Abstract
As the COVID-19 pandemic continues, important discoveries and considerations emerge regarding the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) pathogen; its biological and epidemiological characteristics; and the corresponding psychological, societal, and public health (PH) impacts. During the past year, the global community underwent a massive transformation, including the implementation of numerous nonpharmacological interventions; critical diversions or modifications across various spheres of our economic and public domains; and a transition from consumption-driven to conservation-based behaviors. Providing essential necessities such as food, water, health care, financial, and other services has become a formidable challenge, with significant threats to the existing supply chains and the shortage or reduction of workforce across many sectors of the global economy. Food and pharmaceutical supply chains constitute uniquely vulnerable and critically important areas that require high levels of safety and compliance. Many regional health-care systems faced at least one wave of overwhelming COVID-19 case surges, and still face the possibility of a new wave of infections on the horizon, potentially in combination with other endemic diseases such as influenza, dengue, tuberculosis, and malaria. In this context, the need for an effective and scientifically informed leadership to sustain and improve global capacity to ensure international health security is starkly apparent. Public health “blind spotting,” promulgation of pseudoscience, and academic dishonesty emerged as significant threats to population health and stability during the pandemic. The goal of this consensus statement is to provide a focused summary of such “blind spots” identified during an expert group intense analysis of “missed opportunities” during the initial wave of the pandemic.
Keywords: Blind spots, COVID-19, international health security, lessons learned, pandemic response, public health, public services, risk management, supply chains
Blindspot: An area in which one fails to exercise judgment or discrimination
–Merriam Webster Dictionary
Blind spotting: When a situation or an image can be interpreted in two different ways, but the participant can only see one of the interpretations (primary definition)
Using someone's ignorance, or misinformation, in order to manipulate for selfish gain (alternative definition)
–Urban Dictionary
INTRODUCTION
As the first “rolling wave” of the COVID-19 pandemic transitions into subsequent waves, the world is preparing and waiting in anticipation to see if public health (PH) measures designed to soften the impact are effective.[1,2] The pandemic has proven how interdependent the global community is when facing an international health security (IHS) threat. It also became clear that, governments around the world need to embrace key leadership qualifications in disaster and health security threat education, including a moral and ethical obligation to rely on established expert resources. Given our collective experiences to-date, it has become clear that evident officials may require a “fitness to lead test” (e.g., leadership competency) in the area of health security and pandemic preparedness. More specifically, those in key leadership positions should seek appropriate consultation from established content experts/advisors, with curbs to executive power when it comes to any proposed deviation(s) from scientifically established, life-saving PH measures. Consequences of incompetence or lack of preparedness in this critical area can be devastating and far reaching.
Although much has been learned during the global society's initial encounter with the novel coronavirus, a lot remains to be elucidated. In addition, the collective memory of what worked and did not work during the global response to the first wave may not be long lasting if experiences with past outbreaks and pandemics stay true.[3,4] Furthermore, what is believed to be the “correct” answer as a result of our initial experiences may be easily reversed as new evidence is collected and published (e.g., transition from “no mask” to “mandatory mask” regimes).[3,5,6] Within this very context, we must also acknowledge that the world and the reality around us continue to change, and what has worked in the past may not necessarily be equally applicable in the future.
Effective leadership in the matters of PH concern is mandatory. It is unacceptable for our political leaders to be ill informed and complacent toward political, social, economic, and scientific evidence. For instance, in the USA, many COVID-19 outbreaks appeared to be contained by early June 2020. By the beginning of July, however, the number of new cases skyrocketed to more than 54,500 per day.[7] Moreover, a number of complacent leaders who openly advocated for less strict application of nonpharmacological interventions (NPIs, e.g., hand washing, universal facial coverage, social distancing, and avoidance of crowds and closed spaces) have themselves contracted the disease.[8,9,10] As of the writing of this article (November 2020), many countries are experiencing a well-defined second wave of the pandemic. Although many of the factors associated with this resurgence remain to be elucidated, it is increasingly clear that the degree of implementation and compliance with key NPIs may play an important role.[3,11,12] This is not unique to the USA, as other countries have experienced similar resurgences in cases, resulting in either successful containment or the emergence of a new outbreak.[13,14]
Premature or poorly designed re-openings of local and regional economies, including key public institutions, appear to be an important factor in the resurgence of COVID-19 cases,[15,16] especially when considered in the context of transmission involving asymptomatic carriers and many unknowns associated with this important phenomenon.[3,17] Those who attend public events with hundreds and possibly thousands of people in relatively close proximity should be aware that it does not take many new cases to re-ignite the outbreak, especially when considering that those newly infected will be asymptomatic and infectious for several days after contracting the virus.[3] Therefore, it is important to understand that masks are very effective, but not a perfect solution. At the population level, there appears to be a fine balance between the risks of “social distancing at in-person events” and the effect of “stay-at-home” behavior in terms of net viral transmission.[18] It is evident that government leadership and understanding of PH problems and their consequences is of paramount importance.
The goal of this consensus paper is to provide a high-level overview of potential PH “blind spots” of which political leaders should be cognizant. In addition, the IHS community may need to recognize and address these blind spots during any subsequent waves of the COVID-19 pandemic to assist local, regional, and national governments. The current manuscript is divided into sections dedicated to specific areas that were felt by our Multidisciplinary American College of Academic International Medicine-World Academic Council of Emergency Medicine Consensus Group to represent opportunities for inclusion in a sustainable future pandemic management framework. To help the reader navigate this extensive manuscript, we provide an executive summary of the 14 blind spots discussed in Table 1. In addition, Figure 1 provides a word cloud reflecting the most common themes of this consensus paper.
Table 1.
Summary of COVID-19 “blind spots” discussed in this Multidisciplinary American College of Academic International Medicine-World Academic Council of Emergency Medicine Consensus Group Statement
| Blind spot #1: Politicizing the process |
| Proposed solutions |
| Setting up process curbs for politicians and other stakeholders |
| Enforcing the reliance on content experts to manage a pandemic |
| Use of tactful assertiveness and fact checking to rectify misinformation |
| Blind spot #2: General complacency |
| Proposed solutions |
| Ongoing education regarding the pandemic, including signs of early resurgence of infections as well as any updates regarding known symptoms of the disease |
| Continuous vigilance regarding PPI utilization and NPIs |
| Use of tactful assertiveness and fact checking to rectify misinformation |
| Blind spot #3: Ignoring simple and effective nonpharmacological measures |
| Proposed solutions |
| Rigorous and systematic study of past and current experiences with pandemics, including real-time realignment of priorities, public health education, and behaviors to accommodate required change |
| Instituting well-designed, well-tested reopening strategies, with clearly established escalation and de-escalation points and procedures |
| Focus on excellent contact tracing, especially during the early phases of the outbreak. Implementation of modern epidemiological tools, such as SM and mobile device case tracing and “early warning” systems |
| Blind spot #4: Dealing with concomitant public health challenges and prevention of excess mortality |
| Proposed solutions |
| Implementation of a well-thought-out plan for the management of chronic health conditions during a pandemic |
| Need to embrace modern technological advances, both in terms of point-of-care testing and reliable tele-presence, both for the pandemic illness and key chronic health conditions |
| Close monitoring and support for patients with post-COVID syndrome, including assurance that any post-COVID syndrome manifestations and symptoms are exempt from “preexisting condition” clauses, proactively treated, and appropriate basic, translational, and clinical research is supported |
| Maintenance of robust and flexible capacity to address any simultaneous infectious disease threats, including both endemic and potentially emerging disease threats |
| Blind spot #5: Long-term care needs and the PICS |
| Proposed solutions |
| Implementation of a well-thought-out and robust plan for the management of large number of patients who require chronic rehabilitation after recovering from COVID-19 |
| Provision of necessary support, including appropriate patient assistance and the availability of physical therapy, occupational therapy, and specialty rehabilitation services (e.g., pulmonary, cardiac) |
| Establishment and maintenance of strong mental health support network, both for recovering pandemic victims and for health-care providers |
| Blind spot #6: Pseudoscience and academic dishonesty |
| Proposed solutions |
| The scientific community needs to implement an efficient, peer-driven, real-time “fact-checking” system, with built-in mechanisms for correcting information shown to be incorrect |
| The public must be vigilant about information claimed to be of sound scientific origin. This should include building trust, communication, and mutual reliance between the public and the scientific community |
| Creation of robust mechanisms for ensuring that any information shared on various media platforms, including SM, is “fact checked” and flagged and/ or removed if incorrect |
| Acts of scientific dishonesty must be addressed by the scientific community promptly, with clearly delineated disciplinary process and subsequent sanctions, if indicated |
| Blind spot #7: The emergence of vulnerabilities within health-care systems |
| Proposed solutions |
| Systems that protect equal right to health care for all citizens should be in place during the time of the pandemic, regardless of socioeconomic status, race, gender, or any other consideration |
| Protections should be instituted for those who lost their employment due to COVID-19, including guaranteed continuation of health coverage for both unemployed workers and their families |
| Robust, easy-to-access screening capabilities should be introduced, along with robust contact tracing to help intercept early outbreak propagation |
| Telemedicine platforms should be embraced, implemented, and utilized widely. This is especially relevant in the context of long-term health maintenance, mental health, and chronic health conditions. Corresponding infrastructure (e.g., Internet connections, Wi-Fi, and cellular communication) should be reliable and well maintained |
| PPE should be a priority for leadership at all levels of the government and health-care institutions. Diligent restocking and PPE quality assurance systems should be in place and operating at all times |
| Blind spot #8: Jurisdictional and administrative perspectives |
| Proposed solutions |
| Governments and health-care institutions are strongly encouraged to increase collaborative efforts, inclusive of bidirectional initiatives in the areas of knowledge exchange, skills training, pandemic approaches, and many other directly and indirectly relevant domains |
| Frequent considerations of the balance between personal freedoms and societal “greater good” must be undertaken. Whenever possible, flexible policies should take into consideration emerging scientific evidence and our evolving understanding of the pandemic |
| Human considerations must be kept in the forefront of jurisdictional and administrative policymaking, including a careful balance between NPI, social distancing, quarantine, or shelter-in-place orders, as well as any pertinent considerations regarding PPE |
| Government actions should focus on ensuring that pandemic-related policies, procedures, and recommendations are well balanced with the economic sequelae of said policies, procedures, and recommendations. This preferably includes a sliding-scale, deliberate approach to pandemic-related restrictions in the context of the best available public health data, scientific evidence, and frequent re-assessment of the situation |
| Blind spot #9: Essential infrastructure and public works |
| Proposed solutions |
| Careful consideration of the need for continued operation of various public services should be made on an ongoing basis. Whenever possible, tele-presence is preferred to in-person activities |
| When absolutely necessary, public buildings and key infrastructure should be made as “pandemic proof” as possible. This may include dedicated modifications such as social-distancing markings; plexiglass or glass dividers; dedicated high-efficiency air filtration devices; ample, readily available, and frequently re-stocked hand washing products; readily available PPE, with “no exception” policies; and frequent, strictly followed disinfection schedules |
| Appropriate monitoring of public water, sewage, and waste management facilities needs to contain appropriate mitigation measures and procedures to ensure that disease spread can be controlled if such facilities are found to be within the chain of transmission |
| Critical supply chains, including those involving water, food, pharmaceutical, medical, and PPE supplies, must be protected. Frontline personnel must receive all the necessary protective equipment and any other necessary resources to maximize their safety and well-being (as well as the safety and well-being of all social contacts of frontline personnel) |
| Blind spot #10: Research and development |
| Proposed solutions |
| Open-minded, innovative approaches should be embraced, including the use of novel diagnostic and therapeutic modalities. Appropriate regulatory framework should be put into action, immune to undue influences of asymmetric market participants (e.g., pharma industry, well-established medical equipment makers, and other actors with sufficient political and economic power to prevent new market entrants) |
| Highest possible ethical standards should be embraced by all stakeholders. Therapeutic agents, medical equipment, and vaccines should not bypass fundamental safety and efficacy assessment processes. At the same time, efforts should be made to ensure that any required safety and efficacy assessments can be expedited as much as safely and ethically possible |
| Blind spot #11: Racial and social disparities |
| Proposed solutions |
| Racial and social disparities, for various reasons, tend to become more pronounced during the time of pandemic. It is critical for governments, health-care institutions, and communities to ensure that resources are allocated equitably and that pandemic response effort does not exacerbate the existing inequities |
| Economic effects of the pandemic tend to disproportionately affect racial and other minority groups. Consequently, deliberate efforts must be made to ensure equitable distribution of any economic assistance programs to all segments of the population |
| Education regarding unconscious/implicit biases, diversity, microaggression, and other topics that directly or indirectly contribute to racial and social disparities, should be broadly encouraged |
| Blind spot #12: The COVID-19 economy, mental health, and violence |
| Proposed solutions |
| Appropriately structured, well-thought-out economic stimulus plans should be implemented to help bridge key economic performance gaps resulting from society-wide sacrifices made to control the pandemic. Any such economic stimulus measures should holistically consider other blind spots discussed in this document |
| It is well established that economic downturns may increase the incidence of mental health complaints as well as interpersonal violence. Consequently, efforts to encourage and/or re-start economic activity following any quarantine or stay-at-home orders should be paralleled by efforts to proactively address downstream consequences of economic slowdown and social distancing - mental health issues and interpersonal violence |
| Blind spot #13: Potential viral reservoirs and risks associated with virology research |
| Proposed solutions |
| For SARS-CoV-2 and other zoonotic illnesses, the initial “jump” from an existing animal reservoir into the human population constitutes the single-most critical step required for an outbreak (and subsequently, pandemic) to start. Consequently, efforts to identify, catalog, and monitor any potential zoonotic-to-human “touch points” should be at the forefront of preventing future pandemics |
| Several potential reservoirs of SARS-CoV-2 have now been identified, including feline, ferret, bat, mink, and various rodent populations. These reservoirs represent not only a potential avenue for the virus to re-emerge but may also serve as “mutation and evolution laboratories” for the virus to become more virulent and/or more infectious. Consequently, proactive and aggressive action must be taken if any new knowledge or understanding of the above emerges. One example is the recent discovery of possible human-to-mink-to-human transmission chain, complete with the emergence of new variant of the virus |
| Research facilities actively working on SARS-CoV-2-related projects must take strict precautions regarding the shipping, handling, and disposal of any virus and/or virus-containing materials. Appropriate safety mechanisms and cross-checks must be implemented at all times, without exceptions |
| Blind spot #14: Homelessness and COVID-19 |
| Proposed solutions |
| Homeless populations across the globe are among the most vulnerable to the devastation and rapid spread of SARS-CoV-2. There are numerous documented instances of uncontrolled COVID-19 spread “under the radar” within homeless populations, with the constant potential for rapid emergence of local outbreaks. It is recommended that local, regional, and national governments provide all the necessary support (e.g., food, shelter, and medical care) to homeless populations to help stop the spread of the pandemic. Opponents of such programs, especially those who advocate against widespread social initiatives, must realize that the final cost of the latter will be much less than the cost of subsequent outbreaks (both from economic and more importantly human perspectives) |
| Homeless assistance programs designed to help address the transmission of SARS-CoV-2 may represent an important opportunity to re-introduce (and re-engage) an entire segment of our population into various other assistance programs (e.g., employment, housing, and education) |
| PPE: Personal protective equipment, NPI: Nonpharmacological interventions, SM: Social media, PICS: Postintensive care syndrome |
Figure 1.

Word cloud reflecting the most common themes of the current consensus paper
Blind spot #1: Politicizing the process
Public health blind spotting by senior elected political executives has become a serious problem during the COVID-19 pandemic.[19,20] This type of blind spotting can be political and/or cognitive, and can have devastating consequences.[21,22] For some, the circumstances of this global event are being used as a means to a political end, to enhance division as a form of electioneering; or there may be a cognitive blind spot in some leaders' ability to process important matters related to PH and society's safety.[23,24] Countries that have transformed the pandemic into a political issue have prioritized the destructive element of human conflict, rather than addressing COVID-19-specific challenges, often to the citizen's detriment.[25] In many situations, political leaders fail to fully appreciate the true scope of the problem. Subsequently, these countries have endangered their citizenry through a lack of transparency at best, deception at worst. This, in turn, may have contributed to higher morbidity and mortality and further political divide. Media, and especially social media (SM) outlets, play a significant role in this context.[26,27] Furthermore, the politicization of the process leads to confusing messages. For instance, the information regarding the use of masks seems to have become a political matter.[28] Messages from various medical and political factions have led to confusing perspectives in the general population regarding masks, and hindered educational efforts with regard to how and when to use a mask.[29] In order to avoid such politicization in educational, quarantine, and tracing efforts, it is important to ensure that properly trained personnel are empowered to act in a purely nonpolitical manner.
The use of a pandemic as a political truncheon by a politician or a group, although unacceptable, is difficult to avoid in a nonutopian setting.[30,31] Competitive pressures of modern, fast-paced politics tend to blend with PH agenda in often unpredictable and sometimes harmful ways.[26,27,32,33] Moreover, a cognitive bias regarding PH matters (i.e., the inability to discern the problem and its required or sensible remedies) or the lack of insight into the consequences of such a bias can be incredibly damaging to a society's social fabric, its economy, and its ability to conduct competent international political relations or business/industrial endeavors. Finally, the public should be sufficiently aware of the “political reality” versus the “pandemic reality” to be able to effectively navigate and differentiate between a true leadership “rallying cry” and a populist “political battle cry.” Governments should not only be able to learn from the past but also flexibly apply past experiences in the context of the modern society (e.g., our ability to use modern technological tools to work remotely makes the current economic environment substantially different from previous pandemics).[34,35]
There is no better example of the negative PH effects of confusing and conflicting communication than facial PPE guidelines in the US during the early-to-mid 2020 period. Once it became clear that SARS-CoV-2 was spread through respiratory droplets, it stands to reason that facial PPE would be integral to reducing transmission. Given runs on basic supplies such as toilet paper and disposable gloves, the public was initially advised against mask wearing.3 This was an effort to conserve PPE for health care workers (HCW) but unfortunately established a political dichotomy that was further entrenched by messaging from certain elements within the national leadership.
