Abstract
Objective
To evaluate the effectiveness of inserting a retrievable inferior vena cava filter (IVCF) to prevent pulmonary embolism (PE) in patients with bone fractures and acute deep venous thrombosis (DVT) before major orthopedic surgery.
Methods
Clinical data of patients with fractures and acute DVT who underwent IVCF insertion were analyzed. The patients were divided into above-knee DVT (AKDVT), popliteal vein thrombosis (PVT), and below-knee DVT (BKDVT) groups.
Results
An IVCF was successfully implanted in 964 patients, among whom 929 were followed up (335, 470, and 124 in AKDVT, PVT, and BKDVT groups, respectively). There was no significant difference in the incidence of filter thrombosis among the groups (11.04%, 11.70%, and 8.06%, respectively). No symptomatic PE occurred during follow-up. The mean filter indwelling time was 18.4 ± 4.3 days, and the total filter removal rate was 76.87%. There was no significant difference in the rate of filter implantation, retrieval, complications, or mortality among the groups.
Conclusions
Retrievable filters can effectively prevent PE before orthopedic surgery in patients with fractures and acute DVT of the lower limbs. AKDVT more readily forms a ≥1-cm thrombus in the IVCF than does BKDVT, and PVT more readily forms a <1-cm thrombus than does AKDVT.
Keywords: Deep venous thrombosis, pulmonary embolism, vena cava filter, bone fracture, below-knee deep venous thrombosis, orthopedic surgery
Introduction
Deep venous thrombosis (DVT) is the most common complication in patients with orthopedic trauma. Patients with trauma are prone to develop hypercoagulation, immobilization, and further injury, which are common causes of and risk factors for thrombosis. The incidence of DVT in patients with trauma varies from 0.76% to 58%, which may be related to the severity of injury and prophylactic measures against thrombosis.1–5 DVT is a risk factor for pulmonary embolism (PE). Venous thromboembolism (VTE), which comprises both DVT and PE, is a significant cause of morbidity and mortality in patients hospitalized for trauma. The mainstay of treatment for PE and DVT is anticoagulation. However, one study showed that despite complete anticoagulation, PE occurred in one-third of patients with DVT and that 90% of patients with PE were asymptomatic.6 Furthermore, some patients have contradictions to intraoperative anticoagulation. Several pulling, twisting, and pressing movements of the lower limbs are performed intraoperatively, which may result in clot migration and thus a high risk of acute PE and mortality.7,8 In such situations, inferior vena cava (IVC) filters (IVCFs) are an important alternative measure for PE prevention. They can be used to decrease the potential risk of PE. Notably, placement of permanent filters is associated with several long-term complications, such as recurrence of DVT, IVC thrombosis, IVC occlusion, filter fractures, IVC penetration by the filter legs, and filter migration.9 However, retrievable filters can either be left in place permanently or safely retrieved after a long time when they become unnecessary, which can avoid long-term complications due to filter placement. Therefore, the indications for filters have become extensive, and the number of filters being used has greatly increased.10–12 However, the expanded indications for IVCFs are not supported by evidence, and their clinical utility is controversial, especially in patients with below-knee DVT (BKDVT).13–15
This study was performed to clarify the incidence of perioperative PE due to DVT from different areas in patients with orthopedic trauma who underwent orthopedic surgeries at our institution. We examined the incidence of embolization and thrombotic occlusion of filters and evaluated the efficacy of retrievable IVCF deployment in these patients.
Methods
Clinical data
This study was performed in Tianjin Hospital, the largest trauma center in Tianjin, China, affiliated to Tianjin University. Approximately 5000 bone fracture procedures are performed annually in this hospital. This study was approved by the Ethics Committee of Tianjin Hospital (approval no. 2021-058). Consent for publication was not required because of the retrospective nature of this study.
We retrospectively reviewed the clinical data of inpatients who required orthopedic surgery for repair of spinal, pelvic, or lower extremity fractures in our hospital from January 2017 to June 2020. All study candidates were diagnosed with acute DVT by a lower extremity duplex ultrasound scan, underwent IVCF insertion before the operation, and had no symptoms of PE. Patient inclusion was not related to the severity of trauma. Overall, 964 consecutive patients were screened, including 494 men and 470 women (mean age, 60.36 ± 15.61 years; range, 14–94 years). After diagnosis, the patients underwent IVCF insertion and were followed up until the thrombus was stable, the risk of PE was reduced, and the filter could be removed. We excluded 3 patients who died of severe trauma-induced circulatory failure following filter implantation and 32 patients who were lost to follow-up. Finally, 929 patients were included (477 men and 452 women; mean age, 60.18 ± 15.67 years; range, 14–94 years). The medical records of these patients were reviewed, and the demographic data, locations of fracture and thrombosis, treatment (chemical anticoagulant therapy and placement of IVCF), incidences of embolization and thrombotic occlusions of the filter, and retrieval rate and indwelling time of the filters were analyzed.
