Abstract
Harvey Cushing’s 14-month Wanderjahr had a profound effect on his subsequent personal career, which in turn ushered in the modern age of American neurosurgery. From July 1900 to August 1901, he traveled to European neurosurgical centers in England, France, Switzerland, Italy, and Germany. His excursion happened at a crucial moment in his trajectory; it was built on his existing foundation of Halstedian surgical training and occurred at a time when interest in the special field of neurological surgery was emerging. The research and clinical experiences on his journey—good and bad—undoubtedly informed his fledgling neurosurgical practice. We present a concise account of Harvey Cushing’s time in Europe that consolidates accounts from Cushing’s travel journals, biographers, and other neurosurgeons. This article highlights tensions in prior works and reveals new insights into the transformative nature of his Wanderjahr. Furthermore, we contextualize his travels and achievements within the broader transformation of American medical education at the turn of the 20th century to elucidate how Europe influenced American medicine. We briefly consider parallel benefits of Harvey Cushing’s Wanderjahr and modern domestic or international training opportunities and present potential areas of implementation.
Keywords: Away rotation, Europe, Harvey Cushing, International, Residency, Wanderjahr
ORIGINS OF THE WANDERJAHR TRADITION
The German term Wanderjahr translates to “wander-year” and historically described the years that journeymen would travel and learn in different workshops following an initial apprenticeship in a tradecraft. In the 16th century, this tradition was formalized and mandatory for guild membership in German-speaking areas. Intended benefits of the Wanderjahr tradition for young craftsmen were 3-fold: (1) they learned diverse techniques to build on their apprenticeship, (2) they matured through independent travel,1 and (3) they networked. As a by-product, the rich Wanderjahr tradition helped transmit a variety of craft techniques across the continent.2
An analogous apprenticeship model became a common feature of medical education in the United States during the 17th through early 20th centuries.3,4 The limited scientific and clinical opportunities compelled American medical students to “supplement their regular course of study (Lehrjahr) by a season of travel (Wanderjahr).”5,6 An estimated 15,000 U.S. physicians traveled to Europe to supplement their medical training between 1870 and 1914.7 The popular Wanderjahr destinations varied based on the dominant centers of the time, with Italy and France attracting students in the 16th and 17th centuries, Leiden attracting students in the 18th century, and Paris attracting students in the early 19th century.5 In the late 19th century, Germany incorporated practical laboratory teaching within its university, making it the premier site for foreign training at the turn of the 20th century.8,9
The Wanderjahr tradition within U.S. medical training was distinct from the historical craftsmen tradition in that it was voluntary, limited in scope to students who could afford to travel, and non-standardized. Despite these differences, both Wanderjahr traditions allowed students to supplement their initial single-institution training and facilitated international diffusion of ideas. In this article, we focus on lessons of Dr. Harvey Cushing’s Wanderjahr (Table 1) applicable to his individual career, the greater field of neurosurgery, and current training programs.
Table 1.
