Abstract
Background
Although migraine is widespread and disabling, stigmatisation and poor awareness of the condition still represent barriers to effective care; furthermore, research on migraine individual and social impact must be enhanced to unveil neglected issues, such as caregiving burden. The project investigated the migraine illness experience through Narrative Medicine (NM) to understand daily life, needs and personal resources of migraneurs, their caregivers and clinicians, and to provide insights for clinical practice.
Methods
The project involved 13 Italian headache centres and targeted migraneurs, their caregivers and migraine specialists at these centres. Written narratives, composed by a sociodemographic survey and illness plot or parallel chart, were collected through the project’s webpage. Illness plots and parallel charts employed open words to encourage participants’ expression. Narratives were analysed through Nvivo software, interpretive coding and NM classifications.
Results
One hundred and seven narratives were collected from patients and 26 from caregivers, as well as 45 parallel charts from clinicians. The analysis revealed migraine perception in social, domestic and work life within the care pathway evolution and a bond between chaos narratives and day loss due to migraine; furthermore, narratives suggested the extent of the caregiving burden and a risk of underestimation of migraine burden in patients’ and caregivers’ life.
Conclusion
The project represents the first investigation on migraine illness experience through NM simultaneously considering migraneurs’, caregivers’ and clinicians’ perspectives. Comparing narratives and parallel charts allowed to obtain suggestions for clinical practice, while NM emerged as able to foster the pursuing of migraine knowledge and awareness.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10072-021-05227-w.
Keywords: Migraine, Narrative medicine, Doctor-patient relationship, Illness experience, Quality of life
Introduction
Migraine is a common neurological disorder, defined as a recurrent primary headache disorder [1]; it is experienced by the 14.7% of the global population [2] and has a lifetime incidence three times higher among women than men [3]. Migraine can vary in intensity and severity and is characterised by intolerable pain aggravated by movement and frequently accompanied by nausea, vomiting, photophobia, phonophobia and significant disturbance of usual activities [1]; attacks evolve within 4–72 h and commonly involve a premonitory, headache, and postdrome phase, while one-third of migraineurs experience an aura phase with reversible neurological symptoms [4, 5].
The primary prophylactic treatments in migraine are not specific as they have been designed for other diseases and then addressed to migraine [6], with a low treatment adherence and tolerability issues [7]; thus, new therapies addressed to modulate the Calcitonin Gene Related Peptide (CGRP) activity have opened a promising scenario for both acute and preventive treatment [8–10].
Although migraine is widespread and disabling, stigmatisation and poor awareness of the condition represent two barriers to effective treatment. Moreover, migraine is still misdiagnosed by non-specialised professionals and undertreated: a significant part of migraine patients has never consulted a healthcare specialist or has never been diagnosed, while undergoing unnecessary medical imaging, receiving inappropriate treatments, or self-treating [11–16].
Against this scenario, a broader culture of prevention and a multidisciplinary approach to migraine must integrate the clinical pathway [17]. Furthermore, research on migraine social impact must be enhanced to unveil neglected issues, such as caregiving experience [18]: even if studies in migraineur quality of life have increased [19, 20], the multifaceted burden of migraine [18] has leaded to fragmented results and interventions.
Narrative research has been addressed by the World Health Organisation (WHO) as informative for quality-of-life investigations in leading clinical practice [21]. In particular, Narrative Medicine (NM), based on illness narratives [22], pursues to integrate the disease-centred and biomedical approach with the illness-centred and sickness-centred approaches, respectively looking at the individual experience and the social meaning of a condition [23]. In research, NM indicates potential interventions on a specific condition through integrating the perspectives of all actors involved in the care pathway [24]. Results deriving from NM have been increasingly employed by scientific societies and healthcare facilities to improve the efficacy of healthcare services and quality of care [25].
The NM project “DRONE – Inside the Research: Observatory on Migraine Narratives” aimed to investigate the migraine illness experience by employing the analysis of narratives (a) to understand daily life, real needs and personal resources of migraineurs, their caregivers and clinicians within the evolution of the care pathway, and by doing so (b) providing insights to foster clinical practice as well as migraine knowledge and care. Although other narrative researches concerned the migraine illness experience [26, 27], this is the first project to address personal, relational and care aspects of migraine by considering at the same time these three different points of view.
Methods
Research design and setting
The project was conducted in Italy between December 2019 and October 2020 and targeted migraine patients, their caregivers, and expert clinicians in headache disorders. Thirteen headache centres were selected (Supplement 1), equally distributed among Northern, Central, and Southern Italy. In February 2020, clinicians from these centres underwent a webinar conducted by scholars from ISTUD Foundation to be trained in NM and on the project’s purposes, design and data collection tools. The clinicians were then invited to engage patients and their caregivers to join the research through the dedicated webpage www.medicinanarrativa.eu/drone.
A migraine diagnosis or the caregiving of a migraineur represented the eligibility criteria for patients and caregivers, as well the willingness to share by writing their illness experience; however, the ability to communicate in Italian was indispensable for the inclusion in the project.
Data collection
Written narratives were collected anonymously through the project’s webpage; patients described in parallel charts could not coincide with those who shared their experience. Next, raw and anonymous narratives were downloaded as a Microsoft Excel spreadsheet. A sociodemographic survey constituted the written narrative for patients and caregivers, together with an illness plot [28] aimed to chronologically guide the narrative to identify evolutions over time and characterised by evocative and open words to encourage individual expression [29]. Furthermore, parallel chart [22, 30] was addressed to collect clinicians’ experience: it constitutes a personal notebook to write reflections and feelings in plain language in addition to the technical reports of clinical chart [31]. These narrative tools (Supplement 2) were specifically designed for the three groups of participants while addressing common aspects: (a) the personal and social experience of migraine, (b) migraine management and the care pathway, and (c) the daily living with migraine, with a particular focus on work, domestic and relational spheres.
