Abstract
Purpose
To compare the radiological and clinical outcomes using simple medial meniscus posterior horn (MMPH) root repair using an all-inside meniscal repair device combined with high tibial osteotomy (HTO) and HTO alone.
Methods
Between November 2013 and December 2016, patients treated for MMPH root tear along with HTO were enrolled. Based on the tear gap, the participants were divided into repairable (< 2 mm) and unrepairable (> 2 mm) categories. The participants in each group were divided into those amenable to simple MMPH root repair using an all-inside meniscal repair device and those that required no procedure for meniscus. Radiological parameters including mechanical femorotibial alignment (MA), posterior tibial slope (PTS) and medial joint-space width (JSW) were evaluated preoperatively and postoperatively at 2 years. For clinical evaluation, the WOMAC score was determined at the 2-year visit postoperatively.
Results
A total of 81 knees including 48 repairable (group R) and 33 unrepairable (group I) knees were enrolled. A total of 43 knees underwent simple MMPH root repair using an all-inside meniscal repair device (subgroup r), whereas the other 38 knees did not (subgroup n). The MA, PTS, and their postoperative changes as well as the WOMAC scores showed no differences. However, the JSW in group Rr increased from 3.1 to 3.6 mm, but decreased from 3.7 to 3.4 in group Rn, which was a statistically significant difference.
Conclusion
Simple MMPH root repair using an all-inside meniscal repair device combined with HTO was more effective for the maintenance of JSW compared with HTO without a meniscal procedure in patients with repairable MMPH root tear and varus alignment. However, other options are needed for unrepairable MMPH root tear.
Keywords: Knee, Medial meniscus posterior horn, Medial meniscus posterior horn root tear, Osteotomy, Simple all inside meniscal repair device repair, Joint-space width
Introduction
Medial meniscus (MM) root tear, a complete radial tear of the posterior horn (PH) of the MM, interrupts the continuity of the circumferential fibers and leads to failure of meniscal function, which converts axial loads to transverse hoop stress [1–3]. This pathology also involves meniscal extrusion and medial joint-space narrowing [1, 3–6], and is closely related to progressive osteoarthritis of the medial compartment and varus alignment. A pull-out trans-osseous repair has been suggested and used to maintain the meniscal function [7–12].
High tibial osteotomy (HTO), which is an acceptable option for medial compartment osteoarthritis with varus alignment, has been suggested for the management of MMPH root tear with varus alignment [13, 14]. Nha et al. reported that HTO without a meniscal procedure yielded good clinical outcomes and recovery of half of the patients in second-look arthroscopy [13]. Lee et al. also reported good clinical outcomes; however, the healing was poor or led to scar formation, which resulted in defective hoop tension [14].
Restoration of the hoop tension of MM requires combined meniscal repair and HTO. Studies suggested that a combination of chondroplasty procedures, including microfracture, collagen, stromal vascular fraction, or stem-cell implantation enhanced chondral regeneration more than HTO alone [15–19]. However, for MMPH root tear, the common pull-out trans-osseous repair interfered with the screws of HTO [20]. FasT-Fix, an all-inside meniscal repair device for management of a peripheral tear in the posterior horn, represents an alternative to pull-out repair combined with HTO [21]. Although it cannot restore the original anatomical structure of bone insertion, the hoop tension of MM can be recovered by attaching the MMPH to the posterior cruciate ligament (PCL). However, few studies have explored this alternative option.
We evaluated the clinical and radiological effects of simple MMPH root repair using an all-inside meniscal repair device combined with HTO compared with HTO without any meniscal procedures, especially for the maintenance of hoop tension. We hypothesized that this simple repair procedure for MMPH root tear in a patient with varus alignment ensures the width of joint space better than any meniscal procedure combined with HTO.
Materials and Methods
The study protocol and design were reviewed and approved by the Ethics Committee of the Public Institutional Review Board (IRB approval: 2019-1300-002). Medical records and radiological results of HTO patients were retrospectively reviewed and compared based on the MMPH root tear and repair procedures.
The inclusion criteria were:
Medial compartment osteoarthritis with MMPH root tear and varus alignment greater than 5°.
Medial opening-wedge HTO fixed by the OhtoFix type I plate (Ohtomedical Co. Ltd., Goyang, Korea).
The exclusion criteria were:
Combined surgery including ligament reconstruction and osteotomy.
Loss of follow-up within 2 years.
Surgical Procedures and Post-operative Rehabilitation Protocol
The two surgeons conducted similar preoperative planning and surgical procedures, and post-operative rehabilitation protocols [22]. Preoperatively, the degree of correction was measured by Miniaci’s method, via the standing lower extremity anteroposterior (AP) view. By targeting the mechanical axis passing through the lateral tibial spine, the degree of correction was measured using a picture archiving and communication system (PACS), the PiView STAR (INFINITT, Seoul, Korea).
