Abstract
Purpose
This study aimed to compare the clinical outcomes between accelerated rehabilitation (AR) and non-accelerated rehabilitation (NR) after anterior cruciate ligament reconstruction (ACLR) using hamstring autografts through a systematic review and meta-analysis.
Methods
To compare the outcomes between AR and NR, we searched Medline, Embase, and the Cochrane Library. Studies comparing their clinical outcomes after ACLR using hamstring autografts were included. AR was characterized by the starting range of motion and weight-bearing within 3 days and return to sports within 6–9 months. A meta-analysis of clinical outcome parameters used in ≥ 3 studies was conducted.
Results
Seven studies were included. The International Knee Documentation Committee subjective score was significantly higher in AR than in NR at the 3- (mean difference [MD], 7.30; 95% confidence interval [CI] 1.55–13.05; P = 0.013) and 6-month follow-ups (MD, 5.64; 95% CI 0.11–11.17; P = 0.046). The side-to-side difference in anterior tibial translation at the final follow-up assessed in four studies was significantly lower in NR than in AR (MD, 0.59; 95% CI 0.12–1.07; P = 0.015). Overall Tunnel widening at the final follow-up assessed in four studies was also smaller in NR than in AR (MD, 0.48; 95% CI 0.00–0.96; P = 0.0479). However, the mean side-to-side difference and overall tunnel widening between them was < 1 mm.
Conclusion
The early subjective clinical outcomes of AR after ACLR using hamstring autografts were superior to those of NR. Although tunnel widening and anterior instability were also significantly larger in AR than in NR, the difference was not clinically relevant.
Keywords: Knee, Anterior cruciate ligament reconstruction, Hamstring, Accelerated rehabilitation, Meta-analysis
Introduction
The primary goal of anterior cruciate ligament reconstruction (ACLR) is to maximize knee stability and functional capacity while permitting a safe return to sports [1, 2]. Although surgical aspects are crucial to the success of the treatment, rehabilitation after surgery is equally important [3, 4]. However, currently, there is no consensus on the content and assessment methods of rehabilitation programs [2]. A high variability in the composition and time ranges of rehabilitation components may lead to confusion among patients and therapists [5].
Traditional postoperative restrictions, such as bracing for immobilization, delayed weight-bearing, and limiting early full extension, have all been used in rehabilitation protocols after ACLR to prevent excessive loads on the healing graft [6]. However, Shelbourne and Nitz introduced an accelerated rehabilitation (AR) protocol after ACLR using bone–patellar tendon–bone (BPTB) autografts to overcome many complications, such as prolonged knee stiffness, limitation of complete extension, delay in strength recovery, and anterior knee pain [7]. This rehabilitation protocol permits early range of motion (ROM) and weight-bearing, as well as return to light sporting activities by 2 months and full activity within 4–6 months after reconstruction [7, 8]. Previous studies have reported that AR decreased the incidence of surgical complications and improved knee function in patients who underwent ACLR [9, 10] although it did not affect long-term knee stability [11, 12].
As hamstring autografts have gained popularity in recent years owing to decreased harvest-site morbidity and lower incidence of patellofemoral osteoarthritis [13–16], there has been a concern on whether AR can be applied after ACLR using hamstring autografts. This concern is theoretically based on the slower incorporation rate of soft tissue to the bone tunnel and the increased laxity resulting from excessive graft–tunnel motion [17]. Several clinical studies have evaluated the effectiveness and safety of AR after ACLR using hamstring autografts; however, the results have been controversial [18–21]. Recently, a systematic review reported the clinical outcomes of AR after ACLR using hamstring autografts with the use of a best-evidence synthesis [22]. However, there have been no statistical approach (meta-analysis) to combine the results from previous comparative studies.
Therefore, the purpose of this study was to investigate the effectiveness and safety of AR after ACLR using hamstring autografts through a systematic review and meta-analysis of comparative studies. We hypothesized that AR after ACLR using hamstring autografts would result in early functional recovery and would not cause clinically relevant complications compared with non-accelerated rehabilitation (NR).
Materials and Methods
Literature Search and Data Sources
Multiple comprehensive databases were searched to find studies comparing the clinical outcomes of AR and NR after ACLR using hamstring autografts. This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [23].
To identify relevant articles for inclusion in this meta-analysis, two different authors separately performed Internet searches in Medline (1950 to June 2019), Embase (1974 to June 2019), and the Cochrane Library (1950 to June 2019) databases on the same day (June 30, 2019). In addition, the search was repeated near the completion of the data analysis (July 20, 2019) to ensure a comprehensive investigation.
The following keywords and medical subject heading terms were included in the searches: (anterior cruciate ligament OR ACL) AND (reconstruction) AND (accelerated OR aggressive) AND (rehabilitation). After the initial electronic search, additional relevant articles were retrieved by searching the bibliographies of all selected full-text articles.
