Abstract
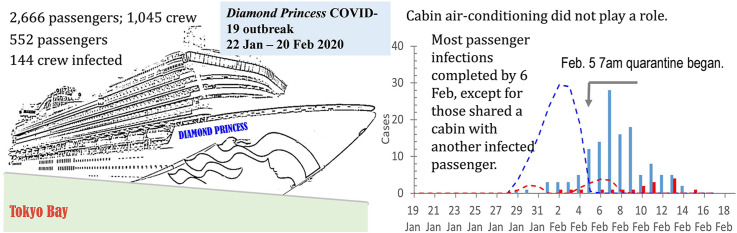
An outbreak of COVID-19 occurred on the Diamond Princess cruise ship in January and February 2020 in Japan. We analysed information on the cases of infection to infer whether airborne transmission of SARS-CoV-2, the causative agent of COVID-19, had occurred between cabins. We infer from our analysis that most infections in passengers started on 28 January and were completed by 6 February, except in those who shared a cabin with another infected passenger. The distribution of the infected cabins was random, and no spatial cluster of the infected can be identified. We infer that the ship's central air-conditioning system for passenger's cabins did not play a role in SARS-CoV-2 transmission, i.e. airborne transmission did not occur between cabins during the outbreak, suggesting that the sufficient ventilation was provided. We also infer that the ship's cabin drainage system did not play a role. Most transmission appears to have occurred in the public areas of the cruise ship, likely due to crowding and insufficient ventilation in some of these areas.
Keywords: COVID-19, SARS-CoV-2, Close-contact transmission, Airborne transmission, Building ventilation, Cruise ship
Graphical abstract
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic continues to spread worldwide, leading to significant morbidity and mortality, disrupting human social interactions and depressing the world economy. However, much remains unknown about the roles of air-conditioning systems on transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of COVID-19. Airborne transmission of SARS-CoV-2 has been acknowledged since October 2020 by leading health authorities [1,2]. Several outbreak investigations also demonstrated the probable existence of airborne transmission of SARS-CoV-2 [3,4]. For airborne respiratory infection, building ventilation plays an important role. However, no existing ventilation standard considers the requirements for infection control in non–health care settings (e.g., Refs. [5,6].
In this context, analysing the effect of quarantine on the large COVID-19 outbreak that occurred on the Diamond Princess cruise ship in Japan may shed light on possible SARS-CoV-2 transmission routes. It may reveal the influence of the central air-conditioning system and ventilation of the ship on transmission.
By 5 March 2020, 696 cases of SARS-CoV-2 infection had been confirmed amongst people who had been passengers or crew on the most recent voyage of the Diamond Princess cruise ship, which comprised 3,711 persons (2,666 passengers and 1,045 crew) [7]. Of the confirmed cases, 552 were passengers and 144 were crew. In addition, 410 cases were asymptomatic. On 20 January, an 80-year-old man (passenger X) came aboard as a passenger in Yokohama, Japan. He developed a fever on 23 January, disembarked at Hong Kong on 25 January and on 1 February was confirmed to be infected with SARS-CoV-2. The Diamond Princess continued her voyage, visiting four other ports in the region and then returning via Yokohama to Tokyo, Japan, arriving on 3 February (earlier than her scheduled date of 4 February). From 7 a.m. on 5 February, the Diamond Princess was quarantined at sea by Japanese authorities, and the 2,666 passengers were told to remain in their cabins. The quarantine ended on 19 February. On 1 March, all of the passengers and crew disembarked.
A cruise ship on a voyage functions like a small town or community. Cruise ships typically replicate all of the possible crowded indoor environments found on land, such as restaurants, swimming pools, casinos, theatres, bars, food streets, and hotels. Thus, as passengers and crew all sleep, eat and play on board, a cruise ship is probably one of the most crowded 24-h human-made communities. Unsurprisingly, large outbreaks of noroviral infection have been reported to frequently occur on cruise ships [8].
During the concerned voyage of the Diamond Princess cruise ship, its on-board public spaces were open to all passengers from 20 January to 4 February, but were immediately closed when the Japanese authorities implemented a 14-day quarantine from 7 a.m. on 5 February. During the quarantine period, passengers were required to remain in their cabins. A cabin in a ship is also nautically referred to a stateroom. Those outer cabins had access to balcony doors. Thus, the transmission routes of SARS-CoV-2 on board may be pinpointed by examining who was infected before and during the quarantine period. That is, as passengers remained in their cabins, an absence of cross-room transmission of SARS-CoV-2 during this period would imply that there was no airborne transmission of SARS-CoV-2 via the ship's recirculating central air-conditioning system or due to is drainage systems. Evidence and a probable explanation of a lack of airborne infection between cabins during such a large outbreak of COVID-19, which has been posited to be an airborne disease [9], would have significant implications.
2. Methods
2.1. Data collection
We collected daily data on the 197 symptomatic cases of SARS-CoV-2 infection on the ship from 20 January to 18 February 2020, and retrieved data on the implemented quarantine measures and implementation schedules from the website of the Ministry of Health, Labour and Welfare, Japan [10]. We also extracted from the same website data on the 146 passenger cases of SARS-CoV-2 infection, which comprised 17 in the ‘close contact’ category, who shared a cabin with one or more infected individuals, and 129 in the ‘non-close contact’ category, who did not share a cabin with infected individuals. We obtained the distribution of the infected cabins on the ship from Ref. [11]. We obtained the itinerary of the ship from Ref. [12]. We searched the websites of national/local health authorities in Vietnam, Hong Kong and Taiwan. We also obtained basic data on the ship, such as its space ratio, and the number and size of its cabins, from Ref. [13]. Finally, the ship's air-conditioning design was obtained from Ref. [14].
