Abstract
Introduction
Ankle arthroscopy has come a long way since it was thought, it is not feasible because of tight joint and anatomical characteristics of ankle joint. The same anatomical features like capsular attachment and safe accessory portals are used to access the whole joint even with a rigid arthroscope. Ankle distraction method was routinely used to access the anterior ankle. However, nowadays, anterior arthroscopy is done in dorsiflexion as this increases the anterior ankle joint volume, and thereby easy access to various anatomical structures. On the other hand, intermittent traction is used to access the posterior ankle. Initially used as a diagnostic tool, ankle arthroscopy is now used extensively as a therapeutic and reconstruction tool. New evidence is published for all inside ligament reconstructions, effective management of impingement syndromes, and osteochondral lesions. The indications are being extended to fracture management and arthrodesis.
Methodology
This narrative review was performed following a literature search in the Pubmed database and Medline using the following keywords: ankle arthroscopy, portals, ankle OCD, functional outcome. Related articles were then reviewed.
Conclusion
Complications rate is reduced with a better understanding of the relative anatomy of surrounding neurovascular structures and tendons with regard to the position of ankle joint. This review on ankle arthroscopy focuses on anatomy, indications, and complications. Ankle arthroscopy is a safe and elegant tool as any other joint arthroscopy.
Keywords: Anterior ankle arthroscopy, Posterior ankle arthroscopy, Arthroscopy portals
Introduction/Background
Ankle arthroscopy is a minimally invasive diagnostic and therapeutic tool that yields speedy recovery and decreased morbidity. Today, surgeons carry out advanced therapeutic procedures like all-inside ankle ligament reconstruction, arthroscopy-assisted fracture fixation, and cartilage repair and reconstruction arthroscopically.
Arthroscopic Ankle Anatomy
A sound understanding of ankle surface anatomy, intraarticular anatomy, and anatomic variation of structures with ankle movements is crucial to make portals, to avoid iatrogenic injuries, and to differentiate and recognize normal versus abnormal.
The ankle is a load-bearing joint with a narrow intraarticular space for the passage of arthroscope and instruments. A unique feature of the ankle joint capsule is its anterior insertion unto the tibia and talus, which occurs away from the cartilage level [1]. Such an anatomic feature gives ample space in the anterior joint for arthroscope and instruments, which can be further increased by dorsiflexing the joint without the need for traction. Because of the convex shape of the talus, it is not easy to navigate a straight nonflexible arthroscope in the ankle joint, and there are chances for iatrogenic injury to the cartilage. van Dijk [2] advocated the dorsiflexion of the ankle while introducing arthroscope and instruments. The bony and soft tissue anatomical landmarks around the ankle are easily palpable and make surface markings easy. Anterior inferior tibiofibular (AITFL) and posterior inferior tibiofibular ligament (PITFL) are both intraarticular. Deltoid ligament, anterior talofibular ligament (ATFL), posterior talofibular ligament (PTFL), and calcaneofibular ligament (CFL) are intracapsular but extra-articular. Such a feature helps in easy visualization of ligaments and the management of associated pathologies during ankle arthroscopy [3].
Anterior Ankle Arthroscopy
Indications
Routine ankle arthroscopy is more sensitive than clinical examination and imaging for chondral lesions and syndesmotic injuries [4]. The main indications are the soft tissue and bony impingements, osteochondral lesions, loose bodies, and performing ankle arthrodesis [5], 6]. Ankle arthroscopy is also indicated for the management of tibial plafond and talus fractures for articular reduction, fixation, and in dealing with osteochondral injury and loose osteochondral fragments [7]. Level IV evidence shows good results following the use of ankle arthroscopy for the reconstruction of lateral ligament s of the ankle. Extended indications of ankle arthroscopy include management of septic arthritis, arthrofibrosis [8] (Table 1).
Table 1.
Anterior ankle arthroscopy indications
| Diagnostic arthroscopy before lateral ligament reconstruction, deformity and malunion correction, and syndesmosis injuries |
| Bony and soft tissue impingement |
| Ligament injury/Instability |
| Syndesmotic injury |
| Osteochondral lesions |
| Periarticular fractures |
| Chronic arthritis—Arthrodesis |
| Loose body extraction |
| Acute septic arthritis |
| Chronic synovitis |
| Arthrofibrosis of ankle |
Patient Positioning
The patient is positioned supine with a thigh tourniquet. With the leg in a knee holder, the foot is dropped 3 to 4 inches off the table to allow the surgeon’s tummy assisted ankle movements. A bolster under the gluteal region maintains the ankle in a neutral position. We do not recommend routine use of distraction. For distraction, the noninvasive ankle strap is used, which can be attached to a traction device or on to the surgeon’s body. An additional posterolateral portal can be easily made in a supine position. A lateral decubitus position and a prone position are also described for combined posterior arthroscopy (Fig. 1).
Fig. 1.