Study Selection
Two reviewers independently confirmed the inclusion of all studies according to the selection criteria. For study selection, the reviewers screened the titles and abstracts of the identified studies and subsequently screened the full text. Table 1 summarizes the inclusion and exclusion criteria. Based on previous studies [22, 24, 25], AR was defined as starting ROM and weight-bearing within 3 days after surgery and return to sports within 6–9 months. If more than one of these criteria (ROM, weight-bearing, and return to sports) was not satisfied, the protocol was defined as NR.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria |
| Studies comparing the clinical outcomes of AR and NR after primary ACLR |
| AR characterized by starting ROM and weight-bearing within 3 days and return to sports within 6–9 months |
| Hamstring autografts |
| Any surgical methods of primary ACLR (number of graft bundle, tunnel technique, and fixation method) |
| English language or with a recognizable data table of results |
| Human subjects |
| Exclusion criteria |
| Non-comparative case series |
| Other than hamstring autografts |
| Not matched AR/NR protocol |
| No usable information/data |
| Review or meta-analysis |
| Case reports |
AR accelerated rehabilitation, NR non-accelerated rehabilitation, ACLR anterior cruciate ligament reconstruction, ROM range of motion
Data Extraction
Two reviewers independently recorded data from each study using a predefined data extraction form; these data included the first author, journal title, year of publication, study design, sample size, mean age, follow-up period, number of graft bundles, femoral tunnel placement technique, graft fixation methods, treatments for meniscal lesions, and values of outcome parameters. Disagreement between the reviewers was resolved by consensus or discussion with a third investigator when consensus was not reached. The primary outcomes of interest were the International Knee Documentation Committee (IKDC) subjective scores at the 3- and 6-month follow-ups. The secondary outcomes of interest included the side-to-side difference (STSD) in anterior tibial translation and tunnel widening of both the femoral and tibial tunnels at the final follow-up.
Study Quality Assessment
Two reviewers independently assessed the risk of bias in the enrolled studies. To assess the risk of bias in these studies, we used the Risk of Bias (RoB) 2 tool for randomized controlled trials and the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool for non-randomized studies. The RoB 2 tool prompts judgments regarding biases in five domains: bias arising from the randomization process, derivations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result [26]. The ROBINS-I tool covers seven domains: bias due to confounding, participant selection, classification of interventions, deviations from intended interventions, missing data, measurement of outcomes, and selection of the reported results [27].
Statistical Analysis
A meta-analysis of the outcome parameters that were used in ≥ 3 studies was conducted (IKDC subjective score, STSD in anterior tibial translation, and tunnel widening). The mean and standard deviation (SD) of these parameters were obtained from each study. In studies with a sample size of ≤ 70 that did not report the SD, we estimated the SD by dividing the range by 4 using the method established by Hozo et al. [28]; in studies that only reported the SD for the total group and did not report the SD and range for each group, we used the SD of the total group in the meta-analysis.
Publication bias could not be assessed in this study. Tests for funnel plot asymmetry are typically performed only when at least ten studies are included in the meta-analysis [29]. As our analysis included only seven studies, tests for asymmetry would be ineffective because they would be unable to differentiate the results.
Statistical analysis was performed using the R software (R Foundation for Statistical Computing, Vienna, Austria). The I2 value was used to estimate statistical heterogeneity. When the I2 value was > 50%, heterogeneity was accepted, and a random-effects model was adopted. Otherwise, a fixed-effects model was adopted. A P value of < 0.05 was considered statistically significant.
Results
Study Selection
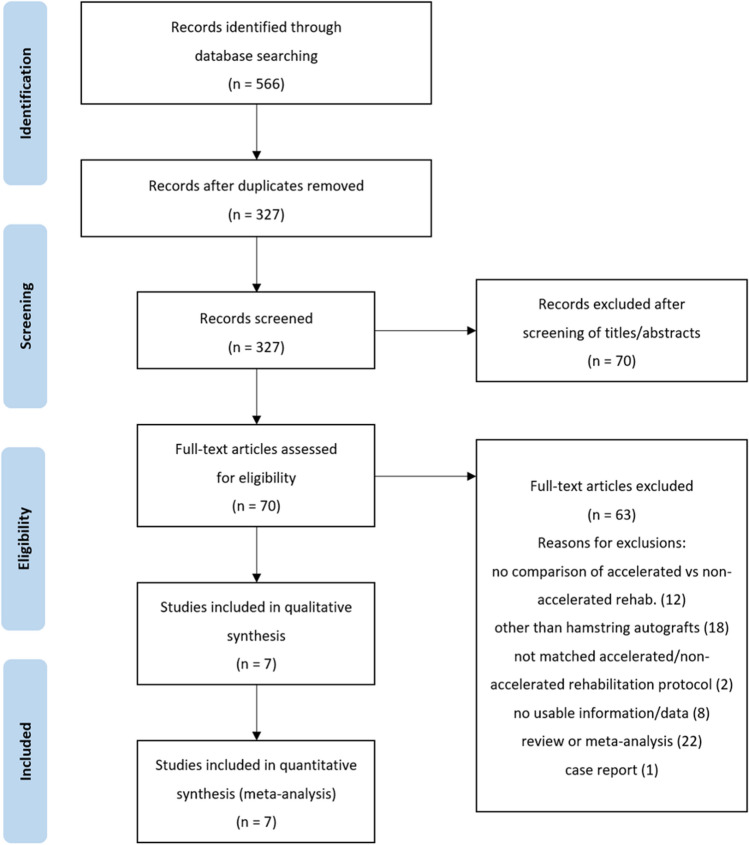
The study selection process is illustrated in Fig. 1. The electronic search yielded 219 studies in PubMed (Medline), 297 studies in Embase, and 50 studies in the Cochrane Library. No further studies were found through manual search, and 239 duplicate studies were removed. After screening of the titles and abstracts and after a full-text review of the 327 remaining studies, seven studies were finally included in the meta-analysis [18–21, 30–32].
