Abstract
Eviction represents an urgent social and economic issue in the United States, with nearly two million evictions occurring annually in the U.S. Still, the population health impacts of evictions, as well as the pathways linking eviction to health, are not well documented or understood, particularly among young adults. Using nationally-representative, longitudinal data from the National Longitudinal Study of Adolescent to Adult Health (1994–2008) (n=9,029), the present study uses a combination of analytic methods—including prospective lagged dependent variable regression models, inverse probabilities of treatment weighting, longitudinal first difference models, causal mediation techniques—to comprehensively assess whether and how evictions relate to depressive risk and self-rated health across early adulthood, paying particular attention to the stress-related pathways linking eviction and health. Results provide robust evidence of positive longitudinal associations between eviction and depressive risk, in particular. In the prospective regression models, young adults who experienced recent eviction had more depressive symptoms and worse self-rated health than those who were not evicted, net a host of background characteristics. Using treatment weighting techniques, results showed that young adults who experienced eviction had more depressive symptoms than those who were not evicted (5.921 vs. 4.998 depressive symptoms, p=0.003). Perceived social stress mediated nearly 18 percent of the associations between eviction and the depressive symptoms (p<0.001). In the first difference models, young people who experienced eviction between survey waves experienced greater increases in depressive symptoms over time compared to those who were not evicted, net of changes in other indicators of socioeconomic status and residential instability. Taken together, our results suggest that the recent surges in evictions in the U.S. serve as a potent threat to population health during the emerging adult period, with especially devastating consequences for low-income individuals and communities of color.
Keywords: Eviction, Health, Depression, Emerging Adulthood, Young Adulthood, Housing, Psychosocial Stress
1. Introduction
Eviction is one of the most urgent social and economic issues the United States currently faces. Though eviction most often refers to the forcible expulsion of a tenant from a residence by a landlord, eviction can also include the loss of housing following end-stage foreclosure. America has experienced a dramatic increase in evictions among renters in the last 20 years, jumping from 518,873 evictions in 2000 to 898,497 in 2016 (Desmond et al., 2018). Similar increases in foreclosures were seen between 2000 and 2012 (Arnio et al., 2012). The COVID-19 pandemic—and the subsequent response by the United States’ government—brought about the worst economic crisis since the Great Depression, leaving millions of people across the country at risk of eviction (Gopinth, 2020). With no significant relief in sight, some 40 million American renters may lose their homes by early 2021 (Benfer et al., 2020) while foreclosures are already on the rise in urban areas (Centopani, 2020).
The parallel rises in housing costs and housing insecurity in the U.S. have potentially dire consequences for population health. America is in the middle of “the worst affordable housing crisis in several generations,” (Desmond & Kimbro, 2015, p. 295). The majority of low income, renting families in the US reported spending over 50% of their income on housing costs (Desmond, 2015). As housing consume a greater portion of household budgets, poor families are left with fewer economic resources for food, school supplies, medical care, transportation, and other necessities (McConnell, 2012; Newman & Holupka, 2015). The shortage of affordable housing, especially in urban areas, also means that low income families disproportionately live in substandard housing, thereby increasing their risk for a number of adverse health outcomes (Bashir, 2002; Krieger & Higgins, 2002; M. Shaw, 2004). Focusing explicitly on eviction, the overwhelming nature of being forcibly removed from one’s home makes eviction a particularly salient stressor in the lives of a growing number of American households. Given that eviction exposes households and individuals to a host of psychosocial, socioeconomic, and physical risks, eviction represents a growing threat to population health in the US.
Despite the initiation of recent investigations into the scope of eviction in the US (Desmond, 2015; Desmond et al., 2018; Desmond & Kimbro, 2015; Thomas et al., 2019), eviction remains relatively poorly documented, and its links to health remain to be better understood. Current data from Princeton’s Eviction Lab indicates that there was one eviction for every 17 renter households between 2000 and 2016, with almost a million evictions occurring each year (Desmond et al., 2018). When foreclosures are included in eviction estimates, the number of households affected doubles to nearly 2 million, despite the fact that foreclosure rates have been declining to reach near pre-Great Recession rates (ibid). In many ways, the recent aggregation of eviction data has shed light on the scale of the problem of housing insecurity and highlighted just how little is known about population patterns and consequences of forced housing loss. In particular, though millions of America families face eviction each year, the health impacts of eviction remain poorly understood, with research in this area providing somewhat inconsistent findings (see Vásquez-Vera et al., 2017 for review). To date, research on the health effects of eviction has been largely limited to singular, cross-sectional outcomes and analytic strategies that raise concerns about reverse causality, confounding, and selection bias. Still, given documented links between housing insecurity and health (ibid), it is likely that the stress, instability, and physical, psychosocial, and environmental exposures associated with eviction likely pose a tremendous threat to population health.
Using nationally-representative, longitudinal data from the National Longitudinal Study of Adolescent to Adult Health, the present study uses a combination of prospective multivariate regression models, individual fixed effects models, causal mediation techniques, and treatment weighting procedures to comprehensively assess whether and how evictions relate to health across early adulthood. By linking changes in eviction status to changes in health, this study provides convincing evidence of the role of evictions in population health inequality. We further elucidate the important role of psychosocial stress as a mediator linking evictions to health. In this way, this study provides new knowledge of the specific role of evictions in the production of health disparities early in the adult life course and informs policy efforts aimed at improving housing security as a means to protect and promote public health.
2. Background
2.1. Housing Insecurity, Housing Loss, Risk, and Mental Health
A large body of research demonstrates a general link between housing instability and mental health. Measures of housing instability, sometimes referred to as housing insecurity, have included missed rent or mortgage payments, being anywhere in the eviction or foreclosure process, housing mobility, housing tenure, overcrowding, perception of adequate housing, physical housing condition, and location in high foreclosure/eviction areas (see Vasquez-Vera et al. 2016 for review linking various forms of housing instability to different health outcomes). The range of mental health outcomes studied in relationship to housing instability has been similarly expansive. Studies have shown a positive association between some form of housing instability and depression (Alley et al., 2011; Bernal-Solano et al., 2019; Burgard et al., 2012; Cagney et al., 2014; Desmond & Kimbro, 2015; Kingsbury et al., 2018; Sadowski et al., 1999; Suglia et al., 2011), anxiety (Bernal-Solano et al., 2019; Suglia et al., 2011), stress (Bernal-Solano et al., 2019; Blair et al., 2011), psychological health (Rollings et al., 2017), mental health score or strain (Aro & Hanninen, 1984; David J. Pevalin et al., 2017), and suicide or suicide risk (Fowler et al., 2014; Houle & Light, 2014; Mateo-Rodríguez et al., 2019). The comparability and quality of several of these studies were recently evaluated in a review by Singh and colleagues (2019).
Several studies link home loss to adverse mental health outcomes. The experience of foreclosure has been associated with depression (Bernal-Solano et al., 2019; Cagney et al., 2014), poorer mental health indicators (McLaughlin et al., 2012; D. J. Pevalin, 2009; Robles-Ortega et al., 2017), and increased risk of suicide (Cook & Davis, 2012; Fowler et al., 2014; Mateo-Rodríguez et al., 2019). Other studies have used census track or county data and have found positive correlations between foreclosure rates and suicides (Houle & Light, 2014). Additional research suggests that the experience of foreclosure itself may have a greater impact on mental health and stress than being behind on payments or in default (Prohaska & Lichtenstein, 2014). Desmond and Kimbro (2015) reported an association between the experience of eviction and depression among renters while Fowler et al., (2014) included both evictions and foreclosures in their study linking home loss to suicide risk.
2.2. Housing Insecurity, Housing Loss, Risk, and Physical Health
In addition to mental health, housing insecurity and loss has been linked to indicators of general and physical health. Studies have found associations between some form of housing insecurity and health behaviors such as alcohol use (Arcaya et al., 2013; Bernal-Solano et al., 2019; Burgard et al., 2012; Murphy et al., 2014), initiation of drug use (Damon et al., 2019), and high-risk behaviors, such as syringe sharing, among individuals who use drugs (Pilarinos et al., 2017). Housing instability has been linked to poorer self-reported health (Burgard et al., 2012; Martin et al., 2019; Schootman et al., 2012), elevated blood pressure and weight gain (Arcaya et al., 2013; Arcaya, 2017), reduced diabetes self-efficacy (Vijayaraghavan et al., 2011), greater presence of chronic medical conditions (Martin et al., 2019), and higher all-cause and cardiovascular-related mortality rates (Chan et al., 2014). Studies have also shown links between housing instability and negative health outcomes among children, including increased risk of physical abuse and subsequent hospitalization (Wood et al., 2012); poorer diet (Bottino et al., 2019); and elevated cortisol levels (Blair et al., 2011). Finally, the consideration of the role of substandard housing as a feature of housing instability has generated an immense body of literature on the health effects of exposures common in substandard housing, such as lead (Jacobs, 2011), asthma triggers (Jacobs, 2011; Miles & Jacobs, 2008), and asbestos (Krieger & Higgins, 2002; Marquez et al., 2019).
Like studies of mental health risk, studies examining the links between eviction (including rent-based and foreclosure) and physical health generally support the idea of forced housing loss as a unique stressor that affects physical health and physiological functioning. Using Census track data, studies have linked increased rates of eviction with rates of sexually transmitted infections (Niccolai et al., 2019) and infant mortality and low birthweight (Hazekamp et al., 2020). Using longitudinal data from the Fragile Families and Child Wellbeing Study, Leifheit et al. (2020) identified a relationship between eviction and food insecurity that was not due to neighborhood effects. Other studies have shown that among people with HIV, the experience of eviction can lead to increased viral load (Kennedy et al., 2017). While representing a distinct experience from eviction, a recent study in Spain found that people in the latter part of the foreclosure process reported increases in sleep disturbances, worsening of previous chronic conditions, and an increase in the consumption of medications (Bernal-Solano et al., 2019). This study is suggestive of the potential physical impacts that may also be experienced by families exposed to eviction.
2.3. Eviction from a Life Course Perspective
The life course perspective (Marshall et al., 2009) offers important insights for the study of eviction. In particular, this study draws on two key concepts from the life course perspective. First, the life course perspective emphasizes the importance of turning points, which are events or circumstances that alter or redirect life course trajectories or pathways. In this study, we conceptualize eviction as particularly salient turning points in the life span that can fundamentally alter future trajectories of physical, mental, social, emotional, and economic well-being in ways that relate to health. Second, the life course perspective also highlights the importance of the life course timing of social exposures, considering how life stages may produce differential risks of and vulnerabilities to exposures in ways that are consequential for health (McDonald, 2011). Research increasingly highlights emerging adulthood as a critical or sensitive period in the life course, during which social exposures like evictions may have especially lasting or consequential impacts on life course trajectories of health and well-being (Wood et al., 2018). Much of the research on the health effects of eviction has focused on middle age and older adults, families, and children. This focus is partly due to the extensive study of foreclosures following the 2008 financial crisis. Foreclosure studies typically include families with children and older adults because young adults are much less likely to have taken on mortgages (Hirschl & Rank, 2010). Still, less is known about how housing loss shapes well-being in the emerging and young adulthood periods, when many young people experience financial instability as they transition to increased independence. Furthermore, studies indicate emergent adulthood as the peak of residential change (Arnett, 2006), making it a period when people may be particularly vulnerable to housing instability and eviction. It is therefore possible that housing loss during this life stage may have particularly salient impacts on young people’s future trajectories of health and well-being, critically and potentially irreversibly altering their physical, mental, and financial well-being.