Anterior ankle arthroscopy-patient positioning
Instrumentation and Set Up
For anterior ankle arthroscopy, a 4 mm 30° arthroscope is routinely used. A 2.7-mm arthroscope is another option that may be used to view the posterior ankle through anterior portals. Large diameter arthroscopes have a substantial field of vision when compared to smaller ones, and the irrigation fluid flow is better in large arthroscopes. With a 30° arthroscope, the visual field increases with a rotation of scope and is useful in reaching difficult areas in the ankle joint. A 70° scope gives better visualization but with a blind spot in the front, where a user cannot see in the direction of scope and may damage normal structures. Arthroscope should have a matching trocar and cannula, which acts as a protective sheath for easy introduction of an arthroscope and also acts as a conduit for the irrigation fluid, both inflow, and outflow [9]. A fluid that is isotonic with body fluids like ringer lactate and isotonic saline is used. Fluid pump is not used routinely due to risk of extravasation and gravity-assisted flow is enough to maintain fluid flow in the ankle joint. The shaver and burr corresponding to the size of arthroscope are used. Sharp burrs are preferred for minimal heat generation. The latest shavers with a hand, as well as foot control, is preferred. A handheld probe is the most versatile instrument like a surgeon’s finger. Different sizes of forceps, awls, and curettes are required for bony procedures. Radiofrequency to vaporize tissues may be used.
Portals
Anteromedial and anterolateral portals are standard workhorse portals. With accurate localization of the superficial peroneal nerve, anterior ankle portals have become secure portals. As per the need, additional portals like accessory anteromedial, accessory anterolateral, sinus tarsi portal, and lateral malleolar portals may be utilized. The anteromedial portal is made first, just medial to the tibialis anterior tendon at joint level with a foot in dorsiflexion to avoid injury to tendon of tibialis anterior. Other potential structures at risk are saphenous nerve and great saphenous vein. The anterolateral portal is made just lateral to extensor digitorum longus (EDL) or peroneus tertius (PT) tendons. Most of the complications described in ankle arthroscopy are related to this portal. The nerve that is at risk is intermediate dorsal cutaneous nerve, the lateral terminal branch of superficial peroneal nerve (SPN). The anatomy of SPN varies considerably; by plantarflexion and inversion, the surgeon can see and palpate these nerves in 30% individuals. With plantarflexion, SPN moves medially and in neutral position SPN moves laterally; hence marking this nerve in plantar flexion and making an entry portal in neutral position injures the nerve. Hence, it is safer to make portal entry medial to the skin marking that is made in plantar flexion [10–13].
The anterocentral portal is not routinely used because of potential injury to neurovascular structures and is made between EDL and EHL. Lateral malleolar portal, sinus tarsi portal, and accessory anteromedial and anterolateral portals may be used. These portals are made proximal to anteromedial or anterolateral portals for ease of introducing instruments (Fig. 2).
Fig. 2.
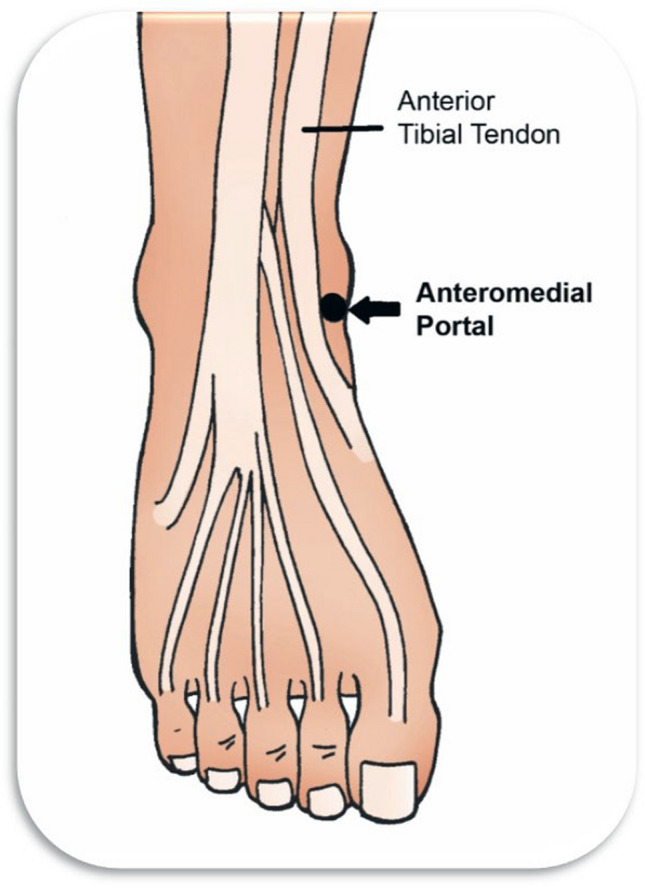
Anteromedial portal
Standard Arthroscopic Evaluation
Ferkel et al. [14] developed a 21-point examination protocol for a complete examination of the ankle joint. J Vega et al. described a 7-point examination protocol for arthroscopy in dorsiflexion and discretionary distraction, which we follow [3, 15]. The first point is the lateral shoulder of the talar dome and distal fascicle of the anterior inferior tibiofibular ligament (AITFL). Lateral talar dome acts like a reference point whenever the surgeon loses the orientation. The second point consists of the fibular attachment of the distal fascicle of AITFL and superior fascicle of the anterior talofibular ligament (ATFL), distal fibula, and lateral talar wall. The third point is the lateral talar neck and talar attachment of ATFL. The fourth point is the medial talar neck and talar neck cartilage. The fifth point is a deltoid ligament, medial malleolus, and medial talar wall. The sixth point is the medial talar dome and notch of Henry. The seventh point is the anterior distal tibial rim and central talar dome. The presence of fat pads is normal, except lateral gutter, and needs shaving for a better vision. With the distraction, and in patients with generalised laxity chronic lateral ligament instability, central and posterior compartments can be accessed [16] (Fig. 3).