Data collection tools were created by three ISTUD researchers, different for academic backgrounds, and then reviewed within the project Steering Committee, involving three professionals in headache disorders, to reduce the cognitive bias.
Ethical considerations
The project was performed according to the Declaration of Helsinki. Before their involvement, participants provided web-based informed consent after being briefed on the project’s purposes and confidential data handling procedures, according to the Italian Law 196/2003 [32] and the General Data Protection Regulation of the European Union 2016/679 [33]. The Ethical Committee of the University Hospital of Rome Tor Vergata (Rome, Italy) approved the project in April 2020.
Analysis
ISTUD researchers analysed the sociodemographic survey through descriptive statistics; no question was mandatory. Anonymous narratives were entered into NVivo software for coding and analysis [34]. Ten narratives were collectively coded for each group to assess consistency across team members; afterwards, each narrative was coded separately and then reviewed within weekly peer debriefings to limit bias in the interpretation.
Researchers employed open interpretive coding to identify and analyse emerging topics, and retrospectively applied two classifications to the analysis of narratives:
Kleinman’s classification [23], which distinguishes among disease-, illness-, and sickness-related aspects in narratives, respectively concerning the biomedical description of the condition, its personal experience and its social perception.
Frank’s classification [35], which identifies chaos narratives, i.e. anti-narratives revealing vulnerability of the narrator, restitution narratives, i.e. when the narrator explores the care pathway experience and meaning, and quest narratives, i.e. when the condition is lived as a motivation for change.
Moreover, we asked participants to describe migraine through a metaphor, attempting to trace spontaneous meaning associations created through daily language.
Results from the analysis were shared with the Steering Committee to address emerged topics and data interpretation collectively.
Results
Sociodemographic aspects
One hundred and seven migraineurs and 26 caregivers (patients’ partners in 56% of cases) participated in the project, as well as 14 clinicians who wrote 45 parallel charts. Table 1 summarises participants’ sociodemographic data and includes non-responses as a separate category.
Table 1.
Sociodemographic data of participants
| Patients (N = 107) |
Caregivers (N = 26) |
Patients in parallel charts (N = 45) | Clinicians (N = 14) |
|
|---|---|---|---|---|
| Gender | ||||
| Women | 89 (83%) | 11 (42%) | 37 (82%) | 6 (43%) |
| Men | 18 (17%) | 15 (58%) | 8 (18%) | 8 (57%) |
| Average age (yrs) | ||||
| Mean (min-max) | 47 (16-80) | 47 (26-77) | 45 (12-80) | 57 (37-68) |
| Nationality | ||||
| Italian | 105 (98%) | 26 (100%) | 45 (100%) | 14 (100%) |
| European | 1 (1%) | – | – | – |
| Extra-European | 1 (1%) | – | – | – |
| Geographic residence | ||||
| Northern Italy | 49 (46%) | 15 (58%) | 22 (49%) | 4 (29%) |
| Central Italy | 24 (22%) | 6 (23%) | 11 (24%) | 6 (42%) |
| Southern Italy | 33 (31%) | 4 (15%) | 12 (27%) | 4 (29%) |
| Nonresponses | 1 (1%) | 1 (4%) | – | – |
| Education | ||||
| Elementary school | - | - | 1 (2%) | – |
| Middle school | 9 (8%) | 2 (8%) | 6 (14%) | – |
| High school | 45 (42%) | 12 (46%) | 19 (42%) | – |
| Bachelor/Master | 52 (49%) | 11 (42%) | 19 (42%) | – |
| Nonresponses | 1 (1%) | 1 (4%) | - | – |
| Employment status | ||||
| Student | 9 (8%) | – | 4 (9%) | – |
| Working | 79 (75%) | 15 (58%) | 32 (71%) | – |
| Not working | 9 (8%) | 2 (8%) | 5 (11%) | – |
| Retired | 8 (7%) | 6 (23%) | 4 (9%) | – |
| Nonresponses | 2 (2%) | 3 (11%) | – | – |
| Marital state | ||||
| Single | 65 (61%) | 2 (8%) | 16 (36%) | – |
| Married | 34 (31%) | 20 (77%) | 24 (53%) | – |
| Separated | 7 (7%) | 3 (11%) | 4 (9%) | – |
| Nonresponses | 1 (1%) | 1 (4%) | 1 (2%) | – |
| Professional activity (yrs) | ||||
| Mean (min-max) | – | – | – | 30 (11-40) |
| Specialisation | ||||
| Pharmacology | – | – | – | 1 (7%) |
| Neuropathology | – | – | – | 1 (7%) |
| Neurology | – | – | – | 12 (86%) |
| Workplace | ||||
| Hospital | – | – | – | 5 (36%) |
| University Hospital | – | – | – | 3 (21%) |
| Local Health Authority | – | – | – | 5 (36%) |
| Private practice | – | – | – | 1 (7%) |
Data presented as N (%) or mean (minimum-maximum)
Results are presented by following three main lines: (a) migraine illness experience analysed through NM classifications and metaphors; (b) migraine management and the evolution of care relationship; (c) migraine impact on activity, work and relational spheres. Figures 1, 2, 3, and 4 and Tables 2 and 4 provide quotes from narratives, while three extracts from participants’ narratives are available in Supplement 3; applied codes differ from those used to identify participants to reduce the risk of re-identification.
