This secondary analysis of the FISH randomized clinical trial compares the 2-year outcomes of patients who required secondary surgery with the outcomes of patients with successful initial operative or nonoperative treatment.
Key Points
Question
Do patients who require secondary surgery after initial nonoperative treatment of closed humeral shaft fracture have inferior outcomes compared with those who undergo uneventful fracture healing after initial operative or nonoperative treatment?
Findings
In this 2-year follow-up of the Finnish Shaft of the Humerus (FISH) randomized clinical trial comparing surgery with nonoperative functional treatment among 82 adults with humeral shaft fractures, 30 of 44 patients (68%) allocated to nonoperative treatment healed uneventfully with similar results as the patients undergoing initial surgery. However, the 2-year functional outcomes (group means using the Disabilities of Arm, Shoulder and Hand score; range, 0 to 100 points; minimal clinically important difference, 10 points) of patients who required secondary surgery (17.5 points) were statistically significantly inferior compared with those who underwent uneventful fracture healing after initial surgery (6.8 points) and after successful nonoperative functional bracing (6.0 points).
Meaning
Nonoperatively treated patients who experienced fracture healing problems that required secondary surgery had inferior outcomes at 2-year follow-up compared with patients whose fractures healed successfully, irrespective of whether the latter were initially treated with surgery or with functional bracing.
Abstract
Importance
Existing evidence indicates that surgery fails to provide superior functional outcome over nonoperative care in patients with a closed humeral shaft fracture. However, up to one-third of patients treated nonoperatively may require secondary surgery.
Objective
To compare the 2-year outcomes of patients who required secondary surgery with the outcomes of patients with successful initial treatment.
Design, Setting, and Participants
This 2-year follow-up of the Finnish Shaft of the Humerus (FISH) randomized clinical trial comparing surgery with nonoperative treatment (functional brace) was completed in January 2020. Enrollment in the original trial was between November 2012 and January 2018 at 2 university hospital trauma centers in Finland. A total of 321 adult patients with closed, displaced humeral shaft fracture were assessed for eligibility. After excluding patients with cognitive disabilities, multimorbidity, or multiple trauma and those refusing randomization, 82 patients were randomized.
Interventions
Interventions were surgery with plate fixation (n = 38; initial surgery group) or functional bracing (n = 44); the latter group was divided into the successful fracture healing group (n = 30; bracing group) and the secondary surgery group (n = 14) with fracture healing problems.
Main Outcomes and Measures
The primary outcome was Disabilities of Arm, Shoulder and Hand (DASH) score at 2 years (range, 0 to 100 points; 0 denotes no disability, 100 extreme disability; minimal clinically important difference, 10 points).
Results
Of 82 randomized patients, 38 (46%) were female. The mean (SD) age was 48.9 (17.1) years. A total of 74 patients (90%) completed the 2-year follow-up. At 2 years, the mean DASH score was 6.8 (95% CI, 2.3 to 11.4) in the initial surgery group, 6.0 (95% CI, 1.0 to 11.0) in the bracing group, and 17.5 (95% CI, 10.5 to 24.5) in the secondary surgery group. The between-group difference was −10.7 points (95% CI, −19.1 to −2.3; P = .01) between the initial and secondary surgery groups and −11.5 points (95% CI, −20.1 to −2.9; P = .009) between the bracing group and secondary surgery group.
Conclusions and Relevance
Patients contemplating treatment for closed humeral shaft fracture should be informed that two-thirds of patients treated with functional bracing may heal successfully while one-third may experience fracture healing problems that require secondary surgery and lead to inferior functional outcomes 2 years after the injury.
Trial Registration
ClinicalTrials.gov Identifier: NCT01719887
Introduction
Two existing randomized clinical trials comparing functional bracing with surgery in the treatment of humeral shaft fractures found no clinically important differences in patient-reported outcomes at 1-year follow-up.1,2 Many would argue that these findings unequivocally favor nonoperative treatment as the first-line treatment for these fractures. However, such inference may be somewhat oversimplified. The caveat to this apparently straightforward strategy is that up to one-third of patients who are initially treated nonoperatively may end up requiring secondary surgery to heal the fracture.3,4,5,6,7 According to our recently published Finnish Shaft of the Humerus (FISH) randomized clinical trial, patients who experienced compromised healing with initial functional bracing had inferior functional outcomes.2
Prompted by this concerning preliminary finding, we carried out a prespecified secondary analysis of the 2-year follow-up data of the FISH trial that specifically addressed this issue. We compared the functional outcomes of patients who required secondary surgery after initial functional bracing with the functional outcomes of patients whose fractures healed successfully, irrespective of whether the latter were initially treated with surgery or with functional bracing.
Methods
Trial Design, Participants, and Interventions
The study design, rationale, and methods of the FISH trial were reported previously.2 The trial protocol8 was approved by the institutional review board of the Helsinki and Uusimaa Hospital District and can be found in Supplement 1. The study was conducted in accordance with the Declaration of Helsinki. All patients gave written informed consent. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
The FISH trial was a multicenter, randomized clinical superiority trial conducted at Helsinki University Hospital and Tampere University Hospital in Finland. Patient recruitment took place from November 2012 to January 2018. Adult patients with unilateral, displaced, and closed humeral shaft fracture were randomized to surgery with open reduction and plate fixation or nonsurgical treatment with functional bracing. Exclusion criteria included history or condition affecting the function of the injured upper limb, pathological fracture, other concomitant injury affecting the same upper limb, other trauma requiring surgery (fracture, internal organ, brachial plexus, or vascular injury), multiple trauma, multimorbidity with high anesthesia risk, or inadequate cooperation for any reason, for example, substance misuse or dementia. Detailed inclusion and exclusion criteria are shown in eTable 1 in Supplement 2. In the surgery group, the surgery was performed either by or under the supervision of an experienced attending orthopedic trauma surgeon using open reduction and plate fixation. In the bracing group, a trained plaster technician applied a functional brace covering the arm from shoulder to elbow but left the motion of both of these joints free. Both groups received written information on early mobilization according to a structured rehabilitation program (eTables 2 and 3 in Supplement 2) and met with a physical therapist at 3 and 9 weeks. Patients with healing problems were treated according to the preference of the treating surgeon. The initial follow-up time points were at 6 weeks and 3, 6, and 12 months, and we reported these results previously.2
The 2-year follow-up was completed in January 2020. The objective of the 2-year follow-up was to compare the functional outcomes of patients who experienced compromised fracture healing after initial functional bracing and required secondary surgery with the outcomes of those who experienced successful fracture healing, irrespective of the initial treatment modality.