In the latter context, it is critically important that political leaders possess appropriate cognitive abilities, procedural hard stops, and advisory capacity to put into place effective solutions.[36] The competence of senior political executives with regard to PH is of paramount importance. A basic knowledge of PH should be required of all candidates for a senior political post, although admittedly this will be difficult to define and/or enforce.[37,38] In this way, briefings held by technical/content experts for the edification of those in power will be better understood, and there can be a firm PH foundation on which proper decisions are based. As such, it is imperative that leaders of nations, regions, and municipalities understand the basic PH tenets of disease spread, disease prevention, as well as the development and use of vaccines and therapeutics. This can then help facilitate the adoption of measures that will ensure supply chains necessary to attain required products and devices, pharmaceuticals (including therapies, vaccines, distribution and storage capacity), the implementation of practical interventions, and effective legislation to protect the public. The COVID-19 pandemic has emphatically demonstrated the blind spotting of governments with regard to key principles of PH and the scientific method.[39,40]
Blind spot #2: General complacency
The current pandemic, at its core, constitutes a collection of fast-moving regional outbreaks that coalesced into a global event.[3] The SARS-CoV-2's high infectivity, asymptomatic carriers, relatively long asymptomatic phase, and general complacency all combine to create a highly volatile environment that facilitates the rapid spread of COVID-19.[41] In many regional outbreaks, the low initial number of cases along with mild disease symptoms among a vast majority of those infected contributed to a false sense of security.[42,43] Due to concerns over the economic consequences of local shutdowns, governmental authorities may initially choose to err on the side of less restrictive NPI policies. This, in turn, may result in faster rise in cases, greater magnitude of outbreak peaks, and more prolonged outbreak tails.[1,3,44] Unfortunately, it is not unusual for governments to fail to recognize the potential of SARS-CoV-2 to rapidly enter the exponential case growth phase, at which point only a massive (and largely reactive) response will be able to mitigate the effects of the out-of-control transmission chain. Mortality rates in the latter scenario tend to be much greater than those observed under better controlled conditions.[3,45,46] Below are two key considerations specific to Blind Spot #2:
Proactive implementation of nonpharmaceutical interventions (NPIs) – In general, regions of the world that took the stay-at-home approach, aggressive testing, contact tracing, and physical distancing with masks have sacrificed short-term inconvenience for long-term success.[3] South Korea and Singapore represent two examples of this critical strategy with positive outcomes.[47] The same can be said about regions in Europe that were able to effectively control the case incidence rate.[48,49] Countries with heterogeneous messaging that did not adequately address the necessary strategy in a unified manner have experienced significantly more new cases and suffering. Furthermore, the authors expect that unique challenges will arise in relation to the increasing size of the country (e.g., the USA, Brazil, and Russian Federation) versus the availability and distribution of critical resources. Finally, the much-dreaded subsequent wave (s) of the COVID-19 pandemic will make the issue of NPI use and adherence truly critical.[50,51,52,53] Of special importance are both timing and coordination of the above efforts and factors[54]
Ensuring NPIs do not terminate prematurely – With the efficacy of NPIs becoming well established,[55,56] it is important to emphasize that such measures alone will not be sufficient to stop the spread of the pandemic. In aggregate, the best we can hope for with active NPIs is to “flatten the curve” but most likely not eliminate the pandemic altogether.[3] Thus, until highly effective vaccine or pharmacological interventions become widely available, both governments and citizenry must remain vigilant and not fall victim to complacency, both in personal and professional domains.[57,58,59]
Blind spot #3: Ignoring simple and effective nonpharmacological measures
There are two important considerations in this domain, both heavily dependent on excellent PH education and the ability to effectively convey key PH concepts, in a highly targeted fashion, to a large proportion of the global population. The combined and synergistic role of PH, corporate, and political leadership in this important process is critical:
Failure to learn from others – There were early success stories in the COVID-19 pandemic fight, with Germany, South Korea, and Japan providing three excellent examples.[47,60,61,62,63] The identification of effective strategies (e.g., contact tracing, diagnostic testing, technology-assisted approaches, and NPIs) early on during the pandemic led to significantly milder outbreaks in those countries. Moreover, countries that employed the said strategies early in the course of regional outbreaks also enjoyed the benefits of early successful COVID-19 containment.[64,65] What is not known at this point is if (and how) experiences from the initial wave of the pandemic will apply to any subsequent waves
Poorly coordinated post-COVID-19 reopenings – It is critically important for governments and PH officials to ensure adequate understanding of how the pandemic spreads, especially within the unique patterns of the local social, economic, and geographic milieu, prior to embarking on the reopening of economic and public life. It should be well understood by the public that NPIs such as social distancing or facial coverage work best when applied universally. It is also important for all stakeholders to know and understand the science behind such interventions, and that the observed effect at the population level will be akin to the application of an accelerator pedal or a brake.[66] There will likely be some unforeseen consequences of NPIs, especially in terms of mental health in general and social development across the younger population segments.[67,68]
Blind spot #4: Concomitant public health challenges and prevention of excess mortality
It is becoming increasingly apparent that effects of the COVID-19 pandemic extend well beyond those directly attributable to the SARS-CoV-2 virus. Recent data demonstrate a significant increase in COVID-19 pandemic-related, non-COVID-19 excess mortality due to a variety of factors, including social determinants of health, chronic health maintenance, mental health, avoidance of health-care settings, and impaired access to care.[69,70,71,72] These and other considerations will be discussed in the current section.
Chronic health conditions (CHCs) – In the setting of an overburdened health system and shelter-in-place regimes, CHCs are at risk of becoming neglected. There are two main mechanisms responsible for this phenomenon – avoidance of health-care facilities by patients with CHCs who are concerned about contracting COVID-19 and diminished access to care due to budgetary cuts related to scaled-down health facility operations.[73,74] Patients with metabolic disorders, chronic lung diseases (including tuberculosis [TB]), as well as cardiovascular diseases are among the most affected because of the pandemic, with projections of both significant care disruptions and deleterious post-COVID-19 after-effects (e.g., late-stage presentations).[75] Although telemedicine helps ameliorate some of these impacts, there is no true substitute for an in-person and in-depth patient evaluation in certain acute care scenarios.[34,76,77,78] Finally, we must not forget the possible deleterious effect of the current pandemic on the management of acute presentations, such as those of myocardial infarction, stroke, acute extremity ischemia, aortic aneurysms, various surgical emergencies, and many others[79,80,81]
Post-COVID syndrome – Several months into the pandemic, it became apparent that although the acute illness may resolve within days or weeks, persistent nonspecific symptoms may continue for much longer.[3,82,83] Since then, substantial evidence emerged regarding cardiac and pulmonary complaints, musculoskeletal issues, chronic fatigue, and other post-COVID sequelae.[82,84,85,86] In addition, early research shows that post-COVID-19 mental health issues may be a combination of environmental (e.g., social isolation) and organic (e.g., direct and secondary effects of viral infection) factors among survivors.[87,88,89,90] It is likely that the full range of post-COVID syndrome manifestations is yet to be discovered, warranting long-term research into this important topic area, as well as its impact on long-term health, expenditures, and worker productivity.[91]
Health-care capacity in the setting of co-existing infectious threats – The emergence of SARS-CoV-2 did not eliminate other (often endemic) infections, leading to widespread uncertainties and logistical challenges. For example, antigenic cross-reactivity between SARS-CoV-2 and dengue caused significant diagnostic confusion in the midst of the pandemic,[92,93] although some authors suggest that pre-exposure to dengue might offer some degree of protection against COVID-19.[94] Nonetheless, it has also been noted that COVID-19 and dengue co-epidemics have the potential to push the already-strained health-care systems beyond their limits.[95,96] Before we move on to discuss the specific aspects of each major co-existing infectious threat, it is important to mention that the current pandemic has put significant competitive pressure on research and development in other infectious disease areas, and this will need to be addressed at the global level as a key priority once COVID-19 is under control.
Tuberculosis care has been critically impacted in high TB burden areas for a number of reasons.[97] Beginning with limited access to health-care facilities, whether driven by the patient's fear of contracting COVID-19 or by insufficient resources, downstream consequences can be significant. For example, delayed diagnosis and treatment may lead to outbreaks of multidrug-resistant and extremely drug resistant TB, and such outbreaks may not be fully appreciated until lockdowns are opened and the surveys are restored.[98,99] Of note, active or latent TB may increase both the susceptibility to COVID-19 and the associated illness severity.[100] In terms of diagnostics, the crowding out of TB diagnostic capacity may occur when facilities are re-tooled to meet the demands of the COVID-19 pandemic. Of importance, transition back to pre-COVID-19 levels may take some time, causing further interference in TB control efforts. One solution to this problem may be the deployment of point-of-care diagnostics and continued focus on telemedicine.[101,102,103,104]
Malaria, another endemic disease in many regions of the world, has been at the forefront of the early COVID-19 epidemic, with the hope and promise of antimalarial agent effectiveness against SARS-CoV-2 based on sophisticated computational models.[105] There was also circumstantial evidence pointing to an inverse relationship between the incidence of malaria and COVID-19.[106] Research has since shown that antimalarial drugs are largely ineffective in treating the novel coronavirus,[107,108] while at the same time the co-presence of SARS-CoV-2 and malaria may present health-care providers with a formidable symptom screening challenge.[109] Moreover, both the direct and indirect deleterious impacts of COVID-19 on malaria prevention activities and treatment (due to diversion of antimalarials) may in fact be associated with substantial loss of life-years,[110] especially in the setting of sparse health-care resources.[111,112]
There is emerging evidence that the co-infection with influenza and COVID-19 may predispose patients to more severe clinical illness than either infection in isolation.[113,114] Some of the hypothetical and observed features of such co-infection include greater risk of cardiac injury, higher risk (and earlier onset) of a cytokine storm, and potentially higher mortality.[114,115] Although much research remains to be done in this important area, the so-called “COVI-Flu” may become a reality if a virulent influenza strain manages to emerge as a “competing and parallel” pandemic alongside COVID-19.[1,113] Still, it has also been noted that COVID-19 control measures may have a positive effect on containing the spread of influenza,[116] potentially balancing out the deleterious effects of a SARS-CoV-2 and influenza co-infection at a population level.
The COVID-19 pandemic has the potential to affect the management and control of human immunodeficiency virus (HIV) across various high-prevalence areas.[117,118] The effects of disruptions in HIV care are likely to be felt across both high-resource regions and low- and-middle resource regions (LMRRs).[110,118,119] Innovative, multinational solutions will be required to appropriately and adequately address this complex, emerging problem.
Blind spot #5: Long-term care needs and the postintensive care syndrome
There are more than 4 million Americans hospitalized with critical illness annually, with sepsis and acute respiratory distress syndrome consistently among the top causes of critical illness. Now with the appearance of COVID-19, a post-COVID syndrome, specifically in those who were survivors requiring an intensive care unit (ICU) stay, including their families (for a variety of medical and non-medical reasons), becomes a serious concern.[120,121] The success of critical care medicine has historically been gauged by short-term mortality outcome; however, with technological and treatment advances, many patients now survive what may have previously been fatal critical illnesses, generating an expanding population of critical care survivors. It is estimated that postintensive care syndrome (PICS) develops in more than 2.4 million Americans who survive critical illness each year, including approximately two-thirds of Medicare beneficiaries who survive critical illness.[122] It is estimated that up to 50% of ICU survivors are at risk for long-term physical, cognitive, and/or behavioral health issues after ICU and hospital discharge.[122] In addition to the direct impact on ICU survivors, PICS has a financial and operational impact on health-care delivery systems as well as a significant and often negative impact on the caregivers and families of ICU survivors.[122] As a consequence of both an aging population and the dramatic improvement in mortality rates in those with critical illness, PICS is rapidly becoming a major PH concern and, as indicated above, the medical community needs to prepare for excess PICS in relation to the COVID-19 pandemic.[123]
Blind spot #6: Pseudoscience and academic dishonesty
It is regretful that one of the very earliest victims of the current pandemic was evidence-based medicine.[124] The profound impact of the virus on the day-to-day life all over the world, combined with an extensive SM use during the pandemic, led to the spread of many unfounded theories about the origin of SARS-CoV-2, including its spread, severity, and possible treatment options.[125,126] The conventional media and the political establishment in many regions of the world added fuel to these (conspiracy) theories, further exacerbating the situation.[127,128,129,130,131]
Scientific dishonesty – Since the outset of the pandemic, some members of the scientific community attempted to advance their career by publishing manuscripts with attention-grabbing but irresponsible conclusions based on suboptimal research, inclusive of original investigations published in some of the most prestigious medical journals on the planet.[132,133,134,135] Some of the questionable research was published by authors with known conflicts of interest.[136] Finally, there is a group of health experts who are actively downplaying the threat of the virus, thus creating confusion and adding even more fuel to the already-prevalent public distrust[137]
Pseudoscience – Pseudoscience, or a collection of beliefs or practices mistakenly regarded as being based on scientific methods, has emerged as a powerful destructive force during the current pandemic.[138,139,140] Powered by a combination of factors, false beliefs that the ultraviolet light in the sunlight will “kill the virus” and “stop the pandemic” have blossomed after significant SM exposure and reinforcement.[26,27,141] To further exacerbate the matters, various political forces tend to latch onto pseudoscientific facts to support agendas that do not necessarily focus on societal health and well-being.[138,142]
The roots of this specific vulnerability have complex origins, from well-meaning politicians trying to reassure citizens with nonscientific musings to desperate citizenry ready to embrace anything that will improve their life condition. Human propensity to dissociate from challenges of an overwhelming pandemic provides a niche for pseudoscience, and other forms of magical thinking, during this and other pandemics.[143,144,145]
Unfortunately, pseudoscience has also found a space in the scientific literature, especially among the so-called predatory publication outlets.[146] One of the demands of the pandemic continues to be the need for scientific understanding and the generation of new, evidence-based treatment modalities. However, many academic institutions witnessed a significant slowdown across their research departments due to the widespread stay-at-home measures.[147,148] In addition, due to the magnitude and speed of SARS-CoV-2 spread, properly conducted, well-controlled scientific research during the early pandemic was essentially replaced by a large number of low-quality, highly biased observational studies, inundating peer-reviewed journals with COVID-based pseudoscience. As peer reviewers felt pressure to deliver scientific direction in the setting of a largely unknown pandemic-causing infectious entity, journal quality and standards suffered.[149,150,151] Under such circumstances, only time and validation of the published data, either through reproducible experimentation or postpublication verification and peer review,[152] can reveal which studies should ultimately be considered pseudoscience and which ones should become a foundation of COVID-19 clinical and scientific mainstream practice.
Blind spot #7: The emergence of vulnerabilities within health-care systems
While the international medical community struggles to contain the COVID-19 pandemic, the focus on this dominant health security threat may expose important vulnerabilities in our health-care systems. Speaking broadly, four primary challenges emerge within this sphere: insurance coverage, provider financial losses, racial and ethnic disparities (see Blind Spot #11), as well as general PH crisis readiness.[3,153] First, more than 20 million workers became unemployed in a short period of time, effectively losing their employer-sponsored health care. The reliance on employers for insurance (a characteristic of the US health-care system) is a major shortcoming, as is the suboptimal utilization of the Affordable Care Act. Second, while there has been an increase in the need for specialized care in many hospitals, the demand for primary care has abated and there have been significant reductions in remuneration.[154,155,156,157] Third, race and ethnicity play a significant role in this pandemic, clearly a complex and multifactorial phenomenon.[158,159] Lack of insurance coverage results in a loss of, or reduction in, access to health care. Chronic diseases cannot be addressed in a prompt and effective manner, and food and housing insecurity is exacerbated for those who lost their jobs and/or remain in poverty.[160,161,162,163,164,165] The fourth factor is that the USA (as well as some other regions of the world) does not have a well-functioning system for responding to pandemics, especially in the face of the proposition that PH is essentially a governmental function, intended for the public good at the local, regional, and national levels.[166,167]
Within the above-stated framework, additional important factors that health systems should be addressing proactively include health care-associated infections (including COVID-19), health care-associated non-COVID illnesses, point-of-care capabilities, as well as implementations of telemedicine intended specifically to ease some of the pandemic-related burdens.[1,34,168,169,170,171,172,173] Although it is beyond the scope of the current discussion, it may be important to create a “vulnerability index” designed to help determine the available resources (e.g., personnel and supplies) specific to the context of pandemic preparedness at both local and regional levels.[174] An early and very important blind spot for health-care workers included the misleading belief that only high-risk patients could get ill with COVID-19 and that our health-care colleagues were relatively spared, ultimately leading to the relaxation of protective measures and viral transmission to other personnel. Thus, it is prudent for all employees to embrace universal precautions and don personal protective equipment (PPE) at all times in the clinical environment.
Effective screening of active or suspected cases is critical in containing the spread of COVID-19 and similar outbreaks. In particular, active screening of high-risk groups is of great importance, and lack of standard operating procedures and/or frequent changes to standard operating procedures can significantly contribute to inefficiency in both screening and treatment protocols.[175] The risk of COVID-19 infection may be increased among minority health-care workers. In one study, factors associated with a positive COVID-19 test in front-line health-care workers included poor PPE adequacy, high-risk clinical settings, and susceptible ethnic minorities (i.e., African-American [AA], Latinx, and Asian backgrounds).[176] Administrators need to address these potential blind spots as they structure health-care worker protective strategies. Well-coordinated screening efforts should incorporate approaches that address both COVID-19 and other high-prevalence pulmonary diseases. For example, some national TB control programs are adopting universal testing of suspected COVID-19 patients for TB and vice versa.[177] Finally, early during the pandemic, there was a lack of standardization in diagnostic tests, which flooded the markets. The sensitivity and specificity were inconsistent, which consequently led to many inaccurate test results. Adding to this complex issue, there were no reliable point-of-care tests as the disease was new and the development process took longer than expected.
