Abstract
Extradigital glomus tumour is uncommon, little-known outside of its subungual location, and may present without its classic triad of tenderness, cold sensitivity and paroxysmal pain. Imaging is non-specific and diagnosis is often delayed, sometimes for years, leading to unnecessary morbidity. Surgical excision is the treatment of choice, although technique depends on case specifics. Histological subtypes depend on the relative prominence of glomus cells, vascular structures and smooth muscle. The vast majority of glomus tumours are benign. We highlight the importance of considering extradigital glomus tumours when generating differential diagnoses of an atypical painful lesion in a variety of clinical specialties.
Keywords: musculoskeletal and joint disorders, orthopaedic and trauma surgery, plastic and reconstructive surgery
Background
Glomus tumours are rare tumours of the glomus body, accounting for less than 2% of all soft tissue tumours. The glomus body is a thermoregulatory unit found in high density in the digits.1 Glomus tumours are most commonly found subungually in the fingers, causing the classic triad of exquisite tenderness, cold sensitivity and excruciating paroxysmal pain. The unusual occurrence of glomus tumours in extradigital locations may lead to difficulties in diagnosis, especially as physical examination can be unremarkable in 50% of lesions,2 and worryingly more likely if the tumour is malignant.3 Furthermore, although subungual glomus tumour is well-described, major textbooks of hand surgery fail to mention its extradigital manifestations or the other subtypes such as glomangiomyoma.1 A lack of specific imaging also hinders diagnosis, which can easily be delayed for a long time (7–10 years for extradigital forms).4 5 Misdiagnoses include osteoarthritis, neuropathy or even psychiatric illness.4 6 Patients may therefore undergo unsuitable treatment including sympathetic ganglionectomy, radicotomy or amputation5 6
We present a case of extradigital glomangiomyoma, the least common subtype of glomus tumour, in the forearm of an elderly man. Peripheral nerve sheath tumour and thrombosed varicose vein were the working (mis)diagnoses until postoperative histological examination revealed glomangiomyoma. Although rare, extradigital glomus tumours can present to a wide variety of clinicians; they should be kept in mind when generating differential diagnoses.
Case presentation
We present an elderly man who attended the orthopaedic hand clinic with an isolated, subcutaneous, subcentimetre, bluish lump on the dorsum of his left distal forearm which had been present for 1 year without history of trauma. The patient was extremely protective of the lump and flinched from clinician examination. The lump was tender on palpation but painless on movement. He was fit and well apart from hypertension and hypercholesterolaemia.
Investigations
A community-ultrasound scan suggested benign nerve sheath tumour or superficial thrombophlebitis. Subsequent MRI demonstrated a lesion within the subcutaneous fat in close proximity to the basilic vein and dorsal branch of ulnar nerve which was likely to be a thrombosed venous varix, although peripheral nerve sheath tumour could not be excluded (figures 1 and 2). A repeat ultrasound performed by a musculoskeletal radiologist confirmed probable peripheral nerve sheath tumour lying directly adjacent to the basilic vein and overlying the left distal ulna (figure 3).
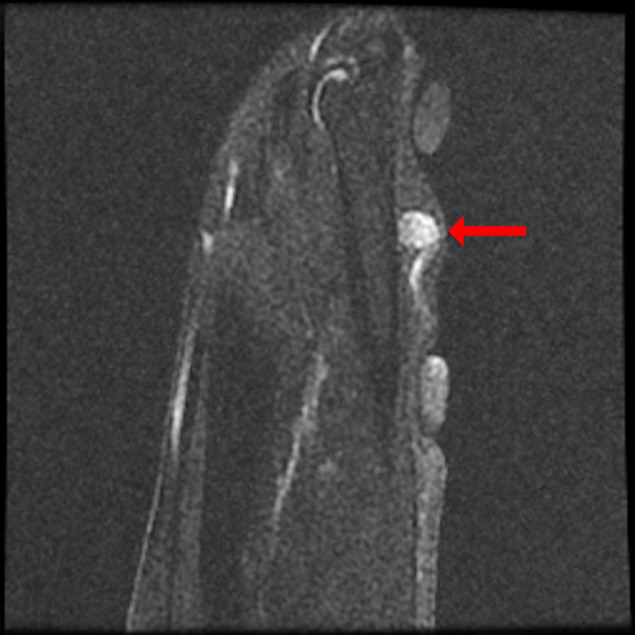
Figure 1.
