Abstract
Introduction
The present study was done to assess the functional outcome and complications of interlocking intramedullary (IM) radius ulna nailing to treat radio-ulna fractures in adults.
Methodology
Thirty adult patients with diaphyseal or segmental fractures of radius and ulna were included and treated with IM nailing. Grace and Eversmann rating system was used to assess functional evaluation and grip strength was measured using grasp dynamometer.
Results
Mean age of the 30 eligible patients was 33.5 years, and males comprised 77% of the study population. Intra-operative complications like nail impaction and proximal screw locking problem for radius was present in one patient each. Increased swelling in three patients (10%) and posterior interosseous nerve palsy in one patient (3%) were observed post-operatively. In the post-operative period, all patients were able to move fingers, had 100° elbow range of motion and good grip strength. Pronation and supination till 80° was present in 80% and 57% of the patients respectively. Wrist flexion and dorsiflexion till 90° was present in 80% and 57% of the patients. Fracture union was confirmed radiologically in all cases at a mean of 3.6 weeks. Functional outcome was excellent in 73% and good in 13%. Grip strength was judged to be excellent in all cases.
Conclusions
Excellent and good functional outcomes were obtained in 86%, and no case developed mal-union or delayed union. Based on our results, IM nail for surgical treatment of radial and ulnar diaphyseal fractures can be used.
Keywords: Forearm injuries, Intramedullary nail, Radius, Ulna
1. Introduction
Intramedullary (IM) nailing is considered a standard treatment for fractures of long bone shaft and is mainly used as a treatment modality for cases involving polytraumatic high-energy long bone fractures, osteoporotic bone fractures and pathological fractures.1,2 Though plate fixation has high union rates, it involves extensive soft tissue dissection and is reported to cause radial nerve damage in approximately 4%.3 IM nailing can avoid these adverse effects and is also biomechanically stronger.4 Furthermore, unlocked IM nailing may offer even better alternative as it requires less soft tissue and vascular supply damage, and promotes secondary periosteal callus formation. However, it may inadequately control fracture rotation, especially in cases of segmental fractures. Locked IM nailing avoids shortening of bones in addition to rotational stability of the fractures. However, the use of IM nailing is not without its set of associated complications, which may bring into question its effectiveness compared to plating. The present study was done to assess the functional outcome and complications of interlocking radius ulna nailing to treat radio-ulna fractures in adults.
2. Methodology
2.1. Study design and sampling
The present prospective observational study was conducted by including 30 adult patients with diaphyseal or segmental fractures of radius and ulna. Patients with open physis, suffering from osteomyelitis, pathological fracture, metaphyseal fracture and having history of a previous radius ulna fracture were excluded from the study. These patients were recruited when they arrived in the casualty of a tertiary care teaching hospital in Navi Mumbai from November 2016 till November 2018. All patients were explained the purpose of the study and an informed written consent was obtained enrolling for the study. The study was approved by the Institutional Ethics Committee.
2.2. Surgical procedure
Pre-operatively work-up radiographs of the injured and not injured forearms (in 2 planes) with the neighbouring joints were taken. We took the anteroposterior (AP) and lateral views of the normal hand to know the length and the diameter of the nail required in the injured forearm. Film tube distance was kept at 1 mm to take true AP and lateral views to know the exact measurements. Pre-bending of the nail template was based on radiographs of the intact bone, preferably on the day before surgery. The necessary nail length was determined and the width of the medullary canal was directly measured on the radiographs. The template was sterilized (when there was not enough time, the non-sterile template was placed in a sterile transparent plastic bag). Shaving of the forearm included wrist and elbow (in cases of hypertrichosis) immediately before surgery.
Nail diameter of 3.0 mm, 3.5 mm, 4.0 mm, 4.5 mm and bolt diameter of 3.0 mm bolt (proximal only) 1.5 mm bolt (distal only for 3.5 mm and 4.0 mm nail were used. Each patient was administered general or regional anesthesia. For nailing of the ulna, the arm was bent at the elbow at 90°, while for the nailing of the radius, the arm was extended. The tourniquet was applied at the upper arm, (was inflated only in open reduction cases). The image intensifier was adjusted such that it came in from the foot end. Entry point for the ulna approach was through the tip of olecranon and through the Lister tubercle approach for radius. A 2.5–3 cm longitudinal incision over distal radius on radial side of Lister’s tubercle starting at the level of wrist joint was made. Subcutaneous tissues were bluntly dissected to avoid injury to superficial radial nerve branches. An opening was made at the second extensor compartment through a longitudinal incision on the extensor retinaculum radial to Lister’s tubercle leaving the proximal third intact. The extensor carpi radial in longus was retracted and the brevis tendon to the radial side. The entry point was about 5 mm to 1 cm proximal to the articular surface. A 2.0 mm trocar pin was inserted into the second compartment and advanced into the medullary canal at a low angle (30°) to prevent engaging the palmer cortex. To avoid penetration of the volar cortex, the wrist was flexed over a stack of towel.