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of the literature selection process
Study Characteristics
All seven articles included in this study were comparative studies published in English between 2001 and 2017 (Table 2). All seven studies used rehabilitation methods consistent with the common AR protocol of early ROM, weight-bearing, and return to sports activity, although the protocol slightly differed from study to study. The detailed rehabilitation protocols for each study are summarized in Table 3. Among them, six studies compared clinical or radiological outcomes between two rehabilitation protocols: AR and NR. In contrast, in the study by Zhu et al., three different rehabilitation protocols were used, and patients were divided into three groups (A, B, and C) [32]. After reviewing the three rehabilitation protocols, we classified group A into the NR group and groups B and C into the AR group.
Table 2.
Summary of the Included Studies
| Authors | Journal (year) | Study design | No. of cases | FU period | Age, years | Graft bundle | Technique(femoral tunnel) | Fixation | Treatment for meniscal lesions | Outcome parameters |
|---|---|---|---|---|---|---|---|---|---|---|
| Murty et al | Knee (2001) | RCS |
AR: 14 NR: 14 |
12 months |
AR: 30.1 NR: 33.1 |
SB | Extra-articular tunnel |
F: Staple T: Pull-out suture |
AR: MS 7, MR 0 NR: MS 8, MR 1 |
STSD, Lachman test, effusion, Tegner activity score, tunnel enlargement (T) |
| Majima et al | CORR (2002) | PCS |
AR: 32 NR: 30 |
AR: mean 43.5 months NR: mean 43.2 months |
AR: 25.9 NR: 24.5 |
SB | Transportal |
F: Double staple T: Double staple |
AR: MS 7, MR 4 NR: MS 4, MR 4 |
STSD, IKDC grade, effusion, IKDC activity level, muscle toque (Q/H) |
| Yu et al | Chin Med J (2005) | RCS |
AR: 33 NR: 32 |
6 months |
AR: 31.2 NR: 30.3 |
SB | Transportal |
F: Tendon node fixation to the bottle neck T: Bone bridge fixation by suture |
AR: no MRs NR: with MR but no number of cases described |
STSD, tunnel enlargement (T) |
| Vadala et al | KSSTA (2007) | RCT |
AR: 20 NR: 25 |
Mean 10 months |
AR: 29 NR: 30 |
SB | Outside-in |
F: CSD T: Interference screw |
AR: MS 5, MR 0 NR: MS 8, MR 0 |
Tunnel enlargement (F/T) |
| Christensen et al |
J Sport Rehabil (2013) |
RCT |
AR: 19 NR: 17 |
1, 12, and 24 weeks |
AR: 30.1 NR: 33.1 |
SB | Transportal |
F: CSD T: Interference screw |
Meniscal tears of > 5 mm were excluded |
STSD, IKDC subjective score, ROM, peak isometric force (Q) |
| Zhu et al | EJOST (2013) | RCT |
AR (groups B and C): 30 NR (group A): 15 |
3, 6, and 12 months | ND | ND | ND |
F: CSD T: Interference screw |
AR: no MR NR: no MR |
ROM, IKDC subjective score, thigh muscle atrophy, tunnel enlargement (F/T) |
| Gupta et al | JAJS (2017) | RCT |
AR: 20 NR: 20 |
6 weeks 3 and 6 months |
AR: 26.5 NR: 28.9 |
SB | ND |
F: CSD T: Interference screw |
No difference in the incidence of meniscal tears between groups | Lachman test, pivot shift test, IKDC subjective score, KOOS, Tegner activity score, single-leg hop test |
CORR: Clinical Orthopaedics and Related Research; Chin Med J: Chinese Medical Journal; KSSTA: Knee Surgery: Sports Traumatology, Arthroscopy; J Sport Rehabil: Journal of Sport Rehabilitation; EJOST: European Journal of Orthopaedic Surgery and Traumatology; JAJS: Journal of Arthroscopy and Joint Surgery
RCT randomized controlled trial, RCS retrospective comparative study, PCS prospective comparative study, FU follow-up, AR accelerated rehabilitation, NR non-accelerated rehabilitation, SB single-bundle, STSD side-to-side difference, F femoral tunnel, T tibial tunnel, MS meniscectomy, MR meniscus repair, Q quadriceps muscle, H hamstring muscle, CSD cortical suspensory device, ND not described, IKDC International Knee Documentation Committee, KOOS Knee Injury and Osteoarthritis Outcome Score, ROM range of motion
Table 3.
