Abstract
Since the emergence of SARS-CoV-2, clinicians have been challenged with a wide spectrum of disease severity. One of the serious complications associated with the virus is multisystem inflammatory syndrome in children (MIS-C). It is characterised by inflammation leading to organ damage, in the setting of positive SARS-CoV-2 infection. MIS-C is thought to be a postviral reaction where most children are negative on PCR testing but are positive for SARS-CoV-2 antibodies. The Centers for Disease Control and Prevention recently defined the same phenomenon occurring in adults as multisystem inflammatory syndrome in adults (MIS-A) and emphasised on the use of antibody testing in this population. Here we describe an adult woman with an exposure to SARS-CoV-2 who presented with unexplained organ failure and shock. Positive antibody testing was the only clue to the diagnosis of MIS-A. We stress the importance of SARS-CoV-2 antibody detection in order to identify these cases.
Keywords: COVID-19, medical management
Background
The COVID-19 pandemic caused by the SARS-CoV-2 virus has affected tens of millions of people around the globe. Novel and complex presentations of the disease are being recognised after almost a year into the pandemic. Multisystem inflammatory syndrome in children (MIS-C) is a rare but severe post-COVID-19 illness that has been recognised by the WHO and the Centers for Disease Control and Prevention (CDC).1 2 It encompasses a variety of symptoms including fever, rash, abdominal pain, diarrhea and a Kawasaki-like syndrome, in conjunction with elevated inflammatory markers. Kawasaki-like syndrome is an acute, systemic vasculitis of medium-sized vessels of unclear aetiology. It has been hypothetically identified as a postinfectious disease process linked to multiple viral and bacterial organisms such as Streptococcus or Epstein-Barr virus,3 where high levels of circulating proinflammatory cytokines might contribute to the distributive component of shock.4 During the recent pandemic, Kawasaki-like disease associated with COVID-19 has been increasingly reported all over the world.4 5 MIS-C can lead to shock and cardiogenic collapse in individuals less than 21 years old.1 2
In October 2020, the CDC introduced a similar illness in adults based on multiple case series, which has been identified as multisystem inflammatory syndrome in adults (MIS-A). Diagnosis of MIS-A is similar to MIS-C, but affects a different age group.6 The CDC concluded that all ages can suffer from the ramifications of an inflammatory cytokine storm following a SARS-CoV-2 infection. MIS-C and MIS-A are distinguished from a severe form of COVID-19 when there is an absence of respiratory symptoms, hypoxemia and radiographic lung injury.6 The pathophysiology of both MIS-C and MIS-A is unknown, but the suggested aetiology is a hyperinflammatory immune response similar to Kawasaki syndrome.4
Because many cases of MIS-C have a negative COVID-19 on PCR testing but elevated titres of COVID-19 antibodies, this finding necessitates antibody testing to identify cases in adults as well.6 In addition, high clinical suspicion is required to detect COVID-19-related complications, as many patients may have had a silent or mild acute phase of infection and therefore not report any previous symptoms suggestive of an acute viral infection.7 Here we present a case of a patient with MIS-A where COVID-19 antibody testing guided diagnosis and successful treatment. Following the recent surge in COVID-19 cases, clinical suspicion for MIS-A should be considered in all sick patients with unexplained organ failure.
Case presentation
Our patient is a 43-year-old woman with no pertinent medical history who presented with gradual onset of the following symptoms: high-grade fever, rash, cramping generalized abdominal pain and diarrhea for 10 days.
On presentation, the patient had a fever of 39.4°C (103°F), heart rate of 128, blood pressure of 114/51 and oxygen saturation of 98%. She was noted to have an erythematous, blanching, non-tender annular macular rash on the upper arms chest, abdomen and back. Lungs were clear to auscultation bilaterally. Examination was otherwise unremarkable.