Following spinal anesthesia, the arthroscopic examination was performed via anteromedial and anterolateral portals. After debridement, microfracture chondroplasty, lateral retinacular release, or baker-cyst decompression were performed to manage the other intra-articular defects, including chondral lesion, tightened lateral retinaculum of patella, and Baker cyst. The MMPH root tear was identified by probing. A single surgeon (BS K) repaired the MMPH root using an all-inside meniscal repair device (FasT-Fix, Smith and Nephew, Andover, MA) if the tear site was reducible. The medial wall of the PCL and the torn site of MMPH were debrided. The first clip of the all-inside meniscal repair device was then attached to the MMPH, and the second clip was fixed to the PCL. The string was pulled to slide the two knots closely. After ensuring the attachment of the torn site to the PCL, the string was severed to restore the hoop tension of medial meniscus (Fig. 1). The arthroscopic surgery ended with irrigation and fluid drainage, and osteotomy was continued.
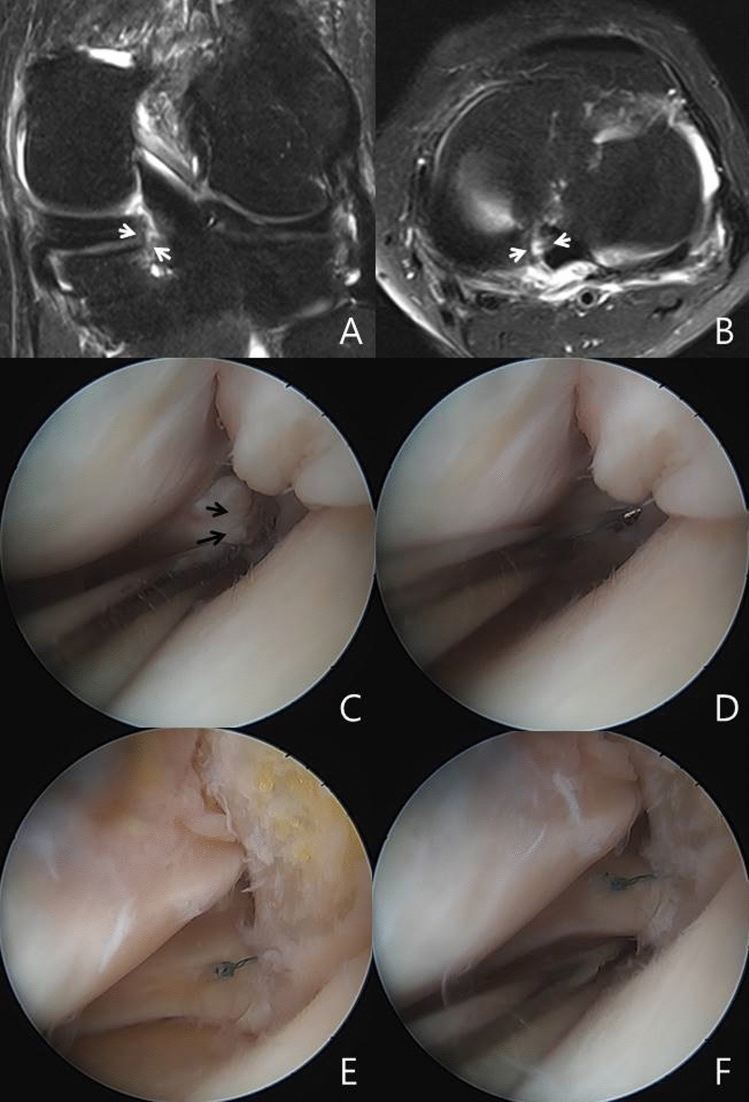
Fig. 1.
Simple MMPH root repair using an all-inside meniscal repair device. a, b Preoperative MRI shows MMPH root tear (white arrow). c, d In the arthroscopic examination, the tear site of MMPH root was probed (black arrow), which revealed no gap after reduction. e, f MMPH was repaired simply using an all-inside meniscal repair device, and the reduction was maintained by probing
A transverse incision was made on the medial side of the proximal tibia, and two guide pins were inserted on the metaphyseal flare. The two pins were placed parallel to the medial joint surface, targeting the safe zone [23]. Biplanar or uniplanar osteotomy was conducted after sawing below the guide pins up to 10 mm from the lateral cortex. The osteotomy site was opened gradually using the three chisels. A metal block with a planned diameter was applied for a widened gap. The OhtoFix type I plate (Ohtomedical Co., Ltd., Goyang, Korea) was fixed with six locking screws and a link screw to the metal block. The cancellous bone-chip was grafted to the osteotomy site, followed by suction with a Hemovac drain, followed by sutures, compressive dressing, and a cylinder splint.
