ABSTRACT
During 2016 to 2019, cholera outbreaks were reported commonly to the Ministry of Health from refugee settlements. To further understand the risks cholera posed to refugees, a review of surveillance data on cholera in Uganda for the period 2016–2019 was carried out. During this 4-year period, there were seven such outbreaks with 1,495 cases and 30 deaths in five refugee settlements and one refugee reception center. Most deaths occurred early in the outbreak, often in the settlements or before arrival at a treatment center rather than after arrival at a treatment center. During the different years, these outbreaks occurred during different times of the year but simultaneously in settlements that were geographically separated and affected all ages and genders. Some outbreaks spread to the local populations within Uganda. Cholera control prevention measures are currently being implemented; however, additional measures are needed to reduce the risk of cholera among refugees including oral cholera vaccination and a water, sanitation and hygiene package during the refugee registration process. A standardized protocol is needed to quickly conduct case–control studies to generate information to guide future cholera outbreak prevention in refugees and the host population.
INTRODUCTION
Cholera is a major global public health issue leading to many deaths annually.1 Cholera is a diarrheal disease caused by a bacterium, Vibrio cholerae, with an incubation period from 1 to 5 days.2 Many infected persons are asymptomatic but can transmit infection to communities with inadequate safe water, sanitation and hygiene (WaSH). Cholera outbreaks can be prevented with improved WaSH, but this is often lacking in developing countries. Oral cholera vaccine is also effective as a preventive measure to complement WaSH strategies.3
Cholera is one of several infections that are reported through the Integrated Disease Surveillance and Response (IDSR) system to the Ministry of Health. Other infections reported through this system include cerebrospinal meningitis, dengue fever, influenza, poliomyelitis, yellow fever, typhoid, hemorrhagic fevers, and other priority public health conditions.4 Refugees constitute a group of people at high risk of diseases and those dying from infectious diseases such as cholera5–8 and other diseases in general.9
During the last 50 years, a large proportion of the reported cholera cases have occurred in sub-Saharan Africa.1,10,11 Devastating cholera outbreaks have occurred in several countries, including Yemen in association with civil war,12–14 Haiti following an earthquake,15,16 and Tanzania with an influx of refugees from Burundi,8 and many other sub-Saharan countries such as Zimbabwe,17 Zambia,18,19 Tanzania,20 the Democratic Republic of the Congo (DRC),21,22 and Nigeria.23
Across these cholera outbreaks, the disease has been especially devastating for refugee settlements or during massive movements of displaced persons. There are 25.9 million refugees around the world, with 85% of them hosted in low- and middle-income countries.24 The number of refugees is increasing amid the host countries’ own economic and developmental challenges. For the purpose of this study, refugee settlements are defined as places in a foreign land that are inhabited by refugees. Article 1(A)(2) of the 1951 Refugee Convention defines a refugee as “someone who has been forced to flee his or her country because of persecution, war, or violence.” A refugee has a well-founded fear of persecution for reasons of race, religion, nationality, political opinion, or membership in a particular social group. Most likely, they cannot return home or are afraid to do so.25 War and ethnic, tribal, and religious violence are leading causes of refugees fleeing their countries. The refugees are traumatized by the pressures that pushed them from their original places of residence and now find themselves at risk of cholera. Notable examples of cholera outbreaks among refugees have occurred during the migration of Rwandese refugees in the DRC26,27 and, more recently, among Burundi refugees in Tanzania8,28 and Somali refugees in Kenya.29,30 Notably, there was no outbreak following the influx of refugees from Myanmar into Bangladesh when oral cholera vaccine was provided quickly to these refugees.31
One of the countries with many refugees is Uganda, which hosts more than 1.33 million people from neighboring countries: the DRC, South Sudan, Burundi, and Eritrea. Unlike some other countries where refugees are kept in defined locations separated from the local populations, Uganda has a unique legal framework of local integration in which basic services are provided initially, but the refugees are given small parcels of land on which they can grow crops; thus, the settlements in Uganda are a type of hybrid between a “camp” and a village.32 The number of refugees has increased tremendously in the last few years, which has constrained social service delivery.32 During the period 2016–2019, several cholera outbreaks occurred among the refugee settlements in Uganda.