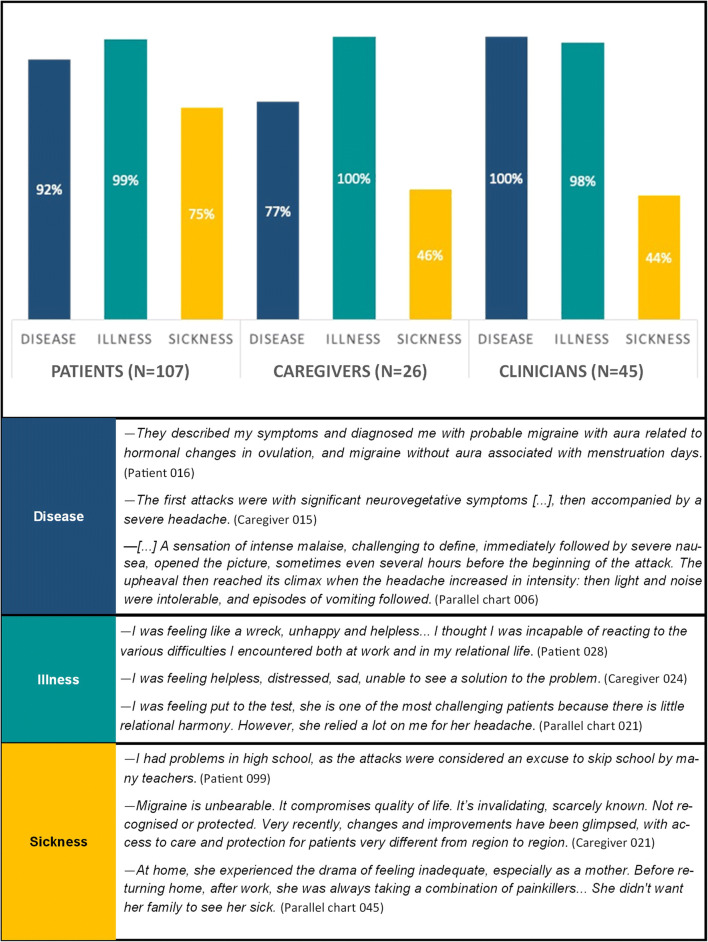
Fig. 1.
Disease-, illness, and sickness-related aspects: distribution and quotes from narratives
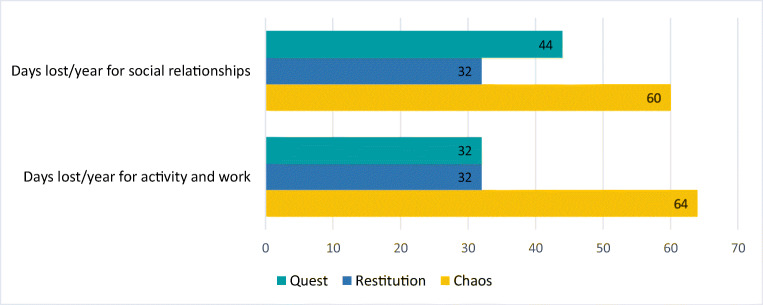
Fig. 2.
Chaos, restitution and quest narratives: distribution and quotes from narratives
Fig. 3.
Average lost days per year for activity/work and social relationships compared to Frank’s narrative classification
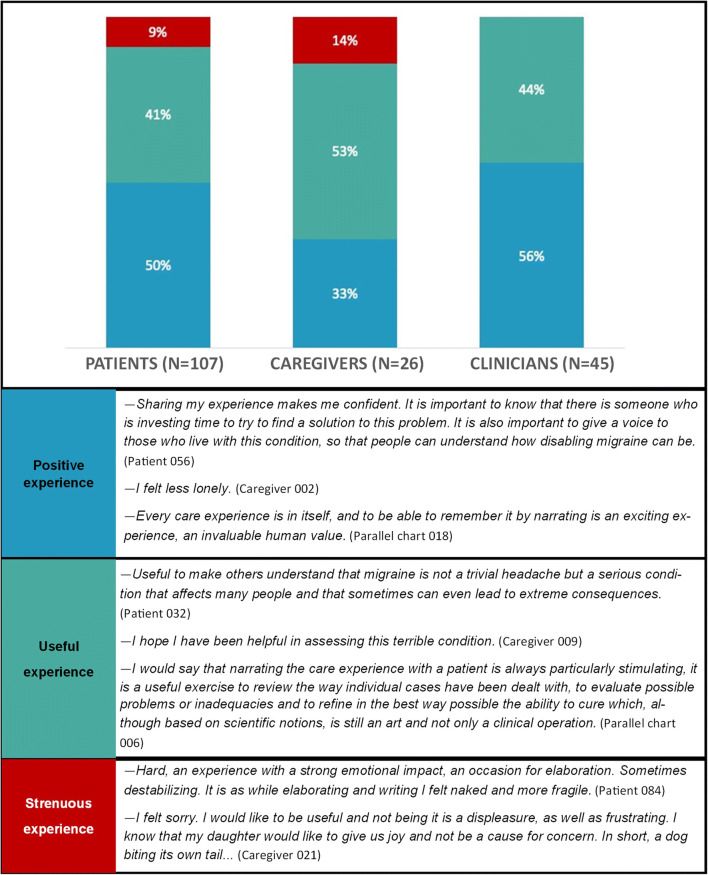
Fig. 4.
The narrating experience for participants: distribution and quotes from narratives
Table 2.
