Abstract
Aims
To explore relationships between mental health problems, mental health shame, self‐compassion and average length of sleep in UK nursing students. The increasing mental health problems in nursing students may be related to a strong sense of shame they experience for having a mental health problem. Self‐compassion has been identified as a protective factor for mental health and shame in other student populations. Further, studies highlight the importance of sleep relating to mental health.
Design
A cross‐sectional design.
Methods
A convenient sampling of 182 nursing students at a university in the East Midlands completed a paper‐based questionnaire regarding these four constructs, from February to April 2019. Correlation, regression and mediation analyses were conducted.
Results
Mental health problems were positively related to shame and negatively related to self‐compassion and sleep. Mental health shame positively predicted and self‐compassion negatively predicted mental health problems: sleep was not a significant predictor of mental health problems. Lastly, self‐compassion completely mediated the impacts of sleep on mental health problems (negative relationship between mental health problems and sleep was fully explained by self‐compassion).
Conclusion
The importance of self‐compassion was highlighted as it can reduce mental health problems and shame. Self‐compassion can protect nursing students from mental distress when they are sleep deprived.
Impact
Nurses and nursing students are required to work irregular hours (e.g. COVID‐19) and mental distress can cause serious consequences in clinical practice. Our findings suggest that nurturing self‐compassion can protect their mental health and the negative impacts of sleep deprivation on mental health.
Keywords: mediation analysis, mental health, mental health shame, nursing students, self‐care, self‐compassion, sleep
1. INTRODUCTION
Nursing is a rewarding but challenging profession. In the UK, nurses are highly respected and at the same time, known to have poor mental health (Kinman et al., 2020). This impairment in mental well‐being can be attributed to a lack of resilience, something that has been recognized and addressed in the new standards of proficiency for nurses (Nursing & Midwifery Council, 2018). One solution for this problem is to educate nursing students about the importance of their own mental well‐being, so that they will be better prepared to cope with occupational stress to protect their mental health, once they are in professional practice (Pulido‐Martos et al., 2012; Reeve et al., 2013). This is essential because not only professional nurses but also nursing students suffer high rates of mental health problems (Hsiung et al., 2019; Lamont et al., 2017). As reported in other healthcare students in the UK (Kotera, Green & Sheffield, 2019a; 2019b), poor mental health of nursing students may be associated with shame about having a mental health problem. Mental health problems may be positively associated with mental health shame in nursing students. Similarly, self‐compassion—understanding and kindness towards oneself—has been identified as a negative correlate and predictor of shame and mental distress in other healthcare students (Authors, 2019a; 2019b). Nursing students who are kind towards themselves may have lower levels of shame and mental health problems. Lastly, recent studies highlight the importance of enough hours of sleep in relation to mental health. Nurses are required to work irregular hours, particularly so during a crisis such as COVID‐19; therefore, evaluating the relationship between sleep and mental health would be useful. Moreover, how a lack of sleep may be associated with mental health has not been explored. Accordingly, this study evaluated the relationship between mental health problems, mental health shame, self‐compassion and sleep, in a cross‐sectional design with correlation, regression and mediation analyses.
2. BACKGROUND
Nursing studies is the study of caring for individuals of all ages, families, groups and communities by promoting health, preventing illness and advocating (Ayala, 2020; International Council of Nurses, 2010). It is one of the most popular subject disciplines in the United Kingdom (UK) and has been so for the past 6 years (Higher Education Statistics Agency, 2019); every year, more than 40,000 prospective students apply (Universities & Colleges Admissions Service, 2019). One notable reason for this popularity is a high employment rate (Van Sabben, 2020): more than 90% of graduates being in employment (i.e. becoming a professional nurse) 6 months after graduation (Higher Education Statistics Agency, 2017; Royal College of Nurses, 2019). Nursing is an attractive profession because of high job satisfaction with over 80% feeling satisfied with their career (AMN Healthcare, 2017), high job security (Buchan et al., 2019) and respect from many patients appreciating the demands of nurses' work (Dolton et al., 2018). As seen in the current coronavirus 2019 (COVID‐19) pandemic, having a sturdy nurse workforce is crucial for the country (Adams & Walls, 2020).
Despite the popularity of nursing programmes in the UK, many nursing students experience mental health problems. Having good mental health is essential for students as it is linked with various student outcomes such as higher academic engagement (Authors, 2019), reduced dropout rate (Hjorth et al., 2016) and higher achievement (Bostani et al., 2014). However, almost a quarter (22%) of nursing students are at risk of developing depression, anxiety, stress or a combination of these (Hsiung et al., 2019). Suicide is reported in 6.5% of nursing students (Aradilla‐Herrero et al., 2014), more than the rate of the general university student population (4.2%) (Sivertsen et al., 2019). In addition to stressors that students in many disciplines experience (stress before examinations and submission deadlines, juggling adult and student identities; Laidlaw et al., 2016; Lipson et al., 2016; Shankland et al., 2019), nursing students experience more pressure to satisfy their academic and professional standards (Findlow, 2012; Gimenez, 2012), which require good performance in academic work and clinical practice where they encounter difficult situations such as death (Jamshidi et al., 2016). Furthermore, demands in the nursing profession have been expanding; more compassionate care for patients and more technical interventions are required for professional nurses today (Nursing & Midwifery Council, 2018). These demands can add pressure on nursing students. Poor mental health is associated with numerous negative consequences: increased risk of suicide and self‐harm (Lipson et al., 2016), limited academic performance, dropping out (Arria et al., 2013; Brydges et al., 2012; Eisenberg et al., 2013) and decreased social connectedness (Eisenberg et al., 2013). Among professional nurses, poor mental health was related to increased risk of medical errors (Melnyk et al., 2018), undermining patient safety and public protection—pivotal elements for fitness to practice in nursing education (Hayes, 2017). This underlines the need for investigating nursing students' mental health.
2.1. Mental health shame
The high rates of mental health problems among nursing may be exacerbated by their “mental health shame” (Kotera, Green & Sheffield, 2019c, p. 136), that is feeling ashamed for having a mental health problem (Kotera, Green & Sheffield, 2019c). Shame is a negative emotion of self‐attributions, based on the perceived evaluation of self by others (Miceli & Castelfranchi, 2018). Mental health shame has been associated with poor mental health in diverse populations including UK social work, psychotherapy, occupational therapy and business students (Kotera, Conway & Van Gordon, 2019; Kotera, Green & Sheffield, 2019a; Kotera, Green & Sheffield, 2019b). Particularly among social work students, mental health shame was strongly associated with increased self‐criticism and decreased self‐compassion (Kotera, Green & Sheffield, 2019a) and a significant predictor of mental health (Kotera, Green & Sheffield, 2019d). Unsurprisingly, students with high mental health shame tend not to seek out help, leading to poor clinical outcomes (Ting, 2013). Despite the strong relationship between mental health problems and mental health shame in various student populations, this relationship in UK nursing students has not been explored to date. Therefore, we hypothesized:
H 1a
Mental health problems are related to mental health shame.
H 2a
Mental health problems are predicted by mental health shame.