2.3. Data collection and data analysis
Using a pre-defined semi-structured study proforma, patient related demographic and medical history was noted form the medical records. Intraoperative details were noted from the operative notes. Bone union was defined as the presence of bridging the periosteal callus in three or four cortices in the anterio-posterior and lateral radiographs (Fig. 1). According to the criteria proposed by Anderson et al. fracture healing in <6 months was considered to have union; fracture healing lasting longer than 6 months without the need for additional surgical intervention was considered as delayed union, and the absence of fracture healing requiring additional surgery was considered as non-union.5 Grace and Eversmann rating system was used to assess functional evaluation.6 With the use of a forearm goniometer, the ranges of pronation and supination were evaluated according to the neutral zero method, with the elbow flexed 90°, and were recorded as a percentage of the range of motion on the contralateral side. The results were rated as excellent when the fracture had united and there was at least 90% of the normal forearm rotation arc, good when the fracture had united and there was 80%–89% of the rotation arc, acceptable when the fracture had united and there was 60%–79% of normal forearm rotation, and poor when there was a nonunion or <60% of normal forearm rotation. Grip strength measurements were done using a grasp dynamometer (Jamar dynamometer, Asimov Engineering) and expressed as percentage of the grip force of the unaffected hand. For the grip strength measurements, the patient was seated in a standard position with shoulder adducted in neutral position, elbow flexed at 90°, and the forearm and wrist in a neutral position.7 Grip measurements were graded according to the published data by Mullerpatan et al. on normal grip strength values among Indian population and was classified as excellent, good, fair and poor using the grading system by Rosenberg et al.8,9
Fig. 1.
Pre- and post-operative x-rays of one of the patient. A) Pre-operative x-ray AP view; B) Pre-operative x-ray lateral view; C) Immediate postoperative x-ray AP view; D) Immediate postoperative x-ray lateral view; E) 2 months postoperative x-ray AP view; F) 2 months postoperative x-ray lateral view; G) 4 months postoperative x-ray AP view; H) 4 months postoperative x-ray lateral view.
3. Results
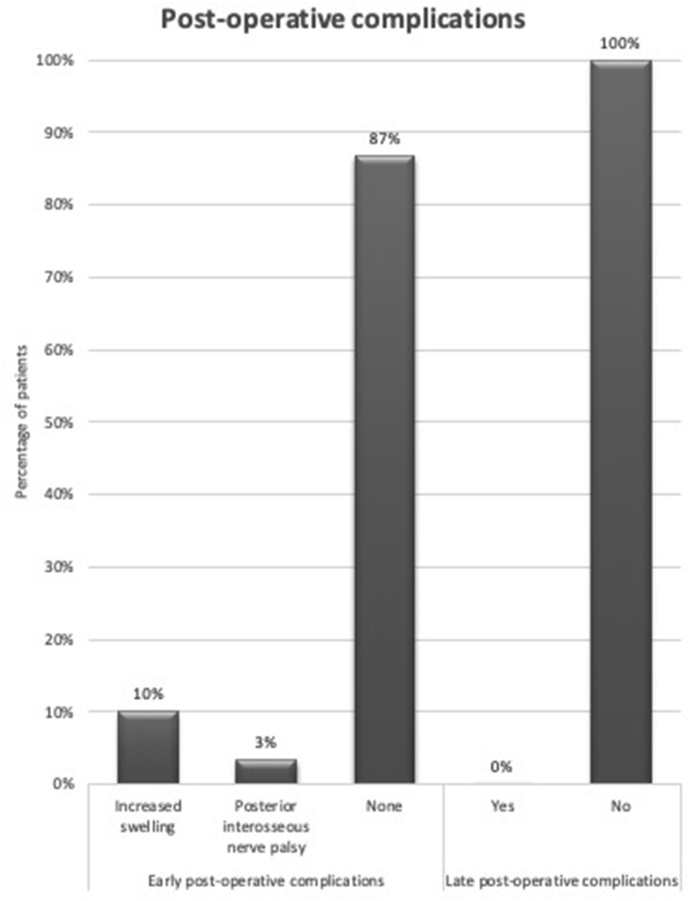
Mean age of the 30 eligible patients was 33.5 years, ranging from 19 to 55 years, 73% of which were in the age group of 21–40 years (Table 1). Males comprised 77% of the study population. Road traffic accident was the mode of injury in 77% of the patients and rest had a fall. Past medical history revealed that four patients had diabetes mellitus and hypertension each. According to the AO classification, 60% had A3 type fracture, while 13% had B3, 10% had C3 and A1 type each and 7% had A2 type. Compound fracture was present in 17% of the patients. Intra-operatively we found that 17% of the patients had more than 50 ml of blood loss, and none of the patients needed blood transfusion (Table 2). Intra-operative