Randomization
Patients were randomized in a block size of 4 by a closed envelope method using separate computer-generated randomization lists for both study centers.8 Two-fold stratification was used: status of the radial nerve (intact, paresthesia, or mild motor deficit; subtotal or total motor palsy) and fracture type classified according to the AO Foundation/Orthopaedic Trauma Association (AO/OTA) as either type A (simple fracture), or type B (separate wedge fragment) or C (segmental fracture).9 After obtaining consent, a surgeon-member of the study group (L.P., M.P., B.S., V.L., and T.L.) randomized participants by opening the next available numbered envelope to undergo either surgery or functional bracing.
Declined Cohort
Eligible patients who were not willing to be randomized were offered the option to participate in a concurrent prospective observational cohort (declined cohort). Participants who consented to participate in this cohort received standard care (either surgery or bracing) according to their preference and were monitored in the same way as the randomized patients.
Outcomes
The primary outcome in the FISH trial was Disabilities of Arm, Shoulder and Hand (DASH) score at 12 months. DASH is a widely used patient-reported outcome measure for upper limb–related physical function and symptoms (range, 0 to 100; 0 denotes no disability and 100 extreme disability; minimal clinically important difference [MCID], 10 points).10,11 The predefined secondary end points were 2, 5, and 10 years.
Secondary outcomes included pain at rest and pain on activities, both measured using a numerical rating scale from 0 to 10; the Constant-Murley score,12,13 a widely used shoulder function score (range, 0 to 100; higher scores denote better function; MCID, 8.3 points); elbow range of motion; DASH work and sports/performing arts modules (Table 1); and 15D score,14 a generic health-related quality of life instrument (range, 0 to 1; higher scores denote better quality of life; MCID, 0.03 points15). The patients’ general satisfaction with the function of the shoulder, elbow, and the entire injured upper limb was assessed on a numerical rating scale from 0 to 10. The proportion of patients with an acceptable symptomatic state was determined using patients’ global assessment of satisfaction regarding the injured arm, based on their answer to the question, “How satisfied are you with the overall condition of your injured upper limb and its effect on your daily life?” Responses were given on a 7-point Likert scale. Very satisfied and satisfied were categorized as having an acceptable symptomatic state, and somewhat satisfied, neither satisfied nor dissatisfied, somewhat dissatisfied, dissatisfied, and very dissatisfied were categorized as not having an acceptable symptomatic state. The proportion of clinically recovered patients was determined at each follow-up time point. Patients reporting a DASH score within MCID (10 points) of their preinjury score were considered to have adequate clinical recovery. The patients were also asked at 2 years whether they would choose the same treatment again if they sustained a similar injury again (yes or no).
Table 1. Baseline Demographic and Clinical Characteristicsa.
| Characteristic | No. (%) | |||
|---|---|---|---|---|
| Randomized to surgery (initial surgery group) (n = 38) | Randomized to bracing (n = 44) | Declined cohort (n = 42) | ||
| Bracing group (n = 30) | Secondary surgery group (n = 14) | |||
| Age at allocation, mean (SD; range), y | 49.6 (18.2; 19-81) | 44.8 (16.7; 19-80) | 56.0 (12.4; 34-74) | 44.6 (17.3; 20-83) |
| Female | 18 (47.4) | 13 (43.3) | 6 (42.9) | 16 (38.1) |
| Weight, mean (SD), kg | 83.5 (21.2) | 87.4 (16.4) | 80.0 (13.0) | 84.4 (17.2) |
| Height, mean (SD), cm | 173 (9) | 174 (9) | 172 (11) | 175 (10) |
| BMI, mean (SD) | 27.7 (5.9) | 28.6 (4.2) | 26.9 (3.7) | 27.4 (4.4) |
| Cigarette use | 12 (31.6) | 5 (16.7) | 4 (28.6) | 10 (23.8) |
| Radial nerve palsyb | 3 (7.9) | 1 (3.3) | 1 (7.1) | 3 (7.1) |
| AO/OTA classification9 | ||||
| Type A (simple) | 34 (89.5) | 26 (86.7) | 10 (71.4) | 30 (68.2) |
| Type B (wedge fragment) | 4 (10.5) | 3 (10.0) | 4 (28.6) | 11 (25.0) |
| Type C (segmental) | 0 | 1 (3.3) | 0 | 1 (2.2) |
| Fracture locationc | ||||
| Proximal shaft | 2 (5.3) | 1 (3.3) | 4 (28.6) | 2 (4.8) |
| Midshaft | 35 (92.1) | 27 (90.0) | 10 (71.4) | 32 (76.2) |
| Distal shaft | 1 (2.6) | 2 (6.7) | 0 | 8 (19.0) |
| Injury mechanismd | ||||
| Low energy | 34 (89.5) | 26 (86.7) | 12 (85.7) | 38 (90.5) |
| High energy | 4 (10.5) | 4 (13.3) | 2 (14.3) | 4 (9.5) |
| Dominant limb injured | 20 (52.6) | 13 (43.3) | 5 (35.7) | 22 (52.4) |
| Preinjury DASH score, median (IQR)e | 0 (0-2.5) | 0 (0-2.5) | 0.8 (0-3.5) | 0.4 (0-1.9) |
| Preinjury DASH optional work module score, mean (SD; No.)f | 0 (0; 26) | 0.3 (1.5; 18) | 0 (0; 9) | 0.2 (1.2; 28) |
| Preinjury DASH optional sports/performing arts module score, mean (SD; No.)f | 0 (0; 23) | 0.4 (1.6; 15) | 0 (0; 4) | 1.0 (3.4; 26) |
| Preinjury 15D score, mean (SD)g | 0.95 (0.05) | 0.96 (0.04) | 0.91 (0.06) | 0.94 (0.09) |
Abbreviations: AO/OTA, the AO Foundation/Orthopaedic Trauma Association; BMI, body mass index, calculated as weight in kilograms divided by height in meters squared; DASH, Disabilities of Arm, Shoulder and Hand; IQR, interquartile range.
