Abstract
Purpose
Intra-articular malunion of tibial plateau fracture is a complex problem to treat. We are presenting outcomes of our series of patients of malunited tibial plateau fractures treated with osteo-chondro-meniscal allograft from lateral tibial plateau harvested from patients undergoing total knee arthroplasty (TKA).
Methods
The technique was used in four patients. Preoperative computed tomography (CT) scan was used to match donor and recipient graft dimensions and to measure any malalignment. Patients were evaluated for Visual analogue Scale (VAS) for pain (scale 1–10 cm), WOMAC (Western Ontario McMaster Osteo-Arthritis Index) score, knee range of motion, and limb alignment.
Results
There were three medial tibial plateau malunions and one lateral tibial plateau malunion. Articular comminution with depression was seen in all of them. One patient underwent concurrent high tibial osteotomy for the elevation of the medial tibial plateau and posterior cruciate ligament reconstruction was performed concurrently in one patient. All patients showed improvement in knee range of motion, WOMAC score, and VAS score for knee pain. Limb alignment improved in all cases. Radiologically there was consolidation of the allograft in all the cases at 6 months. The mean follow-up was 15.2 months (range 12–18 months).
Conclusion
Osteochondral allograft can be a good choice for reconstructing large articular cartilage defects in tibial plateau malunions. Osteo-chondro-meniscal grafts obtained during TKA can be a viable alternative for reconstructing such defects with excellent early clinical, functional, and radiological outcomes.
Level of Evidence
IV.
Keywords: Osteochondral defect, Tibia plateau, Meniscus, Allograft, Bone graft, Malunions
Introduction
Intra-articular malunion of tibial plateau fractures is a complex problem to treat. This is frequently seen in younger patients in whom arthroplasty may not be an appropriate option for treatment. Several techniques, such as extra-articular or intra-articular osteotomies, have been described in the literature for the treatment of malunited tibial plateau fractures [1–8]. However, when the articular surface is involved and cartilage is damaged these osteotomies cannot restore the joint surface. Depression of the joint surface is commonly seen, particularly in the lateral tibial plateau fractures. When they present late, elevation of the articular surface to restore the joint is generally not possible. Joint depression may also lead to limb deformity in varus or valgus and instability on weight-bearing.
Osteochondral allografts have been used for large size cartilage defects [9–12]. Osteochondral allograft of tibial hemi-plateau can be used to replace the damaged articular surface on tibia. These allograft hemi-plateaus also have meniscus attached to them [9]. There are only a few reports of their use in the literature [9, 11, 12]. They are harvested from cadaveric donors, thus limiting their availability. We have used allografts harvested from the proximal tibial cut of total knee arthroplasty (TKA). This has not been described in literature before.
We are presenting outcomes of our series of patients of malunited tibial plateau fractures, treated with osteo-chondro-meniscal allograft obtained from lateral tibial plateau harvested from patients undergoing TKA.
Materials and Methods
This technique was used in four patients after obtaining informed consent. Preoperatively all of the patients were assessed clinically for any laxity or stiffness in the knee. Plain radiographs and computed tomography (CT) scans were performed to assess the deformity and articular cartilage defect. Sizing for allograft transplantation was carried out by comparing the dimensions of the tibial plateau of the recipient on CT scans with the intra-operative dimensions of the tibial plateau of the donor.
We used the tibial plateau osteochondral allograft harvested from the surgical residues during TKA after obtaining informed consents from donors. Routine screening and testing were done for all donors according to the standard bone bank protocols [13]. Fresh osteochondral allograft was saved from the bone obtained from the proximal tibial cut during TKA, under aseptic precautions. Only the allografts with no macroscopic damage to meniscus or articular cartilage were saved. It was thoroughly washed with normal saline solution using pulse lavage, to remove any marrow and fat debris. Then it was dipped in an antibiotic solution containing amoxicillin and gentamicin and stored at 4–8 °C in Ringer lactate solution under strict sterile conditions (Class A) at the institutional bone bank. The graft was not stored in the deep freezer as chondrocyte viability is better when the graft is stored between 4–8 °C [14]. Surgery was planned and the graft was used within 5 days of storage. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Written informed consent was obtained from all patients.