The patients were divided into the following three groups according to the location of thrombosis: above-knee DVT (AKDVT) group (n = 805), BKDVT group (n = 124), and popliteal vein thrombosis (PVT) group (n = 470). The baseline characteristics of these patients are summarized in Table 1.
Table 1.
Summary of baseline characteristics.
| Clinical characteristics | AKDVT | BKDVT | PVT |
|---|---|---|---|
| Number of patients | 335 | 124 | 470 |
| Age, years | 64.43 ± 15.24 | 53.54 ± 13.42 | 58.90 ± 15.72 |
| Sex, male/female | 157/178 | 73/51 | 246/224 |
| Hypertension | 93 | 30 | 126 |
| Diabetes | 44 | 23 | 54 |
| Coronary heart disease | 23 | 10 | 38 |
| Cerebral infarction | 28 | 3 | 11 |
| Varicose veins | 77 | 19 | 98 |
| Fracture location | |||
| Pelvis | 14 | 2 | 7 |
| Femur | 188 | 29 | 185 |
| Tibiofibular | 28 | 32 | 54 |
| Spine | 20 | 4 | 37 |
| Patella | 8 | 20 | 50 |
| Foot and ankle | 7 | 6 | 24 |
| Multiple fractures | 70 | 31 | 113 |
| Injury Severity Score | 10.25 ± 5.01 | 9.53 ± 5.93 | 8.96 ± 5.75 |
Data are presented as number of patients or mean ± standard deviation.
AKDVT, above-knee deep venous thrombosis; PVT, popliteal vein thrombosis; BKDVT, below-knee deep venous thrombosis.
Anticoagulation and filter placement
After establishing the diagnosis, low-molecular-weight heparin was subcutaneously administered as the initial anticoagulant to patients without contraindications with a weight-adjusted dose every 12 or 24 hours (1 mg/kg). This treatment was continued for the duration of hospitalization. The patients subsequently received oral anticoagulants (warfarin or rivaroxaban). Generally, IVCFs were deployed 1 to 2 days before or on the day of orthopedic surgery to prevent perioperative PE. During the perioperative period, anticoagulation was reduced or discontinued depending on each patient’s surgical procedure or anesthetic technique and contraindications for coagulation. Absolute contraindications for anticoagulation were uncontrolled active bleeding following injury or surgery, cerebrovascular accident, active gastrointestinal hemorrhage, intracranial bleeding, systemic coagulopathy, and renal failure. Once the risk of bleeding was reduced, normal anticoagulation treatment was prescribed as soon as possible.
Indications for IVCF placement
According to the Guideline for Diagnosis and Treatment of Deep Vein Thrombosis (3rd edition) of the Chinese Society for Vascular Surgery,16 Chinese Association of Orthopedics,17 American College of Chest Physicians,18 Society of Interventional Radiology,19 and British Committee for Standards in Hematology for therapy of venous thromboembolic disease,20 an academic committee of specialists in vascular surgery and orthopedic surgery at our hospital developed the following indications for IVCF in patients with acute bone trauma: spinal, pelvic, femoral, or multiple fractures that require surgery and acute DVT with the proximal end located above the knee, and patients with DVT undergoing surgical repair of a fracture of the knee or areas below the knee in the ipsilateral limb. We did not perform prophylactic IVCF placement in patients who were scheduled for surgery and had bone fractures and negative DVT ultrasound findings.
IVCF placement
The three retrievable filters that were used in this study were the Aegisy® (LifeTech Scientific Company, Shenzhen, China) (Figure 1), OptEase® (Cordis Endovascular, Johnson & Johnson, Miami, FL, USA) (Figure 2), and Denali® (Bard Peripheral Vascular, Tempe, AZ, USA) (Figure 3). The indications for filter recovery were expected to be satisfied within 21 days; after this time period, the patients were expected to receive an Aegisy® or OptEase® filter at random by a proceduralist because the two filters were similar in structure. When filter retrieval was not expected within 21 days because of multiple trauma or surgeries, the Denali® IVCF was placed. The filters were inserted through the femoral vein or internal jugular vein on the healthy side.