Patients were included in the initial surgery and bracing groups by randomization. The patients in the secondary surgery group were randomized to bracing but underwent secondary surgery to promote the healing of the fracture during the follow-up period.
Patients were categorized as having radial nerve palsy when subtotal or total motor palsy was noted. Normal function, mild motor weakness, and sensory disturbance were categorized as no radial nerve palsy. Patients were stratified according to radial nerve status.
Fracture location was defined by the third of the diaphysis where the center of the fracture was located.
Injury mechanism was classified as high energy if the height of fall was greater than standing height or if the fracture was sustained in a traffic crash.
DASH score is a widely used and validated tool assessing upper extremity–related deficits and symptoms in daily life as reported by the patient. The instrument consists of 30 items. The range of the score is from 0 (no disability) to 100 (extreme disability). Values less than 10 points represent a mean value in a randomly selected population aged between 20 and 60 years. A difference of 10 points is generally regarded as a minimal clinically important difference. At baseline, patients were asked to report their score just before the fracture. A DASH score may not be calculated if there are more than 3 missing items (see eTable 6 in Supplement 2 for missing data).
DASH work and sports/performing arts modules are optional modules comprising 4 questions assessing the effect of upper extremity condition on the work and sports or performing arts activities of the individual. The range of the score is from 0 (no disability) to 100 (extreme disability). Values less than 10 points indicate that the individual can work or participate in sports or performing arts with minimal limitations at most. An optional module score may not be calculated if there are any missing items.
The 15D instrument is a generic health-related quality of life instrument comprising 15 dimensions. The maximum 15D score is 1 (full health), and the minimum score is 0 (death). Values greater than 0.9 in 15D are comparable with those of a randomly selected Finnish population of individuals 30 years and older. At baseline, patients were asked to report their score just before the fracture.
The questionnaires were administered at baseline and at each follow-up visit at 6 weeks and 3, 6, and 12 months, as reported previously,2 and at 2 years after randomization (eTable 4 in Supplement 2). At baseline, we collected data on demographic and clinical characteristics and asked patients to recall their status prior to their fracture using DASH and 15D questionnaires. At each follow-up visit, we assessed fracture union and potential complications, such as implant failure, malunion, and refracture, both clinically and using anteroposterior and lateral radiographs. A trained physical therapist measured/determined the range of motion of the shoulder and elbow using a goniometer and shoulder strength with the Constant-Murley score using a calibrated spring balance.
We collected data on complications, adverse events, and reoperations from medical reports. Adverse events were categorized as serious or minor. For the adjudication of fracture nonunion and malunion, a panel of 5 experienced orthopedic surgeons assessed all radiographs and patient reports. Nonunion was defined as no fracture bridging callus in 3 of the 4 cortices in anteroposterior and lateral radiographs taken at 3 months or later following the fracture and clinically verified motion at the fracture site. To blind the outcome assessors to the treatment group allocation during the follow-up appointments, patients were asked to remove the brace (nonoperatively treated), to wear a long-sleeved shirt, and to not verbally reveal their study group.
Statistical Analysis
This prespecified secondary analysis of the FISH trial was designed to ascertain whether functional outcomes after 2 years differed between patients who required secondary surgery after initial functional bracing and those with uneventful fracture healing. The participants were analyzed in 3 groups: an initial surgery group, a bracing group with successful healing, and a secondary surgery group consisting of patients initially allocated to functional bracing but who underwent secondary surgery to promote fracture healing during the 2-year follow-up period. Because of the potential for type I error with multiple comparisons, findings for the analyses should be interpreted as exploratory. In addition, we carried out 2 preplanned sensitivity analyses: patients were analyzed according to their randomization groups (intention-to-treat analysis) and per latest treatment modality (surgery or nonoperative; as-treated analysis) at the different follow-up time points. The FISH trial was originally designed to ascertain whether surgery is more effective than functional bracing at 12 months after randomization with regard to the primary outcome, namely DASH score. With 80 patients, the FISH trial was powered to detect a 10-point difference in the DASH score between groups.2
The comparison between the study groups was performed using a mixed-model repeated-measures analysis of variance, which can be used to analyze unbalanced data sets where some observations are missing, assuming missingness at random. No data were imputed. Patients with at least some data were included in the analyses. Study group, time of assessment (baseline; 6 weeks; 3, 6, and 12 months; and 2 years), and study site were included as fixed factors, patients as random factors. The model included interactions between study group and time of assessment. Change from baseline was estimated with baseline value as the covariate. The model was used to quantify the treatment effect as the difference in DASH score (mean and 95% CI) between the groups at 2 years after randomization. A similar model was used to analyze secondary outcomes where applicable (pain numerical rating scale at rest and during activities, 15D score, Constant-Murley score). For categorical response variables (the proportion of patients with an acceptable symptomatic state and with adequate clinical recovery, the proportion of patients able to return to previous activities of daily living and hobbies, and patients willing to repeat the same treatment again), we used Fisher exact test because of convergence problems with logistic regression analysis. Fisher exact test was used to calculate relative risk ratios and the method of Katz et al16 was used to obtain the confidence intervals for the relative risk ratios.