2.2. Self‐compassion
Self‐compassion—self‐understanding and self‐kindness aimed at easing suffering during times of hardness (Neff, 2003)—is related to mental health. Self‐compassion improves mental health problems by promoting resilience and decreasing self‐criticism and shame (Braehler et al., 2013; Trompetter et al., 2017). Relating to the three emotion regulatory systems of compassion focused therapy, self‐compassion engages with our soothing system that deals with affects such as safety and contentment to protect our mental health, instead of the other two systems (thread systems and drive systems; both are associated with mental distress) (Gilbert, 2010). This can explain why self‐compassion intervention often employs slow breathing or mindfulness practice, aiming to access our soothing system (Neff & Germer, 2018). Among nursing students in China, self‐compassion was negatively associated with and predicted by anxiety and depression (Luo et al., 2019). In Turkish nursing students, self‐compassion was positively associated with their emotional intelligence (Şenyuva et al., 2014) and negatively correlated with mental distress (Ciarrochi et al., 2002; Resurrección et al., 2014). Among UK student populations, self‐compassion was negatively associated with mental health problems among social work, counselling, occupational therapy and business students (Authors, 2019; Author et al., 2019a; Author et al., 2019b). However, these relationships have not been explored in UK nursing students to date. Accordingly, we hypothesized:
H 1b
Mental health problems are related to self‐compassion.
H 2b
Mental health problems are predicted by self‐compassion.
2.3. Sleep
Poor sleep is common in university students and often results from academic demands and social, personal and employment factors (Cheng et al., 2012). Research into sleep and its health effects has been increasingly developed, reporting that appropriate sleep quantity is positively associated with good mental health (Scott et al., 2017). Having sufficient sleep is also associated with decreased risks for cognitive and emotional health problems (Hirshkowitz et al., 2015a, 2015b). Contrarily, poor sleep increases the risk of stress (Knutson et al., 2017) and mood disorders (e.g. depression and dysthymia) as well as anxiety disorders (e.g. panic disorder and generalized anxiety disorder) (Shi et al., 2020; Stein et al., 2008). Poor sleep is also a predictor of mental health problems (Baglioni et al., 2011). Among professional nurses, who work at night shifts and irregular hours, poor sleep increases the risk of nursing errors in clinical examination and medication administration, possibly leading to serious clinical outcomes (Rahimian & Ghodrati, 2013). Moreover, poor sleep was associated with higher job stress and poorer health status (Lin et al., 2014). Unsurprisingly, regulatory bodies such as the Institute of Medicine noted sleep as an important factor for health of medical staff, relating to the quality of patient care and lower risk of burnout (Ulmer et al., 2008). Sleep was positively associated with self‐compassion and mental health in young health professionals (Kemper et al., 2015). In nursing students, an American study reported that all participating nursing students were sleep‐deprived (n = 179) and more than half (n = 91) were using sleeping‐related medicines (Thomas et al., 2017). Sleep was associated with mental health in Indian nursing students (Menon et al., 2015) and American nursing students (Zhang et al., 2018). Despite the strong relationship between sleep and mental health, no studies have explored the relationship between these factors in UK nursing students:
H 1c
Mental health problems are related to sleep.
H 2c
Mental health problems are predicted by sleep.
2.4. Sleep and self‐compassion
Lastly, sleep has been associated with self‐compassion in German students (Butz & Stahlberg, 2018) and in American young health professionals and trainees (Kemper et al., 2015): individuals who have better sleep reporting higher levels of self‐compassion (Butz & Stahlberg, 2020). Self‐compassion was a protective factor for mental health problems and sleep disturbances among adults over 65 years old in Korea, suggesting that self‐compassionate participants tended to have good mental health and sleep (Kim & Ko, 2018). While these findings imply strong relationships among these three variables, namely mental health, sleep and self‐compassion, how these variables are related to each other has not been explored (e.g. Kemper et al., 2015 explored those variables, however, only correlations with sleep). Considering the strong impact of self‐compassion on mental health (Author, 2019; Author et al., 2019a; Author et al., 2019b), we hypothesized that self‐compassion would mediate the relationship between sleep and mental health problems: the negative impacts of sleep deprivation on mental health can be explained by low levels of self‐compassion:
H 3
Self‐compassion mediates the impacts of sleep on mental health problems.
3. THE STUDY
3.1. Objectives
This study aimed to explore relationships between mental health problems, mental health shame, self‐compassion and sleep in UK nursing students. Mental health was evaluated in terms of depression, anxiety and stress, considering that these are the commonest mental health issues for both the general population (Mental Health Foundation, 2016; Mirzaei et al., 2019) and nursing students (Hsiung et al., 2019). Three hypotheses were established:
H1. Mental health problems are related to mental health shame (a), self‐compassion (b) and sleep (c).
H2. Mental health problems are predicted by mental health shame (a), self‐compassion (b) and sleep (c).
H3. Self‐compassion mediates the impacts of sleep on mental health problems.
3.2. Design
A cross‐sectional design was employed to produce timely output and to investigate all variables altogether. Data were examined through correlation, regression and mediation analyses to test our three hypotheses.
3.3. Participants
Participants needed to be at least 18 years old and studying in a nursing programme at a UK university at the time of the study: students who were on a study break were excluded. Participants were recruited using convenient sampling through hard copy questionnaires distributed by programme tutors instead of the researchers to avoid response biases. Of 198 full‐time students who were introduced to the study, 182 (92%; 144 females, 30 males and 8 did not respond; Age 30.04 ± 8.31 years old, range 18–52 years old; 164 British, 10 Africans, 6 other Europeans and 2 did not respond; 146 undergraduates and 36 postgraduates) completed three mental health measures, satisfying the required sample size calculated by power analysis (84: two tails, p H1 (r) = 0.30 (medium; Cohen, 1988), α = 0.05, Power = 0.80, p H0 = 0; Faul et al., 2009). Compared with the general population of UK nursing students (10%; Office for Students, 2020), our sample recruited slightly more males (16%). No compensation was awarded for completing the survey. Following the ethical guidelines, the withdrawn/incomplete 16 participants were not asked for the reason: no reason nor complaint was received.
3.4. Data collection
Four self‐report measures regarding each construct were used:
Mental health problems were measured using the Depression Anxiety and Stress Scale (DASS21), a shortened version of DASS42 (Lovibond & Lovibond, 1995). DASS21 consists of 21 items on a four‐point Likert scale divided into three seven‐item subscales, depression (e.g. “I couldn't seem to experience any positive feeling at all”), anxiety (e.g. “I felt scared without any good reason”) and stress (e.g. “I felt that I was rather touchy”). High scores indicate poor mental health. These subscales had good reliability; α = 0.87–0.94 (Antony et al., 1998).
Mental health shame was measured using the Attitudes Towards Mental Health Problems (ATMHP), comprising 35 four‐point Likert items. ATMHP consists of four sections: (i) their community's and family's attitudes towards mental health problems (community and family attitudes, e.g. “My community/family sees mental health problems as something to keep secret”), (ii) their perception of how their community and family would perceive them if they had a mental health problem (community and family external shame, e.g. “I think my community/family would look down on me”), (iii) how they perceive themselves if they had a mental health problem (internal shame, e.g. “I would see myself as inferior”) and (iv) how their family would be seen if they had a mental health problem (family‐reflected shame, e.g. “My family would be seen as inferior”) and how worried they become about themselves when a close relative had a mental health problem (self‐reflected shame, e.g. “I would worry that others will look down on me”). High score indicates high shame for mental health problems. All of the subscales had good Cronbach's alphas of between 0.85–0.97 (Gilbert et al., 2007).
