Abstract
Purpose
The proximal tibiofibular joint (PTJF) can be injured with the structures in the lateral aspect of the knee in a multi-ligament knee injury (MLKI) patient. Such injuries are scarce but require attention in the management of the complex MLKIs. The assessment and management of such injuries are not well described in the English literature. This study describes the frequency of PTFJ injuries, clinical assessment and functional outcomes of such injuries in MLKI patients.
Methodology
The data were collected retrospectively from the cohort from 2013 to 2018. The 84 MLKI were included in the study, out of which 9 patients had associated PTFJ injury. All the PTFJ injuries were operated by one single surgeon (D.S) which involves stabilization with K-wires (Kirschner wire) and fixation with 4 mm cancellous cannulated screw along with reconstruction surgery for MLKI in single stage.
Results
The frequency of PTFJ injury in our patient cohort is 10.71%. Three patients out of the nine patients received Larson procedure apart from the fixation of PTFJ. At a mean follow-up of 13 months, the Lysholm score was 77.4 (range: 69–86) and mean modified Cincinnati score was 62 (range: 52–72). There was grade I posterior laxity present in one patient with PCL and PLC injury, one patient with ACL, PCL and PLC injury, and one patient with ACL, PCL, MCL and PLC injury at final follow-up. Terminal flexion of 15° or more restriction was noted in six patients. All patients were satisfied with the outcome.
Conclusion
Evaluation of PTFJ should be an integral part of preoperative as well as an intraoperative examination of MLKI patients. The fixation of this joint is of utmost importance for the reconstructive ligament procedures on the lateral aspect of the knee. The dial test used for the assessment of the integrity of PLC injury should have a prerequisite of proximal tibiofibular joint stability, otherwise, it can lead to erroneous assessment.
Level of evidence
IV.
Keywords: Multi-ligament knee injuries, Proximal tibiofibular joint, Dial test, Posterolateral corner injury, Knee assessment
Introduction
Multi-ligament knee injuries (MLKI) are uncommon but serious injuries mostly suffered due to high-velocity trauma. Such injuries require thorough evaluation and surgical planning for a satisfactory outcome. MLKI can involve the structures in the lateral aspect of the knee and rarely the proximal tibiofibular joint (PTFJ) [1]. Injury to the PTFJ is uncommon and reported mainly in athletes, as an isolated injury or in combination with other bony and ligamentous pathology [2–5]. The presentation of PTFJ injury can range from pain on the lateral aspect of the knee to fibular head subluxation or dislocation, with both acute and chronic presentation [6, 7]. All the currently used classifications for MLKI or knee dislocation do not further sub-classify the lateral side injury of the knee [8–11]. The combination of common injury involving single cruciate along with collateral injury is yet not described in any MLKI classification, thus no established classification system was used in this study. Clinical evaluation of PTFJ should be part of MLKI examination.
There are various components of posterolateral corner (PLC) injury complex including fibular collateral ligament (FCL), biceps femoris, popliteofibular ligament (PFL) and arcuate ligament. They are inserted on the fibular head [12, 13]. Unstable PTFJ can lead to an erroneous assessment of a dial test for PLC injuries. The components of PLC are repaired in acute MLKI; hence a stable PTFJ becomes necessary for the success of the repair. The PLC reconstruction procedure fails to function when PTFJ instability is unrecognized or not stabilized [1]. This can cause persistent knee instability; even put the reconstructed cruciate(s) under higher load leading to failure of reconstruction [14, 15]. Hence clinical evaluation of PTFJ should be part of MLKI examination.
Jabara et al. [1] reported the incidence of PTFJ instability in MLKI, to be 9% in their series of 129 knees in adults. PTFJ instability in chronic MLKI has been scarcely reported.
In this study, we report (A) the frequency of PTFJ instability in chronic MLKI, (B) the patient-reported outcome scores and complications involved in PTFJ stabilization in chronic MLKI, (C) further clarify assessment of lateral sided injury taking PTFJ examination and PLC evaluation by Dial test.