Coronal T2 fat saturated MRI image of the lesion showing high signal intensity.
Figure 2.
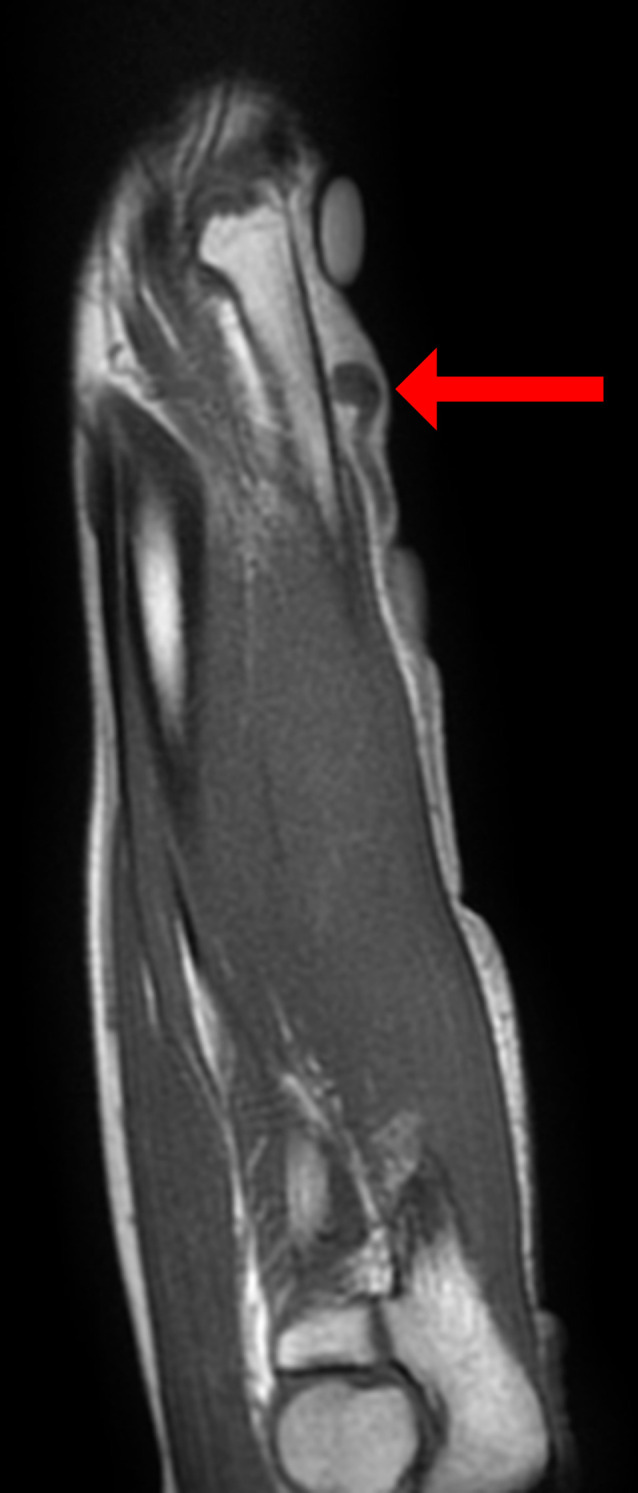
Coronal T1 MRI image of the lesion showing isosignal intensity.
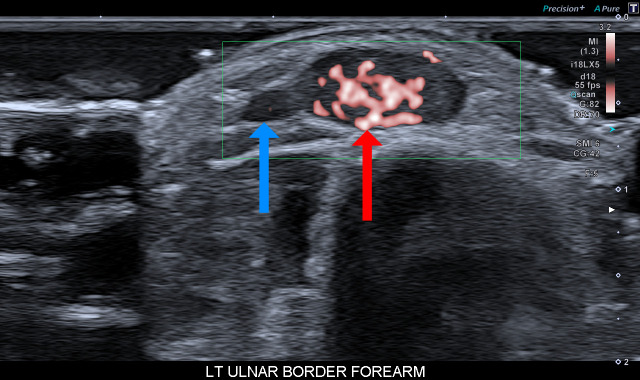
Figure 3.
