Summary
Multisectoral, One Health collaboration is essential for addressing national and international health threats that arise at the human–animal–environment interface. Thanks to the efforts of multiple organisations, countries now have an array of One Health tools available to assess capacities within and between sectors, plan and prioritise activities, and strengthen multisectoral, One Health coordination, communication, and collaboration. By doing so, they are able to address health threats at the human–animal–environment interface, including emerging zoonotic and infectious diseases, more efficiently. However, to ensure optimal outcomes for the countries using these One Health tools, the partners responsible for implementation should regularly collaborate and share information such as implementation timelines, results and lessons learned, so that one process can inform the next. This paper presents a consensus framework on how commonly implemented One Health tools might align to best support countries in strengthening One Health systems. Twelve One Health tools were selected based on their high implementation rates, authors’ experience with these tools and their focus on multisectoral, One Health coordination. Through a four-step process, the authors: a) jointly carried out a landscape analysis of One Health tools, using a Cloud-based spreadsheet to share the unique characteristics and applications of each tool; b) performed an implementation analysis to identify and share implementation dynamics and identify respective outcomes and synergies; c) jointly created a consensus conceptual model of how the authors suggest the tools might logically work together; and d) extrapolated from steps 1–3 an agreed-upon overarching conceptual framework for how current and future One Health tools could be categorised to best support One Health system strengthening at the national level. Highlighted One Health tools include the States Parties Annual Reporting Tool under the International Health Regulations (IHR), the World Organisation for Animal Health Performance of Veterinary Services (PVS) Pathway, the Joint External Evaluation process, IHR/PVS National Bridging Workshops, the Centers for Disease Control and Prevention One Health Zoonotic Disease Prioritization Tool, the Food and Agriculture Organization (FAO) Laboratory Mapping Tool, the FAO Assessment Tool for Laboratories and Antimicrobial Resistance Surveillance Systems, the FAO Surveillance Evaluation Tool, the One Health Systems Mapping and Analysis Resource Toolkit, the National Action Plan for Health Security, and IHR Monitoring and Evaluation Framework tools for After Action Reviews and Simulation Exercises. A new guidance document entitled, Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries was also included as a framework that provides guidance to support the implementation of the outputs of the tools described.
Keywords: Capacity assessment, Infectious disease, Multisectoral, One Health, One Health tools
Résumé
La collaboration multisectorielle suivant l’approche Une seule santé est essentielle pour répondre aux menaces sanitaires survenant à l’interface homme–animal–environnement à l’échelle nationale et internationale. Grâce aux efforts conjugués de nombreuses organisations, les pays disposent désormais d’une gamme d’outils Une seule santé permettant à la fois d’évaluer les capacités intra et intersectorielles, de planifier et prioriser les activités, et de renforcer la coordination, la communication et la collaboration multisectorielles suivant cette approche. Grâce à ces outils, les pays sont mieux armés pour faire face avec efficacité aux menaces sanitaires à l’interface homme–animal–environnement, en particulier celles liées aux maladies zoonotiques et infectieuses émergentes. Néanmoins, pour optimiser les retombées pour les pays du recours aux outils Une seule santé, les partenaires chargés de leur mise en œuvre devraient régulièrement collaborer et partager leurs informations, notamment le calendrier de mise en œuvre, les résultats obtenus et les enseignements tirés, afin que chaque processus contribue à l’amélioration des suivants. Les auteurs présentent un cadre consensuel sur la manière dont les outils Une seule santé les plus courants peuvent converger afin d’aider le mieux possible les pays à renforcer leurs systèmes basés sur cette approche. Douze outils ont été choisis en fonction de leur fréquence d’utilisation, de l’expérience acquise par les auteurs et de l’accent mis sur la coordination multisectorielle Une seule santé. Les auteurs ont ensuite procédé à un examen en quatre étapes, comme suit : a) analyse générale des outils sélectionnés, au moyen d’un tableur sur serveur dématérialisé permettant de saisir et de partager les caractéristiques et les applications spécifiques de chaque outil; b) analyse de la mise en œuvre des outils, visant à déterminer et à partager la dynamique et les caractéristiques de mise en œuvre, ainsi que les résultats respectifs et les synergies qui en ressortent; c) création d’un modèle conceptuel consensuel contenant les propositions des auteurs en vue d’une convergence raisonnée des fonctionnalités de ces outils; d) à partir des trois étapes précédentes, conception d’un cadre conceptuel transversal destiné à catégoriser les outils Une seule santé actuels et futurs afin d’apporter un soutien optimal au renforcement des systèmes Une seule santé à l’échelle des pays. Parmi les outils examinés figurent l’Outil d’autoévaluation pour l’établissement de rapports annuels par les États Parties de l’Organisation mondiale de la santé (OMS), qui concerne l’application du Règlement sanitaire international (RSI); le Processus sur les Performances des Services vétérinaires (PVS) de l’Organisation mondiale de la santé animale (OIE); le processus d’Évaluation extérieure conjointe; les ateliers nationaux de liaison RSI/PVS; l’outil Une seule santé de priorisation des maladies zoonotiques des Centres pour le contrôle et la prévention des maladies (CDC); l’Outil de cartographie des laboratoires de l’Organisation des Nations Unies pour l’alimentation et l’agriculture (FAO); l’Outil d’évaluation de la FAO pour les laboratoires et les systèmes de surveillance de l’antibiorésistance; l’Outil d’évaluation de la FAO sur la surveillance; la Boîte à outils cartographiques et analytiques sur les systèmes Une seule santé; les Plans d’action nationaux de sécurité sanitaire; et enfin les outils d’examen après action et protocoles de simulation du Cadre de suivi et d’évaluation du RSI. Le document d’orientation récemment publié sous le titre Taking a multisectoral One Health approach: a Tripartite guide to addressing zoonotic diseases in countries [Adopter une approche multisectorielle Une seule santé : Guide tripartite pour lutter contre les maladies zoonotiques] est également présenté, en tant qu’il fournit un cadre directeur en appui de la mise en œuvre des résultats des outils d’évaluation ci-dessus.
Mots-clés: Évaluation des capacités, Maladie infectieuse, Multisectoriel, Outils Une seule santé, Une seule santé
Resumen
La colaboración multisectorial en clave de Una sola salud es esencial para responder a las amenazas sanitarias de dimensión nacional e internacional que surgen en la confluencia de personas, animales y medio ambiente. Gracias al trabajo de numerosas organizaciones, los países disponen ahora de un repertorio de herramientas concebidas desde la óptica de Una sola salud para evaluar las capacidades existentes dentro de los sectores y entre ellos, planificar y jerarquizar actividades y potenciar las labores de coordinación, comunicación y colaboración multisectoriales en clave de Una sola salud. Gracias a todo ello, los países están en condiciones de luchar más eficazmente contra las amenazas sanitarias en la interfaz de personas, animales y medio ambiente, en particular las enfermedades infecciosas y zoonóticas emergentes. No obstante, para que los países obtengan resultados óptimos del uso de estas herramientas de Una sola salud es preciso que los distintos colaboradores encargados de aplicarlas colaboren e intercambien información periódicamente, por ejemplo sobre plazos de ejecución, resultados obtenidos y enseñanzas extraídas, de tal manera que un proceso pueda alimentar el siguiente. Los autores presentan un conjunto de principios consensuados sobre el modo en que cabría armonizar entre sí las herramientas de Una sola salud utilizadas con frecuencia para que los países cuenten con un apoyo idóneo a la hora de fortalecer los sistemas de Una sola salud. Ante todo, los autores seleccionaron doce de esas herramientas atendiendo a su (elevado) nivel de utilización, la experiencia de los propios autores con ellas y la medida en que privilegian la coordinación multisectorial en clave de Una sola salud. Después, siguiendo un proceso en cuatro etapas: a) efectuaron colectivamente un análisis general de las herramientas existentes, empleando una hoja de cálculo situada en la «nube» para poner en común las características y aplicaciones únicas de cada herramienta; b) analizaron la utilización práctica de esas herramientas de Una sola salud para dilucidar y poner en común la dinámica de aplicación de cada una y determinar sus respectivos resultados y sinergias; c) elaboraron de forma concertada un modelo teórico del modo en que, a su juicio, sería lógico que las herramientas funcionaran conjuntamente; y d) a partir de los pasos 1 a 3, extrapolaron consensuadamente un marco teórico global con el que se podrían clasificar las herramientas de Una sola salud, actuales y futuras, para prestar un apoyo idóneo al fortalecimiento del sistema de Una sola salud en cada país. Las herramientas de Una sola salud seleccionadas son: el instrumento de evaluación para la presentación anual de informes de los Estados Partes que forma parte del Reglamento Sanitario Internacional (RSI); el proceso PVS (Prestaciones de los Servicios Veterinarios) de la Organización Mundial de Sanidad Animal (OIE); la herramienta de evaluación externa conjunta del RSI; los talleres nacionales de coordinación RSI-PVS; la herramienta de jerarquización de enfermedades zoonóticas en clave de Una sola salud de los Centros para el Control y la Prevención de Enfermedades (CDC); la herramienta de inventario de laboratorios de la Organización de las Naciones Unidas para la Alimentación y la Agricultura (FAO); la herramienta de evaluación de laboratorios y sistemas de vigilancia de las resistencias a los antimicrobianos de la FAO; la herramienta de evaluación de la vigilancia de la FAO; el juego de herramientas y material de análisis y cartografía de los sistemas de Una sola salud; los planes de acción nacional de seguridad sanitaria de la OMS; las herramientas del marco de seguimiento y evaluación del RSI para la realización de exámenes posteriores a la acción y ejercicios de simulación. También se incluyó una nueva guía de la Tripartita para combatir las enfermedades zoonóticas en los países desde la lógica multisectorial de Una sola salud (Taking a multisectoral One Health approach: a Tripartite guide to addressing zoonotic diseases in countries), en el cual se ofrecen pautas para secundar la aplicación en la práctica de los resultados obtenidos con las citadas herramientas.