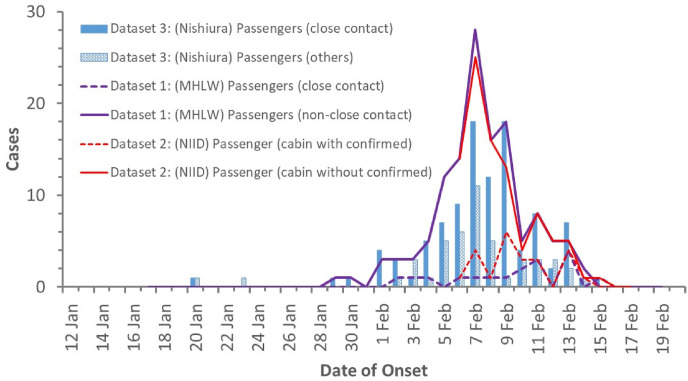
We found a total of three sets of onset data (Table 1 ) on infected passengers for the Diamond Princess COVID-19 outbreak in two categories, i.e. close contact and non-close contact. The three datasets are compared in Fig. 1 .
-
•
Dataset 1: MHLW data [10]: This dataset was presented at the ‘Press conference on the situation of the novel coronavirus disease in the cruise ship off the coast of Yokohama’, held in the MOFA Press Conference Room from 20:40 to 21:40 on Friday 21 February 2020. We extracted the data from the original Fig. 2 in the presentation, entitled ‘Number of COVID-19 cases with symptoms among the passengers on the cruise ship (by close contact status, as of 02/19/2020)’ (https://www.mhlw.go.jp/content/10200000/Fig.2.pdf). There are a total of 146 cases of infected passengers (17 for the close-contact category and 129 for the non-close-contact category). Note that the original figure caption stated that the data covered 149 passengers, but the data shown in the figure actually covered 146 passengers.
-
•
Dataset 2: NIID data [15]: This dataset was obtained from Field briefing: Diamond Princess COVID-19 cases, 20 Feb. Update.
(https://www.niid.go.jp/niid/en/2019-ncov-e/9417-covid-dp-fe-02.html; (Original Table 2. Characteristics of COVID-19 cases with reported onset dates of 6–17 February 2020 (n = 163)). This comprised 115 cases of infected passengers: 23 of these occurred in cabins with a confirmed case, and 52–92 in cabins without a confirmed case.
-
•
Dataset 3: Nishiura data [7]. The paper was received by the journal on 25 February 2020, and was thus assumed to be more up-to-date than the official NIID or MHLW data. It comprised 150 cases of infected passengers, as summarised in Ref. [7].
Table 1.
A summary of the three passenger onset datasets in the Diamond Princess COVID-19 outbreak.
Fig. 1.
A summary of the three datasets of daily onset of symptoms among the two categories of passengers, i.e. close contact (those who shared a room or cabin with an infected passenger) and non-close contact or others (those who did not share a room or cabin with an infected passenger).
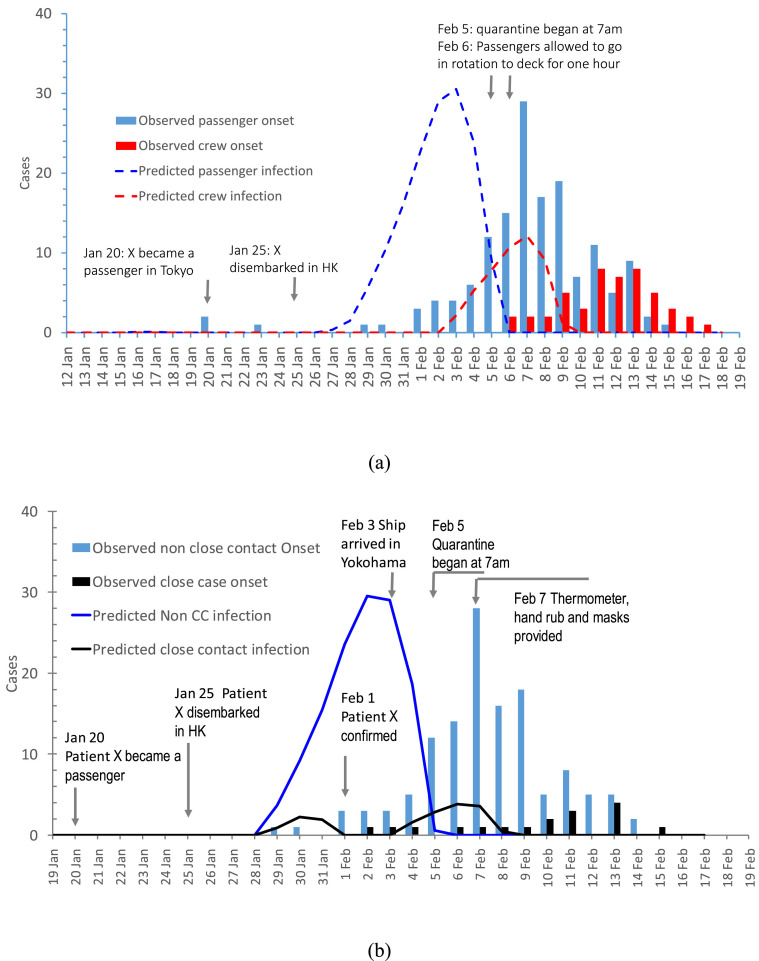
Fig. 2.