The data of the declined cohort were analyzed according to the same principles as the data of the actual randomized cohort. To assess the external validity of the findings of the randomized trial, we also performed a post hoc analysis combining all DASH 2-year follow-up data (randomized trial patients and declined cohort) using mixed-model repeated-measures analysis of variance.
An independent statistician (J.R.) carried out all the analyses according to a prespecified statistical analysis plan. The threshold for statistical significance was set at P < .05 with 2-sided testing. The data were analyzed using Stata version 15.1 (StataCorp LLC).
Results
Patient Characteristics
Of 321 patients assessed for eligibility, 181 were excluded (eTable 5 in Supplement 2). Another 58 declined to be randomized. In the end, a total of 82 patients underwent randomization (Figure 1). Of these, 38 (46%) were female. The mean (SD) age was 48.9 (17.1) years. A total of 74 patients (90%) completed the 2-year follow-up; 38 were assigned to undergo surgery (initial surgery group) and 44 were assigned to functional bracing. Of the 44 patients allocated to functional bracing, 30 (68%) healed successfully (bracing group), while 14 (32%) required secondary surgery during the 2-year follow-up period (secondary surgery group). The baseline characteristics of the 3 groups are given in Table 1. Eight patients were lost to follow-up, 5 from the surgery group and 3 from the bracing group. For a summary of missing data, see eTable 6 in Supplement 2.
Figure 1. Enrollment and Randomization of Patients in the Finnish Shaft of the Humerus (FISH) Trial at 2-Year Follow-up.
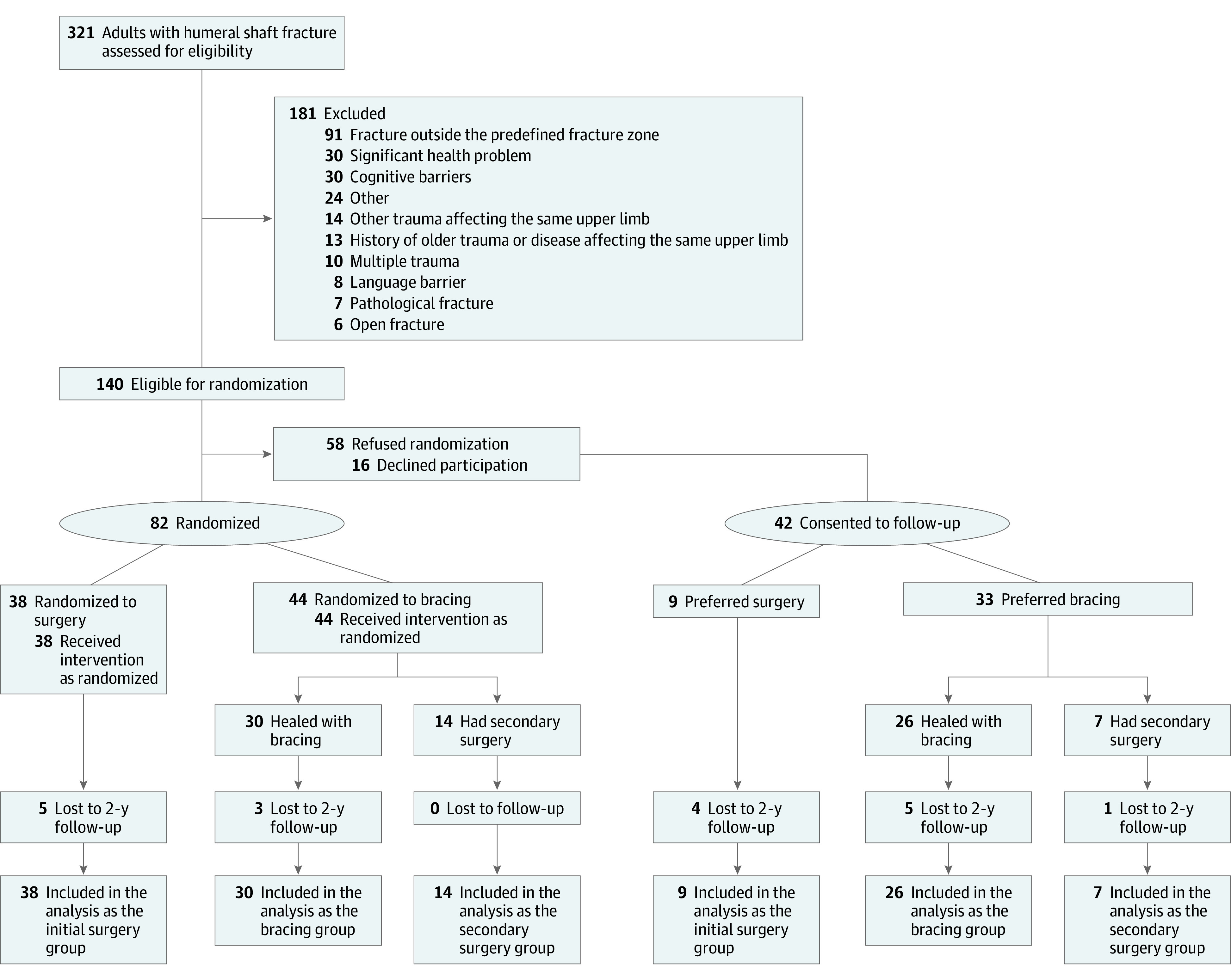
In this secondary analysis of the FISH trial, patients were divided into 3 groups: an initial surgery group (patients who were randomized to surgery), a bracing group (patients whose fracture healed with functional bracing), and a secondary surgery group (patients who were randomized to bracing but who later had surgery because of a healing problem). The aim of this secondary analysis was to compare outcomes of patients who underwent secondary surgery with outcomes of patients who healed with the initially allocated treatment method. Patients not willing to participate in randomization but who consented to follow-up were able to choose their preferred treatment. These 42 patients were included in the declined cohort and were analyzed separately according to the same principles as the randomized cohort. We also performed a post hoc analysis of Disabilities of the Arm, Shoulder and Hand scores at 2 years combining all recruited patients from the randomized cohort and declined cohort.