complications like nail impaction and proximal screw locking problem for radius was present in one patient each. Mean immobilization period of the patients was 6.17 days, ranging from 4 to 14 days and physiotherapy was started at an average of 1.1 weeks. As for the post-operative complications, increased swelling in three patients (10%) and posterior interosseous nerve palsy in one patient (3%) were observed (Fig. 2). Functional assessment of the patients is described in Table 3. In the post-operative period, all patients were able to move fingers, had 100° elbow range of motion and good grip strength (Fig. 3). Pronation and supination till 80° was present in 80% and 57% of the patients respectively. Wrist flexion and dorsiflexion till 90° was present in 80% and 57% of the patients. Fracture union was confirmed radiologically in all cases at a mean of 3.6 weeks, ranging from 3 to 5 weeks. Functional outcome was excellent in 73% and good in 13%. Grip strength was judged to be excellent in all cases.
Table 1.
Baseline characteristics of the patients included in the study.
| Variables | N | % |
|---|---|---|
| Age group (years) | ||
| ≤20 | 2 | 7% |
| 21 to 40 | 22 | 73% |
| >40 | 6 | 20% |
| Gender | ||
| Males | 23 | 77% |
| Females | 7 | 23% |
| Mode of injury | ||
| Road traffic accidents | 23 | 77% |
| Fall | 7 | 23% |
| Associated injury | ||
| Abrasion | 1 | 3% |
| Lacerated wound | 5 | 17% |
| Head injury | 1 | 3% |
| Metacarpal fracture | 1 | 3% |
| None | 22 | 74% |
| Comorbidity | ||
| Diabetes mellitus | 4 | 13% |
| Hypertension | 4 | 13% |
| Hypertension with diabetes | 4 | 13% |
| None | 18 | 61% |
| AO classification | ||
| 2.2A1 | 3 | 10% |
| 2.2A2 | 2 | 7% |
| 2.2A3 | 18 | 60% |
| 2.2B3 | 4 | 13% |
| 2.2C3 | 3 | 10% |
| Compound grade | ||
| Grade 1 | 2 | 7% |
| Grade 2 | 3 | 10% |
| Not compound | 25 | 83% |
Table 2.
Intraoperative assessment of the patients.
| Intraoperative variables | N | % |
|---|---|---|
| Type of anesthesia | ||
| General anesthesia | 6 | 20% |
| Interscalene block | 12 | 40% |
| Supraclavicular block | 12 | 40% |
| Amount of blood loss | ||
| Up to 50 ml | 25 | 83% |
| More than 50 ml | 5 | 17% |
| Need for blood transfusion | 0 | 0% |
| Nail impaction | 1 | 3% |
| Proximal screw locking problem for radius | 1 | 3% |
Fig. 2.
Post-operative complications of the patients.
Table 3.
Assessment of functional outcome of the patients.
| Functional outcome | N | % |
|---|---|---|
| Finger movement | ||
| Started post-operatively | 30 | 100% |
| Nil | 0 | 0% |
| Elbow range of motion | ||
| 0–100° | 30 | 100% |
| Nil | 0 | 0% |
| Pronation (degrees) | ||
| 0 to 50 | 3 | 10% |
| 0 to 60 | 3 | 10% |
| 0 to 80 | 24 | 80% |
| Supination (degrees) | ||
| 0 to 50 | 9 | 30% |
| 0 to 60 | 4 | 13% |
| 0 to 80 | 17 | 57% |
| Wrist flexion (degrees) | ||
| 0 to 70 | 6 | 20% |
| 0 to 90 | 24 | 80% |
| Wrist dorsiflexion (degrees) | ||
| 0 to 70 | 6 | 20% |
| 0 to 80 | 7 | 23% |
| 0 to 90 | 17 | 57% |
| Grace-Eversmann criteria | ||
| Excellent | 22 | 73% |
| Good | 4 | 13% |
| Acceptable | 2 | 7% |
| Poor | 2 | 7% |
| Grip strength | ||
| Excellent | 30 | 100% |
| Good | 0 | 0% |
| Fair | 0 | 0% |
| Poor | 0 | 0% |
Fig. 3.