Living with migraine
| Patients (N = 107) |
Caregivers (N = 26) |
Patients in parallel charts (N = 45) |
|
|---|---|---|---|
| Average migraine duration (yrs) | |||
| Mean (min-max) | 27 (2-60) | 27 (0-50) | 21 (1-65) |
| Average episodes in a month | |||
| Mean (min-max) | 12 (0-31) | 12 (0-31) | 6 (1-25) |
| Specialist who made the diagnosis | |||
| Migraine specialist | 79 (74%) | – | – |
| Neurologist | 19 (18%) | – | – |
| General practitioner | 3 (3%) | – | – |
| Pharmacist | 2 (2%) | – | – |
| Not answered | 4 (4%) | – | – |
| Family member suffering of migraine | |||
| Yes | 78 (73%) | – | – |
| No | 27 (25%) | – | – |
| Not answered | 2 (2%) | – | – |
Data presented as N (%) or mean (minimum-maximum)
Table 4.
Improvements in activity, work and social spheres: distribution and quotes from narratives
| Improvements in domestic and work activities | 65% of patient narratives | —I continued to work, to care for my children. To do so, I was always making medicines varied. I started with nausea, discomfort, vomiting, tiredness, and I felt dull, without wanting to do anything. Then, when migraine became uncontrollable, I just wanted to get into the bed, holding my head and waiting for the effect of the intramuscular medication. Today I am active, more concentrated, I perform better, and I can prolong my activity without paying the consequences as before, that is to say, even if I get tired, I don't get migraines. (Patient 075). |
| 65% of caregiver narratives | —For the most part, she gave up any activity other than lying in bed. Now that she has understood when and how to deal with attacks, she can plan her different activities. (Caregiver 013) | |
| 93% of parallel charts | - The patient's work activities are also going better because her concentration has increased and she feels more ready in solving even difficult tasks, she is eating well, exercising and using fewer symptomatic medications. (Parallel Chart 010) | |
| Relational and social activities | 73% of patient narratives | —Before the attack, I was irritable, so the relationships at that time are compromised. In the days when the attacks are present, I cannot relate because the symptomatology forces me to isolate myself and stay in bed. [...] Today, I can also relate with others because I no longer see myself forced to be isolated and in the dark. (Patient 078) |
| 77% of caregiver narratives | —I felt and worried about our future life. She felt sick. [...] Today I feel decidedly happy, we have found our everyday life again. We go out for dinners and trips as we did twenty years ago, with an even more willing spirit. She feels very well, both physically and mentally. (Caregiver 007) |
The migraine experience through narratives and metaphors
Globally, almost all participants focused on illness-related facets [23] in narrating their stories, while technical and clinical language is less present in caregiver narratives (Fig. 1). Sickness-related aspects similarly emerged in 46% of caregiver narratives and 44% of parallel charts but were more remarkably present within patient narratives (75%), where incomprehension, inadequacy and sense of being discriminated represented three spontaneously emerged issues.
Restitution narratives [35] were prevalent among the three groups (Fig. 2). Caregivers reported no quest narratives, compared to 40% of clinicians and 7% of patients. Chaos narratives were lacking in parallel charts, while characterised 33% of patient and 15% of caregiver experiences.
Metaphors were clustered into four main thematic groups: (a) metaphors related to limitation and still life, mostly employed by caregivers (38%); (b) metaphors concerning malignant nature or entity, mainly used by patients (31%) and clinicians (30%); (c) metaphors referring the action of a hammer, pressure or pulsing, reported in particular by patients (30%) and clinicians (34%); (d) metaphors denoting stabbing and pain mostly employed by caregivers (25%); Supplement 4 provides distribution and examples of these four groups of metaphors. Only the remaining 5% of parallel charts reported positive or neutral metaphors to describe migraine (—My patient’s migraine could be described as an old friend, parallel chart 041).
Migraine management and care relationship
Within the survey, patients reported to have suffered from migraine, on average, from 27 years and to have 12 migraine episodes on average in a month; 74% received the diagnosis at the reference headache centre and 73% declared to have one or more family members suffering from migraine (Table 2).
As for migraine management previous to the current care pathway, three main issues spontaneously emerged from narratives: (a) 49% of patients’ narratives referred to a lack of confidence in previous clinicians, also reported in 31% of caregiver narratives and parallel charts; (b) 48% of patients reported the attitude to self-treat, as emerged in 8% of caregiver narratives and 40% of parallel charts; (c) 35% of patients declared to have overused medications for migraine management.
On the opposite, once the patients reached the headache centres, narratives showed a positive therapeutic pathway: 60% of patients and 58% of caregivers defined current therapies as effective, and respectively 25% and 21% stated they represent hope for a better quality of life; still, 15% of patients and 21% of caregivers reported that current therapies have no efficacy. Conversely, only 9% of parallel charts reported treatment inefficacy.
Indeed, care relationships showed to evolve positively: patients’ mistrust in healthcare professionals decreased from 56 to 5%, conversely trust increased from 44 to 95%. In parallel charts, clinicians indicated which communication and care strategies leaded them through the care pathway (Table 3). Beyond proposing (38%) and sharing a therapeutic path (43%), inviting patients to talk about their emotional state (24%) and listening to their migraine stories (36%) emerged as the leading strategies respectively in communication and care. Furthermore, in parallel charts, going beyond the clinical datum (37%) and actively listening and collaborating with patients emerged as the two main learnt attitudes during the care relationship. At the same time, the sense of improving patient quality of life (61%) and gratification (29%) represented the two main feelings reported by clinicians; in comparison, 33% of parallel charts indicated discomfort and impotence at the beginning of the care relationship. Furthermore, when asked within the survey, clinicians reported that their patients consider them as a reference point (65%), relief source (21%) and guardian angel (14%).
Table 3.
