ABSTRACT
Most African countries have recorded relatively lower COVID-19 burdens than Western countries. This has been attributed to early and strong political commitment and robust implementation of public health measures, such as nationwide lockdowns, travel restrictions, face mask wearing, testing, contact tracing, and isolation, along with community education and engagement. Other factors include the younger population age strata and hypothesized but yet-to-be confirmed partially protective cross-immunity from parasitic diseases and/or other circulating coronaviruses. However, the true burden may also be underestimated due to operational and resource issues for COVID-19 case identification and reporting. In this perspective article, we discuss selected best practices and challenges with COVID-19 contact tracing in Nigeria, Rwanda, South Africa, and Uganda. Best practices from these country case studies include sustained, multi-platform public communications; leveraging of technology innovations; applied public health expertise; deployment of community health workers; and robust community engagement. Challenges include an overwhelming workload of contact tracing and case detection for healthcare workers, misinformation and stigma, and poorly sustained adherence to isolation and quarantine. Important lessons learned include the need for decentralization of contact tracing to the lowest geographic levels of surveillance, rigorous use of data and technology to improve decision-making, and sustainment of both community sensitization and political commitment. Further research is needed to understand the role and importance of contact tracing in controlling community transmission dynamics in African countries, including among children. Also, implementation science will be critically needed to evaluate innovative, accessible, and cost-effective digital solutions to accommodate the contact tracing workload.
INTRODUCTION
As of December 31, 2020, there were 2,280,488 COVID-19 cases and 64,790 deaths (2.8% case fatality rate [CFR]) reported from the African continent.1 A year into the pandemic, African countries have consistently recorded lower COVID-19 incidence and mortality than Western countries.1,2 Several explanations have been put forward for this unexpected finding: early and strong political commitment to robust implementation of public health measures, including early nationwide lockdowns, contact tracing and isolation, travel restrictions, coordinated public health responses and messaging, hypothesized but yet-to-be confirmed cross-immunity from parasitic diseases and/or other circulating coronaviruses, the young age of the African population, other environmental and genetic factors, and, last, inadequate case identification and reporting.3–6 Since the onset of the pandemic, the Africa Centres for Disease Control ad Prevention (Africa CDC), in collaboration with the World Health Organization (WHO) and country governments, has played a key role in mobilizing and coordinating efforts from a wide range of partners to provide support to countries, notably influential leadership in expanding SARS-CoV-2 testing capacity and technical guidance for contact tracing and community surveillance, including online materials.7 In this article, we discuss contact tracing experiences, challenges, and lessons learned from four African countries (Nigeria, Rwanda, South Africa, and Uganda) and highlight the need for shared best practices across Africa during subsequent COVID-19 waves and for future pandemics. The information presented draws from a Webinar hosted by the African Forum for Research and Education in Health and Fogarty International Center, NIH.8
BEST PRACTICES, KEY CHALLENGES, AND LESSONS LEARNED
Nigeria.
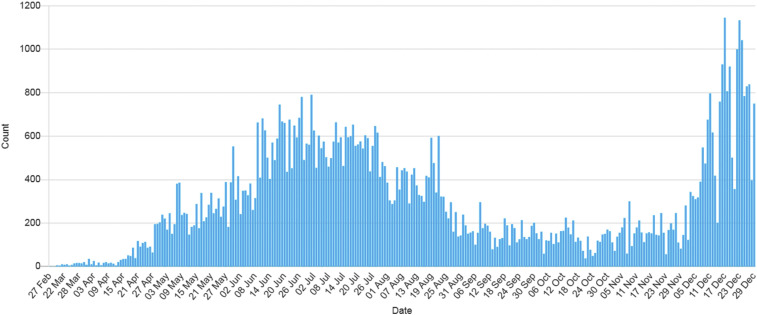
Following the first reports of the SARS-CoV-2 outbreak in Wuhan, China, the Nigeria CDC (NCDC) established a multi-sectoral National Coronavirus Preparedness Group (NCPG) to ensure cohesive and effective coordination of the country’s response.9 As of December 30, 2020, the NCDC reported a cumulative 85,560 COVID-19 cases (4.0 per 10,000 population) with 1,267 deaths (1.5% CFR).10 Figure 1 shows the epidemic curve as of December 30, 2020.8 COVID-19 contact tracing measures were implemented by the multi-sectoral National Coronavirus Preparedness Group (NCPG), which leveraged community networks established previously in response to the Lassa fever, Ebola, and other disease outbreaks. As of October 5, 2020, approximately 80% of Nigeria’s 36 states reported 90% of contacts traced, and 35% of states reported a contact-to-case ratio of more than 5.8 COVID-19 community screening and contact tracing were integrated with well-established strategies and networks for HIV and tuberculosis community case finding.11
Figure 1.