Self‐Compassion Scale‐Short Form (SCS‐SF) was used to measure self‐compassion. This self‐report measure is a shortened version of the Self‐Compassion Scale, comprising 12 five‐point Likert items (e.g. “I try to be understanding and patient towards those aspects of my personality I don't like”; Neff, 2003). High score indicates a high level of self‐compassion. Cronbach's alpha was high (0.86; Raes et al., 2011).
Sleep was asked with a one question item “How long do you sleep every day on average?”
3.5. Ethical considerations
Ethics approval was obtained from the University Research Ethics Committee. Because the questionnaire concerned students’ mental health, at least one nursing lecturer who was a registered nurse and was not a co‐researcher of the study, was present at the site. Physical distance among students was maintained for privacy, helping them respond comfortably. Information about available mental health services inside and outside university was offered before and after the study. Visual aids (e.g. large font print, coloured papers) were prepared for students with visual impairments; however, no students used them.
3.6. Data analysis
First, the collected data were screened for outliers and the assumptions of parametric tests. Second, correlations between their mental health, mental health shame, self‐compassion and sleep were explored (H1). Third, multiple regression analysis was performed to examine the relative contribution of mental health shame, self‐compassion and sleep to mental health problems (H2). Finally, mediation analysis was conducted to appraise whether self‐compassion would mediate the relationship between sleep and mental health problems (H3). Analyses were conducted using IBM SPSS version 25.0 and Process Macro (Hayes, 2013).
3.7. Reliability
All scales used were validated with high reliability. Before the present study, the same study design was employed to explore mental health of other healthcare students (Authors 2019; Author et al. 2019b).
4. RESULTS/FINDINGS
No outliers were identified. All variables demonstrated good internal reliability (α = 0.87–0.96; Table 1).
TABLE 1.
Descriptive statistics: Mental health problems, mental health shame, self‐compassion and sleep in UK nursing students (n = 182)
| Scale (Construct) | Subscale (range) | M | SD | α |
|---|---|---|---|---|
| Depression Anxiety and Stress Scale 21 (Mental Health Problems; High score indicates poor mental health) | Mental Health Problems (0–126) | 41.89 | 29.96 | 0.96 |
| Attitudes Towards Mental Health Problems (Mental Health Shame; High score indicates high shame) | Negative Attitudes (0–24) | 6.99 | 5.41 | 0.89 |
| External Shame (0–30) | 8.27 | 7.76 | 0.95 | |
| Internal Shame (0–15) | 6.09 | 3.68 | 0.94 | |
| Reflected Shame (0–36) | 9.77 | 8.05 | 0.91 | |
| Self‐Compassion Scale‐Short Form (Self‐Compassion; High score indicates strong self‐compassion) | Self‐Compassion (1–5) | 2.68 | 0.70 | 0.87 |
| How long do you sleep every day on average?' (Sleep; 2–10 hr in our sample) | 6.78 | 1.30 | ‐ |
4.1. Relationships between mental health, mental health shame, self‐compassion and sleep
As all variables apart from self‐compassion were not normally distributed (Shapiro–Wilk's test, p < .05), data were square‐root‐transformed to satisfy the assumption of normality (Field, 2017). Pearson's correlation was calculated (Table 2).
TABLE 2.
Correlations between mental health, mental health shame, self‐compassion and sleep in UK nursing students (n = 182)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Gender (1 = M, 2 = F) | ‐ | ||||||||
| 2. Age | −0.19* | ‐ | |||||||
| 3. Mental Health Problems | 0.05 | −0.18* | ‐ | ||||||
| 4. Negative Attitudes | −0.14 | 0.05 | 0.30** | ‐ | |||||
| 5. External Shame | −0.10 | 0.02 | 0.27** | 0.71** | ‐ | ||||
| 6. Internal Shame | 0.05 | −0.08 | 0.41** | 0.20** | 0.41** | ‐ | |||
| 7. Reflected Shame | −0.10 | 0.001 | 0.31** | 0.35** | 0.48** | 0.41** | ‐ | ||
| 8. Self‐Compassion | −0.14 | 0.14 | −0.68** | −0.15 | −0.17* | −0.38** | −0.09 | ‐ | |
| 9. Sleep | 0.17* | −0.03 | −0.19** | −0.11 | −0.13 | −0.11 | −0.06 | 0.16* | ‐ |
p < .05,
p < .01.
Mental health problems were positively associated with all the mental health shame subscales (internal shame being the strongest positive correlate) and negatively associated with age, self‐compassion and sleep (self‐compassion being the strongest negative correlate). Additionally, self‐compassion was positively related to sleep and negatively related to external shame and internal shame. Lastly, sleep was associated with female gender. H1 was supported.
4.1.1. Predictors of mental health problems
Multiple regression analyses were conducted to explore the relative contributions of mental health shame, self‐compassion and sleep to mental health problems (Table 3). Mental health shame was calculated by summing all the subscale scores (Author et al., 2019c). First, gender and age were entered to statistically adjust for their effects (step one), and then, mental health shame, self‐compassion and sleep were entered (step two). Adjusted coefficients of determination (Adj. R 2) were reported. Multicollinearity was not a concern (VIF < 10). Mental health shame, self‐compassion and sleep accounted for 50% of the variance for mental health problems indicating a large effect size (Cohen, 1988; F(5, 166) = 39.31, p < .001). Mental health shame was a positive, and self‐compassion was a negative predictor of mental health problems. Self‐compassion predicted mental health problems (B = −6.65) to a larger degree than mental health shame (B = 0.32). Sleep did not predict mental health problems. H2 was partially supported (H2a‐b were supported while H2c was not).
TABLE 3.
Multiple regression: Mental health shame, self‐compassion and sleep to mental health problems among nursing students (n = 182)
| Mental health problems | ||||
|---|---|---|---|---|
| B | SEB | β | 95% CI for B (lower, upper) | |
| Step 1 | ||||
| Gender (1 = M, 2 = F) | 0.15 | 0.49 | 0.02 | −0.82, 1.11 |
| Age | −0.60* | 0.25 | −0.18 | −1.10, −0.11 |
| Step 2 | ||||
| Gender (1 = M, 2 = F) | −0.06 | 0.35 | −0.01 | −0.75, 0.63 |
| Age | −0.33 | 0.18 | −0.10 | −0.68, 0.02 |
| Mental Health Shame | 0.32*** | 0.07 | 0.25 | 0.18, 0.47 |
| Self‐Compassion | −6.65*** | 0.63 | −0.60 | −7.88, −5.41 |
| Sleep | −0.44 | 0.50 | −0.05 | −1.44, 0.55 |
Δ Adjusted R 2 = .50.
B, unstandardized regression coefficient; SEB, standard error of the coefficient; β, standardized coefficient.
p<.05;
p<.001.
4.1.2. Mediation of self‐compassion between sleep and mental health problems
Lastly, a mediation analysis was conducted to appraise whether the relationship between sleep (predictor variable) and mental health problems (outcome variable) was mediated by self‐compassion (mediator variable), using model 4 in the Process macro (parallel mediation model; Hayes, 2013) (Figure 1).