Postoperatively, the drain was removed on post-operative day 2. Continuous passive motion along with a hinged knee-brace was administered for two months. Weight-bearing protocol was started at postoperative week 1 via toe touch with two crutches and partial weight-bearing exercises were performed with crutches for 3 weeks [24, 25]. A tolerable, full-weight bearing posture was allowed at 4 weeks postoperatively. The union was confirmed via postoperative radiography at 1 and 2 years, and the plate removal was recommended after confirming complete union.
Evaluation and Statistical Analysis
The patients were recommended to undergo postoperative follow-up at 2 months, 6 months, 1 year, and 2 years. During the follow-up, the following radiographic views were obtained: the Rosenberg, lateral, standing AP, and standing lower-extremity AP. The mechanical femorotibial angle (MA) in the standing lower-extremity AP view, posterior tibial slope (PTS) in the lateral view, and medial joint-space width (JSW) in the Rosenberg view [26] were measured in the previous PACS viewer. The software detected a minimum angular difference of 0.1° and a minimum difference in length of 0.1 mm. Radiological data of MA, PTS, and JSW were measured preoperatively and postoperatively at 2 years, and their postoperative changes were also documented. Clinical outcomes were determined using the 2-year postoperative Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores.
Two independent investigators (BS K and SY S) determined the JSW in the Rosenberg view to reduce the observational bias. The intraclass correlation coefficients were 0.858 and 0.855, which were greater than 0.80 for the intraobserver and interobserver reliabilities. Thus, measurements obtained by one investigator (BS K) were used in the analyses.
MMPH root tears were classified previously according to the tear gap depending on whether or not an overlapped type was repairable [4, 5]. Therefore, we divided the participants into two groups: repairable (group R: no tear gap or within 2 mm after debridement) and unrepairable (group I: tear gap greater than 2 mm after debridement). The radiological and clinical outcomes of each group undergoing simple repair (Rr and Ir) were compared with the group without intervention (Rn and In). Statistically, the differences in preoperative and 2-year postoperative values of MA, PTS, and JSW were compared using the Mann–Whitney test. The WOMAC scores at postoperative 2 years were also compared using the Mann–Whitney test. The SPSS 12.0 (SPSS Science, Inc., Chicago, IL) was used for all statistical analyses, and P < 0.05 was considered statistically significant.
Results
Between November 2013 and December 2016, a total of 126 knee joints (110 patients) were treated with medial opening-wedge HTO by the two surgeons. Among them, 81 knees showed MMPH root tear in the arthroscopic examination, 48 knees were repairable (group R) and 33 knees were unrepairable (group I). Of the 81 knees, 43 were managed via simple repair using an all-inside meniscal repair device, and the other 38 knees did not. Among the 48 knees in group R, a simple repair was performed in 29 knees (group Rr), and the remaining 19 knees did not undergo any procedure for MMPH root tear (group Rn). Among the 33 knees included in group I, 14 underwent simple repair (group Ir) and the other 19 knees did not (group In). The demographics of each group are shown in Table 1, without significant differences between treated and untreated cases.
Table 1.
Demographics (Mean ± Standard deviation)
| Group Tr | Group Tn | P | Group Rr | Group Rn | P | Group Ir | Group In | P | |
|---|---|---|---|---|---|---|---|---|---|
| Sex (M/F) | 8/35 | 8/30 | n.s. | 3/26 | 2/17 | n.s. | 5/9 | 6/13 | n.s. |
| Age, years | 55.7 ± 5.6 | 56.2 ± 4.1 | n.s. | 55.7 ± 5.4 | 56.2 ± 3.6 | n.s. | 55.8 ± 6.0 | 56.1 ± 4.7 | n.s. |
| Height, cm | 158 ± 8 | 157 ± 7 | n.s. | 157 ± 8 | 156 ± 4 | n.s. | 160 ± 9 | 158 ± 9 | n.s. |
| Weight, kg | 67 ± 14 | 64 ± 10 | n.s. | 65 ± 13 | 63 ± 10 | n.s. | 72 ± 14 | 66 ± 10 | n.s. |
| BMI | 26.9 ± 4.2 | 26.1 ± 3.2 | n.s. | 26.4 ± 4.2 | 26.1 ± 3.7 | n.s. | 27.9 ± 4.0 | 26.0 ± 2.7 | n.s. |
| Pre MA, ° | 6.8 ± 1.9 | 7.6 ± 2.9 | n.s. | 6.7 ± 2.5 | 7.6 ± 2.7 | n.s. | 6.8 ± 2.2 | 7.6 ± 3.2 | n.s. |
| Pre JSW, mm | 3.2 ± 1.4 | 3.6 ± 1.6 | n.s. | 3.1 ± 1.4 | 3.7 ± 1.2 | n.s. | 3.4 ± 1.4 | 3.4 ± 2.0 | n.s. |
| Pre PTS, ° | 12.3 ± 3.8 | 12.2 ± 3.2 | n.s. | 12.3 ± 4.0 | 12.9 ± 3.3 | n.s. | 12.3 ± 3.5 | 11.5 ± 2.9 | n.s. |
MA mechanical femorotibial angle, JSW joint space width, PTS posterior tibial slope
Based on post hoc power analysis via a two-sided hypothesis to obtain a power of 0.8 and a significance level of 0.05 a total of 46 participants were considered adequate for the detection of significant differences in JSW postoperatively between the two groups (Rr and Rn) of repairable patients.
