Abstract
Background
Anatomical placement of an ACL graft is critical to the clinical outcome of an ACL reconstruction. The purpose of the study was to compare the conventional technique of drilling a femoral tunnel from a medial portal while viewing it from a lateral portal versus viewing it from a high anteromedial portal and drilling it from a low medial portal. We hypothesized that the high anteromedial portal possibly provides an end-on view of the tunnel and would lead to a more favourable tunnel position.
Materials and Methods
Sixty patients underwent arthroscopic single-bundle ACL reconstruction with a soft tissue graft. All patients had the same surgeon and same surgical technique (except viewing portal). Each patient underwent a 3D-CT 1-week post-op. We classified the patients into two groups (technique A and B) of 30 each. Postoperative tunnel position in each patient was visualized on CT scan with 3D reconstruction by the quadrant method described by Bernard et al. The distance of the centre of the femoral tunnel from the superior and posterior border of the Bernard frame was obtained in each patient of the two groups and mean value in each group was obtained and compared by Student ‘t’ test at 5% level of significance. The position of the femoral tunnels was also studied in reference to the lateral intercondylar ridge and classified into type I (well placed), type II (moderately malpositioned) and type III (grossly malpositioned)
Results
The mean distances in technique A from the posterior and superior border of the lateral femoral condyle was 35.8 ± 8.2 and 35.2 ± 6.7, and in technique B was 38.1 ± 8.6 and 35.8 ± 9.4. The two groups did not differ significantly (P > 0.05) in femoral tunnel position as visualized on 3D-CT scan postoperatively. 53.3% patients had well-placed tunnels (type I) overall with 56.67% of technique A and 50% of technique B in this group. None of the tunnels were grossly malpositioned.
Conclusions
The absence of any statistically significant difference between the groups suggests that a high anterolateral portal close to the patellar tendon gives an almost complete view of the lateral aspect of the notch, if not end on. Both techniques produced a majority of well placed (type I) tunnels
Keywords: Femoral tunnel, Portal, Quadrant method, Patellar tendon, Notch
Introduction
Anterior cruciate ligament (ACL) injury comprises between 40 and 50% of all knee ligament injuries [1]. Mechanism of injury is typically a valgus load with internal tibial rotation and anterior tibial translation while the knee is in almost full extension. Arthroscopic single-bundle ACL reconstruction is the standard treatment for ACL tears. Anatomical placement of the ACL graft is critical to the clinical outcome of the ACL reconstruction. Anatomical ACL graft placement is defined as positioning the ACL femoral and tibial tunnel at the centre of the native ACL femoral and tibial attachment sites. Visualising the actual femoral footprint may be possible in fresh cases. However, in chronic ACL tears visualising the exact footprint may not be possible and we rely on bony landmarks in the lateral aspect of the notch. There is no consensus as to the ideal position of the femoral tunnel when the actual anatomical footprint is not seen clearly. However, the femoral tunnel that is posterior and inferior to the lateral intercondylar ridge is accepted as being well placed [2]. There are various methods described to identify the location of the femoral tunnel. The landmark used here was 5 mm from the posterior articular margin and 5 mm from the inferior margin as described by Peterson and Zantop [3].
The transportal technique has been shown to be more anatomical when compared to the transtibial technique. Graft placement by this method controls the rotational stability of the knee better. Non-anatomical femoral tunnel placement is the most common cause of failure with regards to pain and instability post ACL surgery.
Only two studies in the past have focussed on viewing the notch in a more end on position via a medial/central portal while drilling the femoral tunnel [4, 5]. These techniques were described to improve the accuracy and predictability of the femoral tunnel placement. However, these studies did not use any objective methods or measurement using imaging to study whether their technique produced more accurate or predictable femoral tunnels as compared to the technique of viewing through the lateral portal. This study intends to be clinically relevant by analysing the overall femoral tunnel placement in relation to the lateral intercondylar ridge that is taken as a landmark for appropriate femoral tunnel placement. No previous study has compared these two techniques for drilling the femoral tunnel. The conventional transportal ACL reconstruction (technique A) involves viewing from a high anterolateral portal and working from a far medial portal. However, looking at the lateral aspect of the notch is not end on in this technique. In the modified technique (technique B) described in the study, an additional anteromedial portal allows the ACL femoral attachment to be viewed end on, while working instrumentation is inserted into the notch, through a far medial portal.
