportation barriers (Spearman’s ρ = 0.191, p = 0.041) (Fig. 2). Convenience of the VA and chaotic lifestyle were both positively and significantly correlated with experiencing transportation barriers (Spearman’s ρ = 0.245, p = 0.009 and ρ = 0.216, p = 0.022, respectively) and distance to the nearest VA (Spearman’s ρ = 0.454, p < 0.001 and ρ = 0.236, p = 0.012).
Fig. 2.
Relationship Between Transportation-related Factors and Chaotic Lifestyle. Abbreviations: CRC, colorectal cancer care; VA, Veterans Affairs. a SAS was used to calculate Spearman’s correlation coefficients and to create the correlation heatmap. Variables were continuous (chaotic lifestyle) or categorical (transportation barriers: “Always”, “Often”, “Sometimes”, “Never”; distance to the VA: “0 to 20 miles”, “21 to 40 miles”, “41 to 60 miles”, “61 to 80 miles”, “81 to 100 miles”, “101 miles or more”; use of the VA for colorectal cancer care: “All of your cancer care”, “More than half of your cancer care”, “About half of your cancer care”, “Less than half of your cancer care”; convenience of VA: “Very convenient”, “Somewhat convenient”, “Somewhat inconvenient”, “Very convenient”; mode of travel to the VA: “Drive myself’, “Friend or family drives me”, “Health aide”, “Disabled American Veterans (DAV) or other shuttle service”, “Public transportation”, “Another source”). b Participants who did not respond or responded “Don’t know” were excluded from analysis (n = 2). c Participants who did not respond or responded “Don’t know” were excluded from analysis (n = 2). d Mode of travel to the VA is ordered based on decreasing travel independence. Veterans who selected (1) “Drive myself” have access to a vehicle and are in control of traveling to or from the VA as needed; (2) “Friend or family drives me” face some limitations due to others’ availability but are able to tailor transportation to or from the VA according to their needs; (3) “Public transportation” are further limited by fixed travel schedules and routes to or from the VA; or (4) “Another source” are assumed to be the most restricted in terms of travel independence (respondents did not select “Health aide” or “DAV or other shuttle service”). e Participants who did not respond or had missing values were excluded from analysis (n = 3)
Factors associated with reporting transportation barriers
Results from the logistic regression model modestly supported the findings from the pairwise correlations, but were not statistically significant. Findings suggest that Veterans living further from the VA and experiencing greater life chaos have a higher probability of transportation difficulties than those residing within 20 miles of care and reporting a less chaotic lifestyle (predicted probability = 0.272, 95% confidence limit [CL] = 0.159, 0.425 vs. predicted probability = 0.102, 95% CL = 0.036, 0.258) (Table 2).
Table 2.
Predicted Probabilities of Reporting Transportation Barriers
| Distance to the VA | Chaotic Lifestyle | Predicted Probability (95% CL) |
|---|---|---|
| ≤ 20 miles | Less chaotic lifestyle (score < 16) | 0.102 (0.036, 0.258) |
| ≤ 20 miles | More chaotic lifestyle (score ≥ 16) | 0.184 (0.063, 0.431) |
| > 20 miles | Less chaotic lifestyle (score < 16) | 0.158 (0.080, 0.291) |
| > 20 miles | More chaotic lifestyle (score ≥ 16) | 0.272 (0.159, 0.425) |
Abbreviations: CL confidence limits, VA Veterans Affairs
aWe used PROC LOGISTIC in SAS to estimate the predicted probability of transportation barriers for Veterans who (1) traveled ≤20 miles to the VA and had a less chaotic lifestyle, (2) traveled ≤20 miles to the VA and had a more chaotic lifestyle, (3) traveled > 20 miles to the VA and had a less chaotic lifestyle, and (4) traveled > 20 miles to the VA and had a more chaotic lifestyle (the reference group is Veterans who reported no difficulties with transportation to or from cancer care appointments). Predicted probabilities were not statistically significant for all groups
bWe tested goodness of fit with deviance and Pearson chi square tests, which indicated reasonable model fit
Discussion
To our knowledge, this is one of the first studies to evaluate transportation-related factors (e.g., distance to care) and lifestyle characteristics (e.g., life chaos) associated with reporting transportation barriers among Veterans with CRC. Findings indicated that mode of travel was significantly correlated with transportation barriers to or from CRC care appointments, suggesting that Veterans who rely on family, friends, or public transportation may not have consistent access to or use of reliable transportation. Treatment side-effects (e.g., fatigue, vision impairment) [11, 32, 33], coupled with VA care requirements (e.g., an adult must attend a colonoscopy appointment) [34] increases Veterans’ need for and dependence on a stable support system for transportation to or from care. However, competing priorities – employment demands and family obligations – may limit caretakers’ ability to regularly drive a Veteran to CRC treatment or medical visits [35, 36].