Palabras clave: Enfermedad infecciosa, Evaluación de capacidades, Herramientas de Una sola salud, Multisectorial, Una sola salud
Introduction
Countries around the world are increasingly committed to taking a multisectoral, One Health approach to address complex health threats at the human–animal–environment interface, such as zoonotic and emerging infectious diseases and antimicrobial resistance (AMR). Recognition of challenges or gaps in national mechanisms for taking a One Health approach – whether based on national experience with the negative impacts of outbreaks or the results of internal or external reviews and assessments – has prompted countries to explore options for improvement. In addition, countries recognise that taking such an approach is critical to meeting their obligations under multiple global frameworks, including the requirements of the International Health Regulations (IHR, 2005) and the standards of the World Organisation for Animal Health (OIE). The One Health approach is also vital for making progress towards achieving the United Nations Sustainable Development Goals (1, 2, 3, 4).
In the experience of the authors, practical implementation of a One Health approach can be challenging, especially in low-resource settings or where sector-specific structures are well established. Many international agencies, bilateral technical partners, development partners and donors have provided technical and financial support to countries, using available One Health tools to promote the operationalisation of a multisectoral, One Health approach. The intent of this capacity-building work is to assist and maximise the results of national efforts in addressing complex health threats at the human–animal–environment interface by engaging and mobilising resources more effectively across One Health sectors. Decision-makers in many countries are now being offered a wide variety of initiatives, tools and projects that are intended to build sector-specific, disease-specific and/or multisectoral, One Health capacity (5). This paper examines a number of these One Health tools and processes, all of which have the potential to advance the implementation of One Health approaches at the national level.
The Tripartite (OIE, the Food and Agriculture Organization of the United Nations [FAO] and the World Health Organization [WHO]), in collaboration with international experts and country representatives, have developed an operational guide entitled, Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries also referred to as the Tripartite Zoonoses Guide or TZG (6). This guide builds on a 2008 WHO guide, Zoonotic Diseases: A Guide to Establishing Collaboration between Animal and Human Health Sectors at the Country Level (7) and on a rich array of global One Health initiatives and experiences from different countries (5, 8, 9, 10). The TZG is designed to support countries in providing guidance to build multisectoral, One Health capacity to address zoonoses and other health threats at the human–animal–environment interface. This includes building capacity in aligned surveillance, joint outbreak response, preparedness, One Health workforce development, and development of multisectoral coordination mechanisms. As the TZG is launched, it will be important that countries understand how best to use the guidance to operationalise plans and use the outputs from the many One Health tools and processes already being implemented at the national level, as described in this article.
Tool origins and selection process
In 2010, an international meeting, ‘Operationalizing One Health: A Policy Perspective’, was held in Stone Mountain, Georgia, the United States of America (USA) (11). Attendees identified specific projects to advance the implementation of the One Health approach around the world, creating working groups on One Health capacity building, needs assessment and training, among other issues. Discussions during and following the meeting highlighted the importance and value of convening experts working in the One Health realm (intergovernmental organisations, government agencies, academia and other partners) to share information, details of progress and ideas. These discussions also created a shared commitment to harmonise efforts and build tools designed to address specific aspects of strengthening and assessing multisectoral, One Health coordination/implementation mechanisms within a country.
Over the last eight years, the authors have worked both independently and collaboratively to develop a series of tools to further One Health at the operational level. Each tool and associated process was developed to address specific aspects of assessing and/or strengthening One Health capacity. Each was also independently implemented and piloted by the various authors and their organisations in the field. A number of publications describe these efforts (4, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22).
As work on these various tools progressed, the authors began sharing results with partners, inviting observation and participation in implementation and training workshops, and exploring potential opportunities for collaboration and for synergising outputs. The collaborative engagement in developing the TZG during 2017–2018 provided further opportunity for the authors to identify specific tools that encourage and support the implementation of a multisectoral, One Health approach at the national level, as described in the guide. This prompted tool developers to discuss methods for highlighting the complementarity of these One Health tools and how they could assist countries in implementing the guidance in the TZG. As a first step, they collaborated to host a symposium at the annual meeting of the American Society for Tropical Medicine and Hygiene in 2017 (23). The pre- and post-symposium activities led to the creation of a multi-step process to review tools together, share the outcomes of tool implementation, with country permission, and establish synergies.
Additionally, as part of the TZG development effort, the Tripartite, with input from other organisations, including the Centers for Disease Control and Prevention (CDC), developed a review document that summarises and links existing One Health-related processes and activities (e.g. regulations, standards, guidance, manuals, tools, assessments, evaluations and conventions) (internal document available upon request). This review encompasses approximately 50 tools, processes and activities that the Tripartite authors broadly considered One Health-related. This comprehensive list served as a resource to the authors in determining tools for inclusion in this paper and building a conceptual model of how these tools could work together more effectively.
While much progress has been made in developing and implementing various One Health tools and processes, to date there has been limited effort in sharing lessons learned and best practices on how to synergise or link these for maximal benefit at the national level (5). The tools and processes presented in this paper are voluntary, but multiple countries have chosen to use them to advance their own goals related to global health security, trade of animals and products of animal origin, and to prevent, detect, respond to, and control zoonotic diseases. Although not exhaustive, the information presented in this paper should help countries to gain a clearer understanding of the One Health tools that are available, how and when tools and processes can be applied for maximal benefit, and how these tools can be used to support national and international standards and goals for One Health, including goals concerning preparedness, planning, response, operations, workforce development and other capacity-building activities.
While previous efforts have brought partners together to promote collaboration and describe specific One Health tools (5, 23), this paper seeks to provide information on how selected tools might be used together for greatest effect and better outcomes. This paper also presents a more in-depth review of the unique characteristics and applications of operational tools that have been used to assist countries and regions. It focuses specifically on tools that authors have personal experience with, have high ‘implementation rates’, i.e. have been used in multiple countries and regions (12, 24), and emphasise multisectoral, One Health coordination and collaboration. The descriptions in this paper are not meant to present the only potential context and application for each tool, as each tool has its own context, requirements and applications that are independent of how they might be used in synergy to advance One Health.
The overall goals for this work were to review synergies and possible overlaps, clarify expected country outputs, and elucidate options for how countries can use these tools to maximal benefit in the context of both their individual use as well as their use together or in sequence. Specific objectives of this project were to:
jointly conduct a landscape analysis of One Health tools, using a Cloud-based spreadsheet application (Google sheets) to share unique characteristics and applications of each tool online
perform an implementation analysis to identify and share implementation dynamics and identify respective outcomes and synergies
jointly create a consensus conceptual model of how the authors feel the tools might logically work together
extrapolate from steps 1–3 an agreed-upon overarching conceptual framework for how current and future One Health tools could be categorised to best support countries to strengthen their One Health systems.
Methods
Criteria for tool inclusion
This paper does not provide an exhaustive list of all the One Health tools available, but it provides examples of some of the tools that national decision-makers could find useful when developing their strategy for implementing One Health approaches in their countries. A more comprehensive list of tools is available in other publications (5). Each of the tools included in this analysis met all of the following criteria:
The tool helps support a multisectoral, One Health approach to preventing, detecting, responding to and controlling zoonotic diseases or other health threats at the human–animal–environment interface.
The tool has been implemented at the national level in at least five countries.
One or more authors was involved in developing the tool and has/have supported implementation of the tool at the national level.
The one exception was the TZG. This is a new tool that was in development during the preparation of this analysis and has not yet been implemented in any country. The authors included this tool because they predict that the TZG will be used by countries to address gaps in One Health capacity and operationalise the plans developed through the application of the One Health tools described in this paper.
Landscape analysis
The authors identified 12 tools that met the above inclusion criteria and jointly conducted a landscape analysis in order to collectively establish a cohesive understanding of these tools and analyse key aspects of their role, scope and application. This analysis allowed authors to directly compare the key characteristics of the tools and identify the main differences between them. Authors worked collaboratively on the group document to establish the variables and other information to be collected. A consensus-driven iterative review process was used to select the following descriptive variables:
tool name
organisation of origin
scope or category
description
reason for development
implementation process
example applications
key outputs
an Internet link, if available.
The authors then filled in the required information for their tool(s) individually into the Cloud-based spreadsheet.
Country implementation analysis
The authors worked with agency and institutional teams involved in implementation to document where, when and how the included One Health tools had been used since development. The authors compared the implementation date of each tool with that of every other tool so as to determine the order in which they were used. This analysis of temporal directionality was visualised in a matrix showing the percentage number of times one tool followed another to demonstrate any commonly seen implementation patterns. For each tool comparison, if one tool preceded the other more than 50% of the time, it was marked in grey, indicating a stronger tendency to be implemented before the other tools.