Detailed Itinerary of Cushing’s Wanderjahr
| Date | Location | Nonsurgical Activities | Notable Interactions |
|---|---|---|---|
| July 1900 | Liverpool, England | Hunterian Museum | Horsley, Osler, and Robson |
| August 1900 | Paris, France | 13th International Medical Congress, French lessons, sightseeing tours, Eiffel Tower | Hartmann |
| August 1900 | Le Puy en Velay, France | Watercolor, Cathedrale Notre Dame de Puy | Grosvenor Atterbury |
| September 1900 | Lyon, France | Nove-Josserand, Jaboulay, Ollier, and Louis Dor | |
| October 1900 | Geneva and Lausanne, Switzerland | Reverdin and Roux | |
| November 1900 | Bern, Switzerland | Laboratory work, skiing, ice skating | Kocher, Kronecker, and Asher |
| May 1901 | Turin, Italy | Laboratory work | Mosso |
| June 1901 | “Grand Tour”—Genoa, Pisa, Florence, Bologna, Padua, Venice, Pavia, and Milan | Historical sightseeing | Riva-Rocci |
| June 1901 | Bern, Switzerland | Kocher and Kronecker | |
| June 1901 | Strasbourg and Heidelberg, Germany | Recklinghausen, Erb, Cohnheim, and Schmiedberg | |
| July 1901 | London, England | Laboratory work, Hunter Museum | Sherrington |
| August 1901 | Return to Boston on SS Commonwealth |
INSPIRATION
Dr. William Stewart Halsted—father of American surgery, mentor to Harvey Cushing,10 and one of the Johns Hopkins “big four”—was profoundly influenced by his European Wanderjahr from 1878 to 1880.11 When he created the first formal surgical residency in the United States in 1889, he incorporated elements of German, Austrian, and Swiss training models.12,13 In 1896, Cushing applied for Halsted’s new surgical residency program after visiting Johns Hopkins Hospital on a hospital tour.14 Given his profound admiration for medical centers in Europe, Halsted encouraged Cushing to travel to Europe explaining that “there is little if any scientific work done in this country in medicine.” Halsted was known for his fickle tendencies, and he subsequently wrote to Cushing suggesting that he join the surgical residency program in October of that year after all.10
However, by 1900, Cushing grew restless at Hopkins. On the advice of his father Henry Kirke Cushing, Sir William Osler, and Dr. William H. Welch, he ultimately decided to heed Halsted’s original recommendation. Cushing grew a “mustache to look older or more European”15 and prepared for a 14-month Wanderjahr in Europe.16
EMBARKMENT AND INITIAL DISAPPOINTMENTS
In June 1900, Cushing boarded the Servia and arrived in Liverpool, England, on July 2. His first visit was with Victor Horsley, who famously performed the first retrogasserian ganglionectomy in 1890.17 Before his travels, Cushing published a case series of 4 successful extirpations of the trigeminal ganglion with detailed anatomic pictures, a painstaking description of the operative procedure, and description of postoperative pathology.18
In contrast, Horsley used large forceps to “make a great hole in the woman’s skull,” as Cushing described in his travel journal, and quickly operated with “blood everywhere” and left the house “less than an hour after he entered it.”19 Cushing was shocked to see a renowned European surgeon operate so recklessly. More disappointments followed. His diary from this time contains scathing criticisms of poor surgical technique and failure to adopt modern principles of antisepsis.
After a disappointing month in England, he traveled to Paris for the 13th International Medical Congress and met European and American surgeons. He continued his travels in France and French Switzerland, where his mood improved. He greatly admired Cesar Roux, a Lausanne surgeon who could remove a goiter in 12 minutes. However, he was horrified at Roux’s lack of compassion for his patients who were broughat into the operating room “shivering with cold” and “operated [on] with no anesthetic.”19 When Cushing suggested using Halsted’s anesthetic technique, Roux balked at the idea of spending additional time for pain control.16 Poor treatment of patients would continue to shock Cushing during his European travels.
FORMATIVE EXPERIENCES IN BERN, SWITZERLAND
Cushing’s work with physiologist Hugo Kronecker and renowned surgeon Theodor Kocher in Bern would reinforce Cushing’s dedication to rigorous scientific discovery. Kocher tasked Cushing with understanding if “small veins and capillary vessels are dilated by stasis or compressed” owing to increased intracranial pressure (ICP). Cushing devised an intricate pulley system to apply precise pressure to the exposed canine cerebrum. He created small craniectomy defects in experimental animals and inserted fitted glass windows to directly observe the cortical vasculature while pressure was applied.16 Cushing delineated the association between ICP and arterial blood pressure, a reflex to which his name would later be ascribed. Decades later during his own Wanderjahr, thoracic surgeon Edward Churchill would be shown Cushing’s pulley system preserved as a testament to Cushing’s achievements.20
Kocher also influenced his surgical technique. Bliss14 highlighted a diary entry in which Cushing critiqued Kocher for his slow operating technique and claimed Cushing viewed his “debt to Kocher” as only in small part related to “operating technique.” However, Modlin21 cited the rest of Cushing’s glowing diary entries of Kocher’s operative technique as evidence that Cushing’s skill in “meticulous surgery had flourished from observing Kocher’s precise, careful surgical work.” In these entries, Cushing applauded the painstaking technique used by both Halsted and Kocher and complimented the similarities between surgical technique in Bern and Baltimore. Perhaps then Cushing’s early critiques of Kocher that Bliss highlighted are representative of what Fulton16 described as Cushing’s “self-assured” and “provincial” American persona during his travels. After his Wanderjahr, Cushing would continue to travel to Bern and visit Kocher—a testament to his admiration. Cushing’s own words in 1931 formed the greatest tribute to Kocher, in which he recalled telling Kocher that he would “unhesitatingly and with perfect confidence put myself in [your] hands” if he ever needed an operation.22 Cushing’s diary entries from his Wanderjahr and his long-term relationship with Kocher are evidence of the influence that Kocher had on young Cushing during his Wanderjahr.