Although transportation services to or from cancer-related appointments (e.g., VA, community healthcare facility, or patient advocacy programs) have eased the burden of both patients and their caregivers [36, 37], none of the study participants selected or discussed these programs in their survey responses. Veterans may be unaware of the transportation services offered by the VA or their community [38] or they may find available services to be inconvenient (e.g., infrequent pick-off and drop-off times, difficulty traveling to designated pick-up or drop-off locations) [18, 20] or infeasible for their care needs (e.g., not adequately equipped for Veterans using wheelchairs) [18]. Future studies should identify ways in which transportation programs can be aligned with patients’ needs and the circumstances in which telehealth services may replace in-person appointments [18–20].
We also found that distance to the nearest VA facility was not significantly correlated with the reporting of transportation barriers to or from CRC care appointments. This finding suggests that Veterans may have accessed community services located closer to their homes or travel distance may not be a substantial deterrent to the care and support received at VA hospitals or clinics. Some Veterans have cited the importance of the patient-provider relationship [39, 40] as a primary reason for seeking care at the VA, while others value camaraderie – specifically, the kinship in shared military service and cancer care experiences [39, 41]. Together, these factors have been associated with increased patient engagement and adherence with recommended care and improved quality of life [42–45]. Despite these advantages, there may be a threshold at which distance to a VA facility becomes inconvenient and may lead to barriers to or from CRC care.
In some cases, Veterans live more than 100 miles from the nearest VA facility and distance may become a more pronounced barrier to or from care with each CRC treatment or surveillance appointment [16, 18]. Due to the increased risk of delays in care resulting from transportation barriers, VA facilities have established cancer care navigation teams (CCNTs). CCNTs assist high-risk Veterans (those living 100 miles or more from care, receiving multi-modality treatment, or experiencing significant psychosocial barriers to care) with addressing identified barriers to cancer care [16]. For example, CCNTs manage the logistics (e.g., accommodations, transportation) for each appointment and identify other services (e.g., medication management, counseling) that meet Veterans’ medical and psychosocial needs [16]. Future research is necessary to assess the feasibility of implementing or expanding CCNTs across VA facilities, especially since patient navigation services minimize barriers to cancer care, improve the education and support of Veterans, and have the potential to ensure continuity of care across the cancer care continuum [16, 46, 47].
Finally, we noted that a chaotic lifestyle was significantly correlated with the reporting of transportation barriers to or from CRC care appointments. A chaotic lifestyle may affect Veterans’ ability to identify, schedule, and manage access to reliable transportation; however, transportation instability (e.g., public transportation delays or cancelations, inability to afford transportation expenses) may disrupt Veterans’ lives and yield a higher degree of life chaos. Future research is needed to explore this potentially endogenous relationship, as well as to discern which facet of a chaotic lifestyle is the most challenging for Veterans experiencing transportation difficulties and which transportation-related factor is driving life chaos [28]. In turn, this information could determine what type of and when an intervention (e.g., organizational skills training, telehealth services) is warranted [28].
This study had several limitations. First, a small sample size and inability to adjust for potential measured confounders (e.g., demographics) contributes to lack of statistical significance and limits the interpretation and validity of our findings. Future studies should survey a broader population of Veterans with CRC to enable a robust examination of the factors associated with the reporting of transportation barriers. Second, our study focused on a regional sample of Veterans with non-metastatic CRC who had a valid home mailing address, which further limits the generalizability of our findings. Future research is necessary to determine if the frequency of and factors associated with reporting transportation barriers differs among female Veterans and those with advanced disease. Third, based on the definition of the primary outcome, our study did not determine how the association between life chaos and transportation-related factors may have varied across the degrees (e.g., always vs. sometimes) of experiencing transportation barriers. Fourth, we measured distance to and convenience of respondents’ nearest VA location; however, we were not able to discern if this facility was the primary provider of CRC services. Fifth, similar to all surveys, our study may be subject to potential recall and response biases; however, the use of validated and previously tested measures may have minimized the effect of these biases [48]. Sixth, our response rate of 50% may have introduced selection bias as non-responders may have different sociodemographic factors, lifestyle characteristics, and transportation needs than survey respondents. Seventh, as with any observational study, unmeasured confounding could be a potential source of bias. Eighth, this study was not designed to assess the effect of transportation barriers on the use of cancer care services. Future research should not only account for how difficulties with transportation impact CRC care, but also determine whether policies aimed at expanding access (e.g., Choice Act, MISSION Act) [49, 50] have minimized the negative impact of transportation barriers. Lastly, the cross-sectional nature of this study limits our ability to establish a causal relationship between chaotic lifestyle, distance to care, and transportation barriers.