In addition, authors worked with their respective implementation teams to answer a set of questions regarding sharing and use of tool outcomes for implementation in countries where at least four tools were implemented. The authors chose countries with a high rate of tool use, as there are more opportunities to evaluate the number of data-sharing events between the tools. Questions included:
Did you share your tool outcomes with other tool-implementing partners in this table prior to their implementation?
Did you receive other tool outcomes listed in this table prior to your implementation?
If you received other tool outcomes prior to implementation, did those outcomes inform your tool implementation?
Authors were asked to respond in one of four ways: ‘yes’, ‘no’, ‘don’t know’ or ‘not applicable’, and all data were collected into the cloud-based spreadsheet. Tool outcomes could be received in a multitude of ways: published online, direct from the authors involved in implementation, or shared by a country partner.
Linking the tools: developing the conceptual model and the overarching conceptual framework
Once the tools were identified and the implementation spreadsheet developed, the authors began sharing a series of diagrams to understand how tools might logically be applied to strengthen One Health approaches at the national level. Authors shared information on what did and did not work when tools were implemented in countries by highlighting themes from repeated or piloted implementation, particularly in cases where tools were used in a series or together, and lessons learned from those experiences. After iterative review and revision of proposed tool sequencing and relationships, a conceptual model diagram was developed representing a consensus of how the authors believe the tools might maximally inform each other. The conceptual model was designed to describe when tools might be used, what the expected outputs were, and how those outputs might be used in a synergistic manner.
As the authors worked through the landscape analysis and conceptual model, the tools were categorised into groups. The authors worked iteratively on an overarching conceptual framework, starting with identifying the tool categories. A graphical representation was generated and agreed to by author consensus to represent overarching categories that multiple tools might fit into and countries might use.
Results
Landscape analysis
The iterative landscape analysis identified 12 tools that met all criteria, as follows:
IHR After Action Review (AAR)
FAO Assessment Tool for Laboratories and Antimicrobial Resistance Surveillance Systems (FAO–ATLASS)
FAO Laboratory Mapping Tool (FAO–LMT)
FAO Surveillance Evaluation Tool (FAO–SET)
IHR Joint External Evaluation (JEE) Tool
WHO National Action Plan for Health Security (NAPHS)
OIE Performance of Veterinary Services (PVS) Pathway
IHR/PVS National Bridging Workshop (NBW)
One Health Zoonotic Disease Prioritization Tool (OHZDP), developed by the CDC
One Health Systems Mapping and Analysis Resource Toolkit (OH–SMART™), developed by the University of Minnesota and the US Department of Agriculture
WHO Simulation Exercises (SimEx)
WHO States Parties Annual Reporting (SPAR) Tool. (Annual reporting is mandatory, but use of the SPAR Tool is not; countries can choose to submit their reports in another format if they prefer.)
In addition, the TZG was included as guidance to support the implementation of the outputs from the highlighted One Health tools.
Full descriptions of these tools are provided in the complete landscape analysis in Table I. Of these tools, a number fit in multiple categories. Eight were categorised as assessment tools, three as prioritisation tools, two as action planning tools, one as an implementation tool and four as monitoring tools (Table I).
Table I.
Landscape analysis and comparison of the 12 One Health tools that met the inclusion criteria
| Tool | Organisation(s) | Scope/Category | Tool description | Reason for development | How applied/Process | Example applications | Key outputs | Website, if available |
|---|---|---|---|---|---|---|---|---|
| FAO Assessment Tool for Laboratories and Antimicrobial Resistance Surveillance Systems (FAO–ATLASS) | FAO | Assessment and prioritisation | FAO–ATLASS maps the national antimicrobial resistance (AMR) surveillance systems along five pillars (laboratory capacity and network, epidemiology unit, governance, communication and sustainability). The tool consists of two modules – laboratory and surveillance – which include features of FAO–LMT and FAO–SET, focusing on AMR. FAO–ATLASS provides recommendations for improvement of the systems, measures progress relative to the FAO Global AMR Action Plan, and provides evidence for action and advocacy | To assist countries in evaluating their AMR surveillance systems and building their capacity | Five-day assessment carried out by fully trained FAO–ATLASS assessors. The first assessment is always carried out by external assessors, while follow-up assessments may be carried out by national assessors, or by an FAO–ATLASS Focal Point. Evaluations include: 1) a preparatory phase where all relevant documents are gathered; 2) meetings with all national authorities and stakeholders for the assessment of the whole AMR surveillance system; and 3) the evaluation of each laboratory that is already included or is to be included in the national AMR surveillance system |
To date, 19 countries have conducted FAO–ATLASS assessment missions (Africa: 8; Asia: 8; Europe: 3). Seventeen missions involved the full assessment with laboratory and surveillance modules, two were laboratory module only. FAO–ATLASS results can support JEE missions, and since the tool includes components that link to other sectors, such as public health and environment, they may also help to address AMR under the One Health approach | Outputs of FAO–ATLASS evaluations include: 1) A final report summarising the outcome of the assessment including a description of findings and recommendations for the gradual improvement of the AMR surveillance system 2) For each laboratory: FAO–LMT AMR and progressive improvement pathway (PIP) scoring are generated 3) For the National AMR surveillance system: the PIP scoring identifies and prioritises the areas of intervention for five pillars of an AMR surveillance system (laboratory capacity and network, epidemiology unit, governance, communication and sustainability) |
www.fao.org/antimicrobial-resistance/resources/tools/atlass/en/ |
| FAO Laboratory Mapping Tool (FAO–LMT) | FAO | Assessment and monitoring | Standardised, semi-quantitative toolkit used to determine gaps in laboratory functionality and define mechanisms and targets for capacity building. The core assessment tool (FAO–LMT–Core) assesses the veterinary laboratories’ general functionality through 108 questions. The FAO–LMT family was further expanded in 2016 with the release of a separate module for assessing laboratory safety (FAO–LMT–Safety). This module uses 98 questions to provide a standardised assessment of the environmental safety of veterinary laboratories and occupational risks | To allow veterinary laboratories to visualise their performance as compared to national, regional and global networks and thereby further encourage them to improve their capacity | The tool automatically generates graphical outputs and a profile which can be followed over time to evaluate the evolution of laboratory capacities, guide capacity building and develop strategic plans that correspond to individual laboratory needs, addressing all key elements required for an operational laboratory | The FAO–LMT–Core has been used in 117 individual facilities in 42 countries in Africa and Asia since 2010 and yearly follow-up assessments have monitored progress. Outputs from the FAO–LMT evaluations can be used as a resource during JEE missions. The tool can also be used to characterise laboratory functionality together with results from assessments such as a PVS Laboratory Mission or FAO–SET | The tool automatically generates graphical outputs and a profile which can be followed over time to evaluate the evolution of laboratory capacities, guide capacity building and develop strategic plans that will correspond to individual laboratory needs, addressing all key elements required for an operational laboratory | www.fao.org/ag/againfo/programmes/en/empres/news_130514.html |
| FAO Surveillance Evaluation Tool (FAO–SET) | FAO | Assessment and monitoring | Comprehensive and standardised evaluation of national animal/zoonotic disease surveillance systems along 90 indicators organised in 19 categories, including aspects of intersectoral cooperation between Veterinary Services, Public Health Services and Wildlife Services. FAO–SET provides Veterinary Services with a 360° assessment of their surveillance network, which is used to develop a locally relevant action plan for capacity building of national animal disease surveillance | To respond to countries’ requests for an evaluation and work planning tool to specifically enhance capacities of national animal disease surveillance systems | Teams of five to ten people (FAO staff and National Focal Points from the Veterinary Services) conduct an initial evaluation to provide baseline information on the animal disease surveillance system. Missions may last between 10 and 12 days, during which time stakeholders are interviewed at all levels of the system (central, intermediate, field). Information collected is entered into FAO–SET and outputs are automatically generated, allowing the evaluation team to develop an action plan for improvement with specific, measurable, attainable, relevant and prioritised recommendations Subsequent evaluations may take place every three to five years thereafter | To date, 13 countries in West, Central and East Africa have used the tool, leading to the development of locally relevant action plans to improve their animal disease surveillance systems. Decision-makers can use FAO–SET to: 1) directly evaluate their national animal disease surveillance capacity; 2) carry out a targeted evaluation following more general evaluations such as the JEE or PVS, if this aspect is identified as weakness; or 3) monitor progress during follow-up evaluations | Visual outputs generated by the tool include: 1) scores for each of the surveillance capacities evaluated (core capacities); 2) spider graphs indicating the progress of the surveillance system relative to ten different performance attributes, e.g. sensitivity, flexibility; and 3) scores for the JEE indicators related to animal disease surveillance, which may differ from the scores obtained during the JEE itself. A final evaluation report is generated with evaluation results and a locally relevant action plan for improvement of the national animal disease surveillance system | www.fao.org/ag/againfo/programmes/en/empres/tools_SET.html |