Investigations
Laboratory tests were significant for leucocytosis with bandemia, mild transaminitis and elevated inflammatory markers (table 1). She had a negative COVID-19 PCR on admission, and chest X-ray did not show any signs of an infiltrate (figure 1). The patient was started on broad-spectrum antibiotics with a preliminary diagnosis of sepsis with unknown source. She was initially started on ceftriaxone and doxycycline. Although she did not show any improvements with this broad coverage, the antibiotic regimen was not changed as we could not isolate any bacteria or find a focus of infection. Drug rash with eosinophilia and systemic symptom was temporarily in the differential diagnosis due to transient eosinophilia and rash, but eosinophilia self-resolved after a day and there was no facial edema or lymphadenopathy. Therefore the same antibiotic treatment was continued.
Table 1.
The patient’s laboratory findings
| Laboratory | On admission | Peak value | 48 hours post-treatment | Normal range |
| White cell count (×109/L.) | 13.9 | 25.2 | 14.2 | 4.8–1.8 |
| Neutrophil count (K/μL) | 12.7 | 21 | 10.2 | 1.8–7.7 |
| Lymphocyte count (nL) | 0.5 | 4.3 | 3.3 | 1.2–3.5 |
| PPlatelete (×109/L.) | 180 | 687 | 619 | 150–400 |
| Prothrobmin Time (PT) (s) | 16.8 | 16.8 | 13 | 11.8–14.8 |
| Partial thromboplastin time (PTT) (s) | 53 | 54 | 33 | 25.1–38.9 |
| International normalized ratio(INR) | 1.3 | 1.3 | 1 | 0.9–1.2 |
| C reactive protein (mg/dL) | 28.3 | 28 | 8.2 | <0.8 |
| Ferritin (ng/mL) | 985 | 1366 | 455 | 10–150 |
| Lactate dehydrogenase (U/L) | 297 | 389 | 241 | <240 |
| D-dimer (μg/mL Fibrinogen Equivalent Units) | 3.23 | 3.44 | 1.3 | 0.27–0.50 |
| Fibrinogen (mg/dL) | 692 | 692 | 340 | 187–502 |
| Aspartate transferase(U/L) | 94 | 94 | 26 | <40 |
| Alanine transaminase(U/L) | 185 | 185 | 45 | <30 |
| Troponin (ng/mL) | 0.05 | 0.16 | <0.01 | <0.03 |
| Creatinine (mg/dL) | 0.5 | 2.14 | 1.09 | <1.2 |
Figure 1.
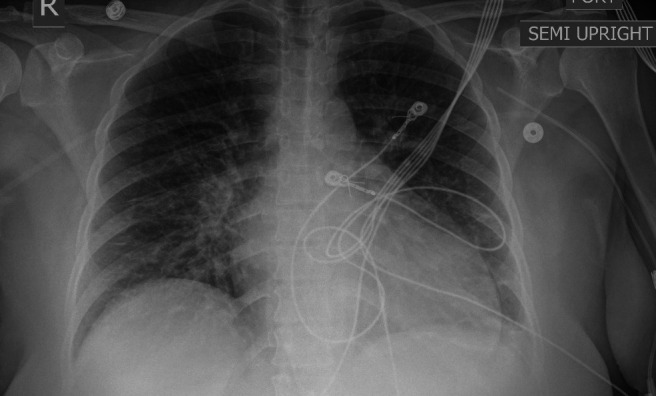
Chest X-ray without any obvious infiltrate.
The patient was persistently hypotensive and febrile despite aggressive hydration and use of broad-spectrum antibiotics. She ultimately required vasopressor support and was transferred to the intensive care unit (ICU) within 24 hours into hospitalisation. In the ICU, she developed acute kidney injury with a rise in creatinine, elevated troponins without ischaemic change on ECG (figure 2), and decreased ejection fraction on echocardiogram suggestive of toxic cardiomyopathy (videos 1 and 2).
Figure 2.

ECG consistent with sinus tachycardia without any evidence of ST-T changes.
Video 1.
Video 2.