2.4. Potential Pathways Between Eviction and Health
Synthesizing the literatures on housing instability, eviction, and health, we identify three primary pathways through which eviction can affect health (see Figure 1). The bolded pathway represents the pathway examined in this analysis while the grayed pathways represent other potential pathways for examination in the study of eviction and health outcomes. The first pathway, which is the focus of the current study, is through psychosocial stress. The second pathway is through increased environmental exposures which often result from substandard housing. The final pathway is through increased disease exposure, an increasingly relevant issue as we continue to battle the COVID-19 pandemic. We briefly review each of these potential pathways here.
Figure One.
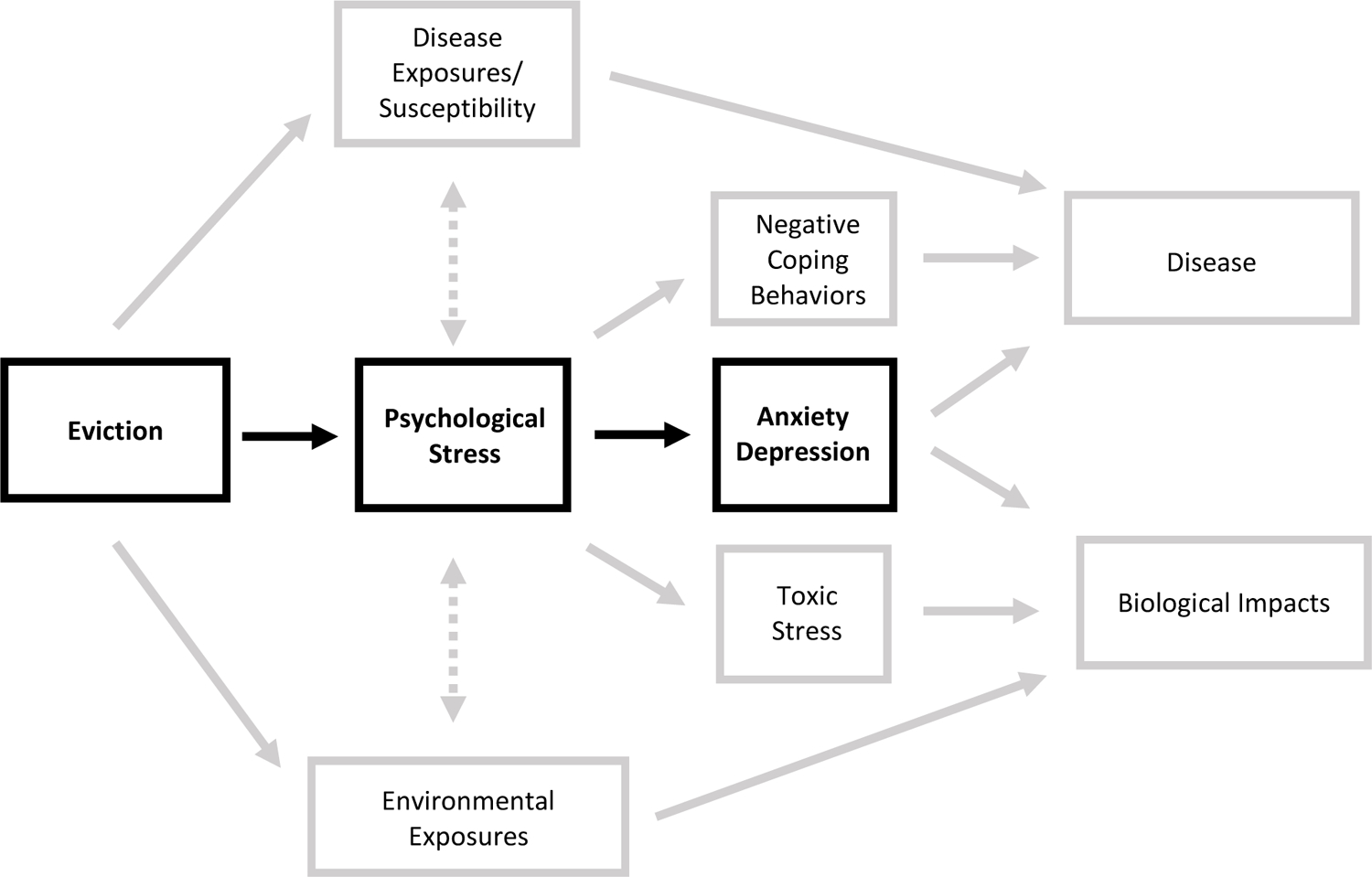
Pathways from Eviction to Poor Health Outcomes. The bolded pathway is tested in the current analysis while other pathways represent potential areas for future research. It should also be noted that more bi-directional and interactive relationships exist than are depicted in this simplified model. For example, biological impacts are likely to interact synergistically with disease outcomes or we might expect that the experience of depression and anxiety might also lead to negative coping behaviors that can in turn increase disease exposure or disease outcomes. We encourage the reader to draw more connections between the elements of this figure than we have included for the ease of interpretation.
First, eviction can act through the stress pathway, increasing the experience of psychosocial stress. Stress over the threat or loss of housing can lead to increased rumination, hopelessness, anxiety, depression, and risk of suicide (Desmond, 2015; Desmond & Kimbro, 2015; Fowler et al., 2014). This stress can be compounded by the experience of social stigma associated with eviction and housing loss (Desmond, 2012; Grainger, 2020). Researchers have shown that various forms of stigma can have significant mental health effects (Brewis, 2014; Hatzenbuehler et al., 2013; Hatzenbuehler & Pachankis, 2016; Mak et al., 2007). In addition to mental health impacts, psychosocial stressors also have biological impacts that alter physical health, including reduced sleep quality, hormonal changes associated with chronic hypothalamic-adrenal-pituitary (HPA) axis activation, and reduced immune function. Additionally, declining mental health and increasing depression can lead to the adoption of coping behaviors that may also put physiological health at risk such as increased substance use.
The second pathway through which eviction relates to health is environmental exposures. Being evicted increases an individual’s likelihood of being exposed to substandard housing or becoming homeless (Desmond, 2012). As previously mentioned, substandard housing brings with it an increased risk of exposure to dangerous and toxic substances including lead, asthma irritants, and asbestos. Additionally, substandard housing may lack the appropriate mitigation for other potential environmental pollutants that can have negative effects on health. These potential exposures may interact synergistically with the biological impacts of chronic stress associated with eviction leading to more severe negative outcomes. For example, research has shown that nutritional inadequacies such as low calcium, irregular food intake, and iron deficiency can increase the absorption of lead (Hubbs-Tait et al., 2005; Kwong et al., 2004; Levander O A, 1979; Mahaffey, 1995).
Finally, eviction can directly increase one’s exposure to infectious disease risks. Upon experiencing eviction, individuals and families may seek shelter in crowded, unsafe situations. This can include homeless shelters, doubling up (moving in with friends or family), or seeking alternative accommodations in one’s vehicle or on the street. Any of these options can lead to increased exposure to those infectious diseases that continue to disproportionately affect homeless populations such as HIV, Hepatitis B, Hepatitis C, and tuberculosis (Badiaga et al., 2008). In addition to direct exposure, risk of diseases contact can be increased by the adoption of coping behaviors and survival strategies such as engaging in sex work to cover housing costs. Finally, disease susceptibility may also be increased as a result of stress-related immune suppression that may make increased exposures even more likely to result in disease. While these pathways are likely to represent just some of the ways that eviction can impact health outcomes, we believe that they represent those that are most easily studied and intervened upon. We acknowledge the directionality and interactional relationships between the elements of this model are likely to be far more complex than depicted here. However, for the ease of legibility we have limited our depictions of these connections and encourage other scholars to build upon this basic model to highlight new pathways and interactions in the study of eviction and health outcomes.
2.3. Gaps in the Literature
Despite growing interest on the relationship between eviction and health, research has on the health impacts of eviction has produced somewhat inconsistent results, leaving four critical questions about the role of eviction in population health inequality unanswered. First, most studies of the health effects of eviction primarily utilize cross-sectional study designs, which raises concerns about reverse causality, confounding, and selection. For one, individuals who are less healthy may have a greater likelihood of experiencing economic shocks such as eviction (McDonough and Amick 2001). Similarly, with omitted variable bias, confounding factors not included in analytic models may put individuals at risk for both declines in health and economic security (Burgard et al. 2007). Even models with extensive adjustment for factors endogenous to health and housing insecurity may not provide convincing evidence of a relationship between eviction and health, as many of the same measured and unmeasured factors that increase risk for eviction—such early-life socioeconomic hardship—are also drivers of health. In this way, the concern is that any observed relationship between evictions and health may reflect underlying differences between those who were never evicted and those who experience eviction, rather the consequences of housing loss. For these reasons, research using treatment weighting procedures can help in obtaining more convincing estimates of the health consequences of eviction. Further, while cross-sectional analyses are particularly prone to issues related to selection and omitted variable bias, intra-individual examinations of how changes in eviction history correspond to subsequent changes in health provide more convincing evidence of the impact of eviction on health. The use of longitudinal individual first difference models are particularly well suited for modeling change in economic outcomes (like eviction) and health over time while controlling for stable individual characteristics (Burgard et al. 2013).
Second, a number of investigations rely on proxy measures for eviction, such as other measures of housing instability, or measures of eviction risk rather than the directly testing the impact of housing loss on health. While several of these studies demonstrate the potential impact of eviction on health, it is reasonable to expect that the experience of eviction may present different or more extreme pressures than other forms of housing instability that result in differing and potentially stronger health impacts. As such, additional studies examining the experience of eviction and its effects on health are necessary.
Third, it is increasingly necessary that researchers elucidate the mechanisms underlying the relationship between eviction and health. Many of these mechanisms have remained unclear, in part because they vary across different markers of health. The lack of clear mechanisms is perhaps one of the reasons for the emphasis on examining mental health as an outcome of eviction, as the mechanistic pathways whereby evictions can lead to increased psychosocial stress and negative ideation and subsequently anxiety, depression, and suicide appears clearer than the pathway through which eviction can lead to, for example, heart disease. However, research examining the long-term impacts of what has been called allostatic load (McEwen, 1998), or the increased physiological burden resulting from chronic and cumulative stress, is shedding new light on potential pathways connecting eviction and a range of poor health outcomes and risk factors (e.g. Blair et al., 2011). Psychosocial stress represents just one potential pathway through which eviction may affect health and as such, the examination of a broader range of health outcomes is likely to enhance our understanding of the extent of these effects and our ability to formulate potential solutions.
Finally, additional research is needed to elucidate the effects of eviction across different points of the life course. As previously noted, much of the research on housing loss has focused on older adults and families with children. Less research focuses on the effects of eviction during emerging and young adulthood. As described, scholarship increasingly points to emerging adulthood as a unique period of life course development (Arnett, 2000, 2006; Nelson, 2020). transition to financial dependence to independence and begin to forge their own economic paths. Emerging adulthood has been described as a period of high optimism, when young people have “an unparalleled opportunity to change transform their lives,” (Arnett, 2006, p. 7). As such, a significant negative event during this period, such as an eviction, may dramatically alter the social, psychological, and economic trajectory of individuals
Using nationally-representative, longitudinal data, our study uses a combination of prospective regression models, inverse probability of treatment weights, individual fixed effects models, and causal mediation techniques to fill these gaps in the literature and advance scientific understanding of the role of eviction in patterning population health among young adults. In particular, we assess how eviction shapes markers of mental and general health status and further examine the mediating role of psychosocial stress in linking eviction to health during emergent and early adulthood. As such, findings from this study shed new light on the role of housing policy in shaping population health, particularly early in the adult life course.