The purpose of the study was to compare the femoral tunnel position by the two techniques A and B on a 3D CT image.
Materials and Methods
This is a pilot study comprising of 60 patients who underwent arthroscopic ACL reconstruction between Nov 2017 and Oct 2018 and followed till Nov 2018. Clinical examination and an MRI diagnosed with the ACL rupture. Patients with multiligamentous knee injuries, ACL with tibial avulsion, osteoarthritis knee, previous femoral fractures, and congenital femoral abnormalities were excluded from the study. Our inclusion criteria were single-bundle ACL reconstruction in complete ACL tear with soft tissue grafts utilizing the same graft fixation method. Randomization was done by the flip of a coin in the operation theatre, done by the attending anaesthetist just before the commencement of the surgery. Heads meant technique A and tails technique B. Patients were divided into two groups of 30 each. In technique A the standard anterolateral portal was used as a viewing portal and a far medial portal for drilling the femoral tunnel. In technique B a high anteromedial portal was used as a viewing portal and a far medial portal for drilling the femoral tunnel (Fig. 1).
Fig. 1.

Position of portals, high anteromedical portals, far medical portal, anterolateral portal
Surgical Technique
The patient was positioned supine on an operating table with the affected knee in 70° of flexion. A tourniquet was applied on the upper thigh. Semitendinosus and gracils grafts were harvested from the ipsilateral knee and prepared as a four tailed graft. The graft was fixed with an Endobutton (Smith and Nephew, UK) on the femur and a PEEK screw (Smith and Nephew, UK) on the tibia. In both the techniques the intercondylar notch area was firstly cleaned with the help of shaver to properly visualize the lateral aspect of the notch and bony landmarks. The over the top position was marked. The surgeon intended to drill the tunnel at a distance of 5 mm from the posterior articular margin and 5 mm from the inferior margin of the lateral aspect of the notch. The Obama ruler (Smith and Nephew, UK) was introduced through the anterolateral portal and visualized from the anteromedial portal. The desired femoral tunnel position was marked with a bone awl introduced through the far medial portal (Fig. 2). After which the femoral tunnel was drilled (Figs. 3, 4).
Fig. 2.

Lateral wall of femoral notch view of making an impression with a bone awl for the femoral entry points. a Technique B. b Technique A
Fig. 3.

a Technique B: AM viewing portal with far medical working portal. b Technique A: AL viewing portal with far medical working portal
Fig. 4.
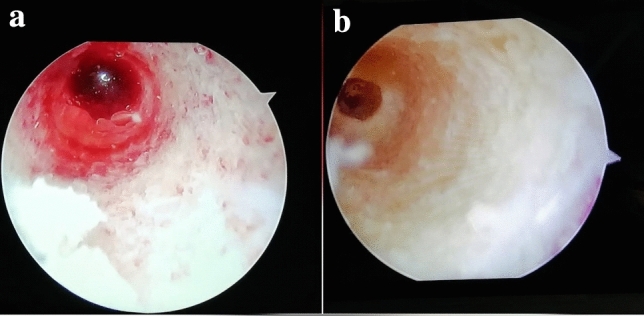
Femoral tunnel view after differential drilling. a Technique B. b Technique A
Portal Placement
The anterolateral (AL) portal was a 1 cm vertical portal made at the level of the inferior pole of patella close to the lateral border of the patellar tendon and just abutting against it. The high anteromedial (AM) portal was also a 1 cm vertical portal made just medial to the patellar tendon and abutting it at the level of the inferior pole of the patella. The higher position of this portal avoids overcrowding of instruments while working from the far medial portal (Fig. 5). The far medial portal position is decided after introducing a spinal needle under vision, just above the medial meniscus and avoiding any contact with the medial condyle of the femur with the knee in 100° of flexion.