Conclusions
Our findings suggest that transportation is an important barrier to or from CRC care visits, especially among Veterans who experience greater life chaos. Future research is needed to determine the association between perceived life chaos and receipt of CRC care (e.g., delayed therapy initiation, missed appointments). However, screening for life chaos should be integrated into routine clinical practice. Identification of Veterans who experience chaotic lifestyles would allow for timely intervention – organizational skills training, patient navigation, and/or telehealth services – which in turn, could lead to the potential modification of observed risk factors and support the continuity of care across the cancer care continuum [16, 36, 37, 46, 47].
Acknowledgements
We thank the Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) at the Durham Veterans Affairs Health Care System for their support (e.g., computers, office space). The content is solely the responsibility of the authors and does not necessarily reflect the position or policy of Duke University, the U.S. Department of Veterans Affairs, or the U.S. government.
Qualitative tools
The Colorectal Cancer Patient Adherence to Survivorship Treatment (COAST) survey is not under license.
Abbreviations
- CCNT
Cancer care navigation team
- CHAOS
Confusion, Hubbub, and Order Scale
- CL
Confidence limit
- COAST
Colorectal Cancer Patient Adherence to Survivorship Treatment
- CRC
Colorectal cancer
- DAV
Disabled American Veterans
- EHR
Electronic health record
- HIPAA
Health Insurance Portability and Accountability Act
- US
United States of America
- VA
Veterans Affairs
- VAMC
Veterans Affairs Medical Center
- VHA
Veterans Health Administration
Authors’ contributions
HB, SD, DP, MK, and LZ contributed to the study’s concept and design. HB, SD, DP, and LZ contributed to the development of the survey instrument. JL performed all statistical analyses. SJ, JL, and VS contributed to the interpretation of study findings. SJ and IS contributed to the writing and revision of the manuscript. All authors reviewed, contributed revisions, and approved the final manuscript.
Funding
This study was funded by a VA Health Services Research and Development (HSR&D) Career Development Award (CDA 13–025). Dr. Zullig was supported by a VA Health Services Research and Development (HSR&D) Career Development Award (CDA 13–025). Dr. Bosworth was supported by a Research Career Scientist Award from VA HSR&D (VA HSR&D 08–027). Funders had no role in the design of the study, collection, analysis, or interpretation of the data, or in the drafting or revision of the manuscript.
Availability of data and materials
The datasets (including de-identified datasets) generated and analyzed during this study are not available publicly or upon request due to privacy and regulatory approvals.
Declarations
Ethics approval and consent to participate
This study and procedures used to obtain implied consent were approved by the Durham VA Health Care System Institutional Review Board (IRB) and performed in accordance with the ethical standards of the Declaration of Helsinki. Participants included in this analysis provided implied consent by returning a completed survey and completed a Health Insurance Portability and Accountability Act (HIPAA) authorization form. Consistent with IRB approval for this research study, permissions to access electronic health records and accompanying data use agreements were obtained from the Veterans Health Administration Patient Care Services and National Data Systems.
Consent for publication
Not Applicable.
Competing interests
Ms. Jazowski, Ms. Sico, Ms. Lindquist, Ms. Danus, Dr. Smith, and Dr. Provenzale report no conflicts of interest. Dr. Bosworth reports research grants from the PhRMA Foundation, Proteus Digital Health, Otsuka, Novo Nordisk, Sanofi, and Improved Patient Outcomes, as well as consulting from Sanofi, Novartis, Otsuka, Abbott, Preventric Diagnostics, Xcenda and the Medicines Company. Dr. Kelley reports research support from Bavarian Nordic, Novartis, AstraZeneca, and Bristol-Myers Squibb, as well as consulting from IBM Japan and Eisai. Dr. Zullig reports research support from Sanofi, Proteus Digital Health, and the PhRMA Foundation, as well as consulting for Novartis.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Health Research & Educational Trust. Social determinant of health series: transportation and the role of hospitals. www.aha.org/transportation. Accessed 15 Apr 2020.