Due to the COVID-19 crisis, telemedicine platforms have become very popular around the world. However, these platforms also bring new challenges, inclusive of patient safety considerations and the inability to obtain a reliable physical examination.[178,179] Some of the major burdens and blind spots specifically related to telemedicine include the lack of strictly defined staff responsibilities, specialty-specific considerations, lack of protocols or limited protocol adherence, screening schedules, additional services, and evolving team roles due to the introduction and ongoing use of new technology.[180] Other considerations include the relatively ambiguous framework for accountability or lack thereof, inadequacy in data storage, suboptimal internet connectivity, insufficiently encrypted (e.g., nonconfidential) interface, as well as inadequate personal clinical examinations.
Blind spot #8: Jurisdictional and administrative perspectives
Many jurisdictional and administrative issues have come to the fore with COVID-19, such as collaboration and coordination across state or national boundaries, patient visitation restrictions, police/law and order, as well as concerns regarding corporate social responsibility (CSR). The crux of most of these issues revolve around the concept of social dilemma,[181,182] especially with regard to local, state, and cross-border collaboration and coordination. Johnson et al.[183] provide an interesting and effective discussion of social dilemma in the time of COVID-19 through a review and explanation of the conceptual framework involved. More specifically they looked at the behavioral instincts, behavioral variation via insulating self-organizing pools of cooperators, examined ways to expand cooperators through group identity, and evaluated centralized and decentralized nonmandatory and mandatory cooperation, inclusive of subsequent organizational and governmental implementations.183 Basically, there is a cost to sheltering in place and social distancing. These effective measures are of greater benefit to the most vulnerable among us (e.g., the elderly and those with chronic health conditions) and the community at large.[184] The other problem that presents with this benefit is that as social distancing compliance improves, exposures decrease, thereby emboldening segments of the society to venture forth while others stay in place.[183] An accompanying social dilemma for governments involves the cooperative distribution of supplies and therapies across state lines or national borders. In this case, hoarding supplies for a particular jurisdiction allows better local survival, but it does not bode well for the health of the society in general. The incentive of one government or one particular individual informs the structure of the social dilemma.[181] Here, “personal incentives compel individuals to act against group welfare, despite an ultimate fate that leaves them wishing they had acted in the community's interest.”[183]
Hospital visitation has been a particular concern for families and patients. It has been argued that a humane approach to families and patients should be person-centered while at the same time complying with the pandemic response.[185,186] During the COVID-19 pandemic, video chats and garden visits have become commonplace,[187,188] but these options were delayed by some facilities/institutions. Sometimes, compassionate exceptions need to be made.[189] If humane and person-centered care cannot be accomplished during this pandemic, then “it could also undermine public solidarity at a point when health-care providers need strong PH support and understanding as they face the challenge of dealing with the fallout from delayed and disrupted care.”[186]
Of course, the topic of law and order cannot be overlooked. First, the laws of quarantine should be addressed. In many cases, the first reaction to a contagion is quarantine and travel bans.[3] While “quarantine” indicates the segregation of someone exposed to the disease, “isolation” indicates that the individual is segregated because he/she is infected. Conventionally, the states have issued quarantine orders, and there does not need to be an emergency declaration in place for their issuance. The Surgeon General and the Centers for Disease Control and Prevention (CDC) have always had the power to intervene, but had confined themselves to giving guidance. However, as of 2017, the CDC made it clear in the new regulations of the federal code that it would no longer defer to state governments. While the government needs a strong basis for quarantine, it must continue to provide medical care for those restricted. Of note, restricted individuals are entitled to certain protections including judicial review. In the 21st century, the USA needs a more creative legal armamentarium to ensure readiness for future quarantine events.[3] Moreover, the impact of this pandemic on law enforcement (LE) needs attention.
LE has the primary function of maintaining peace and protecting the public e.g., “to serve and protect”. However, in the times of medical crises, such as the COVID-19 pandemic, they are there to help the PH arms of government to protect the society from disease spread. Having said that, effective reallocation of LE personnel during a pandemic requires that appropriate training, resources, and protections are in place before any implementations are undertaken. In addition, the existing staffing levels must support such maneuvering or important blind spots may emerge in the area of LE. Moreover, LE departments across the country will respond differently, but generally they have approached this pandemic by, “reassigning personnel to high-traffic areas, suspending training/roll calls, implementing safety precautions for officers, and limiting access to departmental facilities.”[190] Police departments have generally followed established CDC guidelines, namely: (a) maintain a social distance of 6 feet from others, (b) wash hands with soap and water for 20 s, and (c) do not touch your eyes and face. Further, CDC recommendations include use of PPE such as gowns, N-95 masks, eye protection, and disposable gloves.[3] Jennings et al. point out that further policing efforts include a presence in grocery stores, new approaches to handling nonemergency and nonviolent reports, limiting misdemeanor arrests, and spending more time in patrol cars and less time in the community.[190] Another problem facing the LE is the need to be involved in communicating the importance of social distancing measures, mandatory and nonmandatory, and the resultant consequences for disobedience. It has been noted that setting up check points or patrolling for violations is inherently difficult and burdensome.[191,192,193] In addition, there will be financial pressures on departments, thereby making management of resources a priority. Here, the questions of having enough PPE for the LE workforce become critically important.[190] In the end, the officers have to protect the community while protecting themselves, and doing so in an efficient, safe, and nonthreatening manner.
The conduct of corporate social responsibility (CSR), both in the context of the workplace and society in general, will be an important and challenging process during this pandemic. The COVID-19 pandemic is what in 2008 Taleb referred to in his work as a “Black Swan Event.”[194] Such an event can change how the world conducts itself. If a corporation/business offers help to public during such a crisis and demonstrates a genuine CSR, it can build a great and long-lasting rapport with its customers and employees.[195] The question for corporations has been whether it may be advantageous not to invest in CSR in order to protect short stability and gains, or play the long game and thus build a lasting bond with employees and society? Most companies have historically found that CSR is a boon to their standing.[190] And it seems that, in the face of the pandemic and the questions of social justice, companies are opting for enhanced CSR.[196] Some companies have asked if charitable giving to its employees is sanctioned by the Internal Revenue Service (IRS). The fact of the matter is that it is permitted.[197] It falls under IRS section 139, and “having a written policy in place governing relief payments would make it more difficult for the IRS to question any payment made pursuant to the policy.”[197]
Blind spot #9: Essential infrastructure and public works
Public buildings, essential services, and related considerations
During the pandemic, closure of nonessential facilities and public buildings is preferred to ongoing in-person operations, especially if the required business can be conducted via teleconferencing or other equivalent means.[3,34] At the same time, certain governmental and nongovernmental activities must be maintained, regardless of the presence of the pandemic.[198,199,200,201,202] In terms of blind spots relevant to this important general context, the following “lessons learned” and considerations emerge:
Nonpharmacological interventions (NPIs) take on an even greater importance, mainly because most of the business conducted in public buildings can be classified as occurring within “closed spaces” and thus inherently “high-risk” environments.[203,204] Consequently, ample personal hygiene products must be available for frequent use and masks must be worn at all times to reduce and/or prevent active and/or widespread aerosolization and subsequent transmission of the infectious agent[205]
Ongoing focus on frequent disinfection must be maintained. This applies especially to high-frequency, high-traffic locations, such as elevators and bathrooms, where many surfaces are touched by attendees, in addition to the presence of aerosolized infectious agents.[3] Given the emerging nature of the COVID-19 pandemic, further research is needed regarding the exact benefits and most optimal disinfection approaches for SARS-CoV-2
High-efficiency air filtration capable of destroying viral particles should be considered, preferably with increased air turnover within closed spaces.[3,206] Although such systems may not prevent direct, short-distance transmission of airborne virus between individuals in close proximity, there may be a benefit to those at risk of contracting a highly infectious viral disease when the size of the viral particle is smaller than the stated filtration size of currently installed high-efficiency particulate air (HEPA) infrastructure[207]
Considerations pertaining to the above points are also applicable to public transportation and infrastructure, where individuals aggregate in relatively large numbers within a small – and often confined – area or space.[3,208]
Public water, sewage, and waste management
The possibility of sewage as a conduit for COVID-19 spread has been suggested, with a clear warning that this important consideration “must not be neglected” in the overall response to the ongoing pandemic.[209,210] In the Netherlands, active testing of sewage from nearly thirty treatment plants suggested that the presence of SARS-CoV-2 in sewage samples may correlate with the spread of the novel coronavirus.[211] At this time, it is not known whether the presence of SARS-CoV-2 in sewage samples is simply a reflection of the viral presence at the population level within a certain geographic locality, or whether it also serves as a risk factor for nonrespiratory transmission of the virus. The remote possibility of the latter is suggested, but certainly not proven, by a cluster of sanitation workers in China who may have contracted the virus through the use of bathrooms.[212]
Despite global lockdowns, many essential services need to continue to ensure the safety and welfare of citizens. Social/physical-distancing restrictions severely affected the supplies of essential items and services, operations and maintenance of water utilities, and other services throughout the world. Providing essential services such as customer care, hotlines, helplines, and emergency medical and nonmedical services has become a formidable challenge. The COVID-19 crisis disrupted all supply chains across the world. In many countries, the demand for domestic consumption of products and services including drinking water increased markedly due to families staying at homes, with greater demand for residential use, but also across our hospitals due to enhanced hand washing and personal hygiene requirements. The World Economic Forum's Global Risks Perception Survey of 2015 has shown that infectious diseases ranked among the top five perceived threats. However, due to direct aftermath of the Ebola epidemic, infectious diseases ranked second highest in terms of impact.[213] According to the US Department of Homeland Security (DHS), there are around 13 major sectors classified as “essential” to the economy, and the summary is provided in Table 2.[214] This list covers a wide range of occupations such as doctors, nurses, truck drivers and plumbers. Among all sectors, health-care/PH sector contributes to one-third of the total and other sectors contribute two-thirds of the total, with the corresponding distribution shown in Figure 2.[214] Two specific sectors - critical manufacturing and financial services - employ around 21% of the total workforce but are not under the purview of DHS, which may pose a substantial challenge during the COVID-19 crisis. Disposal of bio-medical waste has become a huge challenge and creates a high risk of spread. This potential of blind spot needs special attention from PH officials.
Table 2.
List of essential infrastructure industries, 2018
| DHS category | Employment | Percentage of total |
|---|---|---|
| Health care/public health | 21,096,650 | 33.68 |
| Transportation and logistics | 8,628,640 | 13.77 |
| Government operations and essential functions | 7,658,100 | 12.23 |
| Critical manufacturing | 7,081,790 | 11.31 |
| Financial services | 5,918,880 | 9.45 |
| Food and agriculture | 5,233,210 | 8.35 |
| Energy | 1,950,240 | 3.11 |
| Communications and information technology | 1,639,930 | 2.62 |
| Public works | 1,347,630 | 2.15 |
| Defense industrial base | 943,740 | 1.51 |
| Chemical | 939,960 | 1.50 |
| Hazardous materials | 149,980 | 0.24 |
| Water and wastewater | 51,520 | 0.08 |
Source: https://www.brookings.edu/wp.content/uploads/2020/03/Front-Line-Workers-Appendix.docx. DHS: Department of homeland security
Figure 2.
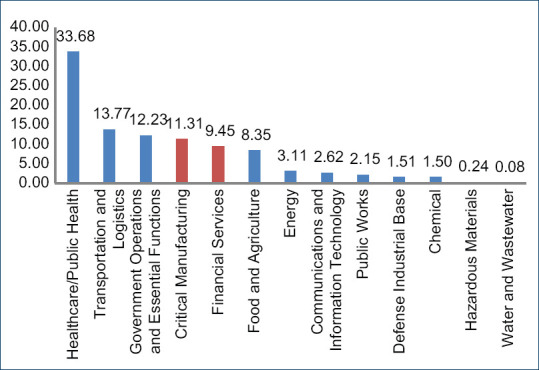
Distribution of employment across essential infrastructure industries
Food supply chain safety-related issues
Safety of food supply chains is one of the major concerns for producers, consumers, and regulators. The Food and Agriculture Organization of the United Nations estimates that 30%–40% of the total food production is lost before it reaches the market due to improper food storage, processing, or transportation. From past experiences, it can be seen that many food products must be discarded due to the presence of contamination at different points along the supply chain. These failure points include, but are not limited to: source/raw material, production and packaging, warehousing and transportation, mandatory check points at the borders/custom clearances, as well as various other delays in the supply chain. The major sources of failures can be attributed to raw material processing, production practices, human interaction, packaging, among other factors. Particularly during the COVID-19 crisis, disruptions in food supply chains have forced regulatory bodies to relax some of the standard practices to facilitate timely supply of food items to consumers. The temporary relaxation of requirements may help helped expedite supply speeds and thus facilitate consumers' food needs, but it is also hard to estimate if any harm may have resulted from deregulation.[215] These kinds of temporary relaxations can result in major safety-related problems within food supply chains. For example, there are recent reports that samples of frozen shrimp tested positive for coronavirus, raising concerns about the patogen's ability to spread through food and/or frozen products.[216]
According to global experts, imported food poses a low risk of transmitting the virus, but many countries continue testing the food they import, particularly meat, fish, and other fresh food. Some jurisdictions have employed more aggressive approaches, such as the halting of meat imports from countries and/or regions with high incidence of COVID-19.[216] Food safety and spoilage along the supply chain is increasing worldwide and can lead to cost escalations, delays, and environmental contamination. By deploying modern technological solutions technological solutions across food supply chains to facilitate waste reduction, nations can improve traceability, transparency, and trust among the customers and supply chain partners. Reliable processes and technologies are needed to ensure traceability and visibility throughout the supply chain.