Material and Methods
The data for our study were retrospectively collected from the cohort of patients diagnosed and treated as chronic MLKI at a tertiary care referral teaching hospital and associated trauma centre. From 2013 to 2018, 84 patients diagnosed with chronic MLKI were operated upon by a single surgeon (D.S.). Chronic MLKI is defined as a grade 3 instability involving two or more major ligaments and time to surgery is more than 6 weeks since the injury [16]. All cases were evaluated clinically, radiologically using radiographs and MRI (Fig. 1), and examination under anaesthesia (EUA) to evaluate the integrity of the cruciate ligaments, collaterals, PLC and posteromedial corner. Associated neurovascular deficits, soft tissue or skin condition and other injuries were noted. The inclusion criteria include MLKI, more than 6-week-old injury of either gender and age more than 18 years old. Whereas the exclusion criteria included fracture-dislocation injury of the knee, bony avulsion fractures, acute (< 6 weeks) injury, vascular knee injury and open knee injury. None of the patients was a professional sportsperson and all were having mild to moderate activity levels.
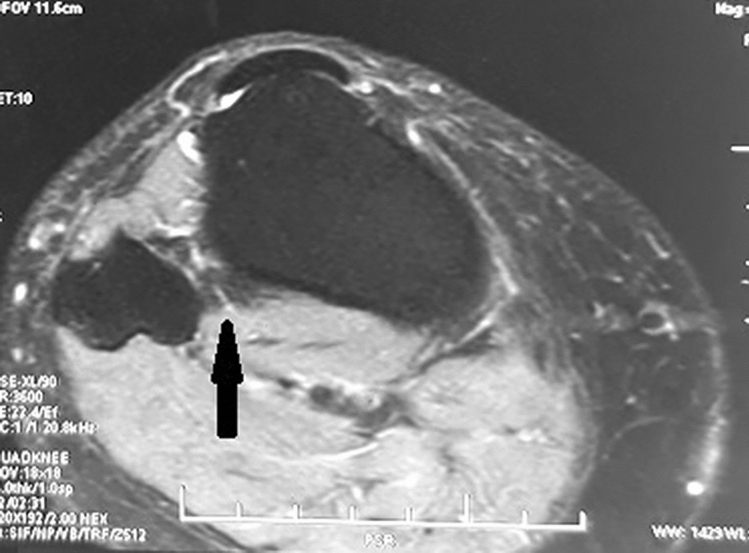
Fig. 1.
MRI STIR images showing hypointense signal intensity at PTFJ depicting injury (solid arrow)
Ethical clearance for publication was taken from the Institutional review board. Informed consent was taken from all the patients included in the study.
The PTFJ was evaluated clinically both in outpatient and under anaesthesia (EUA). Ballotment test was performed for assessment of instability of the PTFJ joint in 900 knee flexion and the translation was compared to the contralateral normal knee for reference. Any palpable difference at the time of EUA is considered as significant PTFJ instability. Grade 1 injuries have less than 5 mm of joint surface separation (opening or subluxation) during stress testing. Grade 2 injuries have between 5 and 10 mm of separation. Grade 3 injuries have greater than 10 mm of separation [17]. The joint was then classified intra-operatively as dislocated or dislocatable. Dial test for the evaluation of PLC was performed in the prone position in the outpatient department, but in the supine position during EUA [17, 18]. The mean time since the injury to definitive surgery was 5 months (range 3–8 months). All these patients were managed with single-stage reconstruction. A total of 41 patients had reconstructive procedures done on the lateral side along with other ligaments reconstruction. Of these, nine patients (Table 1) were identified to have undergone PTFJ stabilization in isolation or with Larson type PLC reconstruction. All these patients were initially managed in some other centers or hospital where these ligaments and PTFJ injuries were either missed or managed non-operatively leading to the chronicity of the injury. There were eight males and one female patient, with a mean age of 31 years (range 24–45 years). All these patients suffered road traffic accidents while on the motorbike and were referred to after initial management. Six patients had PCL injuries with PTFJ instability, two patients had ACL, PCL and PTFJ instability and one patient had ACL, PCL, MCL injury with PTFJ instability. All these cases had posterior type PTFJ dislocation, three had grade 2 and six had grade 3 instability. Dial test was positive in all patients both in the outpatient department as well as EUA.
Table 1.