In the radiological results, the preoperative MA, PTS, and JSW of Tr (total, repair) and Tn (total, no repair) groups were 6.8°, 12.3°, and 3.2 mm, and 7.6°, 12.2°, and 3.6 mm, respectively. The mean size of the metal block was 9.7 mm in the Tr group and 9.9 mm in the Tn group. At 2 years postoperatively, the MA, PTS, and JSW changed to − 1.3°, 13.8°, and 3.5 mm, respectively, in group Tr; and − 0.9°, 14.2°, and 3.6 mm, respectively, in group Tn. The changes in MA, PTS, and JSW were 8.1°, 1.5°, and 0.3 mm, respectively, in group Tr; and 8.5°, 2.0°, and 0 mm, respectively, in group Tn. None of the radiological outcomes of groups Tr and Tn showed any statistically significant differences (Table 2).
Table 2.
Results (Mean ± Standard deviation)
| Group Tr | Group Tn | P | Group Rr | Group Rn | P | Group Ir | Group In | P | |
|---|---|---|---|---|---|---|---|---|---|
| Metal block, mm | 9.7 ± 1.9 | 9.9 ± 2.1 | n.s. | 9.5 ± 1.9 | 9.6 ± 2.2 | n.s. | 10.1 ± 1.8 | 10.2 ± 2.1 | n.s. |
| Pre MA, ° | 6.8 ± 1.9 | 7.6 ± 2.9 | n.s. | 6.7 ± 1.7 | 7.6 ± 2.7 | n.s. | 6.8 ± 2.2 | 7.6 ± 3.2 | n.s. |
| Post MA, ° | − 1.3 ± 1.8 | − 0.9 ± 2.0 | n.s. | − 1.3 ± 1.6 | − 0.7 ± 1.7 | n.s. | − 1.4 ± 2.4 | − 1.1 ± 2.4 | n.s. |
| Diff MA, ° | 8.1 ± 2.2 | 8.5 ± 2.7 | n.s. | 8.1 ± 1.9 | 8.4 ± 2.4 | n.s. | 8.3 ± 2.9 | 8.7 ± 3.0 | n.s. |
| Pre JSW, mm | 3.2 ± 1.4 | 3.6 ± 1.6 | n.s. | 3.1 ± 1.4 | 3.7 ± 1.2 | n.s. | 3.4 ± 1.4 | 3.4 ± 2.0 | n.s. |
| Post JSW, mm | 3.5 ± 1.0 | 3.6 ± 1.2 | n.s. | 3.6 ± 0.8 | 3.4 ± 1.2 | n.s. | 3.4 ± 1.4 | 3.7 ± 1.3 | n.s. |
| Diff JSW, mm | 0.3 ± 1.2 | 0.0 ± 1.6 | n.s. | 0.5 ± 1.2 | − 0.3 ± 0.7 | 0.010a | 0.0 ± 1.0 | 0.3 ± 2.1 | n.s. |
| Pre PTS, ° | 12.3 ± 3.8 | 12.2 ± 3.2 | n.s. | 12.3 ± 4.0 | 12.9 ± 3.3 | n.s. | 12.3 ± 3.5 | 11.5 ± 2.9 | n.s. |
| Post PTS, ° | 13.8 ± 3.5 | 14.2 ± 3.8 | n.s. | 13.7 ± 3.2 | 15.0 ± 4.0 | n.s. | 14.1 ± 4.2 | 13.5 ± 3.5 | n.s. |
| Diff PTS, ° | 1.5 ± 2.6 | 2.0 ± 2.7 | n.s. | 1.4 ± 2.9 | 2.1 ± 2.9 | n.s. | 1.8 ± 1.8 | 2.0 ± 2.5 | n.s. |
| Womac score | 77 ± 11 | 76 ± 11 | n.s. | 78 ± 12 | 77 ± 10 | n.s. | 73 ± 5 | 74 ± 11 | n.s. |
MA mechanical femorotibial angle, JSW joint space width, PTS posterior tibial slope
a Indicates a statistical significant difference (P < 0.05)
However, there was a statistically significant difference in JSW between the repairable groups. Preoperatively, the MA, PTS, and JSW were 6.7°, 12.3°, and 3.1 mm, respectively, in group Rr; and 7.6°, 12.9°, and 3.7 mm, respectively, in group Rn. The mean sizes of the metal block were 9.5 mm and 9.6 mm in groups Rr and Rn, respectively. The MA, PTS, and JSW changed to − 1.3°, 13.7°, and 3.6 mm, respectively, in group Rr; and − 0.7°, 15.0°, and 3.4 mm, respectively, in group Rn, postoperatively at 2 years. The changes were 8.1°, 1.4°, and 0.5 mm, respectively, in group Rr (Fig. 2); and 8.4°, 2.1°, and − 0.3 mm in group Rn. The change in JSW was significant between the two groups, but other numeric results showed no statistically significant differences between the groups Rr and Rn. The 2-year postoperative WOMAC score was 78 in group Rr and 77 in group Rn, without any statistically significant difference (Table 2).