Fig. 3.
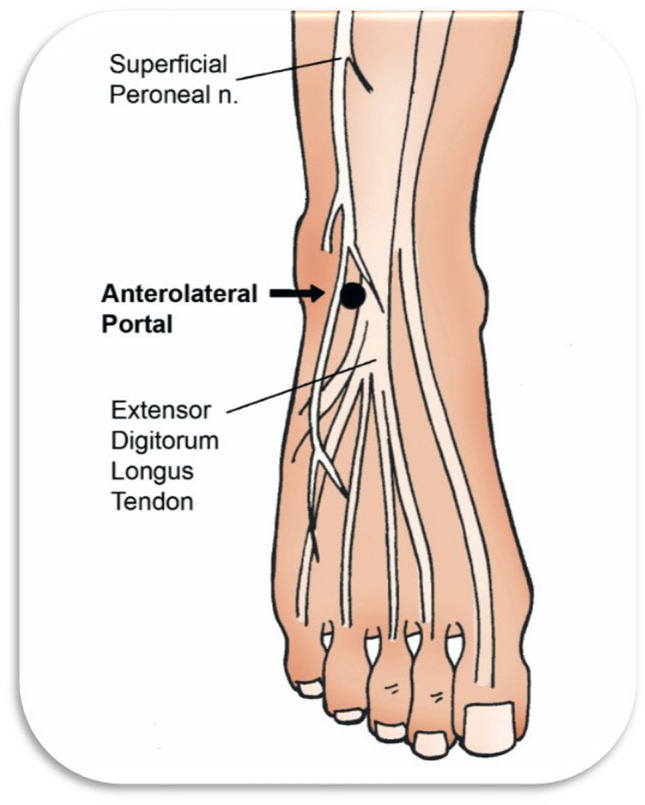
Anterolateral portal
Osteochondral Lesions of Talus
Osteochondral lesion of the ankle is called by many names, osteochondritis dessicans, transchondral talus fracture, and osteochondral (OCL) fracture of the talus. Osteochondral lesion affects cartilage and subchondral bone. Most of the cases will have a history of trauma as the primary cause, although some studies pointed at genetic, vascular, and metabolic causes also. Imaging studies are the mainstay of diagnosis [17]. Based on anatomical grid scheme, central medial, zone 4, or centromedial (53%) is the common location, followed by central lateral, zone 6 (25%) [18]. Treatment is based on the size of the lesion, activity level, symptoms, and age. Restoring the subchondral bone for cartilage regeneration is the aim, which can be achieved by fixing the osteochondral fragment, subchondral bone marrow stimulation, and cartilage transplantation. Stable lesions, irrespective of size and age, are fixed, including large lesions bigger than 15 mm with good bone base, in adolescents [19]. Bone marrow stimulation can be achieved by microfracture, thereby releasing the stem cells and growth factors, which in turn will form fibrocartilage. Arthroscopic drilling is an accepted treatment for lesions smaller than 15 mm. If the cartilage is intact, retrograde drilling assisted by image or navigation is advocated. Osteochondral autograft or allograft transplantation, autologous chondrocyte implantation, and use of juvenile cartilage, have been reported in studies with good outcomes [20–22]. Bone marrow stimulation and tissue transfer procedures like the use of concentrated bone marrow aspirate, platelet-rich plasma, and autologous collagen-induced chondrogenesis as a scaffold can be used to enhance the outcomes [23–25]. In the case of failed surgery, metal implants can be considered for salvage surgery [26].
Ankle Impingement
Ankle impingement is characterized by pain due to friction of pathological bony or soft tissue structures. Anterior joint line pain is the diagnostic feature. Cases with inversion injury may end up with the instability of the lateral ankle joint complex, resulting in scar formation, and synovitis in the lateral gutter, in turn leading to chronic lateral ankle impingement. After failed conservative treatment, arthroscopic debridement of the offending tissues results in good results. If instability is associated with soft tissue impingement, instability is also addressed [27–29]. Bony impingement is caused due to the development of osteophytes secondary to instability and thereby repeated microtrauma. Recurrent trauma, like in sports, causes anterior osteophyte or central osteophyte. In symptomatic cases, chronic pain, and decreased ankle range of motion (mainly dorsiflexion) results. Failed conservative treatment is an indication for arthroscopic osteophyte excision. If ankle instability is associated, it is also treated simultaneously. The rate of recurrent osteophytes after surgical management is high [30–32].