3. Data and Methods
3.1. Data and Samples
This study uses data from the National Longitudinal Study of Adolescent to Adult Health (Add Health) (1994–2009), a nationally representative, longitudinal study of U.S. adolescents (Harris et al. 2009). Add Health began in 1994–5 with in-school questionnaires and in-home interviews at Wave I, relying on a school-based complex cluster sampling frame. Add Health then followed up with respondents through a series of in-home interviews in 1996 (Wave II), 2001–02 (Wave III), and 2007–08 (Wave IV). This study utilizes data from the in-home interviews at Waves I, III, and IV and Census tract-level data linked to respondents’ residences at Wave I, III, and IV.
Our analytic samples vary by outcome and analytic strategy. Generalized linear models (including inverse probability of treatment weighted models) include all respondents with complete data used in the analyses (depressive risk and self-rated health: n=5,934) estimates from the longitudinal first difference models are derived from respondents with complete data on the variables used in the analyses who experienced change in the outcomes across waves (depressive risk: n=9,029; self-rated health: n=897).
3.2. Key Exposures
The key exposure of interest in this study is eviction. In Waves III and IV, Add Health asked respondents if they had been evicted from their house or apartment for not paying rent or mortgage in the past 12 months. Supplementary analyses revealed that the overwhelming majority (more than 90 percent) of individuals who reported experiencing eviction were renters, not homeowners, suggesting that they experienced eviction from a landlord, rather than eviction following foreclosure. Our study includes both a binary measure of ever evicted (where “1” indicates that the respondent reported being evicted in Wave III and/or Wave IV), as well as time-varying measures of recent eviction (1=evicted in the past 12 months) at Waves III and IV.
3.3. Outcomes
Outcomes include two longitudinal measures of health, measured at Waves III and IV. First, depressive symptoms is a continuous measure indicating respondents’ score on the Center for Epidemiological Studies Depression (CES-D) scale. Consistent with previous research (Anonymous et al., 2020), we used nine items that were consistently-measured across waves that asked respondents how often during the past week they: were bothered by things that didn’t usually bother them; felt they could not shake the blues; were just as good as other people (reverse coded); had trouble keeping their mind on what they were doing; felt depressed; were too tired to do things; enjoyed life (reverse coded); felt sad; and felt that people disliked them. In addition to being a critical marker of mental health risk, increases in depressive symptoms have been further associated with increases in physical health risk (Kiecolt-Glaser & Glaser, 2002; Penninx, 1998). Depressive states can both stimulate the production of physiological stress response hormones and down-regulate immune response, putting individuals with high levels of depressive symptoms at increased risk of disease risk and prone to prolonged infection and delayed wound healing (Kiecolt-Glaser & Glaser, 2002). Second, we include a measure of self-rated health, which is derived from a question asking respondents to rate their health as excellent, very good, good, fair, or poor. This variable is coded so that 1 represents poor health and 5 represents excellent health. Supplementary analyses using alternative operationalizations of the self-rated health measure (including a binary measure indicating poor/fair health) yielded substantively similar results. Self-rated health is strongly and consistently associated with a variety of health outcomes, including markers of morbidity, biomarkers of physiological function, and mortality (Idler & Benyamini, 1997; Jylhä, 2009; Jylhä et al., 2006; McDonough & Amick, 2001). Importantly, unlike indicators of disease, disability, or mortality that are more prevalent among older age populations, depressive symptoms and self-rated health reflect continuous changes in well-being over time, making them particularly useful for estimating health trajectories among younger populations (Deaton & Paxson, 1998; B. A. Shaw & Krause, 2002). We also use these health outcomes to reduce concerns related to misclassification error, where individuals who do not yet have a disease, have not yet been diagnosed, or who are otherwise unaware of their health risk are classified as “well” (Aneshensel et al. 1991). Misclassification error is of particular concern in studies of young adults, many of whom may be at risk of developing disease but either do not yet have an official disease diagnosis or have not received an accurate one (Nguyen et al. 2011).
3.4. Covariates
Our models also include a host of individual-, family-, and neighborhood-level covariates, including race-ethnicity (1=non-Hispanic White, 2=non-Hispanic Black, 3=Hispanic, 4=non-Hispanic Asian), age (years), gender (1=female), and individual, family, and neighborhood SES. Our measure of SES in adolescence (Waves I) is the mean of standardized measures of parental education and household income. Our measure of socioeconomic attainment at Waves III and IV is the mean of standardized (z-score) measures of respondent completed education and household income. We also include measures of marital status (1=married) at Waves III and IV. In order to better estimate the role of eviction in shaping health risk, we include several measures of residential moves. In the prospective regression and treatment weighting models, we include an indicator for total number of residential moves between Waves I and III. Our longitudinal models include measures indicating whether respondents moved prior to the Wave III and Wave IV interviews. We also include measures of neighborhood economic disadvantage using a composite index of four Census tract measures of neighborhood economic conditions: proportion of residents who are unemployed, proportion of residents over the age of 25 years without a high school degree, proportion of families living in poverty, and proportion of families receiving public assistance. For each individual neighborhood measure, we created a dummy variable indicating the top quartile of all Census tracts and then summed the four dummy measures, producing an index of neighborhood economic deprivation ranging from 0 (low) to 4 (high). Finally, we include a measure of perceived social stress, indicated by a continuous measure using a subset of measures from Cohen’s Perceived Stress Scale (range 0–16) (Cohen et al., 1983). The items included in the subscale assessed perceived stress in the past two weeks by asking respondents how often respondents: felt unable to control important things in their life; felt confident about their ability to handle personal problems; felt that things were going their way; felt difficulties were piling so high that they could not overcome them. Responses for each of the four individual items were summed, producing total scores ranging from 0 to 16. The measure of perceived social stress was available at Wave IV only.
We ran supplementary models that further adjusted for a variety of additional indicators of family structure and housing instability, including measures of: ever homeless; ever lived in a shelter; ever lived in a group home; ever ran away from home; and total number of individuals who lived with the respondent at Waves I, III, and IV. These indicators were not associated with the outcomes, and including these measures in our models did not change the parameter estimates for eviction. For these reasons, we excluded these measures from the final models presented in the paper.
3.5. Analytic Methods
We begin with descriptive analyses, paying particular attention to disparities in the outcomes and covariates between those who report ever having been evicted and those who did not report being evicted.
Our multivariable analysis of the links between eviction and the outcomes includes three analytic stages, which together provide a robust assessment of the role of eviction in health disparities in early adulthood. First, we examine the association between eviction history (measured using the binary measure indicating whether the respondent reported ever being evicted) and the outcomes measured at Wave IV using generalized linear models (negative binomial for depressive symptoms and ordinal logit for self-rated health). This first set of models regresses the outcomes on eviction history in a stepwise fashion and provides a baseline estimate of the associations between eviction and the outcomes. Model 1 is a basic adjusted model that includes eviction history, gender, race-ethnicity, and age. Model 2 builds on Model 1 by including the measures of individual and family SES at Waves I, III, and IV, marital status at Waves III and IV, and number of residential moves between Waves I and III. Model 3 builds on Model 2 by including the measures of neighborhood economic disadvantage at Waves I, III, and IV. Model 4 builds on Model 3 and includes the marker of perceived social stress at Wave IV. Finally, Model 5 is the fully adjusted model that builds on Model 4 by including a lagged dependent variable (a marker of depressive symptoms at Wave III in the depressive symptoms model and self-rated health at Wave III in the self-rated health model). By including a lagged dependent variable, Model 5 indicates how eviction history relates to the outcomes at Wave IV net of the covariates and controlling for health status at Wave III. Model 5 takes the following generic form, where Xi represents a vector of covariates and β3yit−1 is the lagged dependent variable:
| (Equation 1) |
As described, we are particularly interested in the mechanisms linking eviction to the outcomes. In particular, we formally assess whether perceived stress mediates the association between eviction history and the outcomes using parametric regression models for causal mediation analysis (Emsley & Liu, 2013; Valeri & VanderWeele, 2013). This mediation technique requires estimating two models: a model for the mediator conditional on treatment and covariates and a model for the outcome conditional on treatment and covariates. The mediation analyses determine the proportion of the total effect of eviction history on the outcomes that is mediated by perceived social stress. Because our measure of perceived social stress is measured only at Wave IV, these mediation models assesses the links between eviction history, perceived social stress at Wave IV, and the outcomes measured at Wave IV. The mediation models include the full set of covariates included in Model 5 above. Because of data limitations, we are unable to test the mechanistic effects of environmental exposures or infectious disease susceptibility and instead focus our mediation analyses on the role of psychosocial stress.
In the second analytic stage, we build on these prospective regressing models by using inverse probability of treatment weighting (IPTW) with regression adjustment. As described, concerns about selection bias and confounding are widespread in studies of eviction and health. Even models with extensive adjustment for factors endogenous to eviction and health may not provide convincing estimates, as many of the factors that increase individual risk for eviction—such early-life SES and neighborhood conditions—also shape health risk. Eviction is not randomized in the population, so any observed relationship between eviction and health may reflect underlying differences between those with varied eviction histories, rather than reflecting health consequences of eviction (Thoemmes & Ong, 2016). We use IPTW with regression adjustment to better account for potential confounding and selection. This method involves calculating a propensity score for respondents, which is the probability of eviction conditional on a set of covariates (Rosenbaum & Rubin, 1983). IPTW then uses the propensity scores to weight observations and create a new pseudo-population where the likelihood of eviction is no longer confounded by the covariates. IPTW balances the treatment assignment across the covariates by giving more or less weight to respondents with covariate histories that are under- or over-represented in the exposure groups (Robins et al., 2000). In addition to IPTW, we use a regression adjustment estimator in these models. This strategy combines IPTW with regression modeling of the relationship between the covariates and outcomes. Importantly, these models have the property of being doubly robust, so as long as either the model for the treatment or the outcome is correctly specified, the estimate for eviction will be unbiased. Using the IPTWs with regression adjustment, we model the “treatment” (e.g., probability of eviction) using logistic regression and include measures of respondent race-ethnicity, gender, and age; family SES at Wave I; total number of residential moves between Waves I and III; and the measure of neighborhood socioeconomic conditions at Wave I. We model the outcomes using generalized linear models and include the same set of covariates included in Model 4 of the prospective regression models described above: race-ethnicity; gender; age; SES at Waves I, III, and IV; marital status at Waves III and IV; total number of residential moves between Waves I and III; neighborhood socioeconomic conditions at Waves I, III, and IV; and the measure of perceived social stress. Using this approach, we are able to estimate the prospective associations between our measure of eviction and the outcomes while explicitly modeling and adjusting for the uneven risks of eviction in the sample using treatment weighting procedures.
Still, while these prospective multivariable analyses provide a robust assessment of potential links between eviction and health, longitudinal analyses may be better equipped to deal with potential problems related to selection and confounding than cross sectional models. For this reason, in the third stage of analysis we use multivariable first difference models, which are equivalent to fixed effects models for two-wave panel data. In these models, changes in the outcomes between Waves III and IV are modeled as a function of change in the independent variables, including eviction. Time-invariant predictors, such as gender and race, are “differenced away” and omitted from model estimates, which provides a solution to the problem of unmeasured heterogeneity and omitted variable bias (Allison, 1990, 1994; Gunasekara et al., 2014). We can specify the first difference models as:
| (Equation 2) |
| (Equation 3) |
In Equations 2 and 3, Evictioni1 and Evictioni2 represent eviction status at time 1 (Wave III) and time 2 (Wave IV), respectively. Xi1 and Xi2 represent vectors of time-varying covariates measured at times 1 and 2, and Zi represents vectors of time-constant variables, both measured and unmeasured. The difference equation is specified by subtracting Equation 2 from Equation 3:
| (Equation 4) |
In Equation 4, the vector of Z variables is differenced out of the first difference model on the assumption that the effects of Z are time-constant. Hausman tests indicated that the preferred model is the first difference model, rather than a random effects model (p<0.001).