Patient characteristics, ligament injury and reconstruction performed with graft source
| Patient no | Age, Sex | Time since injury (month) | Ligament injured with laxity grade | Associated injury | Ligament reconstructed (Graft source) |
|---|---|---|---|---|---|
| 1 | 25 M | 3 |
PCL grade III PLC Dial + PTFJ grade III |
– |
PCL (I/L−ST + G) PTFJ−ORIF |
| 2 | 28 M | 5 |
PCL grade III PLC Dial + PTFJ grade II |
– |
PCL (I/L-ST + G) PTFJ−ORIF |
| 3 | 37 M | 6 |
PCL grade III PLC Dial + PTFJ grade III |
– |
PCL (I/L−ST + G) PTFJ−ORIF Larson (C/L-ST) |
| 4 | 35 M | 4 |
ACL grade III PCL grade III PLC Dial + PTFJ grade III |
Healed soft tissue injury on thigh |
ACL (C/L−ST + G) PCL (I/L−ST + G) PTFJ−ORIF |
| 5 | 30 M | 3 |
PCL grade III PLC Dial + PTFJ grade II |
– |
PCL (I/L−ST + G) PTFJ−ORIF |
| 6 | 42 M | 7 |
PCL grade III PLC Dial + PTFJ grade III |
– |
PCL (I/L−PL) PTFJ−ORIF Larson (I/L−ST) |
| 7 | 24 F | 5 |
ACL grade III PCL grade III MCL grade III PLC Dial + PTFJ grade III |
Mid shaft open # both bone leg (well united by the time of surgery) |
ACL (I/L−PL) PCL (C/L−PL) MCL (I/L−ST + G) PTFJ−ORIF |
| 8 | 45 M | 3 |
ACL grade III PCL grade III PLC Dial + PTFJ grade III |
– |
ACL (I/L−ST + G) PCL (C/L−PL) PTFJ−ORIF |
| 9 | 28 M | 2 |
PCL grade III PLC Dial + PTFJ grade II |
– |
PCL (I/L-PL) PTFJ—ORIF Larsen (I/L-ST) |
ACL anterior cruciate ligament, PCL posterior cruciate ligament, PLC postero-lateral complex, PTFJ proximal tibiofibular joint, MCL medial collateral ligament, ST semitendinosus, G gracilis, PL peroneus longus, ORIF open reduction and internal fixation, I/L ipsilateral, C/L contralateral
Operative Technique
All patients were operated under combined spinal-epidural anaesthesia and tourniquet control. The opposite lower limb was also prepared in cases where autograft from the opposite leg was required. A thorough EUA was performed for the affected knee and was compared with the opposite normal knee. Diagnostic arthroscopy was performed to confirm the EUA findings. Special attention was always given to evaluate lateral side Drive Through sign, palpation of popliteus tendon to further delineate lateral side injury.
The required autografts were harvested as per planning, specific to the patient’s injury and donor site. The sequence of reconstruction was decided on the structures damaged and functional demand of the patient. The sequence of ligament reconstruction was PCL, ACL then collateral, PTFJ fixation with or without PLC reconstruction . Tunnels for associated cruciate(s) ligaments were prepared. Initially, PCL tibial and ACL femoral tunnels are prepared followed by PCL femoral and ACL tibial tunnels (Fig. 2). Only autografts grafts (from gracilis, semitendinosus, peroneus longus from either side) were used and passed through the tunnels. The ACL and PCL grafts were fixed on the femoral side, PCL was fixed with interference screw and ACL with a endobutton. MCL reconstruction was done using ipsilateral hamstring and fixed with interference screw when required (case 7). Then lateral side injury was addressed.
Fig. 2.

Post-operative radiograph depicting Larson procedure, PCL reconstruction and PTFJ fixation
The PTFJ was approached through an anterior vertical incision measuring 2–3 cm over the joint. Care was taken considering the proximity of the peroneal nerve to the incision. The joint capsule was opened. One 2 mm k wire was passed through the center of the fibular head from the lateral side and was used as a joystick for reduction. Most of the time, the PTFJ was found to get reduced easily on knee extension. Once reduced, the K wire was advanced to fix the PTFJ temporarily. The guidewire for the screw was then placed at the desired site followed by the drill bit and the insertion of 4 mm cannulated cancellous screw with the washer from the fibular head to proximal tibia crossing three cortices over a guidewire. The screw was directed from the lateral surface of center of fibular head approximately 45-degree posteroanterior direction in the sagittal plane, parallel to the joint line taking hold in three cortices.
