Abstract
Aim
To investigate the extent to which the Revised Oral Assessment Guide–Jönköping (ROAG‐J) is used by nursing staff routinely in nursing homes in Sweden and to describe oral health status of the residents.
Design
An observational, retrospective register‐based study.
Methods
Data from different validated health assessments instruments, including ROAG‐J, for the period 2011–2016 were obtained from the Web‐based national quality register Senior Alert. The basis for the analyses was 190,016 assessments.
Results
About half of all residents had underwent at least one annual ROAG‐J assessment (2014–2016). During the period 2011–2016, 42% of the residents (n = 92,827) were registered to have oral health problems. Significantly more oral health problems were found for men and for those with younger age, poorer physical condition, neurophysiological problems, underweight, impaired mobility and many medications. In conclusion, poorer oral health was found for more care‐dependent individuals, which shows a need of preventive actions.
Keywords: geriatric nursing, older people, oral care, oral health, risk assessments
1. INTRODUCTION
The percentages of older people is increasing in Sweden and worldwide (United Nations, 2015). Between the years 2015–2035, the forecast increase in those aged ≥ 80 years in Sweden is 76%, which indicates a need for an extensive expansion of the nursing care for older people (Statistics Sweden, (2016). In 2018, among adults ≥ 80 years old, 14% were living permanently in nursing homes and 29% were receiving home help services in ordinary housing (National Board of Health & Welfare, 2019).
With increasing frailty in older adults, many become dependent on care from the society. The group of older people moving to nursing homes can be described as the most dependent, who in most cases have multimorbidity and/or substantial impairments in their functional status. Oral health problems, including poor oral hygiene, are commonly seen among older adults in nursing homes, with high prevalence of caries, periodontal disease and ill‐fitting prosthetics (Andersson et al., 2017; Murray Thomson, 2014). It is therefore important to find ways to include oral health and oral care as a natural part of nursing work.
2. BACKGROUND
The oral health of older people has changed dramatically in recent decades, with more people retaining their teeth. These teeth are often heavily restored and/or combined with complex prosthetic constructions, which may complicate daily oral hygiene (Norderyd et al., 2015). A large number of factors have been shown to affect an older person's ability to manage oral hygiene, such as attitudes/motivation, cognitive factors, social context and bodily and oral functions (Grönbeck Linden et al., 2017). Dependent older people are therefore often in need of help or support with their daily oral care (Strömberg et al., 2012). Unfortunately, competence in oral health and attitudes to oral care has been reported to be inadequate in nursing care (Lindqvist et al., 2013). A common opinion by nursing staff is that oral hygiene is a hard and unpleasant task (Forsell et al., 2011). If there is a need for oral hygiene support but it is not offered or insufficient, the risk of developing oral diseases is increased (Zuluaga et al., 2012).
Extensive medication is common for older people and is an aetiological factor for dry mouth, which in turn is highly associated with risk for caries (Anil et al., 2016). Poor oral health may affect old people's quality of life by affecting speech, chewing ability, social interactions and self‐esteem and by the presence of pain and discomfort (Miura et al., 2010; Petersen & Yamamoto, 2005). During the late period in life, meals may be one of the life's few pleasures and having difficulty eating may have great impact on quality of life and also lead to impaired nutrition and risk of weight loss (Petersen & Yamamoto, 2005). Associations have been found between oral diseases and general health, where periodontal disease is linked to a greater risk for aspiration pneumonia and coronary heart diseases (Scannapieco & Cantos, 2016). Poor oral health and swallowing dysfunction are shown to be independent risk factors for mortality in older people in intermediate care (Hägglund et al., 2019).
It is necessary to detect oral health problems at an early stage in dependent old people with disease and/or functional impairments to be able to take actions to reduce these problems. The use of oral (risk) assessment instruments is one way to identify oral health problems in nursing care, which may increase the priority of oral hygiene in routine care of older people (Konradsen et al., 2012). A Swedish Web‐based national quality register for preventive care of adults ≥ 65 years old, the Senior Alert (SA), includes an oral health risk assessment SA is designed to improve the care of older people, reducing health problems and improving accountability. SA was launched in 2008, and almost all municipalities in the 21 regions in Sweden use it. The SA register includes data from five common health risk areas for older people: falls, pressure ulcers, malnutrition, oral health (included 2011) and bladder dysfunction (included 2014). Health professionals use SA in care prevention in care and welfare, for example in nursing homes, short‐term accommodations and home help services and during hospitalization. In all five risk areas, well‐established assessment instruments are used. SA is unique in that it promotes quality improvement by stimulating staff to perform screening and to take action (Senior Alert, 2019).
For risk assessment of oral health in SA, the Revised Oral Assessment Guide (ROAG) is used. ROAG is based on the Oral Assessment Guide, OAG, which was developed in 1988 by Eilers at al. (Eilers et al., 1988). OAG was translated into Swedish and evaluated by Andersson et al. in patients undergoing chemotherapy treatment (Andersson et al., 1999) and then revised and renamed ROAG for use in older adults (Andersson, Hallberg, et al., 2002). The reliability of the instrument was shown to be good between a trained nurse and a dental hygienist (Andersson et al., 2002). In SA, the planned preventive actions in ROAG became somewhat modified and the assessment was renamed the ROAG‐Jönköping (ROAG‐J). By using the instrument, oral health problems can be identified, preventive actions can be implemented, or referral was made to dental care or health care (Senior Alert, 2019). However, there is limited knowledge of the extent to which ROAG‐J is used in Swedish nursing homes and about the quality of the assessments.
3. AIM
The aims of this study were as follows:
First, to describe the extent to which people in nursing homes in Sweden have received at least one ROAG‐J assessment per year in Senior Alert and whether there are any demographic differences (2014–2016) or differences in usage of ROAG‐J compared with the other Senior Alert risk assessment instruments (2011–2018).
Second, in a national perspective to investigate oral health status of older residents at nursing homes between the years 2011–2016, assessed by ROAG‐J in relation to age, gender, physical condition, neurophysiological problems, body mass index, mobility and medication.
4. METHODS
4.1. Design
The study is an observational, retrospective register‐based study based on data from the national quality register Senior Alert (SA).
4.2. Sample
Included in the study were all adults who:
were ≥ 65 years of age
lived in private or municipality‐run nursing homes (including special housing for people with neurocognitive disorders) in Sweden
had received at least one ROAG‐J assessment
For the first aim, the first ROAG‐J assessment per person and year from 2011–2016 was used. Thus, a maximum of six assessments per person could be obtained during the six‐year period. For comparison of ROAG‐J assessments in relation to other SA risk assessments, data also from 2017–2018 were included giving an eight‐year period. For the second aim, only the first ROAG‐J assessment per person in nursing home was included.
Cases with one or more missing values and inaccurate variables were excluded before analyses. Figure 1 shows a flow chart of study samples. This study was guided by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (von Elm et al., 2007).
FIGURE 1.