Surgical Technique
Medial para-patellar approach was used for medial side of the knee and conversely, lateral para-patellar approach was used to expose lateral tibial plateau. A limited incision was made from the inferior pole of the patella to tibial tuberosity, at the edge of the patellar tendon. Retinacular incision was made and partial excision of the fat pad was carried out to expose the joint. The medial or the lateral compartment of the knee joint was exposed.
Depth of the bone cut from the proximal tibia was calculated from pre-operative CT scans. The amount of elevation of the articular surface required to restore the neutral mechanical axis of the lower limb was also calculated. The measured thickness of the articular surface of the joint was removed with the help of sagittal and reciprocating saws. Reciprocating saw was used to make a vertical cut at the edge of the medial or lateral tibial spine, respectively, and a sagittal saw was used to make a horizontal cut at the required depth at the base of the lesion. This is quite similar to the technique used to make the tibial cut in a unicondylar knee arthroplasty. A paper template was used to size the surface of the tibial plateau after the cut was made. This template was laid over the allograft to obtain a good match between the tibial cut and the allograft. The deeper bone defects left at the base of the tibial cut were filled with cortico-cancellous allograft bone. The appropriately sized tibial hemi-plateau allograft along with the meniscus was placed over the tibial cut and secured in place with the help of titanium headless screws. One or two screws were placed in the area of tibial eminence (one anterior to the ACL insertion and the second posterior to it). Two to three screws were placed along the outer border of the graft.
Six non-absorbable sutures were passed at the periphery of the meniscus before it was placed inside the joint. They were subsequently used to secure the meniscus to the articular capsule. The meniscus was already fixed to the tibial plateau at the insertions of its anterior and posterior roots and needed only peripheral fixation to the capsule. Ethibond No. 2 or fiber wire No. 2 sutures were used for the fixation of the meniscus. The sutures were placed at an average distance of 1 cm from one another on the periphery of the meniscus. The sutures were retrieved outside the knee joint using tissue penetrators and suture graspers from shoulder arthroscopy instrumentation. They were tied outside the capsule using a small 2 cm incision on the medial or the lateral side, respectively.
Contralateral lateral tibial plateau allograft was used for the medial tibial plateau defects. It is not possible to retrieve a healthy medial tibial hemi-plateau from the tibial cut of an osteoarthritis knee as the osteoarthritis process generally affects the medial side of the knee joint.
Usual closure of the retinaculum, subcutaneous tissue, and skin was carried out. The duration of surgery ranged from 90 to 120 min. The antibiotics protocol was same for all patients consisting of one dose of Cefuroxime iv preoperatively and 3 doses postoperatively. Post-operatively the limb was placed in a long leg cast for 3 weeks after which knee range of motion was started using a hinged knee brace. Non-weight-bearing mobilization was used for 6 weeks after which partial weight-bearing was started. Full weight-bearing was started at 12 weeks. Patients were evaluated for Visual analogue Scale (VAS) for pain (scale 1–10 cm), WOMAC (Western Ontario McMaster Osteo-Arthritis Index) score, knee range of motion. Plain radiographs were obtained at follow-up for assessing graft incorporation. Limb alignment was assessed clinically as well as with the help of radiographs. The minimum follow-up duration was 1 year. Pre-operative, intra-operative, and post-operative images of patients 1,2,3 and 4 are summarized in Figs. 1, 2, 3, and 4, respectively.