Clinicians’ strategies and learnt attitudes: distribution and quotes from narratives
| Communication strategies | Proposing therapeutic options (38%) | —I told her that we would have tried a new treatment and that I would have committed myself to improve her quality of life. (Parallel chart 021) |
| Inviting patients to share their feelings (24%) | —I tried to understand her discomfort, sharing her emotional state. (Parallel chart 003) | |
| Inviting to a therapeutic alliance (19%) | —I told her that we would go a long way together, that she would grow up and that I would help her to live in the most "normal" way possible, despite migraine. (Parallel chart 020) | |
| Fostering awareness (19%) | —I tried to reassure him; the condition was not invincible. It was enough to have some tricks: starting the therapy as soon as possible, at the first symptoms; avoiding, as far as possible, known triggering factors such as loss of sleep and alcohol. (Parallel chart 006) | |
| Care strategies | Sharing the therapeutic path (43%) | —I made her an appointment for the next day and put her last on the list, I knew the visit would have lasted an eternity! We analysed together the course of her migraine over time, the triggering and predisposing factors, the therapies used with risks and benefits obtained, her lifestyle, her "fears", her "false convictions", her mistakes... In the end, I clearly showed her what for me could be an "innovative" treatment programme, involving not only drugs but also psychological support. (Parallel chart 045) |
| Listening to patient migraine stories (36%) | —I let her talk about her anger towards doctors and the condition, her physical and psychological pain, her difficulties with family and at work. I explained what migraine is and its implications in everyday life. [...] I gave her a diary to record the attacks, the symptoms and to note down the triggering factors. [...] I let her come to the clinic after hours when she was feeling down or when she had doubts about the new therapy. (Parallel chart 001) | |
| Fostering correct information (21%) | —I gave her all the indications to try to control her headaches, averting severe crises, using ad hoc drugs that nip the pain in the bud, ensuring participation in sports and relational life. I also tried to involve and support the family, especially the mother, in the management of the little patient. (Parallel chart 042) | |
| Learnt attitudes | Going beyond clinical issues (37%) | —From this patient, but also from every patient, I learnt that we must go beyond the clinical history. We must never stop at the few words or the few elements that a patient provides to make a diagnosis. We must understand the complexity of a symptom that hides emotional problems, discomfort and even loneliness. We must not be in a hurry. The age of a person, young or old, does not count in the care relationship. (Parallel chart 018) |
| Listening and collaborating with patients (35%) | —[...] The most essential weapon, which cannot be touched or measured, in the daily fight against disease, is the doctor-patient alliance: you are not alone, everyone does their part, as a team. (Parallel chart 040) | |
| Having more patience (16%) | —I have learned to go beyond appearances, to be patient in moments of discouragement, to give myself and to her another chance; I have learned to cultivate hope. (Parallel chart 002) | |
| Aptness of care (12%) | —Data collection, interaction with the patient and evidence of limitations that the patient experiences are very useful in identifying treatment. (Parallel chart 019) |
Living with migraine in relational and work context
In the survey, 90% of patients stated that migraine negatively affected their domestic and work activities. Patients were asked to provide, on average, how many days of social and work activities they annually lose because of migraine. Considering these data together with narratives classified according to Frank [35], patients with chaos narratives revealed to have lost, annually, 64 days for domestic and work activities and 60 days for social activities, significantly differing from patients with restitution or quest narratives (Fig. 3).
In narratives, patients reported an overall improvement in social, domestic and work spheres (Table 4) along with the evolution of the care relationship; nonetheless, patients and of caregivers still experienced difficulties in relationships (respectively 27% and 23%) and fatigue in activities (35%). Notably, clinicians in parallel chart described patients that were able to recover in 92% of cases highlighting a strong difference in what is perceived as improvement by specialists and by patients and their caregivers.
Furthermore, in narratives, 67% of patients and 86% of caregivers reported that migraine negatively impacted their quality of life in terms of time and energy loss; nevertheless, migraine emerged as a stimulus to improve self-awareness for 51% of patients and 41% of caregivers.
Globally, the experience of writing and sharing their narratives was positive for participants (Fig. 4). In particular, 41% of patients, 53% of caregivers and 44% of clinicians referred to a sense of being useful for other people dealing with migraine; still, for 9% of patients and 14% of caregivers, the experience was difficult and challenging.
Discussion
The DRONE project represented the first effort to investigate the migraine illness experience in Italy through NM by considering, at the same time, the perspectives of migraineurs, their caregivers and clinicians.
In patients’ narratives, the coexistence of disease and illness dimensions [23] highlighted the bound between the clinical evolution of migraine and its individual and emotional experience: in this sense, narratives invite us to consider this condition as a psycho-biological unit and to address a global and patient-centred care. At the same time, sickness-related aspects in narratives suggest a demand for social and policy intervention: physical discomfort and pain interfere with patients’ relational and work activities, also confirming previous clinical studies reporting a decrease in work performances for migraineurs [36] with a high impact in terms of stigma [37]. NM classifications allowed to combine stigma with spontaneously emerged issues, namely feeling misunderstood, inadequate or not recognised as subject to a disabling condition. In line with what reported in literature [3], most patients are women of working age, at risk to undergo a double burden [18]. Migraineurs experience loneliness in familiar and work contexts, exclusion from the social sphere, and may feel they can rely only on their own migraine management strategies — as also suggested by the tendency, spontaneously emerged, to self-treat. Moreover, having one or more family members suffering from the same condition may influence them to consider migraine as a “normal” condition.
As emerged within the analysis, patients with chaos narratives [35] lose more days of social, domestic and work activities compared to those with restitution or quest narratives. This finding suggests a bond between the day loss and the capability to find a sequence and meaning in migraine experience — in which chaos can be intensified by both work absenteeism and presenteeism — and may foster other studies on the work impact of the condition [38].