The varus stress test, dial test and arthroscopic drive through sign was re-performed after PTFJ stabilization. If the tests were positive, a 4.5 mm tunnel in anteroposterior direction was made just distal to the screw and a Larson type PLC reconstruction was added using a semitendinosus graft. The cruciate(s) ligaments were fixed on the tibial side at the end with interference screw with appropriate knee flexion (90° for PCL and 20° for ACL) and manual tension. Sterile dressings were applied and a long knee splint with a calf pad was applied.
Patients were discharged on 3rd postoperative day with Polyvinyl chloride (PVC) molded knee hinge brace. The calf pad was used in this brace for patients undergoing PCL reconstruction. The patients with bi-cruciate ligament reconstruction were mobilized non-weight bearing for initial 3 weeks, then toe-touch weight-bearing in full extension with walker and brace for next 3 weeks. Full weight-bearing was allowed after 6 weeks depending upon patient comfort. Whereas patients with only PCL injury with PTFJ injury were allowed toe-touch weight-bearing 2 weeks from the surgery with brace and walker. Full weight-bearing was allowed after 4 weeks with brace depending upon the patient comfort. Static quadriceps exercises, ankle pumps, prone flexion and closed chain exercise were started for initial 6 weeks. Later on, open chain exercises were initiated. Straight leg raising with no weights were allowed after 3 weeks in all the patients. There was no special rehabilitation protocol followed for the ankle. Brace was continued for 3 months. Full return to activities was allowed after 9–12 months when there is a recovery of muscle strength approximately 80–85% of the unaffected leg. There was no weakness or instability of the ankle reported by any of the patients.
Patient Evaluation
Patients were followed in the outpatient department at regular intervals. The assessment included physical examination (knee stability, range of motion, pain and ballottement of fibular head for the stability of proximal tibiofibular joint, ankle stiffness and pain if there), radiographs, subjective functional outcome questionnaires (Lysholm score and modified Cincinnati knee survey score) and satisfaction level of the patients according to the Likert scale.
Radiographs were assessed at 3, 6 and 12 months post-operatively. Functional outcome was assessed by Lysholm score and modified Cincinnati knee survey score. Higher scores depict better functional knee outcome. The ankle functional scores were not included in the study.
Statistical Analysis
The data were analyzed using SPSS 22.0 software. The mean or average of the data was calculated along with the standard deviation. The Likert scale was used to assess the satisfaction level of the patient.
Results
The frequency of PTFJ injury in our patient cohort is 10.7%. Three out of the six patients with PCL, PLC and PTFJ injuries required Larson procedure apart from the fixation of PTFJ. No significant perioperative complications were noted. All the patients presented after an average of 4.2 months old injury (range 2–7 months). At a mean follow-up of 13 months (range 10–16 months, SD 1.93), the Lysholm score was 77.4 (range 69–86, SD 5.17) and mean modified Cincinnati score was 62 (range 52–72, SD 6.63) (Table 2). There was grade I posterior laxity in 3 patients (one each of PCL, PLC and PTFJ injury; bi-cruciate, MCL, PLC and PTFJ injury; bi-cruciate, PLC and PTFJ injury) at final follow-up. Terminal flexion restriction of 15 degrees or more was noted in 6 patients. All patients were satisfied with the outcome according to the Likert scale. None of the patients suffered any iatrogenic neurovascular injury. The satisfaction level, as well as return to work, depends on the associated other ligament injuries as well. One patient complained regarding the prominence of the hardware but the removal was not required in any of the patients.
Table 2.