Epidemic curve for confirmed COVID-19 cases in Nigeria, as of December 30, 2020. Source: Nigeria CDC.10 This figure appears in color at www.ajtmh.org.
A best practice was the use of multiple communication platforms to engage, inform, and educate communities. The NCDC actively leveraged platforms such as social media (including Twitter), SMS messaging, and radio. It also maintained a website replete with information for different populations, including locations of testing and isolation centers, informational flyers to post in health facilities and other institutions, and other messaging to counter myths and misinformation.8,10 Prevailing challenges include 1) limited national testing capacity; 2) community resistance and apathy driven by mistrust and perceived/internal stigma, such as feelings of fear/shame and anger toward others, or enacted stigma in the form of discrimination and misinformation; 3) monitoring adherence to self-isolation and quarantine; and 4) inadequate human and financial resources for contact tracing as case burden increased. Important lessons learned include the critical need for decentralization of contact tracing to the lowest geographic levels of surveillance as well as community engagement and involvement to reduce noncompliance (Table 1).
Table 1.
Contact tracer workforce for COVID-19 response in Nigeria, Rwanda, South Africa, and Uganda10,13,15,17
| Country | Contact tracer characteristics | Challenges | Solutions |
|---|---|---|---|
| Nigeria | Type: CHWs | Stigma and misinformation | Ongoing communication to communities in local languages using multiple platforms and multiple trusted voices |
| Contact-to-case ratio: 2 | Mistrust of political entities | Addressing fake news through trusted, authoritative public health voices and daily myth- busters | |
| Number/estimates nationwide (per state): average (range): 111 (30–304) | Overwhelming load of contact tracing and case detection workload for healthcare workers | Decentralization of screening and PCR testing by expanding capacity of existing laboratories and activating new PCR laboratories in every state | |
| % of tests positive (daily average) in January 2021: 7% in suspected cases; 11% in all contacts | Limited testing capacity | Further expansion of human resources and leveraging on partner funding and support | |
| Payment: no | Poor adherence to quarantine and isolation | ||
| Other incentives: stipends, training, certificates, and jackets | |||
| Rwanda | Type: volunteers and students | ||
| Contact-to-case ratio: 4 | Perceived and enacted stigma | Scale up community COVID-19 sensitization and barrier measures in public places involving both public and private authorities | |
| Number of contact tracers: 8/100,000 population | Overwhelming load of contact tracing and case detection workload for healthcare workers | Leveraging information technology to complement traditional contact tracing methods | |
| % of tests positive (daily average) in January 2021: 1.4 and 2% in contacts | Group of people (elderly) not able to remember all contacts | ||
| Payment: no | |||
| Other incentives: transport, phone communication, training, and refreshments | |||
| South Africa (Western Cape Province) | Type: varying categories including CHWs and volunteers | Staff anxiety for their risk of SARS-CoV-2 infection | Building local capacity to produce personal protective equipment |
| Contact-to-case ratio: 3 | Underutilization of quarantine facilities due to enacted stigma, fear of in-facility property loss, and unwillingness to isolate away from family | Education and ongoing communication to communities in local languages using multiple platforms, multiple players | |
| Number of contact tracers: 3/100,000 population | Overwhelming load of contact tracing and case detection workload for healthcare workers | Decentralized contact tracing activities and leverage of telephone contact tracing approach | |
| % of tests positive in suspected cases (daily average): at 1st peak high (July 2020) = 41%; between peak low (October 2020) = 4%; at 2nd peak high (January 2021) = 51% | Need for digital platform to host and share data across jurisdictions. | ||
| Payment: no—if volunteers, some already working for Department of health, but no extra payment given | |||
| Other incentives: training and reimbursement of calling costs incurred | |||
| Uganda | Type: CHWs, volunteers, students, and epidemiologists | Overwhelming load for contact tracing workforce and case detection workload for healthcare workers | Decentralized contact tracing activities to local health teams |
| Number of contact tracers: 186/100,000 population | Stigma | Community engagement and establishment of COVID-19 in every village across the country | |
| Contact-to-case ratio: 6 | |||
| % of tests positive (daily average): 10% in suspected cases. | |||
| Payment: no | |||
| Other incentives: stipends, training, certificates, T-shirts, badges/calendars, and study tour |
CHWs = community healthcare workers (includes community health extension workers and community health officers).