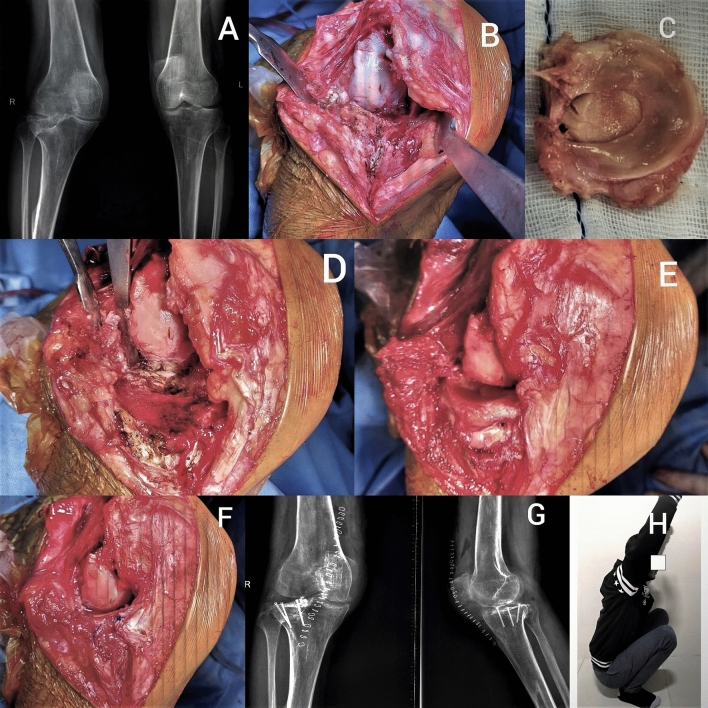
Fig. 1.
Figure showing: a Preoperative radiograph, b Large defect in lateral tibial plateau, c Lateral plateau osteo-chondro-meniscal allograft, d Tibial plateau preparation, e Fixation of allograft, f Fixation of meniscus with peripheral sutures and soft tissue closure, g Postoperative radiograph, h Postoperative clinical picture showing full range of knee motion
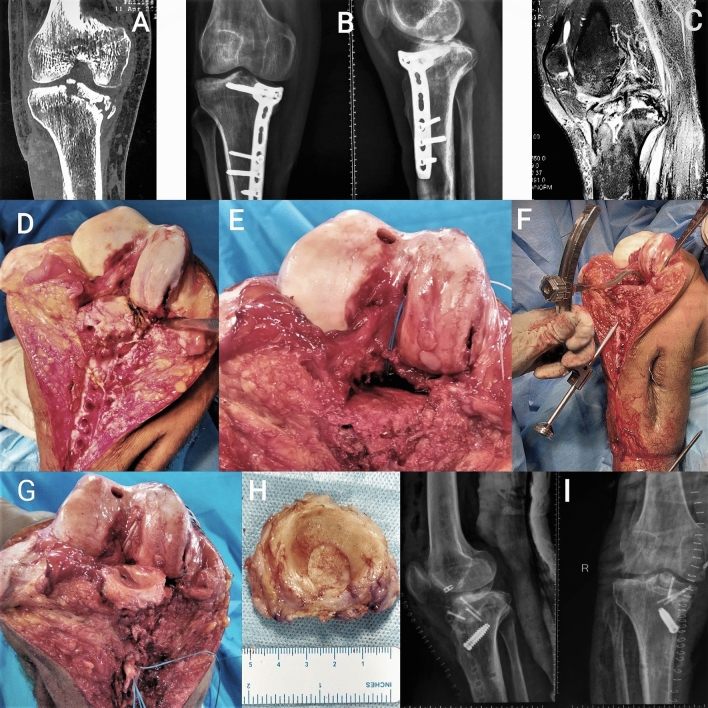
Fig. 2.