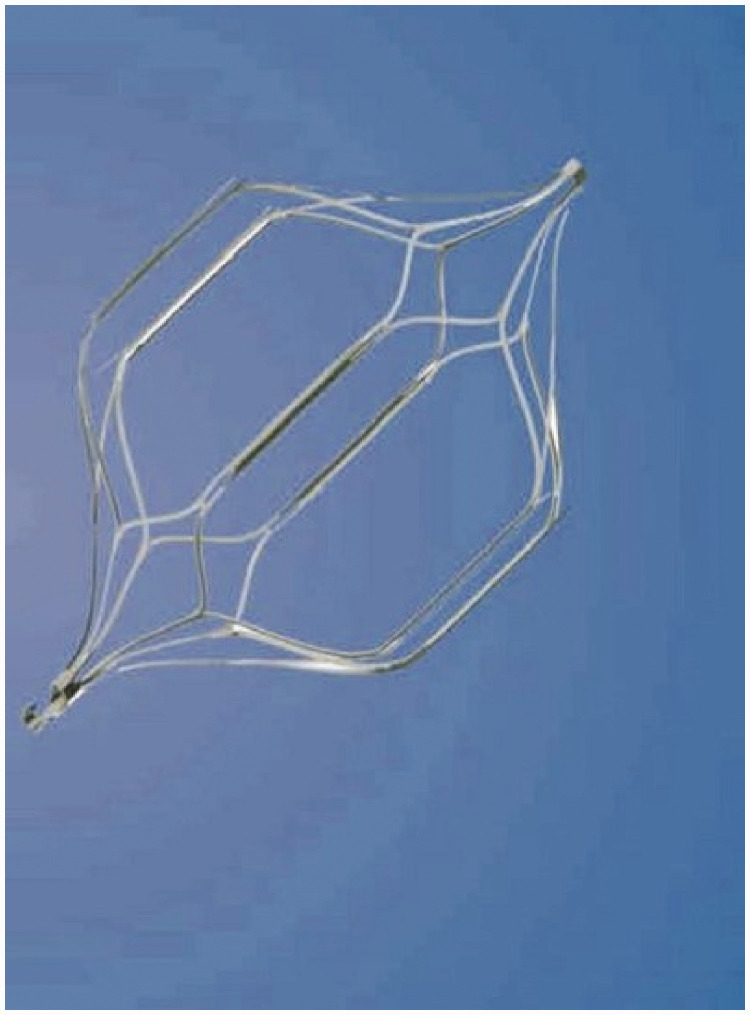
Figure 1.
Aegisy® retrievable filter.
Figure 2.
OptEase® retrievable filter.
Figure 3.
Denali® retrievable filter.
Retrieval of IVCF
Management of IVCF
An important clinical outcome observed during follow-up was symptomatic perioperative PE, which was diagnosed exclusively with pulmonary artery computed tomography angiography. Routine preoperative and postoperative computed tomography angiography was not performed unless there was clinical suspicion of PE. The filters were removed as soon as the patient satisfied the criteria of our hospital. In patients who were temporarily unsuitable for IVCF retrieval, the cause and treatment were recorded, and the patients were monitored weekly until the filter could be retrieved or converted to a permanent filter for any other reasons. At the same time, color Doppler ultrasound was performed weekly to identify any blood clots or thrombosis in the filter. If abnormalities were found, computed tomography venography or venous angiography was performed to measure the size of the thrombosis in the filter. Thrombus size is expressed in terms of length, measured at two vertical angles and averaged. Two chief residents of vascular surgery were responsible for placement of the filter, follow-up of patients, and removal of the filter. After they had been discharged from the hospital, we contacted the patients by telephone, inquired about their status, and made appointments for hospitalization and retrieval of the IVCF.
Indications for IVCF retrieval
At our institution, retrieval is considered in the following clinical scenarios. (1) Before filter retrieval, the patient underwent continuous anticoagulation for >10 days and had no new, recurrent, or progressive symptoms of DVT. Additionally, the DVT disappeared or remained stable, the serum D-dimer concentration was within the reference range twice within 7 days, and the risk of PE was reduced. (2) Anticoagulation is not expected to be terminated because of changes in the treatment plan or additional procedures within a short duration, which can increase the risk of PE. (3) The patient is young (<75 years old) or expected to live long enough to benefit from IVCF retrieval. (4) After assessments, including color Doppler examination of the IVC and IVC angiography, either no obvious thrombosis in the filter or the presence of only a few thromboses of only <1 cm in the filter is confirmed, and the filter can be safely retrieved. (5) The patient or consenting guardian agrees to filter retrieval. (6) The filter indwelling time does not exceed the recommended recovery time. In patients with a strong desire to remove the filter, we appropriately extend the window period to the same.