Ultrasound image of the lesion (red arrow) demonstrating brisk Doppler signal and its location adjacent to the basilic vein (blue arrow).
Treatment
To resolve the exquisite tenderness, the patient underwent surgical excision of the lump under local anaesthesia. Intraoperative macroscopic appearances suggested venous malformation at the confluence of branches of the basilic vein, directly overlying but not incorporating the dorsal branch of the ulnar nerve (figures 4 and 5). The lump was excised in its entirety and sent for histological examination preserved in formalin. Postoperative recovery was unremarkable.
Figure 4.
Intraoperative photograph showing the lesion adherent to the basilic vein.
Figure 5.
Intraoperative photograph showing the unaffected dorsal ulnar nerve on deeper dissection after lesion removal.
Outcome and follow-up
Histological examination of the excised lesion diagnosed glomangiomyoma with no evidence of malignancy (figures 6–8). The patient reported full resolution of preoperative symptoms immediately after surgery. There were no wound healing problems. As there were no features of malignancy and resolution of symptoms, the patient was deemed suitable for discharge after the 2-week postoperative review. Telephone review after 2 months confirmed ongoing resolution of symptoms and no recurrence so far.
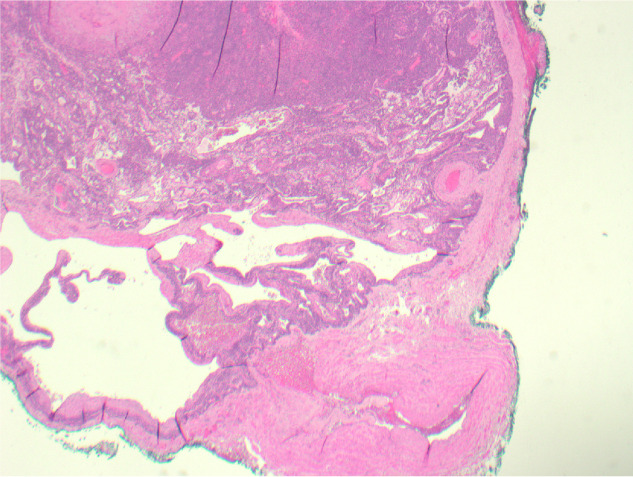
Figure 6.
Histological examination at ×2 objective (H&E stain) showing a vein (bottom right) to which the glomangiomyoma is attached. The tumour contains an organoid mixture of thick-walled, muscular blood vessels, solid sheets of small, uniform glomus cells and irregular, thin-walled vascular channels. There are interspersed areas of smooth muscle which merge focally with the glomus cells.
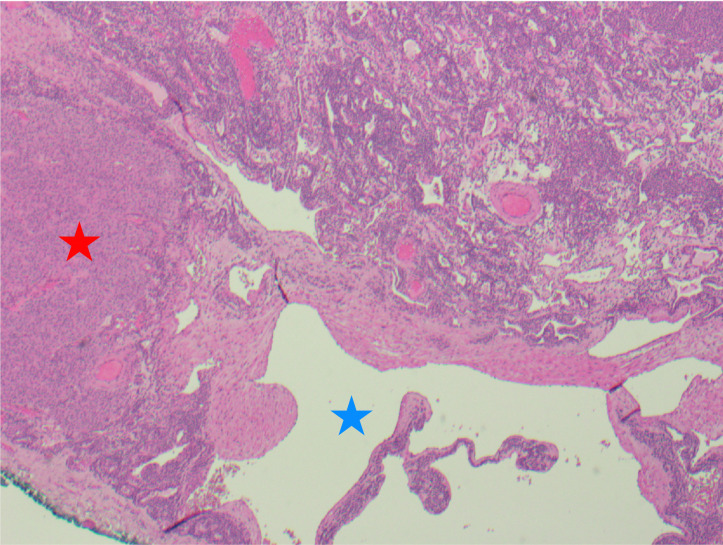
Figure 7.
Histological examination at ×4 objective (H&E stain) showing glomus cells (dark nuclei), including a sheet of epithelioid glomus cells with more abundant, paler cytoplasm (red star), with dilated vascular channels lined by smooth muscle cells (blue star).