| IHR/PVS National Bridging Workshops (NBWs) | WHO and OIE | Assessment | Reviews current collaboration gaps across human and animal health in 15 key technical areas and supports development of a joint roadmap of corrective measures and strategic investments | To improve the prevention, detection and control of health threats at the animal–human interface | In countries that have performed a PVS and (ideally) a JEE. Implemented as a workshop in seven steps over three days: 1) setting the scene; 2) case studies and diagnosis of the levels of collaboration for 15 key technical areas; 3) IHR and PVS tools and mapping of the identified gaps on the IHR–PVS matrix; 4) extraction and compilation of results from previous assessments; 5) development of a joint roadmap (objectives and activities); 6) fine-tuning of the roadmap; 7) way forward and linkages with other mandated plans |
15 countries have implemented an NBW. Results of the IHR/pVs NBWs can feed into the development of the National Action Plan for Health Security (NAPHS) or other national One Health plans | 1) A diagnosis of the strengths and weaknesses of the current collaboration between animal health and human health services (based on five priority zoonotic diseases) 2) A better understanding of the regulatory frameworks and capacity assessment tools from both sectors and how their results can be complementary and synergetic 3) A roadmap of joint activities that both sectors commit to implementing in order to improve their collaboration at the animal–human–environment interface |
https://extranet.who.int/sph/ihr-pvs-bridging-workshop |
| International Health Regulations (IHR) Monitoring and Evaluation Framework: After Action Review (AAR) and Simulation Exercises (SimEx) | WHO | Monitoring | Two of the four components of the IHR Monitoring and Evaluation Framework. These processes allow a qualitative review of national operational capacity for responding to events, either proactively (SimEx) or retrospectively (AAR) SimExes can be used to test specific aspects of a system (e.g. collaboration among partners) under a hypothetical scenario, whereas AARs review the actual functioning of the system during a real event involving hazards as described in the IHR (2005), as well as for other natural and human-made disasters | To allow countries to identify best practices and gaps in operational functioning of the national preparedness and response to emergency events | Duration, scope, focus, structure, and partners vary according to the event or scenario. These voluntary processes are carried out by countries with support from WHO as needed | Out of the 35 AARs conducted since 2016, 17 were associated with zoonotic or food safety events. Out of the 73 WHO simulation exercises conducted since 2016, 41 had a multisectoral, One Health component related to a zoonotic disease | Identification and documentation of the strengths and gaps in the functional, operational aspects of implementation of IHR capacities in the specific scope reviewed or tested through exercises |
www.who.int/ihr/publications/WH0-WHE-CPI-2017.10/en/ https://extranet.who.int/sph/simulation-exercise https://extranet.who.int/sph/after-action-review https://extranet.who.int/sph/ihrmef www.who.int/ihr/procedures/monitoring/en/ |
| Joint External Evaluation (JEE) | WHO | Assessment and monitoring | Evaluation of national capacity – particularly infrastructural capacity – in 19 technical areas that cover the scope of IHR core capacities. Includes evaluation of capacity for collaboration across sectors for public health outcomes. One of the four components of the IHR Monitoring and Evaluation Framework | To provide expert assessment of country capacities under IHR and to identify strengths and areas for strengthening and priority actions to be taken in each of the 19 technical areas being evaluated. Allows continual strengthening of capacities for the implementation of the IHR and, through iterative evaluations, monitoring of progress | Voluntarily undertaken every four to five years by a country, in two stages, using the JEE tool. 1) An initial self-evaluation conducted by the country; and 2) an in-country evaluation conducted jointly by a multisectoral external team and a team of national experts from all relevant sectors. Normally initiated by Ministry of Health; WHO supports logistics and implementation; OIE and FAO are generally invited as external experts | As of 6 November 2018, 86 countries have completed a JEE | Final report prepared by the external team in collaboration with the multisectoral national team and validated by the national government. The report includes, for each of the 19 technical areas, a review of capacity in that technical area, including strengths and areas for strengthening, priority actions, and scores for each of the indicators. The report is posted on the WHO website once cleared by the national government |
https://extranet.who.int/sph/sites/default/files/document-library/document/9789241550222-eng.pdf https://extranet.who.int/sph/ihrmef |
| National Action Plan for Health Security (NAPHS) | WHO | Action planning | Country Planning for Health Security is an activity of Member States that enables them to develop their NAPHS, with the support of WHO. The activity includes coordinating and collaborating on different areas of health security, defining national stakeholders’ roles and responsibilities, and consolidating the information into a single comprehensive national action plan. The principles of Country Planning for Health Security are country ownership, active partnerships, and WHO leadership | To plan and monitor the strengthening of activities required for compliance with the IHR | WHO supports countries in the process of collecting information, planning and conducting the workshop, and developing the plans | As of 6 November 2018, 38 countries have developed an NAPHS | A costed plan to improve the national health system and national and global health security | https://extranet.who.int/sph/country-planning |
| One Health Systems Mapping and Analysis Resource Toolkit (OH–SMART) | University of Minnesota | Assessment, action planning and prioritisation | The OH–SMART process includes six steps and is designed to map and analyse complex One Health challenges such as zoonotic disease outbreaks or antimicrobial resistance. The six OH–SMART steps are: 1) Identify stakeholder network 2) Interview stakeholders 3) Map the system 4) Analyse the system 5) Identify improvement opportunities 6) Develop an action plan |
The tool is targeted to government Ministries, coordination mechanisms/platforms and organisations looking to: 1) improve One Health collaboration in practice by moving from relationship-based systems to institutionalised approaches that maximise resources and effort and provide mutual benefit 2) identify practical and targeted interventions at specific points across the system 3) provide One Health leaders with a suite of tools for stakeholder engagement, advocacy and ongoing collaboration |
OH–SMART is best applied to complex challenges that require a multisectoral and multidisciplinary approach to improve system efficiency and effectiveness. Examples: 1) Pro-actively, to develop surveillance plans, investigation and response plans, workforce development plans and other action plans or simply to improve understanding of the current system around a One Health challenge 2) Retroactively, to analyse an actual system response to a One Health challenge and develop a plan for improving future responses 3) Just in time, during an outbreak or other crisis, to analyse and improve response systems as they are being implemented |
A total of 17 countries have used OH–SMART to strengthen One Health systems for prevention, detection and response to infectious disease threats. 1) National AMR Action Planning in South-East Asia; 2) Development of National Zoonotic Disease Workforce Plans in Africa; 3) Action planning for multisectoral coordination mechanisms in Africa and Asia; 4) After Action Review of zoonotic disease outbreaks in the USA; 5) development of action plans for prioritised zoonotic diseases in South-East Asia, the USA and Europe; 6) strengthening zoonotic disease surveillance and communication plans in South-East Asia | 1) Mapping and analysis of multisectoral agency systems 2) Improvement in agency coordination and collaboration around a specific crisis, outbreak or other complex challenge 3) Multisectoral systems improvement through pro-active planning, retroactive analysis of events and/or just-in-time response using actionable implementation plans developed during the OH-SMART Workshop 4) Development of a consensus action plan to advance systems strengthening across sectors |
www.vetmed.umn.edu/centers-programs/global-one-health-initiative/one-health-systems-mapping-and-analysis-resource-toolkit |
| One Health Zoonotic Disease Prioritization (OHZDP) Process | Centers for Disease Control and Prevention | Prioritisation | The OHZDP process uses a multisectoral, One Health approach to prioritise endemic and emerging zoonotic diseases of major public health concern that should be jointly addressed by national human, animal, and environmental health sectors and other relevant partners The OHZDP tool is flexible in scale and can be applied at the regional, national or sub-national level. The process uses a standardised, mixed-methods approach and is implemented by trained facilitators |