Rwanda.
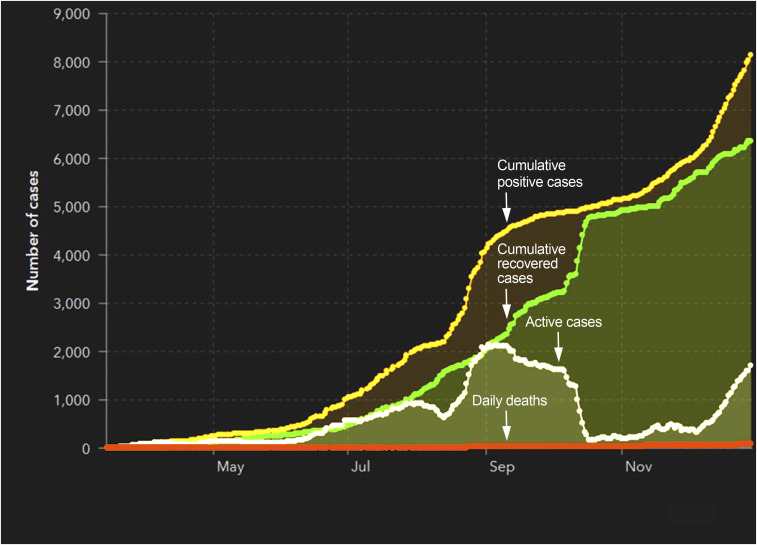
As of December 31, 2020, there were 8,383 cumulative COVID-19 cases (6.4 per 10,000 population) with 94 deaths (1.1% CFR) reported from the Rwanda Ministry of Health.12 Figure 2 shows Rwanda’s COVID-19 epidemic curve.8 Since the onset of the pandemic, the proactive public health response implemented by Rwanda’s COVID-19 National Command Post has included a multi-sectoral approach to contact tracing involving community health worker teams and local government authorities to identify COVID-19 cases early and link them to testing and care. As of October 5, 2020, 19,175 contacts were identified from 4,666 cases; of these contacts, 18,279 were accessed, 642 (3.3%) did not own phones, and 204 (1%) had traveled out of the country.8 Ultimately, 17,243 (89.9%) contacts completed follow-up. The positivity rate among contacts was about 2%, and the contact-to-case ratio was 4.8
Figure 2.
Epidemic curve for confirmed COVID-19 cases in Rwanda, as of December 30, 2020. Source: Ministry of Health, Rwanda Biomedical Centre.13 This figure appears in color at www.ajtmh.org.
A notable best practice was leveraging information technology (IT) to complement traditional contact tracing methods, accommodate the increased workload, and maintain efficiency. Specifically, Rwanda is using cellphone tower data to augment contact tracing efforts.8 A key challenge was spikes in cases, which led to an overwhelming contact tracing and case detection workload for healthcare workers. Solutions required decentralization of contact tracing to community level and further adoption of IT solutions, including geospatial mapping, an electronic notification system leveraged from the national HIV program, an electronic tool for conducting home-based monitoring, and a GPS app for truck drivers. Internalized stigma was another early challenge, and this was addressed by involving both public and private authorities in sensitization campaigns to minimize the impact. Lessons learned include adaptation of the response to local challenges, use of existing community health program platforms (e.g., HIV and tuberculosis), rigorous use of data and technology to improve precision for decision-making, and strengthening of decentralized structures to ensure a comprehensive response at all levels (urban and rural settings) (Table 1).