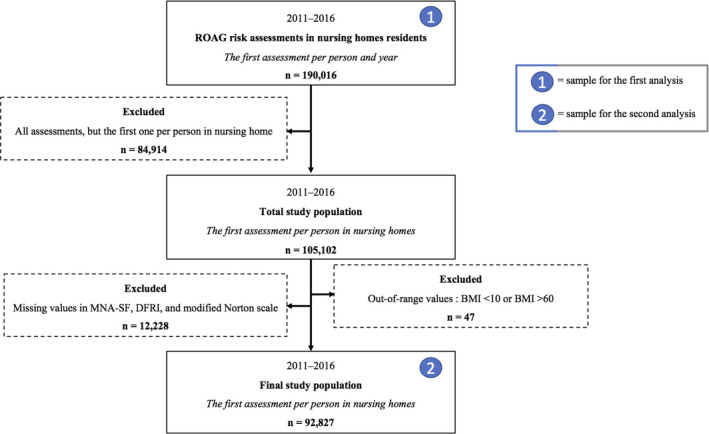
A flow chart showing the samples for the first analysis, to describe the extent to which ROAG‐J in SA is used in nursing homes and whether there are any demographic differences in use between regions in Sweden, and for the second analysis, to investigate oral health status assessed by ROAG‐J in relation to age, gender, physical condition, neurophysiological problems, BMI, mobility, and medication
4.3. Instruments
In Senior Alert, nursing staff perform ROAG‐J assessments on residents at the nursing homes by clinical intra‐ and extraoral examination. Equipment used for the intraoral examination is a flashlight and mouth mirror or if mirror is missing, a teaspoon. The ROAG‐J assessment takes approximately 3–4 min to perform. The nursing staff should have received about 2 to 4 hr’ theoretical training in ROAG‐J from dental personnel (the training may vary between municipalities) or a shorter Web‐based training programme available on the SA website (Senior Alert, 2019).
ROAG‐J consists of the nine items to examine: swallowing, voice, tongue, mucous membranes, lips, saliva, gums, teeth and dentures. The variables and the ratings are shown in Tables 1
TABLE 1.
The variables and the ratings of the nine items in ROAG‐J in Senior Alert
| Grade | Voice | Lips | Mucous membranes |
|---|---|---|---|
| 0 | Not applicable to judge | – | – |
| 1 | Normal | Smooth, bright red, moist | Bright red, moist |
| 2 | Dry, hoarse, smacking | Dry, cracked, sore corners of the mouth | Red, dry, or areas of discoloration, coating |
| 3 | Difficulty speaking | Ulcerated, bleeding | Wounds with or without bleeding, blisters |
| Tongue | Gums | Teeth | |
|---|---|---|---|
| 0 | – | No gums, only oral mucosa | No natural teeth |
| 1 | Pink, moist with papillae | Light red and solid | Clean, no visible coating or food debris |
| 2 | No papillae, red, dry, coating | Swollen, reddened | Coating or food debris locally |
| 3 | Ulcers with or without bleeding, blistering | Spontaneous bleeding | Coating or food debris generally, broken teeth |
| Dentures | Saliva | Swallowing | |
|---|---|---|---|
| 0 | No prosthetics | – | Not applicable to judge |
| 1 | Clean, functioning | Runs freely | Unimpeded swallowing |
| 2 | Coating or food debris | Runs sluggishly | Minor swallowing problems |
| 3 | Not used or malfunctioning | Does not run at all | Pronounced swallowing problems |
Grades 0 = not relevant to assess , 1 = healthy or normal condition, 2 = Moderate changes or divergence, 3 = Severe changes or divergence.
Grade 1 does not require any action. Grade 2 should be treated by the nursing staff by a preventive action plan. These actions are listed in the ROAG‐J manual on the SA website (Senior Alert, 2019). When a grade 3 is identified, a consultation with or referral to a dentist or a physician is recommended. In the present study, registered risk grade 2 and/or 3 on one or more ROAG‐J items means “Risk” (oral health problems), while the absence of grade 2 or 3 means “No risk.” Grades 0–1 are given 0 points, and Grades 2–3 are given 1 point, generating a total score from 0–9. In this study, in some analyses the score was dichotomized to: 0 points = “no risk” and 1–9 points = “risk.”
The SA register also included assessments for detecting and preventing: falls; pressure ulcers; malnutrition; and bladder dysfunction of older people. In the present study, some variables were included from the risk assessment instrument for fall (the Downton Fall Risk Index, DFRI), malnutrition (the Minimal Nutrition Assessment—Short Form, MNA‐SF) and pressure ulcers (the modified Norton; Downton & Andrews, 1991; Ek, 1987; Rubenstein et al., 2001).
There are also other instruments available in SA for assessment of falls, malnutrition and pressure ulcers (one extra for each event), but they are more rarely used and do not include the variables selected from DFRI, MNA‐SF and the modified Norton used in the present study (see below).
In the analyses, the same Senior Alert registration (the first one per person and year) was used for these risk assessment variables as for the ROAG‐J assessment. Assessment of falls, pressure ulcers and malnutrition are mandatory in SA, while oral health and bladder dysfunction are optional.
Variables from the DFRI:
Medication
None, tranquillisers/sedatives, diuretics, antihypertensives (other than diuretics), antiparkinsonian drugs, antidepressants, other medications. Response alternatives: Yes/No.
Variables from the MNA‐SF:
Body mass index (BMI) (<10–18.4 = underweight, 18.5–24.9 = normal range, 25–29.9 = overweight, 30–60 = obese) (WHO, 2000)
Neuropsychological problems (severe dementia or depression, mild dementia or depression, no psychological problems)
Variables from the modified Norton:
Physical condition (very bad, poor, fair, good)
Mobility (immobile/bedridden, very limited, slightly limited, fully mobile)
The risk assessments in SA, including ROAG‐J, are made on admission to the nursing homes and are repeated at least twice a year. They also can be performed more often, in conjunction with other risk assessments in SA and at follow‐ups in 1–3 months in individuals with identified risk (Senior Alert, 2019). After the nursing staff have done a risk assessment, the result is entered into the database of the SA quality register.
4.4. Data collection
After Research Ethics Committee approval, data for the present study were ordered and provided from the Uppsala Clinical Research Center, which is responsible for the database of the quality register SA. The total of 190,016 cases forms the basis for the analyses (Figure 1).
SA changed its database structure in the beginning of 2017, and data from the two databases could not be merged for data analysis. Therefore, statistics from the years 2011–2016 were used in the study, except for the analysis concerning the percentages of ROAG‐J assessments in relation to SA assessments, when data were also included from 2017–2018.
To analyse the percentages of ROAG‐J assessments carried out among those living in nursing homes, statistics from the Swedish National Board of Health and Welfare (SNBHW) on those who were permanently living in nursing homes were used (National Board of Health & Welfare, 2019). Data about the number of residents (65 + years old) in nursing homes from this statistical database were found for the years 2014–2016 (National Board of Health & Welfare, 2019). Statistics from SNBHW for the years before 2014 were inadequate, due to some municipalities having failed to submit data to SNBHW.
The flow chart in Figure 1 shows that in the final study population, for the analysis about oral health status and the relation to age, gender, physical condition, neurophysiological problems, BMI, mobility and medication, 12,275 people are not included, due to missing values in the risk assessments DFRI, MNA‐SF and the modified Norton. The reason for the missing values in these risk assessments is probably that there are also other risk assessments available to use in SA for falls, malnutrition and pressure ulcers (see 4.3 Instruments). These other risk assessments do not include the variables chosen for the present study.
4.5. Statistical methods
Results are shown in number, percentage, median, range, mean and standard deviation (SD).
Binary logistic regression was used for comparisons of oral health problems (Risk/No risk) and for interaction analysis. A multiple logistic regression analysis was used to assess the impact on oral health (Risk/No risk) of the SA variables from the other risk assessment instruments included in the present study. The results are shown with odds ratio (OR), 95% confidence interval (95% CI), p‐value and Nagelkerke R2. All tests were two‐tailed (α = 0.001).
Due to the large sample sizes, many results became statistically significant despite small numerical differences of no clinical relevance and p‐values ≥ .001 were not reported. All statistical analysis was performed by use of SPSS version 25 (IBM Corporation).
4.6. Ethical considerations
Conducting research among people with frail health and reduced capacity requires specific considerations, and although such studies are urgently needed, it is important to place strong emphasis on ethical awareness. All persons in the register were informed by the caregiver about registration in the quality register (Senior Alert, 2019). The study was approved by the Regional Ethical Review Board of Gothenburg, Sweden (Dnr. 026–18). To ensure anonymity, no personal data were included in the study data file.