Rehabilitation protocol of the included studies
| Authors (publication year) | Group | Range of motion | Weight-bearing | Return to sports |
|---|---|---|---|---|
| Murty et al. (2001) | AR | ROM start after 2 days (5°–90°) | PWB from 2 days, increasing as tolerable | ND |
| NR | Immobilization at 50° flexion for 2 weeks | NWB for 2 weeks, FWB from 2 weeks | ND | |
| Majima et al. (2002) | AR | Immediate (0°–90°) | Immediate full as tolerable | 7–9 months |
| NR | Start after 1 week (0°–90°) | PWB from 2 weeks, FWB after 4 weeks | 12 months | |
| Yu et al. (2005) | AR | Full ROM within 4 weeks | Immediate FWB | 6 months |
| NR | 0°–90° for 6 weeks, full ROM from 6 weeks | PWB for 6 weeks, FWB after 6 weeks | 6 months | |
| Vadala et al. (2007) | AR | Immediate | Progressive weight-bearing as tolerated | 4–6 months |
| NR | Start after 2 weeks | Progressive weight-bearing as tolerated | 4–6 months | |
| Christensen et al. (2013) | AR | Immediate | Immediate full as tolerable | 6 months |
| NR | Start after 1 week (10°–120°) | PWB for 2 weeks, FWB after 2 weeks | 6 months | |
| Zhu et al. (2013) | AR (group B) | 0°–90° for 1 week, 10° increased per week, nearly normal after 4 weeks | PWB for 2 weeks, FWB for 2 weeks | 3 months |
| AR (group C) | 0°–90° for 2 weeks, 10° increased per week, nearly normal after 8 weeks | PWB after 2 weeks, FWB after 4 weeks | 6 months | |
| NR (group A) | 0°–60° for 4 weeks, > 90° after 8 weeks, normal after 12 weeks | NWB for 4 weeks, PWB for 8 weeks, FWB for 12 weeks | 12 months | |
| Gupta et al. (2017) | AR | Immediate, full ROM after 3 weeks | NWB for 1 week, FWB after 1 week | ND |
| NR | Start after 1 week, full ROM after 7 weeks | NWB for 1 week, PWB after 1 week, FWB after 3 weeks | ND |
AR accelerated rehabilitation, NR non-accelerated rehabilitation, ROM range of motion, PWB partial weight-bearing, FWB full weight-bearing, NWB non-weight-bearing, ND not described
Of the included articles, four were randomized controlled studies, and one was a prospective comparative study. The two remaining studies were retrospective comparative studies. The mean follow-up duration was 6 months in three studies, 10–12 months in three studies, and 43 months in the remaining study (Table 2).
The results of the risk of bias assessment are summarized in Tables 4 and 5. Therein, all randomized controlled trials had an overall low risk of bias as assessed using the RoB 2 tool (Table 4). Meanwhile, the other non-randomized studies had an overall moderate risk of bias as assessed using the ROBINS-I tool (Table 5).
Table 4.
Risk of bias assessment for randomized controlled trials using the risk of bias 2 tool
| Study (publication year) | Randomization | Intended interventions | Missing data | Measurement of outcome | Reported result | Overall |
|---|---|---|---|---|---|---|
| Vadala et al. (2007) | Low | Low | Low | Low | Low | Low |
| Christensen et al. (2013) | Low | Low | Low | Low | Low | Low |
| Zhu et al. (2013) | Low | Low | Low | Low | Low | Low |
| Gupta et al. (2017) | Low | Low | Low | Low | Low | Low |
Table 5.
Risk of bias assessment for non-randomized studies using the risk of bias in non-randomized studies of interventions tool
| Study (publication year) | Confounding | Selection bias | Classification of interventions | Intended intervention | Missing data | Measurement of outcomes | Reported result | Overall bias |
|---|---|---|---|---|---|---|---|---|
| Murty et al. (2001) | Low | Moderate | Moderate | Low | Low | Low | Low | Moderate |
| Majima et al. (2002) | Low | Moderate | Low | Low | Low | Low | Low | Moderate |
| Yu et al. (2005) | Moderate | Moderate | Low | Moderate | Low | Moderate | Low | Moderate |
International Knee Documentation Committee Subjective Score
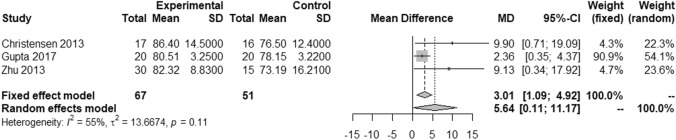
Among the seven included studies, we were able to separately retrieve data on the IKDC subjective scores of the AR and NR groups at the 3- and 6-month follow-ups in three studies [18, 19, 32]. There were 67 cases in the AR group and 51 cases in the NR group. The IKDC subjective score was used in three studies in which pooled data showed a higher score in the AR group than in the NR group by 7.30 points at the 3-month follow-up. The difference was significant (95% confidence interval [CI] 1.55–13.05; P = 0.013; I2 = 73%) (Fig. 2).
Fig. 2.
Forest plots of studies reporting the IKDC subjective scores after accelerated and non-accelerated rehabilitation after anterior cruciate ligament reconstruction using hamstring autografts at the 3-month follow-up. Squares represent the mean IKDC subjective score, with the size of the square being proportional to the sample size. Experimental and control indicate the accelerated and non-accelerated rehabilitation groups, respectively. IKDC International Knee Documentation Committee, SD standard deviation, MD mean difference, CI confidence interval
The IKDC subjective score was used in three studies in which pooled data showed a higher score in the AR group than in the NR group by 5.64 points at the 6-month follow-up. The difference was also significant (95% CI 0.11–11.17; P = 0.046; I2 = 55%) (Fig. 3).
Fig. 3.