Treatment of filter thrombus
Different treatment strategies were developed for thrombi of different sizes in the filters. The retrieval technique and corresponding treatment results were recorded in each group during the follow-up period.
IVCF retrieval
The hook of the filter was captured using the hook filter recovery kit. If filter tilt was significant or the filter hook was in opposition to the IVC wall, it was difficult to insert the trap into the hook of the filter. We adopted various methods for filter removal, including use of a double guide wire, addition of a puncture point to assist in changing the position of the filter, and combined use of a guide wire and snare. If all strategies failed, retrieval was abandoned and the filter was switched to a permanent filter.
Statistical analysis
Data are presented as mean and range for continuous variables and as percentages for incidence rates. The chi-square test was used to evaluate differences in categorical variables among the groups. A p-value of <0.05 was considered statistically significant. Data were analyzed using PASW Statistics for Windows, Version 18.0 (SPSS Inc., Chicago, IL, USA).
Results
Intraoperative and perioperative results
A total of 929 patients met the implantation criteria and underwent successful implantation of an IVCF (technical success rate, 100%). The Denali®, OptEase®, and Aegisy® filter was placed in 31, 597, and 301 patients, respectively. None of the patients developed perioperative complications at the puncture point. Four patients had obvious postoperative lumbar pain, which was relieved after symptomatic treatment. No patients developed intraoperative or postoperative symptomatic PE, and no PE-related deaths occurred.
Follow-up results
No patients developed IVC perforation, filter fracture, lack of filter expansion, blocked renal veins, filter entry into the large branches, filter migration, or IVC rupture. Embolization and thrombosis in the filter were observed in 102 patients; the distribution and treatment of the patients in each group are summarized in Tables 2 and 3. The AKDVT, PVT, and BKDVT groups included 37, 55, and 10 patients with thrombosis in the filter, respectively. The thrombosis rate in the three groups was 11.04%, 11.70%, and 8.06%, respectively, with no significant difference among them. The number of patients with a ≥1-cm length of thrombus around the filter in each of the three groups was 29, 29, and 3 (rates of 8.67%, 6.17%, and 2.42%), respectively, with significant differences among the three groups (p = 0.048). Pairwise comparisons revealed that the incidence of a ≥1-cm length of thrombus around the filter was significantly higher in the AKDVT group than BKDTV group (p = 0.022). The number of patients with a <1-cm length of thrombus around the filter in the AKDVT, PVT, and BKDVT groups was 8, 26, and 7 (rates of 2.39%, 5.53%, and 5.64%, respectively). There was no significant difference among the three groups; however, the incidence of a <1-cm length of thrombus around the filter was significantly higher in the PVT group than AKDVT group (p = 0.032). The mean filter indwelling time was 18.4 ± 4.3 days, and the total filter removal rate was 76.87%. There was no significant difference in the success rate, complication rate, or mortality rate among the groups.
Table 2.
Filter embolization and thrombosis in the three groups.
| Total | AKDVT | PVT | BKDVT | χ2 | p-value | |
|---|---|---|---|---|---|---|
| Number of patients | 929 | 335 | 470 | 124 | ||
| Filter embolization and thrombosis | 102 (10.98) | 37 (11.04) | 55 (11.70) | 10 (8.06) | 1.331 | 0.512 |
| ≥1-cm length of thrombus around filter | 61 (6.57) | 29 (8.67) | 29 (6.17) | 3 (2.42) | 5.982 | 0.048 |
| <1-cm length of thrombus around filter | 41 (4.41) | 8 (2.39) | 26 (5.53) | 7 (5.64) | 5.097 | 0.072 |
Data are presented as n (%) of patients.
AKDVT, above-knee deep venous thrombosis; PVT, popliteal vein thrombosis; BKDVT, below-knee deep venous thrombosis.
Table 3.
Pairwise comparisons of filter thrombosis in each group.
| Filter embolization and thrombosis |
≥1-cm length of thrombus around filter |
<1-cm length of thrombus around filter |
||||
|---|---|---|---|---|---|---|
| χ2 | p-value | χ2 | p-value | χ2 | p-value | |
| AKDVT vs. PVT | 0.083 | 0.773 | 1.809 | 0.213 | 4.779 | 0.032 |
| AKDVT vs. BKDVT | 0.875 | 0.391 | 5.429 | 0.022 | 3.037 | 0.134 |
| PVT vs. BKDVT | 1.332 | 0.264 | 2.708 | 0.119 | 0.002 | 1 |
AKDVT, above-knee deep venous thrombosis; PVT, popliteal vein thrombosis; BKDVT, below-knee deep venous thrombosis.