5. RESULTS
5.1. ROAG‐J assessments over time
In Sweden in 2014, 47% (N = 49,353) of all residents in nursing homes had at least one ROAG‐J risk assessment registered in the SA, and in 2015 and 2016, the percentages were 50% (N = 51,552 and N = 52,822, respectively). During 2014–2016, all 21 regions in Sweden had nursing homes that were assigned to SA and used the ROAG‐J assessment. The use of ROAG‐J in the different regions ranged from 28%–90%. From 2015–2016, in 15 out of 21 regions, a decrease in the percentages of assessments was found. In total, however, there was no decrease in assessments, as in densely populated regions such as Stockholm and Skåne, the number increased.
Figure 2 shows that the number of residents having at least one ROAG‐J assessment per person and year increased substantially every year until 2014, but thereafter, the increase stagnated and remained relatively stable between 2014–2018. In the same figure, the numbers of ROAG‐J (optional) assessments performed are compared with the numbers of the mandatory SA assessments (fall, pressure ulcers and malnutrition). The percentages of SA assessments where ROAG‐J was included increased over time from 44% in 2013 to 87% in 2018.
FIGURE 2.
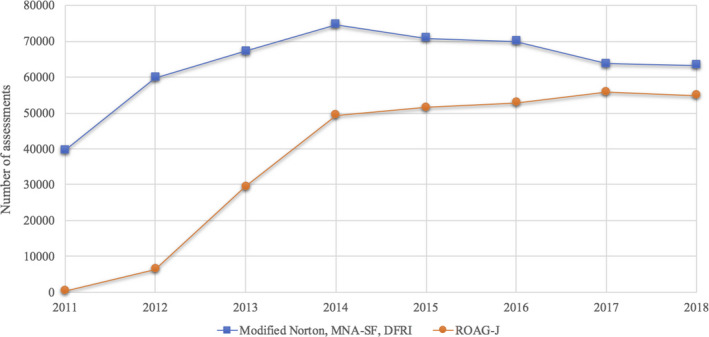
The number of mandatory Senior Alert assessments (Modified Norton, MNA‐SF, DFRI) compared with the number of optional ROAG‐J assessments during the period 2011–2018. One assessment per person and year were included in the analysis
5.2. Characteristics of those assessed
Mean age of the final sample was 85 years (SD 7.5; range 65–109 years), and most were women (Table 2). Eighty‐two per cent of the residents were living in municipality‐run nursing homes and 18% in privately run nursing homes. Edentulousness occurred in 23% of the individuals (women 24%; men 21%). The most commonly used medication was sedative drugs (46%), followed by antihypertensives (38%), antidepressants (36%), diuretics (31%) and antiparkinsonian drugs (4.4%). The response alternative “other medication” was the most commonly registered (70%). “No medication” was registered for 1.8% of the residents only. BMI < 18.5 (underweight) was found in 13% of the women and 7% of the men. More characteristics of the participants are shown in Table 2.
TABLE 2.
Characteristics of the study population (n = 92,827)
| N | % | |
|---|---|---|
| Age | ||
| 65–74 | 9,128 | 9.8 |
| 75–84 | 29,213 | 31.5 |
| 85–94 | 46,893 | 50.5 |
| ≥95 | 7,593 | 8.2 |
| Gender | ||
| Female | 61,460 | 66.2 |
| Male | 31,367 | 33.8 |
| BMI | ||
| Underweight | 10,056 | 10.8 |
| Normal range | 43,197 | 46.5 |
| Overweight | 26,941 | 29.0 |
| Obese | 12,633 | 13.6 |
| Physical condition | ||
| Good | 45,757 | 49.3 |
| Fair | 40,839 | 44.0 |
| Poor | 5,473 | 5.9 |
| Very bad | 758 | 0.8 |
| Neuropsychological problems | ||
| No problems | 27,716 | 29.9 |
| Mild | 45,477 | 49.0 |
| Severe | 19,634 | 21.2 |
| Mobility | ||
| Fully mobile | 45,145 | 48.6 |
| Slightly limited | 30,592 | 33.0 |
| Very limited | 16,139 | 17.4 |
| Immobile | 951 | 1.0 |
5.3. Oral health problems
Oral health problems (Risk) were detected in 42% (N = 39,075) of the residents in nursing home, with a range from 33%–55%, depending on the region they were living in. Whether the nursing home were municipality‐ or privately run did not make any difference (p = .305).
The total ROAG‐J scores of those with detected oral health problems ranged from 1–9 (median 2.0), with a mean value of 2.1 (SD 1.5). Among these, 74% had one or two oral health risk items registered (grade 2 or 3) out of the possible nine items. Grade 3 on at least one item in ROAG‐J was registered for 13% of all the assessed residents. Individuals who were registered as edentulous had fewer oral health problems registered in ROAG‐J than persons with remaining natural teeth (37% vs. 44%, p < .001). Nursing home residents with oral problems, compared with those without, used more (p < .001) sedatives drug (44% vs. 40%), antidepressants (46% vs. 40%) and antiparkinsonian drugs (51% vs. 41%). For “other medication,” differences were small (<2%), and for antihypertensives, small (<2%) and reversed.
In Table 3 the oral health problems assessed with ROAG‐J are presented in relation to other SA variables (age, gender, BMI, physical condition, neurophysiological problems, mobility). The youngest age group (65–74 years) had more oral health problems compared with the other age groups and men had more than women. Significantly more oral health problems were registered for residents with underweight, impaired physical condition, neuropsychological problems and limited mobility. “Immobile” individuals had six times higher odds for oral problems compared with fully mobile individuals, and individuals registered with “poor” or “very bad” physical condition compared with “good” physical condition had about four times higher risk for oral health problems. Furthermore, individuals with “severe” dementia/depression had twice as high odds for oral problems compared with individuals with no neurophysiological problems and “underweight” individuals had 1.4 times higher odds for detected problems in ROAG‐J than for “normal weight.” Residents registered with “overweight” and “obese” had fewer problems in ROAG‐J than those of “normal weight.”
TABLE 3.
Percentage and frequency of residents in nursing homes assessed with ROAG‐J to have oral health problems (risk), and the relation to other factors in Senior Alert. Binary logistic regression analysis with odds ratio (OR), 95% confidence interval (95% CI) and p‐value. The reference variables are specified (ref)
| Oral health problems | ||||
|---|---|---|---|---|
| N | % | OR (95% CI) | p | |
| Total | 39,075 | 42.1 | – | – |
| Age | – | – | 0.89 (0.87–0.90) | <.001 a , b |
| 65–74 | 4,396 | 48.2 | 1.37 (1.31–1.43) | <.001 |
| 75–84 | 12,567 | 43.0 | 1.11 (1.08–1.14) | <.001 |
| 85–94 (ref) | 18,974 | 40.5 | 1.00 | – |
| ≥95 | 3,138 | 41.3 | 1.04 (0.99–1.09) | .154 |
| Gender | ||||
| Female (ref) | 24,968 | 40.6 | 1.00 | – |
| Male | 14,107 | 45.0 | 1.20 (1.16–1.23) | <.001 |
| BMI | – | – | 0.97 (0.97–0.98) | <.001 b |
| Underweight | 5,178 | 51.5 | 1.43 (1.37–1.49) | <.001 |
| Normal range (ref) | 18,434 | 42.7 | 1.00 | – |
| Overweight | 10,577 | 39.3 | 0.87 (0.84–0.90) | <.001 |
| Obese | 4,886 | 38.7 | 0.85 (0.81–0.88) | <.001 |
| Physical condition | ||||
| Good (ref) | 15,522 | 33.9 | 1.00 | – |
| Fair | 19,401 | 47.5 | 1.76 (1.71–1.81) | <.001 |
| Poor | 3,642 | 66.5 | 3.87 (3.65–4.11) | <.001 |
| Very bad | 510 | 67.3 | 4.01 (3.44–4.67) | <.001 |
| Neuropsychological problems | ||||
| No problems (ref) | 9,882 | 35.7 | 1.00 | – |
| Mild | 18,770 | 41.3 | 1.27 (1.23–1.31) | <.001 |
| Severe | 10,423 | 53.1 | 2.04 (1.97–2.12) | <.001 |
| Mobility | ||||
| Fully mobile (ref) | 14,746 | 32.7 | 1.00 | – |
| Slightly limited | 13,751 | 44.9 | 1.68 (1.63–1.73) | <.001 |
| Very limited | 9,869 | 61.2 | 3.25 (3.13–3.37) | <.001 |
| Immobile/Bedridden | 709 | 74.6 | 6.04 (5.21–7.00) | <.001 |
OR per 10 years.