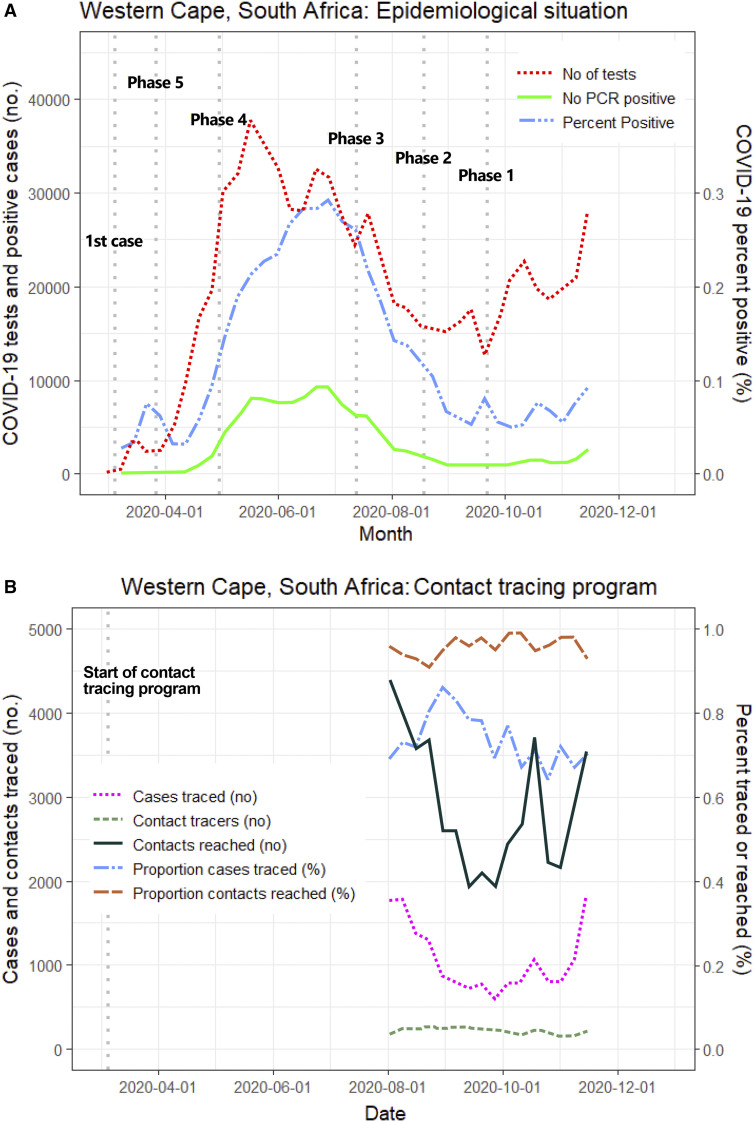
South Africa.
As of December 31, 2020, there were 1,088,889 COVID-19 cases with 29,175 deaths (2.6% CFR) in South Africa, which is epicenter of the pandemic on the continent.1 A 35-day nationwide lockdown was implemented in late March 2020, and more than 30,000 community health workers were immediately deployed for proactive door-to-door testing and contact tracing in 993 prioritized, highly susceptible areas mapped by the social vulnerability index.13 In the hard-hit Western Cape Province, telephonic case and contact tracing also formed the basis of the response (Table 1). A central electronic database of public sector patients was repurposed by the Provincial Health Data Centre to combine new COVID-19 cases from public and private laboratories into a single-line listing. Incorrect telephonic contact details and delays in uploading information were some of the major challenges faced. As community transmission became established and mortality spiked, it became evident that a large proportion of COVID-19 cases had gone undetected. Many cases were unable to be isolated because of poor socioeconomic circumstances. The Department of Health commissioned dedicated quarantine facilities, but these were underused as 14-day quarantine completion was < 50% because of enacted stigma, fear of in-facility property loss, and unwillingness to isolate away from family. Instead, containment was reached through health promotion and education on population-based infection control practices and nonpharmaceutical interventions. Figures 3A and B show the epidemic curve and contact tracing program at different phases of the lockdown in the Western Cape Province.14
Figure 3.
(A) Epidemic curve and contact tracing program. The start dates of the different phases of the lockdown are indicated (phases 5 to 1, 5 being the most stringent). Source: South African Department of Health (SA-DOH).15 (B) Contact tracing program. The start dates of the different phases of the lockdown are indicated (phases 5 to 1, 5 being the most stringent). Source: SA-DOH.15 This figure appears in color at www.ajtmh.org.