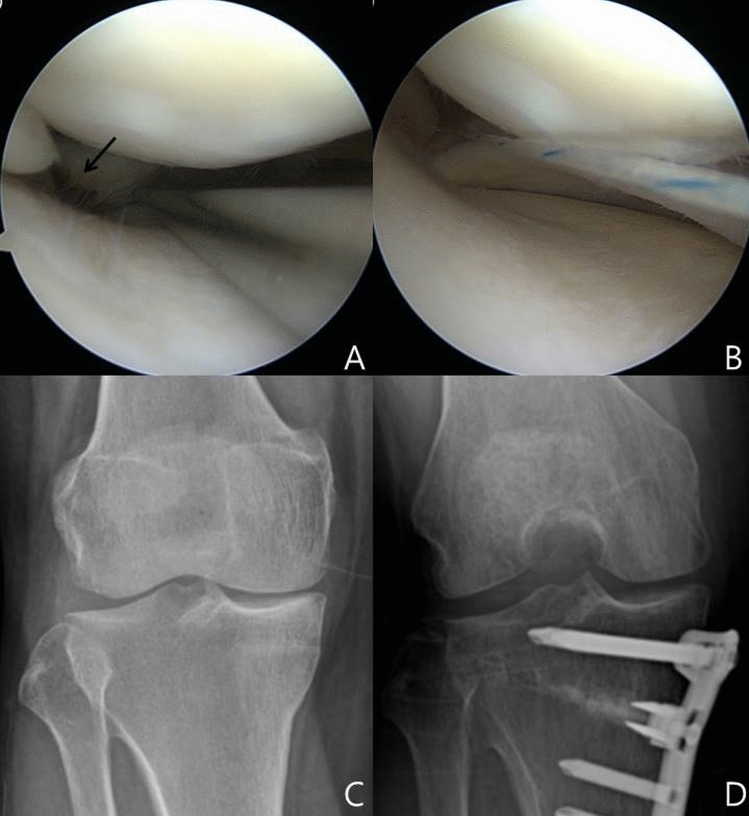
Fig. 2.
Radiological result. a, b The tear site of MMPH root (black arrow) was repaired simply. c, d The postoperative Rosenberg view 2 years later, revealed an increase in the medial joint-space width (JSW) compared with the preoperative view
In the unrepairable groups, the preoperative values of MA, PTS, and JSW were 6.8°, 12.3°, and 3.4 mm, respectively, in group Ir; and 7.6°, 11.5° and 3.4 mm, respectively, in group In. During the operation, the mean sizes of the metal block were 10.1 mm in group Ir and 10.2 mm in group In. The MA, PTS, and JSW changed to − 1.4°, 14.1°, and 3.4 mm, respectively, in group Ir; and − 1.1°, 13.5°, and 3.7 mm, respectively, in group In at 2 years, postoperatively. The respective changes were 8.3°, 1.8°, and 0.0 mm in group Ir and 8.7°, 2.0°, and 0.3 mm in group In. The mean WOMAC score at 2 years postoperatively was 73 in group Ir and 74 in group In. None of the results of groups Ir and In showed any statistically significant difference in Mann–Whitney test (Table 2).
Discussion
The main purpose of this study was to compare the JSW after HTO between knees treated with simple meniscal repair using an all-inside meniscal repair device and those not subjected to any meniscal procedure. A simple meniscal repair combined with HTO maintained the JSW at the 2-year follow-up, but not in the group exposed to HTO without any meniscal procedures in the repairable stage. However, in the unrepairable stage of MMPH root tear, there was no difference in clinical and radiological outcomes compared with the repaired group.