- 2.Ambroggi M, Biasini C, Del Giovane C, Fornari F, Cavanna L. Distance as a barrier to cancer diagnosis and treatment: review of the literature. Oncologist. 2015;20(12):1378–1385. doi: 10.1634/theoncologist.2015-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas AA, Gallagher P, O’Ceilleachair A, Pearce A, Sharp L, Molcho M. Distance from treating hospital and colorectal cancer survivors’ quality of life: a gendered analysis. Support Care Cancer. 2015;23(3):741–751. doi: 10.1007/s00520-014-2407-9. [DOI] [PubMed] [Google Scholar]
- 4.Fazio L, Cotterchio M, Manno M, McLaughlin J, Gallinger S. Association between colonic screening, subject characteristics, and stage of colorectal cancer. Am J Gastroenterol. 2005;100(11):2531–2539. doi: 10.1111/j.1572-0241.2005.00319.x. [DOI] [PubMed] [Google Scholar]
- 5.Campbell NC, Elliott AM, Sharp L, Ritchie LD, Cassidy J, Little J. Impact of deprivation and rural residence on treatment of colorectal and lung cancer. Br J Cancer. 2002;87(6):585–590. doi: 10.1038/sj.bjc.6600515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sacerdote C, Baldi I, Bertetto O, Dicuonzo D, Farina E, Pagano E, et al. Hospital factors and patient characteristics in the treatment of colorectal cancer: a population based study. BMC Public Health. 2012;12(1):775. doi: 10.1186/1471-2458-12-775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cramb SM, Mengersen KL, Turrell G, Baade PD. Spatial inequalities in colorectal and breast cancer survival: premature deaths and associated factors. Health Place. 2012;18(6):1412–1421. doi: 10.1016/j.healthplace.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Sineshaw HM, Robbins AS, Jemal A. Disparities in survival improvement for metastatic colorectal cancer by race/ethnicity and age in the United States. Cancer Causes Control. 2014;5(4):419–423. doi: 10.1007/s10552-014-0344-z. [DOI] [PubMed] [Google Scholar]
- 9.Goins RT, Williams KA, Carter MW, Spencer M, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 10.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zullig LL, Jackson GL, Provenzale D, Griffin JM, Phelan S, van Ryn M. Transportation: a vehicle or roadblock to cancer care for VA patients with colorectal cancer? Clin Colorectal Cancer. 2012;11(1):60–65. doi: 10.1016/j.clcc.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guidry JJ. Aday La, Zhang D, Winn RJ. Transportation as a barrier to cancer treatment. Cancer Pract. 1997;5(6):361–366. [PubMed] [Google Scholar]
- 13.Zullig LL, Jackson GL, Dorn RA, Provenzale DT, McNeil R, Thomas C, et al. Cancer incidence among patients of the United States veterans affairs healthcare system. Mil Med. 2012;177(6):693–701. doi: 10.7205/MILMED-D-11-00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Cancer Institute: Surveillance, Epidemiology, and End Results Program. Cancer stat facts: colorectal cancer. https://seer.cancer.gov/statfacts/html/colorect.html. Accessed 15 Apr 2020.
- 15.U.S. Department of Veterans Affairs. Key statistics by veteran status and period of service. https://www.va.gov/vetdata/docs/SpecialReports/KeyStats.pdf. Accessed 15 Apr 2020.