Ankle Instability
Many surgeons routinely carry out a diagnostic arthroscopy to see the ATFL and any associated osteochondral pathology before proceeding with open Brostrom repair. Most OCL heals well, but those that have not healed give rise to chronic pain and progression of the lesion. Complete arthroscopic treatment for ankle instability is evolving. ATFL and CFL are either repaired or reconstructed with hamstring graft with knotless suture anchors and interference screws under arthroscopic view. Many recent studies have shown comparable results with the all-inside arthroscopic repair of ATFL and fewer complications [33–35]. All inside Deltoid ligament reconstruction is also attempted with good results [36].
Arthrodesis
Indications for arthroscopic ankle arthrodesis include post-traumatic, degenerative, and inflammatory arthritis leading to loss of the articular cartilage. Cases with significant defects, gross deformity, presence of active infection, and cases with neurovascular jeopardy are the contraindications. Indications of arthroscopy-assisted ankle arthrodesis can be extended for cases with gross deformity by addition of supra malleolar and calcaneal osteotomies, Achilles lengthening, and ligament balancing [37]. The advantages of the procedure are the preservation of the inherent stability of the ankle, preservation of malleoli, fewer complications, and faster recovery [38]. However, there is a learning curve. The patient positioning, operation room set up, and equipment are the same as those for routine arthroscopy. Some surgeons prefer to use a 2.7-mm arthroscope in place of a 4-mm arthroscope. Ankle distractor is used for tight joints. The large joint shavers, burrs of different sizes and shapes, straight and curved curettes, and osteotomes are required. Operative steps comprise of removal of cartilage with burrs and curettes, preparation of articulating surfaces with drilling, and osteotome fish scaling followed by fixation. Fixation is carried out with two or three cannulated cancellous screws passed under image guidance. Over the years, the procedure has evolved without the use of skeletal distraction leading to a reduced rate of complications [39]. Outcomes are favourable following arthroscopic ankle arthrodesis, with 92% to 97% reported rates of fusion with minimal complications [40, 41].
Complications
Neurovascular injuries are the most reported complications. These neurovascular injuries could be due to errors in portal placement, prolonged distraction, and prolonged tourniquet time. Anterolateral portal and superficial peroneal nerve account for significant complications. Iatrogenic cartilage damage is also common and under-reported. A study showed 31% of injuries with no significant consequences [42]. Complications specific to arthroscopic ankle arthrodesis include nerve injuries, pin tract infection and stress fractures, and non-union. Cases in literature have been reported of tendon and ligament injuries and pseudoaneurysm of the anterior tibial artery. Rare complications are compartment syndrome secondary to extravasation of fluid, wound healing issues with infection, skin necrosis, hemarthrosis, synovial sinus tract formation, deep vein thrombosis, complex regional pain syndrome, and instrument breakage [43].
Posterior Ankle Arthroscopy
In 2000, van Dijk started a 2-portal posterior ankle arthroscopy as a perfect diagnostic and therapeutic tool [44]. Posterior ankle arthroscopy became very popular due to increased awareness among surgeons regarding posterior ankle impingement syndrome (PAIS) and also due to recent advances in hindfoot imaging.
Indications
The most common indication for a posterior ankle arthroscopy is PAIS, which is a common issue with athletes and dancers. PAIS is related to post-traumatic synovitis, scaring of the capsule, intraarticular fibrosis, and bony prominence. Failed conservative treatment is an indication for posterior ankle arthroscopy in PAIS. The posterior ankle scope can adequately manage many clinical conditions such as posterior ankle and subtalar joint osteochondral lesions, enlarged Stieda process, the pathological os trigonum, osteophytes, loose bodies, chondromatosis, subtalar coalition, subtalar and ankle arthritis, soft tissue impingement, FHL tenosynovitis, synovitis, impingement of the joint capsule and impingement of the anomalous muscles, calcaneoplasty for haglund syndrome, and evaluation of fracture reduction [45] (Table 2).
Table 2.
Posterior ankle arthroscopy indications
| Bony and soft tissue impingements (Os trigonum and Stieda process) |
| Osteophyte clearance |
| Osteochondral lesions |
| Calcaneoplasty |
| FHL tenosynovitis |
| Loose body extraction |
| Chondromatosis |
| Subtalar coalitions |
| Ankle and subtalar arthritis |
| Fracture reduction evaluation |
Patient Positioning
The patient is positioned in a prone position or lazy lateral position with operating side down, with a thigh tourniquet. The ankle is brought out of the edge of the operating table so that the ankle can be moved freely. The operated limb is elevated on bolsters. Such positioning gives freedom for the surgeon to handle foot and instruments. No distraction is needed. Surface markings are a horizontal line from the tip of the lateral malleoli to the Achilles tendon, and borders of Achilles tendon. Portal entry points are marked on either side of the Achilles tendon above the transverse line from the fibular tip (Fig. 4).
Fig. 4.

Posterior ankle arthroscopy-patient positioning
Portals
The lateral portal is made first with the sharp knife and then with blunt hemostat down to the bone. The direction of the hemostat is towards the first webspace. Then a 30°, 2.7 mm, or a 4-mm scope is introduced. For creating a medial portal, either a hemostat or a shaver is introduced from medial to the lateral direction, anterior to tendoachilles to hit the scope. Once shaver or a hemostat hits the scope, it is slid over the scope to reach to the end of the scope. It is at this juncture that scope is withdrawn slightly and structures visualized. A lateral portal is used for scope, and a medial portal is used for instruments. FHL tendon plays the most vital role in protecting the neurovascular structures, and intervention medial to FHL tendon should be avoided. Horibe and colleagues described an accessory lateral portal for excision of Os trigonum [44] (Fig. 5).