Differential diagnosis
Full infectious work-up, including viral/bacterial/fungal/parasitic work-up, was negative for any specific pathology. Stool culture was negative and gastrointestinal-related pathology was not considered given abdominal pain and diarrhea resolved shortly after admission. The patient was also noted to have temporary rise in eosinophil count of unclear aetiology. While there was a slight suspicion for DRESS, the diagnosis remained low on the differential given the Aspartate transaminase (AST) and Alanine transaminase(ALT)were trending down at that time and there was no facial or mucosal involvement o(f the rash. Antinuclear antibody (ANA) was positive (1:80), with a negative subsequent extranuclear antigen panel. Given her elevated serum ferritin levels (table 1) and positive ANA, rheumatology was consulted on day 3 of admission to evaluate the patient for possible autoimmune etiology, such as adult-onset Still’s disease (AOSD) or systemic lupus erythematosus. The diagnosis of AOSD requires the presence of 5 features, with at least 2 being major diagnostic criteria, in the absence of any other possible diagnosis. The major criteria include fever of at least 39°C (102.2°F) lasting at least 1 week, arthralgias or arthritis lasting 2 weeks or longer, a non-pruritic macular or maculopapular skin rash that is salmon-coloured in appearance and usually found on the trunk or extremities during febrile episodes, and leukocytosis (×109/L or greater), with at least 80% granulocytes.
The minor criteria include sore throat, lymphadenopathy, hepatomegaly or splenomegaly, abnormal liver function studies, particularly elevations in aspartate and alanine aminotransferase and lactate dehydrogenase concentrations, and negative tests for ANA and rheumatoid factor.8 Our patient did not meet the diagnostic criteria of AOSD, as she only had fever from the major criteria and elevated liver enzymes as the minor criteria. Also, we would usually expect higher levels of ferritin and liver enzymes in AOSD.
Antineutrophil cytoplasmic antibodies (ANCA) vasculitis was low on the differential because there were no signs of ANCA vasculitis, such as petichae/purpura, mononeuritis, pulmonary infiltrate or sinus involvement.
The patient denied any symptoms suggestive of connective tissue disorder on her review of systems and had no clear signs of one on physical examination, and as such it was felt that this was not likely to be a connective tissue disease.
On further questioning, the patient reported to have attended a crowded family party about 3 weeks prior to her presentation. Her husband developed a mild fever with malaise a few days following the party and he improved with ibuprofen. The prevalence of COVID-19 in New York was increasing exponentially during the fall of 2020 when we saw this patient. Having any febrile illness was highly suspicious of COVID-19 infection in our community. Unfortunately, the husband did not agree to COVID-19 testing, and they did not know if anyone else at the party got sick or tested. Regardless, positive COVID-19 antibody in our patient confirmed recent exposure and infection. Our patient did not work outside of the home and had not been interacting with anyone other than her husband except for the party. We were confident that they were both exposed to COVID-19 at that event. After developing similar symptoms, the patient took ibuprofen, but stopped due to development of rash. The patient and her husband were not tested for COVID-19 at that time and denied any cough or respiratory symptoms. Her symptoms progressively worsened over the next few days, which prompted her to come to the hospital. This part of the history established the possibility of current clinical picture to be related to COVID-19-associated complication. COVID-19 antibody was positive, which suggested previous infection and coincided with given history.
Due to evidence of multiple organ failure and increased inflammatory markers in the setting of recent COVID-19 infection, as evidenced by elevated COVID-19 antibody titres and lack of alternative diagnosis, she was diagnosed with MIS-A.
Treatment
The patient was started on intravenous Solumedrol 1 mg/kg. She had significant clinical improvement within a day post steroid treatment (table 1).
Outcome and follow-up
Over the next 48 hours, the patient’s rash resolved. There was an initial plan for skin biopsy; however, the plan was deferred due to the patient’s clinical improvement and resolution of rash after the steroids. Kidney and liver function improved and she was weaned off of vasopressors. Repeat transthoracic echocardiography showed improved ejection fraction (video 2). Antibiotics were stopped 24 hours after starting the steroids given the patient’s dramatic clinical improvement. C reactive protein (CRP) was trended as it is more closely associated with COVID-19 infection. It gradually normalised within 1 week of steroid treatment.