Various blind spots in the food supply chain affect key stakeholders, increase overall costs, and lead to delays. Challenges in maintaining food safety and security are closely related to the increasing number of “product touch points” between the producer and the customer. For example, if the food requires refrigeration, conditions must remain constant throughout transportation and storage because the provenance of the cold chain has a direct impact on food quality, safety, and expiration dates. Temperature excursions and time delays can promote bacterial growth, which may lead to food spoilage.[217,218] Significant bacterial proliferation can occur under certain transient conditions, highlighting the importance of strict adherence to temperature stability. This can be addressed by using various innovative approaches including blockchain technology.[219]
Public transportation
The CDC has recommended wearing facemasks when using public transportation or when at transportation hubs and transfer points.[220] Adherence to NPIs while traveling can be very challenging, with inherent lack of social distancing when traveling by air or on buses or trains. International or interstate/province travel continues to be an important and significant conduit for viral transmission. This risk has yet to be quantified definitively. The CDC, “strongly recommends appropriate masks be worn by all passengers and by all operating personnel while on public transportation conveyances (e.g., airplanes, ships, ferries, trains, subways, buses, taxis, ride-shares) and at transportation hubs and other locations where people board such conveyances (e.g., airports, bus or ferry terminals, train stations, seaports).”[220] The CDC goes on to further recommend that conveyance operators should refuse entry to passengers/customers or employees that do not wear face masks and that face coverings should be worn for the entirety of the journey. This guidance should be imparted to all passengers when they buy their tickets and anyone violating this recommendation should be disembarked at the earliest convenience. There are suggested exemptions to this recommendation, as follows:
Children under 2 years of age (masks should NOT be worn by children under the age of 2)
Anyone with written instructions from a licensed medical professional to not wear a face cover
Those with disabilities, mental health conditions, or sensory sensitivity that prevents, may prevent or cause difficulties with mask use
The hearing impaired, or communicating with someone who is hearing impaired, when the ability to see the mouth is important for communication
When wearing a mask creates a risk to workplace health, safety, or job duty as determined by the workplace safety guidelines or federal regulations; or
A person operating (or essential to operating) a conveyance for whom wearing a mask would interfere with safely operating a conveyance.[220]
More specifically, airlines frequently note that commercial aircraft use HEPA filters; these are the CDC-recommended air filters used in hospital isolation rooms. They capture 99.97% of airborne particles and significantly decrease the risk of SARS-CoV-2 spread. In addition, the air in plane cabins is completely changed 10–12 times per hour, raising the air quality above that in normal edifices.[221] While there is a risk of contracting COVID-19 during air travel,[222] the odds are very small if passengers wear a mask and middle seats are empty.[223]
In addition, Hu et al. studied COVID-19 transmission risk among train passengers in China. They reported that the overall risk can be modulated by flexible co-travel time and seat configurations. Measures should be taken when traveling on public transportation in confined spaces such as trains to reduce the risk of transmission, including increasing seating distance, reducing passenger density, and using personal hygiene protection.[224]
As far as buses and subways are concerned, many citizens have started using these transportation modalities again, and while there are risks, masking and social distancing seem to provide some degree of safety.[225] Of course, it is highly unlikely that any two situations or circumstances will be identical, and it matters where a passenger sits, who the passenger sits next to, and the travel time involved, among many other variables.[226]
Blind spot #10: Research and development: therapies and treatment limitations
Research and development regarding therapies is very essential to address the outbreaks of PH emergencies of international concern such as Ebola virus and COVID-19. It goes without question that elimination of disease is of paramount importance, far outweighing economic or financial considerations. In fact, preservation of lives is of utmost importance for economic recovery.[227] This is so because “in the aftermath of COVID-19, countries will experience more suicides, alcoholism, and drug-related mortalities, as well as the need for emergency food support, with an accompanying decrease in life expectancy. Furthermore, in not showing a concern for the protection of its citizens, a government may see a change in the number of citizens who can pay to taxes, voting attitudes, and an electorate leaning toward the more extreme elements in politics.”[228]
In 2018, the year before COVID-19 first appeared in China, the Society of Critical Care Medicine produced an ethics of outbreaks position statement regarding therapies and treatments, including key related recommendations.[229] This document began with the concern regarding the use of experimental therapies/interventions during a medical crisis and reviewed justification for such therapies, which was accompanied by cautionary guidance on the conduct of research during a health-care crisis. When approaching vaccines or treatments, the following issues are of importance:[230] “in a dangerous, large-scale emerging infection, the risk of contagion and the resultant morbidity and mortality must be significant enough to justify a novel or untested vaccination or treatment program. Such a justification includes the likelihood of transmission, the agent's severity, and/or its duration of effect.”[229]
The rapid gain of new knowledge is very important during COVID-19. A valid research question has to be defined with appropriate methodology that results in a testable hypothesis. Muller-Nix et al. state that if a treatment or vaccine program is not fully justified, ethical, and feasible, then drugs of questionable efficacy should be used only within an organizational framework that can document the severity of illness in a timely manner while elucidating the treatment details, adverse events, and all confounding factors (clinical and nonclinical).[231] While randomized controlled trials are the gold standard for determining efficacy, when faced with a substantial physiological threat, there has to be adaptation by scientists and physicians to speed up the research process, but within a stated ethical framework, that “can offer the best result, in the fastest manner, with the smallest [possible sacrifice] of scientific accuracy and precision.”[229] The World Health Organization states that clinical trial monitoring and oversight should be performed by a committee that has access to all the relevant data.[232] At the same time, accelerated delivery of devices, drugs, and other products to the field should occur through expedited regulatory mechanisms.[233] It is important to keep our collective scientific minds and research avenues open, and surprising new findings should not be dismissed by default but rather thoroughly investigated and validated (or invalidated). One such example is the recent announcement that a lipopeptide nasal spray may be effective in blocking a key cell membrane protein from adopting a configuration necessary for SARS-CoV-2 entry. Although these observations must be validated and proven safe/effective in the clinical setting, such spray reportedly provides approximately 24 h of protection, is very affordable, does not require refrigeration, and may be amenable to rapid mass production.[234] In another example, recent report by the World Health Organization casts doubts on the efficacy of Remdesivir - citing pooled data from more than 7,000 patients enrolled in 4 different randomized controlled trials.309
There are cautions that need to be observed when conducting research during health crises. Protection of vulnerable populations is extremely important, inclusive of patients with mental handicaps, the young, the elderly, pregnant women and prisoners.[229] Additionally, cultural, religious, ethnic, and socio-economic values and factors must be taken into consideration and respected.[235] Further caution must be used to not rush studies or use poor methodology or fall prey to the pitfalls of data misinterpretation. Researchers, physicians, and government officials must always be aware of the potential for unfair allocation of treatment and preventive resources.[229]
Blind Spot #11: Racial and social disparities
Chronic diseases, economic limitations, and reduced health-care access disproportionately affect minority groups, and are associated with worse clinical outcomes from COVID-19.[236] Abedi et al. looked at the racial and economic inequities in health, focusing specifically on COVID-19 infection rates and mortality across 369 US counties (population total of 102,178117) from the states of New York, Michigan, New Jersey, Pennsylvania, California, and Massachusetts.[237] They reported that counties with greater diversity, larger populations, higher overall education and income levels, and low rates of disability were at higher risk of COVID-19 infections, but counties that had higher rates of disability and poverty had a higher death rate. In terms of mortality, AAs were more affected than other groups within the society (1981/1,000,000 in AA vs. 658/1,000,000 in Caucasian population).[237] The same authors hypothesized that this was due to a higher population density, more comorbidities, and limited access to health-care. A work by Price-Haywood et al. on the rates of hospitalization and mortality among Caucasian and AA patients in Louisiana found that AAs had more obesity, hypertension, diabetes, and chronic kidney disease. Moreover, AAs were 31% of the health system population, but made up 76.9% of hospitalized COVID-19-positive patients.[238] In addition, of those critically ill patients that required mechanical ventilation, 80% were AAs. Furthermore, AAs were also overrepresented among COVID-19 hospital deaths (70.6%). The authors state that, “Black race, increasing age, a higher score on the Charlson Comorbidity Index, public insurance (Medicare or Medicaid), residence in a low-income area, and obesity were associated with increased odds of hospital admission.”[238] The authors further speculate that such differences could be related to service occupation (e.g., higher exposure risks) and the increased presence of chronic conditions. Alobuia et al. examined racial disparities in knowledge, attitudes, and practices (KAPs) in the USA and found that while Caucasians had better knowledge of the disease and higher attitude scores, AAs performed better in relation to putting safe habits into practice. KAPs were associated not only with race, education, and income but also with sex, health insurance status, and political points of view.239 Clearly, more research is required in this important area before any definitive conclusions or action plans can be made.229
There is little doubt that economics and workplace factors play a role in COVID-19's inequalities of distribution. Three points to be made here are: (a) AAs are overrepresented in nine of ten high-contact, lower income services, such as nursing assistants;[240] (b) 39% of jobs held by AAs are not considered stable and are subject to reductions in work hours, pay, layoffs, or furloughs;[241] and (c) almost 70% of the Black US population lives in 16 states that are below the national average in job and economic opportunities, access to health care, and quality health care.[242,243] Furthermore, a significant proportion of AAs do not have jobs that facilitate remote work.[244] As a case in point regarding minority/ethnic working disparities, Bui et al. reported in Morbidity and Mortality Weekly Report (from Utah) that 12% of the COVID-19 outbreaks were associated with a workplace, and that although only 24% of the workforce associated with these workplaces were Latinx, Hispanic-Americans constituted 73% of the cases.[245] Such disparities also carry over into the area of cancer prevention. Carethers et al.[246] state that, “racial and ethnic minorities and other medically underserved populations exhibit lower uptake of cancer screening than nonminorities in the USA. The COVID-19 pandemic, which disproportionately affected minority communities, has curtailed preventive services (including cancer screening) in order to preserve PPE and prevent the spread of infection.”[246]
Finally, the elderly must not be forgotten, for age is a considerable influence on one's health, and it is tends to be entwined with poverty; race and ethnicity; social isolation; home care; and the lack of access, understanding, and support for technology utilization.[247] In fact, the highest proportion of COVID-19 deaths are occurring in our older population.[3] While different considerations related to age and chronic disease affect minorities the most, Cox reminds us there continues to be “ageism [that] perpetuates negative stereotypes that describe older people as frail with diminished status creating burdens on society.”[247] These types of attitudes undervalue older adults. Furthermore, it is not uncommon to exclude older adults from clinical trials, “often [omitting] those over 65. Safety issues, as well as expediency for the researcher, the beliefs that older people lack technology, and are not fluent with computers, are commonly given as reasons for exclusion.”[247]
Racial and social disparities require mandatory examination and action during this pandemic. It is incumbent upon all health-care providers, scientists, social agencies, politicians, institutions, and the society at large to recognize the space of appearance where these disparities play an oversized role in clinical disease characteristics, service delivery, and access to health care.
Blind spot #12: The COVID-19 economy, mental health, and violence
The COVID-19 pandemic can have a profound effect on a person's mental health and may contribute to violence or its serious consideration at individual level.[248] The pandemic stressors regarding disease, isolation, confinement, political philosophy, and the lackluster economic environment have created a global concern. Any of the above factors can directly or indirectly lead to violence, against self or otherwise.3 This may include, but is not limited to, domestic violence, suicide, gender-based violence, street crime, and political violence.[3,248]
The ongoing pandemic has presented the US and the rest of the world with an unprecedented challenge.[194] It is certainly true that creating a vaccine and discovering therapies that will halt this disease are important. However, one must also appreciate the pandemic's economic effects as a global source of worry, anxiety, and dissent. Unemployment fears and the resultant concern for famine, especially in LMRRs are evident.[249,250] Some citizens can work from home, but others may not have such opportunities, and these individuals who cannot (including their families) are confronted with few viable options.[251,252] As a result, approximately 10 years of employment gains in the US disappeared.[253] This economic impact may have been due, at least in part, to various governmental stay-at-home directives. Such a disruption of our existing social fabric may lead to both individual and group violence. Key considerations here include domestic violence, suicide, street crime, and political violence.
The Secretary General of the United Nations, Antonio Guterres, issued a recent appeal, “I urge all governments to put women's safety first as they respond to the pandemic,” because PH emergencies tend to exacerbate inequality and disproportionately expose women to both emotional abuse and physical violence.[254] The COVID-19 lockdown in the spring of 2020 involved 80% of the world's populace; this included 1.6 billion children and more than 3 billion adults.[255] Domestic violence rose globally during this pandemic,[256] and there is a relationship between uncertainty, confusion, anger, posttraumatic stress disorder, and increases in substance abuse during periods of quarantine, which may also exacerbate the propensity for family violence.[3]
According to Keshavjee,[257] certain introduced by various jurisdictions in response to the pandemic shift the cost of health care from government institutions to local communities. As a result, patients receiving care become consumers of health-care services. The associated economic and financial strain may be linked to increased risk for hardship and violence among the most vulnerable members of the society, particularly women. Since the beginning of the COVID-19 crisis, there are reports of violence against women and girls, particularly from LMRRs.[258] Around 67% of health workers worldwide are women and many among them are employed on part-time basis. They are more likely to be the first to be laid off or given shorter contracts during and after the crisis. Millions of women around the world (especially in LMRRs) are employed in informal and unskilled jobs with low wages, where they are often the most marginalized segment of the labor force, with little or no job security. Research also shows that due to traditional gender roles, it takes women longer to go back to work after a significant economic or disaster event. Girls aged between 14 and 18 years are especially vulnerable in this context. For example, in India, around 40% of this population segment are out of school. Because of school closures and the overall economic environment, a significant proportion of affected young women may not return to continue their education. When families are hit with an economic crisis, the nutritional needs of women and girls in the family are also likely to be affected severely.[258] Moreover, women are susceptible to the mental health/psychological issues experienced by the general public, and this too requires immediate attention. If these concerns are not addressed in a timely and effective manner, such psychological burdens will lead to mental exhaustion, decreased morale, and long-term psychological sequelae.[259]
There is little doubt that loss of employment and its resulting economic sequelae are factors that may facilitate acts of suicide or suicidal ideation.[260] Quarantine and isolation (see jurisdictional and administrative perspectives section earlier in this manuscript) can further exacerbate this risk, often for an extended time.[3,251] Therefore, access to readily available items that facilitate self-harm, such as guns and drugs, should be considered a PH priority.[261,262]
Of interest, some have reported that street violence decreased with bars and nightclub closings, as well as the implementation of curfews in the spring of 2020.[255] Marupeng reported that when the South African government imposed pandemic lockdown with a ban on alcohol sales, there was 71% decrease in homicides, an 85% decrease in sex crimes, and an 83% decrease in serious assaults when compared with a similar period from previous year.[263] Analogous reports have emerged from Latin America and California.[255]
Political violence may emerge during a pandemic. The appearance of armed protesters after a governor-mandated lockdown order in Michigan[248] and the targeting of the Ohio Health Director's home by extremists who chanted antisemitic slogans[264] are among several recent examples. For foreign and domestic extremist groups, COVID-19 is an opportunity to assault any opposing viewpoints.[265] In addition, individuals and fringe groups are using SM to harass religious and other minorities, and to disrupt a variety of legitimate societal functions and institutions.[248,265,266]
Blind spot #13: Potential viral reservoirs and risks associated with virology research
Domestic animals play an important part as human companions, and may help ameliorate some of the mental health concerns noted during the current pandemic.[267,268] At the same time, it has been recognized that there exists a risk of human-to-animal transmission (and vice versa) involving domesticated animals.[269,270] Some authors postulate that COVID-19 could evolve into a panzootic, although such risk is likely very low.[271] One potential solution to combat a zoonotic-to-human transmission is to identify all potential zoonotic reservoirs and develop appropriate mitigation measures, inclusive of vaccines, to stop SARS-CoV-2 before it has the opportunity to “jump back into” the human population. Although much remains to be learned about this important issue, a pragmatic approach should be emphasized.[268,272] In this section, we will discuss some of the available evidence that will hopefully raise awareness and illuminate this potential blind spot:
Feline reservoir – Early findings indicate that cats may contract airborne SARS-CoV-2 from infected humans and may serve as asymptomatic carriers.[271,273,274,275] Known cases of felines testing positive for the virus have been reported in both domestic and zoo animals, including tigers and lions.[276,277] Due to the above associations, efforts to develop feline-specific COVID-19 vaccine have been initiated.[269] It is important to emphasize that although SARS-CoV was found to be able to jump from felines to humans during an earlier outbreak,[278] currently there is no available evidence suggesting that SARS-CoV-2 responsible for the ongoing pandemic can jump interchangeably between felines and humans
Ferret reservoir – There is sufficient evidence to suggest that domesticated (and wild) ferrets are permissive to SARS-CoV-2 infection.[275,279] Experimental data indicate that the virus can effectively replicate in the upper respiratory tract of ferrets; however, replication in other organs appears to be undetectable at this time.[275] Of note, infected ferrets exhibit a febrile response, the ability to transmit the virus to naïve ferrets by direct contact, and may develop acute bronchiolitis.[280] Given these findings, caution is warranted regarding ferrets serving as potential reservoir for animal-to-animal and animal-to-human transmission.[281] If the latter hypothesis is confirmed, subsequent work on a ferret-specific COVID-19 vaccine may become beneficial
Canine reservoir – The viral DNA of SARS-CoV-2 has been detected in two dogs belonging to owners infected with the novel coronavirus, with cases reported in Belgium and Hong Kong.[276,279] To be clear, unlike with felines, there is no current evidence to support that canines are likely to become a zoonotic reservoir. In fact, most recent data suggest that SARS-CoV-2 replicates poorly in dogs.[275] While this does not guarantee that a viral mutation resulting in increased canine susceptibility to the COVID-19 pathogen will not happen, it does make such event highly unlikely
Mink reservoir – There is sufficient evidence to demonstrate the ability of SARS-CoV-2 to naturally infect various members of the Mustelidae family, also inclusive of ferrets, weasels, badgers, and otters.[279] Although mink seems to be less susceptible to COVID-19 infection than cats, the possibility that various members of the Mustelidae family may be harboring SARS-CoV-2, both in the wild and in the domesticated setting, is certainly a concern. In a more recent development, the Government of Denmark was considering a nationwide intervention prompted by the discovery that SARS-CoV-2 had mutated in mink, after being passed on by humans, with subsequent evidence of spread to/among humans.[282,283] Further research is clearly warranted in this area, with appropriate mitigation measures (if the above report is confirmed)
Hamster and other small rodent reservoirs – In addition to a significant utility as COVID-19 laboratory subjects,[284,285,286] hamsters and other small rodents also are among the most popular pet animals.[287] Although no evidence of SARS-CoV-2 transmission exists between small rodents and other mammals, their common use in laboratory models presents important risks. First, there is a small but nontrivial risk of cross-species transmission among laboratory animals. Second, there is a smaller but not improbable risk of viral mutation that would enable a rodent-to-human “reverse zoonotic” jump[288]
Livestock versus wild animals as intermediate hosts – Coronaviruses as a group of viruses are known to co-infect a broad range of vertebrate species, including livestock, birds, bats, mice, and a variety of wild animals.[289,290] Reassuring in this context is the finding that neither pigs nor chickens appear to be susceptible to SARS-CoV-2 infection.[291] Similarly, little to no transmission ability was found in the studies of cows, sheep, horses, ducks, or geese.[291] A broad range of wild animals were also tested, reducing the concern regarding their suitability to serve as intermediate hosts[291]
Research laboratory and other important safety and surveillance considerations – Given the ability of the SARS-CoV-2 virus to potentially jump between humans, canines, felines, and the Mustelidae family, important question emerges – Can the current pandemic be the first one to evolve into a panzoonotic event?[271] Certainly, the risk of transmission to pets and other wild and domestic animals strongly mandates a one-health strategy during the global response to the COVID-19 pandemic.[276] In summary, the purpose of this manuscript section is not to instill unnecessary fear, but rather to ensure that global PH systems are prepared in the unlikely case that in its quest to survive, the SARS-CoV-2 manages to successfully mutate and adapt to new, more diverse intermediate hosts and/or animal reservoirs.
Blind spot #14: Homelessness and COVID-19
In May 2020, Nature reported:
“Researchers are beginning to test homeless individuals in the United States for the virus that causes COVID-19, and are discovering that the situation is out of control: tests are rare and outbreaks are spreading below the radar.”[292]
There were approximately 1.4 million people in homeless shelters in America at the start of the pandemic, and with unemployment reaching 40 million at one point, the situation reached unprecedented proportions. Of critical importance, available data reveal that people who are homeless have a higher prevalence of SARS-CoV-2.[293] Much of their plight can be attributed to the lack of safe housing, wherein they experience difficulties in maintaining physical distancing, isolation, and quarantine.[294] At the same time, many services regularly available to the homeless suffer from limited availability during the pandemic, such as support for intimate partner violence and other harm reduction initiatives (e.g., counseling services, places to safely use drugs).[294]
There was a chronic shortage of affordable housing before COVID-19, and this pandemic has magnified and highlighted the importance of the problem. There is little doubt that housing is a determinant of inequities during the current pandemic.[295] A lack of access to acceptable accommodations can be associated with various downstream health manifestations, including worsening heart disease, chronic pulmonary conditions, mental health conditions, and increased mortality.[296,297] Mehdipanah makes an additional important point that, “At the community level, housing instability, especially in low income neighborhoods, could result in long-term vacancy, reducing housing value and increasing blight and crime,” thereby compounding the effects of the pandemic.[295] Regarding homelessness, several specific populations require special attention, including children, youth, drug users, pregnant women as well as those in rural settings.
Adequate housing should be available to all children. Within this context, however, it is important to remember that any shelter provided during a pandemic should be compliant with PH recommendations outlined elsewhere in this paper (e.g., NPIs, adequate PPE and hygiene product supplies, etc.).[298] Although poor housing conditions existed before COVID-19 in this time of high unemployment and increasing homelessness, the conditions are especially difficult for many children. Prior to the pandemic, nearly 60% of all homeless people were children and, on any given night, there were 58,000 homeless families and over 100,000 homeless children in the USA (let alone the rest of the world).[299] While many children may not be out on the streets, they are in situ ations where they and/or their families are living or staying with friends or relatives in crowded situations, or living on campgrounds or motels, which increases their risk of contracting a highly infectious illness.[299,300] When the moratorium on evictions during this pandemic expires, this situation may be exponentially exaggerated.