Fig. 5.

Posterior ankle arthroscopy-surface marking
Technique
Through the medial portal, a shaver is introduced to shave fat behind the talus until the inter malleolar ligament. FHL tendon is identified medial to the capsule and a steida process. Passive motion of the great toe can help in FHL identification. If FHL is covered by soft tissue, a forceps is used to dissect and clear the soft tissue. A shaver or sometimes directly a chisel can be used to remove any bony prominence compressing the FHL. PTIFL, PTFL, and CFL are found lateral to the FHL tendon. For a systematic examination of all anatomical landmarks, a four-quadrant method was described by Yasui et al. [46]. The ankle, and subtalar joints can be accessed anterior to the capsule (Fig. 6).
Fig. 6.

Technique for safe introduction of instruments through medial portal
Posterior Ankle Impingement
Posterior ankle impingement (PAI) can be in the form of soft tissue or a bony impingement. With two portals, space is created in the posterolateral area behind the ankle and subtalar joints, and FHL is identified. Remaining lateral to FHL, debridement of posterior capsules of the ankle and subtalar joints is carried out to address the PAI. Enlarged Stieda process can be shaved with the use of burr or shaver. For cases with symptomatic os trigonum, all soft tissues surrounding the os are removed, os separated from its attachment with the talus, and excised. In cases with stenosing tenosynovitis of FHL, the tenosynovium is debrided. Studies have shown that following posterior ankle impingement clearance procedures, 79% of patients returned to sports in 6 weeks with improved VAS and AOFAS scores [47].
Calcaneoplasty
Calcaneoplasty is a decompressive procedure, done routinely for Haglund syndrome. Haglund syndrome is posterosuperior calcaneal prominence, retrocalcaneal bursitis, insertional tendinopathy of Achilles tendon. Pain is felt medially and laterally near the posterosuperior border of the calcaneus. Dorsiflexion causes pain because of the impingement of the retrocalcaneal bursa between Achilles tendon and posterosuperior prominence of the calcaneus. The condition is initially treated conservatively. Failed conservative treatment is an indication for surgery. Arthroscopic surgery gives superior results in terms of less scar, complications, post-op functional treatment, and early return to work/sport than open calcaneoplasty. Calcaneoplasty is generally done in a prone position, and some even attempted it in supine and lateral position also. Lbib and Pendelton described a different set up for calcaneoplasty in a prone position with a monitor at the foot end and surgeon by the side of the bed. A lateral portal is made first with small vertical skin incision at the superolateral part of calcaneum, and the medial portal is at the same level. Portals are interchangeable for arthroscope and instruments. Some surgeons have attempted Achilles tendon augmentation with suture anchor when Haglund is associated with insertional tendinopathy, with good results. In a cadaver study of biomechanical comparison of arthroscopic versus open calcaneoplasty the resection height was found to be similar, but pull-out strength was much higher in arthroscopic calcaneoplasty than open tendon splitting surgery [48, 49]
Osteochondral Lesion of Talus
A typical location is the middle third of medial or lateral talar dome, rarely can be seen in posterior third. Ninety percent of OCL can be treated by anterior ankle arthroscopy, and some need posterior arthroscopy. Noninvasive distraction in posterior ankle arthroscopy was not needed, and maximum dorsiflexion was sufficient to reach approximately 40% of the talar cartilage for the treatment of OCL through standard portals. If maximal dorsiflexion cannot be achieved because of anterior osteophytes, they must be addressed before posterior arthroscopy. Through the posterior ankle arthroscopy, most of the procedures like curettage and bone marrow stimulation, OATS, large fragment fixation can be carried out smoothly, but sometimes these have to be converted into an open procedure. Kim et al. [50, 51] described a three portal posterior arthroscopic technique for OCL treatment.
Complications
Van Dijk and colleagues reported 86 endoscopic hindfoot procedures done between 1995 and 2000, without complications [44]. Nickisch et al. [52] is a cohort study and not scientific review in 2012 complications of 189 hindfeet arthroscopic procedures carried from 2001 to 2009. The overall complication rate noticed was 8.5%, with common complications being neurologic complications (sural nerve), plantar numbness, complex regional pain syndrome, posterior muscular tightness, and post-op infection. Most of the complications were reversible. Zwiers et al. concluded that based on low complications and early return to activity, posterior ankle arthroscopy is recommended against the open procedure [53].