Caregiver narratives are predominantly illness-centred and highlight the impotence and discomfort, as also suggested by the presence of chaos narratives. Caregivers, mostly patients’ partners, and whose participation is lower than in other NM projects [39], show to be deeply dedicated to their loved ones but do not mention their strategies and resources to deal with migraine experience; thus, sickness-related issues show that they also suffer from migraine social fallout, in line with studies urging to report migraine impact on caregiving [18]. Furthermore, caregivers’ spontaneous meaning association through metaphors reveals their involvement in understanding patients’ experience, as well for clinicians.
Findings from parallel charts show that an empathic relationship and therapeutic alliance can improve the care pathway and patient quality of life. Migraine specialists emerge as attentive to listening and communication, highlighting how migraine treatment should be considered not only a therapeutic outcome, but also (a) as integrated in a broader migraine culture, involving care humanisation and aptness [40], the centrality of therapeutic alliance and patient awareness, and (b) inclusive towards migraine illness and social experience of patients.
Data and narratives report positive evolution of care pathways. Nonetheless, a few issues need to be addressed as potential suggestions for migraine specialists:
There is a mistrust towards healthcare professionals and an abuse of self-medication in patients who suffer of migraine. Patients found relief when started their care pathway with the specialists of the headache centres, but they are still few compared to the amount of people affected by this disease. The underestimation and the sickness related to migraine are a strong barrier to the “on time treatment”.
Findings suggest a misalignment towards what clinicians, on the one side, and patients and caregivers, on the other side, consider as a positive evolution of the therapeutic pathway, as well as an improvement in relational and work spheres; if a misalignment can be reported by patients involved in a care pathway, it may arise to an even greater extent in patients who are discontinuously or not followed up. Consequently, the invitation may be that of evaluating the risk of underestimation of the criticalities concerning the migraine experience. Addressing patients’ emotional and social issues may help professionals in this path.
Since chaos narratives result as linked to challenging situations in terms of day loss, professionals may support patients towards restitution and quest narratives, also inviting them to consider migraine more as an ally than an enemy, as a stimulus towards self-knowledge and awareness, better lifestyle and prevention.
Caregiving burden is often neglected; nonetheless, caregivers participate to the patients’ migraine experience: they also need empathy and to be supported in finding personal resources to overcome fatigue.
These suggestions also indicate a limitation of the project: since narratives were anonymous, we are not able to precisely state the misalignment perceived between patients and caregivers on one side, and clinicians on the other side. Moreover, we involved only patients already attending headache centres and their caregivers: further investigations are needed (a) to intercept migraineurs who have not yet accessed these centres, as well as a broader number of caregivers, and (b) to examine to a greater extent issues spontaneously emerged. Finally, data collection phase partially corresponded to the lockdown measures decided by the Italian government to contain the Sars-Cov-2 pandemic spread which had consequence not only on the management of the disease and the participation to the project but on patients themselves [41].
Conclusion
The DRONE project aimed to investigate migraine illness experience to understand daily life, needs and personal resources of migraineurs, their caregivers and clinicians within the evolution of the care pathway, and represented the first Italian project to simultaneously addressing these three perspectives, integrating them and giving voice to this condition in terms of identity and dignity.
Narrative emerged as crucial for in-depth analysis and self-knowledge, while reconnecting the migraine physical experience to emotional and social issues concerning this condition. Comparing narratives and parallel charts allowed to obtain suggestions for clinical practice and insights for migraine knowledge.
NM allowed to foster the pursuing of a migraine culture and awareness encompassing patients, caregivers, neurologists, and other healthcare providers up to general practitioners, to acknowledge the burden and address the stigma peculiar to this condition.
Supplementary Information
(PDF 81 kb)
(PDF 111 kb)
(PDF 99 kb)
(PDF 126 kb)
Acknowledgements
This work was sponsored and funded by Novartis Farma. The authors wish to thank Vincenza Vinaccia for editorial assistance. The authors would also thank the researchers of Healthcare Area of ISTUD Foundation for their useful role throughout the project and all the people suffering from migraine, their caregivers and physicians who took part to the research.
Abbreviations
- WHO
World Health Organisation
- NM
Narrative Medicine
Author contribution
AC, AF, EG, IR, MGM, RT, MCT and MZ were involved in the project conceptualisation. AC, AF and MGM were involved in methodology. MA, GA, FB, TC, FF, LC, RI, CM, FM, MGP, AR, MCT and MZ contributed to project investigation. AC and AF were involved in project administration. AC, AF, MGM and MCT contributed to data analysis. MA, GA, MAB, FB, TC, FF, LG, EG, RI, CM, FM, MGP, RR, AR, MCT, RT and MZ contributed to data validation. AF and RR were involved in writing; all authors contributed to report visualisation and read and approved the final draft for submission.
Funding
The work was unconditionally supported by Novartis Farma Italia, since Fondazione ISTUD is a not-for-profit organization. The funder had no role in data collection and analysis and in the decision to publish this project.
Data availability
All datasets used and analysed during the current research are available in Italian from the corresponding author upon reasonable request.
Declarations
Ethical approval
The project was performed according to the Declaration of Helsinki. The Ethical Committee of the University Hospital of Rome Tor Vergata (Rome, Italy) approved the project in April 2020 (protocol 59/20).
Consent to participate
Before their involvement, participants provided web-based informed consent after being briefed on the project’s purposes and confidential data handling procedures according to the Italian Law 196/2003 and the General Data Protection Regulation of the European Union 2016/679.
Consent for publication
Not applicable.
Conflict of interest
AC, AF, and MGM report grants from Novartis Farma Italy during the conduct of the project. The funder provided support in the form of salaries for RR, EG, MAB, and RT. RI reports compensations from Teva, Eli Lilly, Novartis, and Allergan for having participated to their meetings; MGP also reports compensation from Teva, Eli Lilly and Novartis for speaking and congress participation. The authors report no other conflicts of interests in this work.