The full scale was used in the analyses.
To determine whether the relationships between oral health problems and BMI, physical condition, neuropsychological problems and mobility are modified by gender or age, we performed interaction analyses with logistic regression. No clinically relevant differences were found.
A multiple logistic regression was performed, with oral health problems (yes/no) as dependent variable and age, gender, BMI, physical condition, neuropsychological problems, mobility and all the medications as independent variables. The analysis showed statistical significance (p < .001) for all included variables except for “antihypertensive,” “other medication” and “no medication.” The strongest predictor of oral health problems was found for the variable “mobility,” followed by “physical condition” and “neurophysiological problems.” The whole model explained 10.3% (Nagelkerke R2) of the variance in ROAG‐J status. The statistically significant results from the first analysis (p < .001) remained in a separate multiple regression analysis, where all 21 regions were included to take clustering effects into account.
The most common oral health problem identified was for the item teeth, which was registered for 27% of the residents, followed by dentures (16%) and swallowing (13%) (Table 4). Fewer than 10% of the residents had problems registered for each of the other six items in ROAG‐J (voice, lips, mucous membranes, tongue, gums and saliva).
TABLE 4.
Percentages of oral health problems (risk) per ROAG‐J items and the relation to other factors registered in Senior Alert. Odds ratio (OR) and 95% confidence interval (95% CI)
| Voice a | Lips | Mucous membranes | Tongue | Gums b | Teeth b | Dentures c | Saliva | Swallowing | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | |
| Total | 9.3 | – | 7.0 | – | 7.3 | – | 7.5 | – | 8.9 | – | 27.4 | – | 15.9 | – | 9.1 | – | 12.8 | – |
| Age | ||||||||||||||||||
| 65–74 | 11.4 | 1.32 (1.23–1.43) | 7.5 | 1.10 (1.01–1.19) | 8.0 | 1.14 (1.04–1.23) | 8.2 | 1.15 (1.06–1.25) | 12.0 | 1.58 (1.47–1.70) | 32.3 | 1.38 (1.31–1.46) | 22.6 | 1.66 (1.50–1.83) | 8.4 | 0.91 (0.84–0.98) | 15.3 | 1.30 (1.22–1.39) |
| 75–84 | 9.4 | 1.07 (1.01–1.12) | 6.9 | 1.01 (0.95–1.07) | 7.6 | 1.02 (0.97–1.08) | 7.5 | 1.06 (1.00–1.12) | 9.7 | 1.25 (1.18–1.32) | 28.3 | 1.14 (1.10–1.19) | 16.6 | 1.13 (1.06–1.21) | 8.9 | 0.97 (0.92–1.02) | 12.9 | 1.07 (1.02–1.12) |
| 85–94 | 8.3 | 1.00 (ref) | 6.9 | 1.00 (ref) | 7.0 | 1.00 (ref) | 7.1 | 1.00 (ref) | 7.9 | 1.00 (ref) | 25.6 | 1.00 (ref) | 14.7 | 1.00 (ref) | 8.8 | 1.00 (ref) | 11.0 | 1.00 (ref) |
| ≥95 | 9.1 | 1.10 (1.01–1.20) | 7.2 | 1.02 (0.93–1.12) | 7.7 | 1.10 (1.00–1.21) | 7.5 | 1.04 (0.95–1.14) | 7.4 | 0.94 (0.85–1.04) | 26.7 | 1.06 (0.99–1.13) | 15.4 | 1.03 (0.94–1.13) | 10.0 | 1.12 (1.03–1.21) | 11.8 | 1.10 (1.02–1.18) |
| Gender | ||||||||||||||||||
| Female | 8.7 | 1.00 (ref) | 7.2 | 1.00 (ref) | 7.1 | 1.00 (ref) | 7.2 | 1.00 (ref) | 8.4 | 1.00 (ref) | 25.2 | 1.00 (ref) | 14.7 | 1.00 (ref) | 9.6 | 1.00 (ref) | 12.5 | 1.00 (ref) |
| Male | 10.6 | 1.25 (1.19–1.31) | 6.4 | 0.88 (0.83–0.93) | 7.6 | 1.08 (1.02–1.13) | 7.9 | 1.11 (1.05–1.16) | 9.7 | 1.17 (1.11–1.23) | 31.4 | 1.36 (1.31–1.41) | 18.8 | 1.34 (1.26–1.42) | 8.1 | 0.84 (0.80–0.88) | 13.4 | 1.09 (1.04–1.13) |
| BMI | ||||||||||||||||||
| Underweight | 15.7 | 1.67 (1.57–1.78) | 11.1 | 1.58 (1.47–1.70) | 11.2 | 1.55 (1.45–1.67) | 10.8 | 1.48 (1.38–1.59) | 11.4 | 1.34 (1.25–1.44) | 31.8 | 1.26 (1.19–1.34) | 20.4 | 1.30 (1.19–1.42) | 14.5 | 1.69 (1.58–1.80) | 21.0 | 1.70 (1.60–1.80) |
| Normal range | 10.0 | 1.00 (ref) | 7.3 | 1.00 (ref) | 7.5 | 1.00 (ref) | 7.6 | 1.00 (ref) | 8.7 | 1.00 (ref) | 27.1 | 1.00 (ref) | 16.5 | 1.00 (ref) | 9.1 | 1.00 (ref) | 13.6 | 1.00 (ref) |
| Overweight | 7.4 | 0.71 (0.67–0.75) | 5.6 | 0.75 (0.71–0.80) | 6.0 | 0.79 (0.74–0.84) | 6.5 | 0.85 (0.80–0.90) | 8.5 | 0.97 (0.92–1.03) | 26.5 | 0.97 (0.93–1.01) | 14.3 | 0.85 (0.79–0.90) | 7.7 | 0.83 (0.79–0.88) | 10.5 | 0.75 (0.71–0.79) |
| Obese | 6.2 | 0.59 (0.55–0.64) | 5.2 | 0.69 (0.64–0.76) | 5.8 | 0.76 (0.70–0.82) | 6.4 | 0.83 (0.77–0.90) | 8.3 | 0.95 (0.88–1.02) | 26.5 | 0.97 (0.92–1.02) | 14.4 | 0.85 (0.78–0.93) | 7.6 | 0.81 (0.76–0.88) | 8.5 | 0.59 (0.55–0.63) |
| Physical condition | ||||||||||||||||||
| Good | 5.4 | 1.00 (ref) | 4.5 | 1.00 (ref) | 4.7 | 1.00 (ref) | 5.0 | 1.00 (ref) | 6.9 | 1.00 (ref) | 22.3 | 1.00 (ref) | 12.9 | 1.00 (ref) | 6.0 | 1.00 (ref) | 7.8 | 1.00 (ref) |
| Fair | 11.3 | 2.22 (2.11–2.33) | 8.0 | 1.86 (1.75–1.96) | 8.3 | 1.84 (1.74–1.94) | 8.5 | 1.76 (1.67–1.86) | 10.0 | 1.52 (1.44–1.59) | 30.9 | 1.56 (1.50–1.61) | 17.9 | 1.47 (1.38–1.55) | 10.3 | 1.79 (1.71–1.89) | 15.7 | 2.20 (2.10–2.30) |
| Poor | 24.7 | 5.68 (5.27–6.12) | 18.0 | 4.69 (4.32–5.09) | 18.5 | 4.61 (4.25–4.99) | 18.1 | 4.20 (3.87–4.55) | 15.6 | 2.51 (2.31–2.74) | 41.4 | 2.45 (2.30–2.62) | 25.5 | 2.30 (2.07–2.55) | 22.6 | 4.58 (4.25–4.93) | 30.8 | 5.25 (4.90–5.63) |
| Very bad | 31.6 | 8.01 (6.78–9.46) | 24.7 | 7.02 (5.92–8.33) | 25.3 | 6.89 (5.81–8.16) | 25.3 | 6.47 (5.46–7.66) | 19.4 | 3.27 (2.70–3.96) | 41.0 | 2.41 (2.04–2.85) | 30.0 | 2.88 (2.24–3.70) | 30.6 | 6.91 (5.89–8.10) | 35.5 | 6.49 (5.52–7.63) |
| Neuropsychological problems | ||||||||||||||||||