In Uganda, the identified hot spots for cholera outbreaks were mostly in districts along the international border and in communities residing near the major water bodies.33–35 During previous cholera outbreaks, fishing communities were the most affected group and comprised 58% of all affected persons in the period 2011–2016.34
Following studies of cholera in Uganda during the previous decade, the government of Uganda developed a comprehensive 5-year plan for cholera prevention and control for 2017–202236 to guide cholera activities and align with the Global Roadmap for Cholera Elimination. In 2017, the Global Task Force for Cholera Control (GTFCC) launched a road map to eliminate cholera by 2030, targeting selected countries, including Uganda.37 Given documented cholera outbreaks among refugees in Uganda, strategies for prevention, control, and elimination of cholera should be comprehensive and integrated in all aspects including prevention of outbreaks among refugees. The aim of this study was to describe the cholera outbreaks that were reported in refugee settlements in Uganda during the period 2016–2019 and to propose recommendations for future prevention and control of cholera among the refugees.
METHODS AND MATERIALS
Study setting.
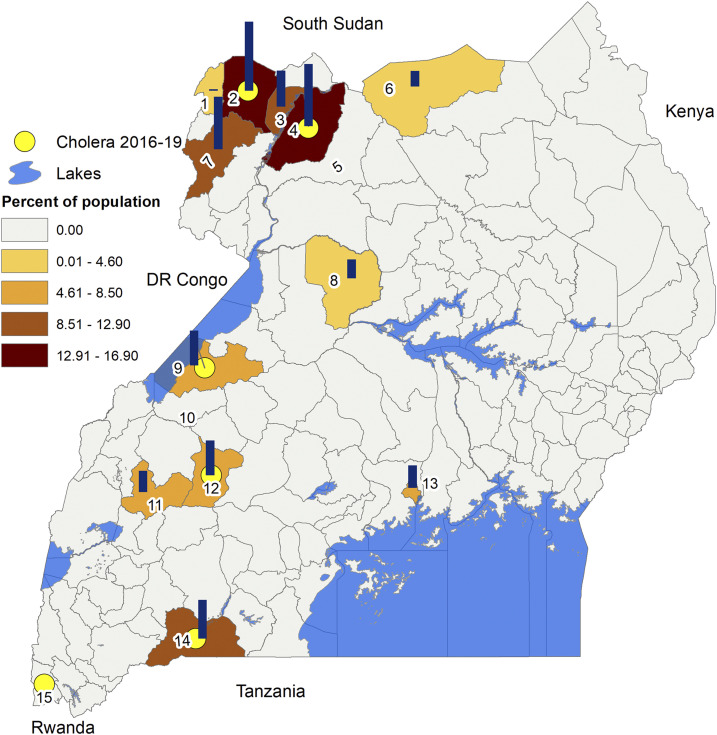
This cross-sectional study was conducted using quantitative data collected by the Uganda Ministry of Health on cholera outbreaks that occurred in the refugee settlements and surrounding districts from 2016 to 2019. The refugee settlements were prioritized because Uganda Ministry of Health weekly epidemiological surveillance reports showed that most cholera outbreaks were occurring in districts with refugees. As of December 31, 2019, Uganda had a reported population of 1,381,122 refugees and asylum seekers. The refugees and asylum seekers in Uganda were located in 12 districts as is shown in Figure 1.38
Figure 1.
Map of Uganda showing distribution of refugee settlements in 2019. Bar: Refugee population in district as % of all refugees in Uganda. Color: Refugee population in district as % of the total population in districts. Circle: Districts with cholera cases among refugees. The identification of the districts are 1) Koboko, 2) Yumbe, 3) Obongi, 4) Adjumani, 5) Amaru, 6) Lamwo, 7) Arua, 8) Kiryandongo, 9) Kikuubi, 10) Kibaale, 11) Kamwenge, 12) Kyegegwa, 13) Kampala, 14) Isingiro, and 13) Kisoro (Nyakabande Reception Centre).
Data collection, analysis, and interpretation.
Districts in Uganda report cholera cases on a weekly basis through the IDSR system. Cholera cases and deaths are recorded on a line list that is transmitted to the Ministry of Health, Kampala. The line lists include information on the date of illness, age and gender, places of residence, nationality status (refugee or Ugandan), presenting symptoms and signs, treatment administered, and status of patients (improved, discharged, referred, or died). These weekly reports are submitted consistently because cholera is one of the notifiable diseases on the WHO IDSR priority list. To better understand the cholera outbreaks in the refugee settlements and their potential for spread to the host population, we reviewed the Uganda Ministry of Health cholera outbreak weekly surveillance data for the period 2016–2019 from refugee settlements and the surrounding districts. Attack rates, incidence, and case fatality proportion were calculated using denominator populations obtained from the United Nations High Commissioner for Refugees (UNHCR) and the Uganda Bureau of Statistics for refugee and local populations, respectively. All analyses were completed in Excel. The shapefiles used to generate the maps were obtained from Humanitarian Data Exchange (https://data.humdata.org/), which is shared under Creative Common Attributions International (CC by License), and the maps were drawn using ArcGIS Desktop 10.7 (ESRI Inc., Redlands, CA).