Figure showing: a Preoperative Computed tomography scan showing depressed comminuted medial tibial plateau fracture. b Preoperative radiograph. c Preoperative magnetic resonance imaging showing posterior cruciate ligament (PCL) tear with comminuted tibial plateau fracture with reversed slope. d Malunited medial tibial plateau without any cartilage or meniscus, cartilage loss over weight bearing part of medial femoral condyle with PCL tear. e Tibial plateau and PCL tunnel preparation with osteochondral autologous transfer for femoral cartilage defect, f Preparation of tibial tunnel for PCL. g Fixation of allograft and reconstructed PCL. h Osteo-chondro-meniscal allograft. i Postoperative radiograph
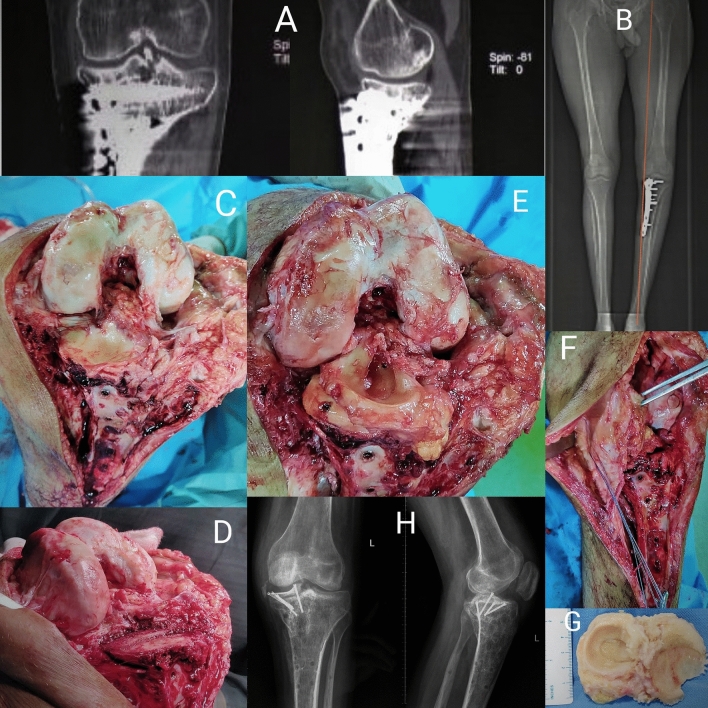
Fig. 3.
Figure showing: a Preoperative computed tomography Showing decreased joint space with implant in situ b Preoperative computed tomography scanogram showing varus deformity in knee. c Malunited medial tibial plateau without any cartilage or meniscus. d Tibial plateau preparation. e Final reconstruction with fixation of osteo-chondro- meniscal allograft. f Quadriceps V–Y plasty being performed. g Osteo-chondro- meniscal allograft. h Postoperative radiograph showing restored level of tibial plateau with optimum alignment
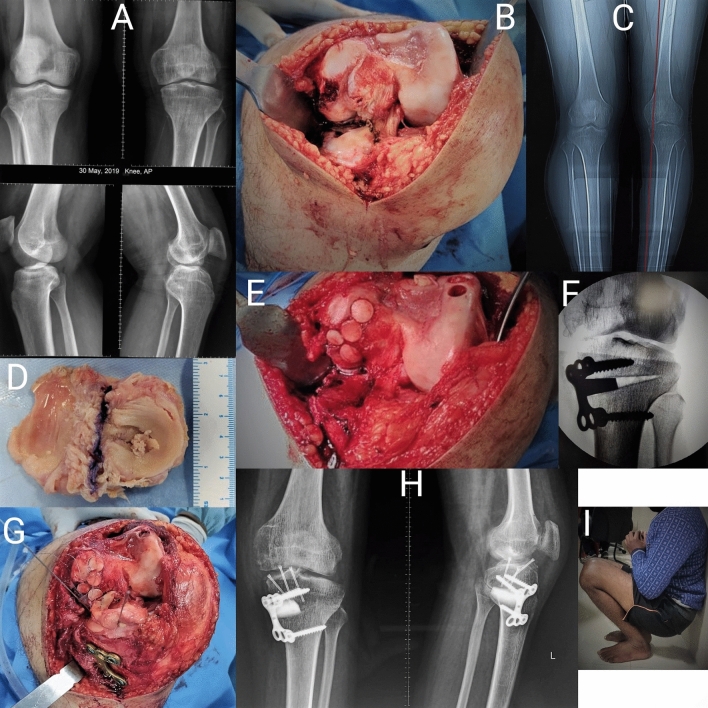
Fig. 4.