The OHZDP process was developed to focus the use of limited resources to build capacity and reduce the impact of prioritised zoonoses using a One Health approach. The OHZDP process is a transparent process that involves all of the relevant One Health sectors and partners working together and providing equal input, which helps to enhance and strengthen One Health networks | The OHZDP process is conducted upon the request of a country, region, or other jurisdiction and consists of an in-person workshop that gathers relevant One Health Ministries and partners to prioritise zoonotic diseases of greatest national concern for One Health collaboration. The OHZDP workshop consists of five steps. Step 1 (Preparation and Logistics) is completed prior to the workshop. Steps 2–5 (Criteria Development, Question Development, Ranking and Scoring the Zoonoses, and Next Steps and Action Planning) occur throughout the multi-day workshop | The OHZDP Process has been used at regional, national, sub-national, and local levels. The process has been used in over 20 locations around the world in various regions and languages | Prioritised list of zoonotic diseases that are agreed upon by all stakeholders by the end of the workshop Discussions about next steps and action plans for prioritised zoonoses and One Health implementation Workshop summary, available shortly after the workshop so governments can begin to work collaboratively to address the newly prioritised zoonoses Final workshop report that is reviewed and approved by all relevant One Health sectors that can be shared with potential funding partners and collaborators |
www.cdc.gov/onehealth/global-activities/prioritization.html www.ghsagenda.org/packages/p2-zoonotic-disease |
| OIE Performance of Veterinary Services (PVS) Pathway (PVS Evaluation, Evaluation Follow-Up, Gap Analysis, Legislation mission, Laboratory mission, veterinary education support, public–private partnerships, etc.) | OIE | Assessment | Voluntary, multi-staged, continuous process which uses a set of complementary tools designed to assist Veterinary Services in improving their capacity to undertake their animal health, veterinary public health and other regulatory functions in closer compliance with the international standards of the OIE Codes.(a) The OIE PVS Pathway has a strong systems approach and supports the strengthening of the cross-sectoral capacities that are needed for the control of zoonoses, food safety and AMR | To promote the strengthening of Veterinary Services and improve their compliance with the international standards in the OIE Codes(a) | OIE PVS Evaluation: Conducted upon country request by certified OIE PVS Pathway experts; evaluation focuses on four Fundamental Components: 1) Human, physical and financial resources 2) Technical authority and capability 3) Interaction with interested parties 4) Access to markets |
As of 1 October 2018, 135 PVS Evaluations, 96 PVS Gap Analysis missions, 51 PVS Evaluation Follow-Up missions, 62 PVS Veterinary Legislation missions, and 14 PVS Laboratory missions have been implemented. The PVS Evaluation is one of the two background documents used in the IHR/ PVS National Bridging Workshops. The OIE PVS Gap Analysis report and costing of the key veterinary public health activities can feed the development and costing of the WHO National Action Plan for Health Security | OIE PVS Evaluation: comprehensive assessment of the country’s animal health system, providing a complete overview of the Veterinary Services’ organisational structure, animal health, food safety and regulatory activities, their weaknesses and strengths | www.oie.int/en/solidarity/pvs-pathway/ |
| States Parties Annual Reporting under the International Health Regulations (2005; SPAR) | WHO | Assessment | Self-assessment of national core public health capacities, particularly infrastructural capacity, as required under the IHR (2005), to prevent, detect, and rapidly respond to public health threats, whether occurring naturally or due to deliberate or accidental events. Includes evaluation of capacity for collaboration across sectors for public health outcomes. Is one of four components of the IHR Monitoring and Evaluation Framework | To provide information on capacity and progress towards achieving IHR core capacities both to WHO and to the country itself | Obligatory annual self-assessment, information reported to the World Health Assembly, provided to the secretariat of IHR in WHO by the IHR National Focal Point. SPAR is the format proposed by WHO but countries are free to use another format for their reporting | State Party annual reporting to the IHR Secretariat in WHO is mandatory | Annually updated information on national capacities under IHR |
https://extranet.who.int/sph/ihrmef www.who.int/ihr/procedures/monitoring/en/ |
| Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries (Tripartite Zoonoses Guide/TZG) | WHO, OIE and FAO | Implementation | The TZG provides standard, practical guidance for countries in taking a multisectoral, One Health approach to zoonotic diseases and other health threats at the human–animal–environment interface. It covers the following topics: multisectoral coordination; understanding national context and priorities; strategic planning and emergency preparedness; surveillance for zoonotic diseases and information sharing; coordinated investigation and response; joint risk assessment for zoonotic disease threats; risk reduction, risk communication, and community engagement; and workforce development | To provide practical, standard guidance from the Tripartite so that countries can involve all relevant sectors to more effectively address issues at the human–animal–environment interface using a multisectoral, One Health approach | A tool that countries can use as appropriate to fill multisectoral gaps identified through various assessments or experiences, and to operationalise national plans. Operational tools (e.g. terms of reference, templates, standard processes) are being developed for each of the included topics | None to date (released 11 March 2019) | Operationalisation of One Health approaches |
www.oie.int/tripartitezoonosesguide
https://extranet.who.int/sph/sites/default/files/document-library/document/Tripartite-Guidance-EN-web%20single%20page.pdf www.fao.org/3/ca2942en/ca2942en.pdf |
FAO: Food and Agriculture Organization of the United Nations
WHO: World Health Organisation
The OIE Terrestrial Animal Health Code and Aquatic Animal Health Code
Country implementation analysis
Implementation data were collected for nine of the 12 tools that met the inclusion criteria, namely: OIE PVS Pathway, JEE, NBW, OHZDP, FAO–LMT, FAO–ATLASS, FAO–SET, OH–SMART and NAPHS. The AAR, SimEx, and SPAR were not assessed in this analysis as implementation data were not readily available for review. The nine tools assessed were implemented in a median of 20 (range 13–134) countries representing four WHO regions (Africa, the Eastern Mediterranean, South-East Asia and the Western Pacific region). There were 30 countries which had implemented ≥4 of the tools assessed (Table II). There were only three countries (Ethiopia, Senegal and Tanzania) where all nine tools had been implemented.
Table II.
Overview of country implementation and other tool outcome use, categorised by tool, for nine multisectoral, One Health tools
| Tool | Year developed | Total no. of countries where tool implemented | No. of countries where tool was implemented with >3 other One Health tools/plans | Percentage of times the below tools were used as input for tools listed in the first column (no. of opportunities to use tools)(a) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OIE PVS Pathway | JEE NBW | FAO–SET | FAO–LMT(b) | FAO–ATLASS(b) | OH–SMART | NAPHS | ||||
| OIE PVS Pathway | 2006 | 134 | 30 (22.40%) | 50% (2) | 100% (1) | |||||
| JEE | 2016 | 84 | 30 (35.70%) | 83% (30) | 88% (8) | |||||
| NBW | 2013 | 14 | 11 (78.60%) | 100% (11) | 100% (10) | 100% (5) | 100% (6) | |||
| FAO–SET | 2017 | 13 | 13 (100.00%) | 100% (8) | 100% (11) | 100% (11) | 100% (8) | |||
| FAO–LMT(b) | 2010 | 38 | 26 (68.40%) | |||||||
| FAO–ATLASS(b) | 2017 | 19 | 13 (68.42%) | |||||||
| OHZDP | 2014 | 20 | 17 (85.00%) | 0% (15) | 100% (9) 100% (1) | 100% (1) | ||||
| OH–SMART | 2015 | 17 | 15 (88.20%) | 100% (8) | 100% (14) 50% (2) | 100% (10) | 100% (4) | |||
| NAPHS | 2016 | 36 | 21 (58.30%) | 100% (11) | ||||||
FAO: Food and Agriculture Organization of the United Nations
FAO–ATLASS: FAO Assessment Tool for Laboratories and Antimicrobial Resistance Surveillance Systems
FAO–LMT: FAO Laboratory Mapping Tool
FAO–SET: FAO Surveillance Evaluation Tool
IHR: International Health Regulations
JEE: Joint External Evaluation
NAPHS: National Action Plan for Health Security
NBW: IHR/PVS National Bridging Workshop
OH–SMART: One Health Systems Mapping and Analysis Resource Toolkit
OHZDP: One Health Zoonotic Disease Prioritization Tool
OIE PVS Pathway: World Organisation for Animal Health Performance of Veterinary Services Pathway
Only countries where four or more tools had been implemented were included in this analysis. Users wishing to obtain information about how these tools had been used previously could access it from publicly available reports or by obtaining reports from earlier users. For example, the JEE tool used results from the OIE PVS Pathway in 25 countries. All questionnaire responses and analysis reflect data available as of 2 November 2018
Questionnaires not completed for the FAO–LMT and FAO–ATLASS tools; blank cells indicate that no data were available for analysis, either because reports or tool outcomes were not available for other partners to reference prior to their tool implementation (e.g. OIE PVS Pathway, NAPHS, etc.) or because questionnaires were not completed regarding specific tools (FAO–LMT and FAO–ATLASS); 17 of 19 FAO–ATLASS missions involved the full assessment with laboratory and surveillance modules, two were laboratory module only
For the temporal directionality of implementation analysis, the authors found that the OIE PVS Pathway and FAO–LMT were implemented before other tools 98% and 80% of the time, respectively. Conversely the FAO–SET, NBW and NAPHS more frequently followed the implementation of all other tools (Table III). This pattern is most likely influenced by the date of tool creation and the total number of countries where the tool has been implemented with other tools. Specific directional relationships regarding tools like the OIE PVS Pathway, JEE, NBW and NAPHS, where one tool output is needed to initiate or inform the other, were the most frequent scenarios seen. However, the authors found that there was still some flexibility regarding the temporality of the implementation of these tools (i.e. one country completed a JEE prior to an OIE PVS Pathway evaluation; one country implemented an NAPHS prior to a JEE; and two countries completed NBWs prior to or during a JEE) (Table III).
Table III. Temporal directionality of the implementation of nine One Health tools.