- 16.Slind LM, Keating TM, Fisher AG, Rose TG. A patient navigation model for veterans traveling for cancer care. Fed Pract. 2016;33(Suppl 1):40–45. [PMC free article] [PubMed] [Google Scholar]
- 17.Washington DL, Bean-Mayberry B, Riopelle D, Yano EM. Access to care for women veterans: delayed healthcare and unmet need. J Gen Intern Med. 2011;26(Suppl 2):655–661. doi: 10.1007/s11606-011-1772-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buzza C, Ono SS, Turvey C, Wittrock S, Noble M, Reddy G, Kaboli PJ, Reisinger HS. Distance is relative: unpacking a principal barrier in rural healthcare. J Gen Intern Med. 2011;26(Suppl 2):648–654. doi: 10.1007/s11606-011-1762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schooley BL, Horan TA, Lee PW, West PA. Rural Veteran access to healthcare services: investigating the role of information and communication technologies in overcoming spatial barriers. Perspect Health Inf Manag. 2010;7:1f. [PMC free article] [PubMed] [Google Scholar]
- 20.Pfeiffer PN, Bowersox N, Birgenheir D, Burgess J, Forman J, Valenstein M. Preferences and barriers to care following psychiatric hospitalization at two veteran affairs medical centers: a mixed methods study. J Behav Health Serv Res. 2016;43(1):88–103. doi: 10.1007/s11414-015-9460-0. [DOI] [PubMed] [Google Scholar]
- 21.Zullig LL, Goldstein KM, Bosworth HB, Andrews SM, Danus S, Jackson GL, Provenzale D, Weinberger M, Kelley MJ, Voils CI. Chronic disease management perspectives of colorectal cancer survivors using the veterans affairs healthcare system: a qualitative analysis. BMC Health Serv Res. 2018;18(1):171. doi: 10.1186/s12913-018-2975-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zullig LL, Jazowski SA, Chawla N, Williams CD, Winski D, Slatore CG, et al. Summary of veterans health administration Cancer data sources. J Registry Manag. 2019;46(3):76–83. [PubMed] [Google Scholar]
- 23.Kim Y, Jeong KH, Kim E. A nationwide cross-sectional survey of student experiential practice at community pharmacies in South Korea. BMC Med Educ. 2019;19(1):445. doi: 10.1186/s12909-019-1879-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nawa N, Fujiwara T. Association between social capital and second dose of measles vaccination in Japan: results from A-CHILD study. Vaccine. 2019;37(6):877–881. doi: 10.1016/j.vaccine.2018.12.037. [DOI] [PubMed] [Google Scholar]
- 25.Brown JD, Vouri SM, Manini TM. Survey-reported medication changes among older adults during the SARS-CoV-2 (COVID-19) pandemic. Res Soc Adm Pharm. 2020;S1551–7411(20):31190–31196. doi: 10.1016/j.sapharm.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wheeler SB, Kuo TM, Durham D, Frizzelle B, Reeder-Hayes K, Meyer AM. Effects of distance to care and rural or urban residence on receipt of radiation therapy among North Carolina Medicare enrollees with breast cancer. NC Med J. 2014;75(4):239–246. doi: 10.18043/ncm.75.4.239. [DOI] [PubMed] [Google Scholar]
- 27.Sparling AS, Song E, Klepin HD, Foley KL. Is distance to chemotherapy an obstacle to adjuvant care among the N.C. Medicaid-enrolled colon cancer patients? J Gastrointest Oncol. 2016;7(3):336–344. doi: 10.21037/jgo.2016.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zullig LL, Shaw RJ, Crowley MJ, Lindquist J, Grambow SC, Peterson E, Shah BR, Bosworth HB. Association between perceived life chaos and medication adherence in a postmyocardial infarction population. Circ Cardiovasc Qual Outcomes. 2013;6(6):619–625. doi: 10.1161/CIRCOUTCOMES.113.000435. [DOI] [PubMed] [Google Scholar]
- 29.Ganasegeran K, Rashid A. The prevalence of medication nonadherence in post-myocardial infarction survivors and its perceived barriers and psychological correlates: a cross-section study in a cardiac facility in Malaysia. Patient Prefer Adherence. 2017;11:1975–1985. doi: 10.2147/PPA.S151053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong MD, Sarkisian CA, Davis C, Kinsler J, Cunningham WE. The association between life chaos, health care use, and health status among HIV-infected persons. J Gen Intern Med. 2007;22(9):1286–1291. doi: 10.1007/s11606-007-0265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ganasegeran K, Rashid A. Factors associated with perceived life chaos among post-myocardial infarction survivors in a Malaysian cardiac care facility. Medicina (Kaunas) 2018;54(5):79. doi: 10.3390/medicina54050079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Cancer Society. Chemotherapy for colorectal cancer. https://www.cancer.org/cancer/colon-rectal-cancer/treating/chemotherapy.html. Accessed 21 Apr 2020.