Outcomes of the surgical reconstruction at final follow up
| Patient no | Follow up (months) | ROM (°) | Post op laxity | Lysholm score | Modified cincinnati knee survey score | Complications |
|---|---|---|---|---|---|---|
| 1 | 16 | 0–110 | PCL—grade 0 Dial test-negative | 76 | 62 | None |
| 2 | 13 | 0–120 | PCL—grade 0 Dial test-negative | 82 | 70 | None |
| 3 | 12 | 0–120 | PCL—grade 1 Dial test-negative | 80 | 66 | Prominence of screw |
| 4 | 15 | 0–100 | PCL—grade 0 Dial test-negative | 72 | 54 | None |
| 5 | 12 | 0–100 | PCL—grade 0 Dial test-negative | 76 | 60 | None |
| 6 | 14 | 0–110 | PCL—grade 0 Dial test-negative | 80 | 62 | None |
| 7 | 10 | 0–90 | PCL—grade 1 Dial test-negative valgus stress at 30°—grade 1 | 69 | 52 | None |
| 8 | 11 | 10–100 | PCL—grade 1 Dial test-negative | 76 | 60 | None |
| 9 | 14 | 0–120 | PCL—grade 0, Dial test-negative | 86 | 72 | None |
Discussion
There is an important role of PLC is providing stability to the knee. Also, PLC injuries can result in posterolateral rotary knee instability and articular cartilage degeneration [19]. Techniques of PLC reconstruction can be broadly categorized into fibular-based techniques and combined tibia-fibula-based techniques. Larson described the first procedure to reconstruct the PLC, involving the tunnel through the fibular head [20]. LaPrade et al. described an ‘anatomic’ PLC reconstruction based on combined tibia-fibula based technique [21]. The anatomic and non-anatomic reconstruction of PLC are well described in the literature. Non-anatomic reconstruction includes the techniques not reproducing the FCL, PFL and the popliteus tendon. Earlier such techniques based on single femoral tunnel and fibular sling, and later tibial-based two-tailed PLC reconstruction were described [21]. LaPrade et al. [13] introduced the concept of anatomic reconstruction of PLC involving the reconstruction of FCL, PFL and PT. This is biomechanically more stable. Hence PLC injuries with PTFJ instability are possibly a relative contradiction to non-anatomic fibular-based PLC reconstruction.
Congruity and stability of the PTFJ are utmost important for the successful reconstruction or repair procedure for PLC [13]. One of the major reasons for the failure of Larson procedure can be the undiagnosed instability of the PTFJ as reconstructive procedure pivots around the fibula head. The ‘popliteofibular ligament reconstruction’ in anatomic PLC reconstruction probably stabilize the PTFJ, thus making LaPrade’s procedure more successful. Even for the success of LaPrade’s procedures, reconstructing all the major components of the PLC requires the stability of the PTFJ to function appropriately [22]. The impact of body mass index (BMI) was not studied in this study group. obese patients are more likely to have MLKI and more complication rates [23].
There is a problem of tunnel convergence in multi-ligament reconstruction procedures. Tunnel convergence is avoided by drilling the tunnels for a collateral ligament in a divergent manner [24]. We used tunnel dilators placed in the tibial tunnels for cruciates to guide for the direction of collateral tunnels and prevent convergence. Moatshe et al. [25] further clarified drilling angles of superficial MCL and posterior oblique ligament in axial and coronal planes to avoid convergence.
The clinico-anatomical importance of the PTJF needs more elaboration and biomechanical studies for better understanding. PTFJ injuries are uncommon, mostly described in isolation. Chronic PTFJ instabilities are mostly anterolateral (67%) caused by knee hyperflexion with forced plantarflexion and eversion of foot [19]. The dislocation of PTFJ is more common when the PTFJ is oriented obliquely rather than horizontal [19]. Surgical stabilization is indicated on such injuries when adequate nonoperative measures fail for more than 3 months; stabilization with screw and free graft has been described [26, 27]. However, the scenario of MLKI associated PTFJ instabilities can be completely different. Most of the knee surgeons assess and perform the ligamentous reconstructive procedures without paying due heed to the stability of PTFJ. Our series has 10.7% PTFJ dislocations in chronic MLKI which is quite high and all are posterior dislocations; probably resulting from the motor bike-related accident rather than sports-related injury when the rider falls on the knee with a direct impact on proximal lateral tibia and fibula. All these patients had no clicking or pain on the lateral side due to the PTFJ instability, hence probably could have been missed by the initial referring surgeon, who does not examine PTFJ as a routine in such cases. The mechanism of injury in all these patients was a direct impact on the PTFJ with the knee in flexion. This leads to injury to the PTFJ sparing the ligamentous components of PLC. As the major brunt of force is borne by the PTFJ leading to its dislocation, the structure medial to it is spared. Thus, in all these patients, there was a minimal injury to the meniscus, chondral surfaces and the components of PLC like popliteus tendon, PFL, FCL, etc. Due to late presentation, such complex injuries to the ligamentous structures on the lateral aspect of the knee are probably healed or in the healing stages. These complex injuries were not identifiable even on the MRI or surgically.