Primary Outcome
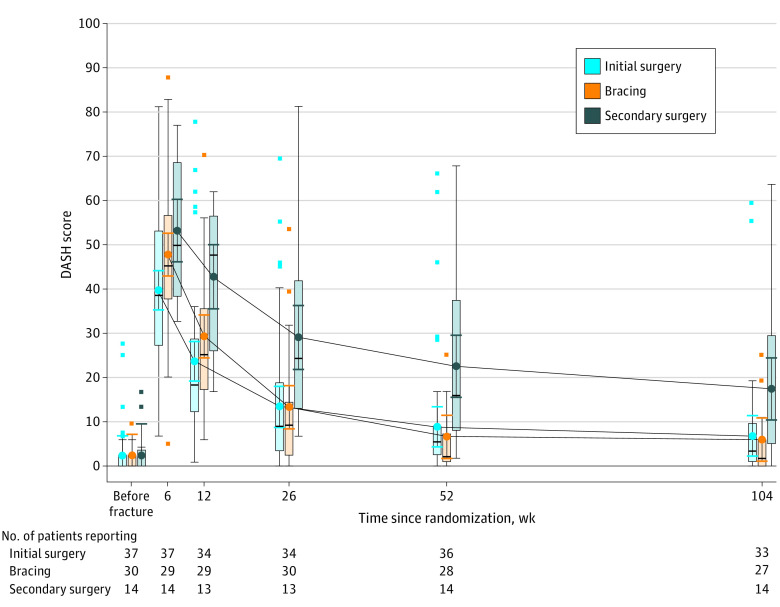
The mean DASH score was 6.8 (95% CI, 2.3 to 11.4) in the initial surgery group, 6.0 (95% CI, 1.0 to 11.0) in the bracing group, and 17.5 (95% CI, 10.5 to 24.5) in the secondary surgery group at 2 years (Figure 2; Table 2). There was a statistically significant and clinically important difference between the initial surgery group and the secondary surgery group (−10.7 points; 95% CI, −19.1 to −2.3; P = .01) and between the successful bracing group and secondary surgery group (−11.5 points; 95% CI, −20.1 to −2.9; P = .009). There was no statistically significant or clinically important difference between the initial surgery group and the bracing group (0.8 points; 95% CI, −6.0 to 7.6; P = .81).
Figure 2. Disabilities of the Arm, Shoulder and Hand (DASH) Score in Initial Surgery, Bracing, and Secondary Surgery Groups Over Time.
Error bars indicate 95% CIs of the point estimates of group means. Boxes indicate 25th and 75th percentiles of observed values; horizontal lines within boxes indicate median DASH scores; error bars indicate the highest and lowest values within 1.5 times the interquartile range; and points beyond the error bars indicate individual values outside of this range. The 14 patients in the bracing group who underwent secondary surgery during the 2-year follow-up period form the secondary surgery group. Before fracture indicates the time point of randomization after sustaining the fracture when patients were asked about their perceived preinjury DASH scores. Number of patients with available DASH scores at each time point is indicated per treatment group. One patient did not report the DASH score at baseline and we were unable to retrieve this information later (eTable 6 in Supplement 2). No imputation was performed for missing data. See eTable 7 in Supplement 2 for data. See eFigure 3 in Supplement 2 for parallel line plot.
Table 2. Primary and Secondary Outcomes at 2 Yearsa.