(a) Estimated infection dates and observed symptom onset dates for 149 passengers and 48 crew during the Diamond Princess COVID-19 outbreak on 22 January-20 February 2020; and (b) for those passengers infected due to close contact (sharing a cabin with an infected passenger) or due to non-close contact (not from sharing a cabin with an infected passenger). Note that some cases of close-contact passenger infection also occurred on 6–7 February, which differs from the inference that no infections occurred on these two days, as shown in (a).
The three datasets appear to differ significantly. Dataset 3 [7] contains the largest number of passengers in the close-contact category. Both the ‘non-close contact’ and ‘passengers in cabins without a confirmed case’ categories in the official MHLW and NIID datasets are referred to as ‘the first confirmed case in each cabin’. The ‘passengers with close contact’ category in Dataset 3 seems to refer to ‘passengers sharing a cabin with an infected passenger’ [36] . This explains why the number of close contacts in Dataset 3 is greater than that in the two official datasets, i.e. Dataset 1 of MHLW and Dataset 2 of NIID, as Dataset 3 contains both the first and the subsequent cases of infections in each cabin. Thus, the three datasets are relatively consistent. The consistency of the three datasets can also been seen from the estimated infected dates (Fig. S1). In this study, we chose to use Dataset 1, which contains more cases than Dataset 2.
2.2. Estimation of incubation period
The incubation period , i.e. the probability of the onset of symptoms on the jth day after exposure, is required for estimating the exposure time of the observed 197 symptomatic cases of SARS-CoV-2 infection. This is done by identifying a sufficient number of confirmed cases of infection with definite exposure periods (less than four days) and symptom-onset dates. In mainland China, local Municipal Health Commissions in most prefecture-level cities announced relatively detailed daily descriptions of the confirmed COVID-19 cases. A case description generally included age, sex, city, symptom onset date, hospitalisation date, confirmation date, and infection trajectory/history of the individual. Descriptions of some cases also included their relationships with other confirmed cases. We searched the nationwide websites of all non-Hubei local municipal health commission, and retrieved all publicly available data before 6 February 2020, as done in Ref. [16]. A total of 7,544 confirmed cases were collected from 303 cities with a population more than 500,000, in 31 provinces, municipalities, and autonomous regions and two special administrative regions (Hong Kong and Macao), accounting for 82.9% of the 9,099 confirmed cases in non-Hubei areas in China during the period (22,112 cases in Hubei alone). Seventeen PhD students and post-doctoral researchers collected the data, prepared a database in a unified format, and performed a cross-check to ensure data accuracy. From the 7,506 confirmed cases with sufficiently detailed descriptions, we selected ones with determined exposure times and symptom onset times, and excluded cases with an exposure period longer than 3 days to reduce the uncertainty of the infection dates [17]. Finally, we identified 234 cases. A list of these confirmed cases is shown in Supplementary Information III.
Eight parametric distributions for the estimations, namely gamma, inverse-Gaussian, Weibull, log-normal, log-logistic, log-student, log-Cauchy and log-Laplace distributions, are attempted for estimating the incubation period. To estimate the parameters in the eight probability distributions, we used three methods, i.e. curve-fitting methods, maximum-likelihood estimation methods and time-series estimation methods. Detailed information is provided in Supplementary Information II. After evaluation (Table S4, and Fig. S3), the log-normal distribution is chosen for the present analysis.
2.3. Pinpointing transmission venues and transmission routes
We adopted an approach to first pinpoint the transmission venues of SARS-CoV-2 on board by examining who was infected before and during the quarantine period. This is done by estimating the exposure time of the observed 197 symptomatic cases of SARS-CoV-2 infection. During the quarantine period, passengers could have only been infected in their cabins. For example, if there were a spatial cluster of infected cabins with the infected during the quarantine period around an air handling unit (AHU) on board, then the roles of the specific air handling unit might be implied.
Thus, we estimated the daily number of exposed (infected) individuals who had received a sufficient dose of SARS-CoV-2 to develop disease symptoms, and defined these individuals as symptomatic cases. Let be the number of exposed (infected) cases on day n, the daily number of individuals with onset of symptoms and the probability of the onset of symptoms on the jth day after exposure, where follows a log-normal distribution; see Section 2.2.
The daily numbers of infected cases and new symptomatic cases are related by the following equation (Eq. (1)), as follows:
| (1) |
where is the longest incubation period from infection (exposure) to symptom onset. By re-writing this equation in a matrix form for the entire study period of N days, we obtain Eq. (2):
| (2) |
where and . is an matrix with for , ; otherwise .
Equation (2) is ill-posed. The daily number of infected cases,, is obtained by ensuring the following constraints.
-
•
A non-negative condition, : i.e. the daily number of infected cases cannot be a negative number.
-
•
The calculation was conducted for the duration to meet the condition, : i.e. the total number of infected individuals must be equal to the total number of individuals displaying symptoms.
-
•
A modulus minimum condition (Tikhonov regularisation): we select the solution that minimises the modulus, i.e. .