Forest plots of studies reporting the IKDC subjective scores after accelerated and non-accelerated rehabilitation after anterior cruciate ligament reconstruction using hamstring autografts at the 6-month follow-up. Squares represent the mean IKDC subjective score, with the size of the square being proportional to the sample size. Experimental and control indicate the accelerated and non-accelerated rehabilitation groups, respectively. IKDC International Knee Documentation Committee, SD standard deviation, MD mean difference, CI confidence interval
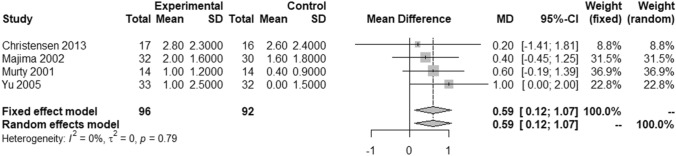
Side-to-side Difference in Anterior Tibial Translation
Four studies were included in the analysis of the STSD in anterior tibial translation at the final follow-up [18, 20, 21, 30]. The follow-up period varied from 6 to 43 months among the studies. The STSD in anterior tibial translation was significantly lower in the NR group than in the AR group (mean difference [MD] 0.59; 95% CI 0.12–1.07; P = 0.015; I2 = 0%) (Fig. 4).
Fig. 4.
Forest plots of studies reporting the side-to-side difference after accelerated and non-accelerated rehabilitation after anterior cruciate ligament reconstruction using hamstring autografts at the final follow-up. Squares represent the mean side-to-side difference, with the size of the square being proportional to the sample size. Experimental and control indicate the accelerated and non-accelerated rehabilitation groups, respectively. SD standard deviation, MD mean difference, CI confidence interval
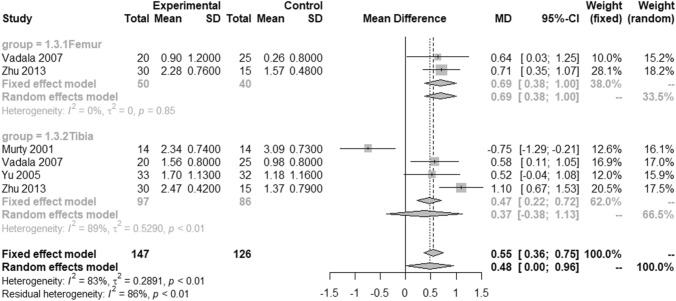
Tunnel Widening (Femoral and Tibial Tunnels)
Four studies reported tunnel widening at the final follow-up [20, 21, 31, 32]. The follow-up periods varied from 6 to 12 months among the studies. An analysis of the overall widening of the femoral or tibial tunnel was performed, followed by a subgroup analysis of the widening of each tunnel.
The overall increase in the femoral or tibial tunnel diameters observed in the AR group was significantly greater than that observed in the NR group (MD 0.48; 95% CI 0.00–0.96; P = 0.0479; I2 = 83%) (Fig. 5).
Fig. 5.
Forest plots of studies reporting widening of the femoral and tibial tunnels after accelerated and non-accelerated rehabilitation after anterior cruciate ligament reconstruction using hamstring autografts at the final follow-up. Squares represent the mean increment for the femoral and tibial tunnels, with the size of the square being proportional to the sample size. Experimental and control indicate the accelerated and non-accelerated rehabilitation groups, respectively. SD standard deviation, MD mean difference, CI confidence interval
Two studies were included in the analysis of the widening of the femoral tunnel at the final follow-up [31, 32]. In these studies, pooled data on femoral tunnel widening showed a greater increase in the AR group than in the NR group by 0.69 mm at the final follow-up. The difference was significant (95% CI 0.38–1.00; P < 0.0001; I2 = 0%) (Fig. 5).
Four studies were included in the analysis of the widening of the tibial tunnel at the final follow-up [20, 21, 31, 32]. In these studies, pooled data on tibial tunnel widening showed a greater increase in the AR group than in the NR group by 0.37 mm at the final follow-up. However, the difference was not significant (95% CI − 0.38 to 1.13; P = 0.446; I2 = 89%) (Fig. 5).
Discussion
The most important finding of this study was that the IKDC subjective score at 3 and 6 months was significantly higher in the AR group than in the NR group. This meta-analysis also showed that the STSD in anterior tibial translation and overall tunnel widening in the AR group were significantly larger than those in the NR group at the final follow-up. However, the difference in the STSD in anterior tibial translation and overall tunnel widening between the two groups was 0.59 mm and 0.48 mm, respectively. These results were not considered to be clinically relevant.
To the best of our knowledge, this is the first meta-analysis to compare the clinical and radiological outcomes between AR and NR after ACLR using hamstring autografts. This study only included studies comparing AR and NR after ACLR using hamstring autografts. Recently, Janssen et al. conducted a systematic review of the clinical outcomes of AR after ACLR using hamstring autografts [22]. They performed a best-evidence synthesis to integrate the results of previous studies and reported that brace-free AR after ACLR using hamstring autografts did not alter the clinical outcomes, including clinical scores and knee laxity (“moderate” level of evidence). Our meta-analysis also showed that there was < 1-mm difference in the STSD in anterior tibial translation between the groups. However, in this study, the IKDC subjective scores at the 3- and 6-month follow-ups were significantly higher in the AR group than in the NR group.