FIGURE 1.
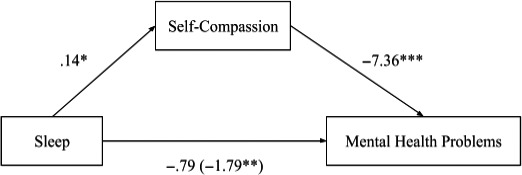
Self‐compassion completely mediates sleep and mental health problems. Direct effect (total effect) of sleep on mental health problems. Parallel mediation: sleep as a predictor of mental health problems, mediated by self‐compassion. The confidence interval for the indirect effect is a BCa‐bootstrapped CI based on 5,000 samples. Values attached to arrows are coefficients indicating impacts. *p < .05, **p < .01, ***p < .001
While the direct effects of sleep on mental health problems were not significant (b = −0.79, t(179) = −1.54, p = .13), the total effects and indirect effects of sleep on mental health problems were significant (total b = −1.79, t(180) = −2.63, p = .009; indirect b = −1.00, BCa CI [−1.94, −0.20]). An increase in sleep was associated with an increase in self‐compassion, which then was associated with a decrease in mental health problems. Self‐compassion completely mediated the effect of sleep on mental health problems. H3 was supported.
5. DISCUSSION
This study explored relationships between mental health problems, mental health shame, self‐compassion and sleep in UK nursing students. Mental health problems were positively associated with mental health shame and negatively associated with self‐compassion and sleep (H1 was supported). Mental health shame and self‐compassion were significant predictors of mental health problems and sleep was not (H2 was partially supported; while H2a‐b were supported, H2c was not). Lastly, self‐compassion completely mediated the impact of sleep on mental health problems (H3 was supported). Relevancy to practice and future research were discussed for each item, as suggested in a review explored mental health in nurses (Edwards & Burnard, 2003).
5.1. Complete mediation of self‐compassion in sleep and mental health problems
One of the original values this study offers is that the negative association between sleep and mental health problems (i.e. students who sleep long tend to have good mental health) was explained by self‐compassion. It was not sleep by itself that had an impact on mental health: it was self‐compassion that impacted mental health. Short sleep negatively impacted self‐compassion, which then damaged mental health. Recently, the relationship between sleep and mental health (Menon et al., 2015; Zhang et al., 2018) and sleep and self‐compassion (Butz & Stahlberg, 2018; Kemper et al., 2015) has been reported. However, how these three variables are related to each other had not been explored (e.g. Kemper et al., 2015 explored sleep's correlations with mental health and self‐compassion separately). Indeed, sleep was correlated with both mental health and self‐compassion in our sample too, and we further identified that self‐compassion was a complete mediator between the two. This suggests the importance of incorporating self‐compassion in nursing curricula: when in employment many graduates will be required to work night shifts and irregular hours, leading to sleep deprivation and sleep problems (Stanojevic et al., 2016) and therefore, as our analyses show, increasing their risk of mental health problems. An example of sleep deprivation in nurses is the coronavirus disease 2019 (COVID‐19) pandemic; sleep deprivation occurred despite nurses being aware of its effect on mental health (Sun et al., 2020; Zhang et al., 2020). In addition, self‐compassion would facilitate nursing students to report mental health problems (Lipson et al., 2016). Therefore, nursing students developing skills to practise self‐compassion will allow them to maintain good mental health both during their studies and when in employment. For example, an eight‐week self‐compassion training (2.5 hr each) increased self‐compassion and reduced mental distress among UK nurses (Delaney, 2018). Likewise, an eight‐week self‐compassion training (1.5 hr each) increased self‐compassion in Iranian nursing students (Khorami et al., 2016). This type of training being embedded in nursing curricula will help nursing students prepare for the demanding nursing practice. New competency standards for registered nurses have recently been implemented, focusing on emotional resilience and emotional intelligence (Nursing & Midwifery Council, 2018). Though compassionate care for patients is noted as important, self‐compassion is not highlighted in these standards. Considering that self‐compassion is a better predictor of mental health than emotional resilience among UK social work students (Author et al., 2019d), UK nursing students may benefit from practising self‐compassion. Moreover, future research should evaluate the effects of self‐compassion training on sleep and mental health for nursing students.
5.2. Importance of self‐compassion and challenges in implementation
In line with previous findings from other healthcare students (Kotera, Green & Sheffield, 2019a; Kotera, Green & Sheffield, 2019b), mental health problems were positively related to and predicted by mental health shame and negatively related to and predicted by self‐compassion. These findings suggest that reducing mental health shame and cultivating self‐compassion would be helpful for nursing students to maintain good mental health. Mental health education is needed for nursing students to reduce mental health shame. Recent findings demonstrated that the risk of depression was not related to whether the person is weak or inadequate; instead, it was related to social components including fatigue and stress (Kobayashi et al., 2020). Having the right knowledge about mental health can help to reduce mental health shame that nursing students may have. Moreover, as increased self‐compassion is associated with a lower level of shame (Sedighimornani et al., 2019), developing self‐compassion would be a helpful approach for nursing students to protect their mental health. By cultivating self‐compassion, nursing students can reduce their mental health shame and mental health problems.
Despite self‐compassion already being taught in other caring professions (Nelson et al., 2018), educators need to be aware of the challenges of nurturing self‐care in nursing curricula: in nursing, taking care of oneself is stigmatized (Glass & Rose, 2008) and sometimes referred to as “responsible selfishness” (Adam & Taylor, 2014). In line with the authors’ experience of teaching self‐compassion to healthcare students, many students feel guilty about taking care of themselves. Therefore, theoretical understanding, before practising exercises, may be important. For example, Watson’s (2008) Theory of Human Caring describes that nurses’ care for self and others is interdependent, suggesting a need for self‐care for nurses (Mills et al., 2015). To offer compassion for others, we need to offer compassion to ourselves first, as caring for others requires caring for oneself (Dalai Lama, 2003; Lloyd et al., 2019). The importance of self‐care in nursing is highlighted in the competency standards for registered nurses established by the International Council of Nurses (Alexander & Runciman, 2003). However, in many countries, including the UK, self‐care is not emphasized (e.g. the competency standards for registered nurses by the Nursing & Midwifery Council, 2018 does not emphasize self‐care). Recently, partly because of the COVID‐19 pandemic, the importance of nursing has been recognized more (Ford, 2020) and the stigma of taking care of oneself may be diminishing. Educators in the UK nursing programmes can take advantage of this to incorporate a self‐care component into their curriculum.
Lastly, the full mediation of self‐compassion in the relationship between sleep and mental health problems may offer helpful insight for nursing students who are sleep deprived. While previously believed that insufficient sleep leads to poor mental health, our analyses did not find a direct linkage between sleep and mental health problems. This may mitigate the noebo effects of sleep deprivation, by which students believe that their mental health should suffer when they fail to secure enough sleep (Weimer et al., 2020). Our findings suggest that if a student has a strong self‐compassion, the impacts of sleep deprivation on mental health can be minimum; therefore, the student does not have to believe that they would not feel good on that day.