Various operative techniques have been described in the literature to stabilize this joint. These include direct repair, reconstruction of supporting ligament with split bicep femoris tendon [28] or autograft [26] (like semitendinosus tendon) and various screw/pin constructs [27]. In this study, 4 mm cannulated cancellous screw with the washer was inserted across three cortices. This technique is simple to execute and does not require much expertise and instrumentation.
To the best of our knowledge, one case series and few case reports described the PTFJ injury in MLKI of the knee. The only case series involves 12 cases of PTFJ in acute MLKI of the knee [1]. The case report mentions acute PTFJ instability [29, 30]. Few authors have noted the importance of PTFJ in weight-bearing and mechanical stability of the knee and ankle [19, 31].
The result and data from our study are in agreement with the results of previously published case series and depicts the importance of PTFJ stability in reconstructive procedures for MLKI patients. The presence of other associated ligament injuries affects the final functional outcomes. Lateral aspect of reconstruction procedures requires stability of PTFJ [32]. This can be one of the important factors for the failure of PLC reconstruction procedures. There is a need for clinical assessment of PTFJ preoperatively as well as intra-operatively in MLKI of the knee. The dial test can be erroneous in the presence of PTFJ instability.
In agreement with the authors of previously described case reports and case series, the usually recommended treatment for the patients of PTFJ instability is surgical with either screw fixation or ligament reconstruction of PTFJ, though the ideal method may be debatable [1, 34]. Recently, a systemic review by Kruckeberg et al. comparing various treatment modalities also supports the view that surgical treatment is superior to conservative management in case of PTFJ instability [16]. Fixation of PTFJ with screw requires only a minimal incision and easy surgical technique compared to the technique of the Horst and LaPrade and other ligament reconstructions [27, 28]. For ligament reconstruction, the preliminary results are good, but the surgery is technically more demanding, with larger incision and more soft tissue dissection with increased risk of common peroneal nerve injury. Results in our series using the technique of screw fixation are satisfactory. The disadvantage of this technique is the need for screw removal in some patients if pain persists at the surgical site. Another problem with screw fixation of the PTFJ is an increase in rotational forces in the ankle, which often leads to pain and instability of the ankle joint [19]. Although it is described in the literature about the effects of PTFJ arthrodesis on the ankle instability and pain, none such phenomenon was seen in this study. Ours is a retrospective study with no ankle functional score documented and none of the patient’s complaint of ankle instability or worrisome pain in the follow up. This might be due to the fact that the joint was not arthrodesed but reduced and fixed at its anatomic position which permitted some movement at PTFJ during ankle dorsiflexion.
The major limitations of our study are: A) The size of the patient cohort was small. It is because the incidence of MLKI is low and most of the PTFJ instability goes undiagnosed. B) It's a retrospective study and there is no comparison with the control group. This can also invite chances of selection and observer bias in the study. Thus, more multicentric studies with larger sample size are required to validate the results and outcomes.
Conclusion
Our study emphasizes the importance of PTFJ during the assessment of MLKI. Evaluation of this joint should be a part of preoperative as well as an intraoperative examination.
The fixation of PTFJ is of utmost importance for the reconstructive ligament procedures on the lateral aspect of the knee in chronic cases with instability. This not only provides stability to the knee joint but also prevent failure of associated ligament reconstruction procedures in long run.
The dial test used for the assessment of the integrity of PLC injury should have a prerequisite of proximal PTFJ stability, otherwise, it can lead to erroneous assessment.
Funding
None.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
Ethical clearance for publication was taken from the Institutional review board.
Informed consent
Informed consent was taken from all the patients included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dhananjaya Sabat, Email: drdsabat@gmail.com.
Rakesh Sehrawat, Email: drrsehrawat@gmail.com.
Bushu Harna, Email: bushu.edu@gmail.com.