South Africa’s key best practices for contact tracing include deployment of community health workers and intensive involvement of public health specialists to appropriately manage different aspects of the response, including case finding and contact identification, epidemiology, and surveillance, and to upgrade central electronic databases. The COVID-19 response in South Africa has shown that a robust healthcare service platform, which includes laboratory testing, hospital bed space, and community engagement, sensitization, and involvement in contact tracing, is essential. Decentralized case investigation and contact tracing worked best because outbreak teams at the local levels were familiar with regional behavior and conditions. A user-friendly, centralized database within a network that fed in data from both private and public sectors was critical to contact tracing, case finding, and overall surveillance.
Uganda.
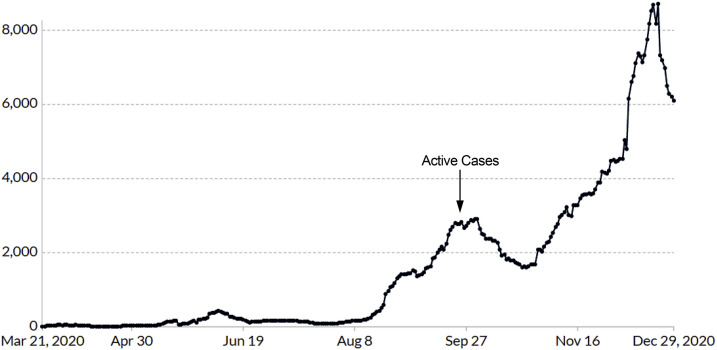
Uganda reported its first COVID-19 case on March 21, 2020, and by December 31, 2020, a cumulative 33,360 cases (3.1 per 10,000 population) and 245 deaths (CFR = 0.7%) were registered. Figure 4 shows Uganda’s COVID-19 epidemic curve.15 There were two waves, the first in May and the second in August/September, and a surge of 11,955 local community cases among the total of 13,351 (90%) cases was detected during this period. Uganda developed a national COVID-19 Response Plan in which an incident management system was activated to coordinate public health mitigation measures, such as banning public gatherings, reducing crowding in public transport, and improving social distancing. Between March and September, 478,687 samples were tested with a positivity rate of 20%.8 In Uganda, contact tracing was driven by central teams; these were deployed to the 14 Ministry of Health regions to train district teams, which worked closely with regional laboratory, surveillance, case investigation, and case management teams. On average, a contact-to-case ratio of 6 was documented (Table 1). Regional contact tracing teams interviewed cases on demographics, lists, and type of contacts and were aided by the WHO GoData tool, a software application used to collect electronic case patient and contact data on mobile phones. By November 3, 2020, Uganda had listed 48,245 contacts; 46,768 (97%) had completed their 14-day follow-up and 6,100 tested positive, giving a secondary attack rate of 13%.8
Figure 4.
Epidemic curve for confirmed COVID-19 cases in Uganda, as of December 30, 2020.16 This figure appears in color at www.ajtmh.org.
A major challenge was that central contact tracing teams could not adequately support all regions and districts because of the rapidly increasing number of cases and contacts, warranting a change of strategy. Subsequently, the contact tracing leadership role transitioned to existing district and community health teams (Table 1). A best practice in Uganda was robust community engagement through building capacity of community health systems to foster trust, contain stigma, and support the contact tracing process,15 especially as activities were decentralized to local health teams. Of note, the Community Engagement Strategy for COVID-19 Response (launched by the Prime Minister on October 20, 2020) requires the establishment of a village COVID-19 task force in every village in the country16 and served as a catalyst for improved coverage and efficiency of contact tracing. Lessons learned: 1) contact tracing played a role in early detection and interruption of transmission and 2) a decentralized approach to district and community health teams was more appropriate once caseload exceeded central capacity.
DISCUSSION
Contact tracing is a traditional pillar of infectious disease control, especially for illnesses involving direct transmission from person to person, such as COVID-19.17 At the onset of the pandemic, the early deployment of local, human-to-human contact tracers (face-to-face and telephone calls) in African countries was crucial to control chains of transmission. Nonetheless, for contact tracing to remain effective during subsequent waves of this pandemic, countries must have sufficient capacity to use targeted tests for high-risk and exposed people in rapid time and adapt contact tracing strategies accordingly.17 Furthermore, the presence and availability of bold and competent public health expertise and leadership, coupled with sustained political commitment and strong health systems, is key to curb the spread of COVID-19.