Among the included studies, three reported the IKDC subjective scores, with a slightly different follow-up period among the studies. All three studies reported the IKDC subjective scores at the 3- and 6-month follow-ups after ACLR, which was probably because AR usually aims to allow return to sports by 6 months after surgery. This meta-analysis then revealed that the AR group had higher IKDC subjective scores than the NR group at the 3- and 6-month follow-ups. These findings suggest that AR improved the subjective outcomes earlier in patients who underwent ACLR using hamstring autografts, which can be considered a rationale for an early return to sports.
A recent systematic review demonstrated that femoral and tibial tunnel widening occurred after ACLR using a hamstring tendon autograft and accelerated brace-free rehabilitation [22]. This meta-analysis also showed that the increase in the femoral and tibial tunnel diameters in the AR group was significantly greater than that in the NR group. Previous studies have shown that tunnel widening was significantly greater after ACLR using hamstring autografts than after ACLR using BPTB autografts [33–35]. Cortical suspensory devices used for hamstring graft fixation have been reported to be susceptible to longitudinal (bungee effect) and sagittal motions (windshield wiper effect) because of the distance between the graft and the point of fixation [36, 37]. Moreover, a previous animal study has reported that histological healing of grafts after ACLR was attained by 12 weeks for tendon–bone grafts and by 8 weeks for bone–bone grafts [38]. Therefore, graft motions might be increased by early AR before graft healing is completed, which results in greater tunnel widening after ACLR using hamstring autografts.
However, the MD in the tunnel widening between the AR and NR groups was < 1 mm in this meta-analysis. The subgroup analysis also showed that the MD in the femoral and tibial tunnel widening was 0.69 mm and 0.37 mm, respectively. Although there was a significant difference found in the overall tunnel widening between the two rehabilitation protocols, the difference did not seem to be clinically significant. Therefore, the statistical difference should not be clinically overestimated. Further studies are then required to verify the criteria for clinically relevant tunnel widening.
The same consideration should be applied when interpreting the differences in the STSD in anterior tibial translation between the two rehabilitation protocols. Although the STSD in anterior tibial translation was significantly lower in the NR group than in the AR group, the MD was only 0.59 mm. Previous studies that investigated anterior instability after ACLR have set the clinically significant difference in the STSD in anterior tibial translation to 1 mm [39, 40]. This result is consistent with the small difference found in the STSD in anterior tibial translation. Therefore, the statistical difference in the STSD in anterior tibial translation in this meta-analysis should not be overestimated clinically.
This meta-analysis has some limitations. First, only seven studies with a total of 321 patients were included. Moreover, only three studies were included in the analysis of the IKDC subjective scores as the primary outcome of interest. Therefore, the reliability of the results may be limited by the small sample size. Second, the follow-up periods in the meta-analysis of the IKDC subjective scores were relatively short (3 and 6 months). Nevertheless, these seem to be sufficient to confirm the effectiveness of AR because the aim of the AR protocol is to allow the return to sports within 6 months. Third, each study evaluated the outcome parameters at different follow-up periods (STSD, 6–43 months; tunnel widening, 6–12 months). However, previous studies have reported that tunnel widening mainly occurred within 6 months after ACLR and that no further significant increase occurred thereafter [41, 42]. In addition, Howell et al. reported that the signal of hamstring autografts on serial magnetic resonance imaging was well established by 3 months and remained unchanged at 1 year [43]. Therefore, we decided to perform a meta-analysis of the results at different follow-up periods. Finally, each study used slightly different rehabilitation methods. To solve this problem, we defined common AR and NR protocols before the study and enrolled studies according to these criteria.
Conclusions
This systematic review and meta-analysis indicated that the early subjective clinical outcomes of AR after ACLR using hamstring autografts were superior to those of NR. Although tunnel widening and anterior instability were also significantly larger in the AR group than in the NR group, the difference was not clinically relevant.
Funding
There is no funding source.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not require ethical approval because it is a meta-analysis of previous studies.
Informed consent
Not applicable for this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sang-Gyun Kim and Dae Hee Lee contributed equally to this work and should be considered co-corresponding authors.
Contributor Information
Jae Gyoon Kim, Email: gowest99@naver.com.
Won Seok Kim, Email: znzooozf@naver.com.
Sang-Gyun Kim, Email: mup81@hotmail.com.
Dae Hee Lee, Email: eoak22@empal.com.