Numbers indicate, from left to right, the number of times both tools were used by the same country, and the number of times and the percentage of times tools in columns preceded tools in rows. Cells shaded in grey indicate where tools in columns precede tools in rows more than 50% of the time. For example, OIE PVS Pathway and JEE were both used in 88 countries, the OIE PVS Pathway preceded the JEE 87 out of 88 times, or 98.9% of the time Questionnaire responses and analysis reflect data available as of 2 November 2018
| Tool | OIE PVS Pathway (precedes) | FAO–LMT (precedes) | OHZDP (precedes) | JEE (precedes) | FAO–ATLASS(a) (precedes) | OH–SMART (precedes) | FAO–SET (precedes) | NBW (precedes) | NAPHS (precedes) |
|---|---|---|---|---|---|---|---|---|---|
| OIE PVS Pathway (follows) | 36, 5, 13.9% | 19, 0, 0% | 88, 1, 1.1% | 16, 0, 0% | 16, 0, 0% | 13, 0, 0% | 12, 0, 0% | 54, 0, 0% | |
| JEE (follows) | 88, 87, 98.9% | 35, 35, 100% | 19, 9, 47.4% | 17, 9, 52.9% | 16, 5, 31.2% | 13, 0, 0% | 10, 2, 20% | 59, 1, 1.7% | |
| NBW (follows) | 12, 12, 100% | 9, 9, 100% | 7, 5, 71.4% | 10, 8, 80% | 5, 3, 60% | 6, 5, 83.3% | 6, 4, 66.7% | 8, 5, 62.5% | |
| FAO–SET (follows) | 13, 13, 100% | 13, 13, 100% | 11, 10, 90.9% | 13, 13, 100% | 4, 2, 50% | 7, 4, 57.1% | 6, 2, 33.3% | 12, 3, 25% | |
| FAO–LMT (follows) | 36, 31, 86.1% | 15, 1, 6.7% | 35, 0, 0% | 12, 0, 0% | 14, 0, 0% | 13, 0, 0% | 9, 0, 0% | 27, 0, 0% | |
| FAO–ATLASS (follows) | 16, 16, 100% | 12, 12, 100% | 6, 4, 66.7% | 16, 7, 43.8% | 9, 3, 33.3% | 4, 2, 50% | 5, 2, 40% | 13, 3, 23.1% | |
| OHZDP (follows) | 19, 19, 100% | 15, 14, 93.3% | 19, 10, 52.6% | 6, 2, 33.3% | 11, 1, 9.1% | 11, 1, 9.1% | 7, 2, 28.6% | 16, 3, 18.8% | |
| OH–SMART (follows) | 16, 16, 100% | 14, 14, 100% | 11, 10, 90.9% | 16, 10, 62.5% | 9, 5, 55.6% | 7, 2, 28.6% | 6, 1, 16.7% | 15, 4, 26.7% | |
| NAPHS (follows) | 54, 54, 100% | 27, 27, 100% | 16, 13, 81.2% | 59, 58, 98.3% | 13, 10, 76.9% | 15, 11, 73.3% | 12, 9, 75% | 8, 3, 37.5% | |
| Compared to all others | 254, 248, 97.6% | 161, 129, 80.1% | 104, 52, 50.0% | 256, 107, 41.8% | 82, 31, 37.8% | 94, 29, 30.6% | 79, 18, 22.8% | 63, 12, 19.0% | 204, 19, 9.3% |
FAO: Food and Agriculture Organization of the United Nations
FAO–ATLASS: FAO Assessment Tool for Laboratories and Antimicrobial Resistance Surveillance Systems
FAO–LMT: FAO Laboratory Mapping Tool
FAO–SET: FAO Surveillance Evaluation Tool
IHR: International Health Regulations
JEE: Joint External Evaluation
NAPHS: National Action Plan for Health Security
NBW: IHR/PVS National Bridging Workshop
OIE PVS Pathway: World Organisation for Animal Health Performance of Veterinary Services Pathway
OHZDP: One Health Zoonotic Disease Prioritization Tool
OH–SMART: One Health Systems Mapping and Analysis Resource Toolkit
17 of 19 FAO–ATLASS missions involved the full assessment with laboratory and surveillance modules, two were laboratory module only
For the 30 countries where the authors assessed sharing and use of tool outcomes for implementation, completed questionnaires were obtained for only seven of the nine tools (OIE PVS Pathway, JEE, NBW, FAO–SET, OHZDP, OH–SMART and NAPHS). Of all the tools, OH–SMART used information from the most tools (OIE PVS Pathway, JEE, NBW, OHZDP and NAPHS) and with more frequency than any other tool. This was, in part, because OH–SMART was used to support multisectoral zoonotic disease workforce planning and National AMR Action Planning, using protocols that explicitly required the synthesising and processing of outcomes and outputs from these other tools. In fact, in some cases, OH–SMART implementation was delayed to allow for prior use of the OHZDP.
The outcomes of the OHZDP were not always available prior to the implementation of other tools but, when they were, countries almost always took the opportunity to use them. For example, there were eight occasions when OHZDP outcomes were available to use as a reference for assessing established zoonotic disease surveillance capacity in the JEE, and they were used on seven of those occasions (7/8, 88%). Similarly, OHZDP outcomes were used to inform the implementation of OH–SMART exercises (10/10, 100%), the FAO–SET tool (8/8, 100%), and the disease-specific group work conducted as part of the NBW (5/5, 100%) (Table II). The JEE outcomes were used by the most tools assessed (NBW, NAPHS, OHZDP and OH–SMART). The JEE (25/30, 83%) and NBW (11/11, 100%) relied heavily on the OIE PVS Pathway for implementation. The OIE PVS Pathway, being one of the earliest tools implemented of those analysed, did not have many opportunities to use other tools during implementation; however, in the two opportunities where the OIE PVS Pathway could have been informed by another tool, it did reference two other tools (JEE and FAO–SET). Not all tool outcomes were readily available for immediate reference by other tool implementers, either due to restrictions on sharing reports broadly, limited ability to access outcomes, delays in report processing, or lack of awareness of other concurrent work on the part of authors (Table II).
Conceptual model and overarching conceptual framework
A conceptual model was generated representing the authors’ consensus on the links and synergies between the 12 tools for advancing One Health implementation (Fig. 1). This flow diagram depicts one way in which tools and their outputs might be used to inform and strengthen outputs from other, subsequently or concurrently, implemented tools. In addition, the model can help countries to select appropriate tools according to the specific output they seek to strengthen. As the conceptual model was being developed, the tools fell into five categories: Assessment, Prioritisation, Action Planning, Implementation and Monitoring. Together they created an implementation cycle that fits an overarching conceptual framework that could inform future tool use (Fig. 2).
Fig. 1.
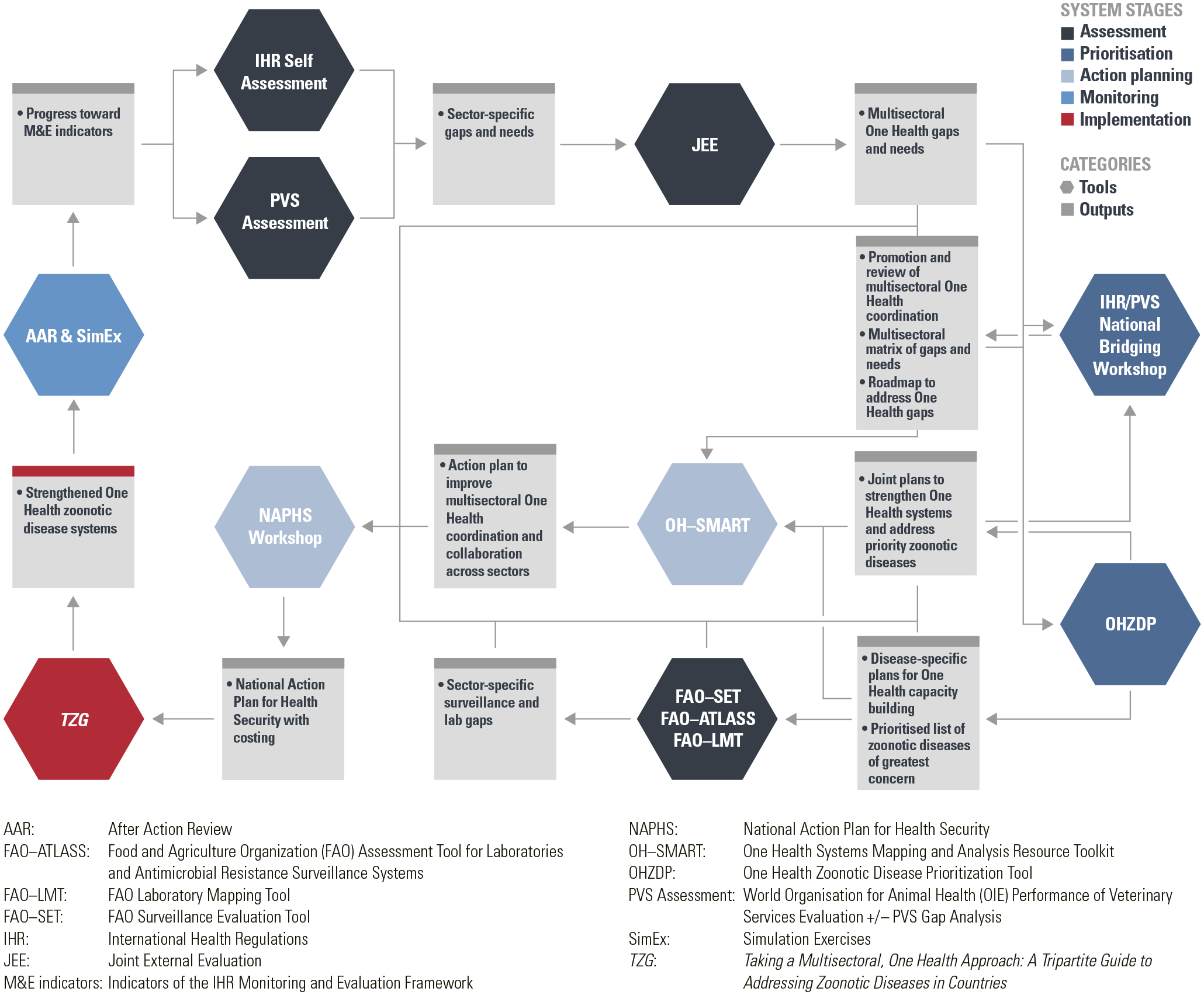
Conceptual model
Fig. 2.

