Abstract
Background and aim
The current COVID-19 pandemic scenario has driven surgical departments to a transformation.
The worldwide spread of the disease has led to a public health quarantine where health care professionals are at high risk of infection. In this context, telemedicine has been promoted and scaled up to reduce the risk of transmission. This study aims to demonstrate that a combined framework based on telematics and in-person clinical encounter not only ensures medical care but the safety of healthcare professionals and patients.
Material and method
Descriptive observational study on the follow-up of patients during the COVID19 Pandemic, combining telephone and traditional.
Results
A total of 5031 telephone calls were made, differentiating between medical referrals, specialised primary care visits, and outpatient consultation.
They were classified as successful, required an in-person visit, or no successful telephone contact. Furthermore, we divided them into 2 groups: resolved and unresolved.
53% of all telematic visits were successful.
Conclusions
Telematic medical systems are a feasible option in a orthopedics department and an interesting resource to preserve once the pandemic is resolved. Future lines of research should be opened to improve system success, analyze its cost-effectiveness ratio, and correct any legal conflicts that may exist.
Keywords: COVID-19, Telemedicine, Consultations, Visits, Telephone
Abstract
Antecedentes y objetivo
Durante la pandemia COVID-19 la actividad de los servicios quirúrgicos se ha visto obligada a adaptarse y transformarse. La telemedicina se está implantando como nunca antes en esta nueva situación en la que los pacientes están confinados y los profesionales sanitarios presentan riesgo de infectarse
El objetivo es mostrar que una reestructuración combinada telemática y presencial de las visitas permite asegurar la asistencia médica, garantizando la protección del personal sanitario y de los pacientes.
Material y método
Estudio descriptivo observacional sobre el seguimiento de pacientes durante la Pandemia COVID combinando la consulta telefónica con la presencial.
Resultados
Se realizaron un total de 5031 llamadas telefónicas diferenciando entre Derivaciones, Visitas de atención primaria especializada y Consulta externa hospitalaria.
Se registraron como efectivas, tributarias de visita presencial y no se logra contacto telefónico. Y las dividimos en 2 grupos resueltas y no resueltas.
Del total de visitas no presenciales telefónicas fueron efectivas un 53%.
Conclusiones
La medicina telemática es una opción factible en un servicio de traumatología y de manera adecuada será una opción interesante de mantener tras la pandemia.
Futuras líneas de investigación deberían ser abiertas para mejorar la capacidad de resolución de este sistema, analizar su relación coste-efectividad y subsanar los conflictos legales que pudieran existir.
Palabras clave: COVID-19, Telemedicina, Consultas, Visitas, Telefónica
Introduction
Telemedicine is a field which uses technological innovation in telecommunications to diagnose and treat patients. It was initially promoted to overcome geographical barriers and provide help in special situations.1
This technology has gained in popularity over the last few years and different applications have been developed: education (among professionals), teleconsultation (among specialists or primary care and specialty clinicians), patient follow-up, and even telesurgical or telerobotic systems.2
At the end of 2019, the first case of infection by SARS-CoV-2 or COVID-19, was identified in Wuhan (Hubei province), China. This infection evolved into a global pandemic, testing the response capacity of healthcare systems.
In a report published in The Lancet,3 Paul Webster analysed how telemedicine is becoming established now more than ever under these new circumstances, where patients are confined and healthcare professionals are at risk of contagion. As indicated by the author, the increase in COVID-19 cases is changing the healthcare model worldwide.
The activity of surgical services has also been forced to adapt and transform. General recommendations from the Spanish Orthopaedic and Trauma Society of Surgery against COVID-19, which were updated on 13th April 2020,4 include:
-
1
Prioritising telework to avoid contact between individuals and, whenever possible, have telematic consultations, reserving only urgent visits (those where delay could lead to permanent sequelae in the patient).
-
2
Suspend scheduled surgery, except oncological surgery or emergency surgery which could otherwise lead to permanent sequelae in the patient.
Although these recommendations would not come before the directives of each health centre, the fact is that most of them have adopted these measures.
In the Hospital Universitari Mútua Terrassa, since the beginning of the state of alarm from the COVID-19 pandemic, visits to specialised primary care (SPC) and to outpatient hospital consultations (OHC) have been suspended. Only essential face-to-face visits have been maintained.
The purpose of this study is to show whether a combined telematic and on-site restructuring of visits would ensure medical care, guarantee the protection of healthcare personnel and that of patients, prevent possible spread of the infection and effectively use telecommunications to maintain the healthcare system’s stability and patient care.