Fig. 5.

Showing over 3 cm distance between high anteromedial and far medial portal
Postoperative 3D-CT Evaluation of Patients
Postoperatively all patients underwent 3D-CT within a week of arthroscopy. The femoral tunnel position was evaluated. A true lateral view of the medial wall of the lateral condyle with neutral rotation was reconstructed and the medial condyle subtracted to see the lateral wall of the notch.
The femoral tunnel position was evaluated on a 3D CT image using the quadrant method by Bernard et al. [6] A reference frame was drawn with the superior border at the Blumensaat’s line of the intercondylar notch and inferior border at the lowest margin of the lateral wall of the intercondylar notch. The anterior and posterior borders of the frame were drawn touching the anterior-most and posterior-most points of the lateral wall of the intercondylar notch respectively. The footprint was covered by the best fit circle using the region of interest tool (ROI) in the CT software that covered all borders of the femoral tunnel. The centre of the circle was marked and perpendiculars from the centre of the circle to the length and breadth of the rectangle were drawn. The distance of the centre of the tunnel with all four sides measured. DS represented the distance of the tunnel from the superior border and DP represented the distance from the posterior border. The mean of DP and DS distance in both groups were obtained and compared (Fig. 6). The individual tunnels were also categorised according to their relationship with the lateral intercondylar ridge. Type 1 (well placed) tunnels were those located posterior and inferior to the lateral intercondylar ridge, type II (slightly mal-positioned) were those that overlapped the intercondylar ridge and type III (grossly mal-positioned) were those located superior and anterior to the ridge [6].
Fig. 6.

Distance measurement technique described by Pisit et al. and Bernad et al.
Results
Sixty knees were evaluated 52 right (technique A: 27 and technique B: 25) and 8 left knees (technique A: 3 and technique B:5). The mean age of the patients was 27.3 years (technique A: 26.7 years (19–41 years) and technique B 27.6 years (18–43 years). There were 41 male and 19 female patients (technique A 18 males and 12 females, technique B had 23 males and 7 females).
The distance of the centre of the femoral tunnel from the superior and posterior border of the Bernard frame was obtained in each patient of the two groups. The mean value in each group was obtained and compared by Student t test at 5% level of significance (Tables 1, 2, 3, 4) (Figs. 7, 8).
Table 1.
Mean distance (DS) of the femoral footprint from superior border described in percentage ratio in both techniques
| Technique | No of cases | Mean | Standard deviation | |
|---|---|---|---|---|
| DS | A | 30 | 35.28 | 6.7339 |
| B | 30 | 35.86 | 9.4441 |
Table 2.
Independent sample test (DS result)
| ‘t’ Test for equality of means | Df | P value | Mean difference | Standard error difference | 95% Confidence interval of difference | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Equal variance assumed | 0.2767 | 58 | 0.783 | −0.586 | 2.118 | −4.825 | 3.653 |
The t value for DS calculated is 0.2767, the P value is 0.7830 and confidence interval is (−4.825, 3.653)
Table 3.
Mean distance (DP) of the femoral footprint from posterior border described in percentage ratio in both techniques
| Technique | No of cases | Mean | Standard deviation | |
|---|---|---|---|---|
| DP | A | 30 | 35.83 | 8.2008 |
| B | 30 | 38.14 | 8.6991 |
Table 4.
Independent sample test (DP result)
| ‘t’ Test for equality of means T | df | P value | Mean difference | Standard error difference | 95% Confidence interval of the difference | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Equal variance assumed | 1.06 | 58 | 0.2937 | −2.313 | 2.183 | −6.682 | 2.056 |
The t value for DP calculated is 1.060, the P value is 0.2937 and confidence interval is (−6.682, 2.056)
Fig. 7.