| Patient outcome | Mean (95% CI) | Difference between initial surgery group and secondary surgery group, mean (95% CI) | P value | Difference between bracing group and secondary surgery group, mean (95% CI) | P value | ||
|---|---|---|---|---|---|---|---|
| Randomized to surgery (initial surgery group) (n = 38) | Randomized to bracing (n = 44) | ||||||
| Bracing group (n = 30) | Secondary surgery group (n = 14) | ||||||
| Primary outcome | |||||||
| DASH scoreb | 6.8 (2.3 to 11.4) | 6.0 (1.0 to 11.0) | 17.5 (10.5 to 24.5) | −10.7 (−19.1 to −2.3) | .01 | −11.5 (−20.1 to −2.9) | .009 |
| Secondary outcome | |||||||
| Pain at restc | 0.6 (0 to 1.1) | 0.4 (0 to 1.0) | 0.7 (0 to 1.6) | −0.1 (−1.2 to 0.9) | .84 | −0.3 (−1.3 to 0.8) | .65 |
| Pain on activitiesc | 1.7 (0.9 to 2.5) | 0.5 (0 to 1.4) | 3.3 (2.1 to 4.6) | −1.7 (−3.1 to −0.2) | .03 | −2.8 (−4.3 to −1.3) | <.001 |
| Constant-Murley scored | 81.7 (76.0 to 87.5) | 85.0 (78.8 to 91.2) | 71.7 (62.9 to 80.5) | 10.0 (−0.5 to 20.5) | .06 | 13.3 (2.6 to 24.1) | .02 |
| Elbow ROM, degreese | 144 (138 to 149) | 140 (134 to 146) | 137 (129 to 146) | 7 (−4 to 17) | .20 | 3 (−8 to 13) | .59 |
| 15D scoreb | 0.90 (0.84 to 0.96) | 0.95 (0.93 to 0.97) | 0.87 (0.81 to 0.93) | 0.03 (−0.05 to 0.11) | .45 | 0.08 (0.02 to 0.14) | .008 |
| DASH work module score, mean (95% CI; No.)b | 5.3 (0 to 14.6; 21) | 0.8 (0 to 11.9; 17) | 15.3 (0 to 31.4; 8) | −10.0 (−28.6 to 8.5) | .29 | −14.5 (−34.0 to 5.1) | .15 |
| DASH sports/performing arts module score, mean (95% CI; No.)b | 4.0 (0 to 16.1; 14) | 5.8 (0 to 18.2; 15) | 40.0 (9.4 to 70.5; 4) | −36.0 (−68.8 to −3.2) | .03 | −34.2 (−67.3 to −1.1) | .04 |
| Patients with acceptable symptomatic state, % (95% CI)f | 82 (65 to 93) | 85 (66 to 96) | 43 (18 to 71) | RRR (95% CI): 1.91 (1.02 to 3.57)g | .01 | RRR (95% CI): 1.99 (1.06 to 3.71)g | .01 |
| Adequate clinical recovery, % (95% CI)h | 88 (71 to 96) | 93 (76 to 99) | 50 (23 to 77) | RRR (95% CI): 1.75 (1.02 to 3.00)g | .01 | RRR (95% CI): 1.85 (1.09 to 3.16)g | .004 |
| Satisfaction with shoulder functioni | 9.0 (8.3 to 9.8) | 9.2 (8.4 to 10) | 7.9 (6.7 to 9.0) | 1.2 (−0.1 to 2.5) | .08 | 1.4 (0 to 2.8) | .05 |
| Satisfaction with elbow functioni | 9.0 (8.3 to 9.6) | 9.4 (8.7 to 10) | 8.3 (7.2 to 9.3) | 0.7 (−0.5 to 1.9) | .23 | 1.1 (−0.1 to 2.4) | .07 |
| Satisfaction with upper extremity functioni | 8.4 (7.6 to 9.1) | 8.7 (7.8 to 9.5) | 7.3 (6.1 to 8.4) | 1.1 (−0.3 to 2.5) | .12 | 1.4 (−0.1 to 2.8) | .06 |
| Return to daily activities, % (95% CI)j | 97 (84 to 100) | 100 (87 to 100) | 93 (66 to 100) | RRR (95% CI): 1.04 (0.89 to 1.22)g | .51 | RRR (95% CI): 1.08 (0.93 to 1.25)g | .34 |
| Return to hobbies, % (95% CI)j | 94 (80 to 99) | 100 (87 to 100) | 62 (32 to 86) | RRR (95% CI): 1.53 (0.98 to 2.37)g | .01 | RRR (95% CI): 1.63 (1.06 to 2.50)g | .002 |
| Willing to repeat the same treatment, % (95% CI)k | 84 (67 to 95) | 85 (66 to 96) | 36 (13 to 65) | RRR (95% CI): 2.36 (1.15 to 4.85)g | .002 | RRR (95% CI): 2.39 (1.16 to 4.90)g | .003 |
Abbreviations: DASH, Disabilities of Arm, Shoulder and Hand; ROM, range of motion; RRR, relative risk ratio.
Complete data set of primary and secondary outcomes at different time points is given in eTable 7 in Supplement 2. The 14 patients in the bracing group who had secondary surgery during the 2-year follow-up period formed the secondary surgery group in this analysis. The point estimates are derived from the mixed-model repeated-measures analysis of variance using all available data. Trajectories of the analyses are presented in eFigure 1 in Supplement 2.
Scale definitions can be found in footnotes e, f, and g in Table 1.
Pain at rest and on activities was reported on a numerical rating scale from 0 to 10 where 0 is no pain and 10 is the worst imaginable pain.
The Constant-Murley score is a widely used instrument assessing various conditions affecting shoulder function. It has 2 subjective subscales (pain, 0 to 15 points; activities of daily living, 0 to 20 points) and 2 objective subscales (shoulder range of motion, 0 to 40 points; strength, 0 to 25 points). The range of the score is from 0 to 100 with higher scores denoting better function. Values around 85 points are considered normal in individuals aged 40 to 60 years. The measurements were performed by a physiotherapist unaware of the treatment group.
Elbow ROM was measured by the physiotherapist using goniometer and calculated using the difference in degrees between full flexion and full extension.
Acceptable symptomatic state was determined using patients’ global assessment of satisfaction regarding the injured arm and was elicited with the question, “How satisfied are you with the overall condition of your injured upper limb and its effect on your daily life?” Responses were given on a 7-point Likert scale. Very satisfied and satisfied were categorized as having an acceptable symptomatic state and somewhat satisfied, neither satisfied nor dissatisfied, somewhat dissatisfied, dissatisfied, and very dissatisfied were categorized as not having an acceptable symptomatic state.
Group comparisons with proportions of patients are given with RRR. Values greater than 1.00 indicate a better result in the initial surgery group or bracing group compared with the secondary surgery group; values less than 1.00 indicate a better result in the secondary surgery group.
Patients reporting a DASH score within a minimal clinically important difference (10 points) of their preinjury score were considered to have adequate clinical recovery.
Satisfaction with shoulder, elbow, and upper extremity function was reported on a numerical rating scale from 0 to 10 where 0 is the worst condition and 10 is the best condition.