We run models for depressive symptoms and self-rated health separately in a stepwise fashion. For each outcome, Model 1 models the change in outcomes as a function of changes in eviction status and age. Models 2 and 3 build on Model 1 by adjusting for changes in SES and neighborhood economic deprivation, respectively. Finally, Model 4 builds on Model 3 by adjusting for changes in residence (e.g., residential moves) between waves. As explained, because race and gender are time-constant measures, they are excluded from the first difference models.
In supplementary analyses, we tested for potential moderation by in the associations between eviction and the outcomes by race, SES, gender, and household size in both the prospective and longitudinal models but found no evidence of moderation.
4. Results
4.1. Descriptive Results
Descriptive statistics for the full sample and by eviction history are in Table 1. Overall, roughly 1.6 percent of young adults report experiencing eviction at Waves III and/or IV. Compared to individuals who do not report eviction, those who report experiencing eviction have higher levels of depressive symptoms at Waves III and IV and had worse self-rated health in Wave IV. There are also striking racial and socioeconomic disparities in eviction history. Black young adults have particularly high levels of eviction; while Black young people comprised approximately 12 percent of the full sample, they represented approximately 23 percent of those who reported being evicted in Waves III and/or IV. Young adults with lower SES at Waves III and IV are more likely to report eviction (p<0.001), as are young people who lived in economically disadvantaged neighborhoods in adolescence (p<0.001) and young adulthood (p=0.003). Compared to young people who did not report eviction, individuals who report experiencing eviction have higher levels of perceived social stress at Wave IV (p<0.001).
Table 1.
Descriptive Statistics (Add Health 1994–2008) (n-5,934)
| Full sample | By eviction history | ||||
|---|---|---|---|---|---|
| Mean/prop. |
Never evicted Mean/prop. |
Ever evicted Mean/prop. |
p-value |
||
| Outcomes | |||||
| Depressive symptoms | |||||
| Wave III | 4.277 | 4.256 | 6.405 | <0.001 | |
| Wave IV | 5.001 | 4.945 | 8.769 | <0.001 | |
| Poor or fair self-rated health (1=yes) | |||||
| Wave III | 4.006 | 4.011 | 3.757 | 0.108 | |
| Wave IV | 3.683 | 3.693 | 3.195 | <0.001 | |
| Key exposures | |||||
| Ever evicted (1=yes) | 0.016 | - | - | - | |
| Evicted in the past 12 months | |||||
| Wave III | 0.008 | - | - | - | |
| Wave IV | 0.009 | - | - | - | |
| Covariates | |||||
| Gender (1=female) | 0.497 | 0.498 | 0.406 | 0.165 | |
| Race | |||||
| White | 0.739 | 0.740 | 0.692 | 0.024 | |
| Black | 0.122 | 0.120 | 0.229 | ||
| Hispanic | 0.108 | 0.109 | 0.043 | ||
| Asian | 0.030 | 0.030 | 0.036 | ||
| Age | |||||
| Wave III | 21.823 | 21.814 | 21.993 | 0.465 | |
| Wave IV | 28.947 | 28.188 | 29.188 | 0.283 | |
| Socioeconomic status | |||||
| Wave I | 0.039 | 0.042 | −0.160 | 0.215 | |
| Wave III | 0.009 | 0.014 | −0.414 | <0.001 | |
| Wave IV | 0.027 | 0.042 | −0.857 | <0.001 | |
| Marital Status (1=married) | |||||
| Wave III | 0.385 | 0.382 | 0.421 | 0.584 | |
| Wave IV | 0.671 | 0.670 | 0.661 | 0.901 | |
| Residential moves | |||||
| Number of moves between Waves I-III | 2.457 | 2.435 | 3.408 | 0.003 | |
| Moved between Waves II-III (1=yes) | 0.193 | 0.196 | 0.148 | 0.470 | |
| Moved between Waves III-IV (1=yes) | 0.139 | 0.140 | 0.166 | 0.668 | |
| Neighborhood economic disadvantage | |||||
| Wave I | 0.834 | 0.827 | 1.407 | <0.001 | |
| Wave III | 0.589 | 0.586 | 0.843 | 0.123 | |
| Wave IV | 0.652 | 0.647 | 1.188 | 0.003 | |
| Perceived social stress (Wave IV) | 4.629 | 4.596 | 7.014 | <0.001 | |
Notes: p-value of difference in means/proportions between never evicted and ever evicted individuals; two-tailed test.
4.2. Depressive Symptoms
Results of the negative binomial models regressing depressive symptoms at Wave IV on eviction history and the covariates are in Table 2. Results from Model 1, the basic adjusted model, show a positive association between eviction history and depressive risk (β=0.565, p<0.001), where individuals who report experiencing eviction at Waves III and/or IV have more depressive symptoms than those who did not report eviction. Model 2 builds on Model 1 by further adjusting for SES at Waves I, III, and IV, marital status at Waves III and IV, and number of residential moves between Waves I and III. Adjusting for these factors attenuates, but does not eliminate, the magnitude of the coefficient estimate for eviction in Model 2 over Model 1. Model 3 builds on Model 2 by including measures of neighborhood economic disadvantage, which does little to change the estimate for eviction over Model 2. Model 4 further adjusts for perceived social stress, which is strongly associated with depressive symptoms (β=0.158, p<0.001). Adjusting for perceived social stress in Model 4 attenuates the coefficient estimate for eviction over Model 3, providing suggestive evidence that perceived stress may mediate the association between eviction and depressive risk. Finally, Model 5 is the fully adjusted model that also includes a measure of depressive symptoms from Wave III. Results from Model 5 show that eviction history is associated with higher levels of depressive symptoms at Wave IV, net of baseline depressive symptoms at Wave III.
Table 2.
Associations between Eviction History and Depressive Risk: Generalized Linear Models (Add Health, 1994–2008) (n=5,934)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Basic Coeff. (SE) | + SES & Fam. Context Coeff. (SE) | + Neigh. SES Coeff. (SE) | + Perceived Stress Coeff. (SE) | + Baseline CESD Coeff. (SE) | |
| Ever evicted (1=yes) | 0.565*** (0.070) |
0.333*** (0.053) |
0.334*** (0.052) |
0.131** (0.046) |
0.115* (0.054) |
| Gender (1=female) | 0.177*** (0.027) |
0.190*** (0.027) |
0.190*** (0.027) |
0.095*** (0.022) |
0.064** (0.020) |
| Race (White is ref.) | |||||
| Black | 0.217*** (0.034) |
0.136*** (0.032) |
0.134** (0.040) |
0.125** (0.038) |
0.098* (0.038) |
| Hispanic | 0.120** (0.044) |
0.080 (0.048) |
0.080 (0.051) |
0.077* (0.030) |
0.050 (0.029) |
| Asian | 0.308*** (0.072) |
0.249*** (0.071) |
0.251*** (0.071) |
0.161** (0.058) |
0.142* (0.061) |
| Age (years) (Wave IV) | −0.008 (0.008) |
−0.001 (0.008) |
−0.001 (0.008) |
−0.000 (0.006) |
0.000 (0.006) |
| Socioeconomic status | |||||
| Wave I | −0.049* (0.019) |
−0.049** (0.018) |
−0.037* (0.014) |
−0.033* (0.013) |
|
| Wave III | −0.053* (0.022) |
−0.053* (0.022) |
−0.029 (0.020) |
−0.023 (0.020) |
|
| Wave IV | −0.187*** (0.021) |
−0.187*** (0.022) |
−0.045* (0.017) |
−0.031 (0.017) |
|
| Marital status (1=married) | |||||
| Wave III | −0.021 (0.028) |
−0.019 (0.028) |
−0.029 (0.020) |
−0.006 (0.020) |
|
| Wave IV | −0.093*** (0.025) |
−0.092*** (0.025) |
−0.050* (0.022) |
−0.053* (0.021) |
|
| Number of residential moves between Waves I-III | 0.031*** (0.006) |
0.031*** (0.006) |
0.015** (0.005) |
0.013** (0.005) |
|
| Neighborhood economic disadvantage | |||||
| Wave I | −0.009 (0.011) |
−0.016 (0.009) |
−0.012 (0.009) |
||
| Wave III | 0.012 (0.013) |
0.030** (0.011) |
0.031** (0.011) |
||
| Wave IV | 0.002 (0.015) |
−0.005 (0.010) |
−0.007 (0.009) |
||
| Perceived stress scale (Wave IV) | 0.158*** (0.003) |
0.144*** (0.003) |
|||
| Depressive symptoms (Wave III) | 0.034*** (0.002) |
||||
| Intercept | 1.693*** (0.227) |
1.480*** (0.225) |
1.469*** (0.228) |
0.684*** (0.189) |
0.598** (0.186) |
Notes: Results of negative binomial regression models. Coefficients and standard errors presented. Outcome measured at Wave IV. All models adjust for survey design effects and attrition using sampling weights.
p<0.001,
p<0.01,
p<0.05
Results from Model 4 of Table 2 suggested that perceived social stress may mediate the link between eviction and depressive symptoms. As described, to formally test this, we used parametric regression models for causal mediation analysis (Emsley & Liu, 2013; Valeri & VanderWeele, 2013). Results from the mediation analyses showed a highly statistically significant indirect effect of perceived social stress, with approximately 17.48 percent of the total effect of eviction history on depressive risk operating indirectly through perceived stress (p<0.001).
In the next stage of multivariable analyses, we used a similar prospective regression design to model the association between eviction history and the outcomes at Wave IV, but this time use inverse probability of treatment weighting with regression adjustment to better account for potential selection and confounding in the association between eviction and depressive risk. This method involves calculating propensity scores for respondents, which indicate the probability of eviction conditional on a set of covariates: race-ethnicity, gender, age, family SES at Wave I, total number of residential moves between Waves I and III, and neighborhood socioeconomic conditions at Wave I. Then, the propensity scores are used to weight observations and create a new pseudo-population where the likelihood of eviction was no longer confounded by the covariates. We also used a regression adjustment estimator to model depressive symptoms using negative binomial regression adjusting for: race-ethnicity; gender; age; SES at Waves I, III, and IV; marital status at Waves III and IV; total number of residential moves between Waves I and III; neighborhood socioeconomic conditions at Waves I, III, and IV; and perceived social stress. Analyses revealed that the covariates predicting eviction were balanced after implementing the IPTW model, indicating that the implementation of the IPTWs balanced covariate histories across the “evicted” and “never evicted” groups as intended. Using IPTW with regression adjustment, we documented a strong association between eviction history and depressive symptoms at Wave IV. We summarize results from the IPTW model in Figure 2, which shows the predicted number of depressive symptoms among respondents who were never evicted and those who reported eviction at Waves III and/or IV using estimates from the IPTW model. Compared to those who were never evicted, respondents reporting recent eviction had greater depressive risk (β=0.914, p=0.003).
Figure Two.