Ethical consideration.
We used anonymous personal data or aggregated data as appropriate to ensure confidentiality and ethical standards at all stages of data handling. This study reviewed data that are part of routine surveillance activity. It is intended to assist with public health control of cholera by the Ministry of Health and is IRB exempted.
RESULTS
Reported cholera outbreaks in refugee settlements.
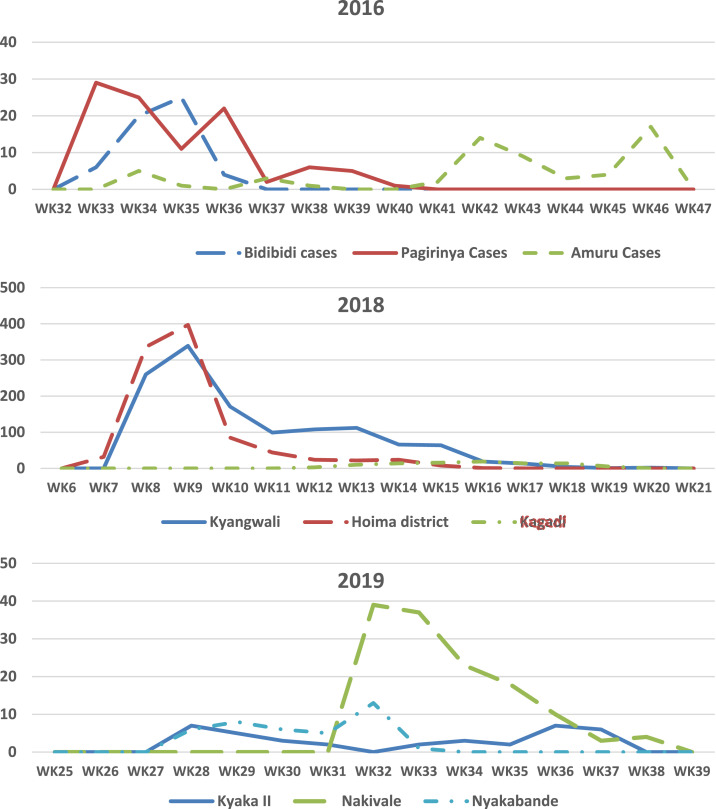
During the period 2016–2019, seven cholera outbreaks were reported from five of the refugee settlements and one reception center. Except for 2017, when there were no reported outbreaks in the refugee settlements, two settlements reported cholera outbreaks each year during this period. The outbreaks occurred at different times of the year (Figure 2); however, they occurred almost simultaneously in locations that were distant from each other but were receiving (settling) new refugees arriving from a common reception center. In 2019, there were three cholera outbreaks. These outbreaks were in Kyaka II and Nakivale refugee settlements and the Nyakabande Reception Centre.
Figure 2.
Weekly reported cholera cases among refugees in Uganda in 2016, 2018, and 2019.
Based on a review of the Ministry of Health’s Situation Reports (Sitreps) and from press reports,39 the outbreaks appeared to start with arrival of new refugees into Uganda related to civil conflicts in neighboring areas of the DRC and many of the cases occurred among the newly arrived refugees.40 The information in the reports on the onset of the outbreaks were supported by data from the line lists analyzed during this study which showed that the index cases and majority of cases at the beginning of the outbreaks were new refugees who developed symptoms before arrival to the reception centers.
Each of the outbreaks were confirmed with positive cultures, but once confirmed, most of the additional cases were reported based on clinical symptoms and signs, as recommended by the GTFCC. A total of 1,495 cholera cases and 30 deaths were reported across the seven cholera outbreaks in the refugee settlements. Kyangwali refugee settlement (Kikuube district [formerly Hoima district]) reported the highest number of cases, the highest attack rate, and the highest case fatality proportion (2.6%). Kyaka II refugee settlement had two cholera outbreaks in two consecutive years (2018 and 2019). Both Inaba and Ogawa serotypes were observed across these outbreaks, but within each specific outbreak, only one serotype was observed. All isolates tested across all outbreaks were sensitive to tetracycline and ciprofloxacin and resistant to trimethoprim/sulfamethoxazole.