Overarching conceptual framework
Discussion
This paper presents, for the first time, a summary of key tools and processes that have supported One Health assessment and implementation globally. It also proposes a model and framework for how these tools could potentially complement each other and be implemented in a coordinated fashion when used in countries to strengthen the implementation of a One Health approach.
The conceptual model is not intended to be prescriptive, but rather to highlight a potential approach to linking and coordinating the implementation of these One Health tools for maximal benefit and impact for countries. While this should be seen as one potential approach among the many opportunities available to countries working to strengthen One Health, the results represent a consensus among diverse partners as to the importance of promoting the sharing of outcomes among partners and working collaboratively as they plan the implementation of additional One Health tools.
Lessons learned
Unique to this paper was the focus on One Health tools that have been implemented extensively in the field (>5 countries), have already been implemented cooperatively using a One Health approach, and focus specifically on strengthening multisectoral, One Health systems. This paper and resulting suggestions have drawn extensively on the authors’ own personal experiences in implementing these tools across many countries. The authors also drew on their experiences in working with many partners to coordinate the implementation of those One Health tools to best support countries. Although the coordination of these tools in countries has been field-tested through ad hoc collaborations and communications during implementation, there is a need for a more systematic way to share timelines and objectives as well as to share outputs and lessons learned. Sharing experiences more systematically would greatly strengthen countries’ ability to select the most relevant tools for greatest impact and would also help to maximise outcomes. Operationalising One Health remains challenging, as it is often driven by funding timelines and organisational priorities, but certain practices can help make the benefit more sustainable. It would be beneficial to consider mechanisms to coordinate One Health efforts more systematically, including following guidance, such as that provided by the TZG, on a) mapping the current national One Health infrastructure and context, b) establishing multisectoral coordination mechanisms to formalise coordination and communication across all relevant sectors, and c) implementing technical activities using a multisectoral, One Health approach. Ensuring the timely, transparent and wide release of results and outcomes from One Health tools and processes through a variety of media, including websites, reports and publications, would further maximise countries’ ability to share successes, lessons learned and best practices to help to strengthen One Health. Improving information and knowledge flow among implementing partners on tool use and outcomes will greatly strengthen country One Health implementation and improve a country’s ability to drive change and strengthen One Health processes. Where possible, funders and implementers should support countries in advancing their abilities to facilitate coordination, collaboration, communication and information sharing through known means; for example, individual countries can support multisectoral coordination mechanisms, establish sharing platforms, including portals and websites, and enhance their own coordination efforts.
The authors found that in almost all instances where outcomes were made available to tool implementers, by direct sharing or through open-sourced online reports, outcomes were used to inform the implementation of other tools. Similarly, tool implementation was most effective when it was coordinated and supported a planned national effort to strengthen One Health across the partners supporting that goal. There are numerous examples of when the outcomes of the implementation of one tool can be used to inform the implementation of another, for example:
In many countries, implementation of the JEE led to increased awareness of the gaps in the country’s One Health capacity, and this then allowed countries to adapt other tools (NBW, OHZDP, OH–SMART) to target their efforts to prioritise these gaps.
The outcomes of an OHZDP, which requires human and animal health and environmental agencies and other relevant partners to work together to identify the zoonoses of greatest concern, have been used to help to focus surveillance evaluations (FAO–SET) and inform disease-specific mapping exercises (NBW and OH–SMART). The outcomes of an OHZDP are also important for obtaining high scores when carrying out a JEE or using the WHO SPAR Tool. For example, for a country to obtain a capacity score of 2 or greater for indicator P.4.1 (Coordinated surveillance systems in place in the animal health and public health sectors for zoonotic diseases/pathogens identified as joint priorities), animal and public health sectors must have jointly prioritised zoonotic diseases using input from all relevant sectors (25).
The planned use of outputs from the IHR SPAR, OIE PVS Pathway, JEE, and OHZDP for OH–SMART-based Zoonotic Disease Workforce Planning and National AMR Action Planning. Through these planned implementation strategies, action plans were developed specifically to build on information and outputs generated during prior implementation of the IHR annual reporting, OIE PVS Pathway evaluation, JEE and OHZDP. This yielded a much more informed and targeted workforce action plan than would have resulted from an isolated workforce planning effort. This kind of planned sequencing, where tool implementation protocols explicitly link to outputs or synergies of other tools, should be encouraged.
When multiple One Health tools have been implemented, and there is coordination among the implementers, the authors have noted better targeted and strengthened assessments, plans and analyses for a country. This provides continuity and clarity for the countries in terms of integrating One Health tool outputs and outcomes to help them to meet their country goals. However, this kind of coordination has not always occurred and, in fact, most often, the implementation has not followed the conceptual model presented. Information is not communicated that might have been valuable to tool implementation. In developing the conceptual model and temporal analysis, the authors realised that lack of coordination and communication resulted in missed opportunities to strengthen the outcomes (plans, assessments, analyses) of their own tools by building on previous tool implementation efforts in the countries.
It is also clear, based on this review, that there has been a disproportionate emphasis placed on building tools and processes for assessment, rather than tools that support One Health prioritisation, action planning, implementation or monitoring. Implementation of the One Health approach is greatly facilitated by tools and guidance that can support countries in implementing sustainable day-to-day One Health operations and functions on the ground, e.g. the TZG, its associated operational tools, and disease-specific tools (e.g. Stepwise Approach to Rabies Elimination [26]). It is also critical to continually improve implementation and the system as a whole through ongoing prioritisation, action planning and monitoring and evaluation. This helps countries to establish a multisectoral, One Health approach to building and sustaining functional multisectoral health systems which, in turn, helps them to achieve optimal health outcomes for people and animals and their shared environment.
Best practices for future implementation
As the authors developed the conceptual model, a flexible conceptual framework emerged that could help countries in implementing One Health tools at the national level in a more systematic way to maximise outcomes and impact. This framework places tools into one (or more) of five operational categories of work: Assessment, Prioritisation, Action Planning, Implementation and Monitoring. This conceptual framework is intended to inform tool implementation and support country One Health mechanisms to ensure strong synergy and that the outputs of tool implementation are used effectively to support the achievement of overall country goals. And, encouragingly, the results from the directionality and outcome use analyses both show that what has been implemented to date, though somewhat ad hoc, also aligns with this suggested conceptual model and framework.
The tools the authors evaluated and listed in the conceptual model only reflect those that met the inclusion criteria; however, there are currently many tools that are at varying stages of development (from those that are fully developed and implemented to those that are in the early stages of planning [5, 24]) that could be used by a country. Moving forward, countries can consider the elements of the framework when implementing One Health and in developing One Health or other multisectoral coordination tools and approaches in their countries. In the experience of the authors, each tool works best when it is supported, targeted and informed by the other categories of tools. The authors recommend that this framework be used to identify where there may be a need to develop new tools in a particular category and determine how best to coordinate data sharing among other existing One Health tools.
Possibly the most important best practice that the authors identified lies in the use of One Health tools themselves. Tools that provide an opportunity to jointly improve coordination and collaboration among diverse sectors and stakeholders produce specific outputs that support assessment, prioritisation, action planning, implementation and monitoring of One Health tools and processes. Additionally, coordinating the use of these tools results in stronger outputs for each, and a stronger One Health system over all. However, one less obvious outcome that the authors feel is actually crucial to advancing One Health is that the use of these tools builds relationships and trust among One Health partners. In implementing these tools, it is clear that One Health is most functional and most active when the different sectors understand and trust each other regardless of other factors in the system. This kind of understanding and trust can only exist where there are shared priorities and ongoing collaboration. These tools provide the kind of continuing collaboration and coordination that make a multisectoral, One Health approach operational and functional.
Conclusions
Over the last decade, global recognition of the inherent value of linking human health, animal health, the environment, and other relevant sectors has been increasing. Similarly, there has been growing awareness of the need to take a multisectoral, One Health approach to health threats existing or arising at the human–animal–environment interface (27). Additionally, the authors have seen increasing recognition of the shared roles and responsibilities of the human health and animal health sectors in many countries (12, 24), and a trend towards growing recognition of the environmental health and wildlife sectors as key partners in One Health. Moreover, recognition that other sectors and disciplines, notably finance, education, civil society and communities, and the security sector, also play key roles in the successful application of a One Health approach. One Health partners in countries are requesting an expansion of tools designed to evaluate and strengthen One Health approaches. In response, a number of additional One Health tools have been developed and are currently under development (5, 24). The best approach to implementation of this growing array of One Health tools is not always clear to countries which are generally offered support for different tools on a case-by-case basis, which may result in an ad hoc approach to tool implementation. Ideally, countries, funding partners and those developing and supporting countries in the implementation of tools could – and should – play a role in ensuring the alignment of One Health tool implementation for maximum impact. The intention of this paper is to highlight the complementary nature of a series of One Health tools by providing a concise conceptual model for the most commonly used tools and an overarching conceptual framework to inform the implementation of these and other tools. The authors’ goal in providing this model and framework is to enhance the operationalisation of One Health at the national level.