Informed consent statement
Before their involvement, participants provided web-based informed consent after being briefed on the project’s purposes and confidential data handling procedures, according to the Italian Law 196/2003 and the General Data Protection Regulation of the European Union 2016/679.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Headache Classification Committee of the International Headache Society (HIS) The international classification of headache disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2016 Disease and Injury and Prevalence Collaborators Global regional and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dodick DW. A phase-by-phase review of migraine pathophysiology. Headache. 2018;58(Suppl 1):4–16. doi: 10.1111/head.13300. [DOI] [PubMed] [Google Scholar]
- 4.Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev. 2017;97:553–622. doi: 10.1152/physrev.00034.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lionetto L, Borro M, Curto M, Capi M, Negro A, Cipolla F, Gentile G, Martelletti P. Choosing the safest acute therapy during chronic migraine prophylactic treatment: pharmacokinetic and pharmacodynamic considerations. Expert Opin Drug Metab Toxicol. 2016;12:399–406. doi: 10.1517/17425255.2016.1154042. [DOI] [PubMed] [Google Scholar]
- 6.Hepp Z, Dodick DW, Varon SF, Chia J, Matthew N, Gillard P, Hansen RN, Devine EB. Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: a retrospective claims analysis. Cephalalgia. 2017;37(5):470–485. doi: 10.1177/0333102416678382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blumenfeld AM, Bloudek LM, Becker WJ, Buse DC, Varon SF, Maglinte GA, Wilcox TK, Kawata AK, Lipton RB. Patterns of use and reasons for discontinuation of prophylactic medications for episodic migraine and chronic migraine: results from the second international burden of migraine study (IBMS-II) Headache. 2013;53(4):644–655. doi: 10.1111/head.12055. [DOI] [PubMed] [Google Scholar]
- 8.Russo A. Calcitonin gene-related peptide (CGRP): a new target for migraine. Annu Rev Pharmacol Toxicol. 2015;55:533–552. doi: 10.1146/annurev-pharmtox-010814-124701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giamberardino MA, Martelletti P. Emerging drugs for migraine treatment. Expert Opin Emerg Drugs. 2015;20(1):137–147. doi: 10.1517/14728214.2015.999040. [DOI] [PubMed] [Google Scholar]
- 10.Huan IH, Wu PC, Lin EY, et al. Effects of anti-calcitonin gene-related peptide for migraines: a systematic review with meta-analysis of randomized clinical trials. Int J Mol Sci. 2019;20(14):3527. doi: 10.3390/ijms20143527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dodick DW, Tepper SJ, Lipton RB, Buse DC, Stewart WF, Bayliss M, Desai P, Sapra S, Anderson K, McInerney-Prichard E. Improving medical communication in migraine management: a modified Delphi study to develop a digital migraine tracker. Headache. 2018;58(9):1358–1372. doi: 10.1111/head.13426. [DOI] [PubMed] [Google Scholar]
- 12.Viana M, Khaliq F, Zecca C, Figuerola MDL, Sances G, di Piero V, Petolicchio B, Alessiani M, Geppetti P, Lupi C, Benemei S, Iannacchero R, Maggioni F, Jurno ME, Odobescu S, Chiriac E, Marfil A, Brighina F, Barrientos Uribe N, Pérez Lago C, Bordini C, Lucchese F, Maffey V, Nappi G, Sandrini G, Tassorelli C. Poor patient awareness and frequent misdiagnosis of migraine: findings from a large transcontinental cohort. Eur J Neurol. 2020;27(3):536–541. doi: 10.1111/ene.14098. [DOI] [PubMed] [Google Scholar]
- 13.Dodick DW, Loder EW, Manack Adams A, Buse DC, Fanning KM, Reed ML, Lipton RB. Assessing barriers to chronic migraine consultation, diagnosis, and treatment: results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache. 2016;56(5):821–834. doi: 10.1111/head.12774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller S, Matharu MS. Migraine is underdiagnosed and undertreated. Practitioner. 2014;258(1774):19–24. [PubMed] [Google Scholar]
- 15.Cevoli S, D’Amico D, Martelletti P, et al. Underdiagnosis and undertreatment of migraine 85 in Italy: a survey of patients attending for the first time 10 headache centres. Cephalalgia. 2009;29(12):1285–1293. doi: 10.1111/j.1468-2982.2009.01874.x. [DOI] [PubMed] [Google Scholar]
- 16.Brusa P, Allais G, Scarinzi C, Baratta F, Parente M, Rolando S, Gnavi R, Spadea T, Costa G, Benedetto C, Mana M, Giaccone M, Mandelli A, Manzoni GC, Bussone G. Self-medication for migraine: a nationwide cross-sectional study in Italy. PLoS One. 2019;14(1):e0211191. doi: 10.1371/journal.pone.0211191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agostoni EC, Barbanti P, Calabresi P, et al. Current and emerging evidence-based treatment options in chronic migraine: a narrative review. J Headache Pain. 2019;20(1):92. doi: 10.1186/s10194-019-1038-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leonardi M, Raggi A. A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain. 2019;20(1):41. doi: 10.1186/s10194-019-0993-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leonardi M, Raggi A, Bussone G, D’Amico D. Health-related quality of life, disability and severity of disease in patients with migraine attending to a specialty headache centre. Headache. 2010;50(10):1576–1586. doi: 10.1111/j.1526-4610.2010.01770.x. [DOI] [PubMed] [Google Scholar]
