Deep vein thrombosis (DVT) is a manifestation of venous thromboembolism, which can result from long-term bed and lead to pulmonary embolism (PE), stroke, mesenteric artery embolis, etc. Patients after surgery without bed-off activity may prone to thrombosis, but traditional anticoagulant therapy is a contraindication for them because of high risk of postoperative hemorrhage. Inferior vena cava filter (IVCF) implantation is the most effective method to intercept thrombosis from lower limb and to prevent PE. However, radiation and contrast agent limit its application. Our team have successfully performed an IVCF implantation guided by a mixed-reality (MR) system,[1] which is a chance for critically ill patients to allow the IVCF implantation exposed under no X-ray and require no contrast agent. 5G can help remote holographic projection images between distant range, meeting the needs of experts to guide the operation of critically ill patients. We describe a case of weak woman after neurosurgery who can not tolerate traditional interventional surgery to prevent DVT from falling off. We performed a mixed-reality system guided IVCF implantation under remote guidance of 5G communication.
The patient was a 48-year-old woman with intraventricular cyst and obstructive hydrocephalus. She underwent an endoscopic cyst resection, cerebral cortex incision and fistulation, and cerebrospinal fluid leakage repair under general anesthesia in Oct 16 2020. Postoperative had a fever, headache, and lip herpes. The cerebrospinal fluid examination suggested intracranial infection. In Oct 24, the patient had a sudden disturbance of consciousness, with left pupil larger than before. She underwent an emergency right ventricular drainage. After the surgery, the patient awaked gradually with mental improvement and lip herpes improved, body temperature dropped to normal. In Nov. 22nd, the consciousness disorder and sleepiness occurred again. Blood biochemical parameters showed that serum sodium (Na) was 183.0 mmol/L, chloride (Cl) was 140.6 mmol/L, and brain computed tomography (CT) suggested no significant change. The disturbance of electrolyte was rectified immediately. In Nov. 28th, she underwent ultrasound for her right leg swelling and thrombosis were found in external iliac vein, femoral vein and fibular veins.
In summary, the patient had a history of neurosurgery and the diagnosis of DVT was confirmed. But the anticoagulation therapy was a contraindication for this patient with surgery in 35 days. Inferior vena cava filter (IVCF) implantation is a most prevention for thromboembolic diseases. This patient has been in bed for two months, and long-term bed is the main risk factor for DVT. PE and thromboembolism may occur without anticoagulant therapy. IVCF implantation is a most prevention for thromboembolism, but IVCF implantation with contrast agent injection may lead a high risk for contrast-induced nephropathy (CIN). Though her frail general conditions mattered, the management of DVT and prevention of PE was prioritized. We hoped to find a method that can not only avoid contrast agent, but also invite experts to instruct catheter surgery on site. Our team have successfully performed an IVCF implantation guided by a mixed-reality (MR) system in 2019,[1] which can visualize human anatomy without contrast agents. 5G communication allowed remote holographic projection experts images from Beijing to Yibin, Sichuan.
Surgery can result in transient reduced mobility places, which is the main cause of DVT. DVT is a main manifestation of venous thromboembolism, causing a large medical and economic burden all over the world. The lifetime risk of venous thromboembolism is 8% in people of 45 years of age or older.[2] In this case, DVT was caused by long-term bed rest after neurosurgery, which may lead to intracranial and wound bleeding after anticoagulant therapy. For this patient who cannot tolerate anticoagulant therapy, IVCF implantation is suitable if the injection of 30−50 mL contrast agents can be replaced in order to decrease the risk of CIN. Though her general state mattered, the prevention of PE was prioritized. We hope to find a method that can avoid the radiation and contrast agents with expert on-site guidance. MR system can visualize anatomy maker, 5G signal transmission can remote holographic projection expert image, and meet the requirements of avoid CIN and expert on-site guidance.