ACL femoral tunnel positions in technique A (red square). ACL femoral tunnel positions in technique B (blue diamond)
Fig. 8.

Mean ACL femoral footprint as described by Young Mo Kim et al. (blue). Mean ACL femoral footprint as described by Hu Xu et al. (yellow). Mean ACL femoral footprint as described by Peifer et al. (green). Mean ACL femoral footprint as dectected in present study technique A (orange). Mean ACL femoral footprint as dectected in present study technique B (red)
Statistical Analysis
Technique A had 17 type I tunnels and 13 type II tunnels, technique B had 15 type I and 15 type II tunnels. None of the tunnels were Type III both techniques.
Discussion
The most common aetiology of a failed ACL reconstruction is a surgical technical error. Among the surgical technical errors, tunnel malposition is the most common etiology [7, 8]. Although tunnel malposition can be multifactorial, poor visualization of the ACL remnants and bony landmarks contributes in the majority of cases [9]. According to the data from the multicentre ACL revision society (MARS) 80% of all technical ACL failure is because of faulty femoral tunnel [10].
There is no consensus on the anatomical positioning of the femoral tunnel, and the anatomical centre of the native femoral insertion in direction with the collagen fibres is primarily taken into account. In a chronic tear, the footprint is often not clearly appreciable [11]. Studies have been done previously to determine the anatomic centre of the ACL footprint according to the quadrant method with variable results that are enumerated in Table 5.
Table 5.
Studies on ACL femoral footprint anatomical location
| Author | Type of study | Method used to locate ACL footprint | Location of footprint in saggital plane from posterior to anterior in % ratio | Location of footprint from proximal to distal (from Blumenstat’s line) |
|---|---|---|---|---|
| Kim et al. [12] | Cadaveric study | Quadrant method by Bernard et al. | 29.5 ± 2.8% | 38.5 ± 3.2% |
| Columbet et al. [13] | Cadaveric and radiographic study | Quadrant method by Bernard et al. |
AM bundle 26.4 ± 2.6% PL bundle 32.3 ± 3.9% |
AM bundle 25.3 ± 4.2% PL bundle 47.6 ± 6.5% |
| Xu et al. [14] | Systematic review | Quadrant method by Bernard et al. | 28.4 ± 5.1% | 35.7 ± 6.9% |
| Peifer et al. [15] | Systematic review | Quadrant method by Bernard et al. | 28.5% (mean) | 35.2% (mean) |
| Present study technique A | Pilot study | Quadrant method by Bernard et al. | 35.8 ± 8.2 | 35.2 ± 6.7 |
| Present study technique B | Pilot study | Quadrant method Bernard et al. | 38.1± 8.6 | 35.8 ± 9.4 |
Investigators have used more than two portals for better visualization of ACL footprints however they have not compared whether an additional portal actually improves accuracy or predictability of tunnel positioning. The first study was a technical note using three portal techniques for ACL reconstruction. They utilized a central portal in addition to the standard anterolateral and anteromedial portal to enhance visualization of the lateral wall. The central portal was placed one centimetre lateral to the medial border of the patellar tendon (intratendinous) just inferior-to-inferior pole of the patella with the knee in 60° flexion. However, they did not analyse whether making this extra central portal did objectively improve tunnel position [3]. A similar technical note was also published in 2018 in which two medial portals were used to view and drill the femoral tunnel but they did not analyse tunnel position [4]. These studies have subjectively analysed the convenience of using an extra portal. However, no objective evidence like measurements on a CT or X-ray was used to determine tunnel positions.