5.3. Limitations
While this study offers helpful insights into the mental health of UK nursing students, several limitations should be noted. First, our sample was recruited through convenient sampling from one UK university, which limits the generalizability of our findings (e.g. our sample recruited more males than the general sample of UK nursing students). Second, self‐report measures were used, which restricts the accuracy of participant responses for social desirability bias (Authors, 2020). Further, we only evaluated the length of sleep; other aspects of sleep (e.g. sleep quality and efficiency and time in bed) were not considered. Also, self‐compassion was measured using the Self‐Compassion Scale‐Short Form (Raes et al., 2011), which has been debated for its accuracy (Authors, 2020). Likewise, mental health problems were assessed using the total scale of DASS21; however, difference among depression, anxiety and stress has been debated, thus should be considered (Magalhaes et al., 2010). Lastly, because we employed a cross‐sectional design, the causal direction of the relationships among these variables could not be ascertained. Longitudinal studies would be useful to identify the causality.
6. CONCLUSION
Nursing is one of the most popular subjects in the UK partly because of good graduate prospects. Despite the popularity, many nursing students live with mental health problems. We found that mental health problems were positively associated with mental health shame and negatively associated with self‐compassion and sleep length (H1a‐c). Mental health shame was a positive predictor, and self‐compassion was a negative predictor of mental health problems (H2a‐b). Lastly, self‐compassion completely mediated the relationship between sleep and mental health problems (H3). Our findings suggest the importance of self‐compassion for nursing students and recommend self‐compassion training to be embedded in the current nursing curriculum, while addressing guilt for self‐care by introducing self‐care theories. Further, the UK nursing competency standards can support practising nurses more by further emphasizing self‐care, as is done in the international framework.
CONFLICTS OF INTEREST
No potential conflict of interest was reported by the authors.
AUTHOR CONTRIBUTIONS
YK: Substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data. VC and JC: Drafting the manuscript or revising it critically for important intellectual content. YK, VC, JC and DF: Given final approval of the version to be published and accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Funding information
The authors received no financial support for the research.
Kotera Y, Cockerill V, Chircop JGE, Forman D. Mental health shame, self‐compassion and sleep in UK nursing students: Complete mediation of self‐compassion in sleep and mental health. Nurs Open.2021;8:1325–1335. 10.1002/nop2.749
DATA AVAILABILITY STATEMENT
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- Adam, D. , & Taylor, R. (2014). Compassionate care: Empowering students through nurse education. Nurse Education Today, 34(9), 1242–1245. 10.1016/j.nedt.2013.07.011 [DOI] [PubMed] [Google Scholar]
- Adams, J. G. , & Walls, R. M. (2020). Supporting the health care workforce during the COVID‐19 global epidemic. JAMA, 323(15), 1439. 10.1001/jama.2020.3972 [DOI] [PubMed] [Google Scholar]
- Alexander, M. , & Runciman, P. (2003). ICN framework of competencies for the generalist nurse: Report of the development process and consultation. International Council of Nurses. [Google Scholar]
- AMN Healthcare . (2017). 2017 Survey of Registered Nurses: Viewpoints on leadership, nursing shortages and their profession. AMN Healthcare. [Google Scholar]
- Antony, M. M. , Bieling, P. J. , Cox, B. J. , Enns, M. W. , & Swinson, R. P. (1998). Psychometric properties of the 42‐item and 21‐item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment, 10(2), 176–181. 10.1037/1040-3590.10.2.176 [DOI] [Google Scholar]
- Aradilla‐Herrero, A. , Tomás‐Sábado, J. , & Gómez‐Benito, J. (2014). Associations between emotional intelligence, depression and suicide risk in nursing students. Nurse Education Today, 34(4), 520–525. 10.1016/j.nedt.2013.07.001 [DOI] [PubMed] [Google Scholar]
- Arria, A. M. , Caldeira, K. M. , Vincent, K. B. , Winick, E. R. , Baron, R. A. , & O'Grady, K. E. (2013). Discontinuous college enrollment: Associations with substance use and mental health. Psychiatric Services, 64(2), 165–172. 10.1176/appi.ps.201200106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayala, R. A. (2020). Towards a sociology of nursing. Springer. 10.1007/978-981-13-8887-3 [DOI] [Google Scholar]
- Baglioni, C. , Battagliese, G. , Feige, B. , Spiegelhalder, K. , Nissen, C. , Voderholzer, U. , Lombardo, C. , & Riemann, D. (2011). Insomnia as a predictor of depression: A meta‐analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders, 135(1‐3), 10–19. 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- Bostani, M. , Nadri, A. , & Nasab, A. R. (2014). A study of the relation between mental health and academic performance of students of the Islamic Azad University Ahvaz Branch. Procedia ‐ Social and Behavioral Sciences, 116, 163–165. 10.1016/j.sbspro.2014.01.186 [DOI] [Google Scholar]
- Braehler, C. , Gumley, A. , Harper, J. , Wallace, S. , Norrie, J. , & Gilbert, P. (2013). Exploring change processes in compassion focused therapy in psychosis: Results of a feasibility randomized controlled trial. British Journal of Clinical Psychology, 52(2), 199–214. 10.1111/bjc.12009 [DOI] [PubMed] [Google Scholar]
- Brydges, R. , Butler, D. , Studnek, J. J. R. J. R. , Fernandez, A. R. , Shimberg, B. , Garifo, M. et al (2012). Nursing student retention: Understanding the process and making a difference. In the National Association of EMS Educators Annual Meeting. 10.14507/epaa.v10n18.2002 [DOI]
- Buchan, J. , Charlesworth, A. , Gershlick, B. , & Seccombe, I. (2019). A critical moment: NHS staffing trends, retention and attrition. Health.Org.Uk. [Google Scholar]
- Butz, S. , & Stahlberg, D. (2018). Can self‐compassion improve sleep quality via reduced rumination? Self and Identity, 17(6), 666–686. 10.1080/15298868.2018.1456482 [DOI] [Google Scholar]
- Butz, S. , & Stahlberg, D. (2020). The relationship between self‐compassion and sleep quality: An overview of a seven‐year German research program. Behavioral Sciences, 10(3), 64. 10.3390/bs10030064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, S. H. , Shih, C. C. , Lee, I. H. , Hou, Y. W. , Chen, K. C. , Chen, K.‐T. , Yang, Y. K. , & Yang, Y. C. (2012). A study on the sleep quality of incoming university students. Psychiatry Research, 197(3), 270–274. 10.1016/j.psychres.2011.08.011 [DOI] [PubMed] [Google Scholar]