Overall, 102 patients were found to have thrombi in the filters; retrieval was attempted in 94 patients and was successful in 88 (86.21%) of them. In the remaining 827 patients without thrombi in the filters, the DVT disappeared or remained stable, and the risk of PE was considered adequately reduced for filter removal. In 189 of these patients, however, the filter was not removed and was instead converted to a permanent filter for the following non-thrombotic reasons: advanced age (n = 100); combined presence of an advanced tumor (n = 8); treatment with another orthopedic surgery, thus exceeding the window for filter removal (n = 9); and refusal of filter removal (n = 72). Retrieval was attempted in 638 patients without significant thrombosis and was successful in 626 (98.12%) of them. Overall, 714 patients underwent successful removal of the filter (214, 390, and 110 patients in the AKDVT, PVT, and BKDVT group, respectively). The total filter removal rate was 76.87%, and there was no significant difference among the groups. The longest indwelling time with the Denali® filter was 290 days (96.75 ± 59.32), and that for the OptEase® and Aegisy® filters was 52 days (19.02 ± 6.80); the removal rate was 77.42%, 75.71%, and 79.06%, respectively. There were no significant differences among the different filter brands. The distribution of patients with filter obstruction and removal in each group is shown in Table 4.
Table 4.
Filter thrombosis and removal in each group.
| AFDVT | PVT | BKDVT | Total | |
|---|---|---|---|---|
| Number of patients | 335 | 470 | 124 | 929 |
| Aegisy® | 98 | 126 | 77 | 301 |
| OptEase® | 220 | 330 | 47 | 597 |
| Denali® | 17 | 14 | 0 | 31 |
| Filter embolization and thrombosis | 37 | 55 | 10 | 102 |
| ≥1-cm length of thrombus around filter | ||||
| Massive thrombosis in the filter | 6 | 7 | 0 | 13 |
| Spread of thrombosis to distal inferior vena cava and unilateral or bilateral iliac veins | 16 | 7 | 0 | 23 |
| Partial thrombosis in the filter | 7 | 15 | 3 | 25 |
| Total | 29 | 29 | 3 | 61 |
| <1-cm length of thrombus around filter | 8 | 26 | 7 | 41 |
| Successfully removed | 31 | 49 | 8 | 88 |
| Patients without thrombus in filter | 298 | 415 | 114 | 827 |
| Converted to permanent filter | 107 | 71 | 11 | 189 |
| Converted to permanent filter for non-thrombotic reason | 71 | 41 | 5 | 117 |
| Refused filter removal | 36 | 30 | 6 | 72 |
| Attempted retrieval | 191 | 344 | 103 | 638 |
| Unsuccessful | 8 | 3 | 1 | 12 |
| Successful | 183 | 341 | 102 | 626 |
| Total patients with successful removal | 214 | 390 | 110 | 714 |
| Aegisy® (79.06%) | 74 | 104 | 60 | 238 |
| OptEase® (75.71%) | 128 | 274 | 50 | 452 |
| Denali® (77.42%) | 12 | 12 | 0 | 24 |
Data are presented as number of patients.
AKDVT, above-knee deep venous thrombosis; PVT, popliteal vein thrombosis; BKDVT, below-knee deep venous thrombosis.
Discussion
VTE is the most common major complication in patients with orthopedic trauma.3 A meta-analysis in Asia showed that the incidence of DVT in patients with fractures was 1.5%.4 A retrospective analysis of 24,049 patients with trauma in our hospital concluded that the overall incidence of DVT was 6.14%.5 As the Injury Severity Score (ISS) increases, the risk factors for VTE also increase. Hereford et al.21 reported that in patients with head, neck, chest, and limb trauma, the probability of VTE significantly increased with an ISS of >12. Chu and Haga22 reported that the risk of VTE in patients with an ISS of >15 was six times higher than that in patients with an ISS of ≤15.
Patients with severe trauma often require orthopedic surgery. Intraoperatively moving, twisting, and pulling of the limbs is inevitable, and a hemostasis belt may be required to reduce bleeding. However, many of these patients have absolute or relative contraindications for anticoagulation. These factors increase the risk of perioperative thrombus shedding and the incidence of PE. In one study, the incidence of PE was as high as 32% in patients with DVT who underwent orthopedic surgery without filter implantation.23 IVCF placement is an effective method for the prevention of fatal perioperative PE in these patients. Some experiments have demonstrated that IVCFs significantly reduce the incidence and mortality of PE.24 None of the 929 patients in the present trial developed symptomatic PE after filter implantation, suggesting that retrievable IVCFs are effective in preventing perioperative PE in patients with post-trauma DVT.