Youth (ages 18–25 years) experiencing homelessness (YEH) are also vulnerable. In a report by Tucker et al., most YEH engage in protective behaviors (masks and social distancing), but 38%–48% reported mental health complaints. In addition, 16%–28% of YEH reported increased use of alcohol, tobacco, and marijuana; over 50% could not meet basic food needs; and 32%–44% could not obtain mental health access.[301] For this reason, special consideration should be given to the YEH population, focusing on providing not only housing, medical care, and educational opportunities, but also fostering their entry into the workforce.[302]
People who inject drugs (PWID) are also in need of special attention during the pandemic in that many are homeless and living in poor hygienic conditions that have a high population density. Moreover, PWID have an increased rate of comorbidities and chronic health conditions.[303] Along with increased rates of homelessness, PWID may engage in unsafe intravenous drug injections and unsafe sex practices, all of which may be exacerbated during this pandemic. Additional risk to the PWID population is associated with the inability to readily access critical PH information while facing potential reductions in key public services.[303] In Europe, these problems may be exceptionally challenging because of the post-2008 economic crisis measures in which PH expenditures and harm reduction efforts were substantially limited.[304]
Rural settings have just as high a rate of homelessness as cities during this pandemic. At the same time, rural regions have also seen significant cuts in both funding and the availability of important public health services.[305,306] Because of these rural-urban disparities, it is crucial that appropriate support programs are created and funded to serve the homeless in rural regions. At present, food and housing security for the rural population is under a much higher threat than that of the urban homeless.[307]
One final point to be made in regard to housing the homeless during the pandemic is that shelter characteristics matter immensely. Karb et al. demonstrated that SARS-CoV-2 prevalence varies with the practices and characteristics of the shelter environment.[308] These authors demonstrated that shelters with greater proportion of transient residents, and at full or high capacity, had higher rates of SARS-CoV-2 infections than those with limited number of spaces and lower throughput of new occupants; also, the population density of the local neighborhood in which the shelter is located may play a role.[308] Homelessness is a pervasive problem in this pandemic and will only get worse as employment opportunities deteriorate, especially if evictions are allowed.
SYNTHESIS AND CONCLUSIONS
The COVID-19 crisis has affected the general public, health-care providers, and the economy. Our collective ability to organize rational, flexible, and effective responses to the pandemic represents nothing less than an existential crisis for humanity. The pandemic has proven how interdependent the global community is today. We have seen how the consequences of incompetent leadership and lack of PH preparedness can be both far reaching and devastating, affecting not only morbidity and mortality from the virus itself, but also excess mortality from other communicable and noncommunicable diseases. The damage inflicted on local and global economies continues to represent an ongoing threat to social stability.309
To resolve the pandemic, and improve global resiliency and preparedness for future international health security threats in the process, the world needs evidence-based strategies to address the existing health system vulnerabilities across several domains. This depends not only on the generation of public health data but also on the education of more scientifically informed leaders at all levels of the society to interpret and use such data constructively. We have identified a number of potential “blind spots” that became apparent during the COVID-19 pandemic. Health-care workers, PH advocates, politicians, and the general public will need to carefully and rigorously examine these blind spots, as lack of awareness or ignoring them will cause unpredictable, long-lasting harms and consume significant amounts of resources.[259]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chauhan V, Galwankar SC, Yellapu V, Perez-Figueroa IJ, Stawicki SP. State of the Globe: The trials and tribulations of the COVID-19 pandemic: Separated but together, telemedicine revolution, frontline struggle against “silent hypoxia,” the relentless search for novel therapeutics and vaccines, and the daunting prospect of “COVIFLU”. J Glob Infect Dis. 2020;12:39–43. doi: 10.4103/jgid.jgid_96_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strzelecki A. The second worldwide wave of interest in coronavirus since the COVID-19 outbreaks in South Korea, Italy and Iran: A Google Trends study. Brain Behav Immun. 2020;88:950–1. doi: 10.1016/j.bbi.2020.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stawicki SP, Jeanmonod R, Miller AC, Paladino L, Gaieski DF, Yaffee AQ. The 2019-2020 novel coronavirus (severe acute respiratory syndrome coronavirus 2) pandemic: A joint American college of academic international medicine-world academic council of emergency medicine multidisciplinary COVID-19 working group consensus paper. J Global Infect Dis. 2020;12:47. doi: 10.4103/jgid.jgid_86_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kalra S, Kelkar D, Galwankar SC, Papadimos TJ, Stawicki SP, Arquilla B. The emergence of Ebola as a global health security threat: From 'lessons learned' to coordinated multilateral containment efforts. J Global Infect Dis. 2014;6:164. doi: 10.4103/0974-777X.145247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalil AC. Treating COVID-19-off-label drug use, compassionate use, and randomized clinical trials during pandemics. JAMA. 2020;323:1897–8. doi: 10.1001/jama.2020.4742. [DOI] [PubMed] [Google Scholar]
- 6.Gupta R, Misra A. Contentious issues and evolving concepts in the clinical presentation and management of patients with COVID-19 infection with reference to use of therapeutic and other drugs used in co-morbid diseases (hypertension, diabetes etc.) Diabetes Metab Syndr. 2020;14:251–4. doi: 10.1016/j.dsx.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lush T, Chandler K, Foody K. Coronavirus: 4th of July Fuels Worries about Skyrocketing Coronavirus Cases in US. 2020. Jul 5, [Last accessed 2020 Nov15]. Available from: https://abc7.com/coronavirus-us-cases-covid-19/6299780/
- 8.Mirvis P. Reflections: US coronavirus crisis management-learning from failure Donald Trump and more, January-April, 2020. J Change Manag. 2020;23:1–29. [Google Scholar]
- 9.Graham A, Cullen F, Pickett J, Jonson C, Haner M, Sloan M. Faith in Trump, Moral Foundations, and Social Distancing Defiance during the Coronavirus Pandemic. Moral Foundations, and Social Distancing Defiance during the Coronavirus Pandemic (April 22, 2020) 2020 [Google Scholar]
- 10.Tanne JH. COVID-19: Trump returns to white house amid confusion over his illness and treatment. Br Med J 2020. 2020;371:m3897. doi: 10.1136/bmj.m3897. [DOI] [PubMed] [Google Scholar]
- 11.Stawicki SP, Galwankar SC. Winning together: Novel coronavirus (COVID-19) infographic. J Emerg Trauma Shock. 2020;13:103. doi: 10.4103/0974-2700.281047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ngonghala CN, Iboi E, Gumel AB. Could masks curtail the post-lockdown resurgence of COVID-19 in the US? Mathemat Biosci. 2020;329:108452. doi: 10.1016/j.mbs.2020.108452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saul A, Scott N, Crabb BS, Majundar SS, Coghlan B, Hellard ME. Victoria's response to a resurgence of COVID-19 has averted 9,000-37,000 cases in July 2020. Med J Australia. 2020;4:1. [Google Scholar]
- 14.Eurosurveillance Editorial Team. Rapid risk assessment from ECDC: Resurgence of reported cases of COVID-19 in the EU/EEA, the UK and EU candidate and potential candidate countries. Euro Surveill. 2020;25:2007021. doi: 10.2807/1560-7917.ES.2020.25.26.2007021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Panovska-Griffiths J, Kerr CC, Stuart RM, Mistry D, Klein DJ, Viner RM, et al. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: A modelling study. Lancet Child Adolesc Health. 2020;4:817–27. doi: 10.1016/S2352-4642(20)30250-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkatesan P. COVID-19 in Iran: Round 2. Lancet Infect Dis. 2020;20:784. doi: 10.1016/S1473-3099(20)30500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang L, Zhang X, Zhang X, Wei Z, Zhang L, Xu J, et al. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J Infect. 2020;80:e1–13. doi: 10.1016/j.jinf.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dave DM, Friedson AI, Matsuzawa K, Sabia JJ, Safford S. Black lives matter protests, social distancing, and COVID-19. Natl Bureau Econom Res. 2020;6:1. [Google Scholar]
- 19.Roberts R. The Three Blind Spots of Politics. 2020. [Lasdt accessed on 2020 Nov 15]. Available from: https://medium.com/@russroberts/the-three-blind-spots-of-politicsc5e8cc7c60b6 .
- 20.Brende B. COVID-19 Pandemic Shows We Must Reduce Our Blind Spots to Risk. 2020. [Last accessd on 2020 Nov 15]. Available from: https://www.weforum.org/agenda/2020/03/covid-19-pandemic-shows-we-must-reduce-our-blindspots-to-risk/
- 21.Sergison M. How 'Blindspotting' Makes the Personal Political. 2020. [Lasdt accessed on 2020 Nov 15]. Available from: https://filmschoolrejects.com/how-blindspotting-makes-the-personal-political/
- 22.Rea S. Researchers Find Everyone has a Bias Blind Spot. 2020. [Lasdt accessed on 2020 Nov 15]. Available from: https://www.cmu.edu/news/stories/archives/2015/june/bias-blind-spot.html .
- 23.Scopelliti I, Min HL, McCormick E, Kassam KS, Morewedge CK. Individual differences in correspondence bias: Measurement, consequences, and correction of biased interpersonal attributions. Manag Sci. 2018;64:1879–910. [Google Scholar]
- 24.Scopelliti I, Morewedge CK, McCormick E, Min HL, Lebrecht S, Kassam KS. Bias blind spot: Structure, measurement, and consequences. Manag Sci. 2015;61:2468–86. [Google Scholar]
- 25.Lofredo MP. Social Cohesion, Trust, and Government Action against Pandemics. 2020 [Google Scholar]
- 26.Conti K, Desai S, Stawicki SP, Papadimos TJ. The evolving interplay between social media and international health security: A point of view, in contemporary developments and perspectives in international health security-volume 1. IntechOpen. 2020;7:1. [Google Scholar]
- 27.Stawicki SP, Firstenberg MS, Papadimos TJ. The Growing Role of Social Media in International Health Security: The Good, the Bad, and the Ugly, in Global Health Security. Cham, Switzerland: Springer; 2020. pp. 341–57. [Google Scholar]
- 28.Stanley-Becker I. Mask or No Mask? Face Coverings Become Tool in Partisan Combat. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.washingtonpost.com/politics/in-virus-response-riven-by-politics-masks-are-latest-rorschachtest/2020/05/12/698477d4-93e6-11ea-91d7-cf4423d47683_story.html .
- 29.WHO. Coronavirus Disease (COVID-19) Advice for the Public: When and how to use Masks. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/whenand-how-to-use-masks .
- 30.Yoosefi Lebni J, Abbas J, Moradi F, Salahshoor MR, Chaboksavar F, Irandoost SF. How the COVID-19 pandemic effected economic, social, political, and cultural factors: A lesson from Iran. Int J Soc Psychiatry. 2020;7:0020764020939984. doi: 10.1177/0020764020939984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Motta M, Stecula D, Farhart C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the US. Canadian J Political Sci Rev Canad de Sci Politique. 2020;5:1–8. [Google Scholar]
- 32.Lasco G. Medical populism and the COVID-19 pandemic. Global Public Health. 2020;15:1–13. doi: 10.1080/17441692.2020.1807581. [DOI] [PubMed] [Google Scholar]
- 33.Bosancianu CM, Dionne KY, Hilbig H, Humphreys M, Sampada KC, Lieber N, et al. Political and Social Correlates of Covid-19 Mortality. 2020 [Google Scholar]
- 34.Chauhan V, Galwankar S, Arquilla B, Garg M, Di Somma S, El-Menyar A, et al. Novel coronavirus (COVID-19): Leveraging telemedicine to optimize care while minimizing exposures and viral transmission. J Emerg Trauma Shock. 2020;13:20. doi: 10.4103/JETS.JETS_32_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Markel H. America's Coronavirus Endurance test. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.newyorker.com/science/medical-dispatch/americas-coronavirus-endurance-test .
- 36.Gutierrez P, Clarke S. Coronavirus World Map: Which Countries have the Most COVID-19 Cases and Deaths? 2020. [Retrieved 2020 Nov 15]. Available from: https://www.theguardian.com/world/2020/aug/12/coronavirus-world-mapwhich-countries-have-the-most-covid-19-cases-and-deaths .
- 37.Cozzens SE, Woodhouse EJ. Handbook of Science and Technology Studies. Combridge, MA: MIT Press; 1995. Science, government, and the politics of knowledge; pp. 533–53. [Google Scholar]
- 38.Lupton D. Risk as moral danger: The social and political functions of risk discourse in public health. Int J Health Serv. 1993;23:425–35. doi: 10.2190/16AY-E2GC-DFLD-51X2. [DOI] [PubMed] [Google Scholar]
- 39.Barrett CD, Yaffe MB. COVID-19: All the wrong moves in all the wrong places. Am Assoc Adv Sci. 2020;13:eabe4242. doi: 10.1126/scisignal.abe4242. [DOI] [PubMed] [Google Scholar]
- 40.Hartley K, Jarvis DS. Policymaking in a low-trust state: Legitimacy, state capacity, and responses to COVID-19 in Hong Kong. Policy Soc. 2020;39:403–23. doi: 10.1080/14494035.2020.1783791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Capano G, Howlett M, Jarvis DS, Ramesh M, Goyal N. Mobilizing policy (in) capacity to fight COVID-19: Understanding variations in state responses. Policy Soc. 2020;39:285–308. doi: 10.1080/14494035.2020.1787628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scott D. The Covid-19 risks for different age groups, explained. Vox Med. 2020;23:3:1. [Google Scholar]
- 43.Day M. Covid-19: Four fifths of cases are asymptomatic, China figures indicate. Br Med J. 2020;369:m1375. doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- 44.Khan N, Naushad M, Akbar A, Faisal S, Fahad S. Critical review of COVID-2019 in Italy and impact on its economy. SSRN. 2020;6:3632007. [Google Scholar]
- 45.Mayilvaganan M. COVID-19 Pandemic in the indo-pacific: How the countries are dealing amidst changing geopolitics (NIAS/CSS/ISSSP/U/RR/15/2020) National Institute of Advanced Studies. 2020;1:1–139. [Google Scholar]
- 46.Kaustuv C, Chatterjee K, Kumar A, Shankar S. Healthcare impact of COVID-19 epidemic in India: A stochastic mathematical model. Med J Armed Forces India. 2020;22:1–10. doi: 10.1016/j.mjafi.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lu N, Cheng KW, Qamar N, Huang KC, Johnson JA. Weathering COVID-19 storm: Successful control measures of five Asian countries. Am J Infect Control. 2020;48:851–2. doi: 10.1016/j.ajic.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fritz P. COVID-19 Be Damned: How Poland Is Beating another Crisis. 2020. [Last accessd on 2020 Nov 15]. Available from: https://worldcrunch.com/business-finance/covid-19-be-damned-how-poland-is-beating-another-crisis .
- 49.Walker S, Smith H. Why has Eastern Europe Suffered Less from Coronavirus than the West? 2020. [Last accessd on 2020 Nov 15]. Available from: https://www.theguardian.com/world/2020/may/05/why-has-eastern-europe-suffered-less-from-coronavirus-than-the-west .