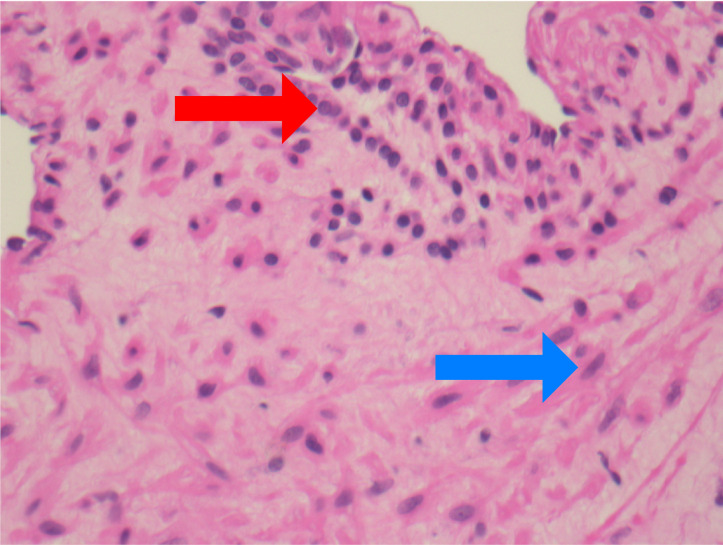
Figure 8.
Histological examination at ×40 objective (H&E stain) showing glomus cells (red arrow) merging with smooth muscle cells (blue arrow).
Discussion
Glomus tumours are mesenchymal hamartomas composed of cells that closely resemble the modified smooth muscle cells of the normal glomus body.3 A glomus body is a neuromyoarterial body found within the reticular dermis that functions as a specialised form of arteriovenous anastomosis and is responsible for thermoregulation.7
Glomus tumours are uncommon, accounting for less than 2% of all soft tissue tumours.3 They can occur in any age, although typically occur in young adulthood.3 By far the most common site of occurrence is in the hand (75%),2 particularly subungually (65%),2 although individual case reports of extradigital glomus tumours have been published (e.g. in the lung, stomach, penis, mediastinum).3 They are almost always cutaneous or within the superficial soft tissues; there is a greater chance of malignancy (up to 33%) with deeper lesions.8 They are small, blue–red nodules associated with the established symptom triad of exquisite tenderness, cold sensitivity and excruciating paroxysmal pain out of proportion to tumour size.8 In extradigital tumours, pain and point tenderness are the most specific symptoms.9
Glomus tumours are subcategorised as solid glomus tumour, glomangioma or glomangiomyoma depending on the relative prominence of glomus cells, vascular structures and smooth muscle.3 Solid glomus tumours are the most common variant, accounting for 75%; glomangiomas show a more vascularised growth pattern and account for 20%,7 although this is the most common subgroup in multiple or familial cases8; glomangiomyomas are the rarest subtype, with a transition of cell type from glomus cells to cells resembling smooth muscle.3 Malignant glomus tumours are vanishingly rare, accounting for less than 1%.3 Criteria for malignancy include any of the following: size greater than 2 cm, deep location (subfascial or visceral), presence of atypical mitotic figures or marked nuclear atypia.3 Glomus cells are immunohistochemically relatively non-specific, but show positivity for smooth muscle actin, vimentin and neuron specific enolase.6 They are usually negative for other markers of soft tissue tumours such as desmin, CD34, cytokeratin or S100 protein.3 Differential diagnoses include intradermal naevus, haemangioma and other vascular lesions, other soft tissue lesions such as leiomyoma, leiomyosarcoma with epithelioid differentiation and rhabdomyosarcoma.6 Histological evaluation is usually the only reliable method to confirm final diagnosis.