The current literature suggests that there is no additional benefit of IVCF placement in patients with VTE who can receive anticoagulant therapy.25,26 However, IVCF implantation is recommended if a patient is at risk of bleeding because of the need for major surgery or the presence of severe trauma or neurosurgical injury, which are contraindications for anticoagulation. However, these indications are mainly for patients with central-type or proximal lower extremity DVT. For patients with trauma and calf DVT, preoperative filter implantation remains controversial. A previous study suggested minimal risk of BKDVT progressing to AKDVT or PE.27 In contrast, other studies have suggested that inserting a filter before lower extremity orthopedic surgery may be useful in patients with calf DVT.28,29 Olson et al.29 reviewed 11,330 patients with trauma and suggested that BKDVT should not be ignored because it progressed to AKDVT or PE in 1 in 8 patients, respectively. The authors suggested that aggressive chemical prophylaxis and perhaps therapeutic anticoagulation or IVCF placement should be considered in patients with BKDVT.29
Our results demonstrated no significant differences in the incidence of filter thrombosis among the three groups. Therefore, patients with trauma and DVT who require orthopedic surgery have the same risk of filter thrombosis as those with thrombosis above the knee. We believe that IVCF implantation is necessary in these patients with combined DVT.
IVCF thrombosis is not a rare complication; it occurs in 2% to 10% of patients.30 Whether this occurs by a trapped embolus or in situ filter thrombosis remains unclear. Teo et al.9 reported that the incidence of IVCF thrombosis was highest (up to 8%) within 30 days of implantation. We believe that this rate is associated with thrombus shedding during the acute phase of the thrombus. Kim et al.31 reported that thrombosis progression was a risk factor for thrombosis in a filter, and no thrombosis in the filter was found in patients with isolated calf thrombosis. However, other studies have suggested that thrombosis in the filter is independent of anticoagulation.32 We believe that thrombosis in IVCFs is associated with inadequate anticoagulation, thrombosis progression, and thrombus shedding in the acute phase of DVT. Most importantly, if we hypothesize that the thrombus in IVCFs has occurred from shedding in the acute phase of DVT, these patients might develop PE.
In the present study, clots were observed in the filters in 102 patients without symptomatic PE. We believe that without an IVCF, these 102 patients would have a high probability of PE. In contrast, the severity of the thrombus in the filter can vary. In some patients, the thrombus is small, even <1 cm in length, while in others, it can occupy the entire filter and extended to the distal IVC or iliac vein. When the thrombus is ≥1 cm, patients may develop symptomatic PE; when the thrombus is <1 cm, patients may develop asymptomatic PE. We thus calculated the incidences of ≥1-cm and <1-cm thrombi in each group.
Our data showed that the number of patients with a ≥1-cm thrombus was significantly higher in the AKDVT group than BKDVT group, suggesting that iliofemoral vein thrombosis and PVT are more likely to cause thrombus or thrombosis in the filter than BKDVT and in turn cause symptomatic PE; therefore, IVCF implantation is necessary in these patients. However, there was no significant difference in the incidence of a <1-cm thrombus among the three groups, suggesting that patients with calf thrombosis, even without a filter, would be asymptomatic if they developed PE. Preoperative filter insertion in patients with trauma and ipsilateral DVT is controversial. We believe that if these patients have advanced age or cardiopulmonary insufficiency, implantation of a filter is necessary. The placement of a filter may prevent asymptomatic PE and result in better protection of lung function, especially in older patients. Whether the insertion of a filter in patients with calf DVT can reduce the incidence of fatal PE requires further investigation.
In this study, the number of patients with a <1-cm thrombus was significantly higher in the PVT group than AKDVT group, suggesting that the risk of thrombus or thrombosis in the filter may be greater in patients with PVT than in those with iliofemoral vein thrombosis. We believe that this might be related to greater knee mobility and the possibility of more passive activity during the surgery. Additionally, symptomatic PE may not develop because of the small diameter of the popliteal vein and limited volume of the shed thrombus. Therefore, IVCF implantation can be considered in patients with trauma and PVT. Small PEs may also have serious clinical consequences, especially in elderly patients with cardiopulmonary insufficiency.