| No problems | 9.1 | 1.00 (ref) | 6.3 | 1.00 (ref) | 6.1 | 1.00 (ref) | 6.4 | 1.00 (ref) | 5.2 | 1.00 (ref) | 17.8 | 1.00 (ref) | 11.4 | 1.00 (ref) | 9.0 | 1.00 (ref) | 11.4 | 1.00 (ref) |
| Mild | 8.1 | 0.88 (0.84–0.93) | 6.4 | 1.03 (0.96–1.09) | 6.8 | 1.11 (1.04–1.18) | 7.1 | 1.12 (1.05–1.19) | 8.7 | 1.71 (1.60–1.83) | 28.0 | 1.79 (1.72–1.87) | 16.7 | 1.56 (1.46–1.67) | 8.1 | 0.90 (0.85–0.95) | 11.9 | 1.06 (1.01–1.11) |
| Severe | 12.5 | 1.42 (1.34–1.51) | 9.2 | 1.51 (1.41–1.61) | 10.0 | 1.70 (1.59–1.82) | 9.8 | 1.59 (1.49–1.70) | 14.5 | 3.06 (2.86–3.28) | 38.6 | 2.90 (2.76–3.04) | 22.9 | 2.31 (2.14–2.50) | 11.3 | 1.30 (1.22–1.38) | 16.9 | 1.58 (1.50–1.67) |
| Mobility | ||||||||||||||||||
| Fully mobile | 4.6 | 1.00 (ref) | 4.6 | 1.00 (ref) | 4.7 | 1.00 (ref) | 4.9 | 1.00 (ref) | 6.5 | 1.00 (ref) | 21.9 | 1.00 (ref) | 13.7 | 1.00 (ref) | 5.9 | 1.00 (ref) | 5.7 | 1.00 (ref) |
| Slightly limited | 9.8 | 2.26 (2.13–2.40) | 7.7 | 1.74 (1.63–1.85) | 7.7 | 1.70 (1.60–1.80) | 8.0 | 1.69 (1.59–1.79) | 8.9 | 1.40 (1.32–1.48) | 29.0 | 1.46 (1.41–1.52) | 16.4 | 1.24 (1.16–1.31) | 9.9 | 1.75 (1.66–1.85) | 13.7 | 2.61 (2.47–2.76) |
| Very limited | 20.8 | 5.50 (5.18–5.83) | 11.8 | 2.79 (2.61–2.98) | 12.9 | 3.01 (2.82–3.20) | 12.9 | 2.89 (2.72–3.08) | 14.6 | 2.45 (2.30–2.60) | 38.9 | 2.27 (2.17–2.37) | 21.4 | 1.72 (1.60–1.85) | 15.3 | 2.88 (2.72–3.05) | 28.8 | 6.67 (6.32–7.05) |
| Immobile/Bedridden | 41.7 | 15.0 (12.9–17.5) | 17.4 | 4.40 (3.70–5.23) | 20.8 | 5.36 (4.55–6.30) | 21.7 | 5.40 (4.60–6.34) | 21.5 | 3.91 (3.30–4.63) | 45.8 | 3.02 (2.60–3.50) | 26.6 | 2.28 (1.71–3.04) | 25.8 | 5.52 (4.75–6.41) | 51.3 | 17.4 (15.1–20.1) |
Statistically significant values (p < .001) are reported in italics.
Grade 0 (“not applicable to judge”) excluded.
Grade 0 (edentulous individuals) excluded.
Grade 0 (individuals without dentures) excluded.
Oral health problems were reported most frequently in the younger age group (65–74 years) for most of the ROAG‐J items, but for the item saliva, more residents with dry mouth were found in the older age groups (Table 4). In the youngest age group (65–74 years) compared with older age groups (85–94 and ≥ 95 years), men and severe dementia/depression and limited mobility were more common (p < .001). They also had more remaining natural teeth than older age groups (p < .001). In this younger group antidepressant, sedative and antiparkinsonian drugs are more regularly used than in older groups of residents (p < .001).
Men had significantly higher prevalence of risk in all ROAG‐J items, except for problem with lips and saliva, which were more common for women (difference: < 2%) (Table 4).
For the item saliva, assessing dry mouth, a higher percentage with risk (p < .001) was found among those with sedative drugs (10.1% vs. 8.2%; OR 1.25, 95% CI 1.20–1.31), diuretics (10.3% vs. 8.5%; OR 1.24, 95% CI 1.18–1.29), antidepressants (10.6% vs. 8.2%; OR 1.32, 95% CI 1.27–1.39) and those with antiparkinsonian drugs (11.3% vs. 9.0%; OR 1.30, 95% CI 1.17–1.43).
6. DISCUSSION
The scope of this quality register study was to describe oral health in almost 93,000 frail and dependent older residents in nursing homes in Sweden. To our knowledge, this is the first large‐scale study to evaluate the use of ROAG‐J in nursing care nationally.
Sweden is a global leader in the field of quality registries, with over 100 registries available in health and medical care. They are a “gold mine” for improving quality of care and efficiency and for research, since they generate large amounts of data. The SA register is unique compared with other registries, as it has a standardized and systematic approach that covers preventive actions, and all health professionals have access to information in the register. The systematic preventive care process can be followed over time for each individual, per unit and between units. For example, nursing staff can see whether a patient has a specific risk, whether a prevention plan exists, whether there has been follow‐up or whether incidents have occurred. Providers or policymakers can see number and types of risks and whether preventions plans are not in place in the unit or in the regions and take remedial actions. Senior Alert and researcher can also do comparisons across geographic areas and over time and help the improvement of the register (Rosén, 2010; Trinks et al., 2018).
When old people become frail, suffer from diseases or/and become functionally dependent, the risk increases for oral diseases and loss of a previous regular dental contact (Eckerblad et al., 2015; Grönbeck‐Linden et al., 2016). Therefore, oral assessments by nursing staff are important to detect oral health problems in the frail and dependent older population and enable prevention and treatment of oral problems in an early stage. Not least, it is important because the number of dependent older people living at home with the support of home care is increasing (National Board of Health & Welfare, 2019). The implementation of SA and ROAG in nursing homes, home care and hospitals can play an important role in this direction. This new way of working may improve the quality and increase cooperation between dentistry and nursing care (Zenthöfer et al., 2014).