Future
The future of arthroscopic ankle procedures is bright, with more and more surgeons getting familiar with the technique. Complex procedures like arthroscopy-assisted fixation of fractures and all-inside reconstruction of lateral ligaments have become popular.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this review article formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tol JL, van Dijk CN. Etiology of the anterior ankle impingement syndrome: a descriptive anatomical study. Foot and Ankle International. 2004;25(6):382–386. doi: 10.1177/107110070402500603. [DOI] [PubMed] [Google Scholar]
- 2.Zengerink M, van Dijk CN. Complications in ankle arthroscopy. Knee Surgery, Sports Traumatology, Arthroscopy. 2012;20(8):1420–1431. doi: 10.1007/s00167-012-2063-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dalmau-Pastor M, Malagelada F, Kerkhoffs GM, Karlsson J, Guelfi M, Vega J. Redefining anterior ankle arthroscopic anatomy: medial and lateral ankle collateral ligaments are visible through dorsiflexion and non-distraction anterior ankle arthroscopy. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(1):18–23. doi: 10.1007/s00167-019-05603-2. [DOI] [PubMed] [Google Scholar]
- 4.Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. Journal of Bone and Joint Surgery. 2009;91(2):333–339. doi: 10.2106/JBJS.H.00584. [DOI] [PubMed] [Google Scholar]
- 5.van Bergen CJA, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GMMJ, van Dijk CN. Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. Journal of Bone and Joint Surgery. 2013;95(6):519–525. doi: 10.2106/JBJS.L.00675. [DOI] [PubMed] [Google Scholar]
- 6.Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard J-P. (2009). Evidence-based indications for ankle arthroscopy. Arthroscopy, 25(12), 1478–1490. https://www.arthroscopyjournal.org/article/S0749-8063(09)00418-6/abstract [DOI] [PubMed]
- 7.Bonasia DE, Rossi R, Saltzman CL, Amendola A. The role of arthroscopy in the management of fractures about the ankle. Journal of American Academy of Orthopaedic Surgeons. 2011;19(4):226–235. doi: 10.5435/00124635-201104000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Quayle J, Shafafy R, Khan MA, Ghosh K, Sakellariou A, Gougoulias N. Arthroscopic versus open ankle arthrodesis. Foot and Ankle Surgery. 2018;24(2):137–142. doi: 10.1016/j.fas.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Tonogai I, Hayashi F, Tsuruo Y, Sairyo K. Comparison of ankle joint visualization between the 70° and 30° arthroscopes: a cadaveric study. Foot and Ankle Specialist. 2018;11(1):72–76. doi: 10.1177/1938640017733099. [DOI] [PubMed] [Google Scholar]
- 10.de Leeuw PAJ, Golanó P, Sierevelt IN, van Dijk CN. The course of the superficial peroneal nerve in relation to the ankle position: anatomical study with ankle arthroscopic implications. Knee Surgery, Sports Traumatology, Arthroscopy. 2010;18(5):612–617. doi: 10.1007/s00167-010-1099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mercer D, Morrell NT, Fitzpatrick J, Silva S, Child Z, Miller R, et al. (2020). the course of the distal saphenous nerve: a cadaveric investigation and clinical implications. Iowa Orthopedic Journal, 31, 231–235. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3215141/ [PMC free article] [PubMed]
- 12.Prakash R, Bhardwaj AK, Singh DK, Rajini T, Jayanthi V, Singh G. Anatomic variations of superficial peroneal nerve: clinical implications of a cadaver study. Italian Journal of Anatomy and Embryology. 2010;115(3):223–228. [PubMed] [Google Scholar]
- 13.Needleman RL. Use of cannulated instruments to localize the portals in anterior ankle arthroscopy: a technique tip. Journal of Foot and Ankle Surgery. 2016;55(3):659–663. doi: 10.1053/j.jfas.2016.01.049. [DOI] [PubMed] [Google Scholar]
- 14.Ferkel, R.D. (1996). Diagnostic arthroscopic anatomy. In: T. L. Whipple (Ed.) Arthroscopic surgery. The foot and ankle. Philadelphia: Lippincot
- 15.Vega J, Malagelada F, Karlsson J, Kerkhoffs GM, Guelfi M, Dalmau-Pastor M. A step-by-step arthroscopic examination of the anterior ankle compartment. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(1):24–33. doi: 10.1007/s00167-019-05756-0. [DOI] [PubMed] [Google Scholar]
- 16.Phisitkul P, Akoh CC, Rungprai C, Barg A, Amendola A, Dibbern K, et al. Optimizing arthroscopy for osteochondral lesions of the talus: the effect of ankle positions and distraction during anterior and posterior arthroscopy in a cadaveric model. Arthroscopy. 2017;33(12):2238–2245. doi: 10.1016/j.arthro.2017.06.027. [DOI] [PubMed] [Google Scholar]
- 17.Potter HG, Chong LR, Sneag DB. Magnetic resonance imaging of cartilage repair. Sports Medicine and Arthroscopy Review. 2008;16(4):236–245. doi: 10.1097/JSA.0b013e31818cdcaf. [DOI] [PubMed] [Google Scholar]