- Ciarrochi, J. , Deane, F. P. , & Anderson, S. (2002). Emotional intelligence moderates the relationship between stress and mental health. Personality and Individual Differences, 32(2), 197–209. 10.1016/S0191-8869(01)00012-5 [DOI] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. L. Erlbaum Associates. [Google Scholar]
- Dalai Lama . (2003). Transforming the mind: Teachings on generating compassion. Thorsons. [Google Scholar]
- Delaney, M. C. (2018). Caring for the caregivers: Evaluation of the effect of an eight‐week pilot mindful self‐compassion (MSC) training program on nurses’ compassion fatigue and resilience. PLoS One, 13(11), e0207261. 10.1371/journal.pone.0207261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolton, P. , Marcenaro, O. , De Vries, R. , & She, P.‐W. (2018). Global Teacher Status Index 2018. Education Journal. [Google Scholar]
- Edwards, D. , & Burnard, P. (2003). A systematic review of stress and stress management interventions for mental health nurses. Journal of Advanced Nursing, 42(2), 169–200. 10.1046/j.1365-2648.2003.02600.x [DOI] [PubMed] [Google Scholar]
- Eisenberg, D. , Hunt, J. , & Speer, N. (2013). Mental health in American colleges and universities: Variation across student subgroups and across campuses. Journal of Nervous and Mental Disease, 201(1), 60–67. 10.1097/NMD.0b013e31827ab077 [DOI] [PubMed] [Google Scholar]
- Faul, F. , Erdfelder, E. , Buchner, A. , & Lang, A.‐G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Field, A. P. (2017). Discovering statistics using IBM SPSS statistics. Sage. [Google Scholar]
- Findlow, S. (2012). Higher education change and professional‐academic identity in newly “academic” disciplines: The case of nurse education. Higher Education, 63(1), 117–133. 10.1007/s10734-011-9449-4 [DOI] [Google Scholar]
- Ford, M. (2020). Calls to recognise student nursing response to Covid‐19 by wiping fees. Nursing Times. Retrieved from https://www.nursingtimes.net/news/education/calls-to-recognise-student-nursing-response-to-covid-19-by-wiping-fees-07-05-2020/ [Google Scholar]
- Gilbert, P. (2010). The compassionate mind: A new approach to life's challenges. Constable. [Google Scholar]
- Gilbert, P. , Bhundia, R. , Mitra, R. , McEwan, K. , Irons, C. , & Sanghera, J. (2007). Cultural differences in shame‐focused attitudes towards mental health problems in Asian and Non‐Asian student women. Mental Health, Religion & Culture, 10(2), 127–141. 10.1080/13694670500415124 [DOI] [Google Scholar]
- Gimenez, J. (2012). Disciplinary epistemologies, generic attributes and undergraduate academic writing in nursing and midwifery. Higher Education, 63(4), 401–419. 10.1007/s10734-011-9447-6 [DOI] [Google Scholar]
- Glass, N. , & Rose, J. (2008). Enhancing emotional well‐being through self‐care: The experiences of community health nurses in Australia. Holistic Nursing Practice, 22(6), 336–347. 10.1097/01.HNP.0000339345.26500.62 [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2013). Introduction to mediation, moderation and conditional process analysis: A regression‐based approach. [Google Scholar]
- Hayes, J.‐A. (2017). Values‐based nursing and fitness to practice issues BT – Key concepts and issues in nursing ethics. Springer International Publishing. 10.1007/978-3-319-49250-6_13 [DOI] [Google Scholar]
- Higher Education Statistics Agency . (2017). Destinations of leavers from Higher Education in the United Kingdom for the academic year 2016/17. HESA. Retrieved from https://www.hesa.ac.uk/news/19-07-2018/DLHE-publication-201617 [Google Scholar]
- Higher Education Statistics Agency . (2019). What do HE students study? Higher Education Statistics Agency. Retrieved from https://www.hesa.ac.uk/data-and-analysis/students/what-study [Google Scholar]
- Hirshkowitz, M. , Whiton, K. , Albert, S. M. , Alessi, C. , Bruni, O. , DonCarlos, L. , Hazen, N. , Herman, J. , Adams Hillard, P. J. , Katz, E. S. , Kheirandish‐Gozal, L. , Neubauer, D. N. , O’Donnell, A. E. , Ohayon, M. , Peever, J. , Rawding, R. , Sachdeva, R. C. , Setters, B. , Vitiello, M. V. , & Ware, J. C. (2015a). National Sleep Foundation's updated sleep duration recommendations: Final report. Sleep Health, 1(4), 233–243. 10.1016/j.sleh.2015.10.004 [DOI] [PubMed] [Google Scholar]
- Hirshkowitz, M. , Whiton, K. , Albert, S. M. , Alessi, C. , Bruni, O. , DonCarlos, L. , Hazen, N. , Herman, J. , Katz, E. S. , Kheirandish‐Gozal, L. , Neubauer, D. N. , O'Donnell, A. E. , Ohayon, M. , Peever, J. , Rawding, R. , Sachdeva, R. C. , Setters, B. , Vitiello, M. V. , Ware, J. C. , & Adams Hillard, P. J. (2015b). National sleep foundation's sleep time duration recommendations: Methodology and results summary. Sleep Health, 1(1), 40–43. 10.1016/j.sleh.2014.12.010 [DOI] [PubMed] [Google Scholar]
- Hjorth, C. F. , Bilgrav, L. , Frandsen, L. S. , Overgaard, C. , Torp‐Pedersen, C. , Nielsen, B. , & Bøggild, H. (2016). Mental health and school dropout across educational levels and genders: A 4.8‐year follow‐up study. BMC Public Health, 16(1). 10.1186/s12889-016-3622-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiung, D. Y. , Tsai, C. L. , Chiang, L. C. , & Ma, W. F. (2019). Screening nursing students to identify those at high risk of poor mental health: A cross‐sectional survey. British Medical Journal Open, 9(6), e025912. 10.1136/bmjopen-2018-025912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Council of Nurses . (2010). Definition of nursing. Retrieved from https://www.icn.ch/nursing-policy/nursing-definitions [Google Scholar]
- Jamshidi, N. , Molazem, Z. , Sharif, F. , Torabizadeh, C. , & Kalyani, M. N. (2016). The challenges of nursing students in the clinical learning environment: A qualitative study. The Scientific World Journal, 2016, 1–7. 10.1155/2016/1846178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemper, K. J. , Mo, X. , & Khayat, R. (2015). Are mindfulness and self‐compassion associated with sleep and resilience in health professionals? Journal of Alternative and Complementary Medicine, 21(8), 496–503. 10.1089/acm.2014.0281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khorami, E. S. , Moeini, M. , & Ghamarani, A. (2016). The effectiveness of self‐compassion training: A field trial. Global Journal of Medicine Researches and Studies, 3(1), 15–20. [Google Scholar]
- Kim, C. , & Ko, H. (2018). The impact of self‐compassion on mental health, sleep, quality of life and life satisfaction among older adults. Geriatric Nursing, 39(6), 623–628. 10.1016/j.gerinurse.2018.06.005 [DOI] [PubMed] [Google Scholar]
- Kinman, G. , Teoh, K. , & Harriss, A. (2020). The mental health and wellbeing of nurses and midwives in the United Kingdom. The Society of Occupational Medicine. [Google Scholar]