Thermography and scintigraphy are not helpful in the diagnosis of glomus tumours. Plain radiographs are minimally useful in the digit as phalangeal cortical erosions are visible in only 25% of cases, and even less in extradigital tumours.1 Marked vascularity on Doppler ultrasound has been described,8 as seen in our case. Angiography is not routinely required, although it can help in excluding vascular malformations.1 MRI is thought to be the most sensitive modality;8 glomus tumours are described as slightly hypointense to slightly hyperintense on a T1-weighted image, and hyperintense on a T2-weighted image. Contrast-enhanced T1-weighted images of the lesion demonstrate stronger enhancement.4 However, these features are not specific to glomus tumours,1 with a specificity of 50%.9
Surgical excision is uniformly agreed as the treatment of choice for glomangiomyoma.4 5 10 11 This ensures immediate resolution of pain without recurrence in 90% of cases.4 Margins of tissue clearance are not universally agreed: Lee et al5 report that unless there are malignant features, en bloc resection is not necessary; however, other authors recommend wide local excision to prevent risk of recurrence.6 12 Sclerosants such as sodium tetradecyl sulphate, polidocanol and hypertonic saline have been reported to be effective. Ablative therapy with argon and carbon dioxide laser may be of potential benefit for small, superficial lesions.1 10
Patient’s perspective.
Over a period of about 12 months the lump became very tender to the touch. After a few months, things changed for no apparent reason; all of a sudden I would get a massive surge of pain in the lump. But only for about ten seconds. As time went by, this happened more frequently (3–4 times a day). After two visits to the doctors, [there was] still no explanation as to what it was. On the third visit [my doctor] arranged for a scan at the hospital. I would like to thank [the authors] for the fantastic care and treatment they showed towards me. Thanks again.
Learning points.
Glomus tumour in the finger is well-known to hand surgeons but its extradigital existence is not.
Physical examination can be unremarkable in up to half of cases, and more likely if the tumour is malignant. Imaging is non-specific.
A high level of suspicion is required to diagnose extradigital glomus tumour.
Although rare, extradigital glomus tumour can present to a wide variety of clinicians; it should be kept in mind when generating differential diagnoses.
Footnotes
Contributors: LL wrote the paper; VB provided the histological input and reviewed the final draft; AG provided the radiological input and reviewed the final draft; PJ planned the paper and reviewed the final draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Myers RS, Lo AKM, Pawel BR. The glomangioma in the differential diagnosis of vascular malformations. Ann Plast Surg 2006;57:443–6. 10.1097/01.sap.0000222729.59856.e1 [DOI] [PubMed] [Google Scholar]
- 2.Akman YE, Yalcinkaya M, Arikan Y, et al. Atypically localized glomus tumor causing anterior interosseous nerve syndrome: a case report. Acta Orthop Traumatol Turc 2017;51:492–4. 10.1016/j.aott.2017.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fletcher CDM, Krishnan Unni K, Mertens F. WHO classification of tumors of soft tissue and bone. ARC Press Lyon, 2002. [Google Scholar]
- 4.Lancien U, Duteille F, Perrot P. Extradigital glomic tumor of the forearm. about a case and review of literature. Ann Chir Plast Esthet 2018;63:187–9. 10.1016/j.anplas.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 5.Lee W, Kwon SB, Cho SH, et al. Glomus tumor of the hand. Arch Plast Surg 2015;42:295–301. 10.5999/aps.2015.42.3.295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deger AN, Deger H, Tayfur M, et al. Acquired solitary Glomangiomyoma on the forearm: a rare case report. J Clin Diagn Res 2016;10:ED10–11. 10.7860/JCDR/2016/19062.8195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCullough M, Balzer B, Kushner SH. Glomangioma of uncertain malignant potential: a case report. Case Rep Orthop 2020;4237076. 10.1155/2020/4237076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mravic M, LaChaud G, Nguyen A, et al. Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases. Int J Surg Pathol 2015;23:181–8. 10.1177/1066896914567330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiefer TK, Parker WL, Anakwenze OA, et al. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc 2006;81:1337–44. 10.4065/81.10.1337 [DOI] [PubMed] [Google Scholar]
- 10.Tulachan B, Borgohain BN. Glomangiomyoma of the neck in a child in Nepal: a rare case report and literature review. BMC Ear Nose Throat Disord 2017;17:8. 10.1186/s12901-017-0041-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hrubý J, Novotný R, Spaček M, et al. Surgical extirpation of glomus tumor from rare localization on the upper extremity. Case Rep Vasc Med 2013;2013:1–3. 10.1155/2013/570945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ning X, Wang N, Yan H, et al. A nodule on the forearm. Dermatol Online J 2020;26. [Epub ahead of print: 15 Jan 2020]. [PubMed] [Google Scholar]