Material and methods
The Hospital Universitari Mútua Terrassa (HUMT) provides primary and specialised care to a population of 260,000 inhabitants, covering the areas of the Vallés Occidental Oest and the Baix Llobregat.
Since 14th March 2020, when the national state of emergency was declared, on-site visits to primary care centres (PCC) and OHC were cancelled for all non-emergency patients, generating an accumulation of 2572 visits which did not take place.
Once the need for collaboration between trauma clinicians in the medical emergency services had dropped, from 20th April 2020 onwards the orthopaedic and trauma surgery department (OTS) was reorganised to recover its non-surgical activity. The impossibility of recuperating on-site visits necessitated the introduction of a telemedicine programme to ensure continuity of medical care.
In keeping with hospital management, an emergency plan was designed for telephone and on-site care.
Reviewed visits were of three types:
Referrals (R): patients referred by the family doctor (GP) to SPC, pending an appointment.
Visits to specialised primary care: patients with appointment in PCC practices, for assessment or follow-up by the trauma surgeon.
Outpatient’s consultations: visits for postoperative check-ups and follow-up or to include patients on the waiting list for surgery.
Telephone calls were considered:
Effective: when they resolved the user’s need in four possible ways: solving the pathology or cure; communication of results from complementary tests; medical recommendations and follow-up visits.
Face-to-face consultation referral: where telephone contact did not prevent an on-site visit for examination, treatment or inclusion onto the waiting list for surgery.
No telephone contact made: telephone contact was unable to be made with the user after three attempts.
All telephone consultations were carried out by the OTS department by attending physicians.
In the first two weeks a total of 2572 telephone calls were made, 922 of which were not resolved (667 SPC + 255 OHC).
Later, at the start of the scaling down on 27th April, the reduction in the prevalence of the disease made it possible to initiate on-site consultations. A total of 497 face-to-face visits were combined, (255 OHC unresolved by phone and 242 appointments already made prior to the pandemic) with telephone consultation of 2459 R.
To ensure the safety of both the patients and the healthcare personnel, a care protocol was made for on-site visits (Appendix BANEXO I).
A model was designed which led to 160 visits per day (20 patients/day/consulting room), which amounted to a maximum of 800 on-site visits per week.
From the third week of scaling down, on 11th May 2020, the on-site visits scheduled prior to the pandemic began and telephone consultation was maintained for the R visits and the SPC visits, since the PCCs remained closed.
Results
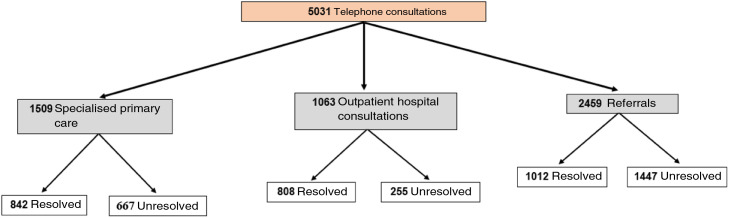
A total of 5031 telephone calls were made, distributed in the following manner (Fig. 1 ):
Figure 1.
Flow chart of consultations.
Some 2572 telephone non face-to-face visits were made (SPC and OHC). Of these, 1650 (64%) were effective or discharges and 922 (36%) required on-site visits, or no telephone contact was made.
Within the telephone consultations of SPC, out of 1509, 842 (56%) were resolved over the phone and the remainder 667 (44%) required on-site visits or no phone contact was made.
Of the patients whose outpatient consultations were cancelled (check-ups on patients who had undergone surgery or were in treatment and initial visits), 1063 patients were called: 808 (76%) were considered effective and 255 (24%) were unresolved, required on-site visits or were unable to be contacted over the phone.
The first week of on-site visits were undertaken with a total of effective 586 OHC, 16 did not attend and 172 were not given appointments because risk was detected in the questionnaire prior to consultation, or they were not able to be contacted by phone.
A total of 2459 patients had referrals from GPs, of whom 1010 (41%) were resolved by phone and the remaining 1447 (59%) required on-site visits or were unable to be contacted by phone.
53% of the total telephone consultations were effective.
Discussion
Telemedicine is defined as the remote diagnosis or treatment of patients through telecommunications technology.5 In 2017, only 6.6 consultations per 100,000 inhabitants were made in U.S.A.6 The appearance of the COVID-19 pandemic changed this reality.
The COVID-19 pandemic in 2020 in Spain has posed a challenge for both specialists and trauma surgeons, who have provided support to different services with major care load.