- Knutson, K. L. , Phelan, J. , Paskow, M. J. , Roach, A. , Whiton, K. , & Langer, G. , Hillygus, D. S. , Mokrzycki, M. , Broughton, W. A. , Chokroverty, S. , Lichstein, K. L. , Weaver, T. E. , & Hirshkowitz, M. (2017). The National Sleep Foundation's Sleep Health Index. Sleep Health, 3(4), 234–240. 10.1016/j.sleh.2017.05.011 [DOI] [PubMed] [Google Scholar]
- Kobayashi, N. , Oka, N. , Takahashi, M. , Shimada, K. , Ishii, A. , Tatebayashi, Y. , Shigeta, M. , Yanagisawa, H. , & Kondo, K. (2020). Human Herpesvirus 6B greatly increases risk of depression by activating Hypothalamic‐Pituitary‐Adrenal Axis during latent phase of infection. Iscience, 23(6), 101187. 10.1016/j.isci.2020.101187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotera, Y. , Conway, E. , & Van Gordon, W. (2019). Mental health of UK university business students: Relationship with shame, motivation and self‐compassion. Journal of Education for Business, 94(1), 11–20. 10.1080/08832323.2018.1496898 [DOI] [Google Scholar]
- Kotera, Y. , Green, P. , & Sheffield, D. (2019a). Mental health attitudes, self‐criticism, compassion, and role identity among UK social work students. British Journal of Social Work, 49(2), 351–370. 10.1093/bjsw/bcy072 [DOI] [Google Scholar]
- Kotera, Y. , Green, P. , & Sheffield, D. (2019b). Mental health of therapeutic students: Relationships with attitudes, self‐criticism, self‐compassion, and caregiver identity. British Journal of Guidance and Counselling, 10.1080/03069885.2019.1704683 [DOI] [Google Scholar]
- Kotera, Y. , Green, P. , & Sheffield, D. (2019c). Mental health shame of UK construction workers: Relationship with masculinity, work motivation, and self‐compassion. Journal of Work and Organizational Psychology, 35(2), 135–143. 10.5093/jwop2019a15 [DOI] [Google Scholar]
- Kotera, Y. , Green, P. , & Sheffield, D. (2019d). Roles of positive psychology for mental health in UK social work students: Self‐compassion as a predictor of better mental health. British Journal of Social Work, 10.1093/bjsw/bcz149 [DOI] [Google Scholar]
- Laidlaw, A. , McLellan, J. , & Ozakinci, G. (2016). Understanding undergraduate student perceptions of mental health, mental well‐being and help‐seeking behaviour. Studies in Higher Education, 41(12), 2156–2168. 10.1080/03075079.2015.1026890 [DOI] [Google Scholar]
- Lamont, S. , Brunero, S. , Perry, L. , Duffield, C. , Sibbritt, D. , Gallagher, R. , & Nicholls, R. (2017). ‘Mental health day’ sickness absence amongst nurses and midwives: Workplace, workforce, psychosocial and health characteristics. Journal of Advanced Nursing, 73(5), 1172–1181. 10.1111/jan.13212 [DOI] [PubMed] [Google Scholar]
- Lin, S. H. , Liao, W. C. , Chen, M. Y. , & Fan, J. Y. (2014). The impact of shift work on nurses' job stress, sleep quality and self‐perceived health status. Journal of Nursing Management, 22(5), 604–612. 10.1111/jonm.12020 [DOI] [PubMed] [Google Scholar]
- Lipson, S. K. , Zhou, S. , Wagner, B. , Beck, K. , & Eisenberg, D. (2016). Major differences: Variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. Journal of College Student Psychotherapy, 30(1), 23–41. 10.1080/87568225.2016.1105657 [DOI] [Google Scholar]
- Lloyd, J. , Muers, J. , Patterson, T. G. , & Marczak, M. (2019). Self‐compassion, coping strategies and caregiver burden in caregivers of people with dementia. Clinical Gerontologist, 42(1), 47–59. 10.1080/07317115.2018.1461162 [DOI] [PubMed] [Google Scholar]
- Lovibond, S. , & Lovibond, P. (1995). Manual for the depression anxiety stress scales (2nd ed.). Psychology Foundation of Australia. [Google Scholar]
- Luo, Y. , Meng, R. , Li, J. , Liu, B. , Cao, X. , & Ge, W. (2019). Self‐compassion may reduce anxiety and depression in nursing students: A pathway through perceived stress. Public Health, 174, 1–10. 10.1016/j.puhe.2019.05.015 [DOI] [PubMed] [Google Scholar]
- Magalhaes, A. C. , Holmes, K. D. , Dale, L. B. , Comps‐Agrar, L. , Lee, D. , Yadav, P. N. , Drysdale, L. , Poulter, M. O. , Roth, B. L. , Pin, J.‐P. , Anisman, H. , & Ferguson, S. S. G. (2010). CRF receptor 1 regulates anxiety behavior via sensitization of 5‐HT2 receptor signaling. Nature Neuroscience, 13(5), 622–629. 10.1038/nn.2529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk, B. M. , Orsolini, L. , Tan, A. , Arslanian‐Engoren, C. , Melkus, G. D. E. , Dunbar‐Jacob, J. , Rice, V. H. , Millan, A. , Dunbar, S. B. , Braun, L. T. , Wilbur, J. E. , Chyun, D. A. , Gawlik, K. , & Lewis, L. M. (2018). A national study links nurses' physical and mental health to medical errors and perceived worksite wellness. Journal of Occupational and Environmental Medicine, 60(2), 126–131. 10.1097/JOM.0000000000001198 [DOI] [PubMed] [Google Scholar]
- Menon, B. , Karishma, H. P. , & Mamatha, I. V. (2015). Sleep quality and health complaints among nursing students. Annals of Indian Academy of Neurology, 18(3), 363. 10.4103/0972-2327.157252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mental Health Foundation . (2016). Fundamental facts about mental health 2016. Mental Health Foundation. [Google Scholar]
- Miceli, M. , & Castelfranchi, C. (2018). Reconsidering the differences between shame and guilt. Europe's Journal of Psychology, 14(3), 710–733. 10.5964/ejop.v14i3.1564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills, J. , Wand, T. , & Fraser, J. A. (2015). On self‐compassion and self‐care in nursing: Selfish or essential for compassionate care? International Journal of Nursing Studies, 52(4), 791–793. 10.1016/j.ijnurstu.2014.10.009 [DOI] [PubMed] [Google Scholar]
- Mirzaei, M. , Ardekani, S. M. Y. , Mirzaei, M. , & Dehghani, A. (2019). Prevalence of depression, anxiety and stress among adult population: Results of Yazd health study. Iranian Journal of Psychiatry, 14(2), 137–146. 10.18502/ijps.v14i2.993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff, K. (2003). The development and validation of a scale to measure self‐compassion. Self and Identity, 2(3), 223–250. 10.1080/15298860309027 [DOI] [Google Scholar]
- Neff, K. , & Germer, C. (2018). The mindful self‐compassion workbook: A proven way to accept yourself, build inner strength and thrive. Guilford. [Google Scholar]
- Nelson, J. R. , Hall, B. S. , Anderson, J. L. , Birtles, C. , & Hemming, L. (2018). Self–compassion as self‐care: A simple and effective tool for counselor educators and counseling students. Journal of Creativity in Mental Health, 13(1), 121–133. 10.1080/15401383.2017.1328292 [DOI] [Google Scholar]
- Nursing and Midwifery Council . (2018). Future nurse: Standards of proficiency for registered nurses. Retrieved from https://www.nmc.org.uk/globalassets/sitedocuments/education-standards/future-nurse-proficiencies.pdf [DOI] [PubMed] [Google Scholar]