The reported number of cases and deaths for each of the five refugee settlements and the one reception center is shown in Table 1. Of the 28 deaths in Kyangwali, 19 occurred during the first week, and 13 of these occurred in the settlement and not at a health center. Four additional deaths occurred in the second week, including three in the settlement. Thus, most deaths occurred very early in the outbreak and in the settlement.
Table 1.
Reported cholera cases and deaths in the refugee settlements in Uganda for the period 2016–2019
| Name of the refugee settlement | District name | Year | Cases | Deaths | CFR (%) | Refugee population | AR (%) |
|---|---|---|---|---|---|---|---|
| Bidibidi | Yumbe | 2016 | 55 | 0 | 0.00 | 227,909 | 0.02 |
| Pagirinya | Adjumani | 2016 | 101 | 0 | 0.00 | 204,987 | 0.05 |
| Kyangwali | Kikube (Hoima) | 2018 | 997 | 28 | 2.81 | 43,600 | 2.29 |
| Kyaka II | Kyegegwa | 2018 | 132 | 1 | 0.76 | 79,842 | 0.17 |
| Kyaka II | Kyegegwa | 2019 | 37 | 0 | 0.00 | 101,050 | 0.04 |
| Nakivale | Isingiro | 2019 | 134 | 1 | 0.75 | 117,894 | 0.11 |
| Nyakabande Reception Centre | Kisoro | 2019 | 39 | 0 | 0.00 | – | – |
| Total | – | – | 1,495 | 30 | 2.01 | – | – |
CFR = case fatality ratio; AR = attack rate.
The weekly reported cases in the five refugee settlements and one reception center are shown in Figure 2. The outbreaks occurred late in the year in 2016, whereas in 2018, they occurred early in the year, and in 2019, they occurred midyear. The figures also reflect outbreaks in Kagadi and Amuru districts. Although these two districts do not host refugees, they share an administrative border with districts that do. The temporal distribution of cholera cases across neighboring districts highlight the elevated risk of cross-district spread of infection associated with the strong community connectivity.
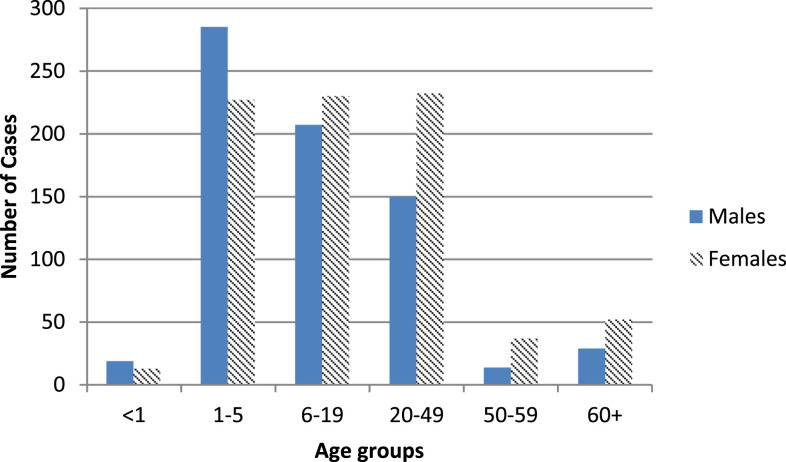
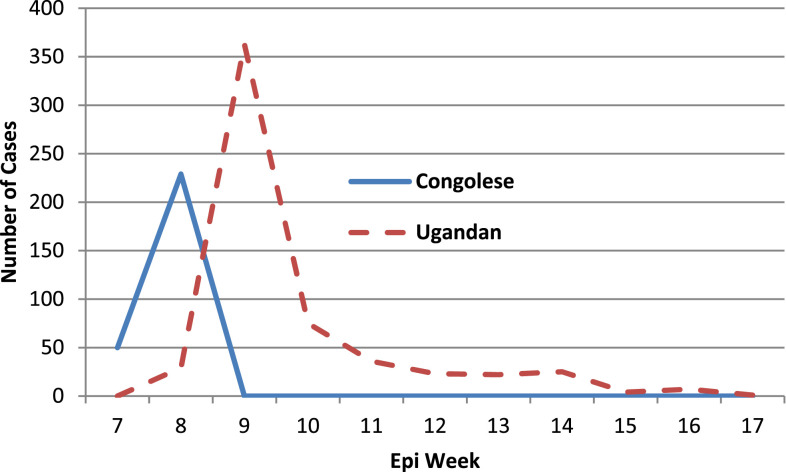
During these outbreaks, all ages and genders of the communities in the resettlements were affected. The age and gender distribution of the cases is shown in Figure 3 and appeared to be consistent across the different outbreaks. Relatively more males than females were affected in the age-group < 6 years. By contrast, in the age-group 20–49 years, more females than males were affected. Although this study focused on refugees themselves, the outbreak in Hoima appeared to start among the refugees and then spread to the local population as well, as shown in Figure 4. The reported cholera cases among refugee and general population is shown in Table 2.