The present study has used a postoperative CT scan of the lateral intercondylar notch area and used the Bernard quadrant method for comparison of the femoral tunnel positioning between the two techniques. The portal described here on the medial side gives a more end on view of the ACL footprint as compared to a central portal. The portal is made medial to the patellar tendon reduces the obstruction caused by the fat pad in visualisation as well as gives better manoeuvrability of the arthroscope in the joint, as it does not pass through the patellar tendon. It also has the advantage of not violating the patellar tendon. However, it does have the potential disadvantage of overcrowding instruments as both the portals are on the medial side. This problem is less when the viewing anteromedial portal is made higher up as described in this study.
In our study, we compared the position of the femoral tunnel in the two surgical techniques keeping the surgeon’s intention to drill the tunnel at a distance of 5 mm from the posterior articular margin and 5 mm from the inferior aspect of the lateral femoral notch.. In technique A we see the medial wall of lateral condyle from AL portal which is not an end on view as this portal is almost parallel to the medial wall of the lateral condyle, In technique B we see the medial wall of lateral condyle from high AM portal which is an end-on view as this portal is almost perpendicular to the medial wall of the lateral condyle. The intention was to compare whether the predictability of drilling a femoral tunnel at a particular location differed in both techniques and did visualize the lateral aspect of the notched end on give better predictability of tunnel position. The study results showed that there is no statistical difference in the position of the femoral tunnel using either technique A or B. On individually analysing tunnel position it was found that both techniques had most of the tunnels well placed (53.3%), with none of them being grossly malpositioned. Technique A had slightly more tunnels that were Type I (well placed) and this could be attributed to the surgeons preferred technique of doing ACL’s prior to this study being technique A. However the smaller sample size does not give us a statistically significant result.
These results could be explained by a few factors. Making the high anterolateral portal close to the patellar tendon gives an almost complete view of the lateral aspect of the notch even if not end on., However this technique would be useful for relatively less experienced surgeons as looking end on does make measurements of the femoral tunnel and visualizing the button while flipping easier. This is especially useful in cases where an adjustable loop is used. These devices have a propensity to flip over the iliotibial band if excess traction is put rather than the lateral femoral cortex. Directly observing the button cross the femoral tunnel guides the surgeon when to pull the flipping suture and potentially reduces the risk of the button going beyond where it should be.
The unique features of this study are it is the first radiological or CT based study comparing two transportal techniques of ACL reconstruction, This study proves that there is no additional benefit of an accessory portal in terms of tunnel position accuracy as suggested in the technical note published [3]. This study is clinically relevant as femoral tunnel malposition is a leading cause of failure in ACL reconstructions and this study was done to investigate whether either of the two techniques improved femur tunnel positions. Results of this study suggest that the femoral tunnel positions are well placed in over 50% cases and none being grossly malpositioned using both techniques. Working and viewing the lateral femoral notch from the same side may cause overcrowding of instruments and potentially harder to execute. The conventional viewing from the lateral side and working from a low medial portal produces the same femoral tunnel positions in this study without the problem of overcrowding of instruments.
The possible drawbacks are a small sample size, as this was a pilot study. Measurement of the femoral tunnel using the best-fit circle may have inaccuracies, as at times the tunnel can be elliptical. Thus small measurement errors, especially in a small area like the lateral aspect of the notch, could potentially lead to inaccurate results. However, this is a prescribed CT scan technique to measure the femoral tunnel and has been used in previous studies to measure femoral tunnel position. Future studies with larger sample size and comparing tunnel position to patient-reported outcome measures could potentially determine an ideal femoral tunnel position and could potentially give a more statistically and clinically significant result.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Standard Statement
This study was approved by the Max Healthcare Ethics Committee.
Informed Consent
Informed consent was taken from every patient recruited in this study as per the protocol sanctioned by the Max Healthcare Ethics Committee.
Patient Declaration Statement
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Contributor Information
Vikram A. Mhaskar, Email: drvikrammhaskar@gmail.com
Ajay K. Singh, Email: dr.ajaysingh282@gmail.com
Pankaj Soni, Email: pankaj.soni0206@gmail.com.
Jitendra Maheshwari, Email: Jitendra.Maheshwari@maxhealthcare.com.