Postoperative clinical examination of a patient at 2 months follow up. A) Extension; B) Flexion; C) Pronation; D) Supination.
4. Discussion
In case of long bone fractures, intramedullary nailing is an accepted modality of treatment. However, the same cannot be said about forearm fractures as high non-union rates have been reported.10,11 We treated 30 cases of forearm fracture with intramedullary interlocking forearm nailing and were immobilized for a mean period of 6.17 days, ranging from 4 to 14 days and physiotherapy was started at an average of 1.1 weeks. Use of supplementary material to improve stability of the fixed fracture have been reported previously. For instance, long arm case was used by for a period of three months,12 and brace has been used for a period of 6 weeks.11 Another investigator used splint immobilization for a mean period of 2.5 days in all their patients, irrespective of fracture stability.13 On the contrary, Bansal et al. did not immobilize their patients.14 Likewise, Crenshaw et al. concluded from their study that the decision to lock the fracture should be made after assessing rotational stability after nailing, rather than using it in all patients.15 Moreover, employing screws to guide distal locking is recommended as the risk of iatrogenic injury to distal ulna is high. More biomechanical studies are required to support these observations.
In our study, radiological union was achieved in a mean period of 3.6 (3–5) weeks. There was no patient with mal-union or delayed union. Recently developed forearm nails have resulted in high functional results and union rates, which used to be a drawback of these nails.16 Plating has demonstrated union ratios ranging between 87 and 98%.17 Previous studies using IM nail procedure have reported union ratios as 88.6% by Visna et al.,18 92% by Lee et al.11 and 100% by De Pedro et al.16 According to Grace-Eversman criteria, we observed functional outcome to be excellent in 73% and good in 13%. Lee et al. reported excellent outcomes in 81% of their patients.11 Shivakumar et al. reported that 81.8% had excellent or good results, 13.6% had an acceptable result whereas 4.5% patient had an unacceptable result cause of non-union.19 Ozkaya et al. obtained 90% excellent and 2% fair results.20
Intra-operatively nail impaction and proximal screw locking problem for radius was observed in one patient each in our study (total = 6.6%). This impaction was left alone and nothing was done for it. We had no case of iatrogenic vascular, neural, tendon or bone injury. Irrespective of the technique and nail preferences, appropriate pre-operative planning and a controlled surgical approach minimizes the intra-operative complications. As for the post-operative complications, increased swelling in three patients (10%) and posterior interosseous nerve palsy in one patient (3%) were observed in our study population. Shivakumar et al. reported that 18.18% had superficial infection, who had open fractures and it subsided with course of oral antibiotic therapy, 13.64% had pain at K-wire site, which was addressed by removal of wire once union was attained and 9.09% had pain at olecranon i.e. ulnar nail insertion site.19 Kose13 reported complications in 5.6%, Lee11 in 3.7, Ozkaya20 in 10% and Bansal14 in 8.3%. Azboy et al. reported superficial infection sin 6.3%, radioulnar synostosis in 3.1% and delayed union in 3.1% of the patients.21
5. Conclusion
Recently developed forearm nails require limited soft tissue dissection of the fracture area allowing for early mobilization. In our patient series, excellent and good functional outcomes were obtained in 86%, and no case developed mal-union or delayed union. Overall complication rate in our study was 6.6%. Based on our results, IM nail for surgical treatment of radial and ulnar diaphyseal fractures can be used. Future comparative analytical studies are recommended to support our findings.
Study funding
None.
Declaration of competing interest
None.