Some West (Liberia, Sierra Leone, and Guinea), central (the Democratic Republic of Congo), and east (Uganda) African countries have established best practices for contact tracing from experience with previous large outbreaks, such as the Ebola virus; these practices were adapted for the COVID-19 response.18,19 However, past experiences cannot fully compensate for limited resources and underequipped health infrastructure.20 The key challenge was increased case burdens, which overwhelmed traditional time-consuming, labor-intensive contact tracing strategies. To address this issue, South Africa and Rwanda have implemented best practices that include digital contact tracing with the use of a mobile app and cellphone tower data, respectively, hence reducing the required workforce.21 In Nigeria and Uganda, best practices include leveraging multi-platform public communications21,22 and strong community engagement.16 In addition, the WHO is developing a global app for checking symptoms and tracing contacts that will support low- and middle-income countries in their COVID-19 responses.17 However, the low digital coverage and higher costs for Internet access in these countries may limit the success of such initiatives.23
To be maximally effective, contact tracing capability needs to be matched with capacity to test and isolate and isolate positive cases.24,25 For instance, mobile testing services that piggyback on existing platforms can significantly improve testing access and coverage.26 These services can be rapidly deployed for contact tracing and testing as well as routine surveillance in identified hot spots; highly sensitive point of care (PoC) tests with rapid turnaround time are ideal. The GeneXpert platform, already in place for tuberculosis testing across Africa, can allow for decentralization of COVID-19 testing (beyond referral hospitals) with the use of SARS-CoV-2 cartridges.27 However, PoC viral antigen detection is not yet sufficiently sensitive and needs further validation in Africa.27
COVID-19-associated perceived or enacted stigma is a significant issue and has been reported from African countries.4,28 Community sensitization through all available communication outlets, such as radio, TV, SMS messaging, social media, and other accessible platforms, is critical to debunk myths, reduce stigma to at-risk groups, and improve/sustain public attitude and compliance. Contact tracing should also incorporate comprehensive approaches to reduce stigma, including training of healthcare workers and demonstration to the public that people identified positive are managed in a humane manner without stigmatization, whether in the community or at isolation and treatment facilities. These approaches will also be important for acceptance and uptake of COVID-19 vaccines, which are soon to be rolled-out in African countries.
The full impact of the pandemic remains difficult to evaluate in Africa and elsewhere, as reported cases and deaths likely underestimate the full extent of transmission. Serosurveys have reported high attack rates in several African countries, up to 40% in select populations after the first wave.29–31 Yet, despite the economic limitations, fragile public health infrastructure, limited human resources for health, and relatively higher political instability, Africa remains the least affected region globally, with < 1% of global COVID-19 cases and < 0·1% of deaths. Furthermore, it is unclear to what extent specific COVID-19 mitigation measures have contributed to the observed epidemiology in Africa.
Specifically, the effectiveness of contact tracing and population-level interventions on pandemic control remains difficult to evaluate because these interventions were used in combination. SARS-CoV-2 transmission rates could be informed by serology and modeling of detailed epidemiological data, particularly to monitor changes in household transmission risk and the size of traced clusters over time. As community transmission continues to rapidly spread, there is a need to assess and determine the thresholds at which contact tracing may no longer be feasible and cost-effective for different African countries and communities. Furthermore, the impact of contact tracing and other COVID-19 surveillance on case finding among children and its implications for community transmission are largely unknown. For these and other population-level considerations, it would be beneficial to have a multi-country mechanism for sharing COVID-19 experiences, lessons learned, and best practices across the African continent. Such a platform would allow for rapid synthesis of key information that can be promptly evaluated and/or acted on by policymakers; for example, national COVID-19 Task Forces through country-specific decision-making processes.
In conclusion, contact tracing is an important public health strategy for disease control. It is imperative to sustain community-level contact tracing and case identification and to continuously adjust strategies as subsequent waves ensue. Leveraging IT to accommodate rising case burdens reduces the health workforce needed, and these workers could be deployed for upcoming COVID-19 vaccination efforts and other critical health programs. Further data and research are needed to understand the role and importance of contact tracing in community transmission dynamics in African countries, including among children. Also needed are implementation science-based evaluations to assess innovative, accessible digital solutions to maintain and improve contact tracing efficiency while conducting economic analyses to establish cost-effectiveness.