- 18.Elias I, Raikin SM, Schweitzer ME, Besser MP, Morrison WB, Zoga AC. Osteochondral lesions of the distal tibial plafond: localization and morphologic characteristics with an anatomical grid. Foot and Ankle International. 2009;30(6):524–529. doi: 10.3113/FAI.2009.0524. [DOI] [PubMed] [Google Scholar]
- 19.Larsen MW, Pietrzak WS, DeLee JC. Fixation of osteochondritisdissecans lesions using poly(l-lactic acid)/poly(glycolic acid) copolymer bioabsorbable screws. American Journal of Sports Medicine. 2005;33(1):68–76. doi: 10.1177/0363546504265927. [DOI] [PubMed] [Google Scholar]
- 20.Ahmad J, Jones K. Comparison of osteochondralautografts and allografts for treatment of recurrent or large talarosteochondral lesions. Foot and Ankle International. 2016;37(1):40–50. doi: 10.1177/1071100715603191. [DOI] [PubMed] [Google Scholar]
- 21.Giannini S, Buda R, Ruffilli A, Cavallo M, Pagliazzi G, Bulzamini MC, et al. Arthroscopic autologous chondrocyte implantation in the ankle joint. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(6):1311–1319. doi: 10.1007/s00167-013-2640-7. [DOI] [PubMed] [Google Scholar]
- 22.Giza E, Delman C, Coetzee JC, Schon LC. Arthroscopic treatment of talus osteochondral lesions with particulated juvenile allograft cartilage. Foot and Ankle International. 2014;35(10):1087–1094. doi: 10.1177/1071100714548704. [DOI] [PubMed] [Google Scholar]
- 23.Wylie JD, Hartley MK, Kapron AL, Aoki SK, Maak TG. What is the effect of matrices on cartilage repair? A systematic review. Clinical Orthopaedics and Related Research. 2015;473(5):1673–1682. doi: 10.1007/s11999-015-4141-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zengerink M, Szerb I, Hangody L, Dopirak RM, Ferkel RD, van Dijk CN. Current concepts: treatment of osteochondral ankle defects. Foot and Ankle Clinics. 2006;11(2):331–359. doi: 10.1016/j.fcl.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 25.Savage-Elliott I, Ross KA, Smyth NA, Murawski CD, Kennedy JG. Osteochondral lesions of the talus: a current concepts review and evidence-based treatment paradigm. Foot and Ankle Specialist. 2014;7(5):414–422. doi: 10.1177/1938640014543362. [DOI] [PubMed] [Google Scholar]
- 26.van Bergen CJA, van Eekeren ICM, Reilingh ML, Sierevelt IN, van Dijk CN. Treatment of osteochondral defects of the talus with a metal resurfacing inlay implant after failed previous surgery: a prospective study. Bone Joint Journal. 2013;95(12):1650–2165. doi: 10.1302/0301-620X.95B12.32455. [DOI] [PubMed] [Google Scholar]
- 27.Mardani-Kivi M, Mirbolook A, Khajeh-Jahromi S, Hassanzadeh R, Hashemi-Motlagh K, Saheb-Ekhtiari K. Arthroscopic treatment of patients with anterolateral impingement of the ankle with and without chondral lesions. Journal of Foot and Ankle Surgery. 2013;52(2):188–191. doi: 10.1053/j.jfas.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 28.Vega J, Dalmau-Pastor M, Malagelada F, Fargues-Polo B, Peña F. Ankle arthroscopy: an update. The Journal of Bone and Joint Surgery. 2017;99:1395–1407. doi: 10.2106/JBJS.16.00046. [DOI] [PubMed] [Google Scholar]
- 29.Urgüden M, Söyüncü Y, Ozdemir H, Sekban H, Akyildiz FF, Aydin AT. Arthroscopic treatment of anterolateral soft tissue impingement of the ankle: evaluation of factors affecting outcome. Arthroscopy. 2005;21(3):317–322. doi: 10.1016/j.arthro.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 30.Parma A, Buda R, Vannini F, Ruffilli A, Cavallo M, Ferruzzi A, et al. Arthroscopic treatment of ankle anterior bony impingement: the long-term clinical outcome. Foot and Ankle International. 2014;35(2):148–155. doi: 10.1177/1071100713510912. [DOI] [PubMed] [Google Scholar]
- 31.Zwiers R, Wiegerinck JI, Murawski CD, Fraser EJ, Kennedy JG, van Dijk CN. Arthroscopic treatment for anterior ankle impingement: a systematic review of the current literature. Arthroscopy. 2015;31(8):1585–1596. doi: 10.1016/j.arthro.2015.01.023. [DOI] [PubMed] [Google Scholar]
- 32.Walsh SJ, Twaddle BC, Rosenfeldt MP, Boyle MJ. Arthroscopic treatment of anterior ankle impingement: a prospective study of 46 patients with 5-year follow-up. American Journal of Sports Medicine. 2014;42(11):2722–2726. doi: 10.1177/0363546514550976. [DOI] [PubMed] [Google Scholar]
- 33.Feng S-M, Wang A-G, Sun Q-Q, Zhang Z-Y. Functional Results of All-Inside Arthroscopic Broström-Gould Surgery With 2 Anchors Versus Single Anchor. Foot and Ankle International. 2020 doi: 10.1177/1071100720908858. [DOI] [PubMed] [Google Scholar]