This study shows that ROAG‐J was used relative frequently in Sweden in nursing homes, since half of all residents had at least one oral assessment registered. However, there was a large difference in the use of ROAG‐J between the Swedish regions (28%–90%). The reason may be that ROAG‐J is optional in SA.
The use of ROAG‐J increased fourfold between 2012–2013. This high increase in ROAG‐J assessments between these years was certainly partly due to a state performance compensation to the regions between 2012–2014 for using SA and performing risk assessments and planning preventive actions and follow‐ups (Ministry of Health and Social Affairs 2013). Since 2014, in the absence of funding from the government, the ROAG‐J assessments have almost stagnated and there are major differences in risk assessments across regions. The government funding for ROAG‐J assessments may have been the main motivator factor for some regions together with lack of understanding of the purpose of the ROAG‐J instrument. However, in densely populated regions an increase in ROAG‐J assessments after 2014 was found. To reduce the negative trend in many of the regions, the importance of risk assessments has to be emphasized by dental care, nursing and medical care, and that this is done in collaboration.
The study also shows that the oral assessment over time (2011–2018) was more frequently used together with the risk assessments for falls, pressure ulcers and malnourishment in SA. This is a welcome result, which hopefully reflects that oral health is more and more becoming a part of the general health regime in nursing care settings.
In the present study, the main findings were that poor oral health conditions were detected in 42% of the residents living in nursing homes in Sweden. Among these, 13% of the residents had one or more grade 3 in ROAG‐J, meaning need of contact with dental care service or a physician. The results show a somewhat higher percentages of risk in comparison with the results from a study by Johansson et al., (2016) analysing ROAG‐J data from one Swedish municipality, where less than one third of older people were considered to have oral problems (Johansson et al., 2016). In a recent study by Andersson et al., (2017) examining oral health (not with ROAG‐J) of about 20,000 residents (aged 65 + years), receiving domiciliary dental care by dental hygienists or dentists in nursing homes in Sweden, as many as 68% were found to have manifest caries and 90% had moderate to high risk for periodontitis (Andersson et al., 2017). Thus, those results and others (Andersson, Westergren et al., 2002; Holmén et al., 2012; Strömberg et al., 2012) are in conflict with the results of the SA quality register from the present study and the study by Johansson et al., (2016). The result of the present study showed for the item “teeth” that 73% had a registered grade 1, meaning clean teeth with no visible coating or food debris, and for the item “gums,” 91% had registered grade 1, healthy light red and solid gums. Based on clinical experience, these results may seem unlikely. Since the study by Andersson et al., (2017) also was a large‐scale study but the clinical examinations were performed by dental professionals and with more resources and not by nursing staff with brief education and few resources (at the best a mouth mirror and flashlight), their results probably can be considered more reliable for dependent older residents in nursing homes in Sweden.
The difference in findings between nursing staff and dental professionals could indicate that many oral problems of dependent older people are not detected by nursing staff using the oral assessment instrument. Oral problems that go undetected could lead to pain and nutrition difficulties and have an impact on general health and the quality of life for the already sick and dependent older adults (Glick et al., 2016). The conflicting results about detected oral health problems between nursing staff and dental professionals can probably be explained by nursing staff's lack of knowledge about oral health, uncertainty when examining the oral cavity and discomfort performing oral hygiene on old people (Miegel & Wachtel, 2009; Wårdh et al., 1997; Wårdh et al., 2012). Also, the ROAG‐J data in SA are registered by many different nurses and the training in ROAG‐J may be inadequate, in the sense that it is too short and almost always lacks practical training and follow‐up. To be able to assess oral health adequately, nursing staff need support from dental care and extensive skills development in oral health. Oral health must become part of the general health in nursing care.
In a study by Andersson et al., the ROAG assessment showed moderate to good inter‐rater reliability between a dental hygienist and a well‐trained Registered Nurse (Andersson, et al., 2002). When inter‐rater reliability was low, the Registered Nurse had assessed a better oral score than the dental hygienist (Andersson, et al., 2002; Andersson et al., 1999). In another study by Konradsen et al., poor or fair reliability of ROAG between nurses was shown (Konradsen et al., 2014). In that study, the Registered Nurses had not received any training in performing the assessment, only visual guides showing oral health problems and a healthy mouth. Ribeiro et al. (2014) conducted a more developed training programme (approximately 5 hr) for the use of ROAG and then tested the validity and reproducibility of the instrument. The reproducibility was good for almost all categories (Ribeiro et al., 2014). These studies point to the importance of ensuring in future that non‐dental healthcare professionals are well trained and provided sufficient training in oral health and in the use of the oral health assessment to ensure good validity and reliability of the instrument.
The results of the present study showed that more oral health problems were registered in the youngest age group (65–74 years) compared with the older age groups in nursing homes. This may seem surprising, since being younger, they ought to have better oral health. The results showed also that the youngest group had more natural remaining teeth, more limited mobility, more severe neurophysiological problems, and poorer physical condition and used more drugs like sedatives, antidepressants and antiparkinsonians. The reason could be that people in this group also had previously been living in a nursing home due to long‐term illness, but only now had reached 65 + years and been included in this 65‐ to 74‐year‐old group. Long‐lasting illnesses such as Parkinson's disease, mental illness and alcohol‐related diseases often affect oral health negatively (Kisely et al., 2011; Petersen et al., 2005).
More oral health problems were registered for individuals with general health problems than those without. This was evident for neurophysiological problems, underweight, poor physical condition and limited mobility. Limitations, both functionally and mentally, often lead to inability to perform the daily routines like tooth brushing. Help with daily preventive oral actions from staff in nursing homes often are needed to avoid oral health problems. Studies show, however, that most of the dependent residents in nursing homes, who have difficulty in maintaining good oral health by themselves, do not get assistance from health professionals with their daily oral hygiene (Forsell et al., 2009). With the use of SA and ROAG‐J, oral health may become a natural part of nursing care of older dependent adults, as the nursing staff become more experienced and accustomed to the oral cavities of those in their care.
In an ongoing study using the same national register data from SA, the authors investigate whether the implemented preventive actions in ROAG‐J have a positive effect on oral health over time. It is important to evaluate such an already existing and implemented instrument in nursing homes in Sweden. There is a need to explore the effect of the preventive actions and whether improvements are necessary for making ROAG‐J become more efficient in nursing care of older people.
7. CONCLUSION
In the present study, significantly poorer oral health was found among individuals who were more care‐dependent, which indicates a need for help and improvement of oral care in this group. In contrast to other recent studies, where dental professionals had conducted the examinations on older residents in nursing homes, this study showed in general fewer oral health problems. This may indicate a need for improved training and education of nursing staff in the use of the ROAG‐J to ensure good reliability and validity of the instrument.
8. RELEVANCE TO CLINICAL PRACTICE
Oral health assessments in nursing care might be valuable to help health professionals detect need of oral prevention and care in older adults who are ill and/or functionally dependent and to help them to maintain regular contact with dental services. This way of working may improve the quality of care and increase collaboration between dentistry and nursing care. By routinely carrying out ROAG‐J assessments in nursing care of older people, nursing staff can become experienced and accustomed to inspecting the oral cavity. Hopefully, then, the mouth may come to be a natural part of nursing care in a way that it now rarely is. However, this study indicates a need of better training to improve the quality of the assessments.
CONFLICT OF INTEREST
The authors have no conflicts of interest.