The results of MMPH root repair combined with HTO were reported previously [21]. No clinical or radiological difference was detected between the repaired and unrepaired groups, suggesting that the radiological outcomes do not suggest the repair of MMPH root tear [21]. The current study also revealed no differences between Tr and Tn groups. However, in the subgroup of repairable patients, the changes in JSW differed between Rr and Rn groups. A superior healing rate associated with repaired MMPH root tear combined with HTO was reported in the previous study [21]. Therefore, a simple MMPH root repair using an all-inside meniscal repair device is effective for repairable MMPH root tear.
JSW in the Rosenberg view, which is the radiological result in this study, is an appropriate parameter for the evaluation of progressive osteoarthritis or meniscal hoop tension. In previous studies, JSW was used to reflect cartilage thickness and was considered the simplest and the easiest parameter to evaluate the progression of osteoarthritis of the knee joint [26–28]. Two studies investigating the lateral closing HTO used the standing AP view [26, 27]. Another study utilized the standardized weight-bearing, semi-flexed PA views to compare the medial opening-wedge HTO and the knee-joint distraction [28]. In a recent study, the Rosenberg view, 45° PA flexion weight-bearing radiography, showed a significant correlation with clinical outcomes after medial opening-wedge HTO [29]. Because we focused on the progression of osteoarthritis after medial opening-wedge HTO, the JSW in the Rosenberg view was used as the main quantitative value, and the difference between Rr and Rn groups underscored the need for simple MMPH root repair.
Correction of alignment is an important factor in the management of MMPH root tear. In previous studies, the MMPH root-tear patients showed acceptable clinical outcomes after HTO, even though no additional meniscal procedures were performed [13, 14]. Nakamura et al. suggested that the lateral tilt of the tibia plateau and load-shifting effect after HTO positively affected the healing of MMPH root tear. Our study showed that all groups, with or without repair, showed good clinical outcomes 2 years post-HTO.
However, the need to recover hoop tension of MM has been suggested, despite the strong clinical outcomes of HTO. In the second-look arthroscopy after HTO described in two previous studies, the torn root was healed in only half the cases, and all healing states were lax or scarred, which was limited to recovery of hoop tension, the most important mechanical property of the meniscus [13, 14]. Previous studies investigated the MMPH root tear in well-aligned non-arthritic knees. These reported an association between non-operative treatment or partial menisectomy and good clinical outcomes, without any benefit in halting arthritic progression [30–33]. In this study, the Rn group showed good clinical outcomes at 2 years; however, the JSW was reduced, which may suggest that the loss of hoop tension of MM causes progression of osteoarthritis leading to poor long-term clinical outcomes. Although the simple MMPH root repair is a non-anatomical repair and may not be strong enough to resolve the hoop tension, this simple repair method combined with HTO maintained the JSW more than any other procedure. This finding appears to be consistent with a previous meta-analysis, which reported that the repair of MMPH root tear alleviates osteoarthritis [32].
The disadvantages of this simple method include non-anatomical repair and the probability of excessive tension on the repair site. Ideally, anatomically complex methods, such as pull-out repair, are more appropriate for MMPH root tear. Therefore, the results of the current study only suggest that this simple method is better than no procedure at all in cases amenable to MMPH root repair when the tear gap is less than 2 mm. However, its advantage compared with anatomical pull-out repair is unknown. Nonetheless, this method is simple, faster and easier than anatomical repair and is indicated for repairable cases. A further study is needed to compare our simple method with anatomical repair techniques.
This simple method is not effective for all patients with MMPH root tears. Previous studies investigating the classification of MMPH root tear focused on the tear gap [4, 5]. Kim et al. suggested that patients with an MMPH root tear gap greater than 1 mm were more likely to exhibit poor clinical outcomes after surgical repair [5]. Tear gap is the most important factor in evaluating the MMPH root tears. Repair of MMPH root tear in combination with HTO is effective. We found that simple MMPH root repair was effective in the repairable group of knees with a tear gap less than 2 mm in arthroscopy. However, the irreparable group with a tear gap greater than 2 mm showed no difference in clinical outcome or JSW change between groups with or without repair. This finding suggests that the simple repair combined with HTO was effective only for the repairable MMPH root tear, but not for irreparable states, which require a more sophisticated method such as suture anchor repair with centralization [20].
This study limitation relates to the inclusion of two different surgeons, with each surgeon mainly allocated to the repair group but not to the group without the intervention, resulting in possible differences in JSW change. For instance, the postoperative 2-year MA values in the Rr and Rn groups were − 1.3° and − 0.7°, respectively. The Rn group was more neutral or varus than the Rr group. Our study cannot confirm whether the insufficient correction was reflected in reduced JSW or vice versa. However, the reduced JSW was more prominent between the two Rr and Rn groups than the alignment, and the statistical analysis showed a significant difference only in JSW reduction. Therefore, we suggest that the difference in MMPH root repair techniques reduces JSW and leads to a mildly insufficient correction. Additional studies are needed to resolve this issue.