Figure showing: a Preoperative radiograph. b Kissing cartilage lesion in medial tibial plateau and femoral condyle without any meniscus. c Preoperative computed tomography scanogram showing varus deformity in the knee. d Osteo-chondro- meniscal allograft. e Tibial plateau preparation with osteochondral autologous transfer for femoral cartilage defect, f Intraoperative C-arm image of final correction after high tibial osteotomy (HTO), g Fixation of allograft with provisional K-wires after fixation of HTO with plate, (H)Postoperative clinical picture showing the full range of knee motion, i Postoperative clinical picture showing full range of knee motion
Results
Characteristics of the patients in terms of age, sex, BMI, mechanism, duration of injury, symptoms, are presented in Table 1.
Table 1.
Table showing the distribution of patient parameters
| Variables | Patient 1 | Patient 2 | Patient 3 | Patient 4 |
|---|---|---|---|---|
| Age in years | 32 | 25 | 21 | 27 |
| Side | Right | Right | Left | Left |
| Sex | Male | Male | Male | Male |
| BMI | 23.8 | 22.4 | 19.1 | 27.3 |
| Mechanism of injury | RTA | Fall from height | RTA | RTA |
| Duration since injury (months) | 54 | 36 | 10 | 120 |
| Symptoms | ||||
| Pain while walking | Present | Present | Present | Present |
| Pain at rest | Present | – | Present | – |
| Instability | – | Present | – | Present |
| Limp | Present | Present | Present | Present |
| Ambulatory status | Community ambulator | Fully mobile | Not able to walk | Fully mobile |
| Post-operative symptoms | – | – | Pain while walking | – |
| Duration of follow-up (months) | 14 | 17 | 12 | 18 |
| Treatment history | Conservative | ORIF with medial plate | ORIF with medial plate | Conservative |
| Associated ligament injury | – | PCL | – | – |
| Thickness of osteochondral allograft (mm) | 8.6 | 9.3 | 9.7 | 9.4 |
PCL posterior cruciate ligament, ORIF open reduction and internal fixation, RTA road traffic accident, BMI body mass index
There were three medial tibial plateau malunions (Patient 2, 3 and 4) and one lateral tibial plateau malunion (patient 1). Articular comminution with depression was seen in all of the patients. One patient had associated posterior cruciate ligament injury (Patient 2). Open reduction with fixation with a medial locking plate had been done in two patients immediately after injury (Patient 2, 3). While rest of the two patients were managed conservatively with plaster of Paris slab or casts (Patient 1, 4). Pain while walking was the most important symptom.
Thickness of grafts are noted in Table 1. High tibial osteotomy for elevation of the medial tibial plateau was performed concurrently in one patient. Simultaneous posterior cruciate ligament reconstruction was done in one patient and osteo-chondral autograft transfer from contralateral knee for cartilage defect on femoral condyle (kissing lesion) was done in two patients. All patients showed improvement in knee range of motion, WOMAC score, and VAS score for knee pain. Limb alignment improved in all cases (Table 2). Radiologically there was consolidation of the allograft in all the cases within 6 months. The mean follow-up was 15.2 months (Range 12–18 months). Three patients had fixed flexion deformity pre-operatively, 30 degrees in one patient, and 10 degrees in the other two patients. None of the patients had any fixed deformities post-operatively. One patient (Patient 3) developed knee stiffness post-operatively, which improved after manipulation under anaesthesia.
Table 2.