ACKNOWLEDGMENTS
We acknowledge critical review by Jay K. Varma, New York City Mayor’s Office, New York, NY, and the U.S. Centers for Disease Control and Prevention, Atlanta, GA; Justin Maeda, the Africa Centers for Disease Control and Prevention, Addis-Ababa, Ethiopia; as well as the continued support of the AFREhealth Executive Secretariat in Kumasi, Ghana (Ireneous N. Dasoberi, Clara Sam-Woode, and Georgina Yeboah). This article is generated from a COVID-19 Webinar hosted by AFREhealth and Fogarty International Center, National Institutes of Health (www.fic.nih.gov), and presented on October 5, 2020. AFREhealth is a pan-African multi-disciplinary and interprofessional health organization that seeks to work with Ministries of Health, training institutions, and other stakeholders to improve the quality of health care in Africa through research, education, and capacity building (www.afrehealth.org). The American Society of Tropical Medicine and Hygiene has waived the Open Access fee for this article due to the ongoing COVID-19 pandemic.
REFERENCES
- 1.Africa CDC , 2020. Latest Updates on the COVID-19 Crisis in Africa. Available at: https://africacdc.org/covid-19/. [Google Scholar]
- 2.Nachega JB, Seydi M, Zumla A, 2020. The late arrival of COVID-19 in Africa–mitigating pan-continental spread. Clin Infect Dis 71: 875–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehtar S, Preiser W, Lakhe NA, Bousso A, TamFum JM, Kallay O, Seydi M, Zumla A, Nachega JB, 2020. Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Glob Health 8: e881–e883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maeda JM, Nkengasong JN, 2021. The puzzle of the COVID-19 pandemic in Africa. Science 371: 27–28. [DOI] [PubMed] [Google Scholar]
- 5.Massinga Loembé M, Tshangela A, Salyer SJ, Varma JK, Ouma AEO, Nkengasong JN, 2020. COVID-19 in Africa: the spread and response. Nat Med 26: 999–1003. [DOI] [PubMed] [Google Scholar]
- 6.Zeberg H, Pääbo S, 2020. The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature 587: 610–612. [DOI] [PubMed] [Google Scholar]
- 7.Africa Centre for Disease Control , 2020. COVID-19 Contact Tracing. Available at: https://africacdc.org/?s=tracing. Accessed January 6, 2021. [Google Scholar]
- 8.AFREhealth , 2020. COVID-19 Contact Tracing Best Practices in Africa. Audio-Video Recording Available at: https://www.afrehealth.org/mediapage/webinar/253-contact-tracing-in-the-covid-19-response-best-practices-in-africa. Accessed December 30, 2020. [Google Scholar]
- 9.Dan-Nwafor C, et al. 2020. Nigeria’s public health response to the COVID-19 pandemic: January to May 2020. J Glob Health 10: 020399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nigeria CDC , 2020. Available at: https://covid19.ncdc.gov.ng/state/. Accessed December 30, 2020.
- 11.Gidado M, Odume B, Ogbudebe C, Useni S, Tukur M, Chukwuogo O, Ajiboye P, Sadiq I, Yahaya K, Adebola L, 2020. Early experience in implementation of an integrated COVID-19 and TB community-based active case finding. Afr J Respir Med 15: 18–23. [Google Scholar]
- 12.Ministry of Health, Rwanda Biomedical Center , 2020. Update on COVID-19 Data. Available at: https://rbc.gov.rw/index.php?id=188. Accessed December 30, 2020. [Google Scholar]
- 13.Le Roux A, Naude A, 2020. Social Vulnerability – Locating South Africa’s Vulnerable People. Available at: http://stepsa.org/pdf/social_vulnerability.pdf. Accessed December 30, 2020. [Google Scholar]
- 14.The South African Government, Western Cape Province MEC Health , 2020. Available at: https://www.gov.za/portfolio/western-cape-mec-health?gclid=EAIaIQobChMIgs64kor27QIVCb_tCh20LQvBEAAYASAAEgKs4vD_BwE. Accessed December 30, 2020.