References
- 1.Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25:192–199. doi: 10.1007/s00167-016-4246-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Melick N, van Cingel RE, Brooijmans F, Neeter C, van Tienen T, Hullegie W, Nijhuis-van der Sanden MW. Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. British Journal of Sports Medicine. 2016;50:1506–1515. doi: 10.1136/bjsports-2015-095898. [DOI] [PubMed] [Google Scholar]
- 3.Wright RW, Haas AK, Anderson J, Calabrese G, Cavanaugh J, Hewett TE, Lorring D, McKenzie C, Preston E, Williams G. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2015;7:239–243. doi: 10.1177/1941738113517855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surgery & Related Research. 2013;25:165. doi: 10.5792/ksrr.2013.25.4.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Makhni EC, Crump EK, Steinhaus ME, Verma NN, Ahmad CS, Cole BJ, Bach BR., Jr Quality and variability of online available physical therapy protocols from academic orthopaedic surgery programs for anterior cruciate ligament reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016;32:1612–1621. doi: 10.1016/j.arthro.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 6.Wright RW, Preston E, Fleming BC, Amendola A, Andrish JT, Bergfeld JA, Dunn WR, Kaeding C, Kuhn JE, Marx RG. A systematic review of anterior cruciate ligament reconstruction rehabilitation–part I: Continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. Journal of Knee Surgery. 2008;21:217–224. doi: 10.1055/s-0030-1247822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 1990;18:292–299. doi: 10.1177/036354659001800313. [DOI] [PubMed] [Google Scholar]
- 8.Shelbourne KD, Klootwyk TE, Decarlo MS. Update on accelerated rehabilitation after anterior cruciate ligament reconstruction. Journal of Orthopaedic & Sports Physical Therapy. 1992;15:303–308. doi: 10.2519/jospt.1992.15.6.303. [DOI] [PubMed] [Google Scholar]
- 9.Decarlo MS, Shelbourne KD, McCarroll JR, Rettig AC. Traditional versus accelerated rehabilitation following ACL reconstruction: A one-year follow-up. Journal of Orthopaedic & Sports Physical Therapy. 1992;15:309–316. doi: 10.2519/jospt.1992.15.6.309. [DOI] [PubMed] [Google Scholar]
- 10.Draper V, Ladd C. Subjective evaluation of function following moderately accelerated rehabilitation of anterior cruciate ligament reconstructed knees. Journal of Athletic Training. 1993;28:38–41. [PMC free article] [PubMed] [Google Scholar]
- 11.Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. American Journal of Sports Medicine. 1997;25:786–795. doi: 10.1177/036354659702500610. [DOI] [PubMed] [Google Scholar]
- 12.Shelbourne KD, Klootwyk TE, Wilckens JH, De Carlo MS. Ligament stability two to six years after anterior cruciate ligament reconstruction with autogenous patellar tendon graft and participation in accelerated rehabilitation program. American Journal of Sports Medicine. 1995;23:575–579. doi: 10.1177/036354659502300510. [DOI] [PubMed] [Google Scholar]
- 13.Budny J, Fox J, Rauh M, Fineberg M. Emerging trends in anterior cruciate ligament reconstruction. Journal of Knee Surgery. 2017;30:63–69. doi: 10.1055/s-0036-1579788. [DOI] [PubMed] [Google Scholar]
- 14.Hardy A, Casabianca L, Andrieu K, Baverel L, Noailles T. Complications following harvesting of patellar tendon or hamstring tendon grafts for anterior cruciate ligament reconstruction: Systematic review of literature. Orthopaedics & Traumatology: Surgery & Research. 2017;103:S245–S248. doi: 10.1016/j.otsr.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Seo S-S, Kim C-W, Nam T-S, Choi S-Y. ACL reconstruction with autologous hamstring tendon: Comparison of short term clinical results between Rigid-fix and PINN-ACL cross pin. Knee surgery & related research. 2011;23:208. doi: 10.5792/ksrr.2011.23.4.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kyung H-S, Baek S-G, Lee B-J, Lee C-H. Single-bundle anterior cruciate ligament reconstruction with semitendinosus tendon using the PINN-ACL CrossPin system: Minimum 4-year follow-up. Knee Surgery & Related Research. 2015;27:43. doi: 10.5792/ksrr.2015.27.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu H, Chen C, Xie S, Tang Y, Qu J. Tendon healing in bone tunnel after human anterior cruciate ligament reconstruction: A systematic review of histological results. Journal of Knee Surgery. 2019;32:454–462. doi: 10.1055/s-0038-1653964. [DOI] [PubMed] [Google Scholar]
- 18.Christensen JC, Goldfine LR, West HS. The effects of early aggressive rehabilitation on outcomes after anterior cruciate ligament reconstruction using autologous hamstring tendon: A randomized clinical trial. Journal of Sport Rehabilitation. 2013;22:191–201. doi: 10.1123/jsr.22.3.191. [DOI] [PubMed] [Google Scholar]
- 19.Gupta PK, Acharya A, Mourya A, Ameriya D. Role of accelerated rehabilitation versus standard rehabilitation following anterior cruciate ligament reconstruction using hamstring graft. Journal of Arthroscopy and Joint Surgery. 2017;4:89–93. [Google Scholar]
- 20.Murty AN, el Zebdeh MY, Ireland J. Tibial tunnel enlargement following anterior cruciate reconstruction: Does post-operative immobilisation make a difference? The Knee. 2001;8:39–43. doi: 10.1016/s0968-0160(01)00064-3. [DOI] [PubMed] [Google Scholar]
- 21.Yu JK, Paessler HH. Relationship between tunnel widening and different rehabilitation procedures after anterior cruciate ligament reconstruction with quadrupled hamstring tendons. Chinese Medical Journal (England) 2005;118:320–326. [PubMed] [Google Scholar]