ITALIAN SOJOURN
In late February, Cushing had completed the bulk of his experimental work and ventured south to Italy. He had an avid interest in the humanities and medical history, and he dedicated a significant amount of his Wanderjahr to studying the lives of notable artists, authors, and scientists. He admired sculpture work in Bologna and notable operating theaters in Padua.19,23
Cushing then traveled to Turin to work with Angelo Mosso, the Italian physiologist credited with implementing the first real-time intracranial monitoring system.24 Cushing appreciated that Mosso’s research subjects with craniectomy defects were analogous to his animal experimental models from Kocher’s laboratory in Bern. Using patients from what he called “Mosso’s asylum,” he hypothesized that with increased ICP, cutaneous vasculature would constrict to divert blood flow intracranially, thereby causing a compensatory increase in arterial blood pressure.25
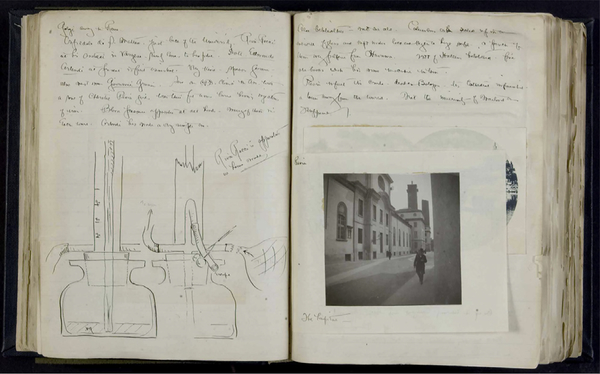
After a month in Turin, Cushing traveled to Pavia. Here he encountered the Riva-Rocci blood pressure device and quickly recognized its potential as a clinical and research tool.16 Before this point, the detailed anesthetic records Cushing had developed with Ernest Amory Codman relied on pulse measurements as the only indication of impending shock.14,26 Now he could incorporate regular blood pressure measurements. He made careful sketches of the apparatus and brought an inflatable cuff back to Baltimore (Figure 1).
Figure 1.
Sketches of Riva-Rocci’s new blood pressure apparatus from “Harvey Cushing’s Journal from Travel Abroad, 1900–1901.” (From “Harvey Cushing’s Journal from Travel Abroad, 1900–1901.” Online Exhibits@Yale, accessed January 29, 2020, http://exhibits.library.yale.edu/document/10992. Reprinted with permission from Yale University, Harvey Cushing/John Hay Whitney Medical Library.)