Other study limitations were as follows. First, the study design was not prospective or randomized. Furthermore, the allocation was mainly decided by the two different surgeons, as previously described. Second, there was no follow-up evaluation of the MMPH root tear via MRI or arthroscopic examination. Third, there was only a short-term follow-up of 2 years. However, the demographics of the groups revealed no statistically significant differences, but only a significant reduction in JSW in the Rn group compared with the Rr group. Based on the importance of JSW reduction in evaluating the progression of osteoarthritis, a simple MMPH root repair using an all-inside meniscal repair device combined with HTO is recommended for patients with repairable MMPH root tear.
Conclusion
A simple MMPH root repair using an all-inside meniscal repair device with HTO is superior to HTO without a meniscal procedure to maintain the JSW in patients with repairable MMPH root tear and varus alignment. However, other options are needed for the management of unrepairable MMPH root tear.
Compliance with ethical standards
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standard of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patients included in the current study.
References
- 1.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. American Journal of Sports Medicine. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 2.Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20:373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Chahla J, LaPrade RF. Meniscal root tears. Arthroscopy. 2019;35:1304–1305. doi: 10.1016/j.arthro.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Bin SI, Jeong TW, Kim SJ, Lee DH. A new arthroscopic classification of degenerative medial meniscus root tear that correlates with meniscus extrusion on magnetic resonance imaging. The Knee. 2016;23:246–250. doi: 10.1016/j.knee.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Kim JY, Bin SI, Kim JM, Lee BS, Oh SM, Cho WJ. A novel arthroscopic classification of degenerative medial meniscus posterior root tears based on the tear gap. Orthopaedic Journal of Sports Medicine. 2019;7:2325967119827945. doi: 10.1177/2325967119827945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park JY, Kim BH, Ro DH, Lee MC, Han HS. Characteristic location and rapid progression of medial femoral condylar chondral lesions accompanying medial meniscus posterior root tear. The Knee. 2019;26:673–678. doi: 10.1016/j.knee.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24:1455–1468. doi: 10.1007/s00167-015-3832-0. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. American Journal of Sports Medicine. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan DJ, Alaia EF, Dold AP, Meislin RJ, Strauss EJ, Jazrawi LM, et al. Increased extrusion and ICRS grades at 2-year follow-up following transtibial medial meniscal root repair evaluated by MRI. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26:2826–2834. doi: 10.1007/s00167-017-4755-8. [DOI] [PubMed] [Google Scholar]
- 10.Kodama Y, Furumatsu T, Fujii M, Tanaka T, Miyazawa S, Ozaki T. Pullout repair of a medial meniscus posterior root tear using a FasT-Fix((R)) all-inside suture technique. Orthopaedics & Traumatology: Surgery & Research. 2016;102:951–954. doi: 10.1016/j.otsr.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Furumatsu T, Okazaki Y, Kodama Y, Okazaki Y, Masuda S, Kamatsuki Y, et al. Pullout repair using modified Mason-Allen suture induces better meniscal healing and superior clinical outcomes: A comparison between two surgical methods. The Knee. 2019;26:653–659. doi: 10.1016/j.knee.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Feucht MJ, Kuhle J, Bode G, Mehl J, Schmal H, Sudkamp NP, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31:1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 13.Nha KW, Lee YS, Hwang DH, Kwon JH, Chae DJ, Park YJ, et al. Second-look arthroscopic findings after open-wedge high tibia osteotomy focusing on the posterior root tears of the medial meniscus. Arthroscopy. 2013;29:226–231. doi: 10.1016/j.arthro.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 14.Lee HI, Park D, Cho J. Clinical and radiological results with second-look arthroscopic findings after open wedge high tibial osteotomy without arthroscopic procedures for medial meniscal root tears. Knee Surgery & Related Research. 2018;30:34–41. doi: 10.5792/ksrr.17.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong KL, Lee KB, Tai BC, Law P, Lee EH, Hui JH. Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: a prospective, randomized controlled clinical trial with 2 years' follow-up. Arthroscopy. 2013;29:2020–2028. doi: 10.1016/j.arthro.2013.09.074. [DOI] [PubMed] [Google Scholar]