AUTHOR CONTRIBUTIONS
LB and CH: Project design with input from all the authors. LB: Data analysis and manuscript drafting with input from CH and PA. DN: Data file creation and review of the statistical analyses that were made. CH and PA: Project supervision. All authors provided critical feedback on the final version of the manuscript.
Supporting information
File S1
ACKNOWLEDGEMENTS
The authors would like to thank Lars Gahnberg, who participated in the design of the study. The study was supported by grants from the Local Research and Development Board for Gothenburg and Södra Bohuslän, Region Västra Götaland; TUA Research Funding, the Sahlgrenska Academy at the University of Gothenburg / Region Västra Götaland, Sweden; Health Promotion Research Funding, Region Västra Götaland; the Swedish Order of Freemasons, Grand Lodge of Sweden; and the Swedish Dental Society.
Bellander L, Andersson P, Nordvall D, Hägglin C. Oral health among older adults in nursing homes: A survey in a national quality register, the Senior Alert. Nurs Open.2021;8:1262–1274. 10.1002/nop2.743
Funding informations
Swedish Order of Freemasons, Grand Lodge of Sweden; the Swedish Dental Society; Local Research and Development Board for Gothenburg and Södra Bohuslän, Region Västra Götaland; TUA Research Funding, the Sahlgrenska Academy at the University of Gothenburg/Region Västra Götaland; Health Promotion Research Funding, Region Västra Götaland, Sweden.
DATA AVAILABILITY STATEMENT
Data from the Swedish quality register Senior Alert were ordered from the administrator Uppsala Clinical Research Center. Data were also obtained from the National Board of Health and Welfare. The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Senior Alert (2019). Senior alert ‐ more than just a quality register. Retrieved from https://plus.rjl.se/infopage.jsf?nodeId=43617 [Google Scholar]
- Andersson, P. , Hallberg, I. R. , & Renvert, S. (2002). Inter‐rater reliability of an oral assessment guide for elderly patients residing in a rehabilitation ward. Special Care in Dentistry, 22(5), 181–186. [DOI] [PubMed] [Google Scholar]
- Andersson, P. , Persson, L. , Hallberg, I. R. , & Renvert, S. (1999). Testing an oral assessment guide during chemotherapy treatment in a Swedish care setting: A pilot study. Journal of Clinical Nursing, 8(2), 150–158. 10.1046/j.1365-2702.1999.00237.x [DOI] [PubMed] [Google Scholar]
- Andersson, P. , Renvert, S. , Sjögren, P. , & Zimmerman, M. (2017). Dental status in nursing home residents with domiciliary dental care in Sweden. Community Dental Health Journal, 34(4), 203–207. 10.1922/CDH_4100Andersson05 [DOI] [PubMed] [Google Scholar]
- Andersson, P. , Westergren, A. , Karlsson, S. , Rahm Hallberg, I. , & Renvert, S. (2002). Oral health and nutritional status in a group of geriatric rehabilitation patients. Scandinavian Journal of Caring Sciences, 16(3), 311–318. 10.1046/j.1471-6712.2002.00086.x [DOI] [PubMed] [Google Scholar]
- Anil, S. , Vellappally, S. , Hashem, M. , Preethanath, R. S. , Patil, S. , & Samaranayake, L. P. (2016). Xerostomia in geriatric patients: A burgeoning global concern. Journal of Investigative and Clinical Dentistry, 7(1), 5–12. 10.1111/jicd.12120 [DOI] [PubMed] [Google Scholar]
- Downton, J. H. , & Andrews, K. (1991). Prevalence, characteristics and factors associated with falls among the elderly living at home. Aging, 3(3), 219–228. [DOI] [PubMed] [Google Scholar]
- Eckerblad, J. , Theander, K. , Ekdahl, A. , Unosson, M. , Wirehn, A.‐B. , Milberg, A. , Krevers, B. , & Jaarsma, T. (2015). Symptom burden in community‐dwelling older people with multimorbidity: A cross‐sectional study. BMC Geriatrics, 15, 1. 10.1186/1471-2318-15-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eilers, J. , Berger, A. M. , & Petersen, M. C. (1988). Development, testing and application of the oral assessment guide. Oncology Nursing Forum, 15(3), 325–330. [PubMed] [Google Scholar]
- Ek, A. C. (1987). Prediction of pressure sore development. Scandinavian Journal of Caring Sciences, 1(2), 77–84. 10.1111/j.1471-6712.1987.tb00603.x [DOI] [PubMed] [Google Scholar]
- Forsell, M. , Sjögren, P. , & Johansson, O. (2009). Need of assistance with daily oral hygiene measures among nursing home resident elderly versus the actual assistance received from the staff. The Open Dentistry Journal, 3, 241–244. 10.2174/1874210600903010241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsell, M. , Sjögren, P. , Kullberg, E. , Johansson, O. , Wedel, P. , Herbst, B. , & Hoogstraate, J. (2011). Attitudes and perceptions towards oral hygiene tasks among geriatric nursing home staff. International Journal of Dental Hygiene, 9(3), 199–203. 10.1111/j.1601-5037.2010.00477.x [DOI] [PubMed] [Google Scholar]
- Glick, M. , Williams, D. M. , Kleinman, D. V. , Vujicic, M. , Watt, R. G. , & Weyant, R. J. (2016). A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. International Dental Journal, 66(6), 322–324. 10.1111/idj.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grönbeck Linden, I. , Hägglin, C. , Gahnberg, L. , & Andersson, P. (2017). Factors affecting older persons' ability to manage oral hygiene: A qualitative study. JDR Clinical & Translational Research, 2(3), 223–232. 10.1177/2380084417709267 [DOI] [PubMed] [Google Scholar]
- Grönbeck‐Linden, I. , Hägglin, C. , Petersson, A. , Linander, P. O. , & Gahnberg, L. (2016). Discontinued dental attendance among elderly people in Sweden. Journal of International Society of Preventive & Community Dentistry, 6(3), 224–229. 10.4103/2231-0762.183101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hägglund, P. , Koistinen, S. , Olai, L. , Ståhlnacke, K. , Wester, P. , & Levring Jäghagen, E. (2019). Older people with swallowing dysfunction and poor oral health are at greater risk of early death. Community Dentistry and Oral Epidemiology, 47(6), 494–550. 10.1111/cdoe.12491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmén, A. , Strömberg, E. , Hagman‐Gustafsson, M. L. , Wårdh, I. , & Gabre, P. (2012). Oral status in home‐dwelling elderly dependent on moderate or substantial supportive care for daily living: Prevalence of edentulous subjects, caries and periodontal disease. Gerodontology, 29(2), e503–511. 10.1111/j.1741-2358.2011.00507.x [DOI] [PubMed] [Google Scholar]
- Johansson, I. , Jansson, H. , & Lindmark, U. (2016). Oral health status of older adults in Sweden receiving elder care: Findings from nursing assessments. Nursing Research, 65(3), 215–223. 10.1097/nnr.0000000000000158 [DOI] [PubMed] [Google Scholar]
- Kisely, S. , Quek, L. H. , Pais, J. , Lalloo, R. , Johnson, N. W. , & Lawrence, D. (2011). Advanced dental disease in people with severe mental illness: Systematic review and meta‐analysis. British Journal of Psychiatry, 199(3), 187–193. 10.1192/bjp.bp.110.081695 [DOI] [PubMed] [Google Scholar]
- Konradsen, H. , Trosborg, I. , Christensen, L. , & Pedersen, P. U. (2012). Oral status and the need for oral health care among patients hospitalised with acute medical conditions. Journal of Clinical Nursing, 21(19–20), 2851–2859. 10.1111/j.1365-2702.2012.04197.x [DOI] [PubMed] [Google Scholar]
- Konradsen, H. , Trosborg, I. , Christensen, L. , & Pedersen, P. U. (2014). Evaluation of interrater reliability assessing oral health in acute care settings. International Journal of Nursing Practice, 20(3), 258–264. 10.1111/ijn.12140 [DOI] [PubMed] [Google Scholar]
- Lindqvist, L. , Seleskog, B. , Wårdh, I. , & von Bültzingslöwen, I. (2013). Oral care perspectives of professionals in nursing homes for the elderly. International Journal of Dental Hygiene, 11(4), 298–305. 10.1111/idh.12016 [DOI] [PubMed] [Google Scholar]
- Miegel, K. , & Wachtel, T. (2009). Improving the oral health of older people in long‐term residential care: A review of the literature. International Journal of Older People Nursing, 4(2), 97–113. 10.1111/j.1748-3743.2008.00150.x [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Social Affairs . (2013). Godkännande av en överenskommelse om en sammanhållen vård och omsorg om de mest sjuka äldre. (In Swedish) [Approval of an agreement on coherent care and care for the most ill elderly] (S2013/8803/FST). Stockholm, Sweden Swedish Parliament. Retrieved from https://www.regeringen.se/49b6cc/contentassets/5df6b5d01aa343bbb11d314f9962ae31/godkannande‐av‐en‐overenskommelse‐om‐en‐sammanhallen‐vard‐och‐omsorg‐om‐de‐mest‐sjuka‐aldre‐2013‐s20128765fst
- Miura, H. , Yamasaki, K. , Morizaki, N. , Moriya, S. , & Sumi, Y. (2010). Factors influencing oral health‐related quality of life (OHRQoL) among the frail elderly residing in the community with their family. Archives of Gerontology and Geriatrics, 51(3), e62–65. 10.1016/j.archger.2009.12.003 [DOI] [PubMed] [Google Scholar]
- Murray Thomson, W. (2014). Epidemiology of oral health conditions in older people. Gerodontology, 31(Suppl 1), 9–16. 10.1111/ger.12085 [DOI] [PubMed] [Google Scholar]
- National Board of Health and Welfare (2019). Statistikdatabas för äldreomsorg (In Swedish) [Statistical databases for geriatric care]. Retrieved from https://sdb.socialstyrelsen.se/if_ald/.