Predicted number of depressive symptoms at Wave IV based on model using inverse probability of treatment weighting with a regression adjustment estimator. n=5,394. The model predicting the “treatment” (e.g., ever reporting eviction) includes measures of respondent race-ethnicity, gender, and age; family SES at Wave I; total number of residential moves between Waves I and III; and the measure of neighborhood socioeconomic conditions at Wave I. The model of the outcome (depressive symptoms) includes race-ethnicity; gender; age; SES at Waves I, III, and IV; marital status at Waves III and IV; total number of residential moves between Waves I and III; neighborhood socioeconomic conditions at Waves I, III, and IV; and perceived social stress.
Finally, Table 3 provides results of the longitudinal first difference models where we modeled change in depressive risk from Wave III to IV as a function of change in eviction status and the covariates. Model 1 of Table 3 shows a strong, positive association between changes in eviction and changes in depressive risk (β=0.139, p<0.021), such that those who experienced eviction between Waves III and IV saw increases in depressive symptoms. Model 2 further adjusts for changes in socioeconomic status and marital status across waves, which are not associated with changes in depressive risk. Finally, Models 3 and 4 include changes in neighborhood conditions and changes in residence (e.g., residential moves), respectively, which are not associated with changes in depressive symptoms. The parameter estimate for eviction in Model 4 of Table 3, which is the fully adjusted model, indicates a positive association between changes in eviction and changes in depressive symptoms that is largely consistent with estimates across Models 1–4.
Table 3.
Change in Eviction Status and Change in Depressive Risk: First Difference Models (Add Health, 2001–2008) (n=9,029)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Basic Coeff. (SE) | + SES & Fam. Context Coeff. (SE) | + Neigh. SES Coeff. (SE) | + Moves Coeff. (SE) | |
| Δ Eviction | 0.139* (0.060) |
0.135* (0.060) |
0.135* (0.060) |
0.136* (0.060) |
| Δ Age (years) | 0.022*** (0.001) |
0.023*** (0.001) |
0.024*** (0.001) |
0.024** (0.001) |
| Δ Socioeconomic status | −0.020 (0.013) |
−0.020 (0.013) |
−0.020 (0.013) |
|
| Δ Marital status (1=married) | −0.030 (0.016) |
−0.030 (0.016) |
−0.028 (0.016) |
|
| Δ Neighborhood economic disadvantage | −0.003 (0.008) |
−0.003 (0.008) |
||
| Δ Residence (1=moved) | 0.015 (0.018) |
|||
| Number of respondents | 9,201 | 9,201 | 9,201 | 9,201 |
| Number of observations | 18,402 | 18,402 | 18,402 | 18,402 |
Notes: Results from first difference models; coefficient estimates indicate how changes in the independent variables (“Δ x”) correspond to changes in depressive symptoms (“Δ y”).
p<0.001,
p<0.01,
p<0.05
4.3. Self-Rated Health
Table 4 includes results of the ordinal logistic regression models for the self-rated health outcome. Consistent with the depressive risk models, results from Model 1 of Table 4 reveal a positive association between eviction history and poor/fair self-rated health (β=−1.138, p<0.001), with individuals who reported eviction having worse self-rated health compared to those who did not report eviction. In Model 2, we adjust for SES across waves, marital status, and residential moves from adolescence though emerging adulthood. In Model 2, SES at Waves I and IV is strongly associated with self-rated health. Including the measures of SES and family context attenuates but does not eliminate the association between eviction and self-rated health. Model 3 adjusts for neighborhood economic conditions at Waves I, III, and IV, which are not associated with self-rated health net of the other covariates. Model 4 adjusts for perceived social stress, which is strongly associated with depressive symptoms (β=−0.136, p<0.001). Adjusting for perceived social stress in Model 4 fully attenuates the coefficient estimate for eviction. Finally, Model 5 is the fully adjusted model that also includes a measure of self-rated health from Wave III. The coefficient estimate for eviction remains statistically insignificant in Model 5.
Table 4.
Associations between Eviction History and Self-Rated Health: Generalized Linear Models (Add Health, 1994–2008) (n=5,934)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Basic Coeff. (SE) | + SES & Fam. Context Coeff. (SE) | + Neigh. SES Coeff. (SE) | + Perceived Stress Coeff. (SE) | + Baseline Health Coeff. (SE) | |
| Ever evicted (1=yes) | −1.138*** (0.304) |
−0.656* (0.319) |
−0.638* (0.321) |
−0.448 (0.302) |
−0.566 (0.293) |
| Gender (1=female) | −0.113 (0.061) |
−0.141* (0.062) |
−0.142* (0.062) |
−0.069 (0.063) |
0.019 (0.062) |
| Race (White is ref.) | |||||
| Black | −0.289** (0.089) |
−0.050 (0.094) |
0.032 (0.108) |
0.053 (0.104) |
−0.001 (0.120) |
| Hispanic | −0.471*** (0.124) |
−0.310* (0.123) |
−0.275* (0.125) |
−0.271* (0.127) |
−0.283* (0.131) |
| Asian | −0.586*** (0.162) |
−0.379* (0.166) |
−0.350* (0.169) |
−0.274 (0.165) |
−0.201 (0.180) |
| Age (years) (Wave IV) | −0.007 (0.021) |
−0.035 (0.019) |
−0.034 (0.019) |
−0.039* (0.019) |
−0.022 (0.018) |
| Socioeconomic status | |||||
| Wave I | 0.163*** (0.045) |
0.147** (0.045) |
0.150*** (0.044) |
0.106* (0.048) |
|
| Wave III | 0.103 (0.059) |
0.099 (0.059) |
0.085 (0.059) |
0.022 (0.059) |
|
| Wave IV | 0.518*** (0.062) |
0.508*** 0.062) |
0.396*** (0.062) |
0.314*** (0.065) |
|
| Marital status (1=married) | |||||
| Wave III | −0.029 (0.080) |
−0.018 (0.079) |
−0.012 (0.077) |
−0.062 0.082) |
|
| Wave IV | 0.033 (0.067) |
0.040 (0.068) |
0.001 (0.069) |
−0.033 (0.072) |
|
| Number of residential moves between Waves I-III | −0.001 (0.017) |
−0.004 (0.017) |
0.007 (0.017) |
0.019 (0.018) |
|
| Neighborhood economic disadvantage | |||||
| Wave I | −0.055 (0.030) |
−0.052 (0.028) |
−0.076* (0.029) |
||
| Wave III | 0.005 (0.035) |
−0.009 (0.035) |
0.000 (0.037) |
||
| Wave IV | −0.006 (0.038) |
0.001 (0.039) |
0.017 (0.042) |
||
| Perceived stress scale (Wave IV) | −0.136*** (0.012) |
−0.107*** (0.012) |
|||
| Self-rated health (Wave III) | 0.900*** (0.045) |
||||
Notes: Results of ordinal logistic regression models. Self-rated health coded so that 1=poor and 5=excellent. Outcome measured at Wave IV. All models adjust for survey design effects and attrition using sampling weights.
p<0.001,
p<0.01,
p<0.05
Results from Model 4 of Table 4 provided suggestive evidence that perceived stress may mediate the association between eviction and self-rated health, and we again used parametric regression models for causal mediation analysis to formally test for mediation. However, in models testing for potential mediation, the estimate of the direct effect of eviction was not statistically significant, so the mediation test failed to achieve statistical significance. Similarly, estimates from the IPTW models also revealed no statistically significant (p<0.05) association between eviction and self-rated health, so results are excluded from the final paper. The parameter estimate for eviction in the longitudinal first difference models of self-rated health were also not statistically significant and thus excluded from final results.
5. Discussion
Despite an increase in studies on housing insecurity and health in recent years, studies on the specific health risks associated with eviction are limited, leaving critical gaps in our understanding of the role of eviction in shaping population health unanswered. Of the few studies assessing the health effects of eviction, most rely on cross-sectional data or aggregate population data, which restricts understanding of how the experience of eviction shapes intra-individual trajectories of health over time. Using nationally-representative, longitudinal data, the current study builds on previous research on the links between housing insecurity and health to provide new evidence of whether and how eviction patterns population health risk over time, with particular focus on stress-related pathways linking eviction to health.
5.1. Support for the Study of Eviction as a Unique Stressor
This study provides strong evidence that eviction represents a unique and significant stressor that must be accounted for in studies of health and wellbeing, particularly among low income, urban, and racially marginalized populations. Across a variety of analytic techniques—including prospective lagged dependent variable models, inverse probability of treatment weighted regression models, and longitudinal fixed effects models—we consistently documented significant, positive associations between eviction and changes in depressive risk, in particular. Results from the regression models in Tables 2 and 4 showed prospective associations between eviction history and the outcomes, net of factors like individual and family SES, other markers of residential instability, and neighborhood economic conditions. The estimate of prospective association between eviction and depressive risk was robust to alternative modeling strategies, including inverse probability of treatment weighting. In Table 3, results from the longitudinal first difference models for depressive risk showed that individuals who experienced eviction between survey waves saw increases in depressive symptoms over time. The longitudinal associations between changes in eviction and changes in depressive risk persisted after adjusting for other markers of household and neighborhood socioeconomic conditions as well as additional measures of housing and financial insecurity, which suggests that eviction serves as a particular salient health risk among young adults. By using longitudinal data, prospective regression models, treatment weighting procedures, and fixed effects models, our study advances this literature by using longitudinal data on individuals to reveal how changes in eviction experiences over time shape trajectories of health risk in emerging adulthood.
In addition to examining the prospective and longitudinal links between eviction and health risk, this study also assessed the mechanisms linking eviction to health, paying particular attention to the role of psychosocial stress. Results from Model 4 of Tables 2 and 4 provided suggestive evidence that stress may mediate the associations between eviction and depressive symptoms and self-rated health. To formally test this, we used causal mediation analysis (Emsley & Liu, 2013; Valeri & VanderWeele, 2013) to determine the proportion of the total effect of eviction history on the outcomes that is mediated by perceived social stress. Results from these models revealed strong indirect effects of psychosocial stress on depressive risk, in particular, with a sizable proportion (nearly one-fifth) of the total effect of eviction on depressive risk operating through perceived social stress. These results provided support for the notion that eviction is a salient stressor in the lives of young adults. Evictions were associated with increases in perceived social stress among young people, with important consequences for health risk. Previous research shows that eviction can affect health through environmental and physical exposures (Desmond, 2012) and by increasing exposure and vulnerability to communicable diseases (Leifheit & Jennings, 2019; Niccolai et al., 2019) as described in Figure 1. Our results show that stress is also an important pathway linking eviction to health. It is likely that the many primary and secondary stressors associated with eviction—which can include the many strains and challenges of finding and securing housing, the difficulties in navigating the many bureaucratic and administrative burdens associated with eviction, disruptions to schooling, employment, or social ties that result from eviction—upregulate and exhaust psychological functioning in ways that erode health over time.
Finally, our focus on the emerging adulthood period of the life course offers an important contribution to the literature on housing insecurity. Much of the previous work focuses on families with children and adults, with very few studies examining the effects eviction during the emerging and young adulthood. Early adulthood is a particularly important time for psychological and financial development, with social exposures during this period having lasting implications for lifetime financial status and wellbeing (Arnett, 2000, 2006; Nelson, 2020). In this way, experiencing a social, emotionally, and financially impactful event such as eviction during this period may have especially important consequences for future health and well-being. Our results indicate that stress and depression pathways represent a key mechanism through which eviction impacts young adults which makes sense given both the primary and aforementioned secondary stressors associated with eviction. Taken together, our results provide new evidence of the links between eviction, stress, and health during a critical, but largely understudied, life course stage.