Table showing clinical and functional outcome parameters
| Variables | Patient 1 | Patient 2 | Patient 3 | Patient 4 |
|---|---|---|---|---|
| Pre-operative range of motion | 30–90 | 0–100 | 10–30 | 10–90 |
| Post-operative range of motion | 0–110 | 0–130 | 0–90 | 0–110 |
| Pre-operative VAS | 7 | 6 | 8 | 6 |
| Post-operative VAS | 2 | 1 | 6 | 3 |
| Pre-operative WOMAC | 22.2 | 44.8 | 16.0 | 32.6 |
| Post-operative WOMAC | 76.0 | 78.8 | 41.2 | 68.0 |
| Pre-operative limb alignment | Neutral | 4-degrees varus | 11-degrees varus | 16-degrees varus |
| Post-operative limb alignment | 10-degree valgus | Neutral | Neutral | 5-degree valgus |
| Associated procedures | – | PCL reconstruction with contralateral semitendinosus graft and OATS | OATS and quadriceps V–Y plasty | HTO and OATS |
PCL posterior cruciate ligament, OATS osteochondral autologous transfer system, HTO high tibial osteotomy
Discussion
Osteoarthritis of the knee joint frequently affects the medial compartment of the knee while sparing the lateral compartment. This medial osteoarthritis in majority of the knee joints damages cartilage and meniscus of the medial tibial plateau. Lateral tibial plateau and lateral meniscus are frequently spared in this process. When proximal tibial cut is made during TKA, 8–10 mm thick slice of the lateral tibial plateau along with the lateral meniscus is removed. If grossly there no articular cartilage lesions and the lateral meniscus appears to be normal, this can be stored and used as a tibial plateau allograft.
Lateral tibial plateau fractures are more common than medial tibial plateau fractures [15, 16]. Depressed fractures are more common than pure split fractures [16]. Malunion patterns in which there is no articular comminution can be addressed with intra-articular or extra-articular osteotomies. In the setting of comminution and depression of articular cartilage, treatment options become more limited and strategies to restore the articular cartilage are needed. Defects arising from split depressed tibial plateau fractures are generally partially contained defects. No attempt is made to reach the base of the defect during the horizontal tibial cut. Only a limited amount of bone and remaining cartilage is removed to obtain a healthy bed for fixation of the graft. This is done to minimize the thickness of the tibial allograft needed, to increase the chances of graft uptake with minimal bone resorption [17]. Deeper contained defects can be managed with impaction bone grafting with cortico-cancellous allograft, to prepare a bony bed over which the osteochondral allograft can be placed. Remaining cruciate ligament attachments should be protected during the vertical bone cut and the collateral ligaments of the respective side should be protected during the horizontal bone cut. Partial elevation of the iliotibial band can be carried out on the lateral side to improve exposure and graft fixation. The tibial plateau fractures are often associated with meniscal injuries [18]. Intra-articular malunions of these fractures will often have degenerated meniscus. Sometimes the meniscus can be incarcerated within the bony fragments. Three out of four patients had either complex meniscal tears or a completely degenerated meniscus at the time of surgery. Thus, these tibial plateau osteo-chondro-meniscal allografts are appropriate to restore both the cartilage and the meniscus. Preservation of the meniscus along with the osteochondral allograft has better outcomes as compared to only osteochondral allograft transfer [9]. Shasha et al. [9] have shown a significant decrease in time of conversion to TKA after using osteo-chondro-meniscal allografts (10.6 years) compared to osteochondral grafts (7.1 years).
Results of a tibial osteochondral allograft have been promising in the literature [19]. Abolghasemian et al. [11] presented long-term outcomes of post-traumatic tibial plateau defects treated with fresh osteochondral allograft transplantation. Survivorship of the graft, defined as the need for total knee arthroplasty was 90% at 5 years, 79% at 10 years, 64% at 15 years, and 47% at 20 years. These grafts were sourced from fresh cadaveric allograft donations. When compared to the femoral osteochondral allografts, tibial defects would need grafting of the entire tibial hemi-plateau. Krettek et al. [10] described a case of a large tibial plateau defect secondary to a non-union of the tibial plateau. It was managed using a large osteochondral allograft from a cadaveric proximal tibia. They added postero-lateral approach to improve the exposure of the tibial plateau. The maximum thickness of the graft was 8 mm. There was functional and radiological improvement at follow-up. The mean thickness of the grafts obtained from TKA cuts was 8.7 mm, which was quite similar to the previous studies, and was optimum for osteo-integration [17]. Gelber et al. [12] indicated that this is a good technique for tibial defects measuring more than 30 mm in diameter and 10 mm in depth. Krettek et al. [10] had shown radiological signs of osseous integration of osteochondral allograft within 3 months. We have seen incorporation of graft in all our cases within 6 months.