- 15.Roser M, Ritchie H, Ortiz-Ospina E, Hasell J, 2020. Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. Available at: https://ourworldindata.org/coronavirus. Accessed December 30, 2020. [Google Scholar]
- 16.The Government of Uganda , 2020. National Community Engagement Strategy for COVID-19 Response. Available at: https://www.redcrossug.org/images/forms/NATIONAL-COVID-19-COMMUNITY-ENGAGEMENT-STRATEGY-300920-V3.pdf. Accessed January 6, 2021. [Google Scholar]
- 17.World Health Organization , 2020. Contact Tracing in the Context of COVID-19. WHO Guidelines. [Google Scholar]
- 18.Greiner AL, Angelo KM, McCollum AM, Mirkovic K, Arthur R, Angulo FJ, 2015. Addressing contact tracing challenges—critical to halting Ebola virus disease transmission. Int J Infect Dis 41: 53–55. [DOI] [PubMed] [Google Scholar]
- 19.Nachega JB, et al. 2020. Responding to the challenge of the dual COVID-19 and Ebola epidemics in the Democratic Republic of Congo-priorities for achieving control. Am J Trop Med Hyg 103: 597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Largent EA, 2016. EBOLA and FDA: reviewing the response to the 2014 outbreak, to find lessons for the future. J L Biosci 3: 489–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nachega JB, Leisegang R, Kallay O, Mills EJ, Zumla A, Lester RT, 2020. Mobile health technology for enhancing the COVID-19 response in Africa: a potential game changer? Am J Trop Med Hyg 103: 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ekong I, Chukwu E, Chukwu M, 2020. COVID-19 mobile positioning data contact tracing and patient privacy regulations: exploratory search of global response strategies and the use of digital tools in Nigeria. JMIR Mhealth Uhealth 8: e19139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jayaram K, Leke A, Leiby K, Ooko-Ombaka A, 2020. Reopening and Reimagining Africa. McKinsey Report. Available at: https://www.mckinsey.com/featured-insights/middle-east-and-africa/reopening-and-reimagining-africa. Accessed December 30, 2020. [Google Scholar]
- 24.The Centre for Respiratory Diseases and Meningitis, Outbreak Response Unit, Division of Public Health Surveillance and Response Services NI for CD (NICD) of the NHLS, National Department of Health SA , 2020. Coronavirus disease 2019 (COVID-19) Caused by a Novel Coronavirus Guideline for Case-Finding, Diagnosis, and Public Health Response in South Africa, Vol. 3. Amsterdam, The Netherlands: Elsevier. [Google Scholar]
- 25.Foundation for Innovative New Diagnostics. SARS-CoV-2 Diagnostics: Performance Data. Available at: https://www.finddx.org/covid-19/dx-data. Accessed May 2, 2020. [Google Scholar]
- 26.Towns R, Corbie-Smith G, Richmond A, Gwynne M, 2020. Lynne FiscusRapid deployment of a community-centered mobile covid 19 testing unit to improve health equity. NEJM Catal Innov Care Deliv, 10.1056/CAT.20.0522. [DOI] [Google Scholar]
- 27.Jacobs J, Kühne V, Lunguya O, Affolabi D, Hardy L, Vandenberg O, 2020. Implementing COVID-19 (SARS-CoV-2) rapid diagnostic tests in sub-Saharan Africa: a review. Front Med (Lausanne) 7: 557797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adesegun OA, et al. 2020. The COVID-19 crisis in sub-Saharan Africa: knowledge, attitudes, and practices of the Nigerian public. Am J Trop Med Hyg 103: 1997–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO , 2020. World Health Organization-AFRO Coronavirus Disease, (COVID-19) Dashboard. Available at: WHO Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard. Accessed December 30, 2020. [Google Scholar]
- 30.Nordling L, 2020. The Pandemic Appears to Have Spared Africa So Far. Scientists Are Struggling to Explain Why. Science. Available at: https://www.sciencemag.org/news/2020/08/pandemic-appears-have-spared-africa-so-far-scientists-are-struggling-explain-why. Accessed December 30, 2020. [Google Scholar]
- 31.Hsiao M, et al. 2020. SARS-COV-2 Seroprevalence in the Cape Town Metropolitain Sub-districts after Peak of Infections, Vol. 18, 2–7. Also, available at: https://www.nicd.ac.za/wp-content/uploads/2020/09/COVID-19-Special-Public-Health-Surveillance-Bulletin_Issue-5.pdf. Accessed December 30, 2020. [Google Scholar]