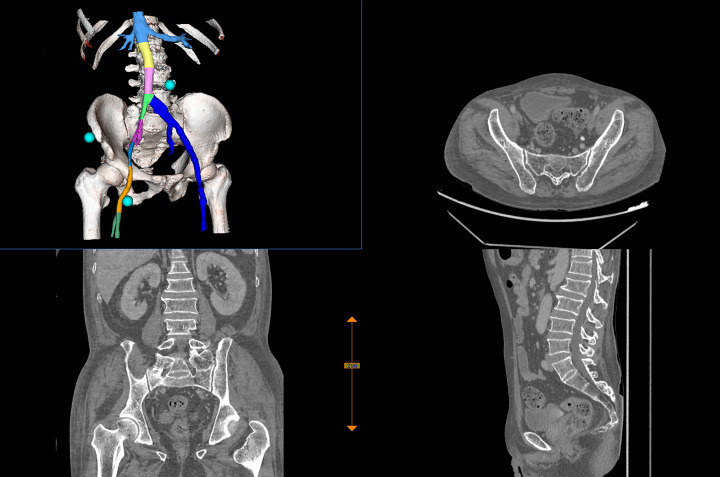
There was some previous work. A 3D-reconstruction was performed depend on CT DICOM images, and three markers were placed on the body surface to help measurement and location. We measured the length from the puncture point of the femoral vein to the implantation position of the IVCF, which was 33.8 cm. Then the route was divided into 5 cm segments in order to obtain the current position during the operation. The synthetic holographic image data was output in v3d format (a data transmission format in Weizhuo Zhiyuan Technology Co., LTD, Beijing), and pushed to the MR display device (Figure 1). Before the operation, the holographic image was superimposed with the patient in the same body position and proportion according to the three markers. Through image fusion and spatial positioning, the 3D holographic images of the femoral vein, inferior vena cava and renal vein of this patient would display in the MR glasses worn by the operator (Figure 2).
Figure 1.
CT three-dimensional reconstruction depend on DICOM data.
Figure 2.
3D holographic images displayed in MR glasses worn by experts.
During the operation, experts in Beijing were projected to the operating room in Yibin profit from the application of augmented reality (AR) technology combined with 5G technology. With the support of MR and 5G technology, the holographic images of anatomy in the MR glasses of the surgeon are transmitted in real time to the MR glasses of the experts in long distance. Firstly, a 6F vascular sheath was inserted through the right femoral vein under local anesthesia. Then, the operators inserted a guide wire of IVCF implant set (LifeTech Scientific Corporation) below the renal vein opening, withdraw the 6F vascular sheath and inserted the filter delivery sheath. Secondly, the position of the sheath was appeared in real time in MR glasses in order to guide the distance from the body surface puncture point to the vessel. Then the most important step was that the operator sent the sheath to 1–2 cm below the renal vein opening under the guidance of experts, and confirmed the position (Figure 3). Finally, the filter was released, and the sheath tube was removed. The patient returned to the ward without complains of discomfort.
Figure 3.
The scene of the operation.
DVT is the main cause of PE, which is one of the most common cardiovascular disease with high mortality.[3] Patients who are bedridden for long-term after surgery have poor venous reflux of lower limbs, which is easy to form DVT of lower limbs. Thrombosis may break off and block the pulmonary artery and its branches.[4] In this case, anticoagulation therapy after neurosurgery may lead to intracranial hemorrhage and bleeding wound, which is fatal for this patient. So, IVCF implantation is an important and suitable measure to prevent PE.[5] Traditional catheter surgery under X-ray with 30−50 mL contrast agents may lead to CIN, a major complications of interventional surgery, with incidence of 1.2%−1.6% in general population.[6] Critical ill patient need effective cure by specialist team. But this is subject to distance and time.
MR system and holograms are useful whenever a problem arose due to blocking and difficult anatomy, which can cause the error between the actual structure and the operator’s range of vision.[7] Novel 3D printing techniques also presented value of navigation and guidance during surgery.[8,9] However, physical models cost long time to manufacture and consumables. Before surgery, 3D printing models need to be sterilized.[10] MR system and holograms are free from these restrictions. MR system had been applied in orthopedics,[11] thoracic,[12] neurosurgical[13] and urinary surgery.[14] But reports regarding catheter operate with MR system and holographic imaging are scarce. Rynio, et al.[15] successfully repaired abdominal aortic aneurysm under the guidance of holographic images. At the same time, 5G communication and holographic projection technology allow the operators to access the guidance of experts on-site.