- 20.Raggi A, Giovannetti AM, Quintas R, D’Amico D, Cieza A, Sabariego C, Bickenbach JE, Leonardi M. A systematic review of the psychosocial difficulties relevant to patients with migraine. J Headache Pain. 2012;13(8):595–606. doi: 10.1007/s10194-012-0482-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenhalgh T. Cultural contexts of health: the use of narrative research in the health sector. Copenhagen: WHO Regional Office for Europe; 2016, Health Evidence Network (HEN) synthesis report 49. http://www.euro.who.int/__data/assets/pdf_file/0004/317623/HEN-synthesis-report-49.pdf. Last accessed on December 16, 2020 [PubMed]
- 22.Marini MG. Narrative Medicine: bridging the gap between evidence-based care and medical humanities. London: Springer International Publishing; 2016. [Google Scholar]
- 23.Kleinman A. The illness narrative, suffering and healing the human condition. New York: Basic Book; 1989. [Google Scholar]
- 24.Greenhalgh T, Hurwitz B. Why study narrative? BMJ. 1999;318:48–50. doi: 10.1136/bmj.318.7175.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marini MG. Languages of care in narrative medicine. words, space and time in the healthcare ecosystem. London: Springer International Publishing; 2019. [Google Scholar]
- 26.Grazzi L, Covelli V, Memini F, Rizzoli PB. Deeper inside the experience of pediatric headache: a narrative study. Journal of Behavioral and Brain Sciences. 2020;10:432–454. doi: 10.4236/jbbs.2020.1010028. [DOI] [Google Scholar]
- 27.Scaratti C, Covelli V, Guastafierro E, Leonardi M, Grazzi L, Rizzoli PB, D’Amico D, Raggi A. A qualitative study on patients with chronic migraine with medication overuse headache: comparing frequent and non-frequent relapsers. Headache. 2018;58(9):1373–1388. doi: 10.1111/head.13385. [DOI] [PubMed] [Google Scholar]
- 28.Reid K, Soundy A. A qualitative study examining the illness narrative master plots of people with head and neck cancer. Behav Sci. 2019;9:110. doi: 10.3390/bs9100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peeters B, Marini M. Narrative medicine across languages and cultures: using minimal English for increased comparability of patients’ narratives. In: Goddard C, editor. Minimal English for a Global World: Improved Communication Using Fewer Words. Basingstoke: Palgrave Macmillan; 2018. pp. 259–286. [Google Scholar]
- 30.Charon R. The patient-physician relationship. Narrative Medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286:1897–1902. doi: 10.1001/jama.286.15.1897. [DOI] [PubMed] [Google Scholar]
- 31.Banfi P, Cappuccio A, Latella ME, Reale L, Muscianisi E, Marini MG. Narrative medicine to improve the management and quality of life of patients with COPD: the first experience applying parallel chart in Italy. Int J Chron Obstruct Pulmon Dis. 2018;13:287–297. doi: 10.2147/COPD.S148685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Personal data code protection. Legislat. Decree no. 196 of 30 June 2003. Published on the Italian Official Journal n. 174, July 29, 2003, Supplementary n. 123. https://www.camera.it/parlam/leggi/deleghe/Testi/03196dl.htm. Last accessed on December 16, 2020
- 33.Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data and repealing Directive 95/46/EC (General Data Protection Regulation. Published on the Official Journal of the European Union L 119, May 4, 2016. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32016R0679. Last accessed on December 16, 2020
- 34.Bazeley P, Jackson K. Qualitative data analysis with NVivo. London: SAGE; 2013. [Google Scholar]
- 35.Frank AW. The wounded storyteller: body, illness, and ethics. Chicago: University of Chicago Press; 2013. [Google Scholar]
- 36.D’Amico D, Genco S, Perini F. Workplace disability in migraine: an Italian experience. Neurol Sci. 2004;25:S251–S252. doi: 10.1007/s10072-004-0299-z. [DOI] [PubMed] [Google Scholar]
- 37.Young WB, Park JE, Tian IX, Kempner J. The stigma of migraine. PLoS One. 2013;8(1):e54074. doi: 10.1371/journal.pone.0054074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raggi A, Covelli V, Guastafierro E, Leonardi M, Scaratti C, Grazzi L, Bartolini M, Viticchi G, Cevoli S, Pierangeli G, Tedeschi G, Russo A, Barbanti P, Aurilia C, Lovati C, Giani L, Frediani F, di Fiore P, Bono F, Rapisarda L, D’Amico D. Validation of a self-reported instrument to assess work-related difficulties in patients with migraine: the HEADWORK questionnaire. J Headache Pain. 2018;19(1):85. doi: 10.1186/s10194-018-0914-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gatti V, Banfi P, Centanni S, D’Antonio S, Saffi Giustini E, Piraino A, et al. Enlightening chronic obstructive pulmonary disease through patients’ and caregivers’ narratives. Int J Chron Obstruct Pulmon Dis. 2018;13:3095–3105. doi: 10.2147/COPD.S172214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tonini MC, Chesi P. Narrative Medicine, an innovative approach to migraine management. Neurol Sci. 2018;39(Suppl 1):137–138. doi: 10.1007/s10072-018-3377-3. [DOI] [PubMed] [Google Scholar]
- 41.Parodi IC, Poeta MG, Assini A, Schirinzi E, del Sette P. Impact of quarantine due to COVID infection on migraine: a survey in Genova Italy. Neurol Sci. 2020;41:2025–2027. doi: 10.1007/s10072-020-04543-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 81 kb)
(PDF 111 kb)
(PDF 99 kb)
(PDF 126 kb)
Data Availability Statement
All datasets used and analysed during the current research are available in Italian from the corresponding author upon reasonable request.