Acknowledgements
The authors gratefully acknowledge the contributions of Kendra McCormack Grahl and Benjamin Blair to the manuscript, tables and figures.
References
- 1.Wernli D, Haustein T, Conly J, Carmeli Y, Kickbusch I & Harbarth S (2011). – A call for action: the application of the International Health Regulations to the global threat of antimicrobial resistance. PLoS Med, 8 (4), e1001022. doi: 10.1371/journal.pmed.1001022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griggs D, Stafford-Smith M, Gaffney O, Rockström J, Ohman MC, Shyamsundar P, Steffen W, Glaser G, Kanie N & Noble I (2013). – Sustainable Development Goals for people and planet [Policy]. Nature, 495 (7441), 305–307. doi: 10.1038/495305a. [DOI] [PubMed] [Google Scholar]
- 3.Sachs JD (2012). – From Millennium Development Goals to Sustainable Development Goals. Lancet, 379 (9832), 2206–2211. doi: 10.1016/S0140-6736(12)60685-0. [DOI] [PubMed] [Google Scholar]
- 4.World Organisation for Animal Health (OIE) (2019). – PVS Pathway, 10 years together to improve Veterinary Services. Available at: www.oie.int/for-the-media/press-releases/detail/article/pvs-pathway-10-years-together-to-improve-veterinary-services/ (accessed on 14 February 2019).
- 5.Berthe FCJ, Bouley T, Karesh WB, Le Gall FG, Machalaba CC, Plante CA & Seifman RM (2018). – Operational framework for strengthening human, animal and environmental public health systems at their interface. World Bank, Washington, D.C., United States of America, 152 pp. Available at: http://documents.worldbank.org/curated/en/703711517234402168/Operational-framework-for-strengthening-human-animal-and-environmental-public-health-systems-at-their-interface (accessed on 14 February 2019). [Google Scholar]
- 6.World Health Organization (WHO), World Organisation for Animal Heath (OIE) & Food and Agriculture Organization of the United Nations (FAO) (2019). – Taking a multisectoral, One Health approach: a Tripartite guide to addressing zoonotic diseases in countries. WHO, Geneva, Switzerland; OIE, Paris, France; & FAO, Rome, Italy, 166 pp. Available at: www.oie.int/tripartitezoonosesguide (accessed on 29 March 2019). [Google Scholar]
- 7.World Health Organization (WHO) (2008). – Zoonotic diseases: a guide to establishing collaboration between animal and human health sectors at the country level. WHO, Geneva, Switzerland, 20 pp. Available at: https://apps.who.int/iris/handle/10665/207731 (accessed on 14 February 2019). [Google Scholar]
- 8.Travis DA, Chapman DW […] & Rwego IB (2014). – One Health: lessons learned from East Africa. Microbiol. Spectr, 2 (1), OH–0017–2012. doi: 10.1128/microbiolspec.OH-0017-2012. [DOI] [PubMed] [Google Scholar]
- 9.Rwego IB, Babalobi OO, Musotsi P, Nzietchueng S, Tiambo CK, Kabasa JD, Naigaga I, Kalema-Zikusoka G & Pelican K (2016). – One Health capacity building in sub-Saharan Africa. Infect. Ecol. Epidemiol, 6, 34032. doi: 10.3402/iee.v6.34032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sukumaran A & Pradeepkumar AS (2015). – One Health approach: a platform for intervention in emerging public health challenges of Kerala State. Int. J. One Hlth, 1, 14–25. doi: 10.14202/IJOH.2015.14-25. [DOI] [Google Scholar]
- 11.National Center for Emerging and Zoonotic Infectious Diseases, Division of High-Consequence Pathogens and Pathology, Centers for Disease Control and Prevention (CDC) (2011). – Operationalizing ‘One Health’: a policy perspective – taking stock and shaping an implementation roadmap. CDC, Atlanta, Georgia, United States of America, 24 pp. Available at: www.cdc.gov/onehealth/pdf/atlanta/meeting-overview.pdf (accessed on 14 February 2019). [Google Scholar]
- 12.Salyer SJ, Silver R, Simone K & Barton Behravesh C (2017). – Prioritizing zoonoses for global health capacity building – themes from One Health zoonotic disease workshops in 7 countries, 2014–2016. Emerg. Infect. Dis, 23 (Suppl. 1), S55–S64. doi: 10.3201/eid2313.170418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Food and Agriculture Organization of the United Nations (FAO) (2019). – Emergency Prevention System for Animal Health (EMPRES–AH). Available at: www.fao.org/ag/againfo/programmes/en/empres/tools_SET.html (accessed on 14 February 2019).
- 14.Food and Agriculture Organization of the United Nations (FAO) (2019). – FAO to release laboratory mapping tool on the Web. Available at: www.fao.org/ag/againfo/programmes/en/empres/news_130514.html (accessed on 14 February 2019).
- 15.Food and Agriculture Organization of the United Nations (FAO) (2018). – FAO regional training aims to improve access to new tool for assessment of laboratories and AMR surveillance systems. Available at: www.fao.org/asiapacific/news/detail-events/en/c/1129839/ (accessed on 14 February 2019).
- 16.World Health Organization (WHO) (2014). – WHO–OIE Operational Framework for Good Governance at the Human–Animal Interface. WHO, Geneva, Switzerland, 103 pp. Available at: www.who.int/ihr/publications/WHO-OIE_Operational_Framework/en/ (accessed on 14 February 2019). [Google Scholar]
- 17.World Health Organization (WHO) (2016). – IHR (2005) Monitoring and Evaluation Framework. Joint External Evaluation Tool: International Health Regulations (2005). Joint External Evaluation Tool and process overview. WHO, Geneva, Switzerland, 7 pp. Available at: http://apps.who.int/iris/bitstream/handle/10665/252755/WHO-HSE-GCR-2016.18-eng.pdf?sequence=1&isAllowed=y (accessed on 14 February 2019). [Google Scholar]
- 18.World Organisation for Animal Health (OIE) (2019). – The OIE Tool for the Evaluation of Performance of Veterinary Services (OIE PVS Tool). Available at: www.oie.int/solidarity/pvs-evaluations/oie-pvs-tool/ (accessed on 14 February 2019).
- 19.World Organisation for Animal Health (OIE) (2019). – PVS gap analysis. Available at: www.oie.int/solidarity/pvs-gap-analysis/ (accessed on 14 February 2019).
- 20.World Health Organization (WHO) (2013). – WHO/HSE/GCR/2013.2. International Health Regulations (2005). IHR core capacity monitoring framework: checklist and indicators for monitoring progress in the development of IHR core capacities in States Parties. WHO, Geneva, Switzerland, 53 pp. Available at: www.who.int/ihr/checklist/en/ (accessed on 14 February 2019). [Google Scholar]
- 21.Errecaborde KM, Pelican KM, Kassenborg H, Prasarnphanich OO, Valeri L, Yuuzar E, Fauzi RPS, Budayanti NS, Suwandono A, Artama WT, Adisasmito W & Dutcher T (2017). – Piloting the One Health Systems Mapping and Analysis Resource Toolkit in Indonesia. Ecohealth, 14 (1), 178–181. doi: 10.1007/s10393-017-1207-3. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) (2018). – One Health Zoonotic Disease Prioritization Workshop. Available at: www.cdc.gov/onehealth/global-activities/prioritization-workshop.html (accessed on 14 February 2019).
- 23.Barton Behravesh C, Dutcher T, Salyer S, Riviere Cinnamond A, Pelican K & Nel LH (2017). – Papers presented at the Symposium ‘Operationalizing One Health: One Health Tools in the Context of Global Health Security’, held during the 66th Annual Meeting of the American Society of Tropical Medicine and Hygiene, 5–9 November, Baltimore, Maryland, United States of America. Available at: www.abstractsonline.com/pp8/#!/4395/session/12 (accessed on 14 November 2018).
- 24.Machalaba CC, Salerno RH […] & Wannous C (2018) – Institutionalizing One Health: from assessment to action. Hlth Secur, 16 (Suppl. 1), S37–S43. doi: 10.1089/hs.2018.0064. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization (WHO) (2018). – International Health Regulations (2005): State Party Self-Assessment Annual Reporting Tool. WHO, Geneva, Switzerland, 34 pp. Available at: www.who.int/ihr/publications/WHO-WHE-CPI-2018.16/en/ (accessed on 13 February 2019). [Google Scholar]
- 26.Lembo T & Partners for Rabies Prevention (2012). – The Blueprint for Rabies Prevention and Control: a novel operational toolkit for rabies elimination. PLoS Negl. Trop. Dis, 6 (2), e1388. doi: 10.1371/journal.pntd.0001388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Häsler B, Cornelsen L, Bennani H & Rushton J (2014). – A review of the metrics for One Health benefits. In One Health (Karesh WB, ed.). Rev. Sci. Tech. Off. Int. Epiz, 33 (2), 453–464. doi: 10.20506/rst.33.2.2294. [DOI] [PubMed] [Google Scholar]