5G communication combined with MR technology has a great advantage in precise, timeless, and convenience. In future, this technology can bring subversive changes to remote consultation, medical training, doctor-patient communication and military medicine, and promote the rapid development of medicine.
ACKNOWLEDGMENTS
This work was supported by Capital Clinical Application Research Project (No. Z181100001718042) and Cultivation and Enrichment of Front-Line Teachers, Battle Field Internal Medicine of Construction of Key Military Disciplines, 13th Five Year Plan (No. A350109). We thank the participating patient in our operation and her families for their belief. The authors declare no conflict of interests.
References
- 1.Zhu H, Li Y, Wang C, et al A first attempt of inferior vena cava filter successfully guided by a mixed-reality system: a case report. J Geriatr Cardiol. 2019;16:575–577. doi: 10.11909/j.issn.1671-5411.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Nisio M, van Es N, Buller HR Deep vein thrombosis and pulmonary embolism. Lancet. 2016;388:3060–3073. doi: 10.1016/S0140-6736(16)30514-1. [DOI] [PubMed] [Google Scholar]
- 3.Phillippe HM Overview of venous thromboembolism. Am J Manag Care. 2017;23(20 Suppl):S376–S382. [PubMed] [Google Scholar]
- 4.Stone J, Hangge P, Albadawi H, et al Deep vein thrombosis: pathogenesis, diagnosis, and medical management. Cardiovasc Diagn Ther. 2017;7:S276–S284. doi: 10.21037/cdt.2017.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wadhwa V, Trivedi PS, Chatterjee K, et al Decreasing utilization of inferior vena cava filters in post-fda warning era: insights from 2005 to 2014 nationwide inpatient sample. J Am Coll Radiol. 2017;14:1144–1150. doi: 10.1016/j.jacr.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 6.Pucelikova T, Dangas G, Mehran R Contrast-induced nephropathy. Catheter Cardiovasc Interv. 2008;71:62–72. doi: 10.1002/ccd.21207. [DOI] [PubMed] [Google Scholar]
- 7.Sauer IM, Queisner M, Tang P, et al Mixed reality in visceral surgery: development of a suitable workflow and evaluation of intraoperative use-cases. Ann Surg. 2017;266:706–712. doi: 10.1097/SLA.0000000000002448. [DOI] [PubMed] [Google Scholar]
- 8.Yuan D, Luo H, Yang H, et al Precise treatment of aortic aneurysm by three-dimensional printing and simulation before endovascular intervention. Sci Rep. 2017;7:795. doi: 10.1038/s41598-017-00644-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tam CHA, Chan YC, Law Y, et al The role of three-dimensional printing in contemporary vascular and endovascular surgery: a systematic review. Ann Vasc Surg. 2018;53:243–254. doi: 10.1016/j.avsg.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 10.Rynio P, Kazimierczak A, Jedrzejczak T, et al A 3-Dimensional Printed Aortic Arch Template to Facilitate the Creation of Physician-Modified Stent-Grafts. J Endovasc Ther. 2018;25:554–558. doi: 10.1177/1526602818792266. [DOI] [PubMed] [Google Scholar]
- 11.Lee SC, Fuerst B, Tateno K, et al Multi-modal imaging, model-based tracking, and mixed reality visualisation for orthopaedic surgery. Healthc Technol Lett. 2017;4:168–173. doi: 10.1049/htl.2017.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fischer M, Fuerst B, Lee SC, et al Preclinical usability study of multiple augmented reality concepts for K-wire placement. Int J Comput Assist Radiol Surg. 2016;11:1007–1014. doi: 10.1007/s11548-016-1363-x. [DOI] [PubMed] [Google Scholar]
- 13.Barsom EZ, Graafland M, Schijven MP Systematic review on the effectiveness of augmented reality applications in medical training. Surg Endosc. 2016;30:4174–4183. doi: 10.1007/s00464-016-4800-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamacher A, Kim SJ, Cho ST, et al Application of virtual, augmented, and mixed reality to urology. Int Neurourol J. 2016;20:172–181. doi: 10.5213/inj.1632714.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rynio P, Witowski J, Kaminski J, et al Holographically-guided endovascular aneurysm repair. J Endovasc Ther. 2019;26:544–547. doi: 10.1177/1526602819854468. [DOI] [PubMed] [Google Scholar]