In conclusion, IVCF implantation may be necessary in patients with trauma and DVT who require orthopedic surgery on the ipsilateral limb. AKDVT more readily forms a ≥1-cm thrombus in the IVCF than does BKDVT, and PVT more readily forms a <1-cm thrombus than does AKDVT. Large-scale trials are needed to determine whether IVCF implantation in patients with calf DVT reduces the incidence of PE and mortality. We should also pay attention to PVT, which is more easily shed during the perioperative period than iliofemoral vein thrombosis, although it may not result in severe fatal PE.
Footnotes
Author contributions: JH and XD designed the research. CL, ZZ, LX, and XH were involved in data collection. LL, NL, and JK took part in data analysis. JH, XD, and MH drafted and revised the article. JL and XZ provided intellectual content of critical importance to the work. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs: Junjie Huang https://orcid.org/0000-0001-8358-4993
Xiangchen Dai https://orcid.org/0000-0001-9074-6452
References
- 1.Geerts WH, Code KI, Jay RM, et al. A prospective study of venous thromboembolism after major trauma. N Engl J Med 1994; 331: 1601–1606. DOI: 10.1056/NEJM199412153312401. [DOI] [PubMed] [Google Scholar]
- 2.Haut ER, Chang DC, Pierce CA, et al. Predictors of posttraumatic deep vein thrombosis (DVT): hospital practice versus patient factors-an analysis of the National Trauma Data Bank (NTDB). J Trauma 2009; 66: 994–999; discussion 999-1001. DOI: 10.1097/TA.0b013e3181991adc. [DOI] [PubMed] [Google Scholar]
- 3.Knudson MM, Gomez D, Haas B, et al. Three thousand seven hundred thirty-eight posttraumatic pulmonary emboli: a new look at an old disease. Ann Surg 2011; 254: 625–632. DOI: 10.1097/SLA.0b013e3182300209. [DOI] [PubMed] [Google Scholar]
- 4.Kanchanabat B, Stapanavatr W, Meknavin S, et al. Systematic review and meta-analysis on the rate of postoperative venous thromboembolism in orthopaedic surgery in Asian patients without thromboprophylaxis. Br J Surg 2011; 98: 1356–1364. DOI: 10.1002/bjs.7589. [DOI] [PubMed] [Google Scholar]
- 5.Zang J, Ma X, Ma J, et al. Epidemiological study on the incidence of deep vein thrombosis associated with fracture sites. Chin J Orthop Trauma 2016; 36: 540–546. DOI: 10.3760/cma.j.issn.0253-2352.2016.09.005. [Google Scholar]
- 6.Weichman K, Ansell JE. Inferior vena cava filters in venous thromboembolism. Prog Cardiovasc Dis 2006; 49: 98–105. DOI: 10.1016/j.pcad.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Gillern SM, Sheppard FR, Evans KN, et al. Incidence of pulmonary embolus in combat casualties with extremity amputations and fractures. J Trauma 2011; 71: 607–612; discussion 612-603. DOI: 10.1097/TA.0b013e3182282574. [DOI] [PubMed] [Google Scholar]
- 8.Colwell CW. Evidence-based guidelines for venous thromboembolism prophylaxis in orthopedic surgery. Orthopedics 2007; 30: 129–135; quiz 136-127. DOI: 10.3928/01477447-20070201-07. [DOI] [PubMed] [Google Scholar]
- 9.Teo TK, Angle JF, Shipp JI, et al. Incidence and management of inferior vena cava filter thrombus detected at time of filter retrieval. J Vasc Interv Radiol 2011; 22: 1514–1520. DOI: 10.1016/j.jvir.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Young T, Tang H, Hughes R. Vena caval filters for the prevention of pulmonary embolism. Cochrane Database Syst Rev 2010; 2010: CD006212. DOI: 10.1002/14651858.CD006212.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan Y, Shao M, Zhang H, et al. The application of retrievable vena cava filters in patients of bone fracture combined with deep venous thrombosis. Chin J Vasc Surg (Electronic Version) 2013; 5: 5. [Google Scholar]
- 12.Geerts W, Selby R. Inferior vena cava filter use and patient safety: legacy or science? Hematology Am Soc Hematol Educ Program 2017; 2017: 686–692. DOI: 10.1182/asheducation-2017.1.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Group PS. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study. Circulation 2005; 112: 416–422. DOI: 10.1161/CIRCULATIONAHA.104.512834. [DOI] [PubMed] [Google Scholar]
- 14.Toro JB, Gardner MJ, Hierholzer C, et al. Long-term consequences of pelvic trauma patients with thromboembolic disease treated with inferior vena caval filters. J Trauma 2008; 65: 25–29. DOI: 10.1097/TA.0b013e318075e97a. [DOI] [PubMed] [Google Scholar]