Following these constraint conditions, we define the extended symptom-onset matrix , and the extended incubation period matrix as follows:
We then obtain the following equation (Eq. (3)):
| (3) |
where .
The choice of affects the numerical solutions. Parametric analyses indicated that the use of afforded the best solutions. The validation of this method for SARS-CoV-2 infection-time analysis is shown in Fig. S4.
The steepest descent method was used to solve the above nonlinear problem. A previous version of this approach was combined with an approximation method to estimate the infection rate due to general infection spreaders during the 2003 SARS epidemic. This method predicted the reported occurrence of all seven of the SARS super-spreading events in Hong Kong and Singapore in 2003 [18], in terms of both the exposure times and the numbers of infected cases.
After the exposure time is determined, we determine the exposure time of the ‘close contact’ and ‘non-close contact’ category passengers. Such information is used to determine the likely infection venue, i.e.in the cabins or in the public areas.
3. Results
Fig. 2a shows the inferred daily SARS-CoV-2 infections for the 146 passengers and 48 crew of the Diamond Princess who were infected from 20 January to 18 February 2020. The figure suggests that the infection actually started on January 28 in passengers (other than in passenger X), and that no new cases of infection occurred after 6 February (Fig. 2a). However, it seems that crew members continued to become infected on and after 6 February.
By classifying the 146 infected passengers into ‘close contact’ and ‘non-close contact’ categories, we found that the close contact infections occurred after the quarantine began on 5 February. These close contact infections occurred in those passengers who shared a cabin with infected passengers (Fig. 2b). There appear to have been two waves of infection within the close contact passengers. The number of close contact infected passengers was small, as a maximum of four passengers shared each cabin [13].
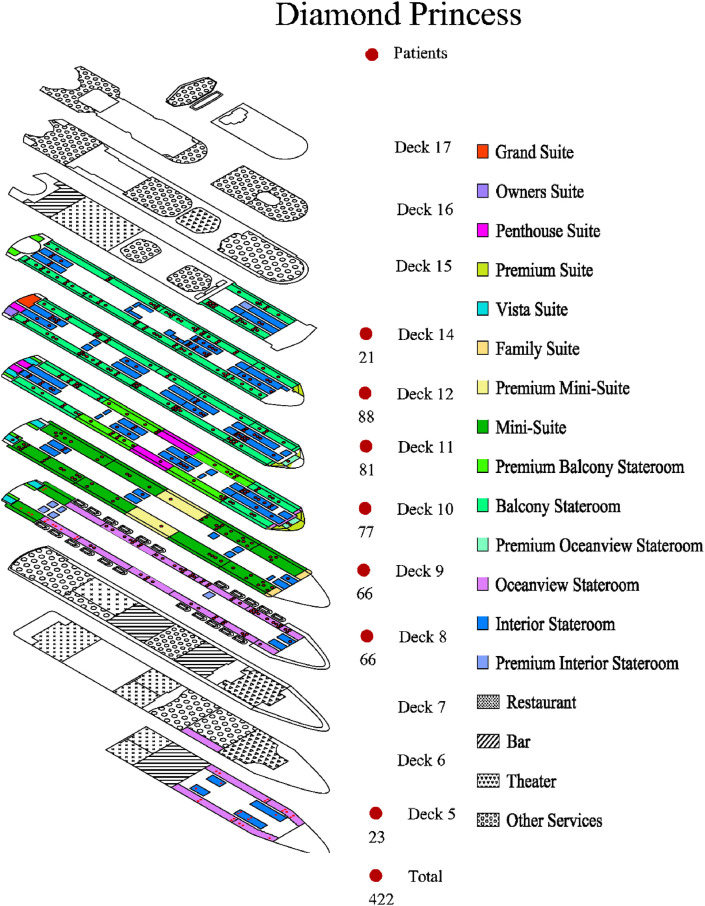
Amongst the 1,353 cabins available on board, the cabin area is 15–16 m2 for 1,137 ‘interior’, ‘oceanview’ and ‘balcony’ rooms, 26 m2 for 186 ‘mini suite’ rooms, 31 m2 for 29 suites or family suites, and 58 m2 for one grand room. We obtained the data on the distribution of the confirmed cases in these different types of rooms, and no difference was found. The distribution of the infected cabins was random (Fig. 3 ), and no spatial cluster of the infected can be identified.
Fig. 3.
The distribution of the infected cabins with data retrieved from Ref. [11]. Each confirmed case is shown by a black dot in where the cabin of the infected passenger lived on the ship. The total number of the infected cases on each deck is shown by a large red dot. The cabin types are coloured. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
4. Discussion
4.1. Most infections occurred before quarantine with no cross-room transmission between cabins during quarantine
Our major finding is that passengers who became infected but who did not share a cabin with an infected individual (i.e. non-close-contact passengers) were estimated to have been infected prior to 5 February, and after 6 February, infections occurred only in those passengers who were in close contact with previously infected passengers, i.e. passengers who shared a cabin with one or more previously infected passengers (Fig. 2b).
It is known that the infection began amongst the passengers [19], and the peak day of passenger infections is inferred to have been 3 February, the date on which the ship arrived in Yokohama, Japan. The decline of the estimated daily infection rate after 3 February is unsurprising, as from this day some passengers probably started to minimise their close contact and social gatherings. The daily rate of crew infection is inferred to have peaked on 7 February, suggesting that substantial close contact continued to occur between crew members after the quarantine was imposed on 5 February. This is not surprising, as the crew members will have had to continue providing services to the passengers [19].