- 34.Lan S, Zeng W, Yuan G, Xu F, Cai X, Tang M, et al. All-inside arthroscopic anterior talofibular ligament anatomic reconstruction with a gracilis tendon autograft for chronic ankle instability in high-demand patients. Journal of Foot and Ankle Surgery. 2020;59(2):222–230. doi: 10.1053/j.jfas.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 35.Vega J, Golanó P, Pellegrino A, Rabat E, Peña F. All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot and Ankle International. 2013;34(12):1701–1709. doi: 10.1177/1071100713502322. [DOI] [PubMed] [Google Scholar]
- 36.Higashiyama R, Sekiguchi H, Takata K, Endo T, Takamori Y, Takaso M. Arthroscopic reconstruction of the anterior tibiotalar ligament using a free tendon graft. Arthroscopy Techniques. 2020;9(4):e541–e547. doi: 10.1016/j.eats.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dent C, Patil M, Fairclough J. Arthroscopic ankle arthrodesis. The Journal of Bone and Joint Surgery. 1993;75(B5):830–832. doi: 10.1302/0301-620X.75B5.8376451. [DOI] [PubMed] [Google Scholar]
- 38.Ferkel RD, Hewitt M. Long-term results of arthroscopic ankle arthrodesis. Foot and Ankle International. 2005;26(4):275–280. doi: 10.1177/107110070502600402. [DOI] [PubMed] [Google Scholar]
- 39.Crosby LA, Yee TC, Formanek TS, Fitzgibbons TC. Complications following arthroscopic ankle arthrodesis. Foot and Ankle International. 1996;17(6):340–342. doi: 10.1177/107110079601700608. [DOI] [PubMed] [Google Scholar]
- 40.Vivek Panikkar K, Taylor A, Kamath S, Henry APJ. (2003).A comparison of open and arthroscopic ankle fusion. Foot and Ankle Surgery 9(3), 169–72. http://www.sciencedirect.com/science/article/pii/S1268773103000730
- 41.Myerson MS, Quill G. Ankle arthrodesis. A comparison of an arthroscopic and an open method of treatment. ClinOrthopaedRelat Res. 1991;268:84–95. [PubMed] [Google Scholar]
- 42.Vega J, Golan׳o P, Peña F. Iatrogenic articular cartilage injuries during ankle arthroscopy. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(4):1304–1310. doi: 10.1007/s00167-014-3237-5. [DOI] [PubMed] [Google Scholar]
- 43.Young BH, Flanigan RM, DiGiovanni BF. Complications of ankle arthroscopy utilizing a contemporary noninvasive distraction technique. Journal of Bone and Joint Surgery. 2011;93(10):963–968. doi: 10.2106/JBJS.I.00977. [DOI] [PubMed] [Google Scholar]
- 44.van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16(8):871–876. doi: 10.1053/jars.2000.19430. [DOI] [PubMed] [Google Scholar]
- 45.Hayashi D, Roemer FW, D’Hooghe P, Guermazi A. Posterior ankle impingement in athletes: pathogenesis, imaging features and differential diagnoses. European Journal of Radiology. 2015;84(11):2231–2241. doi: 10.1016/j.ejrad.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 46.Yasui, Y., Hannon, C.P., Hurley, E., Kennedy, J.G. (2016). Posterior ankle impingement syndrome: a systematic four-stage approach. World Journal of Orthopedics7(10), 657–663. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5065672/ [DOI] [PMC free article] [PubMed]
- 47.Ribbans WJ, Ribbans HA, Cruickshank JA, Wood EV. The management of posterior ankle impingement syndrome in sport: a review. Foot and Ankle Surgery. 2015;21(1):1–10. doi: 10.1016/j.fas.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 48.Labib SA, Pendleton AM. Endoscopic calcaneoplasty: an improved technique. Journal of Surgical Orthopaedic Advances. 2012;21(3):176–180. doi: 10.3113/jsoa.2012.0176. [DOI] [PubMed] [Google Scholar]
- 49.Vega J, Baduell A, Malagelada F, Allmendinger J, Dalmau-Pastor M. Endoscopic achilles tendon augmentation with suture anchors after calcaneal exostectomy in Haglund syndrome. Foot and Ankle International. 2018;39(5):551–559. doi: 10.1177/1071100717750888. [DOI] [PubMed] [Google Scholar]
- 50.Hirtler L, Schellander K, Schuh R. Accessibility to talar dome in neutral position, dorsiflexion, or noninvasive distraction in posterior ankle arthroscopy. Foot and Ankle International. 2019;40(8):978–986. doi: 10.1177/1071100719847134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim HN, Kim GL, Park JY, Woo KJ, Park YW. Fixation of a posteromedial osteochondral lesion of the talus using a three-portal posterior arthroscopic technique. Journal of Foot and Ankle Surgery. 2013;52(3):402–405. doi: 10.1053/j.jfas.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 52.Nickisch F, Barg A, Saltzman CL, Beals TC, Bonasia DE, Phisitkul P, et al. Postoperative complications of posterior ankle and hindfoot arthroscopy. Journal of Bone and Joint Surgery. 2012;94(5):439–446. doi: 10.2106/JBJS.K.00069. [DOI] [PubMed] [Google Scholar]
- 53.Zwiers R, Wiegerinck JI, Murawski CD, Smyth NA, Kennedy JG, van Dijk CN. Surgical treatment for posterior ankle impingement. Arthroscopy. 2013;29(7):1263–1270. doi: 10.1016/j.arthro.2013.01.029. [DOI] [PubMed] [Google Scholar]