5.2. Who Gets Evicted?
Importantly, estimates provided in Table 1 are consistent with previous research showing stark social inequalities in eviction. We found that Black young people experience a disproportionate burden of eviction when compared to their white counterparts in this study. While Black youth made up just 12% of the sample, they accounted for nearly a quarter of the reported evictions. These findings are consistent with recent studies from Washington (Thomas et al., 2019) and Virginia (Teresa, 2018), which found that eviction rates were disproportionately high among Black and Latinx populations. Another report from Milwaukee revealed that Black women with children made up 9.6% of renters but accounted for 30% of evictions (Desmond, 2014). Taken together, findings from all of these studies suggest that eviction represents a major issue for Black populations, with particularly devastating consequences for Black youth and children.
Housing insecurity and unequal access to quality housing has been a major source of racial health and economic disparities in the United States for centuries (Bianchi et al., 1982; Flippen, 2001; Kurtulus, 2019; Pager & Shepherd, 2008; Zenou & Boccard, 2000). Practices such as housing segregation and redlining have long been implicated in racial inequalities in the US (Jacoby et al., 2018; McClure et al., 2019). This study suggests that eviction not only perpetuates racial inequality in a general sense, but may also contribute to racial health disparities. In this way, evictions may represent a critical pathway linking structural and institutional racism to population health inequities. Amidst growing levels of economic inequality, stark and persistent levels of racial residential segregation, and rapid gentrification across many urban areas in the U.S., population health scholars should continue to investigate the role of eviction in producing racial health inequities.
Results from our study also indicate that important socioeconomic disparities exist when it comes to eviction. Individuals with lower SES and those who lived in more economically disadvantaged neighborhoods during adolescence and young adulthood were more likely to report eviction. These findings are consistent with previous research that indicates that lower SES neighborhoods exhibit higher rates of eviction (Desmond & Shollenberger, 2015). In this way, evictions may serve as both a cause and consequence of economic insecurity and a source of population-level socioeconomic health inequality.
5.3. Limitations of Study
This study has several limitations that should be addressed in future research. First, we are unable to test for longitudinal mediation of perceived stress since it was only measured once in Wave IV. While we found cross-sectional evidence that perceived stress mediated the prospective association between eviction and depressive symptoms, we were unable to assess these links across time with multiple measures of perceived stress. Future research efforts should consider examining how longitudinal changes in perceived stress may mediate or alter the relationship between eviction and mental health outcomes. As longitudinal data on evictions, stress, and health become available, our ability to make causal inferences will only be improved. Another limitation of this study is the timing of the measurement of eviction. The survey only measured eviction in the past 12 months rather than recording lifetime eviction experiences. Future studies should aim to capture more detailed eviction histories that may reveal the impact of multiple evictions as well as the recovery or wash out period of the effects of experiencing an eviction. Research in this area should build on the findings here to also test for differential vulnerability to evictions by continuing to test for moderation by race-ethnicity, gender, and other dimensions of social context and stratification, as various social, economic, and household conditions may make the experience of eviction more or less stressful for individuals.
While we were able to examine the relationship between eviction and mental health outcomes as well as self-reported health, we were unable to assess how eviction related to biomarkers of physiological functioning over time as the Add Health study only included cross-sectional biomarker data at the time of this study. Given the role of perceived stress in producing poor mental health outcomes in association with eviction, future studies of eviction would greatly benefit from the inclusion of stress related biomarkers that can elucidate the specific biological pathways through with the experience of eviction “gets under the skin” to impact health and wellbeing. Results from our self-rated health models were less robust than those modeling depressive risk. This may reflect the lagged nature of the associations between eviction and markers of physical health and functioning, which may take longer to manifest than mental health impacts. The use of biomarkers can help document the initial impacts of eviction but longitudinal collection of such biomarkers may reveal the lagged and lasting impacts of eviction.
Additionally, because of data limitations, we are unable to distinguish between the effects of eviction within the context of renting versus foreclosure. There is a large body of research linking foreclosure and health, but less research on the health effects of eviction among renters. Still, renters and homeowners may face differential health risk as a consequence of housing loss. As such, future research should distinguish the effects of rent eviction from foreclosure.
Finally, it is worth noting that while we have found a significant relationship between eviction in this population and depression, this study likely offers a significant underestimation of those affected by eviction. Individuals facing housing insecurity are less likely to participate in studies such as Add Health. If they do participate, the instability of residence may lead them to be lost to follow up. Future studies should consider creative research designs that allow for the inclusion and follow-up of housing insecure participants. While the prospective study of eviction may be extremely challenging, such a design would greatly enhance our ability to examine the specific effects of eviction on health and wellbeing.
5.4. Future Research
Considering the frequency and scale of eviction in the US, population health research should continue to examine the causes and consequences of eviction. While a large and growing body of research assess the impacts foreclosure, particularly in the wake of the 2008 financial crisis, only a handful of studies examine or have included the effects of forced movement among renters. This dearth of research is even more significant given the economic fallout from the COVID-19 pandemic which is ongoing at the time of this writing. The recent CDC eviction moratorium lasts only through the end of the year and does not absolve the tenant from paying rent or restrict landlords from applying penalties, interest, or late fees on the tenant’s account for non-payment of rent. Further, it does not prevent landlords from evicting tenants for other violations including damaging or posing an immediate and significant risk of property damage and failing to meet any non-rent or fee related contractual obligation, among others. Thus, while the immediate threat of eviction for failure to pay rent may have subsided for the time being, the solution is incomplete and temporary, leaving the door open for predatory landlords to continue with evictions under the guise of other violations. Without more significant actions, we are likely to see massive evictions as soon as the moratorium lapses resulting from unpaid back rent. Further, we are likely to see additional increases in the rising foreclosure rates associated with unemployment and the ongoing economic fallout of COVID-19 (Centopani, 2020).
Given the potential scope of the coming eviction crisis, understanding the effects of eviction are now more important than ever. As of the time of this writing, researchers have already demonstrated a link between lifting eviction moratoriums and increases in COIVD-19 incidence and mortality (Leifheit et al., 2020). However, the possible health impacts of this potential wave of evictions go far beyond our immediate health crisis. While this analysis has examined just one potential pathway by which eviction can impact health, Figure 1 indicates other pathways that can and should be examined in future research. Further, in order to more effectively assess the impacts of eviction, prospective studies should seek to follow at risk families through the process of eviction in order to document its repercussions via these multiple pathways. Prospective studies of eviction may shed light on which parts of the eviction process are most harmful, thereby illuminating effective intervention points. Another future research direction includes the consideration of the variable effects of eviction across the life course. It is highly likely that the health effects of eviction may be variable depending on the age of the individual. Different pathways may be more or less frequently activated at different stages of the life course. For example, psychosocial stress leading to poorer mental health outcomes may have more significant effects among adolescents, young adults, and adults who may be more conscious of eviction struggles and thus more likely to ruminate or experience stigma. On the other hand, infants and children may be more vulnerable to environmental or disease exposures resulting from eviction due to their immature immune systems and biological sensitivity to environmental influences.
6. Conclusion
This study is one of relatively few to examine the impacts of eviction on the health and wellbeing of young people as they age from adolescence to young adulthood. Taken together, results indicated that the experience of eviction represents a significant stressor that is associated with declines in mental and self-reported health outcomes as young people age. Importantly, increased perceived psychosocial stress represents a critical pathway through which the experience of eviction increases health risk among individuals who have reported experiencing recent eviction. Additional research, especially longitudinal and prospective studies, are necessary to better elucidate the effects of eviction on health. The potential for a massive eviction crisis in the U.S. resulting from the ongoing economic crisis associated with the COVID-19 pandemic, makes the need for greater research more pressing than ever. Future studies should seek to examine other potential pathways through which eviction may affect health as well as consider the potentially variable impacts of eviction across the life course so that policy and intervention efforts can be best targeted to prevent population health impacts.
Highlights.
Eviction represents a major public health issue
Eviction is associated with increased depressive risk over time in young adults
Eviction represents a unique stressor even when confounding factors are considered
Stress mediates the association between eviction and depressive symptoms
Acknowledgements
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Information on how to obtain the Add Health data files is available on the Add Health website (https://addhealth.cpc.unc.edu/). No direct support was received from grant P01-HD31921 for this analysis. The authors are grateful to the Population Studies Center at the University of Pennsylvania (National Institutes of Health’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH Grant No. R24 HD044964) and the Axilrod Faculty Fellowship program at the University of Pennsylvania for general support. The authors wish to acknowledge the work of several students including Nicole da Costa, Junduo Liu, and Nicole Mayer, who aided in reviewing literature cited throughout this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alley DE, Lloyd J, Pagán JA, Pollack CE, Shardell M, & Cannuscio C (2011). Mortgage Delinquency and Changes in Access to Health Resources and Depressive Symptoms in a Nationally Representative Cohort of Americans Older Than 50 Years. American Journal of Public Health, 101(12), 2293–2298. 10.2105/AJPH.2011.300245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison PD (1990). Change Scores as Dependent Variables in Regression Analysis. Sociological Methodology, 20, 93–114. JSTOR. 10.2307/271083 [DOI] [Google Scholar]