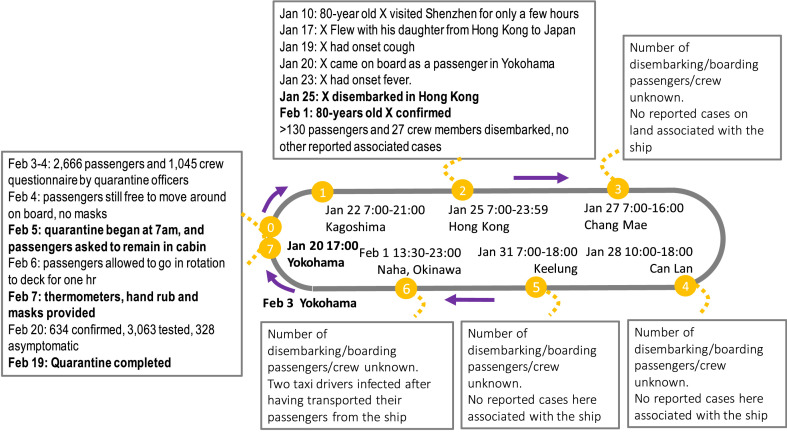
Our major finding is also supported by the chronological events associated with the outbreak, which are summarised in Fig. 4 . As can be seen, aside from the two taxi-drivers in Okinawa, Japan, there were no secondary infections reported in any of the ports visited by the ship during its 14-day round-trip voyage, prior to its arrival in Yokohama, Japan. More than 130 passengers and 27 crew members disembarked in Hong Kong on 25 January, including 80-year-old passenger X (case no. 14 in Hong Kong, [20]. No other confirmed cases were identified among these disembarked passengers (86 Hong Kong residents) and crew members in Hong Kong, suggesting that minimal SARS-CoV-2 transmission occurred on board on 20–25 January, which is consistent with the observed onset data and our estimated infection data (Fig. 2a). No confirmed cases associated with disembarked passengers from this ship were reported in its visited ports in Vietnam and Taiwan [21]. identified 627,386 potential contact-persons of the more than 3,000 passengers that disembarked at Keelung, and none were found to be infected.
Fig. 4.
Chronological events associated with the Diamond Princess COVID-19 outbreak on 22 January-20 February 2020, Which were compiled using official information from websites of the local/national health authorities from Japan, Hong Kong, Vietnam and Taiwan, and the data from Ref. [22].
The significantly lower numbers of infection among passengers after 6 February are in line with the quarantine that was imposed from 7 a.m. on 5 February, during which passengers were required to remain in their cabins, and with masks being made available from 7 February; see the left-side box in Fig. 4. Thus, after 6 February, infections occurred only in those passengers who were in close contact with previously infected passengers, i.e. passengers who shared a cabin with one or more previously infected passengers (Fig. 2b).
The daily number of infections among passengers decreased significantly following the imposition of quarantine, but according to our estimation, daily passenger infections declined from 3 February, as passengers had by this date become aware of the outbreak and begun to take precautions. In contrast, passengers who became infected by sharing a cabin with a previously infected passenger (i.e. the close-contact category) acquired their infections either prior to or after the 5 February quarantine.
4.2. Implication to the roles of air conditioning in cabins and public areas as infection venues
The differences in our estimated daily infections prior to and after the 5 February quarantine reveal the possible transmission venues and the transmission routes involved in the outbreak of COVID-19 on the Diamond Princess cruise ship.
Notably, our estimated data show that there was no cross-room transmission between passengers who were in different cabins during the quarantine period. This might be partially explained by the fact that no recirculation was allowed during the quarantine period. On the other hand, among the 46 confirmed passenger cases, 129 were non-close-contact passengers and only 17 were close-contact ones, suggesting that the possible lack of cross infection within each individual infected cabin even prior to quarantine, not to mention between cabins. This strongly suggests that the ship's central air-conditioning system did not play a role in SARS-CoV-2 transmission, i.e. that long-range airborne transmission did not occur between cabins during the outbreak. Rather, the estimated higher infection of non-close contact passengers prior to the quarantine implies that most transmission occurred in public areas, which such public area infection was absent during the quarantine as access to the public areas was not possible. All non-close-contact transmission between passengers who did not share cabins appears to have occurred prior to 5 February. However, as in the available dataset, only 17 passengers became infected via close-contact (within-cabin) transmission, the estimated infection dates might not be sufficiently accurate, and thus the data presented in Fig. 2b are indicative only. It is nevertheless clear that the peak daily infection date of the close-contact category is behind that of the non-close-contact or beyond-cabin contact category. The spatial distribution of the infected passengers' cabins (Fig. 3) also revealed that the central air-conditioning of cabins did not play a role in transmission.
The Diamond Princess was built in 2004 by Mitsubishi Industries [14]. A centralised full-air air-conditioning system with variable air volume was designed and installed in all of the passenger cabins and crew cabins. This supplies 30% fresh outdoor air for cabins, 50% for public areas and 100% for clinics and kitchens. A fully independent exhaust-air system was installed in all of the bathrooms. The additional air supply to each cabin escapes to the corridor where the ceiling return is located. Central air-conditioning systems are commonly designed in spatial zones, as was done on this ship, where each air handling unit (AHU) serves one zone. There are 88 AHUs on the Diamond Princess [14]. The random distribution of cases of infection on all of the ship's decks and the lack of any spatial clusters of close contact (within cabin) infection (Fig. 3) suggests that no particular AHU cabin zones had more cases of infection, and thus no AHUs were more responsible for the spread of SARS-CoV-2 than others [23]. analysed the World Dream cruise ship COVID-19 outbreak, and also stated that ‘all COVID-19 patients were widely distributed in all 18 decks across the ship’, i.e. there were no spatial clusters of infection.