References
- 1.Rüedi, Thomas P., Murphy W.M. first ed. Thieme; Stuttgart: 2007. AO Principles of Fracture Management. Print. [Google Scholar]
- 2.Baltov A., Mihail R., Dian E. Complications after interlocking intramedullary nailing of humeral shaft fractures. Injury. 2014;45:S9–S15. doi: 10.1016/j.injury.2013.10.044. [DOI] [PubMed] [Google Scholar]
- 3.Baldwin K., Morrison M.J., 3rd, Tomlinson L.A., Ramirez R., Flynn J.M. Both bone forearm fractures in children and adolescents, which fixation strategy is superior – plates or nails? A systematic review and meta-analysis of observational studies. J Orthop Trauma. 2014;28(1):e8–e14. doi: 10.1097/BOT.0b013e31829203ea. [DOI] [PubMed] [Google Scholar]
- 4.Putti A.B., Uppin R.B., Putti B.B. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg. 2009;17(2):139–141. doi: 10.1177/230949900901700202. [DOI] [PubMed] [Google Scholar]
- 5.Anderson L.D., Sisk D., Tooms R.E., Park W.I. 3rd Compression-plate fixation in acute diaphyseal fractures of the radius and ulna. J Bone Joint Surg Am. 1975;57:287–297. [PubMed] [Google Scholar]
- 6.Grace T.G., Eversmann W.W. Jr Forearm fractures: treatment by rigid fixation with early motion. J Bone Joint Surg Am. 1980;62:433–438. [PubMed] [Google Scholar]
- 7.Tredgett M.W., Davis T.R.C. Rapid repeat testing of grip strength for detection of faked hand weakness. J Hand Surg Br. 2000;25:372–375. doi: 10.1054/jhsb.2000.0433. [DOI] [PubMed] [Google Scholar]
- 8.Mullerpatan R.P., Karnik G., John R. Grip and pinch strength: normative data for healthy Indian adults. Hand Ther. 2013;18(1):11–16. [Google Scholar]
- 9.Rosenberg N., Soudry M., Stahl S. Comparison of two methods for the evaluation of treatment in medial epicondylitis: pain estimation vs grip strength measurements. Arch Orthop Trauma Surg. 2004;124(6):363–365. doi: 10.1007/s00402-004-0658-5. [DOI] [PubMed] [Google Scholar]
- 10.Brumback R.J., Virkus W.W. Intramedullary nailing of the femur: reamed versus nonreamed. J Am Acad Orthop Surg. 2000;8:83–90. doi: 10.5435/00124635-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Lee Y.H., Lee S.K., Chung M.S. Interlocking contoured intramedullary nail fixation for selected diaphyseal fractures of the forearm in adults. J Bone Joint Surg Am. 2008;90:1891–1898. doi: 10.2106/JBJS.G.01636. [DOI] [PubMed] [Google Scholar]
- 12.Sage F.P., Smith H. Medullary fixation of forearm fractures. J Bone Joint Surg Am. 1957;39-A(1):91–98. [PubMed] [Google Scholar]
- 13.Köse A., Aydın A., Ezirmik N., Can C.E., Topal M., Tipi T. Alternative treatment of forearm double fractures: new design intramedullary nail. Arch Orthop Trauma Surg. 2014;134(10):1387–1396. doi: 10.1007/s00402-014-2058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bansal H. Intramedullary fixation of forearm fractures with new locked nail. Indian J Orthop. 2011;45:410–416. doi: 10.4103/0019-5413.83760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crenshaw A.H., Jr. Fractures of Shoulder, Arm and Forearm. In: Canale S.T., Daugherty K., Jones L., editors. Campbell’s Operative Orthopaedics. tenth ed. Mosby; St. Louis: 2003. pp. 3049–3058. [Google Scholar]
- 16.De Pedro J.A., Garcia-Navarrete F., Garcia De Lucas F. Internal fixation of ulnar fractures by locking nail. Clin Orthop Relat Res. 1992;283:81–85. [PubMed] [Google Scholar]
- 17.Leung F., Chow S.P. A prospective, randomized trial comparing the limited contact dynamic compression plate with the point contact fixator for forearm fractures. J Bone Joint Surg Am. 2003;85:2343–2348. doi: 10.2106/00004623-200312000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Visn’a P., Beitl E., Pilny ´ J. Interlocking nailing of forearm fractures. Acta Chir Belg. 2008;108:333–338. doi: 10.1080/00015458.2008.11680232. [DOI] [PubMed] [Google Scholar]
- 19.Shivakumar G.V., Afzal P.A., Naveen P.R., Manjunath M.L. A study on functional outcome of patients treated with interlock nailing in the forearm fracture bones. Indian J Orthop. 2016;2(4):313–317. [Google Scholar]
- 20.Ozkaya U., Kilic A., Ozdog ˘an U Comparison between locked intramedullary nailing and plate osteosynthesis in the management of adult forearm fractures. Acta Orthop Traumatol Turcica. 2009;43:14–20. doi: 10.3944/AOTT.2009.014. [DOI] [PubMed] [Google Scholar]
- 21.Azboy I., Demirtaş A., Alemdar C., Gem M., Uzel K., Arslan H. A newly designed intramedullary nail for the treatment of diaphyseal forearm fractures in adults. Indian J Orthop. 2017 Dec;51:697–703. doi: 10.4103/ortho.IJOrtho_79_16. [DOI] [PMC free article] [PubMed] [Google Scholar]