References
- 1.Thompson SR, Miller MD. Sports Medicine. In: Thompson SR, Miller MD, editors. Miller’s review of orthopaedics. 7. Amsterdam: Elsevier; 2016. p. 349. [Google Scholar]
- 2.Magnussen RA, Debieux P, Benjamin B, Lustig S, Demey G, Servien E, Neyret P. A CT-based classification of prior ACL femoral tunnel location for planning revision ACL surgery. Knee Surgery, Sports Traumatology, Arthroscopy. 2012;20(7):1298–1306. doi: 10.1007/s00167-011-1814-4. [DOI] [PubMed] [Google Scholar]
- 3.Petersen W, Zantop T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthopae Relat Res. 2007;454:35–47. doi: 10.1097/BLO.0b013e31802b4a59. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SB, Fu FH. Three portal technique for anterior cruciate ligament reconstruction arthroscopy. J Arthrosc Relat Surg. 2007;23(3):3251–3255. doi: 10.1016/j.arthro.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal A, et al. switching portal technique in anterior cruciate ligament reconstruction: use of an extra low and medial portal. Int J Res Orthop. 2019;5(4):635–638. doi: 10.18203/issn.2455-4510.IntJResOrthop20192675. [DOI] [Google Scholar]
- 6.Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL. Radiographic quadrant method. American Journal of Knee Surgery. 1997;10(1):14–21. [PubMed] [Google Scholar]
- 7.Bedi A, Altchek DW. The “footprint” anterior cruciate ligament technique: an anatomic approach to anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(10):1128–1138. doi: 10.1016/j.arthro.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DL, Swenson TM, Irrgang JJ, et al. revision anterior cruciate ligament surgery: experience from Pittsburg. Clinical Orthopaedics and Related Research. 1996;325:100–109. doi: 10.1097/00003086-199604000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Sommer C, Friederich NF, Muller W. Improperly placed anterior cruciate ligament grafts: co-relation between radiological parameters and clinical results. Knee Surg Sports Traum Arthros. 2000;8(4):207–213. doi: 10.1007/s001670000125. [DOI] [PubMed] [Google Scholar]
- 10.MARS Group. Wright RW, Huston LJ, et al. Descriptive epidemiology of the multicenter ACL study (MARS) cohort. American Journal of Sports Medicine. 2010;38:1979–1986. doi: 10.1177/0363546510378645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Eck CF, Schreiber VM, Mejca HA, et al. Anatomic anterior cruciate ligament reconstruction: a systematic review of surgical technique and reporting of surgical data. Arthroscopy. 2010;26(9 supp):502–512. doi: 10.1016/j.arthro.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Kim YM, et al. Femoral footprint for anatomical single bundle anterior cruciate ligament reconstruction: a cadaveric study. Knee Surg Relat Res. 2018;30(2):128–132. doi: 10.5792/ksrr.17.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Columbet P, Robinson J, Christel P, Franceschi JP, Djian P, Bellier G, Sbihi A. Morphology of anterior cruciate ligament attachment for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy. 2006;22:984–992. doi: 10.1016/j.arthro.2006.04.102. [DOI] [PubMed] [Google Scholar]
- 14.Xu H, Zhang C, Zhang Q, Du T, Ding M, Wang Y, Fu SC, Hopkins C, Yung SH. A systematic review of anterior cruciate ligament femoral footprint location. Evaluated by quadrant method for single bundle and double bundle anatomic reconstruction. Arthroscopy. 2016;32(8):1724–1734. doi: 10.1016/j.arthro.2016.01.065. [DOI] [PubMed] [Google Scholar]
- 15.Piefer JW, Pflugner TR, Hwang MD, Lubowitz JH. Anterior cruciate ligament femoral footprint anatomy: systematic review of the 21st century literature. Arthroscopy. 2012;28(6):872–881. doi: 10.1016/j.arthro.2011.11.026. [DOI] [PubMed] [Google Scholar]