This advance has helped to preserve healthcare resources, and personal protection equipment, leading to safe and quality patient care, maintaining social distance and minimising virus propagation. In the area of orthopaedic surgery telemedicine is already being used to make virtual visits in geographically decentralised areas (rural Iowa7 and Norway8) and in follow-up of prosthetic surgery.9
Our experience during the pandemic is that, in addition to care, it has provided a communication system both for graduate training programmes and for the training of residence medical interns. This experienced has been published by Elkbuli et al.10
However, in situations where there is no crisis, the adoption of telemedicine programmes requires time, as noted by Moazzami, together with resources, financing and specific guidelines.11
In our case, the model was created without financing and with the personal resources generated by the absence of surgical activity. As the number of infections falls and with it the affluence of people using the emergency services with breathing problems, the trauma surgeons have been able to progressively return to treating patients of their specialty.
During the initial stage of the downscaling of lockdown, the number of patients who had stopped consulting was assessed. The fact that elective surgery was not initiated and that ICCs were closed, allowed specialists to begin care of OTS patients. Similarly, given the state of emergency, most of the population were at home, which facilitated telephone contact.
In 2020, Cremades et al. published the results of a study in which they included a randomised sample of 200 patients for on-site or telemedicine consultations for postoperative follow-up. The first aim was to demonstrate whether they had the capacity to complete follow-up of all patients. This objective was met for 90% of the patients with on-site consultations and for 74% of telephone consultations. Among secondary objectives was the fact that clinical outcomes were similar and that patient satisfaction was extremely high in both groups.12
Telephone consultations were completely made by orthopaedic and trauma surgery specialists in order to increase the ability for resolution and to reassure the patient.
The number of referrals resolved over the phone has shown that a patient’s demand for a specialist may be regarded as satisfied through a telephone conversation. The fact that many pathologies were resolved also suggests that there could have been a number of primary care referrals which were avoidable. This situation changed the relationship with family medical specialists, creating a non on-site referral circuit that could be resolved in electronic medical history, with a phone call or an on-site consultation in PCC or hospital, depending on the trauma criterion.
Similarly, these visits have led to the detection of cases which have been directly referred to hospital outpatient consultation, due to their severity, cutting delayed access to the specialist and reducing the number of trauma surgeon visits in the PCC.
Regarding SPC visits, telephone consultation has led to the finalisation of a prior process, to follow-up or to hospital referral, and to request further appropriate complementary examination for future on-site consultation. Cases are thus resolved and second visits avoided.
The OHC have reported that total hip or knee replacement check-ups for the period between two and 10 years after surgery, may be sufficiently performed over the phone.
Forbes et al. listed the factors which require optimisation prior to extending the establishment of telemedicine. These factors include: leadership among healthcare professionals; the development of invoicing processes; the creation of licences; data integration systems; privacy and safely measures and the determination of clinical assessment methods for patients. With the COVID-19 pandemic, most of these barriers have been quickly resolved or circumvented, facilitating their implementation.13
Smith et al. published eight elements which establish a quick guide of implementation and integration of telemedicine in its service. These elements are: electronic medical infrastructure for recording of patients and data; audiovisual platforms; institution computer support; development of provider hardware for the service and the patients; training of personnel; patient training; participation of patients and caregivers and integration of codification and invoicing systems.14
The context in which this project was developed has accelerated its implementation and encouraged patient acceptance of the change in format.
Like other state centres, once the model has been established, they will begin to add new tools to maintain this activity without losing quality in care and reducing on-site visits that facilitate earlier access when it is truly necessary.
Conclusion
Analysing our experience, we could say that telematic medicine is a viable option in a trauma surgery service and when appropriately processed, it would be an interesting option to maintain after the pandemic.
The exceptional circumstances of the healthcare situation during the COVID-19 pandemic has accelerated the introduction of a telemedicine model where consultations can be carried out safely, comfortably and effectively for the patient. Future lines of investigation should be open to improving the problem-solving capacity of this system, analysing cost-effectiveness and amending any possible legal conflicts.
Screening and detection of possible COVID-19 symptoms: the day before the appointment a telephone survey was performed to detect symptoms compatible with infection in the 15 days before the call (Table 1 ).
Table 1.
Results of telephone consultations.
| Referrals | Specialised primary care | Outpatient consultations | Total | |
|---|---|---|---|---|
| Total | 2459 | 1509 | 1063 | 5031 |
| Effective | 1012 | 842 | 808 | 2662 |
| Unresolved | 1447 | 667 | 255 | 2369 |
Safe space design: opening of an outpatient floor in a building annexed to the hospital, closed during the pandemic. Based on this space, the number of patients was calculated according to the number of offices and waiting rooms available. Eight offices and four waiting rooms were used to safely accommodate the patient arriving for consultations.