The infection settings prior to the quarantine on 5 February may have been similar to those during norovirus outbreaks that have occurred on cruise ships in recent years. The Diamond Princess herself had an outbreak of gastroenteritis caused by norovirus in February 2016, which afflicted 158 passengers and crew, according to the New South Wales Ministry of Health [24]. Noroviral infections on cruise ships affect large numbers of people [25], often a hundred or more. Crowding has been cited as an explanation for this cruise-ship noroviral infection phenomenon [25,26]. Surfaces in cruise-ship public restrooms are known to have high potential for faecal contamination during the norovirus outbreaks [27]. A significant number of positive SARS-CoV-2 RNA surface samples were found on the Diamond Princess on 22–23 February [28]. It may be interesting to note that no positive samples were found in two of the studied public areas (a clinic and 5th floor restaurants).
However, the dominate transmission routes of SARS-CoV-2 and norovirus are expected to differ, and for SARS-CoV-2, the “chance of transmission through inanimate surfaces is less frequent” [29]. The crowding and close contact common in leisure and social activities enjoyed by passengers outside their cabins may explain the observed higher rates of infections prior to the quarantine amongst passengers who did not share a room with previously infected passengers. Significant SARS-CoV-2 transmission on the Diamond Princess may have occurred due to crowding and the insufficient ventilation in public spaces. The ventilation rates per person in these public areas are also unknown.
More than two thousands of superspreading events or outbreaks of COVID-19 have been documented [30]. Swinkels concluded that “nearly all SSEs [super spreading events] in the database took place indoors”. High attack rates have bene reported in venues or activities such as Choir rehearsal with an attack rate of 53–87% [3,31], fitness centers [32], and nightclubs [4] with either heavy activities or deep breathing. Restaurants, gyms and cafes were found to be the high risk venues for COVID-19 infection, following an analyses of the mobile phone data in 10 cities in the US [33]. The restaurants, casinos, theatres, and bars on the cruise ship offer similar venues. The possibility of SARS-CoV-2 cross-infection in public areas in this superspreading event suggests the importance of controlling occupancy or improving ventilation in crowded spaces.
The above analyses are notable, as [28] reported that a surface swab taken from a corridor ceiling return vent on board the Diamond Princess tested positive for SARS-CoV-2 RNA, which suggests that these ceiling vents were difficult to access for disinfection and cleaning, and that SARS-CoV-2 may be airborne. The infection data from this large outbreak of COVID-19 provide what appears to be one of the first evidences that the airborne transmission of SARS-CoV-2 may not necessarily occur in the presence of infection sources and susceptible individuals. It is important yet difficult to obtain evidence of the airborne transmission of SARS-CoV-2 during outbreaks of COVID-19, and similar evidence for other respiratory viruses, but less is known about the difficulty and importance of obtaining evidence that an airborne virus does not cause airborne infection. Crucially, such evidence may enable the threshold ventilation rate for minimising airborne infection risk to be determined.
No measured ventilation rate has been reported for the Diamond Princess. International standards, such as ISO 7547:2004 [37], stipulate a minimum ventilation rate of 8 L/s per person. It has also been reported that the maximum possible volume of outdoor air was supplied during the quarantine period, suggesting that the operating ventilation rate may have been higher than 8 L/s per person during the outbreak. No information is available for the ventilation distribution among cabins, which depends on the system balance. The lack of transmission between cabins prior to quarantine implies that a reasonably ventilated indoor environment, such as the cabins on the ship, prevented airborne infection. It will be very useful if the ventilation rates in such infection venues could be measured immediately after such an outbreak is identified.
4.3. Importance of implementation of immediate intervention
We determined that most infections on the ship occurred during the pre-quarantine period, when passengers and crew members were still in regular and often close contact in public areas. The data also show that the on-board transmission must have been rather limited prior to 28 January. This was shown by the fact that none of the more than 130 passengers and 27 crew members who disembarked in Hong Kong on 25 January developed COVID-19, and that no on-land cases were reported in Chang Mae and Cai Lan in Vietnam, or in Keelung [21].
Seventy-seven (59.7%) of the 129 cases of infections amongst the passengers occurred during the ship's journey between Okinawa and Yokohama, Japan, i.e. on 2–4 February. It is notable that the daily numbers of on-board infections only started to increase from 28 January (Fig. 2a). However, there were few symptomatic cases of infection on board on 31 January. This probably explains why no local residents became infected in the port of Keelung. Interestingly, two taxi drivers in Okinawa, Japan were confirmed to be infected on 14 February and 19 February, respectively [34], and both had transported ship passengers on 1 February. This possible infection date is consistent with the significant number of infected individuals on the ship, although most of these individuals were pre-symptomatic or asymptomatic at this time. We did not have access to the passenger/crew boarding and disembarking data at the other three ports; we only had data for Hong Kong and Keelung [21] for analysis.