She was continued on intravenous steroid for 3 days’ duration and transitioned to oral prednisone with a plan to taper off over 1 month. On discharge, her creatinine improved to her baseline (0.6 g/dL), troponin was negative and AST/ALT were within normal limits. The patient was stable enough to be discharged home within 1 week of initiating steroid therapy. During follow-up 3 weeks post discharge, the patient remained symptom-free and continued with the plan to finish a month of steroid taper.
Discussion
New manifestations of COVID-19 continue to emerge as we learn more about the current pandemic. COVID-19 presentation ranges from asymptomatic carriers to acute respiratory distress syndrome that can affect all ages. MIS-C was introduced by the CDC as a unique complication of COVID-19 in June 2020. It is defined as an individual aged <21 years presenting with fever, laboratory evidence of inflammation and evidence of clinically severe illness requiring hospitalisation, with multisystem (>2) organ involvement (cardiac, renal, respiratory, haematological, gastrointestinal, dermatological or neurological), in addition to no alternative diagnoses, and positive for current or recent SARS-CoV-2 infection by RT-PCR, serology or antigen test.1 The difference between severe COVID-19 cases and MIS-C is the lack of respiratory failure and hypoxaemia.6 The CDC expanded their recognition of MIS phenomenon to adults in October 2020 after reports of similar complications in older age groups.6 Our case fits the criteria for MIS-A while presented with multiple organ failure and a lack of respiratory involvement in the setting of positive COVID-19 serum antibody.
The most common symptoms of MIS-A reported by the CDC include heart-related symptoms such as arrhythmias, elevated troponin concentrations and left or right ventricular dysfunction. Other common presentations of the syndrome are gastrointestinal symptoms, dermatological abnormalities and a Kawasaki-like reaction. Most patients have elevated concentrations of CRP, ferritin and D-dimer.6 Our patient had a similar symptomatic profile in conjunction with increased inflammatory markers.
The exact pathophysiology of MIS-A is unclear. It has been suggested that the syndrome results from an abnormal immune response to the virus, with some clinical similarities to Kawasaki disease, toxic shock syndrome and cytokine release syndrome. Given the high proportion of cases with positive antibodies, there is a possibility that antibodies can play a role in the pathophysiology of MIS-A. Antibodies can augment the inflammatory response by triggering the host immune response with antibody-dependent enhancement of viral entry and amplification of viral replication as is similarly seen in dengue.9 10 Thirty per cent of adults in a CDC report had negative PCR while testing positive for the SARS-CoV-2 antibody, suggesting MIS-A might represent a postinfectious process within 2–4 weeks of exposure.6 These cases may represent a new phenomenon in adults equivalent to what was recently described in the paediatric population.
Studies estimate the lack of symptoms in one-fifth of infected individuals with SARS-CoV-2.7 Absence of recent upper respiratory symptoms makes the diagnosis of MIS-A more challenging. Linking patients with unexplained multiple organ failure to COVID-19-related complication requires accurate history taking and a high clinical suspicion. The patient in this case did not report recent upper respiratory infection, but her attendance in a crowded party and the upper airway illness (URI) symptoms of her husband 2 weeks prior to her presentation provided a clue towards conducting COVID-19 antibody testing and ultimate diagnosis of MIS-A.