Osteo-chondral allograft also has the advantage of correcting the limb deformity, because the depressed articular surface is replaced by a full-thickness allograft. This can also correct the symptoms of instability caused by large intra-articular deformities. In patients with severe depression of the joint surface, osteotomy to elevate the hemi-plateau can be carried out along with the osteochondral allograft transplantation. This was performed in one patient with successful outcomes in this study. Three patients complained of instability while walking pre-operatively, and none of them had instability post-operatively.
This study has limitations of small sample size and lack of a long-term follow-up. There is a morphological difference between medial and lateral tibial plateau. We have described the use of lateral side allograft for medial tibial defects, in view of issues related to availability. Longer follow-up of these patients is warranted to assess the survival of the osteochondral allograft obtained from relatively older patients (Mean age 51.5 ± 4.1 years).
To the best of our knowledge, this is the first study reporting this method of using osteo-chondro-meniscal allografts from TKA. These allografts can be easily available. This procedure has shown excellent early outcomes and graft incorporation without any notable complications.
Conclusion
Osteochondral allograft is a good choice for large articular cartilage defects in tibial plateau malunions. Osteo-chondro-meniscal grafts obtained during TKA can be a viable alternative for reconstructing such defects with good early clinical, functional, and radiological outcomes.
Funding
There was no funding source.
Compliance with Ethical Standards
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical standard statement
Institutional review board approved for the study (AIIMS/IEC/18/281).
Informed consent
Written informed consents were obtained from all patients.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tarun Goyal, Email: goyal.tarun@gmail.com.
Souvik Paul, Email: 1990.souvik@gmail.com.
Arghya Kundu Choudhury, Email: arghyakunduchoudhury@gmail.com.
V. Abdusamad, Email: abdusamaddr@gmail.com
References
- 1.Pagkalos J, Molloy R, Snow M. Bi-planar intra-articular deformity following malunion of a Schatzker V tibial plateau fracture: correction with intra-articular osteotomy using patient-specific guides and arthroscopic resection of the tibial spine bone block. The Knee. 2018;25(5):959–965. doi: 10.1016/j.knee.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 2.Prasad G, Zahn H. Medial tibial hemi-condylar elevation osteotomy as an operative technique to treat varus mal-united tibial plateau fracture. Musculoskeletal Surgery. 2012;96(1):63–66. doi: 10.1007/s12306-011-0152-5. [DOI] [PubMed] [Google Scholar]
- 3.Singh H, Singh VR, Yuvarajan P, Maini L, Gautam VK. Open wedge osteotomy of the proximal medial tibia for malunitedtibial plateau fractures. Journal of Orthopaedic Surgery. 2011;19(1):57–59. doi: 10.1177/230949901101900113. [DOI] [PubMed] [Google Scholar]
- 4.Sundararajan SR, Nagaraja HS, Rajasekaran S. Medial open wedge high tibial osteotomy for varus malunited tibial plateau fractures. Arthroscopy: The Journal of Arthroscopic and Related Surgery. 2017;33(3):586–594. doi: 10.1016/j.arthro.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Luo C, Hu C, Sun H, Zhan Y. An innovative intra-articular osteotomy in the treatment of posterolateral tibial plateau fracture malunion. The Journal of Knee Surgery. 2017;30(4):329–335. doi: 10.1055/s-0036-1584922. [DOI] [PubMed] [Google Scholar]
- 6.Wang H, Newman S, Wang J, Wang Q, Wang Q. Corrective osteotomies for complex intra-articular tibial plateau malunions using three-dimensional virtual planning and novel patient-specific guides. The Journal of Knee Surgery. 2018;31(7):642–648. doi: 10.1055/s-0037-1605563. [DOI] [PubMed] [Google Scholar]