- 22.Janssen RPA, van Melick N, van Mourik JBA, Reijman M, van Rhijn LW. ACL reconstruction with hamstring tendon autograft and accelerated brace-free rehabilitation: A systematic review of clinical outcomes. BMJ Open Sport & Exercise Medicine. 2018;4:e000301. doi: 10.1136/bmjsem-2017-000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 24.Grant JA. Updating recommendations for rehabilitation after ACL reconstruction: A review. Clinical Journal of Sport Medicine. 2013;23:501–502. doi: 10.1097/JSM.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 25.Kruse LM, Gray B, Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: A systematic review. The Journal of Bone and Joint Surgery American. 2012;94:1737–1748. doi: 10.2106/JBJS.K.01246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sterne, J. A., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H.-Y., Corbett, M. S., & Eldridge, S. M. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. The BMJ,366, l4898. [DOI] [PubMed]
- 27.Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., & Boutron, I. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. The BMJ,355, i4919. [DOI] [PMC free article] [PubMed]
- 28.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. New York: John Wiley & Sons; 2011. [Google Scholar]
- 30.Majima T, Yasuda K, Tago H, Tanabe Y, Minami A. Rehabilitation after hamstring anterior cruciate ligament reconstruction. Clinical Orthopaedics and Related Research. 2002;397:370–380. doi: 10.1097/00003086-200204000-00043. [DOI] [PubMed] [Google Scholar]
- 31.Vadala A, Iorio R, De Carli A, Argento G, Di Sanzo V, Conteduca F, Ferretti A. The effect of accelerated, brace free, rehabilitation on bone tunnel enlargement after ACL reconstruction using hamstring tendons: A CT study. Knee Surgery, Sports Traumatology, Arthroscopy. 2007;15:365–371. doi: 10.1007/s00167-006-0219-2. [DOI] [PubMed] [Google Scholar]
- 32.Zhu W, Wang D, Han Y, Zhang N, Zeng Y. Anterior cruciate ligament (ACL) autograft reconstruction with hamstring tendons: Clinical research among three rehabilitation procedures. European Journal of Orthopaedic Surgery & Traumatology. 2013;23:939–943. doi: 10.1007/s00590-012-1106-9. [DOI] [PubMed] [Google Scholar]
- 33.Clatworthy M, Annear P, Bulow J-U, Bartlett R. Tunnel widening in anterior cruciate ligament reconstruction: A prospective evaluation of hamstring and patella tendon grafts. Knee Surgery, Sports Traumatology, Arthroscopy. 1999;7:138–145. doi: 10.1007/s001670050138. [DOI] [PubMed] [Google Scholar]
- 34.L’Insalata JC, Klatt B, Fu FH, Harner CD. Tunnel expansion following anterior cruciate ligament reconstruction: A comparison of hamstring and patellar tendon autografts. Knee Surgery, Sports Traumatology, Arthroscopy. 1997;5:234–238. doi: 10.1007/s001670050056. [DOI] [PubMed] [Google Scholar]
- 35.Webster K, Feller J, Hameister K. Bone tunnel enlargement following anterior cruciate ligament reconstruction: A randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surgery, Sports Traumatology, Arthroscopy. 2001;9:86–91. doi: 10.1007/s001670100191. [DOI] [PubMed] [Google Scholar]
- 36.Höher J, Livesay GA, Ma CB, Withrow JD, Fu FH, Woo SL. Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surgery, Sports Traumatology, Arthroscopy. 1999;7:215–219. doi: 10.1007/s001670050151. [DOI] [PubMed] [Google Scholar]
- 37.Saccomanno MF, Shin JJ, Mascarenhas R, Haro M, Verma NN, Cole BJ, Bach BR., Jr Clinical and functional outcomes after anterior cruciate ligament reconstruction using cortical button fixation versus transfemoral suspensory fixation: A systematic review of randomized controlled trials. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014;30:1491–1498. doi: 10.1016/j.arthro.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 38.Park M, Lee MC, Seong S. A comparative study of the healing of tendon autograft and tendon-bone autograft using patellar tendon in rabbits. International Orthopaedics. 2001;25:35–39. doi: 10.1007/s002640000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N. Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. American Journal of Sports Medicine. 2010;38:25–34. doi: 10.1177/0363546509347096. [DOI] [PubMed] [Google Scholar]
- 40.Trichine F, Chouteau J, Moyen B, Bouzitouna M, Maza R. Patellar tendon autograft reconstruction of the anterior cruciate ligament with and without lateral plasty in advanced-stage chronic laxity. A clinical, prospective, randomized, single-blind study using passive dynamic X-rays. The Knee. 2014;21:58–65. doi: 10.1016/j.knee.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 41.Harris NL, Indelicato PA, Bloomberg MS, Meister K, Wheeler DL. Radiographic and histologic analysis of the tibial tunnel after allograft anterior cruciate ligament reconstruction in goats. American Journal of Sports Medicine. 2002;30:368–373. doi: 10.1177/03635465020300031101. [DOI] [PubMed] [Google Scholar]
- 42.Chen B, Sun R, Wang X, Shao D, Lu B, Chen J. The incidence and variation of tunnel enlargement after anterior cruciate ligament reconstruction. Chinese Journal of Surgery. 2007;45:78–81. [PubMed] [Google Scholar]
- 43.Howell SM, Clark JA, Blasier RD. Serial magnetic resonance imaging of hamstring anterior cruciate ligament autografts during the first year of implantation: A preliminary study. American Journal of Sports Medicine. 1991;19:42–47. doi: 10.1177/036354659101900107. [DOI] [PubMed] [Google Scholar]