Our analyses show that when the 80-year-old former passenger X's infection had been confirmed on 1 February, the ship should have immediately disembarked all of its passengers and quarantined them on land. However, this may have been considered unachievable. Our estimation shows that the quarantine implemented at 7 a.m. on 5 February effectively protected the passengers, but not the crew, probably because the crew had to continue servicing the needs of passengers. There is therefore a need for improved prevention measures for crews in similar situations.
4.4. Limitations of the study
Our estimation method was not without limitations. Due to incomplete data, we were unable to rule out the possibility that additional infections occurred during the latter part of the quarantine period. Of the 634 cases confirmed by 20 February, although 328 were asymptomatic, 306 were symptomatic at the time of confirmation. However, onset data were available for only 197 of the 306 symptomatic individuals, and the analysis of further data from the remaining 109 symptomatic individuals may change our estimation. Asymptomatic cases can also contribute to the infection, which are not included in our analysis. Our estimated data also did not include possible transmission between crew and passengers prior to and during the quarantine period, as may have occurred during meal service.
We used the estimated SARS-CoV-2 incubation period from 234 patients in China, with known dates of infection and onset of symptoms. As the governing equation for this is known to be ill-posed, we made assumptions (see Methods section and [18]. However, this method successfully predicted all seven of the reported super-spreading events in the 2003 SARS epidemics in Hong Kong and Singapore. Fig. S4 shows that we also successfully estimated the infection date for the 234 patients.
Finally, our approach cannot be used to study the role of asymptomatic cases in the transmission of SARS-CoV-2. These cases were first detected on the ship when testing was extended to all of the passengers on 15 February, subsequent to testing only those with symptoms [35]. If data on the spatial distribution of both symptomatic and asymptomatic cases become available (i.e. the rooms where all of the passengers with confirmed cases of infection stayed), it may be possible to infer whether and how any asymptomatic transmission occurred.
Author contributions
Y.L. and H.Q. contributed to the conception and design of the study; P.X. contributed to the modelling; Y.L., W.J., S.X., H.Q., T.M., M.K. and H.T. contributed to the data collection and analyses; and H.-L.Y., W.J., B.J.C. M.K and H.T. contributed to the analyses and interpretation. Y.L. wrote the manuscript and all of the authors contributed to the revision.
Declaration of competing interest
The authors declare no competing financial interest.
Acknowledgements
This work was supported by the Research Grants Council of Hong Kong’s General Research Fund (grant number 17202719) and the Collaborative Research Fund (grant number C7025-16G). We thank Dr Emi Takashita of the National Institute of Infectious Diseases, Tokyo for clarifying the differences between the three datasets.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.buildenv.2021.107839.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.US CDC . 2020. Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission.https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html Updated on 15 October 2020. (Accessed on 15 November 2020) [Google Scholar]
- 2.World Health Organization Coronavirus disease (COVID-19): how is it transmitted? 2020. https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted
- 3.Miller S.L., Nazaroff W.W., Jimenez J.L., et al. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air. 2020:1–10. doi: 10.1111/ina.12751. 00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kang C.R., Lee J.Y., Park Y., et al. Coronavirus disease exposure and spread from nightclubs, South Korea. Emerg. Infect. Dis. 2020;26(10):2499–2501. doi: 10.3201/eid2610.202573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ASHRAE Standard 62.1-2019. Ventilation for Acceptable Indoor Air Quality. American Society of Heating, Refrigerating and Air-Conditioning Engineers, Atlanta, USA.
- 6.European Committee for Standardization CEN . European Standard EN 16798-3:2017; Brussels: 2017. Energy Performance of Buildings - Ventilation for Buildings - Part 3: for Non-residential Buildings - Performance Requirements for Ventilation and Room-Conditioning Systems (Modules M5-1, M5-4) [Google Scholar]
- 7.Nishiura H. Backcalculating the incidence of infection with COVID-19 on the Diamond princess (editorial) J. Clin. Med. 2020;9(3):657. doi: 10.3390/jcm9030657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US CDC Outbreak updates for international cruise ships. 2020. https://www.cdc.gov/nceh/vsp/surv/gilist.htm
- 9.Morawska L., Milton D.K. It is time to address airborne transmission of COVID-19. Clin. Infect. Dis. 2020;71(9):2311–2313. doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mhlw Press conference: situation of the COVID-19 in the cruise ship ‘Diamond Princess’. 2020. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/newpage_00032.html
- 11.NHK. COVID-19 Battle on the cruise ship. NHK documentary. https://www3.nhk.or.jp/nhkworld/en/ondemand/video/4001368
- 12.Yutaka Club Cruises International 2020/1/20 Diamond princess: 16 days of exploring Southeast Asia in early spring (in Japanese) 2020. https://www.yutakaclub.co.jp/tourdetail/point/4589