Current available treatment for MIS-A is based on case series and clinical reports. The principles of treatment include supportive measures and anti-inflammatory therapies with frequent use of intravenous immunoglobulin (IVIG) and steroids.6 Based on the CDC report, 7 patients were treated with IVIG, 10 with corticosteroids and 2 with the interleukin 6 (IL-6) inhibitor tocilizumab.6 Given the fact that our patient improved so dramatically with steroids, she was not given further therapies. As was the case with our patient, use of moderate-dose steroids showed dramatic improvement in shock and end-organ dysfunction in a case series of sevenyoung adult men with cardiogenic shock and evidence of MIS-A.11 A larger case series of 11 adults with suspected myocarditis related to multisystem inflammatory syndrome demonstrated drastic improvement of ejection fraction when treated with steroids and IVIG.12 Further research is needed to understand the pathogenesis and long-term effects of this condition. COVID-19 antibody might have a role in the pathogenesis of this syndrome.
Conclusion
Given the abrupt increase in COVID-19 cases, clinicians should retain an elevated clinical suspicion for MIS-A. Routine SARS-CoV-2 antibody testing may be helpful in effectively diagnosing and treating patients with MIS-A. Expeditious diagnosis may be greatly beneficial to patients as anti-inflammatory treatment such as steroids and potentially IVIG or anti-IL-6 antibodies has shown to improve outcomes.
Learning points.
Novel and complex presentations of COVID-19 pandemic are emerging as we learn more about this illness.
Given the high proportion of patients with asymptomatic infection or mild upper airway illness symptoms, diagnosis of multisystem inflammatory syndrome in adults (MIS-A) remains challenging.
Linking patients with unexplained multiple organ failure to COVID-19-related complication requires accurate history taking and a high clinical suspicion.
Following the recent surge in SARS-CoV-2 cases, clinical suspicion for MIS-A should be considered in all sick patients with unexplained organ failure.
COVID-19 antibody should be checked in all cases with suspected MIS-A to establish the diagnosis.
Footnotes
Contributors: The report was supervised and reviewed by IB. The patient was under the care of MV and PW. The report was written by MV and PW.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Godfred-Cato S, Bryant B, Leung J, et al. COVID-19-Associated Multisystem Inflammatory Syndrome in Children - United States, March-July 2020. MMWR Morb Mortal Wkly Rep 2020;69:1074–80. 10.15585/mmwr.mm6932e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . Multisystem inflammatory syndrome in children and adolescents temporally related to COVID‐19, 2020. [Google Scholar]
- 3.Akca UK, Kesici S, Ozsurekci Y, et al. Kawasaki-like disease in children with COVID-19. Rheumatol Int 2020;40:2105–15. 10.1007/s00296-020-04701-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toubiana J, Poirault C, Corsia A, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ 2020;369:m2094. 10.1136/bmj.m2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet 2020;395:1771–8. 10.1016/S0140-6736(20)31103-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris SB, Schwartz NG, Patel P, et al. Case Series of Multisystem Inflammatory Syndrome in Adults Associated with SARS-CoV-2 Infection - United Kingdom and United States, March-August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1450–6. 10.15585/mmwr.mm6940e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim G-u, Kim M-J, Ra SH. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID-19. Clinical Microbiology and Infection 2020;26:948.e1–948.e3. 10.1016/j.cmi.2020.04.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamaguchi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult still's disease. J Rheumatol 1992;19:424–30. [PubMed] [Google Scholar]
- 9.Jiang L, Tang K, Levin M, et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis 2020;20:e276–88. 10.1016/S1473-3099(20)30651-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang S-F, Tseng S-P, Yen C-H, et al. Antibody-Dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem Biophys Res Commun 2014;451:208–14. 10.1016/j.bbrc.2014.07.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chau VQ, Giustino G, Mahmood K, et al. Cardiogenic shock and hyperinflammatory syndrome in young males with COVID-19. Circulation 2020;13:e007485. 10.1161/CIRCHEARTFAILURE.120.007485 [DOI] [PubMed] [Google Scholar]
- 12.Hékimian G, Kerneis M, Zeitouni M, et al. Coronavirus disease 2019 acute myocarditis and multisystem inflammatory syndrome in adult intensive and cardiac care units. Chest 2021;159:657–62. 10.1016/j.chest.2020.08.2099 [DOI] [PMC free article] [PubMed] [Google Scholar]