DENOUEMENT
After Italy, Cushing briefly revisited Bern to complete writing the manuscript that described what would later be called the Cushing reflex.25 Then he left for a whirlwind tour through the German cities of Strasbourg and Heidelberg before ending his Wanderjahr where he started in England. He worked with Sir Charles Scott Sherrington, the renowned English neurophysiologist whose seminal work, The Integrative Action of the Nervous System, laid the foundation of modern understanding of neurophysiology.27
Cushing’s diary entries here are enthusiastic and playful. He remarks on a happy, interactive chimpanzee that had a large part of his brain removed: “What a useless and annoying thing [the brain] is after all.”19 These entries stand in stark contrast to the scathing criticisms that characterize his entries from his first month in England. This transformation in tone suggests Cushing’s growing maturity and temperament—akin to the purpose of the original craftsman Wanderjahr tradition. John Fulton, a mentee, close friend, and biographer of Cushing, characterized his personal growth best. He wrote, “[Cushing] had gone to Europe a self-assured and somewhat provincial young American with many a deep-rooted prejudice; he returned a cosmopolitan with a greatly broadened point of view on medical matters, and a deep respect for European culture and tradition.”16
SEQUELAE AND LEGACY
Following his return to the United States, Cushing’s neurosurgical career flourished; his record-low brain tumor operative mortality rate offered a modicum of measured optimism for a field previously plagued by dismal outcomes.28 His success was multifactorial, but his travels abroad were undoubtedly influential.
First, his Wanderjahr afforded him expert mentorship and resources necessary to investigate the effects of increased ICP at a time when, as Sir William Osler suggested, American physicians lacked the “investigative spirit” characteristic of their German-educated counterparts.29 Second, Cushing’s time in Pavia showcases how scholarly travel facilitates the propagation of knowledge. Riva-Rocci first published on the sphygmomanometer in 1896 and then incrementally improved the design through 1897.30 When Cushing arrived 4 years later, the cuff and blood pressure device were already in routine use at their hospitals. The introduction of the sphygmomanometer in the United States revolutionized anesthetic monitoring and the understanding of blood pressure physiology.31
Cushing’s personal and academic growth during his Wanderjahr and the years that followed resulted in an exhaustive 1908 textbook titled Surgery of the Head. This work cemented him as a global neurosurgery expert, and, as Modlin suggested, this “marked a turning point, because American physicians who had previously studied in Europe now sought to pursue the discipline of brain surgery in the United States itself.”15,32 For example, Scottish surgeon Norman M. Dott used his Rockefeller fellowship to study with Cushing in 1923e1924. Dott was transformed by this experience, just as Cushing was by his Wanderjahr, and attested that it “sealed his destiny to devote himself to the field of neurosurgery.”33
PARALLELS FOR MODERN TRAINING
Combined with his own innate potential, Cushing’s exposure to a diverse set of prominent surgeons and physiologists was a catalyst for his early career. The neurosurgical training paradigm, practice environment, and sheer volume of available medical knowledge today are vastly different than in Cushing’s era, yet some features of his Wanderjahr experience can be paralleled by incorporating cross-institutional opportunities into modern neurosurgical training. These opportunities would allow for diversified training, disseminate techniques, and improve scientific collaboration—important sequelae of Cushing’s own Wanderjahr.
The education of aspiring surgeons at the turn of the 20th century was limited in part by the relative scarcity and quality of master clinicians from whom to learn.4 On one hand, today the diversity of the operative training experience for residents in the United States is threatened by—among multiple factors—regionalization and subspecialization of experts.34,35 On the other hand, the shrinking world permits rapid dissemination of data and evidence via journal articles, online textbooks, surgical videos, simulators, interviews, and anatomic atlases that may supplement traditional education. Nonetheless, in-person, mentored instruction allows the transmission of subtleties, nuances, and intangibles that may not be well suited for these other learning media. Furthermore, in-person training allows for the formation of relationships that can further facilitate cross-institutional basic science and clinical practice collaboration. Though technology has enabled rapid and global dissemination of experience, these longer, in-person training opportunities remain invaluable for surgical training.
Leaders in neurosurgical education have developed many innovative solutions to current and future challenges in contemporary training.36,37 The benefits of away rotations in ensuring adequate subspecialty case volume have been described,35 but perhaps these initiatives could be used more broadly. For example, a subset of programs might establish an inter-residency rotation program in which senior residents participate in a brief, chainlike exchange system. Logistical, financial, regulatory, insurance, and licensing barriers to creating such a program certainly abound. Nevertheless, the potential benefits of domestic or international rotational systems for training and development (as employed in business,38 the military,39 and the historical Wanderjahr) may be a consideration for future neurosurgical educators.