- 13.Cruisedeckplans Deck plans for Diamond princess. 2020. https://www.cruisedeckplans.com/DP/deckplans/Diamond-Princess
- 14.Kosako M., Shiiyama K. Introduction of air-conditioning system design for a large cruise ship: Princess Cruises Mitsubishi Grand Series implementation example. Journal of the Japan Society of Naval and Ocean Engineers. 2008;17:24–26. doi: 10.14856/kanrin.17.0_24. [DOI] [Google Scholar]
- 15.NIID (National Institute of Infectious Diseases) Field briefing: Diamond princess COVID-19 cases. February 19, 2020 with correction on February 20. https://www.niid.go.jp/niid/en/2019-ncov-e/9407-covid-dp-fe-01.html https://www.niid.go.jp/niid/en/2019-ncov-e/9417-covid-dp-fe-02.html
- 16.Qian H., Miao T., Liu L., Zheng X., Luo D., Li Y. Indoor transmission of SARS‐CoV‐2. Indoor Air. 2020 doi: 10.1111/ina.12766. 2020. [DOI] [PubMed] [Google Scholar]
- 17.Cowling B.J., Muller M.P., Wong I.O., et al. Alternative methods of estimating an incubation distribution: examples from severe acute respiratory syndrome. Epidemiology. 2007;18(2):253–259. doi: 10.1097/01.ede.0000254660.07942.fb. [DOI] [PubMed] [Google Scholar]
- 18.Li Y., Yu I.T., Xu P., et al. Predicting super spreading events during the 2003 severe acute respiratory syndrome epidemics in Hong Kong and Singapore. Am. J. Epidemiol. 2004;160(8):719–728. doi: 10.1093/aje/kwh273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kakimoto K., Kamiya H., Yamagishi T., et al. Initial investigation of transmission of COVID-19 Among crew members during quarantine of a cruise ship — Yokohama, Japan, February 2020. Morb. Mortal. Wkly. Rep. 2020;69(11):312–313. doi: 10.15585/mmwr.mm6911e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CHP CHP investigates additional case of novel coronavirus infection. https://www.info.gov.hk/gia/general/202002/01/P2020020100795.htm
- 21.Chen C.M., Jyan H.W., Chien S.C., et al. Containing COVID-19 among 627,386 persons in contact with the Diamond Princess cruise ship passengers who disembarked in Taiwan: big data analytics. J. Med. Internet Res. 2020;22(5):1–9. doi: 10.2196/19540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakazawa E., Ino H., Akabayashi A. Chronology of COVID-19 cases on the Diamond Princess cruise ship and ethical considerations: a report from Japan. Disaster Med. Public Health Prep. 2020;14(4):506–513. doi: 10.1017/dmp.2020.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sekizuka T., Itokawa K., Kageyama T., et al. Haplotype networks of SARS-CoV-2 infections in the Diamond Princess cruise ship outbreak. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(33):20198–20201. doi: 10.1073/pnas.2006824117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ABC News . 4 Feb. 2016. Cruise Ship Hit by Norovirus Gastroenteritis Docks in Sydney.https://www.abc.net.au/news/2016-02-04/gastro-outbreak-hits-158-aboard-luxury-cruise-liner-in-sydney/7138950 [Google Scholar]
- 25.Harris J.P., Lopman B.A., et al. Infection control measures for norovirus: a systematic review of outbreaks in semi-enclosed settings. J. Hosp. Infect. 2010;74:1–9. doi: 10.1016/j.jhin.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 26.Bert F., Scaioli G., et al. Norovirus outbreaks on commercial cruise ships: a systematic review and new targets for the public health agenda. Food Environ Virol. 2014;6:67–74. doi: 10.1007/s12560-014-9145-5. [DOI] [PubMed] [Google Scholar]
- 27.Carling P.C., Bruno-Murtha L.A., et al. Cruise ship environmental hygiene and the risk of norovirus infection outbreaks: an objective assessment of 56 vessels over 3 years. Clin. Infect. Dis. 2009;49:1312–1317. doi: 10.1086/606058. [DOI] [PubMed] [Google Scholar]
- 28.Yamagishi T., Ohnishi M., Matsunaga N., Kakimoto K., et al. Environmental sampling for severe acute respiratory syndrome coronavirus 2 during COVID-19 outbreak in the Diamond Princess cruise ship. J. Infect. Dis. 2020;222(7):1098–1102. doi: 10.1093/infdis/jiaa437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mondelli M.U., Colaneri M., Seminari E.M., et al. Low risk of SARS-CoV-2 transmission by fomites in real-life conditions. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30678-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Swinkels K. SARS-CoV-2 Superspreading events around the world. 2020. https://docs.google.com/spreadsheets/d/1c9jwMyT1lw2P0d6SDTno6nHLGMtpheO9xJyGHgdBoco/edit?usp=sharing
- 31.Charlotte N. High rate of SARS-CoV-2 transmission due to choir practice in France at the beginning of the COVID-19 pandemic. J. Voice. 2020 doi: 10.1016/j.jvoice.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bae S., Kim H., Jung T.Y., et al. Epidemiological characteristics of COVID-19 outbreak at fitness centers in Cheonan, Korea. J. Kor. Med. Sci. 2020;35(31):e288. doi: 10.3346/jkms.2020.35.e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang S., Pierson E., Koh P.W., et al. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2020:1–6. doi: 10.1038/s41586-020-2923-3. [DOI] [PubMed] [Google Scholar]
- 34.Mhlw 2020. https://www.mhlw.go.jp/content/10906000/000598149.pdfhttps://www.mhlw.go.jp/stf/newpage_09539.html
- 35.Wikipedia Coronavirus pandemic on cruise ships. 2020. https://en.wikipedia.org/wiki/2020_coronavirus_pandemic_on_cruise_ships
- 36.Takashita E (personal Communication), WHO Collaborating Center for Reference and Research on Influenza Virus Research Center, National Institute of Infectious Diseases, Tokyo, Japan.
- 37.ISO 7547:2004 . ISO Standard; 2004. Ships and Marine Technology – Air-Conditioning and Ventilation of Accommodation Spaces – Design Conditions and Basis of Calculations. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.