Administrative staff were appointed for reception and location in waiting rooms, depending on which consulting room they were to go to.
Timings were changed for each visit every 20 min, with a maximum of 16 patients waiting each hour (32 if they came accompanied), distributed in four waiting rooms with 97 seats, thus guaranteeing a safe distance between each person.
Recommendations for care:
-
a
Punctuality.
-
b
No companions if possible.
-
c
Wearing a mask, or being given one on entry.
-
d
Use of hydroalcoholic gel for hand hygiene, prior to entry, available at the door of the building.
-
e
Respect for safe distancing.
Financing
This study received no type of financing.
Conflict of interests
The authors have no conflict of interests to declare.
Level of evidence
Level of evidence IV.
Footnotes
Please cite this article as: Miguela Álvarez SM, Bartra Ylla A, Salvador Carreño J, Castillón P, García Cardona C, Anglès Crespo F. Consultoría telefónica en COT durante la pandemia por COVID-19. ¿Ha venido para quedarse? Rev Esp Cir Ortop Traumatol. 2021;65:167–171.
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.recot.2020.07.008.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Waterman B.R., Laughlin M.D., Belmont P.J., Schoenfeld A.J., Pallis M.P. Enhanced casualty care from a Global Military Orthopaedic Teleconsultation Program. Injury. 2014;45:1736–1740. doi: 10.1016/j.injury.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 2.Huang E.Y., Knight S., Roginski C., Hambleton Davis C., Moller M., Slama E. The American Journal of Surgery Telemedicine and telementoring in the surgical specialties: a narrative review. Am J Surg. 2019;218:760–766. doi: 10.1016/j.amjsurg.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Webster P. Virtual health care in the era of COVID-19. Lancet. 2019;395(10231):1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.SECOT. Recomendaciones generales de la Sociedad Espa ñola de Cirugía Ortopédica y Traumatología frenteal COVID-19. Accessed 13 April 20. Available from: https://sogacot.org/wp-content/uploads/2020/05/RecomendacionesSECOTGeneralesDeCOTFrenteAlCovid19.pdf.
- 5.Bashshur R.L., Shannon G.W., Krupinski E.A., Grigsby E., Kvedar J.C., Weinstein R.C. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15:600–610. doi: 10.1089/tmj.2009.9960. [DOI] [PubMed] [Google Scholar]
- 6.Barnett M.L., Ray K.N., Souza J., Mehrotra A. Trends in Telemedicine Use in a Large Commercially Insured Population, 2005-2017. JAMA. 2018;320:2147–2149. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gruca T.S., Pyo T.-H., Nelson G.C. Improving Rural Access to Orthopaedic Care Through Visiting Consultant Clinics. J Bone Joint Surg Am. 2016;98:768–774. doi: 10.2106/JBJS.15.00946. [DOI] [PubMed] [Google Scholar]
- 8.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25:451–459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
- 9.Marsh J., Hoch J.S., Bryant D., MacDonald S.J., Naudie D., McCalden R. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am. 2014;96:1910–1916. doi: 10.2106/JBJS.M.01558. [DOI] [PubMed] [Google Scholar]
- 10.Elkbuli A., Ehrlich H., McKenney M. The effective use of telemedicine to save lives and maintain structure in a healthcare system: current response to COVID-19. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moazzami B., Razavi-Khorasani N., Dooghaie Moghadam A., Farokhi E., Rezaei N. COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. J Clin Virol Off Publ Pan Am Soc Clin Virol. 2020;126 doi: 10.1016/j.jcv.2020.104345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cremades M., Ferret G., Parés D., Navinés J., Espin F., Pardo F. Telemedicine to follow patients in a general surgery department. A randomized controlled trial. Am J Surg. 2020;219:882–887. doi: 10.1016/j.amjsurg.2020.03.023. [DOI] [PubMed] [Google Scholar]
- 13.Forbes R.C., Solorzano C.C., Concepcion B.P. Surgical telemedicine here to stay: more support from a randomized controlled trial on postoperative surgery visits. Am J Surg. 2020 doi: 10.1016/j.amjsurg.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith W.R., Atala A.J., Terlecki R.P., Kelly E.E., Matthews C.A. Implementation Guide for Rapid Integration of an Outpatient Telemedicine Program During the COVID-19 Pandemic. J Am Coll Surg. 2020 doi: 10.1016/j.jamcollsurg.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.