Acknowledgments
Conflict of interest statement: P. D. Kelly is supported by a training grant from the National Cancer Institute of the National Institutes of Health (award number T32CA106183).
Abbreviations and Acronyms
- ICP
Intracranial pressure
REFERENCES
- 1.Walker M German Home Towns: Community, State, and General Estate, 1648–1871. Ithaca, NY: Cornell University Press; 1998. [Google Scholar]
- 2.Werner GS. Traveling journeymen in Metternichian South Germany. Proc Am Philos Soc. 1981;125: 190–219. [Google Scholar]
- 3.Custers EJFM, Cate OT. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018; 93(3 Suppl):S49–S54. [DOI] [PubMed] [Google Scholar]
- 4.Flexner A Medical Education in the United States and Canada. Washington, DC: Science and Health Publications; 1910. [Google Scholar]
- 5.Koehler PJ. European ‘Wanderjahr’: postgraduate training in nervous diseases for Americans in the 1880s. World Neurology. January 2016. https://worldneurologyonline.com/article/european-wanderjahr-postgraduate-training-in-nervous-diseases-for-americans-in-the-1880s/. [Accessed 5 January 2020]. [Google Scholar]
- 6.Hun H A Guide to American Medical Students in Europe. New York: William Wood; 1883. [Google Scholar]
- 7.Herfarth CH. German surgery at a turning point—between tradition and internationalization (Leopoldina Lecture). Am J Surg. 2007;194(4 Suppl): S165–S170. [Google Scholar]
- 8.Fulton JF. History of medical education. Br Med J. 1953;2:457461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duffy TP. The Flexner Report—100 years later. Yale J Biol Med. 2011;84:269–276. [PMC free article] [PubMed] [Google Scholar]
- 10.Voorhees JR, Tubbs RS, Nahed B, Cohen-Gadol AA. William S. Halsted and Harvey W. Cushing: reflections on their complex association. J Neurosurg. 2009;110:384. [DOI] [PubMed] [Google Scholar]
- 11.Roberts CSHL. Mencken and the four doctors: Osler, Halsted, Welch, and Kelly. Proc (Bayl Univ Med Cent). 2010;23:377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cameron JL. Halsted William Stewart. Our surgical heritage. Ann Surg. 1997;225:445–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grillo HC. To impart this art: the development of graduate surgical education in the United States. Surgery. 1999;125:1–14. [PubMed] [Google Scholar]
- 14.Bliss M Harvey Cushing: A Life in Surgery. New York: Oxford University Press; 2005. [Google Scholar]
- 15.Modlin IM, Shin JH. Harvey Cushing: first guest at “The Divine Banquet of the Brayne.” Surgery. 1992; 113:438–455. [PubMed] [Google Scholar]
- 16.Fulton J Harvey Cushing: A Biography. Springfield, IL: Charles C Thomas; 1946. [Google Scholar]
- 17.Wilkins RH. Neurosurgical classic—XIII. J Neurosurg. 1963;20:1009–1022. [DOI] [PubMed] [Google Scholar]
- 18.Cushing H A method of total extirpation of the Gasserian ganglion for trigeminal neuralgia. JAMA. 1900;34:1035–1041. [DOI] [PubMed] [Google Scholar]
- 19.Cushing H Notes Made During a Sojourn of Fourteen Months in Some Parts of the Old World, 1900 Junee1901 August. Manuscripts and Archives, Yale University Library. New Haven, CT: Yale University; 1900–1901. [Google Scholar]
- 20.Churchill ED. Wanderjahr: The Education of a Surgeon. Boston, MA: The Francis A. Countway Library of Medicine; 1990. [Google Scholar]
- 21.Modlin IM. Surgical triumvirate of Theodor Kocher, Harvey Cushing, and William Halsted. World J Surg. 1998;22:103–113. [DOI] [PubMed] [Google Scholar]