The proportion of patients reporting they were able to return to previous hobbies and activities of daily living.
Patients were asked whether they would like to have the same treatment again if they sustained a similar injury again. Responses were given as yes or no.
Secondary Outcomes
Table 2 summarizes the outcomes at 2 years, while all follow-up time points are presented in eTable 7 and eFigure 1 in Supplement 2. At 2 years, we found statistically significant differences between the secondary surgery group and the other 2 treatment groups in most secondary outcomes in favor of the 2 latter groups. The trajectories of the outcomes based on intention-to-treat analyses and the DASH scores for as-treated analyses are given in eTable 8 and eFigure 2 in Supplement 2. When the groups were analyzed as randomized, there were no statistically significant differences in any of the outcomes at 2 years (eTable 9 in Supplement 2).
Declined Cohort
Of the 58 eligible patients declining randomization, 42 consented to be monitored (Table 1). Of these, 9 chose surgery and 33 chose functional bracing as their preferred treatment (Figure 1). At 2 years, the difference in DASH score between the initial surgery group (12.3; 95% CI, 0.3 to 24.3; n = 9) and the secondary surgery group (20.5; 95% CI, 9.4 to 31.6; n = 7) was not statistically significant (−8.2 points; 95% CI, −24.6 to 8.2). The difference between the successful bracing group (3.4; 95% CI, 0 to 9.3; n = 26) and the secondary surgery group was statistically significant (−17.2 points; 95% CI, −29.7 to −4.6). We conducted a post hoc analysis combining the randomized cohort and the declined cohort. The mean DASH score was 7.8 (95% CI, 3.5 to 12.0; n = 47) in the initial surgery cohort, 4.7 (95% CI, 1.0 to 8.5; n = 56) in the successful bracing cohort, and 18.7 (95% CI, 12.8 to 24.6; n = 21) in the secondary surgery cohort at 2 years. The difference was statistically significant between the initial surgery cohort and secondary surgery cohort (−11.0 points; 95% CI, −18.3 to −3.7), and between the successful bracing cohort and secondary surgery cohort (−14.0 points; 95% CI, −21.0 to −7.0).
Adverse Events
No additional serious adverse events occurred over the course of the 2-year follow-up compared with 1-year follow-up. There was 1 patient in the surgery group with cardiac arrhythmia warranting immediate postoperative cardioversion and 1 patient in the bracing group with pulmonary embolism 4 weeks after the fracture. There were also 7 minor adverse events in the initial surgery group, including 3 temporary iatrogenic radial nerve palsies, all of which were resolved within 12 months, and 2 superficial wound infections treated with oral antibiotics. Functional bracing led to fracture nonunions in 11 patients (25%). Of these, 9 patients underwent secondary surgery because of symptoms while 2 did not require secondary surgery and were included in the successful bracing group. Altogether, 14 of 44 patients (32%) had secondary surgery during the 2-year follow-up period. Reasons for secondary surgery are given in Table 3. Of the 14 patients who underwent secondary surgery, 13 (93%) eventually experienced fracture union. There were 4 other minor adverse events, 3 of which were related to the secondary surgical procedures. For details on adverse events, see eTable 10 in Supplement 2.
Table 3. Reasons for and Timing of Secondary Surgery Among 14 Patients in the Secondary Surgery Group.
| Reason for secondary surgery (timing) | Patients, No. |
|---|---|
| Nonunion (time range, 3-14 mo) | 9 |
| Loss of reduction (at 6 wk) | 1 |
| Refracture (at 8 mo) | 1 |
| Intolerable pain at the fracture site (at 1 wk) | 1 |
| Failure to tolerate bracing (at 1 wk and 6 wk) | 2 |
Discussion
According to this prespecified secondary analysis of the FISH trial, nonoperatively treated patients who experienced fracture healing problems that required secondary surgery had inferior outcomes at 2-year follow-up compared with patients whose fractures healed successfully, irrespective of whether the latter patients had initially been treated with surgery or with functional bracing.
We argue that this novel finding has direct ramifications for patients with a closed humeral shaft fracture contemplating the optimal treatment strategy. Rather than being informed that on average, the outcomes of surgery and functional bracing are comparable, patients should be informed that while two-thirds may heal successfully with functional bracing, one-third may experience compromised fracture healing requiring secondary surgery and leading to prolonged functional impairment. As the risk of compromised healing and secondary surgery we observed in our randomized trial (14 of 44 patients [32%]) aligns well with the corresponding rates in the existing literature,5,6,7 we feel that our rough estimates are sufficiently robust for the purpose of shared decision-making.
Limitations
This study has several limitations. First, although this was a prespecified secondary analysis, the estimates should be considered exploratory as the trial was primarily designed as an intention-to-treat analysis at 12 months. Second, our findings are only applicable to patients with closed, isolated fractures, as patients with more complex injuries or comorbidities were excluded. Third, the estimates on the incidence of adverse events are subject to considerable uncertainty because of the relatively small sample size. Fourth, the preinjury scores have an inherent risk of recall bias as they could be asked only after the fracture had occurred and, accordingly, these scores cannot be used to reflect normative scores in a population similar to our study population.
Conclusions
Future shared decision-making between clinicians and patients on the optimal initial treatment strategy for a closed humeral shaft fracture should weigh the prospect that two-thirds of patients treated with functional bracing may heal successfully against the risks of compromised fracture healing requiring secondary surgery leading to inferior functional outcomes even at 2 years after the injury. Future research on patients with humeral shaft fractures should focus on identifying optimal candidates for both nonoperative and surgical treatment.