References
- 1.Jabara M, Bradley J, Merrick M. Is stability of the proximal tibiofibular joint important in the multiligament-injured knee? Clinical Orthopaedics and Related Research. 2014;472:2691–2697. doi: 10.1007/s11999-014-3574-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmad R, Case R. Dislocation of the fibular head in an unusual sports injury: A case report. Journal of Medical Case Reports. 2008;2:158. doi: 10.1186/1752-1947-2-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lord CD, Coutts JW. A study of typical parachute injuries occurring in two hundred and fifty thousand jumps at the parachute school. The Journal of Bone and Joint Surgery. 1944;26:547–557. [Google Scholar]
- 4.Thomason PA, Linson MA. Isolated dislocation of the proximal tibiofibular joint. Journal of Trauma. 1986;26(2):192–195. doi: 10.1097/00005373-198602000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Turco VJ, Spinella AJ. Anterolateral dislocation of the head of the fibula in sports. American Journal of Sports Medicine. 1985;13:209–215. doi: 10.1177/036354658501300401. [DOI] [PubMed] [Google Scholar]
- 6.Lenehan B, McCarthy T, Gilmore SM. Dislocation of the proximal tibiofibular joint: A new method of fixation. Injury Extra. 2006;37:385–389. doi: 10.1016/j.injury.2006.02.058. [DOI] [Google Scholar]
- 7.Sekiya JK, Kuhn JE. Instability of the proximal tibiofibular joint. Journal of American Academy of Orthopaedic Surgeons. 2003;11:120–128. doi: 10.5435/00124635-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy JC. Complete dislocation of the knee joint. Journal of Bone and Joint Surgery. American Volume. 1963;45:889–904. doi: 10.2106/00004623-196345050-00001. [DOI] [PubMed] [Google Scholar]
- 9.Schenck R. Classification of knee dislocations. Operative Techniques in Sports Medicine. 2003;11(3):193–198. doi: 10.1053/otsm.2003.35918. [DOI] [Google Scholar]
- 10.Stellhorn CE. Complete dislocation of the knee joint. The American Journal of Surgery. 1934;26(2):332–335. doi: 10.1016/S0002-9610(34)90675-9. [DOI] [Google Scholar]
- 11.Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. Journal of Orthopaedic Trauma. 1997;11(7):525–529. doi: 10.1097/00005131-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Cooper JM, McAndrews PT, LaPrade RF. Posterolateral corner injuries of the knee: Anatomy, diagnosis, and treatment. Sports Medicine and Arthroscopy Review. 2006;14(4):213–220. doi: 10.1097/01.jsa.0000212324.46430.60. [DOI] [PubMed] [Google Scholar]
- 13.LaPrade RF, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clinical Orthopaedics and Related Research. 2002;402:110–112. doi: 10.1097/00003086-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Bonanzinga T, Signorelli C, Lopomo N, Grassi A, Neri MP, Filardo G, Zaffagnini S, Marcacci M. Biomechanical effect of posterolateral corner sectioning after ACL injury and reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2015;23(10):2918–2924. doi: 10.1007/s00167-015-3696-3. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade iii posterolateral knee complex injuries on anterior cruciate ligament graft force a biomechanical analysis. American Journal of Sports Medicine. 1999;27(4):469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 16.Kruckeberg BM, Cinque ME, Moatshe G, Marchetti D, DePhillipo NN, Chahla J, LaPrade RF. Proximal tibiofibular joint instability and treatment approaches: a systematic review of the literature. Arthroscopy. 2017;33(9):1743–1751. doi: 10.1016/j.arthro.2017.03.027. [DOI] [PubMed] [Google Scholar]
- 17.Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. Journal of Bone and Joint Surgery American Volume. 1976;58:159–172. doi: 10.2106/00004623-197658020-00001. [DOI] [PubMed] [Google Scholar]
- 18.Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part II. The lateral compartment. Journal of Bone and Joint Surgery American Volume. 1976;58:173–179. doi: 10.2106/00004623-197658020-00002. [DOI] [PubMed] [Google Scholar]