Figure 3.
Age (year) and gender distribution of cholera cases among refugees in Uganda, 2016–2019.
Figure 4.
Cases of cholera among refugee and Ugandan residents in Hoima during outbreak in 2018.
Table 2.
Cholera cases and deaths in the general population vs. refugee population by year, 2016–2019
| Year | Number of districts reporting cholera | Number of districts with refugees reporting cholera outbreaks (names) | Reported cholera cases (deaths) | Reported cholera cases (deaths) among refugees |
|---|---|---|---|---|
| 2016 | 25 | 2 (Yumbe, Adjumani) | 2,316 (64) | 156 (0) |
| 2017 | 3 | 1 (Kisoro) | 265 (5) | 1 (0) |
| 2018 | 11 | 2 (Hoima, Kyegegwa) | 2,754 (59) | 1,129 (29) |
| 2019 | 6 | 3 (Kisoro, Kyegegwa, Isingiro) | 326 (5) | 210 (1) |
DISCUSSION
This review of the cholera outbreaks among refugee settlements demonstrates that cholera is a significant risk among refugees arriving in Uganda. People at highest risk include new refugee arrivals, refugees already living in the settlements, and the host population which lives nearby. In recent years, the number of cholera cases reported nationally in Uganda had been declining; however, during the period 2016–2019, new communities started to dominate the weekly reports. Notably, cholera outbreaks occurring in refugee settlements may slow or reverse the decline in the overall cholera rates in Uganda.
Cholera outbreaks affected all age-groups and both genders and had the potential to spread to the host communities. These outbreaks tended to spread very quickly but lasted only a few weeks. The highest risk of death occurred during the first 2 weeks. Most deaths occurred in the settlement, with very few deaths occurring after arrival at the health facility. The case fatality ratios for patients treated at the health facility were considerably less than 1%, suggesting that medical care was adequate at the health facilities. However, additional efforts are needed to manage severe cases in the community or immediately transport them to the health facility. Also, because cholera deaths are relatively unusual, additional information should be gathered on every cholera death to identify the social and medical barriers that contributed to the deaths.
These outbreaks occurred simultaneously in at least two resettlement centers, and for each of the six outbreaks reported in this study, the epidemics started with arrival of new refugees to the settlements. Cross-border spread between Uganda and neighboring countries is now widely recognized for cholera.41,42 Clearly, refugees are not the only mechanism for such transmission; however, this group is very vulnerable because of the socioeconomic situation and the WaSH conditions in the communities from which they come. Because most of these refugees to Uganda were from the DRC, with some from South Sudan, they were from areas where cholera was endemic and thus were at higher risk. The spread of cholera to the local communities from the refugee settlements has the potential to increase the need for health services in both the settlements and surrounding communities.32 Although a recent review of cholera among refugees concluded that the global cholera problem appeared to be declining,43 this was not the case in Uganda.
This study suggests that additional measures are needed to reduce cholera among refugees. Currently, refugees arrive at a resettlement center where they reside for one day to more than a week until there is space identified at a refugee settlement. At the resettlement center or in the refugee settlement, refugees typically receive both food assistance and nonfood items. In Uganda, the nonfood items are known as a “Non-Food Item (NFI) kit.” The kit includes a bar of soap, a jerrican and basin, and minimal clothes and supplies for women and supplies for a makeshift shelter. Some kit components are one-off items, but others are replenished at regular intervals.