- 33.Harman LE. Ophthalmic complications related to chemotherapy in medically complex patients. Cancer Control. 2016;23(2):150–156. doi: 10.1177/107327481602300209. [DOI] [PubMed] [Google Scholar]
- 34.Veterans Affairs Medical Center Wilmington, Delaware. How to get ready for you colonoscopy. https://www.wilmington.va.gov/docs/services/How_to_Get_Ready_for_Your_Colonoscopy.pdf. Accessed 21 Apr 2020.
- 35.Mendes E. Seven key findings from 8-year study of cancer caregivers. Am Cancer Soc. https://www.cancer.org/latest-news/seven-key-findings-from-8-year-study-of-cancer-caregivers.html. Accessed 21 Apr 2020.
- 36.Northside Hospital. Transportation Program Eases Burden for Cancer Patients and Their Caretakers. https://www.northside.com/wtn/Page.asp?PageID=WTN000362. Accessed 21 Apr 2020.
- 37.CancerCare. A helping hand: the 2020 resource guide for people with cancer. https://media.cancercare.org/publications/original/178-helping_hand.pdf. Accessed 21 Apr 2020.
- 38.National Academies of Sciences, Engineering, and Medicine Transportation Research Board . Exploring data and metrics of value at the intersection of health care and transportation: proceedings of a workshop. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 39.Hilgeman MM, Moye J, Archambault E, Billings RL, Karel MJ, Gosian J, et al. In the Veteran’s voice: psychosocial needs after cancer treatment. Fed Pract. 2012;29(Suppl 3):51–59. [PMC free article] [PubMed] [Google Scholar]
- 40.Katz DA, McCoy K, Vaughan SM. Does improved continuity of primary care affect clinician-patient communication in VA? J Gen Intern Med. 2014;29(Suppl 2):682–688. doi: 10.1007/s11606-013-2633-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.U.S. Department of Veterans Affairs. VA NY Harbor Health Care System. Strength of camaraderie. https://www.nyharbor.va.gov/features/Strength_of_Camaraderie.asp. Accessed 21 Apr 2020.
- 42.Li CC, Matthews AK, Dossaji M, Fullam F. The relationship of patient-provider communication on quality of life among African-American and white cancer survivors. J Health Commun. 2017;22(7):584–592. doi: 10.1080/10810730.2017.1324540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jennerette CM, Mayer DK. Patient-provider communication: the rise of patient engagement. Semin Oncol Nurs. 2016;32(2):134–143. doi: 10.1016/j.soncn.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 44.Siple J, Harris EA, Morey JM, Skaperdas E, Weinberg KL, Tuepker A. Experiences of veterans with diabetes from shared medical appointments. Fed Pract. 2015;32(5):40–45. [PMC free article] [PubMed] [Google Scholar]
- 45.Mallya S, Daniels M, Kanter C, Stone A, Cipolla A, Edelstein K, D’Agostino N. A qualitative analysis of the benefits and barriers or support groups for patients with brain tumours and their caregivers. Support Care Cancer. 2020;28(6):2659–2667. doi: 10.1007/s00520-019-05069-5. [DOI] [PubMed] [Google Scholar]
- 46.Carroll JK, Humiston SG, Meldrum SC, Salamone CM, Jean-Pierre P, Epstein RM, Fiscella K. Patients’ experiences with navigation for cancer care. Patient Educ Couns. 2010;80(2):241–247. doi: 10.1016/j.pec.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rohan EA, Slotman B, DeGroff A, Morrissey KG, Murillo J, Schroy P. Refining the patient navigation role in a colorectal cancer screening program: results from an intervention study. J Natl Compr Cancer Netw. 2016;14(11):1371–1378. doi: 10.6004/jnccn.2016.0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Althubaiti A. Information bias in health research: definition, pitfalls and adjustment methods. J Multidiscip Healthc. 2016;9:211–217. doi: 10.2147/JMDH.S104807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.U.S. Department of Veterans Affairs. VA MISSION Act. https://missionact.va.gov/#. Accessed 21 Apr 2020.
- 50.U.S. Department of Veterans Affairs. Veterans Access, Choice and Accountability Act of 2014 (“Choice Act”) Fact Sheet. https://www.va.gov/opa/choiceact/documents/choice-act-summary.pdf. Accessed 21 Apr 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets (including de-identified datasets) generated and analyzed during this study are not available publicly or upon request due to privacy and regulatory approvals.