- Allison PD (1994). Using panel data to estimate the effects of events. Sociological Methods & Research, 23(2), 174–199. [Google Scholar]
- Arcaya MC (2017). Invited Commentary: Foreclosures and Health in a Neighborhood Context. American Journal of Epidemiology, 185(6), 436–439. 10.1093/aje/kww169 [DOI] [PubMed] [Google Scholar]
- Aneshensel Carol S., Rutter Carolyn M., and Lachenbruch Peter A. 1991. “Social Structure, Stress, and Mental Health: Competing Conceptual and Analytic Models.” American Sociological Review 56(2):166–178. 10.2307/2095777. [DOI] [Google Scholar]
- Arcaya M, Glymour MM, Chakrabarti P, Christakis NA, Kawachi I, & Subramanian SV (2013). Effects of Proximate Foreclosed Properties on Individuals’ Weight Gain in Massachusetts, 1987–2008. American Journal of Public Health, 103(9), e50–e56. 10.2105/AJPH.2013.301460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2006). Emerging Adulthood: Understanding the New Way of Coming of Age. In Emerging adults in America: Coming of age in the 21st century (pp. 3–19). American Psychological Association. 10.1037/11381-001 [DOI] [Google Scholar]
- Arnio AN, Baumer EP, & Wolff KT (2012). The contemporary foreclosure crisis and US crime rates. Social Science Research, 41(6), 1598–1614. 10.1016/j.ssresearch.2012.05.013 [DOI] [PubMed] [Google Scholar]
- Aro S, & Hanninen V (1984). Life events or life processes as determinants of mental strain? A 5-year follow-up study. Social Science & Medicine, 18(12), 1037–1044. 10.1016/0277-9536(84)90162-X [DOI] [PubMed] [Google Scholar]
- Badiaga S, Raoult D, & Brouqui P (2008). Preventing and Controlling Emerging and Reemerging Transmissible Diseases in the Homeless. Emerging Infectious Diseases, 14(9), 1353–1359. 10.3201/eid1409.082042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir SA (2002). Home Is Where the Harm Is: Inadequate Housing as a Public Health Crisis. American Journal of Public Health, 92(5), 733–738. 10.2105/AJPH.92.5.733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benfer E, Robinson DB, Butler S, Edmonds L, Gilman S, McKay KL, Neumann Z, Owens L, Steinkamp N, & Yentel D (2020, August 7). The COVID-19 Eviction Crisis: An Estimated 30–40 Million People in America Are at Risk. Aspen Institute. https://www.aspeninstitute.org/blog-posts/the-covid-19-eviction-crisis-an-estimated-30-40-million-people-in-america-are-at-risk/
- Bernal-Solano M, Bolívar-Muñoz J, Mateo-Rodríguez I, Robles-Ortega H, Fernández-Santaella M. del C., Mata-Martín JL, Vila-Castellar J, & Daponte-Codina A (2019). Associations between Home Foreclosure and Health Outcomes in a Spanish City. International Journal of Environmental Research and Public Health, 16(6), 981. 10.3390/ijerph16060981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi SM, Farley R, & Spain D (1982). Racial inequalities in housing: An examiation of recent trends. Demography, 19(1), 37–51. 10.2307/2061127 [DOI] [PubMed] [Google Scholar]
- Blair C, Raver C, Granger D, Mills-Koonce R, & Hibel L (2011). Allostasis and Allostatic Load in the Context of Poverty in Early Childhood. Development and Psychopathology, 23(3), 845–857. 10.1017/S0954579411000344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen CE, Kozlowski K, & Tyson KD (2020). “Toxic” schools? How school exposures during adolescence influence trajectories of health through young adulthood. SSM - Population Health, 11, 100623. 10.1016/j.ssmph.2020.100623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottino CJ, Fleegler EW, Cox JE, & Rhodes ET (2019). The Relationship Between Housing Instability and Poor Diet Quality Among Urban Families. Academic Pediatrics, 19(8), 891–898. 10.1016/j.acap.2019.04.004 [DOI] [PubMed] [Google Scholar]
- Brewis AA (2014). Stigma and the perpetuation of obesity. Social Science & Medicine, 118, 152–158. 10.1016/j.socscimed.2014.08.003 [DOI] [PubMed] [Google Scholar]
- Burgard SA, Seefeldt KS, & Zelner S (2012). Housing instability and health: Findings from the Michigan recession and recovery study. Social Science & Medicine, 75(12), 2215–2224. 10.1016/j.socscimed.2012.08.020 [DOI] [PubMed] [Google Scholar]
- Cagney KA, Browning CR, Iveniuk J, & English N (2014). The Onset of Depression During the Great Recession: Foreclosure and Older Adult Mental Health. American Journal of Public Health, 104(3), 498–505. 10.2105/AJPH.2013.301566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centopani P (2020, November 10). Rise in mortgage foreclosures reflects unemployment, COVID-19 woes. National Mortgage News. https://www.nationalmortgagenews.com/news/rise-in-mortgage-foreclosures-reflects-unemployment-covid-19-woes [Google Scholar]
- Chan KS, Roberts E, McCleary R, Buttorff C, & Gaskin DJ (2014). Community Characteristics and Mortality: The Relative Strength of Association of Different Community Characteristics. American Journal of Public Health, 104(9), 1751–1758. 10.2105/AJPH.2014.301944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A Global Measure of Perceived Stress. Journal of Health and Social Behavior, 24(4), 385–396. JSTOR. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cook TB, & Davis MS (2012). Assessing Legal Strains and Risk of Suicide Using Archived Court Data. Suicide and Life-Threatening Behavior, 42(5), 495–506. 10.1111/j.1943-278X.2012.00107.x [DOI] [PubMed] [Google Scholar]
- Damon W, McNeil R, Milloy M-J, Nosova E, Kerr T, & Hayashi K (2019). Residential eviction predicts initiation of or relapse into crystal methamphetamine use among people who inject drugs: A prospective cohort study. Journal of Public Health, 41(1), 36–45. 10.1093/pubmed/fdx187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deaton AS, & Paxson CH (1998). Aging and Inequality in Income and Health. The American Economic Review, 88(2), 248–253. JSTOR. [Google Scholar]
- Desmond M (2012). Eviction and the Reproduction of Urban Poverty. American Journal of Sociology, 118(1), 88–133. 10.1086/666082 [DOI] [Google Scholar]
- Desmond M (2014). Poor Black Women Are Evicted at Alarming Rates, Setting Off a Chain of Hardship (Why Housing Matters, p. 4) [Policy Research Brief]. MacArthur Foundation. [Google Scholar]
- Desmond M (2015). Unaffordable America: Poverty, Housing, and Eviction. Fast Focus: Institue for Research on Poverty, 22(22), 1–6. [Google Scholar]
- Desmond M, Gromis A, Edmonds L, Krywokulski K, Leung L, & Porton A (2018). Eviction Lab National Database: Version 1.0. Princeton: Princeton University. https://evictionlab.org/ [Google Scholar]
- Desmond M, & Kimbro RT (2015). Eviction’s Fallout: Housing, Hardship, and Health. Social Forces, 94(1), 295–324. 10.1093/sf/sov044 [DOI] [Google Scholar]
- Desmond M, & Shollenberger T (2015). Forced Displacement From Rental Housing: Prevalence and Neighborhood Consequences. Demography, 52(5), 1751–1772. 10.1007/s13524-015-0419-9 [DOI] [PubMed] [Google Scholar]
- Emsley R, & Liu H (2013). PARAMED: Stata module to perform causal mediation analysis using parametric regression models. https://econpapers.repec.org/software/bocbocode/s457581.htm
- Flippen CA (2001). Racial and Ethnic Inequality in Homeownership and Housing Equity. The Sociological Quarterly, 42(2), 121–149. 10.1111/j.1533-8525.2001.tb00028.x [DOI] [Google Scholar]
- Fowler KA, Gladden RM, Vagi KJ, Barnes J, & Frazier L (2014). Increase in Suicides Associated With Home Eviction and Foreclosure During the US Housing Crisis: Findings From 16 National Violent Death Reporting System States, 2005–2010. American Journal of Public Health, 105(2), 311–316. 10.2105/AJPH.2014.301945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopinth G (2020, April 14). The Great Lockdown: Worst Economic Downturn Since the Great Depression. IMF Blog. https://blogs.imf.org/2020/04/14/the-great-lockdown-worst-economic-downturn-since-the-great-depression/
- Grainger GL (2020). “It’s Not a Pattern of Behavior”: Proxy Deflection of Eviction Stigma by Community Care Providers. Symbolic Interaction, symb.511. 10.1002/symb.511 [DOI]
- Gunasekara FI, Richardson K, Carter K, & Blakely T (2014). Fixed effects analysis of repeated measures data. International Journal of Epidemiology, 43(1), 264–269. 10.1093/ije/dyt221 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & Pachankis JE (2016). Stigma and Minority Stress as Social Determinants of Health Among Lesbian, Gay, Bisexual, and Transgender Youth: Research Evidence and Clinical Implications. Pediatric Clinics, 63(6), 985–997. 10.1016/j.pcl.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, & Link BG (2013). Stigma as a Fundamental Cause of Population Health Inequalities. American Journal of Public Health, 103(5), 813–821. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazekamp C, Yousuf S, Day K, Daly MK, & Sheehan K (2020). Eviction and Pediatric Health Outcomes in Chicago. Journal of Community Health, 45(5), 891–899. 10.1007/s10900-020-00806-y [DOI] [PubMed] [Google Scholar]
- Hirschl TA, & Rank MR (2010). Homeownership Across the American Life Course: Estimating the Racial Divide. Race and Social Problems, 2(3–4), 125–136. 10.1007/s12552-010-9033-z [DOI] [Google Scholar]
- Houle JN (2014). Mental health in the foreclosure crisis. Social Science & Medicine, 118, 1–8. 10.1016/j.socscimed.2014.07.054 [DOI] [PubMed] [Google Scholar]
- Houle JN, & Light MT (2014). The Home Foreclosure Crisis and Rising Suicide Rates, 2005 to 2010. American Journal of Public Health, 104(6), 1073–1079. 10.2105/AJPH.2013.301774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbs-Tait L, Nation JR, Krebs NF, & Bellinger DC (2005). Neurotoxicants, Micronutrients, and Social Environments: Individual and Combined Effects on Children’s Development. Psychological Science in the Public Interest, 6(3), 57–121. 10.1111/j.1529-1006.2005.00024.x [DOI] [PubMed] [Google Scholar]
- Idler EL, & Benyamini Y (1997). Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior, 38(1), 21–37. JSTOR. 10.2307/2955359 [DOI] [PubMed] [Google Scholar]
- Jacobs DE (2011). Environmental Health Disparities in Housing. American Journal of Public Health, 101(S1), S115–S122. 10.2105/AJPH.2010.300058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacoby SF, Dong B, Beard JH, Wiebe DJ, & Morrison CN (2018). The enduring impact of historical and structural racism on urban violence in Philadelphia. Social Science & Medicine, 199, 87–95. 10.1016/j.socscimed.2017.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jylhä M (2009). What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science & Medicine, 69(3), 307–316. 10.1016/j.socscimed.2009.05.013 [DOI] [PubMed] [Google Scholar]
- Jylhä M, Volpato S, & Guralnik JM (2006). Self-rated health showed a graded association with frequently used biomarkers in a large population sample. Journal of Clinical Epidemiology, 59(5), 465–471. 10.1016/j.jclinepi.2005.12.004 [DOI] [PubMed] [Google Scholar]
- Kennedy MC, Kerr T, McNeil R, Parashar S, Montaner J, Wood E, & Milloy M-J (2017). Residential Eviction and Risk of Detectable Plasma HIV-1 RNA Viral Load Among HIV-Positive People Who Use Drugs. AIDS and Behavior, 21(3), 678–687. 10.1007/s10461-016-1315-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, & Glaser R (2002). Depression and immune function: Central pathways to morbidity and mortality. Journal of Psychosomatic Research, 53(4), 873–876. 10.1016/S0022-3999(02)00309-4 [DOI] [PubMed] [Google Scholar]
- Kingsbury AM, Plotnikova M, Clavarino A, Mamun A, & Najman JM (2018). Social adversity in pregnancy and trajectories of women’s depressive symptoms: A longitudinal study. Women and Birth, 31(1), 52–58. 10.1016/j.wombi.2017.06.016 [DOI] [PubMed] [Google Scholar]