- 22.Fulton JF. Arnold Klebs and Harvey Cushing at the 1st International Neurological Congress at Berne in 1931. Bull Hist Med. 1940;8:332–354. [PubMed] [Google Scholar]
- 23.Wahl CJ, Tubbs RS, Spencer DD, Cohen-Gadol AA. Harvey Cushing as a book collector, bibliophile, and archivist: the precedence for the genesis of the Brain Tumor Registry. Historical vignette. J Neurosurg. 2009;111:1091–1095. [DOI] [PubMed] [Google Scholar]
- 24.Nowinski WL. Anatomy of the Brain. In: Miller K, ed. Biomechanics of the Brain. New York, NY: Springer; 2011:1–35. [Google Scholar]
- 25.Cushing H Concerning a definite regulatory mechanism of the vaso-motor centre which controls blood pressure during cerebral compression. Johns Hop Hos Bul. 1901;12:290–292. [Google Scholar]
- 26.Sundararaman LV, Desai SP. The anesthesia records of Harvey Cushing and Ernest Codman. Anesth Analg. 2018;126:322–329. [DOI] [PubMed] [Google Scholar]
- 27.Burke RE. Sir Charles Sherrington’s The integrative action of the nervous system: a centenary appreciation. Brain. 2007;130(Pt 4):887–894. [DOI] [PubMed] [Google Scholar]
- 28.Greenblatt SH. Harvey Cushing’s paradigmatic contribution to neurosurgery and the evolution of his thoughts about specialization. Bull Hist Med. 2003;77:789–822. [DOI] [PubMed] [Google Scholar]
- 29.Cushing H Biography of Sir William Osler. Oxford: Clarendon Press; 1926. [Google Scholar]
- 30.Alberto Zanchetti GM. The centenary of blood pressure measurement: a tribute to Scipione Riva-Rocci. Blood Press. 1996;5:325–326. [DOI] [PubMed] [Google Scholar]
- 31.Crenner CW. Introduction of the blood pressure cuff into U.S. medical practice: technology and skilled practice. Ann Intern Med. 1998;128:488–493. [DOI] [PubMed] [Google Scholar]
- 32.Preul MC, Feindel W. Origins of Wilder Penfield’s surgical technique. J Neurosurg. 1991;75:812. [DOI] [PubMed] [Google Scholar]
- 33.Prieto R, Pascual JM, Norman M. Dott, master of hypothalamic craniopharyngioma surgery: the decisive mentoring of Harvey Cushing and Percival Bailey at Peter Bent Brigham Hospital. J Neurosurg. 2017;127:927. [DOI] [PubMed] [Google Scholar]
- 34.Das P, Guillaume DJ. Improving outcomes with subspecialization and regionalization. In: Guillaume DJ, Hunt MA, eds. Quality and Safety in Neurosurgery. London: Academic Press; 2018: 225–236. [Google Scholar]
- 35.Gephart MH, Derstine P, Oyesiku NM, et al. Resident away rotations allow adaptive neurosurgical training. Neurosurgery. 2015;76:421–426. [DOI] [PubMed] [Google Scholar]
- 36.Mazzola CA, Lobel DA, Krishnamurthy S, Bloomgarden GM, Benzil DL. Efficacy of neurosurgery resident education in the new millennium: the 2008 Council of State Neurosurgical Societies post-residency survey results. Neurosurgery. 2010;67:225–232 [discussion: 232–233]. [DOI] [PubMed] [Google Scholar]
- 37.Kim DH, Dacey RG, Zipfel GJ, et al. Neurosurgical education in a changing healthcare and regulatory environment: a consensus statement from 6 programs. Neurosurgery. 2017;80(4 Suppl):S75–S82. [DOI] [PubMed] [Google Scholar]
- 38.Eriksson T, Ortega J. The adoption of job rotation: testing the theories. Ind Labor Relat Rev. 2006;59: 653–666. [Google Scholar]
- 39.Jans N, Frazer-Jans J. Career development, job rotation, and professional performance. Armed Forces Soc. 2004;30:255–277. [Google Scholar]