- 7.Kerkhoffs GMMJ, Rademakers MV, Altena M, Marti RK. Combined intra-articular and varus opening wedge osteotomy for lateral depression and valgus malunion of the proximal part of the tibia:surgical technique. The Journal of Bone and Joint Surgery Series A. 2009;91(SUPPL. 2):101–115. doi: 10.2106/JBJS.H.01500. [DOI] [PubMed] [Google Scholar]
- 8.Mastrokalos DS, Panagopoulos GN, Koulalis D, Soultanis KC, Kontogeorgakos VA, Papagelopoulos PJ. Reconstruction of a neglected tibial plateau fracture malunion with an open-book osteotomy: a case report. JBJS Case Connecter. 2017;7(1):e21. doi: 10.2106/JBJS.CC.16.00041. [DOI] [PubMed] [Google Scholar]
- 9.Shasha N, Krywulak S, Backstein D, Pressman A, Gross AE. Long-term follow-up of fresh tibial osteochondral allografts for failed tibial plateau fractures. The Journal of Bone and Joint Surgery Series A. 2003;85(Suppl.1):33–39. doi: 10.2106/00004623-200300002-00005. [DOI] [PubMed] [Google Scholar]
- 10.Krettek C, Clausen J, Omar M, Noack S, Neunaber C. Two-stage late reconstruction with a fresh large osteochondral shell allograft transplantation (FLOCSAT) for a large ostechondral defect in a non-union after a lateral tibia plateau fracture 2-year follow up. Injury. 2017;48(7):1309–1318. doi: 10.1016/j.injury.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 11.Abolghasemian M, León S, Lee PT, Safir O, Backstein D, Gross AE, Kuzyk PR. Long-term results of treating large posttraumatic tibial plateau lesions with fresh osteochondral allograft transplantation. JBJS. 2019;101(12):1102–1108. doi: 10.2106/JBJS.18.00802. [DOI] [PubMed] [Google Scholar]
- 12.Gelber PE, Erquicia JI, Ramírez-Bermejo E, Fariñas O, Monllau JC. Fresh osteochondral and meniscus allografting for post-traumatic tibial plateau defects. Arthroscopy Techniques. 2018;7(6):e661–e667. doi: 10.1016/j.eats.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gajiwala AL. Tissue banking in India: gamma-irradiated allografts. Cell and Tissue Banking. 2003;4(2–4):203–211. doi: 10.1023/B:CATB.0000007022.91458.00. [DOI] [PubMed] [Google Scholar]
- 14.Csönge L, Bravo D, Newman-Gage H, Rigley T, Conrad EU, Bakay A, et al. Banking of osteochondral allografts, part II. Preservation of chondrocyte viability during long-term storage. Cell and Tissue Banking. 2002;3(3):161–168. doi: 10.1023/A:1023687419152. [DOI] [PubMed] [Google Scholar]
- 15.Ramponi DR, McSwigan T. Tibial plateau fractures. Advanced Emergency Nursing Journal. 2018;40(3):155–161. doi: 10.1097/TME.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 16.Albuquerque RP, Hara R, Prado J, Schiavo L, Giordano V, do Amaral NP. Epidemiological study on tibial plateau fractures at a level I trauma center. Acta Ortopedica Brasileira. 2013;21(2):109–115. doi: 10.1590/S1413-78522013000200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts TT, Rosenbaum AJ. Bone grafts, bone substitutes and orthobiologics the bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012;8(4):114–124. doi: 10.4161/org.23306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gardner MJ, Yacoubian S, Geller D, Suk M, Mintz D, Potter H, et al. The incidence of soft tissue injury in operative tibial plateau fractures. A magnetic resonance imaging analysis of 103 patients. Journal of Orthopeadic Trauma. 2005;19(2):79–84. doi: 10.1097/00005131-200502000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Melugin HP, Bernard CD, Camp CL, Stuart MJ, Saris DBF, Nakamura N, et al. Tibial plateau cartilage lesions: a systematic review of techniques, outcomes, and complications. Cartilage. 2019;16:1947603519855767. doi: 10.1177/1947603519855767. [DOI] [PMC free article] [PubMed] [Google Scholar]