Within the refugee settlements, the Office of the Prime Minister and UNHCR lead all refugee activities in Uganda with additional support from UNICEF, the WHO, the World Food Program, the Lutheran World Federation, Uganda Red Cross, Medicine Sans Frontiers, International Medical Corps, the International Rescue Committee, Oxfam, CARE, and others. Ideally, the guiding principle in the provision of these social services is to meet Sphere Humanitarian Standards.44 In addition to these basic services, additional interventions would seem to be needed to prevent these cholera outbreaks.
A potential intervention to minimize the risk of cholera spread in Uganda may be to support arriving refugees for a longer period at the refugee resettlement center to provide a “cholera prevention package.” This package would include oral cholera vaccination and WaSH promotion supplies with Information, Education, Communication materials; water treatment tablets appropriate for the water containers issued; and supplies to prepare soapy water for handwashing for at least a month as the refugees adapt to their new environment. Providing services at the reception center for 2–3 weeks would allow time to give two doses of oral cholera vaccine and to orient them to improved WaSH standards while monitoring them for cholera symptoms. The additional time and orientation at the resettlement center would require some additional organization and resources at the centers but may be cost-effective by preventing the need to respond to outbreaks in the settlements.
This study has several limitations. In 2018, a small cholera outbreak occurred in Kampala city in informal settlements where refugees also reside. However, obtaining complete reports from this area was not possible because of stigma, and this information was not included in this analysis. Second, the population of refugees is mobile and the denominators are not constant, limiting the accuracy of the attack rates. Although the number of cholera cases is relatively small compared to the 1.3 million refugees in Uganda, we did not have the number of newly arrived refugees for each of these outbreaks to clearly identify the risks for this subgroup of newly arrived refugees. Third, careful case–control studies from each outbreak may have identified specific risk factors associated with each outbreak and might have identified specific geographic areas from which the refugees came. A predefined protocol for such case–control studies should be developed so that consistent data can be collected if future outbreaks occur. Finally, comparing the molecular characteristics of the strains in Uganda with strains in the geographic areas from which the refugees came would strengthen the conclusion of cross-border transmission. A strength of the study was the use of cleaned Ministry of Health data on cholera outbreaks; thus, the data are as valid as is possible in this situation.
CONCLUSION
This study illustrates the importance of mitigating the risk of cholera outbreaks in refugee settlements in Uganda. Apart from causing disease among the newly arriving refugees, infected refugees may also spread the infection to others in the refugee settlements as well as in neighboring communities. Although cholera rates decreased nationally during the period under review, it increased among the refugees. Therefore, for Uganda to achieve the WHO cholera elimination targets by 2030, special efforts are needed to prevent cholera among newly arriving refugees, especially among those from countries with cholera. A cholera prevention intervention could include oral cholera vaccination and a WaSH package during the refugee registration process. A predefined protocol is needed to quickly carry out case–control studies to generate information to prevent future outbreaks from occurring in refugee settlements. Furthermore, additional studies are needed to document the molecular characteristics of the V. cholerae organisms responsible for the outbreaks in these settlements in relation to the strains from neighboring countries.
ACKNOWLEDGMENTS
We extend our special thanks to the research assistants who dedicated their time to meticulously collect the data for this study through the IDSR system. We thank the Ministry of Health leadership for guidance and for permission to access data on the refugee population.