- 16.Kahlenberg CA, Nwachukwu BU, Hamid KS, Steinhaus ME, Williams RJ., 3rd Analysis of outcomes for high tibial osteotomies performed with cartilage restoration techniques. Arthroscopy. 2017;33:486–492. doi: 10.1016/j.arthro.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 17.Kim MS, Koh IJ, Choi YJ, Pak KH, In Y. Collagen augmentation improves the quality of cartilage repair after microfracture in patients undergoing high tibial osteotomy: a randomized controlled trial. American Journal of Sports Medicine. 2017;45:1845–1855. doi: 10.1177/0363546517691942. [DOI] [PubMed] [Google Scholar]
- 18.Kim YS, Koh YG. Comparative matched-pair analysis of open-wedge high tibial osteotomy with versus without an injection of adipose-derived mesenchymal stem cells for varus knee osteoarthritis: clinical and second-look arthroscopic results. American Journal of Sports Medicine. 2018;46:2669–2677. doi: 10.1177/0363546518785973. [DOI] [PubMed] [Google Scholar]
- 19.Lee OS, Lee SH, Mok SJ, Lee YS. Comparison of the regeneration of cartilage and the clinical outcomes after the open wedge high tibial osteotomy with or without microfracture: a retrospective case control study. BMC Musculoskeletal Disorders. 2019;20:267. doi: 10.1186/s12891-019-2607-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakamura R, Takahashi M, Kuroda K, Katsuki Y. Suture anchor repair for a medial meniscus posterior root tear combined with arthroscopic meniscal centralization and open wedge high tibial osteotomy. Arthroscopy Techniques. 2018;7:e755–e761. doi: 10.1016/j.eats.2018.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee OS, Lee SH, Lee YS. Comparison of the radiologic, arthroscopic, and clinical outcomes between repaired versus unrepaired medial meniscus posterior horn root tear during open wedge high tibial osteotomy. The Journal of Knee Surgery. 2019 doi: 10.1055/s-0039-1692992. [DOI] [PubMed] [Google Scholar]
- 22.Suh DW, Kyung BS, Han SB, Cheong K, Lee WH. Efficacy of tranexamic acid for hemostasis in patients undergoing high tibial osteotomy. The Journal of Knee Surgery. 2018;31:50–55. doi: 10.1055/s-0037-1600091. [DOI] [PubMed] [Google Scholar]
- 23.Han SB, Lee DH, Shetty GM, Chae DJ, Song JG, Nha KW. A "safe zone" in medial open-wedge high tibia osteotomy to prevent lateral cortex fracture. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21:90–95. doi: 10.1007/s00167-011-1706-7. [DOI] [PubMed] [Google Scholar]
- 24.Takeuchi R, Ishikawa H, Aratake M, Bito H, Saito I, Kumagai K, et al. Medial opening wedge high tibial osteotomy with early full weight bearing. Arthroscopy. 2009;25:46–53. doi: 10.1016/j.arthro.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 25.Lansdaal JR, Mouton T, Wascher DC, Demey G, Lustig S, Neyret P, et al. Early weight bearing versus delayed weight bearing in medial opening wedge high tibial osteotomy: a randomized controlled trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25:3670–3678. doi: 10.1007/s00167-016-4225-8. [DOI] [PubMed] [Google Scholar]
- 26.Park CH, Bae DK, Kim KI, Lee JW, Song SJ. Serial changes in the joint space width and joint line convergence angle after closed-wedge high tibial osteotomy. American Journal of Sports Medicine. 2017;45:3254–3261. doi: 10.1177/0363546517729153. [DOI] [PubMed] [Google Scholar]
- 27.Koshino T, Wada S, Ara Y, Saito T. Regeneration of degenerated articular cartilage after high tibial valgus osteotomy for medial compartmental osteoarthritis of the knee. The Knee. 2003;10:229–236. doi: 10.1016/S0968-0160(03)00005-X. [DOI] [PubMed] [Google Scholar]
- 28.van der Woude JAD, Wiegant K, van Heerwaarden RJ, Spruijt S, van Roermund PM, Custers RJH, et al. Knee joint distraction compared with high tibial osteotomy: a randomized controlled trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25:876–886. doi: 10.1007/s00167-016-4131-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nha KW, Oh SM, Ha YW, Patel MK, Seo JH, Lee BH. Radiological grading of osteoarthritis on Rosenberg view has a significant correlation with clinical outcomes after medial open-wedge high-tibial osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy. 2019;27:2021–2029. doi: 10.1007/s00167-018-5121-1. [DOI] [PubMed] [Google Scholar]
- 30.Krych AJ, Reardon PJ, Johnson NR, Mohan R, Peter L, Levy BA, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25:383–389. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 31.Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26:1117–1122. doi: 10.1007/s00167-017-4454-5. [DOI] [PubMed] [Google Scholar]
- 32.Faucett SC, Geisler BP, Chahla J, Krych AJ, Kurzweil PR, Garner AM, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. American Journal of Sports Medicine. 2019;47:762–769. doi: 10.1177/0363546518755754. [DOI] [PubMed] [Google Scholar]
- 33.Lee BS, Bin SI, Kim JM, Park MH, Lee SM, Bae KH. Partial meniscectomy for degenerative medial meniscal root tears shows favorable outcomes in well-aligned, nonarthritic knees. American Journal of Sports Medicine. 2019;47:606–611. doi: 10.1177/0363546518819225. [DOI] [PubMed] [Google Scholar]