- Krieger J, & Higgins DL (2002). Housing and Health: Time Again for Public Health Action. American Journal of Public Health, 92(5), 758–768. 10.2105/AJPH.92.5.758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtulus FA (2019). The color of law: The forgotten history of how our government segregated America. Labor History, 60(2), 162–163. 10.1080/0023656X.2019.1534318 [DOI] [Google Scholar]
- Kwong WT, Friello P, & Semba RD (2004). Interactions between iron deficiency and lead poisoning: Epidemiology and pathogenesis. Science of The Total Environment, 330(1), 21–37. 10.1016/j.scitotenv.2004.03.017 [DOI] [PubMed] [Google Scholar]
- Leifheit KM, & Jennings JM (2019). Eviction as a social determinant of sexual health outcomes. Sexually Transmitted Diseases, 46(1), 69–71. 10.1097/OLQ.0000000000000936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leifheit KM, Linton SL, Raifman J, Schwartz G, Benfer EA, Zimmerman FJ, & Pollack C (2020). Expiring Eviction Moratoriums and COVID-19 Incidence and Mortality (SSRN Scholarly Paper ID 3739576). Social Science Research Network. 10.2139/ssrn.3739576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leifheit KM, Schwartz GL, Pollack CE, Black MM, Edin KJ, Althoff KN, & Jennings JM (2020). Eviction in early childhood and neighborhood poverty, food security, and obesity in later childhood and adolescence: Evidence from a longitudinal birth cohort. SSM - Population Health, 11, 100575. 10.1016/j.ssmph.2020.100575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levander OA (1979). Lead toxicity and nutritional deficiencies. Environmental Health Perspectives, 29, 115–125. 10.1289/ehp.7929115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahaffey KR (1995). Nutrition and lead: Strategies for public health. Environmental Health Perspectives, 103(suppl 6), 191–196. 10.1289/ehp.95103s6191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak WWS, Poon CYM, Pun LYK, & Cheung SF (2007). Meta-analysis of stigma and mental health. Social Science & Medicine, 65(2), 245–261. 10.1016/j.socscimed.2007.03.015 [DOI] [PubMed] [Google Scholar]
- Marquez E, Dodge Francis C, & Gerstenberger S (2019). Where I live: A qualitative analysis of renters living in poor housing. Health & Place, 58, 102143. 10.1016/j.healthplace.2019.05.021 [DOI] [PubMed] [Google Scholar]
- Marshall VW, Bengston VL, Gans D, Putney N, & Silverstein M (2009). Theory Informing Public Policy: The Life Course Perspective as a Policy Tool. In Handbook of Theories of Aging (pp. 573–593). Springer. [Google Scholar]
- Martin P, Liaw W, Bazemore A, Jetty A, Petterson S, & Kushel M (2019). Adults with Housing Insecurity Have Worse Access to Primary and Preventive Care. The Journal of the American Board of Family Medicine, 32(4), 521–530. 10.3122/jabfm.2019.04.180374 [DOI] [PubMed] [Google Scholar]
- Mateo-Rodríguez I, Miccoli L, Daponte-Codina A, Bolívar-Muñoz J, Escudero-Espinosa C, Fernández-Santaella MC, Vila-Castellar J, Robles-Ortega H, Mata-Martín JL, & Bernal-Solano M (2019). Risk of suicide in households threatened with eviction: The role of banks and social support. BMC Public Health, 19(1), 1250. 10.1186/s12889-019-7548-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure E, Feinstein L, Cordoba E, Douglas C, Emch M, Robinson W, Galea S, & Aiello AE (2019). The legacy of redlining in the effect of foreclosures on Detroit residents’ self-rated health. Health & Place, 55, 9–19. 10.1016/j.healthplace.2018.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell ED (2012). House poor in Los Angeles: Examining patterns of housing-induced poverty by race, nativity, and legal status. Housing Policy Debate, 22(4), 605–631. 10.1080/10511482.2012.697908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald L (2011). Examining Evictions through a Life-Course Lens. Canadian Public Policy, 37(Supplement 1), S115–S133. 10.3138/cpp.37.suppl.s115 [DOI] [Google Scholar]
- McDonough P, & Amick BC (2001). The social context of health selection: A longitudinal study of health and employment. Social Science & Medicine, 53(1), 135–145. 10.1016/S0277-9536(00)00318-X [DOI] [PubMed] [Google Scholar]
- McEwen BS (1998). Stress, Adaptation, and Disease: Allostasis and Allostatic Load. Annals of the New York Academy of Sciences, 840(1), 33–44. 10.1111/j.1749-6632.1998.tb09546.x [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Nandi A, Keyes KM, Uddin M, Aiello AE, Galea S, & Koenen KC (2012). Home foreclosure and risk of psychiatric morbidity during the recent financial crisis. Psychological Medicine, 42(7), 1441–1448. 10.1017/S0033291711002613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles R, & Jacobs DE (2008). Future Directions in Housing and Public Health: Findings From Europe With Broader Implications for Planners. Journal of the American Planning Association, 74(1), 77–89. 10.1080/01944360701784287 [DOI] [Google Scholar]
- Murphy RD, Zemore SE, & Mulia N (2014). Housing Instability and Alcohol Problems during the 2007–2009 US Recession: The Moderating Role of Perceived Family Support. Journal of Urban Health, 91(1), 17–32. 10.1007/s11524-013-9813-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson LJ (2020). The Theory of Emerging Adulthood 20 Years Later: A Look at Where It Has Taken Us, What We Know Now, and Where We Need to Go. Emerging Adulthood, 2167696820950884. 10.1177/2167696820950884 [DOI]
- Newman SJ, & Holupka CS (2015). Housing Affordability and Child Well-Being. Housing Policy Debate, 25(1), 116–151. 10.1080/10511482.2014.899261 [DOI] [Google Scholar]
- Nguyen Q, Tabor J, Entzel P, Lau Y, Suchindran C, Hussey J, and Whitsel E 2011. “Discordance in National Estimates of Hypertension among Young Adults.” Epidemiology, 22(4), 532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niccolai LM, Blankenship KM, & Keene DE (2019). Eviction from Renter-Occupied Households and Rates of Sexually Transmitted Infections: A County-Level Ecological Analysis. Sexually Transmitted Diseases, 46(1), 63–68. 10.1097/OLQ.0000000000000904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pager D, & Shepherd H (2008). The Sociology of Discrimination: Racial Discrimination in Employment, Housing, Credit, and Consumer Markets. Annual Review of Sociology, 34(1), 181–209. 10.1146/annurev.soc.33.040406.131740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx BWJH (1998). Depressive Symptoms and Physical Decline in Community-Dwelling Older Persons. JAMA, 279(21), 1720. 10.1001/jama.279.21.1720 [DOI] [PubMed] [Google Scholar]
- Pevalin DJ (2009). Housing repossessions, evictions and common mental illness in the UK: Results from a household panel study. Journal of Epidemiology & Community Health, 63(11), 949–951. 10.1136/jech.2008.083477 [DOI] [PubMed] [Google Scholar]
- Pevalin David J., Reeves A, Baker E, & Bentley R (2017). The impact of persistent poor housing conditions on mental health: A longitudinal population-based study. Preventive Medicine, 105, 304–310. 10.1016/j.ypmed.2017.09.020 [DOI] [PubMed] [Google Scholar]
- Pilarinos A, Kennedy MC, McNeil R, Dong H, Kerr T, & DeBeck K (2017). The association between residential eviction and syringe sharing among a prospective cohort of street-involved youth. Harm Reduction Journal, 14(1), 24. 10.1186/s12954-017-0150-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prohaska A, & Lichtenstein B (2014). Losing a Home to Mortgage Foreclosure: Temporary Setback or Chronic Stressor? Social Justice, 40(3 (133)), 65–80. JSTOR. [Google Scholar]
- Robins JM, Hernán MÁ, & Brumback B (2000). Marginal Structural Models and Causal Inference in Epidemiology. Epidemiology, 11(5), 550–560. [DOI] [PubMed] [Google Scholar]
- Robles-Ortega H, Guerra P, González-Usera I, Mata-Martín JL, Fernández-Santaella MC, Vila J, Bolívar-Muñoz J, Bernal-Solano M, Mateo-Rodríguez I, & Daponte-Codina A (2017). Post-Traumatic Stress Disorder Symptomatology in People affected by Home Eviction in Spain. The Spanish Journal of Psychology, 20. 10.1017/sjp.2017.56 [DOI] [PubMed] [Google Scholar]
- Rollings KA, Wells NM, Evans GW, Bednarz A, & Yang Y (2017). Housing and neighborhood physical quality: Children’s mental health and motivation. Journal of Environmental Psychology, 50, 17–23. 10.1016/j.jenvp.2017.01.004 [DOI] [Google Scholar]
- Rosenbaum PR, & Rubin DB (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70(1), 41–55. 10.1093/biomet/70.1.41 [DOI] [Google Scholar]
- Sadowski HS, Ugarte B, Kolvin I, Kaplan CE, & Barnes J (1999). Early life family disadvantages and major depression in adulthood. British Journal of Psychiatry, 174(2), 112–120. 10.1192/bjp.174.2.112 [DOI] [PubMed] [Google Scholar]
- Schootman M, Deshpande AD, Pruitt SL, & Jeffe DB (2012). Neighborhood foreclosures and self-rated health among breast cancer survivors. Quality of Life Research, 21(1), 133–141. 10.1007/s11136-011-9929-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw BA, & Krause N (2002). Exposure to Physical Violence During Childhood, Aging, and Health. Journal of Aging and Health, 14(4), 467–494. 10.1177/089826402237179 [DOI] [PubMed] [Google Scholar]
- Shaw M (2004). Housing and Public Health. Annual Review of Public Health, 25(1), 397–418. 10.1146/annurev.publhealth.25.101802.123036 [DOI] [PubMed] [Google Scholar]
- Singh A, Daniel L, Baker E, & Bentley R (2019). Housing Disadvantage and Poor Mental Health: A Systematic Review. American Journal of Preventive Medicine, 57(2), 262–272. 10.1016/j.amepre.2019.03.018 [DOI] [PubMed] [Google Scholar]
- Suglia SF, Duarte CS, & Sandel MT (2011). Housing Quality, Housing Instability, and Maternal Mental Health. Journal of Urban Health : Bulletin of the New York Academy of Medicine, 88(6), 1105–1116. 10.1007/s11524-011-9587-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teresa BF (2018). The Geography of Eviction in Richmond: Beyond Poverty. 8. [Google Scholar]
- Thoemmes F, & Ong AD (2016). A Primer on Inverse Probability of Treatment Weighting and Marginal Structural Models. Emerging Adulthood, 4(1), 40–59. 10.1177/2167696815621645 [DOI] [Google Scholar]
- Thomas TA, Toomet O, Kennedy I, & Ramiller A (2019, February 17). The State of Evictions: Results from the University of Washington Evictions Project. The State of Evictions: Results from the University of Washington Evictions Project. https://evictions.study/washington/ [Google Scholar]
- Valeri L, & VanderWeele TJ (2013). Mediation analysis allowing for exposure–mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychological Methods, 18(2), 137–150. 10.1037/a0031034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vásquez-Vera H, Palència L, Magna I, Mena C, Neira J, & Borrell C (2017). The threat of home eviction and its effects on health through the equity lens: A systematic review. Social Science & Medicine, 175, 199–208. 10.1016/j.socscimed.2017.01.010 [DOI] [PubMed] [Google Scholar]
- Vásquez-Vera H, Rodríguez-Sanz M, Palència L, & Borrell C (2016). Foreclosure and Health in Southern Europe: Results from the Platform for People Affected by Mortgages. Journal of Urban Health, 93(2), 312–330. 10.1007/s11524-016-0030-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayaraghavan M, Jacobs EA, Seligman H, & Fernandez A (2011). The Association Between Housing Instability, Food Insecurity, and Diabetes Self-Efficacy in Low-Income Adults. Journal of Health Care for the Poor and Underserved, 22(4), 1279–1291. 10.1353/hpu.2011.0131 [DOI] [PubMed] [Google Scholar]
- Wood D, Crapnell T, Bennett A, Lotstein D, Ferris M, & Kuo A (2018). Emerging adulthood as a critical stage in the life course. In Handbook of life course health development (pp. 123–143). Springer. [PubMed] [Google Scholar]
- Wood JN, Medina SP, Feudtner C, Luan X, Localio R, Fieldston ES, & Rubin DM (2012). Local Macroeconomic Trends and Hospital Admissions for Child Abuse, 2000–2009. Pediatrics, 130(2), e358–e364. 10.1542/peds.2011-3755 [DOI] [PubMed] [Google Scholar]
- Zenou Y, & Boccard N (2000). Racial Discrimination and Redlining in Cities. Journal of Urban Economics, 48(2), 260–285. 10.1006/juec.1999.2166 [DOI] [Google Scholar]