- 50.Parro V, Lafetá M, Ipolito F, Toporcov T. Predicting COVID-19 in very large countries: The case of Brazil. Researchsquare. 2020;9:1–12. doi: 10.1371/journal.pone.0253146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schellekens P, Sourrouille DM. COVID-19 Mortality in Rich and Poor Countries: A Tale of Two Pandemics? World Bank Policy Research Working Paper. 2020 [Google Scholar]
- 52.Xu S, Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395:1321–2. doi: 10.1016/S0140-6736(20)30845-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adebowale V, Alderson D, Burn W, Dixon J, Godlee F, Goddard A, et al. Covid-19: Call for a rapid forward looking review of the UK's preparedness for a second wave-an open letter to the leaders of all UK political parties. BMJ. 2020;6:369. doi: 10.1136/bmj.m2514. [DOI] [PubMed] [Google Scholar]
- 54.Jayatilleke AU, Dayarathne S, de Silva P, Siribaddana P, Abeygunawardana RA, Nieveras O. COVID-19 case forecasting model for Sri Lanka based on Stringency Index. medRxiv. 2020;1:1–18. [Google Scholar]
- 55.Fowler JH, Hill SJ, Obradovich N, Levin R. The effect of stay-at-home orders on COVID-19 infections in the United States. arXiv Preprint arXiv. 2020;1:1–16. [Google Scholar]
- 56.Flaxman S, Mishra S, Gandy A, Unwin HJ, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584:257–61. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 57.Lee J, Chen K. Tackling COVID-19 complacency in the workplace. Psychol Res Against. 2020;21:1–4. [Google Scholar]
- 58.Stanford JL. I was wrong: A surgeon's first-person account of his COVID-19 illness. Am Surg. 2020;86:572–6. doi: 10.1177/0003134820924398. [DOI] [PubMed] [Google Scholar]
- 59.Miller KA, Mannix R, Schmitz G, Monuteaux MC, Lee LK. Impact of COVID-19 on professional and personal responsibilities of Massachusetts physicians. Am J Emerg Med. 2020;8 doi: 10.1016/j.ajem.2020.08.051. doi: 10.1016/j.ajem.2020.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee S, Hwang C, Moon MJ. Policy learning and crisis policy-making: Quadruple-loop learning and COVID-19 responses in South Korea. Policy Soc. 2020;39:363–81. doi: 10.1080/14494035.2020.1785195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jung J, Hong MJ, Kim EO, Lee J, Kim MN, Kim SH. Investigation of a nosocomial outbreak of COVID-19 in a pediatric ward in South Korea: Successful control by early detection and extensive contact tracing with testing. Clin Microbiol Infect. 2020;26:1574–5. doi: 10.1016/j.cmi.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baniamin HM, Rahman M, Hasan MT. The COVID-19 pandemic: Why are some countries coping more successfully than others? Asia Pacific J Public Administ. 2020;42:153–69. [Google Scholar]
- 63.Esposito S, Principi N, Leung CC, Migliori GB. Universal use of face masks for success against COVID-19: Evidence and implications for prevention policies. Eur Respir J. 2020;55 doi: 10.1183/13993003.01260-2020. doi: 10.1183/13993003.01260-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Deb P, Furceri D, Ostry JD, Tawk N. The effect of containment measures on the COVID-19 pandemic. IMF Working Paper. 2020;WP/20/159:1–42. [Google Scholar]
- 65.Gupta M, Abdelsalam M, Mittal S. Enabling and enforcing social distancing measures using smart city and its infrastructures: A COVID-19 Use case. arXiv Preprint. 2020;2004:09246. [Google Scholar]
- 66.Nishimoto Y, Inoue K. Curve-fitting approach for COVID-19 data and its physical background. medRxiv. 2020;1 doi: 10.1101/2020.07.02.20144899. [Google Scholar]
- 67.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7:547–60. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Imran N, Aamer I, Sharif MI, Bodla ZH, Naveed S. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pak J Med Sci. 2020;36:1106–16. doi: 10.12669/pjms.36.5.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Volpato S, Landi F, Incalzi RA. A frail health care system for an old population: Lesson form the COVID-19 outbreak in Italy. J Gerontol A Biol Sci Med Sci. 2020;4:glaa087. doi: 10.1093/gerona/glaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Emmanuel Awucha N, Chinelo Janefrances O, Chima Meshach A, Chiamaka Henrietta J, Ibilolia Daniel A, Esther Chidiebere N. Impact of the COVID-19 pandemic on consumers' access to essential medicines in Nigeria. Am J Trop Med Hyg. 2020;103:1630–4. doi: 10.4269/ajtmh.20-0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Choudhari R. COVID 19 pandemic: Mental health challenges of internal migrant workers of India. Asian J Psychiatr. 2020;54:102254. doi: 10.1016/j.ajp.2020.102254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiov Dis. 2020;4 doi: 10.1016/j.pcad.2020.04.005. doi:10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kaysin A, Carvajal DN, Callahan CW. The role of alternate care sites in health system responsiveness to COVID-19. Am Public Health Assoc. 2020;110:1344–75. doi: 10.2105/AJPH.2020.305838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moroni F, Gramegna M, Ajello S, Beneduce A, Baldetti L, Vilca LM, et al. Collateral damage: Medical care avoidance behavior among patients with acute coronary syndrome during the COVID-19 pandemic. JACC. 2020;2:1620–4. doi: 10.1016/j.jaccas.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Allahwala UK, Denniss AR, Zaman S, Bhindi R. Cardiovascular disease in the post-COVID-19 era-the impending tsunami? Heart Lung Circul. 2020;29:809–811. doi: 10.1016/j.hlc.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kaldy J. Telemedicine: Not new but never more useful. Caring Ages. 2020;21:19. [Google Scholar]
- 77.Grossman SN, Han SC, Balcer LJ, Kurzweil A, Weinberg H, Galetta SL, et al. Rapid implementation of virtual neurology in response to the COVID-19 pandemic. Neurology. 2020;94:1077–87. doi: 10.1212/WNL.0000000000009677. [DOI] [PubMed] [Google Scholar]
- 78.Montgomery A, Hunter D, Blair E, Hendricksen M. Telemedicine Today: The State of Affairs. Ann Arbor, MI: Altarum Institute; 2015. [Google Scholar]
- 79.Bonalumi G, Giambuzzi I, Barbone A, Ranieri C, Cavallotti L, Trabattoni P, et al. A call to action becomes practice: Cardiac and vascular surgery during the COVID-19 pandemic based on the Lombardy emergency guidelines. Eur J Cardiothorac Surg. 2020;58:319–27. doi: 10.1093/ejcts/ezaa204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Puech-Leão P, César LA, De Luccia N. COVID-19, vascular diseases, and vascular services. Clinics. 2020;75 doi: 10.6061/clinics/2020/e1979. doi: 10.6061/clinics/2020/e1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Patriti A, Baiocchi GL, Catena F, Marini P, Catarci M. Emergency general surgery in Italy during the COVID-19 outbreak:First survey from the real life. World J Emerg Surg. 2020;15:1–7. doi: 10.1186/s13017-020-00314-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Perrin R, Riste L, Hann M, Walther A, Mukherjee A, Heald A. Into the looking glass: Post-viral syndrome post COVID-19. Med Hypoth. 2020;144:110055. doi: 10.1016/j.mehy.2020.110055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Islam MF, Cotler J, Jason LA. Post-viral fatigue and COVID-19: Lessons from past epidemics. Fatigue. 2020;8:61–9. [Google Scholar]
- 84.Metzl JD, McElheny K, Robinson JN, Scott DA, Sutton KM, Toresdahl BG. Considerations for return to exercise following mild-to-moderate COVID-19 in the recreational athlete. HSS J. 2020;8:1–6. doi: 10.1007/s11420-020-09777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13:2330–9. doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shah S, Danda D, Kavadichanda C, Das S, Adarsh MB, Negi VS. Autoimmune and rheumatic musculoskeletal diseases as a consequence of SARS-CoV-2 infection and its treatment. Rheumatol Int. 2020;40:1539–54. doi: 10.1007/s00296-020-04639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vaknin S. The Effect of Coronavirus on Mental Health. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.youtube.com/watch?v=ZT6Wn-weaNM .
- 88.Sheehy LM. Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Health Surveillance. 2020;6:e19462. doi: 10.2196/19462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Menon V, Padhy SK. Mental health among COVID-19 survivors: Are we overlooking the biological links? Asian J Psychiatry. 2020;53:102217. doi: 10.1016/j.ajp.2020.102217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Firstenberg MS, Libby M, Roberts R, Petersen C, Hanna J. Complete pulmonary recovery after COVID-19 infection requiring extracorporeal membrane oxygenation: A case report. Int J Critical Illness Injury Sci. 2020;10:155. doi: 10.4103/IJCIIS.IJCIIS_132_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yan G, Lee CK, Lam LT, Yan B, Chua YX, Lim AY, et al. Covert COVID-19 and false-positive dengue serology in Singapore. Lancet Infect Dis. 2020;20:536. doi: 10.1016/S1473-3099(20)30158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lustig Y, Keler S, Kolodny R, Ben-Tal N, Atias-Varon D, Shlush E, et al. Potential antigenic cross-reactivity between SARS-CoV-2 and Dengue viruses. Clin Infect Dis. 2020;7:ciaa1207. doi: 10.1093/cid/ciaa1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nath H, Mallick A, Roy S, Sukla S, Biswas S. Computational modelling predicts that Dengue virus antibodies can bind to SARS-CoV-2 receptor binding sites: Is pre-exposure to dengue virus protective against COVID-19 severity? OSF Preprint. 2020;6:1–22. doi: 10.1016/j.csbj.2020.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Navarro JC, Arrivillaga-Henríquez J, Salazar-Loor J, Rodriguez-Morales AJ. COVID-19 and dengue, co-epidemics in Ecuador and other countries in Latin America: Pushing strained health care systems over the edge. Travel Med Infect Dis. 2020;37:101656. doi: 10.1016/j.tmaid.2020.101656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lorenz C, Azevedo TS, Chiaravalloti-Neto F. COVID-19 and dengue fever: A dangerous combination for the health system in Brazil. Travel Med Infect Dis. 2020;35:101659. doi: 10.1016/j.tmaid.2020.101659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Iyengar KP, Jain VK. Tuberculosis and COVID-19 in India-double trouble! Indian J Tubercul. 2020;7 doi: 10.1016/j.ijtb.2020.07.014. doi 10.1016/j.ijtb.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kost GJ. Geospatial spread of antimicrobial resistance, bacterial and fungal threats to COVID-19 survival, and point-of-care solutions. Arch Pathol Lab Med. 2020;7 doi: 10.5858/arpa.2020-0284-RA. doi: 10.5858/arpa.2020-0284-RA. [DOI] [PubMed] [Google Scholar]
- 99.Chopra K, Arora V, Singh S. COVID 19 and tuberculosis. Indian J Tubercul. 2020;67:149. doi: 10.1016/j.ijtb.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Liu Y, Bi L, Chen Y, Wang Y, Fleming J, Yu Y, Gu Y, et al. Active or latent tuberculosis increases susceptibility to COVID-19 and disease severity. medRxiv. 2020;1:1–15. [Google Scholar]
- 101.Cepheid_USA. Rapid, Nera-Patient Test for the Detection of the 2019 Novel Coronavirus that Causes COVID-19. 2020. [Retrieved on Nov 15]. Available from: https://www.cepheid.com/coronavirus .
- 102.ICMR. Advisory for use of Cartridge Based Nucleic Acid Amplification Test (CBNAAT) using Cepheid Xpert Xpress SARS-CoV-2. 2020. [Retrieved on Nov 15]. Available from: https://www.icmr.gov.in/pdf/covid/labs/Cepheid_Xpert_Xpress_SARS-CoV2_advisory_v3.pdf .
- 103.Burzynski J, Macaraig M, Nilsen D, Schluger NW. Transforming essential services for tuberculosis during the COVID-19 pandemic: Lessons from New York City. Int J Tuberc Lung Dis. 2020;24:735–6. doi: 10.5588/ijtld.20.0283. [DOI] [PubMed] [Google Scholar]
- 104.Udwadia ZF, Vora A, Tripathi AR, Malu KN, Lange C, Raju RS. COVID-19-Tuberculosis interactions: When dark forces collide. Indian J Tubercul. 2020;7 doi: 10.1016/j.ijtb.2020.07.003. doi: 10.1016/j.ijtb.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lee VS, Chong WL, Sukumaran SD, Nimmanpipug P, Letchumanan V, Goh BH, et al. Computational screening and identifying binding interaction of anti-viral and anti-malarial drugs: Toward the potential cure for SARS-CoV-2. Prog Drug Dis Biomed Sci. 2020;3:a0000065. [Google Scholar]
- 106.Ahmed AE. Incidence of coronavirus disease (COVID-19) and countries affected by malarial infections. Travel Med Infect Dis. 2020;37:101693. doi: 10.1016/j.tmaid.2020.101693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bernard FO, Akaito JA, Joseph I, David KB. COVID-19: The trends of conspiracy theories vs. facts. Pan Afr Med J. 2020;35(Suppl 2):147. doi: 10.11604/pamj.supp.2020.35.147.25536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mahase E. Covid-19: Hydroxychloroquine was ineffective as postexposure prophylaxis, study finds. Br Med J. 2020;6:369. doi: 10.1136/bmj.m2242. [DOI] [PubMed] [Google Scholar]
- 109.Chanda-Kapata P, Kapata N, Zumla A. COVID-19 and malaria: A symptom screening challenge for malaria endemic countries. Int J Infect Dis. 2020;94:151–3. doi: 10.1016/j.ijid.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hogan AB, Jewell BL, Sherrard-Smith E, Vesga JF, Watson OJ, Whittaker C, et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: A modelling study. Lancet Glob Health. 2020;8:e1132–41. doi: 10.1016/S2214-109X(20)30288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rogerson SJ, Beeson JG, Laman M, Poespoprodjo JR, William T, Simpson JA, et al. Identifying and combating the impacts of COVID-19 on malaria. BMC Med. 2020;18:239. doi: 10.1186/s12916-020-01710-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ansumana R, Sankoh O, Zumla A. Effects of disruption from COVID-19 on antimalarial strategies. Nature Med. 2020;26:1–2. doi: 10.1038/s41591-020-1047-5. [DOI] [PubMed] [Google Scholar]
- 113.Leyfman Y, Erick TK, Reddy SS, Galwankar S, Nanayakkara PW, Di Somma S, et al. Potential immunotherapeutic targets for hypoxia due to COVI-FLU. Shock. 2020;54:438–50. doi: 10.1097/SHK.0000000000001627. [DOI] [PubMed] [Google Scholar]
- 114.Ma S, Lai X, Chen Z, Tu S, Qin K. Clinical characteristics of critically ill patients co-infected with SARS-CoV-2 and the influenza virus in Wuhan, China. Int J Infect Dis. 2020;96:683–7. doi: 10.1016/j.ijid.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hashemi SA, Safamanesh S, Ghasemzadeh-Moghaddam H, Ghafouri M, Azimian A. High prevalence of SARS-CoV-2 and influenza A virus (H1N1) co-infection in dead patients in Northeastern Iran. J Med Virol. 2020;10:1–5. doi: 10.1002/jmv.26364. [DOI] [PubMed] [Google Scholar]
- 116.Wu D, Lu J, Liu Y, Zhang Z, Luo L. Positive effects of COVID-19 control measures on influenza prevention. Int J Infect Dis. 2020;95:345–6. doi: 10.1016/j.ijid.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jewell BL, Mudimu E, Stover J, Ten Brink D, Phillips AN, Smith JA, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: Results from multiple mathematical models. Lancet HIV. 2020;7:e629–40. doi: 10.1016/S2352-3018(20)30211-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nachega J, Seydi M, Zumla A. The late arrival of coronavirus disease 2019 (COVID-19) in Africa: Mitigating pan-continental spread. Clin Infect Dis. 2020;71:875–8. doi: 10.1093/cid/ciaa353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ridgway JP, Schmitt J, Friedman E, Taylor M, Devlin S, McNulty M, et al. HIV Care Continuum and COVID-19 Outcomes among People Living with HIV during the COVID-19 Pandemic, Chicago, IL. AIDS Behav. 2020;24:2770–2. doi: 10.1007/s10461-020-02905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Healthline. Fauci Warns about 'Post-Viral' Syndrome after COVID-19. 2020. [Retrieved on Nov 15]. Available from: https://www.healthline.com/health-news/fauci-warns-about-post-viral-syndrome-after-covid-19 .