- 19.Ogden JA. Subluxation and dislocation of the proximal tibiofibular joint. Journal of Bone and Joint Surgery American Volume. 1974;56:145–154. doi: 10.2106/00004623-197456010-00015. [DOI] [PubMed] [Google Scholar]
- 20.Sidles JA, Larson RV, Garbini JL, Downey DJ, Matsen FA. Ligament length relationships in the moving knee. Journal of Orthopaedic Research. 1988;6:593–610. doi: 10.1002/jor.1100060418. [DOI] [PubMed] [Google Scholar]
- 21.Blackman AJ, Engasser WM, Krych AJ, Stuart MJ, Levy BA. Fibular head and tibial-based (2-tailed) posterolateral corner reconstruction. Sports Medicine and Arthroscopy Review. 2015;23:44–50. doi: 10.1097/JSA.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 22.Noyes FR, Barber-Westin SD, Albright JC. An analysis of the causes of failure in 57 consecutive posterolateral operative procedures. The American Journal of Sports Medicine. 2006;34(9):1419–1430. doi: 10.1177/0363546506287743. [DOI] [PubMed] [Google Scholar]
- 23.Ridley TJ, Cook S, Bollier M, McCarthy M, Gao Y, Wolf B, Amendola A. Effect of body mass index on patients with multiligamentous knee injuries. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014;30(11):1447–1452. doi: 10.1016/j.arthro.2014.05.035. [DOI] [PubMed] [Google Scholar]
- 24.Moatshe G, LaPrade RF, Engebretsen L. How to avoid tunnel convergence in a multiligament injured knee. Annals of Joint. 2018;1(3):93. doi: 10.21037/aoj.2018.11.05. [DOI] [Google Scholar]
- 25.Moatshe G, Brady AW, Slette EL, et al. Multiple ligament reconstruction femoral tunnels: intertunnel relationships and guidelines to avoid convergence. American Journal of Sports Medicine. 2017;45:563–569. doi: 10.1177/0363546516673616. [DOI] [PubMed] [Google Scholar]
- 26.Van den Bekerom MP, Weir A, van der Flier RE. Surgical stabilisation of the proximal tibiofibular joint using temporary fixation: A technical note. Acta Orthopaedica Belgica. 2004;70(6):604. [PubMed] [Google Scholar]
- 27.Horst PK, LaPrade RF. Anatomic reconstruction of chronic symptomatic anterolateral proximal tibiofibular joint instability. Knee Surgery, Sports Traumatology, Arthroscopy. 2010;18(11):1452–1455. doi: 10.1007/s00167-010-1049-9. [DOI] [PubMed] [Google Scholar]
- 28.Giachino AA. Recurrent dislocations of the proximal tibiofibular joint: Report of two cases. Journal of Bone and Joint Surgery. American Volume. 1986;68:1104–1106. doi: 10.2106/00004623-198668070-00023. [DOI] [PubMed] [Google Scholar]
- 29.Gabrion A, Vernois J, Havet E, Mertl P, De ML. Dislocation of the proximal tibio-fibular joint due to severe leg and knee trauma. Revue de Chirurgie Orthopedique et Reparatrice de L'appareil Moteur. 2004;90(8):749–756. doi: 10.1016/S0035-1040(04)70755-2. [DOI] [PubMed] [Google Scholar]
- 30.Reynolds AW, Bhat SB, Stull JD, Krieg JC. Case report of an isolated proximal tibiofibular joint dislocation in a professional ice hockey player. Journal of Orthopaedic Case Reports. 2018;8(1):93–95. doi: 10.13107/jocr.2250-0685.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lambert KL. The weight-bearing function of the fibula. A strain gauge study. The Journal of Bone and Joint Surgery. 1971;53:507–513. doi: 10.2106/00004623-197153030-00007. [DOI] [PubMed] [Google Scholar]
- 32.Van Seymortier P, Ryckaert A, Verdonk P, Almqvist KF, Verdonk R. Traumatic proximal tibiofibular dislocation. American Journal of Sports Medicine. 2008;36:793–798. doi: 10.1177/0363546507312162. [DOI] [PubMed] [Google Scholar]
- 33.Rajkumar P, Schmitgen GF. A new surgical treatment of an acute dislocation of the proximal tibiofibular joint. International Journal of Clinical Practice. 2002;56:556–557. [PubMed] [Google Scholar]
- 34.Robinson Y, Reinke M, Heyde CE, Ertel W, Oberholzer A. Traumatic proximal tibiofibular joint dislocation treated by open reduction and temporary fixation: A case report. Knee Surgery, Sports Traumatology, Arthroscopy. 2007;15:199–201. doi: 10.1007/s00167-006-0147-1. [DOI] [PubMed] [Google Scholar]