- 15.Montgomery JP, Kaufman JA. Inferior vena cava filters: indications, outcomes, and evidence. Curr Treat Options Cardiovasc Med 2015; 17: 401. DOI: 10.1007/s11936-015-0401-2. [DOI] [PubMed] [Google Scholar]
- 16.Chinese Vascular Surgery Association. Diagnosis and treatment guideline for deep vein thrombosis (3rd edition). Chinese Journal of General Surgery 2017; 32: 807–812. [Article in Chinese]. DOI: l0.3760/cma.j.issn.1007-631X.2017.09.032. [Google Scholar]
- 17.Chinese Vascular Surgery Association. The expert consensus of Chinese Association of Orthopedics for diagnosis and therapy of DVT. Chin J Orthop Trauma 2013; 15: 1013–1017. [Article in Chinese]. DOI: 10.3760/cma.j.issn.1671-7600.2013.12.001. [Google Scholar]
- 18.Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141: e278S–e325S. DOI: 10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaufman JA, Kinney TB, Streiff MB, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol 2006; 17: 449–459. DOI: 10.1097/01.rvi.0000203418-39769.0d. [DOI] [PubMed] [Google Scholar]
- 20.British Committee for Standards in Haematology Writing G, Baglin TP, Brush J, et al. Guidelines on use of vena cava filters. Br J Haematol 2006; 134: 590–595. DOI: 10.1111/j.1365-2141.2006.06226.x. [DOI] [PubMed] [Google Scholar]
- 21.Hereford T, Thrush C, Kimbrough MK. Using Injury Severity Score and Abbreviated Injury Score to determine venous thromboembolism risk. Cureus 2019; 11: e5977. DOI: 10.7759/cureus.5977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chu CC, Haga H. Venous thromboembolism associated with lower limb fractures after trauma: dilemma and management. J Orthop Sci 2015; 20: 364–372. DOI: 10.1007/s00776-014-0690-4. [DOI] [PubMed] [Google Scholar]
- 23.Rogers FB, Cipolle MD, Velmahos G, et al. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma 2002; 53: 142–164. DOI: 10.1097/00005373-200207000-00032. [DOI] [PubMed] [Google Scholar]
- 24.Kidane B, Madani AM, Vogt K, et al. The use of prophylactic inferior vena cava filters in trauma patients: a systematic review. Injury 2012; 43: 542–547. DOI: 10.1016/j.injury.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 25.Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016; 149: 315–352. DOI: 10.1016/j.chest.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 26.Mismetti P, Laporte S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA 2015; 313: 1627–1635. DOI: 10.1001/jama.2015.3780. [DOI] [PubMed] [Google Scholar]
- 27.Sharpe RP, Gupta R, Gracias VH, et al. Incidence and natural history of below-knee deep venous thrombosis in high-risk trauma patients. J Trauma 2002; 53: 1048–1052. DOI: 10.1097/00005373-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Pan Y, Mei J, Wang L, et al. Investigation of the incidence of perioperative pulmonary embolism in patients with below-knee deep vein thrombosis after lower extremity fracture and evaluation of retrievable inferior vena cava filter deployment in these patients. Ann Vasc Surg 2019; 60: 45–51. DOI: 10.1016/j.avsg.2019.02.027. [DOI] [PubMed] [Google Scholar]
- 29.Olson EJ, Zander AL, Van Gent JM, et al. Below-knee deep vein thrombosis: an opportunity to prevent pulmonary embolism? J Trauma Acute Care Surg 2014; 77: 459–463. DOI: 10.1097/TA.0000000000000305. [DOI] [PubMed] [Google Scholar]
- 30.Vedantham S, Vesely TM, Parti N, et al. Endovascular recanalization of the thrombosed filter-bearing inferior vena cava. J Vasc Interv Radiol 2003; 14: 893–903. DOI: 10.1097/01.rvi.0000083842.97061.c9. [DOI] [PubMed] [Google Scholar]
- 31.Kim HK, Song I, Jang JH, et al. Outcomes of retrievable inferior vena cava filters in patients with deep vein thrombosis and transient contraindication for anticoagulation. Ann Surg Treat Res 2015; 89: 30–36. DOI: 10.4174/astr.2015.89.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hinojosa CA, Olivares-Cruz S, Laparra-Escareno H, et al. Incidence of thrombotic events and complications associated to inferior vena cava filters in patients with and without anticoagulation therapy. Arch Cardiol Mex 2019; 89: 216–221. DOI: 10.24875/ACM.M19000048. [DOI] [PubMed] [Google Scholar]