- 121.Hosey MM, Needham DM. Survivorship after COVID-19 ICU stay. Nature Rev Dis Primers. 2020;6:1–2. doi: 10.1038/s41572-020-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Korzick KA, Layon AJ. The post-ICU clinic: Implications for critical care medicine and the health care system. ASA Newsletter. 2017;81:10–2. [Google Scholar]
- 123.Stam H, Stucki G, Bickenbach J. Covid-19 and post intensive care syndrome: A call for action. J Rehabilit Med. 2020;52:jrm00044. doi: 10.2340/16501977-2677. [DOI] [PubMed] [Google Scholar]
- 124.Greenhalgh T. Will COVID-19 be evidence-based medicine's nemesis? PLoS Med. 2020;17:e1003266. doi: 10.1371/journal.pmed.1003266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sugavanam SC, Natarajan B. Pseudoscientific beliefs and practices in the COVID-19 pandemic: A narrative review of unwanted experiments attributed to social media-based misinformation afflicting the public health. J Health Biol Sci. 2020;8:1–9. [Google Scholar]
- 126.Memon SA, Carley KM. Characterizing covid-19 misinformation communities using a novel Twitter dataset. arXiv Preprint. 2020;2008:00791. [Google Scholar]
- 127.Tapia L. COVID-19 and fake news in the Dominican Republic. Am J Tropical Med Hygiene. 2020;102:1172–4. doi: 10.4269/ajtmh.20-0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ahinkorah BO, Ameyaw EK, Hagan JE, Jr, Seidu AA, Schack T. Rising above misinformation or fake news in Africa: Another strategy to control COVID-19 spread. Front Communicat. 2020;5:45. [Google Scholar]
- 129.Freckelton QI. COVID-19: Fear, quackery, false representations and the law. Int J Law Psychiatry. 2020;72:101611. doi: 10.1016/j.ijlp.2020.101611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Shahi GK, Nandini D. FakeCovid-a multilingual cross-domain fact check news dataset for COVID-19. arXiv Preprint. 2020;6:11343. [Google Scholar]
- 131.Payande IA, Ronaghikhameneh A, Mirzapour H. [Retrieved on Nov 15];There must be a culpable behind the scenes; A novel trend in misinformation diffusion during the COVID-19 pandemic. Available at SSRN: https://ssrn.com/abstract=3596049. or http://dx.doi.org/10.2139/ssrn.3596049 . [Google Scholar]
- 132.Boetto E, Golinelli D, Carullo G, Fantini MP. Frauds in scientific research may be overcome with distributed ledger technologies. Preprints. 2020;6 doi: 10.1136/medethics-2020-106639. doi:10.20944/preprints202006.0310.v1. [DOI] [PubMed] [Google Scholar]
- 133.Rappoport J. Category Archives: Medical Fraud. [Retrieved 2020 Nov 15]. Available from: https://blog.nomorefakenews.com/2020/04/
- 134.Todaro JM, Angell M. [Retrieved on Nov 15];Gilead: Twenty-one billion reasons to discredit hydroxychloroquine. Available at SSRN: https://ssrn.com/abstract=3596049. or http://dx.doi.org/10.2139/ssrn.3596049 . [Google Scholar]
- 135.Lipworth W, Gentgall M, Kerridge I, Stewart C. Science at warp speed: Medical research, publication, and translation during the COVID-19 pandemic. J Bioeth Inq. 2020 doi: 10.1007/s11673-020-10013-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Besançon L, Peiffer-Smadja N, Segalas C, Jiang H, Masuzzo P, Smout CA, et al. Open science saves lives: Lessons from the COVID-19 pandemic. BioRxiv 2020. 2020 doi: 10.1186/s12874-021-01304-y. doi.org/10.1101/2020.08.13.249847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rothgerber H, Wilson T, Whaley D, Rosenfeld DL, Humphrey M, Moore A, et al. Politicizing the covid-19 pandemic: Ideological differences in adherence to social distancing. Bellarmine University. 2020;4:1–36. [Google Scholar]
- 138.Desta TT, Mulugeta T. Living with COVID-19-triggered pseudoscience and conspiracies. Int J Public Health. 2020;65:713–4. doi: 10.1007/s00038-020-01412-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Marín FX, Rusiñol J, Gallifa J. Pseudoscientific beliefs and psychopathological risks increase after COVID-19 social quarantine. Global Health. 2020;16:1–11. doi: 10.1186/s12992-020-00603-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Banai IP, Banai B, Mikloušić I. Beliefs in COVID-19 conspiracy theories predict lower level of compliance with the preventive measures both directly and indirectly by lowering trust in government medical officials. University of Zadar, Croatia. 2020;7:1–28. [Google Scholar]
- 141.Cinelli M, Quattrociocchi W, Galeazzi A, Valensise CM, Brugnoli E, Schmidt AL, et al. The covid-19 social media infodemic. arXiv Preprint. 2020;2003:05004. doi: 10.1038/s41598-020-73510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Amir Singh J. COVID-19: Science and global health governance under attack. South Afri Med J. 2020;110:1–2. doi: 10.7196/SAMJ.2020v110i5.14820. [DOI] [PubMed] [Google Scholar]
- 143.Kalichman SC. Denying AIDS: Conspiracy Theories, Pseudoscience, and Human Tragedy. New York, NY: Springer Science & Business Media; 2009. [Google Scholar]
- 144.Kaminstein D. Through a psychological lens darkly: Interpreting current reactions to the pandemic. Organizational Dynamics Working Papers. 2020;28:20–01. [Google Scholar]
- 145.Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Newcastle upon Tyne: Cambridge Scholars Publishing; 2019. [Google Scholar]
- 146.da Silva JA. An alert to COVID-19 Literature in Predatory Publishing Venues. Journal of Academic Librarianship. 2020;46:102187. doi: 10.1016/j.acalib.2020.102187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Myers K, Tham WY, Yin Y, Cohodes N, Thursby JG, Thursby M, et al. Quantifying the immediate effects of the COVID-19 pandemic on scientists. SSRN. 2020;5:3608302. doi: 10.1038/s41562-020-0921-y. [DOI] [PubMed] [Google Scholar]
- 148.Ghebreyesus TA. Safeguard research in the time of COVID-19. Nature Med. 2020;26:443. doi: 10.1038/s41591-020-0852-1. [DOI] [PubMed] [Google Scholar]
- 149.Fry CV, Cai X, Zhang Y, Wagner CS. Consolidation in a crisis: Patterns of international collaboration in early COVID-19 research. PLoS One. 2020;15:e0236307. doi: 10.1371/journal.pone.0236307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Horbach SP. Pandemic publishing: Medical journals strongly speed up their publication process for Covid-19. Quantitat Sci Stud. 2020;1(3):1056–67. [Google Scholar]
- 151.Rzymski P, Nowicki M, Mullin GE, Abraham A, Rodríguez-Román E, Petzold MB, et al. Quantity does not equal quality: Scientific principles cannot be sacrificed. Int Immunopharmacol. 2020;86:106711. doi: 10.1016/j.intimp.2020.106711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Plaza M, Paladino L, Opara IN, Firstenberg MS, Wilson B, Papadimos TJ, et al. The use of distributed consensus algorithms to curtail the spread of medical misinformation. Int J Acad Med. 2019;5:93. [Google Scholar]
- 153.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg (London, England) 2020;78:185. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Cavallo JJ, Forman HP. The economic impact of the COVID-19 pandemic on radiology practices. Radiology. 2020;4:201495. doi: 10.1148/radiol.2020201495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Burdorf A, Porru F, Rugulies R. The COVID-19 (Coronavirus) pandemic: Consequences for occupational health. Scand J Work Environ Health. 2020;46:229–30. doi: 10.5271/sjweh.3893. [DOI] [PubMed] [Google Scholar]
- 156.Ozili P, Arun T. Spillover of COVID-19: Impact on the global economy. SSRN. 2020;3:3562570. [Google Scholar]
- 157.Anoushiravani AA, O'Connor CM, DiCaprio MR, Iorio R. Economic impacts of the COVID-19 crisis: An orthopaedic perspective. J Bone Joint Surg Am. 2020;4 doi: 10.2106/JBJS.20.00557. 10.2106/JBJS.20.00557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from covid-19 by race/ethnicity and income. Am J Prevent Med. 2020;59:137–9. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kim SJ, Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ Behav. 2020;47:4:1. doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Thakur N, Lovinsky-Desir S, Bime C, Wisnivesky JP, Celedón JC. The structural and social determinants of the racial/ethnic disparities in the US COVID-19 pandemic: What's our role? Am J Resp Critical Care Med. 2020;202:943–9. doi: 10.1164/rccm.202005-1523PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Phillips D, Paul G, Fahy M, Dowling-Hetherington L, Kroll T, Moloney B, et al. The invisible workforce during the COVID-19 pandemic: Family carers at the frontline. HRB Open Res. 2020;3:24. doi: 10.12688/hrbopenres.13059.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Shadmi E, Chen Y, Dourado I, Faran-Perach I, Furler J, Hangoma P, et al. Health equity and COVID-19: Global perspectives. Int J Equity Health. 2020;19:104. doi: 10.1186/s12939-020-01218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ortega F, Orsini M. Governing COVID-19 without government in Brazil: Ignorance, neoliberal authoritarianism, and the collapse of public health leadership. Global Public Health. 2020;15:1257–77. doi: 10.1080/17441692.2020.1795223. [DOI] [PubMed] [Google Scholar]
- 164.Clark E, Fredricks K, Woc-Colburn L, Bottazzi ME, Weatherhead J. Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLoS Negl Trop Dis. 2020;14:e0008484. doi: 10.1371/journal.pntd.0008484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Fortuna LR, Tolou-Shams M, Robles-Ramamurthy B, Porche MV. Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: The need for a trauma-informed social justice response. Psychol Trauma. 2020;12:443–5. doi: 10.1037/tra0000889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Rowden R. The Deadly Ideas of Neoliberalism: How the IMF has Undermined Public Health and the Fight against AIDS. New York, NY: Zed Books Ltd; 2013. [Google Scholar]
- 167.Jennings B, Arras J. Ethical guidance for public health emergency preparedness and response: Highlighting ethics and values in a vital public health service. Centers for Disease Control and Prevention. 2008;10:1–192. [Google Scholar]
- 168.He W, Chen L, Chen L, Yuan G, Fang Y, Chen W, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;4:1–9. doi: 10.1038/s41375-020-0836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Cioffi A, Rinaldi R. COVID-19 and healthcare-associated infections. Int J Risk Safety Med. 2020;8:1–2. doi: 10.3233/JRS-200056. [DOI] [PubMed] [Google Scholar]
- 170.Fusco FM, Pisaturo M, Iodice V, Bellopede R, Tambaro O, Parrella G, et al. COVID-19 infections among healthcare workers in an infectious diseases specialized setting in Naples, Southern Italy: Results of a cross-sectional surveillance study. J Hosp Infect. 2020;105:596–600. doi: 10.1016/j.jhin.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. Jama. 2020;323:1439–40. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 172.McRae MP, Simmons GW, Christodoulides NJ, Lu Z, Kang SK, Fenyo D, et al. Clinical decision support tool and rapid point-of-care platform for determining disease severity in patients with COVID-19. Lab Chip. 2020;20:2075–85. doi: 10.1039/d0lc00373e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Stawicki SP, Stoltzfus JC, Aggarwal P, Bhoi S, Bhatt S, Kalra OP, et al. Academic college of emergency experts in India's INDO-US Joint Working Group and OPUS12 foundation consensus statement on creating a coordinated, multi-disciplinary, patient-centered, global point-of-care biomarker discovery network. Int J Crit Illness Injury Sci. 2014;4:200. doi: 10.4103/2229-5151.141398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Acharya R, Porwal A. A vulnerability index for the management of and response to the COVID-19 epidemic in India: An ecological study. Lancet Global Health. 2020;8:e1142–51. doi: 10.1016/S2214-109X(20)30300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kehr J. Blind spots and adverse conditions of care: Screening migrants for tuberculosis in France and Germany. Sociol Health Illness. 2018;34:251–65. doi: 10.1111/j.1467-9566.2011.01415.x. [DOI] [PubMed] [Google Scholar]
- 176.Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health. 2020;5:e475–83. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Government of India. Guidance Note on Bi-Directional TB-COVID Screening and Screening of TB among ILI/SARIcases. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.mohfw.gov.in/pdf/1TBCOVIDscreeningguidancenote.pdf .
- 178.Haimi M, Brammli-Greenberg S, Waisman Y, Baron-Epel O. Physicians' experiences, attitudes and challenges in a Pediatric Telemedicine Service. Pediatr Res. 2018;84:650–6. doi: 10.1038/s41390-018-0117-6. [DOI] [PubMed] [Google Scholar]
- 179.Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett ML, Huskamp HA. Suddenly becoming a “virtual doctor”: Experiences of psychiatrists transitioning to telemedicine during the COVID-19 pandemic. Psychiatric Serv. 2020;9:202000250. doi: 10.1176/appi.ps.202000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bouskill K, Smith-Morris C, Bresnick G, Cuadros J, Pedersen ER. Blind spots in telemedicine: A qualitative study of staff workarounds to resolve gaps in diabetes management. BMC Health Serv Res. 2018;18:617. doi: 10.1186/s12913-018-3427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Dawes RM. Social dilemmas. Ann Rev Psychol. 1980;31:169–93. [Google Scholar]
- 182.Nowak M, Highfield R. Supercooperators: Altruism, Evolution, and Why we Need Each other to Succeed. Delran, NJ: Simon and Schuster; 2011. [Google Scholar]
- 183.Johnson T, Dawes C, Fowler J, Smirnov O. Slowing COVID-19 transmission as a social dilemma: Lessons for government officials from interdisciplinary research on cooperation. J Behav Public Administ. 2020;3:1. [Google Scholar]
- 184.Li R, Rivers C, Tan Q, Murray MB, Toner E, Lipsitch M. The demand for inpatient and ICU beds for COVID-19 in the US: Lessons from Chinese cities. medRxiv. 2020;3 doi: 10.1101/2020.03.09.20033241. [Google Scholar]
- 185.Papadimos TJ, Marcolini EG, Hadian M, Hardart GE, Ward N, Levy MM, et al. Ethics of outbreaks position statement. Part 2: Family-centered care. Critical Care Med. 2018;46:1856–60. doi: 10.1097/CCM.0000000000003363. [DOI] [PubMed] [Google Scholar]
- 186.Coulter A, Richards T. Care during covid-19 must be humane and person centred. Br Med J. 2020;370:m3483. doi: 10.1136/bmj.m3483. [DOI] [PubMed] [Google Scholar]
- 187.Murray PD, Swanson JR. Visitation restrictions: Is it right and how do we support families in the NICU during COVID-19? J Perinatol. 2020;40:1576–81. doi: 10.1038/s41372-020-00781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.BBC. Coronavirus: Care Home Creates Garden Visits. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.bbc.com/news/av/uk-53100600 .
- 189.Virani AK, Puls HT, Mitsos R, Longstaff H, Goldman RD, Lantos JD. Benefits and risks of visitor restrictions for hospitalized children during the COVID pandemic. Pediatrics. 2020;146:e2020000786. doi: 10.1542/peds.2020-000786. [DOI] [PubMed] [Google Scholar]
- 190.Jennings WG, Perez NM. The immediate impact of COVID-19 on law enforcement in the United States. Am J Criminal Justice. 2020;11:1. doi: 10.1007/s12103-020-09536-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.CDC. What Law Enforcement Personnel Need to Know about Coronavirus Disease 2019 (COVID-19) 2020. [Retrieved 2020 Nov 15]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-law-enforcement.html .
- 192.Brito CS, Luna AM, Sanberg EL. Benchmarks for Developing a Law Enforcement Pandemic Flu Plan. 2009. [Retrieved 2020 Nov 15]. Available from: https://www.ojp.gov/sites/g/files/xyckuh186/files/Publications/PERF_PandemicBenchmarks.pdf .
- 193.Garcia UJ. Phoenix Police to Decrease Arrests for Nonviolent Crimes, Chief Says. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.azcentral.com/story/news/local/phoenix/2020/03/24/phoenix-police-decrease-arrestsnonviolent-crimes-chief-jeri-williams-says-coronavirus/2912891001/
- 194.Taleb NN. The black swan: The impact of the highly improbable. Vol. 2. New York: Random House; 2007. [Google Scholar]
- 195.He H, Harris L. The impact of COVID-19 pandemic on corporate social responsibility and marketing philosophy. J Bus Res. 2020;116:176–82. doi: 10.1016/j.jbusres.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.The Sidley Podcast. COVID-19 Places Corporate Social Responsibility in Sharp Relief. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.sidley.com/en/insights/newsupdates/2020/06/podcast-covid19-places-corporate-social-responsibility-in-sharp-relief .
- 197.Yokobosky LR. Ten questions on COVID-19 and charitable giving. CPA J. 2020;90:62–5. [Google Scholar]
- 198.Coppola DP. Introduction to International Disaster Management. Burlington, MA: Elsevier; 2006. [Google Scholar]
- 199.Liu BF, Fowler BM, Roberts HA, Herovic E. Keeping hospitals operating during disasters through crisis communication preparedness. Public Relat Rev. 2018;44:585–97. [Google Scholar]
- 200.Homeland Security Council. National Strategy for Pandemic Influenza. Washington, D.C: Homeland Security Council; 2005. [Google Scholar]
- 201.Liu S, Luo P, Tang M, Hu Q, Polidoro JP, Sun S, et al. Providing pharmacy services during the coronavirus pandemic. Int J Clin Pharm. 2020;42:299–304. doi: 10.1007/s11096-020-01017-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Duchene M. Infection control in soup kitchens and shelters. Home Healthc Now. 2010;28:471–8. doi: 10.1097/NHH.0b013e3181ed754f. [DOI] [PubMed] [Google Scholar]
- 203.Liebrenz M, Bhugra D, Buadze A, Schleifer R. Caring for persons in detention suffering with mental illness during the Covid-19 outbreak. Forensic Sci Int Mind Law. 2020;1:100013. doi: 10.1016/j.fsiml.2020.100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Franco-Paredes C, Jankousky K, Schultz J, Bernfeld J, Cullen K, Quan NG, et al. COVID-19 in jails and prisons: A neglected infection in a marginalized population. PLoS Negl Trop Dis. 2020;14:e0008409. doi: 10.1371/journal.pntd.0008409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Kim H, Kim S. Woman Spread COVID to 27 Customers at a Starbucks. Its Mask-Wearing Employees Escaped Infection. 2020. [Retrieved 2020 Nov 15]. Available from: https://fortune.com/2020/08/25/covid-outbreak-starbucks-seoul-masks-employees/
- 206.Stawicki SP, Wolfe S, Brisendine C, Eid S, Zangari M, Ford F, et al. The impact of comprehensive air purification on patient duration of stay, discharge outcomes, and health care economics: A retrospective cohort study. Surgery. 2020;168:968–74. doi: 10.1016/j.surg.2020.07.021. [DOI] [PubMed] [Google Scholar]
- 207.PBS. The Quest for Cleaner Hospital Air. PBS. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.youtube.com/watch?v=gdQDkh_f3cg&feature=emb_logo .
- 208.Bouffanais R, Lim SS. Cities Try to predict superspreading hotspots for COVID-19. Nature. 2020;583:352–5. doi: 10.1038/d41586-020-02072-3. [DOI] [PubMed] [Google Scholar]
- 209.University_of_Stirling. Environmental Biologists at the University of Stirling Have Warned That the Potential Spread of COVID-19 Via Sewage “Must not be Neglected” in the Battle to Protect Human Health. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.sciencedaily.com/releases/2020/05/200506133603.htm .
- 210.Quilliam RS, Weidmann M, Moresco V, Purshouse H, O'Hara Z, Oliver DM. COVID-19: The environmental implications of shedding SARS-CoV-2 in human faeces. Environ Int. 2020;140:105790. doi: 10.1016/j.envint.2020.105790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.RIVM. Coronavirus Monitoring in Sewage Research. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.rivm.nl/en/novel-coronavirus-covid-19/research/sewage#:~:text=Since%201%20April%2C%20RIVM%20has,the%20presence%20of%20the%20virus .
- 212.Cai J, Sun W, Huang J, Gamber M, Wu J, He G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg Infect Dis. 2020;26:1343–5. doi: 10.3201/eid2606.200412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Brende B. COVID-19 Pandemic Shows We Must Reduce Our Blind Spots to Risk. 2020. Mar 23, [Retrieved 2020 Nov 15]. Available from: https://www.forbes.com/sites/worldeconomicforum/2020/03/23/covid-19-pandemic-shows-we-must-reduce-our-blind-spots-to-risk/#5f0b26454688 .
- 214.Bureau of Labor Statistics Occupational Employment Statistics (OES) Program, F.L.W.M. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.brookings.edu/wp-content/uploads/2020/03/Front-Line-Workers-Appendix.docx2020 .
- 215.Food Safety Insights, E.I.Q.A.W.N., on Food Supply Chains in Crisis during the COVID-19 Pandemic. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.foodsafetystrategies.com/articles/1403-exclusive-interview-qa-withnicelabel-on-food-supply-chains-in-crisis-during-the-covid-19-pandemic .
- 216.Bloomberg News, C.P.T.S.A.V.C.A.S.D. 2020. [Retrieved 2020 Nov 15]. Available from: https://finance.yahoo.com/news/china-points-shrimp-covid-19-081937694.html .
- 217.Nychas GJ, Skandamis PN, Tassou CC, Koutsoumanis KP. Meat spoilage during distribution. Meat Sci. 2008;78:77–89. doi: 10.1016/j.meatsci.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 218.Sahin E, Babaï MZ, Dallery Y, Vaillant R. Ensuring supply chain safety through time temperature integrators. Int J Logist Manage. 2007;18:102–24. [Google Scholar]
- 219.DLT Labs, B.S.A.Y.S.C.C.T.A.M.M. 2020. [Retrieved 2020 Nov 15]. Available from: https://medium.com/@dltlabs/blind-spots-along-your-supply-chain-cost-timeand-money-aa891c860628 2020 .
- 220.CDC. Wear Face Masks on Public Transportation Conveyances and at Transportation Hubs. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/travelers/face-masks-public-transportation.html .
- 221.CDC. Interim Infection Prevention and Control Recommendations for Healthcare Personnel during the Coronavirus Disease 2019 (COVID-19) Pandemic. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html .
- 222.Freedman DO, Wilder-Smith A. In-flight transmission of SARS-CoV-2: A review of the attack rates and available data on the efficacy of face masks. J Travel Med. 2020;9:taaa178. doi: 10.1093/jtm/taaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Hardingham-Gill T. The Odds of Catching Covid-19 on an Airplane are Slimmer than you Think, Scientists Say. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.cnn.com/travel/article/odds-catching-covid-19-flight-wellnessscn/index.html .
- 224.Hu M, Lin H, Wang J, Xu C, Tatem AJ, Meng B, et al. The risk of COVID-19 transmission in train passengers: An epidemiological and modelling study. Clin Infect Dis. 2020;7:1. doi: 10.1093/cid/ciaa1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Baskar P. Coronavirus FAQ: Is It Safe to Get on The Bus (Or Subway)? 2020. [Retrieved 2020 Nov 15]. Available from: https://www.npr.org/sections/goatsandsoda/2020/08/28/907106441/coronavirus-faq-is-it-safe-to-get-on-the-bus-or-subway .