REFERENCES
- 1.Ali M, Nelson AR, Lopez AL, Sack DA, 2015. Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis 9: e0003832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Azman AS, Rudolph KE, Cummings DA, Lessler J, 2013. The incubation period of cholera: a systematic review. J Infect 66: 432–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bi Q, et al. Oral Cholera Vaccine Working Group of The Global Task Force on Cholera Control , 2017. Protection against cholera from killed whole-cell oral cholera vaccines: a systematic review and meta-analysis. Lancet Infect Dis 17: 1080–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Masiira B, et al. 2019. Evaluation of integrated disease surveillance and response (IDSR) core and support functions after the revitalisation of IDSR in Uganda from 2012 to 2016. BMC Public Health 19: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Djeddah C, Miozzo A, Di Gennaro M, Rosmini F, Martino P, Pasquini P, 1988. An outbreak of cholera in a refugee camp in Africa. Eur J Epidemiol 4: 227–230. [DOI] [PubMed] [Google Scholar]
- 6.Siddique AK, 1995. Failure of treatment centres to prevent cholera deaths in Goma. Lancet 346: 379. [DOI] [PubMed] [Google Scholar]
- 7.Hatch DL, Waldman RJ, Lungu GW, Piri C, 1994. Epidemic cholera during refugee resettlement in Malawi. Int J Epidemiol 23: 1292–1299. [DOI] [PubMed] [Google Scholar]
- 8.MSF , 2015. Cholera Outbreak Among Burundian Refugees. Available at: https://www.msf.org/tanzania-cholera-outbreak-among-burundian-refugees. Accessed September 8, 2019. [Google Scholar]
- 9.Polonsky JA, Ronsse A, Ciglenecki I, Rull M, Porten K, 2013. High levels of mortality, malnutrition, and measles, among recently-displaced Somali refugees in Dagahaley camp, Dadaab refugee camp complex, Kenya, 2011. Confl Health 7: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weill FX, et al. 2017. Genomic history of the seventh pandemic of cholera in Africa. Science 358: 785–789. [DOI] [PubMed] [Google Scholar]
- 11.Lessler J, et al. 2018. Mapping the burden of cholera in sub-Saharan Africa and implications for control: an analysis of data across geographical scales. Lancet 391: 1908–1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Camacho A, et al. 2018. Cholera epidemic in Yemen, 2016–18: an analysis of surveillance data. Lancet Glob Health 6: e680–e690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qadri F, Islam T, Clemens JD, 2017. Cholera in Yemen - an old foe rearing its ugly head. N Engl J Med 377: 2005–2007. [DOI] [PubMed] [Google Scholar]
- 14.von Seidlein L, Sack D, Azman AS, Ivers LC, Lopez AL, Deen JL, 2017. Cholera outbreak in Yemen. Lancet Gastroenterol Hepatol 2: 777. [DOI] [PubMed] [Google Scholar]
- 15.Farmer P, et al. 2011. Meeting cholera’s challenge to Haiti and the world: a joint statement on cholera prevention and care. PLoS Negl Trop Dis 5: e1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barzilay EJ, Schaad N, Magloire R, Mung KS, Boncy J, Dahourou GA, Mintz ED, Steenland MW, Vertefeuille JF, Tappero JW, 2013. Cholera surveillance during the Haiti epidemic--the first 2 years. N Engl J Med 368: 599–609. [DOI] [PubMed] [Google Scholar]
- 17.Makoni M, 2018. Inside Zimbabwe’s efforts to tame cholera. Lancet 392: e8. [DOI] [PubMed] [Google Scholar]
- 18.Sinyange N, et al. 2018. Cholera epidemic-Lusaka, Zambia, October 2017–May 2018. MMWR Morb Mortal Wkly Rep 67: 556–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poncin M, et al. 2018. Implementation research: reactive mass vaccination with single-dose oral cholera vaccine, Zambia. Bull World Health Organ 96: 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Narra R, et al. 2017. Notes from the field: ongoing cholera epidemic-Tanzania, 2015–2016. MMWR Morb Mortal Wkly Rep 66: 177–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ingelbeen B, et al. 2019. Recurrent cholera outbreaks, Democratic Republic of the Congo, 2008–2017. Emerg Infect Dis 25: 856–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azman AS, et al. 2018. Micro-hotspots of risk in urban cholera epidemics. J Infect Dis 218: 1164–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elimian KO, et al. 2019. Descriptive epidemiology of cholera outbreak in Nigeria, January–November, 2018: implications for the global roadmap strategy. BMC Public Health 19: 1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.UNHCR , 2019. Figures at a Glance. Statistical Yearbook. Available at: https://www.unhcr.org/en-us/publications/legal/58359afe7/unhcr-guidelines-international-protection-12-claims-refugee-status-related.html. Accessed December 27, 2019. [Google Scholar]