- Office for Students . (2020). Male participation in nursing and allied health higher education courses. Office for Students. Retrieved from https://www.officeforstudents.org.uk/publications/male-participation-in-nursing-and-allied-health-higher-education-courses/ [Google Scholar]
- Pulido‐Martos, M. , Augusto‐Landa, J. M. , & Lopez‐Zafra, E. (2012). Sources of stress in nursing students: A systematic review of quantitative studies. International Nursing Review, 59(1), 15–25. 10.1111/j.1466-7657.2011.00939.x [DOI] [Google Scholar]
- Raes, F. , Pommier, E. , Neff, K. D. , & Van Gucht, D. (2011). Construction and factorial validation of a short form of the Self‐Compassion Scale. Clinical Psychology & Psychotherapy, 18, 250–255. 10.1002/cpp.702 [DOI] [PubMed] [Google Scholar]
- Rahimian, B. I. , & Ghodrati, M. M. (2013). Role of workload, sleep, mental health and individual factors in occurrence of nursing errors. Journal of Gorgan University of Medical Sciences, 15(3). [Google Scholar]
- Reeve, K. L. , Shumaker, C. J. , Yearwood, E. L. , Crowell, N. A. , & Riley, J. B. (2013). Perceived stress and social support in undergraduate nursing students' educational experiences. Nurse Education Today, 33(4), 419–424. 10.1016/j.nedt.2012.11.009 [DOI] [PubMed] [Google Scholar]
- Resurrección, D. M. , Salguero, J. M. , & Ruiz‐Aranda, D. (2014). Emotional intelligence and psychological maladjustment in adolescence: A systematic review. Journal of Adolescence, 37(4), 461–472. 10.1016/j.adolescence.2014.03.012 [DOI] [PubMed] [Google Scholar]
- Royal College of Nurses . (2019). The UK nursing labour market review 2018. Royal College of Nursing. 10.1016/S0304-4238(03)00043-8 [DOI] [PubMed] [Google Scholar]
- Scott, A. , Webb, T. , & Rowse, G. (2017). Does improving sleep lead to better mental health? A protocol for a meta‐analytic review of randomised controlled trials. British Medical Journal Open, 7(9), e016873. 10.1136/bmjopen-2017-016873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedighimornani, N. , Rimes, K. A. , & Verplanken, B. (2019). Exploring the relationships between mindfulness, self‐compassion and shame. SAGE Open, 9(3), 215824401986629. 10.1177/2158244019866294 [DOI] [Google Scholar]
- Şenyuva, E. , Kaya, H. , Işik, B. , & Bodur, G. (2014). Relationship between self‐compassion and emotional intelligence in nursing students. International Journal of Nursing Practice, 20(6), 588–596. 10.1111/ijn.12204 [DOI] [PubMed] [Google Scholar]
- Shankland, R. , Kotsou, I. , Vallet, F. , Bouteyre, E. , Dantzer, C. , & Leys, C. (2019). Burnout in university students: The mediating role of sense of coherence on the relationship between daily hassles and burnout. Higher Education, 78(1), 91–113. 10.1007/s10734-018-0332-4 [DOI] [Google Scholar]
- Shi, W. Y. , Guo, M. H. , Du, P. , Zhang, Y. , Wang, J. N. , Li, T. T. , Lyu, Y. B. , Zhou, J. H. , Duan, J. , Kang, Q. , & Shi, X. M. (2020). Association of sleep with anxiety in the elderly aged 60 years and older in China. Chinese Journal of Endemiology, 41(1), 13–19. 10.3760/cma.j.issn.0254-6450.2020.01.004 [DOI] [PubMed] [Google Scholar]
- Sivertsen, B. , Hysing, M. , Knapstad, M. , Harvey, A. G. , Reneflot, A. , Lønning, K. J. , & O'Connor, R. C. (2019). Suicide attempts and non‐suicidal self‐harm among university students: Prevalence study. Bjpsych Open, 5(2), e26. 10.1192/bjo.2019.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanojevic, C. , Simic, S. , & Milutinovic, D. (2016). Health effects of sleep deprivation on nurses working shifts. Medicinski Pregled, 69(5–6), 183–188. 10.2298/MPNS1606183S [DOI] [PubMed] [Google Scholar]
- Stein, M. B. , Belik, S. L. , Jacobi, F. , & Sareen, J. (2008). Impairment associated with sleep problems in the community: Relationship to physical and mental health comorbidity. Psychosomatic Medicine, 70(8), 913–919. 10.1097/PSY.0b013e3181871405 [DOI] [PubMed] [Google Scholar]
- Sun, N. , Wei, L. , Shi, S. , Jiao, D. , Song, R. , Ma, L. , Wang, H. , Wang, C. , Wang, Z. , You, Y. , Liu, S. , & Wang, H. (2020). A qualitative study on the psychological experience of caregivers of COVID‐19 patients. American Journal of Infection Control, 48(6), 592–598. 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, C. M. , McIntosh, C. E. , Lamar, R. A. , & Allen, R. L. (2017). Sleep deprivation in nursing students: The negative impact for quality and safety. Journal of Nursing Education and Practice, 7(5), 87. 10.5430/jnep.v7n5p87 [DOI] [Google Scholar]
- Ting, L. (2013). Depressive symptoms in a sample of social work students and reasons preventing students from using mental health services: An exploratory study. Journal of Social Work Education, 47(2), 253–268. 10.5175/JSWE.2011.200900092 [DOI] [Google Scholar]
- Trompetter, H. R. , de Kleine, E. , & Bohlmeijer, E. T. (2017). Why does positive mental health buffer against psychopathology? An exploratory study on self‐compassion as a resilience mechanism and adaptive emotion regulation strategy. Cognitive Therapy and Research, 41(3), 459–468. 10.1007/s10608-016-9774-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulmer, C. , Miller, D. , Wolman, M. , & Johns, E. (Eds.) (2008). Resident duty hours: Enhancing sleep, supervision and safety. The National Academies Press. [PubMed] [Google Scholar]
- Universities and Colleges Admissions Service . (2019). End of cycle report. UCAS. Retrieved from https://www.ucas.com/data-and-analysis/undergraduate-statistics-and-reports/ucas-undergraduate-sector-level-end-cycle-data-resources-2019 [Google Scholar]
- Van Sabben, E. (2020). 8 reasons why you should study nursing. Retrieved from https://www.whatuni.com/advice/choosing-a-course/8-reasons-why-you-should-study-nursing/73115/
- Watson, J. (2008). Nursing: The philosophy and science of caring. University Press of Colorado. [Google Scholar]
- Weimer, K. , Enck, P. , Dodd, S. , & Colloca, L. (2020). Placebo and nocebo effects in psychiatry and beyond. Frontiers Psychiatry, 11, 801. 10.3389/fpsyt.2020.00801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, C. , Yang, L. , Liu, S. , Ma, S. , Wang, Y. , Cai, Z. , Du, H. , Li, R. , Kang, L. , Su, M. , Zhang, J. , Liu, Z. , & Zhang, B. (2020). Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in Psychiatry, 11, 306. 10.3389/fpsyt.2020.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Peters, A. , & Chen, G. (2018). Perceived stress mediates the associations between sleep quality and symptoms of anxiety and depression among college nursing students. International Journal of Nursing Education Scholarship, 15(1). 10.1515/ijnes-2017-0020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.