- 226.Rettner R. What's the Risk of Catching COVID-19 on Public Transportation? 2020. [Retrieved 2020 Nov 15]. Available from: https://www.livescience.com/covid19-risk-train.html .
- 227.McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat Med. 2020;26:640–2. doi: 10.1038/s41591-020-0863-y. [DOI] [PubMed] [Google Scholar]
- 228.Papadimos TJ. COVID-19 in Greece: People take precedence over economics. J Glob Health. 2020;10:20337. doi: 10.7189/jogh.10.020337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Papadimos TJ, Marcolini EG, Hadian M, Hardart GE, Ward N, Levy MM, et al. Ethics of outbreaks position statement. Part 1: Therapies, treatment limitations, and duty to treat. Crit Care Med. 2018;46:1842–55. doi: 10.1097/CCM.0000000000003416. [DOI] [PubMed] [Google Scholar]
- 230.Rhodes RS, Telford GL, Hierholzer WJ, Jr, Barnes M. Bloodborne pathogen transmission from healthcare worker to patients. Legal issues and provider perspectives. Surg Clin North Am. 1995;75:1205–17. doi: 10.1016/s0039-6109(16)46792-7. [DOI] [PubMed] [Google Scholar]
- 231.Muller-Nix C, Forcada-Guex M, Pierrehumbert B, Jaunin L, Borghini A, Ansermet F. Prematurity, maternal stress and mother Child interactions. Early Hum Dev. 2004;79:145–58. doi: 10.1016/j.earlhumdev.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 232.World Health Organization. Potential Ebola Therapies and Vaccines: Interim Guidance. World Health Organization; 2014 [Google Scholar]
- 233.Singh JA. Humanitarian access to unapproved interventions in public health emergencies of international concern. PLoS Med. 2015;12:e1001793. doi: 10.1371/journal.pmed.1001793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Fingas J. Nasal Spray Might Prevent COVID-19 Infections. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.yahoo.com/finance/news/nasal-spray-prevents-covid-19-infections-204611720.html .
- 235.Dawson AJ. Ebola: What it tells us about medical ethics. J Med Ethics. 2015;41:107–10. doi: 10.1136/medethics-2014-102304. [DOI] [PubMed] [Google Scholar]
- 236.Tai DB, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2020;7:ciaa815. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Abedi V, Olulana O, Avula V, Chaudhary D, Khan A, Shahjouei S, et al. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J Racial Ethn Health Disparities. 2020;9:1–11. doi: 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382:2534–43. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Alobuia WM, Dalva-Baird NP, Forrester JD, Bendavid E, Bhattacharya J, Kebebew E. Racial disparities in knowledge, attitudes and practices related to COVID-19 in the USA. J Public Health (Oxf) 2020;42:470–8. doi: 10.1093/pubmed/fdaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Doede MS. Black jobs matter: Racial inequalities in conditions of employment and subsequent health outcomes. Public Health Nurs. 2016;33:151–8. doi: 10.1111/phn.12241. [DOI] [PubMed] [Google Scholar]
- 241.Meschede T, Taylor J, Mann A, Shapiro TM. Family achievements? How a College Degree Accumulates Wealth for Whites and Not for Blacks. Federal Reserve Bank of St. Louis Review. 2017;99:121–37. [Google Scholar]
- 242.Abatemarco A, Beraldo S, Stroffolini F. Equality of opportunity in health care: Access and equal access revisited. Int Rev Econ. 2020;67:13–29. [Google Scholar]
- 243.Chetty R, Hendren N, Jones MR, Porter SR. Race and economic opportunity in the United States: An intergenerational perspective. Q J Econ. 2020;135:711–83. [Google Scholar]
- 244.Perna LW. Differences in the decision to attend college among African Americans, Hispanics, and Whites. J Higher Educ. 2000;71:117–41. [Google Scholar]
- 245.Bui DP, McCaffrey K, Friedrichs M, LaCross N, Lewis NM, Sage K, et al. Racial and ethnic disparities among COVID-19 cases in workplace outbreaks by industry sector Utah, March 6 June 5, 2020. Morb Mortal Wkly Rep. 2020;69:1133. doi: 10.15585/mmwr.mm6933e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Carethers JM, Sengupta R, Blakey R, Ribas A, D'Souza G. Disparities in cancer prevention in the COVID-19 Era. Cancer Prev Res (Phila) 2020;13:893–6. doi: 10.1158/1940-6207.CAPR-20-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Cox C. Older adults and COVID-19: Social justice, disparities, and social work practice. J Gerontol Soc Work. 2020;16:1–4. doi: 10.1080/01634372.2020.1808141. [DOI] [PubMed] [Google Scholar]
- 248.Papadimos TJ. What's New in Critical Illness and Injury Science? Mental health and COVID-19: Self-inflicted and interpersonal violence amid a pandemic. Int J Crit Illn Inj Sci. 2020;10:45. doi: 10.4103/IJCIIS.IJCIIS_66_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Harvey F. Coronavirus Pandemic Will Cause Famine of Biblical Proportions. The Guardian. 2020;4:21. [Google Scholar]
- 250.Fernandes N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. SSRN. 2020;3:3557504. [Google Scholar]
- 251.Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.McKee M, Reeves A, Clair A, Stuckler D. Living on the edge: Precariousness and why it matters for health. Arch Public Health. 2017;75:13. doi: 10.1186/s13690-017-0183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Long H. U.S. Now has 22 Million Unemployed, Wiping out a Decade of Job Gains. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.washingtonpost.com/business/2020/04/16/unemployment-claims-coronavirus/
- 254.Al Gasseer N, Dresden E, Keeney GB, Warren N. Status of women and infants in complex humanitarian emergencies. J Midwifery Womens Health. 2004;49:7–13. doi: 10.1016/j.jmwh.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 255.Eisner M, Nivette A. Violence and the Pandemic: Urgent Questions for Research. New York: Harry Frank Guggenheim Foundation; 2020. [Google Scholar]
- 256.Taub A. A new COVID-19 crisis: Domestic abuse rises worldwide. N Y Times. 2020;6:6. [Google Scholar]
- 257.Keshavjee S. Blind Spot: How Neoliberalism Infiltrated Global Health. 2014. [Retrieved 2020 Nov 15]. Available from: https://www.researchgate.net/publication/299542604_Blind_Spot_How_Neoliberalism_Infiltrated_Global_Health_by_Salmaan_Keshavjee__2014_288_pp .
- 258.Bhattacharya S. The Blindspot in our Response to COVID-19. 2020 Apr 3; [Google Scholar]
- 259.Zhang L. Blind Spots in fighting the outbreak of Coronavirus Disease. Explor Res Hypothesis Med. 2020;5:6–7. [Google Scholar]
- 260.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: An empirical analysis. Lancet. 2009;374:315–23. doi: 10.1016/S0140-6736(09)61124-7. [DOI] [PubMed] [Google Scholar]
- 261.Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–71. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Mannix R, Lee LK, Fleegler EW. Coronavirus disease 2019 (COVID-19) and firearms in the United States: Will an epidemic of suicide follow? Ann Intern Med. 2020;173:228–9. doi: 10.7326/M20-1678. [DOI] [PubMed] [Google Scholar]
- 263.Marupeng P. Bheki Cele Says Serious Violent Crimes Dropped Since Nationwide Lockdown [SowetanLIVE] Library Catalog. 2020. [Last retrieved on 2020 Apr 27]. Available from: http://www.sowetanlive.co.za .
- 264.Feldman A. Jewish Head of Ohio Health Department Targeted with Protest at her Home, Anti-Semitic Slurs. 2020. [Retrieved 2020 Nov 15]. Available from: https://forward.com/fast-forward/445481/amy-acton-ohio-shutdown-protests-globalist/
- 265.Tony_Blair_Institute_for_Global_Change. Snapshot: How Extremist Groups are Responding to COVID-19 (6 May 2020) 2020. [Retrieved 2020 Nov 15]. Available from: https://institute.global/policy/snapshot-how-extremist-groups-are-responding-covid-19-6-may-2020 .
- 266.Burchill R. Extremism in the Time of COVID-19. Bussola Research Paper. 2020 [Google Scholar]
- 267.Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020;17:4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Vincent A, Mamzer H, Ng Z, Farkas KJ. People and their pets in the times of the COVID-19 pandemic. Soc Regist. 2020;4:111–28. [Google Scholar]
- 269.Steinbuch Y. Russia Races to Develop World'sFirst COVID-19 Vaccine for Cats. 2020. [Retrieved 2020 Nov 15]. Available from: https://nypost.com/2020/08/18/russia-races-to-develop-worlds-first-covid-19-vaccine-for-cats/
- 270.Kumar V, Pruthvishree B, Pande T, Sinha D, Singh B, Dhama K, et al. Malik, SARS-CoV-2 (COVID-19): Zoonotic origin and susceptibility of domestic and wild animals. J Pure Appl Microbiol. 2020;14:741–7. [Google Scholar]
- 271.Gollakner R, Capua I. Is COVID-19 the first pandemic that evolves into a panzootic? Vet Ital. 2020;56:11–2. doi: 10.12834/VetIt.2246.12523.1. [DOI] [PubMed] [Google Scholar]
- 272.Parry NM. COVID-19 and pets: When pandemic meets panic. Forensic Sci Int. 2020;2:100090. doi: 10.1016/j.fsir.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Ali M, Zaid M, Saqib MA, Ahmed H, Afzal MS. SARS-CoV-2 and the hidden carriers Sewage, feline, and blood transfusion. J Med Virol. 2020;92:2291–2. doi: 10.1002/jmv.25956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Kumar R, Harilal S, Al-Sehemi AG, Mathew GE, Carradori S, Mathew B. The chronicle of COVID-19 and possible strategies to curb the pandemic. Curr Med Chem. 2020 doi: 10.2174/0929867327666200702151018. DOI: https://doi.org/10.2174/0929867327666200702151018. [DOI] [PubMed] [Google Scholar]
- 275.Shi J, Wen Z, Zhong G, Yang H, Wang C, Huang B, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2. Science. 2020;368:1016–20. doi: 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Leroy EM, Gouilh MA, Brugère-Picoux J. The risk of SARS-CoV-2 transmission to pets and other wild and domestic animals strongly mandates a one-health strategy to control the COVID-19 pandemic. One Health. 2020;10:100133. doi: 10.1016/j.onehlt.2020.100133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Halfmann PJ, Hatta M, Chiba S, Maemura T, Fan S, Takeda M, et al. Transmission of SARS-CoV-2 in domestic cats. N Engl J Med. 2020;383:592–4. doi: 10.1056/NEJMc2013400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Dhiman N, Sharma M. Fuzzy logic inference system for identification and prevention of Coronavirus (COVID-19) International Journal of Innovative Technology and Exploring Engineering. 2020;9:1575–80. [Google Scholar]
- 279.Opriessnig T, Huang YW. Update on possible animal sources for COVID-19 in humans. Xenotransplantation. 2020;27:e12621. doi: 10.1111/xen.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Kim YI, Kim SG, Kim SM, Kim EH, Park SJ, Yu KM, et al. Infection and rapid transmission of SARS-CoV-2 in ferrets. Cell Host Microbe. 2020;27:704–9.e2. doi: 10.1016/j.chom.2020.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Martina BE, Haagmans BL, Kuiken T, Fouchier RA, Rimmelzwaan GF, Van Amerongen G, et al. SARS virus infection of cats and ferrets. Nature. 2003;425:915. doi: 10.1038/425915a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.McGee L, Cotovio V. Denmark Mink COVID Crisis Worsens. Here’s What it Means. [Last accessed on 2020 Nov 07]. Available from: https://www.cnn.com/2020/11/07/europe/mink-covid-19-denmark-update-intl/index.html .
- 283.WHO. SARS-CoV-2 Mink-Associated Variant Strain – Denmark. [Last accessed on 2020 Nov 07]. Available from: https://www.who.int/csr/don/06-november-2020-mink-associated-sars-cov2-denmark/en/
- 284.Chan FW, Zhang AJ, Yuan S, Poon KM, Chan CS, Lee CY, et al. Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID-19) in golden Syrian hamster model: Implications for disease pathogenesis and transmissibility. Clin Infect Dis. 2020;3:ciaa325. doi: 10.1093/cid/ciaa325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Kaptein SJ, Jacobs S, Langendries L, Seldeslachts L, ter Horst S, Liesenborghs L, et al. Antiviral treatment of SARS-CoV-2-infected hamsters reveals a weak effect of favipiravir and a complete lack of effect for hydroxychloroquine. BioRxiv. 2020;1:1. [Google Scholar]
- 286.Yen H, Sia SF, Yan L, Chin AW, Fung K, Poon LL, et al. Pathogenesis and transmission of SARS-CoV-2 virus in golden Syrian hamsters. Nature. 2020;583:834–8. doi: 10.1038/s41586-020-2342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Attride T. 10 of the Most Popular pets in the US that Aren't Cats or Dogs. 2018. [Retrieved 2020 Nov 15]. Available from: https://www.insider.com/most-popular-pets-in-the-us-2018-7 .
- 288.McKenna S. Human Viruses Can Jump into Animals, Too Sowing the Seeds of Future Epidemics. 2020. [Retrieved 2020 Nov 15]. Available from: https://www.scientificamerican.com/article/human-viruses-can-jump-into-animals-too-sowing-the-seeds-of-future-epidemics/
- 289.Wang LF, Shi Z, Zhang S, Field H, Daszak P, Eaton BT. Review of bats and SARS. Emerg Infect Dis. 2006;12:1834–40. doi: 10.3201/eid1212.060401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Xu J, Zhao S, Teng T, Abdalla AE, Zhu W, Xie L, et al. systematic comparison of two animal-to-human transmitted human coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses. 2020;12:244. doi: 10.3390/v12020244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Schlottau K, Rissmann M, Graaf A, Schön J, Sehl J, Wylezich C, et al. SARS-CoV-2 in fruit bats, ferrets, pigs, and chickens: An experimental transmission study. Lancet Microbe. 2020;1:e218–25. doi: 10.1016/S2666-5247(20)30089-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Maxmen A. Coronavirus is spreading under the radar in US homeless shelters. Nature. 2020;581:129. doi: 10.1038/d41586-020-01389-3. [DOI] [PubMed] [Google Scholar]
- 293.Mosites E, Parker EM, Clarke KE, Gaeta JM, Baggett TP, Imbert E, et al. Assessment of SARS-CoV-2 infection prevalence in homeless shelters Four US cities, March 27 April 15, 2020. Morb Mortal Wkly Rep. 2020;69:521–2. doi: 10.15585/mmwr.mm6917e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Perri M, Dosani N, Hwang SW. COVID-19 and people experiencing homelessness: Challenges and mitigation strategies. CMAJ. 2020;192:E716–9. doi: 10.1503/cmaj.200834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Mehdipanah R. Housing as a determinant of COVID-19 inequities. Am J Public Health. 2020;110:1369–70. doi: 10.2105/AJPH.2020.305845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Krieger J, Higgins DL. Housing and health: Time again for public health action. American J Public Health. 2002;92:758–68. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Hernández D, Swope CB. Housing as a platform for health and equity: Evidence and future directions. Am J Public Health. 2019;109:1363–6. doi: 10.2105/AJPH.2019.305210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Coughlin CG, Sandel M, Stewart AM. Homelessness, children, and COVID-19: A looming crisis. Pediatrics. 2020;146:e20201408. doi: 10.1542/peds.2020-1408. [DOI] [PubMed] [Google Scholar]
- 299.Homelessness, U.I.C.O., Homelessness in America: Focus on Families with Children. Washington, DC: US Interagency Council on Homelessness; 2018. [Google Scholar]
- 300.Beharry MS, Christensen R. Homelessness in pediatric populations: Strategies for prevention, assistance, and advocacy. Pediatr Clin. 2020;67:357–72. doi: 10.1016/j.pcl.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 301.Tucker JS, D'Amico EJ, Pedersen ER, Garvay R, Rodriguez A, Klein DJ. Behavioral health and service usage during the COVID-19 pandemic among emerging adults currently or recently experiencing homelessness. J Adolesc Health. 2020;67:603–5. doi: 10.1016/j.jadohealth.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Auerswald CL, Adams S, Lightfoot M. The urgent and growing needs of youths experiencing homelessness during the COVID-19 pandemic. J Adolesc Health. 2020;67:461–2. doi: 10.1016/j.jadohealth.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Vasylyeva TI, Smyrnov P, Strathdee S, Friedman SR. Challenges posed by COVID-19 to people who inject drugs and lessons from other outbreaks. J Int AIDS Soc. 2020;23:e25583. doi: 10.1002/jia2.25583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Mackey TK, Strathdee SA. Big events and risks to global substance using populations: Unique threats and common challenges. Subst Use Misuse. 2015;50:885–90. doi: 10.3109/10826084.2015.983008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Schiff R, Buccieri K, Schiff JW, Kauppi C, Riva M. COVID-19 and pandemic planning in the context of rural and remote homelessness. Can J Public Health. 2020;9:1–4. doi: 10.17269/s41997-020-00415-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Schiff JW, Pauly B, Schiff R. Needs and Analysis of Pandemic Planning in Four Canadian Cities. Lessons from H1N1 in Canada. Toronto: Canadian Observatory on Homelessness; 2016. p. 163. [Google Scholar]
- 307.Frankish CJ, Hwang SW, Quantz D. Homelessness and health in Canada: Research lessons and priorities. Can J Public Health. 2005;96(Suppl 2):S23–9. doi: 10.1007/BF03403700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Karb R, Samuels E, Vanjani R, Trimbur C, Napoli A. Homeless shelter characteristics and prevalence of SARS-CoV-2. West J Emerg Med. 2020;21:1048–53. doi: 10.5811/westjem.2020.7.48725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.World Health Organization. WHO recommends against the use of remdesivir in COVID-19 patients. 2020. [Retrieved 2020 Nov 24]. Available from: https://www.who.int/news-room/feature-stories/detail/who-recommends-against-the-use-of-remdesivir-in-covid-19-patients .