- Norderyd, O. , Koch, G. , Papias, A. , Köhler, A. A. , Helkimo, A. N. , Brahm, C. O. , Frisk, F. (2015). Oral health of individuals aged 3–80 years in Jonkoping, Sweden during 40 years (1973–2013). II. Review of clinical and radiographic findings. Swedish Dental Journal, 39(2), 69–86. [PubMed] [Google Scholar]
- Petersen, P. E. , Bourgeois, D. , Ogawa, H. , Estupinan‐Day, S. , & Ndiaye, C. (2005). The global burden of oral diseases and risks to oral health. Bulletin of the World Health Organization, 83(9), 661–669. s0042‐96862005000900011 [PMC free article] [PubMed] [Google Scholar]
- Petersen, P. E. , & Yamamoto, T. (2005). Improving the oral health of older people: The approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology, 33(2), 81–92. 10.1111/j.1600-0528.2004.00219.x [DOI] [PubMed] [Google Scholar]
- Ribeiro, M. T. , Ferreira, R. C. , Vargas, A. M. , & Ferreira e Ferreira, E. (2014). Validity and reproducibility of the revised oral assessment guide applied by community health workers. Gerodontology, 31(2), 101–110. 10.1111/ger.12014 [DOI] [PubMed] [Google Scholar]
- Rosén, M. (2010). Översyn av de nationella kvalitetsregistren ‐ Guldgruvan i hälso‐ och sjukvården. Förslag till gemensam satsning 2011–2015. (In Swedish) [The gold mine in the healthcare proposal proposes joint investment in 2011–2015]. Retrieved from https://webbutik.skr.se/bilder/artiklar/pdf/7164‐613‐2.pdf?issuusl=ignore
- Rubenstein, L. Z. , Harker, J. O. , Salvà, A. , Guigoz, Y. , & Vellas, B. (2001). Screening for undernutrition in geriatric practice: Developing the short‐form mini‐nutritional assessment (MNA‐SF). Journals of Gerontology, 56(6), M366–372. 10.1093/gerona/56.6.m366 [DOI] [PubMed] [Google Scholar]
- Scannapieco, F. A. , & Cantos, A. (2016). Oral inflammation and infection and chronic medical diseases: Implications for the elderly. Periodontology 2000, 72(1), 153–175. 10.1111/prd.12129 [DOI] [PubMed] [Google Scholar]
- Statistics Sweden . (2016). Stora insatser krävs för att klara 40‐talisternas äldreomsorg. (In Swedish) [Great efforts are needed to cope with the elderly care of the 1940s baby boomers]. Retrieved from https://www.scb.se/hitta‐statistik/artiklar/2016/Stora‐insatser‐kravs‐for‐att‐klara‐40‐talisternas‐aldreomsorg/
- Strömberg, E. , Hagman‐Gustafsson, M. L. , Holmén, A. , Wårdh, I. , & Gabre, P. (2012). Oral status, oral hygiene habits and caries risk factors in home‐dwelling elderly dependent on moderate or substantial supportive care for daily living. Community Dentistry and Oral Epidemiology, 40(3), 221–229. 10.1111/j.1600-0528.2011.00653.x [DOI] [PubMed] [Google Scholar]
- Trinks, A. , Hägglin, C. , Nordvall, D. , Rothenberg, E. , & Wijk, H. (2018). The impact of a national quality register in the analysis of risks and adverse events among older adults in nursing homes and hospital wards—a Swedish Senior Alert survey. Safety in Health, 4(1), 10. 10.1186/s40886-018-0077-x [DOI] [Google Scholar]
- United Nations . (2015). World population ageing, 2015. New York, NY: United States: Department of Economic and Social Affairs, Population Division.
- von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gotzsche, P. C. , & Vandenbroucke, J. P. (2007). The strengthening the reporting of observational studies in epidemiology (strobe) statement: Guidelines for reporting observational studies. Bulletin of the World Health Organization, 85(11), 867–872. 10.2471/blt.07.045120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wårdh, I. , Andersson, L. , & Sörensen, S. (1997). Staff attitudes to oral health care. A comparative study of registered nurses, nursing assistants and home care aides. Gerodontology, 14(1), 28–32. [DOI] [PubMed] [Google Scholar]
- Wårdh, I. , Jonsson, M. , & Wikström, M. (2012). Oral care perspectives of professionals in nursing homes for the elderly. Gerodontology, 29(2), e787–792. 10.1111/j.1741-2358.2011.00562.x [DOI] [PubMed] [Google Scholar]
- WHO (2000). Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization Technical Report Series, 894, i–xii, 1–253. [PubMed] [Google Scholar]
- Zenthöfer, A. , Rammelsberg, P. , Cabrera, T. , & Hassel, A. J. (2014). Increasing dependency of older people in nursing homes is associated with need for dental treatments. Neuropsychiatric Disease and Treatment, 10, 2285–2290. 10.2147/ndt.S71184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuluaga, D. J. , Ferreira, J. , Montoya, J. A. , & Willumsen, T. (2012). Oral health in institutionalised elderly people in Oslo, Norway and its relationship with dependence and cognitive impairment. Gerodontology, 29(2), e420–426. 10.1111/j.1741-2358.2011.00490.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1
Data Availability Statement
Data from the Swedish quality register Senior Alert were ordered from the administrator Uppsala Clinical Research Center. Data were also obtained from the National Board of Health and Welfare. The data that support the findings of this study are available from the corresponding author upon reasonable request.