- 25.UNHCR , 2016. Guidelines on International Protection No. 12: Claims for Refugee Status Related to Situations of Armed Conflict and Violence under Article 1A(2) of the 1951 Convention and/or 1967 Protocol Relating to the Status of Refugees and the Regional Refugee Definition. Geneva, Switzerland: UNHCR. [Google Scholar]
- 26.Siddique AK, 1994. Cholera epidemic among Rwandan refugees: experience of ICDDR,B in Goma, Zaire. Glimpse 16: 3–4. [PubMed] [Google Scholar]
- 27.CDC , 1998. Cholera outbreak among Rwandan refugees--Democratic Republic of Congo, April 1997. MMWR Morb Mortal Wkly Rep 47: 389–391. [PubMed] [Google Scholar]
- 28.UNHCR , 2015. Cholera Epidemic Among Refugee and Host Communities in Tanzania Claims 31 Lives, Situation Worsening. Available at: https://www.unhcr.org/en-us/news/briefing/2015/5/555f12089/cholera-epidemic-among-refugee-host-communities-tanzania-claims-31-lives.html. Accessed December 27, 2019. [Google Scholar]
- 29.Golicha Q, et al. 2018. Cholera outbreak in Dadaab refugee camp, Kenya-November 2015–June 2016. MMWR Morb Mortal Wkly Rep 67: 958–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahamud AS, et al. 2012. Epidemic cholera in Kakuma refugee Camp, Kenya, 2009: the importance of sanitation and soap. J Infect Dev Ctries 6: 234–241. [DOI] [PubMed] [Google Scholar]
- 31.Qadri F, Azad AK, Flora MS, Khan AI, Islam MT, Nair GB, Singh PK, Clemens JD, 2018. Emergency deployment of oral cholera vaccine for the Rohingya in Bangladesh. Lancet 391: 1877–1879. [DOI] [PubMed] [Google Scholar]
- 32.Kreibaum K, 2016. Their suffering, our burden? How Congolese refugees affect the Ugandan population. World Dev 78: 262–287. [Google Scholar]
- 33.Bwire G, Ali M, Sack DA, Nakinsige A, Naigaga M, Debes AK, Ngwa MC, Brooks WA, Garimoi Orach C, 2017. Identifying cholera “hotspots” in Uganda: an analysis of cholera surveillance data from 2011 to 2016. PLoS Negl Trop Dis 11: e0006118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bwire G, et al. 2017. Epidemiology of cholera outbreaks and socio-economic characteristics of the communities in the fishing villages of Uganda: 2011–2015. PLoS Negl Trop Dis 11: e0005407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kwesiga B, Pande G, Ario AR, Tumwesigye NM, Matovu JKB, Zhu BP, 2017. A prolonged, community-wide cholera outbreak associated with drinking water contaminated by sewage in Kasese District, western Uganda. BMC Public Health 18: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Uganda Sau Oficial Republica , 2017. National Integrated Comprehensive Cholera Prevention and Control Plan, Fiscal Years (2017/18–2021/22). Available at: https://ifrcwatsanmissionassistant.files.wordpress.com/2018/10/uganda-mhealth-national-cholera-plan.pdf. Accessed August 19, 2020. [Google Scholar]
- 37.Legros D; Partners of the Global Task Force on Cholera Control , 2018. Global cholera epidemiology: opportunities to reduce the burden of cholera by 2030. J Infect Dis 218 (Suppl 3): S137–S140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.UNHCR , 2019. Refugees and Asylum-Seekers in Uganda. Available at: https://data2.unhcr.org/en/documents/download/73196. Accessed June 20, 2020. [Google Scholar]
- 39.Xinhua , 2018. 9 refugees die in Uganda cholera break. Xinhua. Available at: http://www.xinhuanet.com/english/2018-02/22/c_136991380.htm. Accessed April 8, 2020. [Google Scholar]
- 40.Reliefweb , 2017. 3500 Congolese Refugees Moved to Kwangali Settlement Camp. Available at: https://reliefweb.int/report/uganda/3500-congolese-refugees-moved-kwangali-settlement-camp. Accessed June 20, 2020. [Google Scholar]
- 41.Bwire G, Mwesawina M, Baluku Y, Kanyanda SS, Orach CG, 2016. Cross-border cholera outbreaks in sub-Saharan Africa, the mystery behind the silent illness: what needs to be done? PLoS One 11: e0156674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.WHO , 2011. Cholera: Mechanism for Control and Prevention: The Resolution Was Adopted by the Sixty Fourth World Health Assembly. Available at: http://www.who.int/cholera/technical/resolution/en/. Accessed June 20, 2020. [Google Scholar]
- 43.Shannon K, Hast M, Azman AS, Legros D, McKay H, Lessler J, 2019. Cholera prevention and control in refugee settings: successes and continued challenges. PLoS Negl Trop Dis 13: e0007347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sphere-Association , 2018. The Sphere Handbook: Humanitarian Charter and Minimum Standards in Humanitarian Response. Available at: https://spherestandards.org/handbook-2018/. Accessed August 19, 2020. [Google Scholar]