Study protocol.
eTable 1. Inclusion and exclusion criteria used in the FISH trial
eTable 2. Rehabilitation protocol
eTable 3. Interventions
eTable 4. Schedule of enrollment, interventions and assessments
eTable 5. Reasons for exclusion in 181 patients
eTable 6. Missing data items
eTable 7. Primary and secondary outcomes at different time points
eTable 8. Sensitivity analyses: DASH score in as-treated and intention-to-treat analyses
eTable 9. Results of the intention-to-treat analyses at 2 years.
eTable 10. Adverse events and reasons for secondary surgery
eFigure 1. Trajectories of secondary outcomes—per protocol analysis with secondary surgery group
eFigure 2. Trajectories of intention to treat analysis—groups presented as randomized
eFigure 3. Parallel line plot of the initial surgery, bracing and secondary surgery groups.
Nonauthor collaborators. The FISH investigators.
Data sharing statement.
References
- 1.Matsunaga FT, Tamaoki MJS, Matsumoto MH, Netto NA, Faloppa F, Belloti JC. Minimally invasive osteosynthesis with a bridge plate versus a functional brace for humeral shaft fractures: a randomized controlled trial. J Bone Joint Surg Am. 2017;99(7):583-592. doi: 10.2106/JBJS.16.00628 [DOI] [PubMed] [Google Scholar]
- 2.Rämö L, Sumrein BO, Lepola V, et al. ; FISH Investigators . Effect of surgery vs functional bracing on functional outcome among patients with closed displaced humeral shaft fractures: the FISH randomized clinical trial. JAMA. 2020;323(18):1792-1801. doi: 10.1001/jama.2020.3182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toivanen JAK, Nieminen J, Laine HJ, Honkonen SE, Järvinen MJ. Functional treatment of closed humeral shaft fractures. Int Orthop. 2005;29(1):10-13. doi: 10.1007/s00264-004-0612-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denard A Jr, Richards JE, Obremskey WT, Tucker MC, Floyd M, Herzog GA. Outcome of nonoperative vs operative treatment of humeral shaft fractures: a retrospective study of 213 patients. Orthopedics. 2010;33(8). doi: 10.3928/01477447-20100625-16 [DOI] [PubMed] [Google Scholar]
- 5.Westrick E, Hamilton B, Toogood P, Henley B, Firoozabadi R. Humeral shaft fractures: results of operative and non-operative treatment. Int Orthop. 2017;41(2):385-395. doi: 10.1007/s00264-016-3210-7 [DOI] [PubMed] [Google Scholar]
- 6.Harkin FE, Large RJ. Humeral shaft fractures: union outcomes in a large cohort. J Shoulder Elbow Surg. 2017;26(11):1881-1888. doi: 10.1016/j.jse.2017.07.001 [DOI] [PubMed] [Google Scholar]
- 7.Serrano R, Mir HR, Sagi HC, et al. Modern results of functional bracing of humeral shaft fractures: a multicenter retrospective analysis. J Orthop Trauma. 2020;34(4):206-209. doi: 10.1097/BOT.0000000000001666 [DOI] [PubMed] [Google Scholar]
- 8.Rämö L, Taimela S, Lepola V, Malmivaara A, Lähdeoja T, Paavola M. Open reduction and internal fixation of humeral shaft fractures versus conservative treatment with a functional brace: a study protocol of a randomised controlled trial embedded in a cohort. BMJ Open. 2017;7(7):e014076. doi: 10.1136/bmjopen-2016-014076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium—2018. J Orthop Trauma. 2018;32(1):S1-S170. doi: 10.1097/BOT.0000000000001063 [DOI] [PubMed] [Google Scholar]
- 10.Gummesson C, Atroshi I, Ekdahl C. The Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. doi: 10.1186/1471-2474-4-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128-146. doi: 10.1016/S0894-1130(01)80043-0 [DOI] [PubMed] [Google Scholar]
- 12.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160-164. doi: 10.1097/00003086-198701000-00023 [DOI] [PubMed] [Google Scholar]
- 13.Hao Q, Devji T, Zeraatkar D, et al. Minimal important differences for improvement in shoulder condition patient-reported outcomes: a systematic review to inform a BMJ Rapid Recommendation. BMJ Open. 2019;9(2):e028777. doi: 10.1136/bmjopen-2018-028777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33(5):328-336. doi: 10.3109/07853890109002086 [DOI] [PubMed] [Google Scholar]
- 15.Alanne S, Roine RP, Räsänen P, Vainiola T, Sintonen H. Estimating the minimum important change in the 15D scores. Qual Life Res. 2015;24(3):599-606. doi: 10.1007/s11136-014-0787-4 [DOI] [PubMed] [Google Scholar]
- 16.Katz D, Baptista J, Azen SP, Pike MC. Obtaining confidence intervals for the risk ratio in cohort studies. Biometrics. 1978;34(3):469-474. doi: 10.2307/2530610 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Study protocol.
eTable 1. Inclusion and exclusion criteria used in the FISH trial
eTable 2. Rehabilitation protocol
eTable 3. Interventions
eTable 4. Schedule of enrollment, interventions and assessments
eTable 5. Reasons for exclusion in 181 patients
eTable 6. Missing data items
eTable 7. Primary and secondary outcomes at different time points
eTable 8. Sensitivity analyses: DASH score in as-treated and intention-to-treat analyses
eTable 9. Results of the intention-to-treat analyses at 2 years.
eTable 10. Adverse events and reasons for secondary surgery
eFigure 1. Trajectories of secondary outcomes—per protocol analysis with secondary surgery group
eFigure 2. Trajectories of intention to treat analysis—groups presented as randomized
eFigure 3. Parallel line plot of the initial surgery, bracing and secondary surgery groups.
Nonauthor collaborators. The FISH investigators.
Data sharing statement.