Summary
Caesarean section is associated with moderate‐to‐severe postoperative pain, which can influence postoperative recovery and patient satisfaction as well as breastfeeding success and mother‐child bonding. The aim of this systematic review was to update the available literature and develop recommendations for optimal pain management after elective caesarean section under neuraxial anaesthesia. A systematic review utilising procedure‐specific postoperative pain management (PROSPECT) methodology was undertaken. Randomised controlled trials published in the English language between 1 May 2014 and 22 October 2020 evaluating the effects of analgesic, anaesthetic and surgical interventions were retrieved from MEDLINE, Embase and Cochrane databases. Studies evaluating pain management for emergency or unplanned operative deliveries or caesarean section performed under general anaesthesia were excluded. A total of 145 studies met the inclusion criteria. For patients undergoing elective caesarean section performed under neuraxial anaesthesia, recommendations include intrathecal morphine 50–100 µg or diamorphine 300 µg administered pre‐operatively; paracetamol; non‐steroidal anti‐inflammatory drugs; and intravenous dexamethasone administered after delivery. If intrathecal opioid was not administered, single‐injection local anaesthetic wound infiltration; continuous wound local anaesthetic infusion; and/or fascial plane blocks such as transversus abdominis plane or quadratus lumborum blocks are recommended. The postoperative regimen should include regular paracetamol and non‐steroidal anti‐inflammatory drugs with opioids used for rescue. The surgical technique should include a Joel‐Cohen incision; non‐closure of the peritoneum; and abdominal binders. Transcutaneous electrical nerve stimulation could be used as analgesic adjunct. Some of the interventions, although effective, carry risks, and consequentially were omitted from the recommendations. Some interventions were not recommended due to insufficient, inconsistent or lack of evidence. Of note, these recommendations may not be applicable to unplanned deliveries or caesarean section performed under general anaesthesia.
Keywords: analgesia, caesarean section, caesarean delivery, pain
Recommendations
Implement strategies to minimise systemic opioid utilisation and develop individualised or stratified post‐discharge opioid prescribing practices to reduce unnecessary opioid analgesic consumption after elective caesarean section.
Add intrathecal morphine 50–100 µg or diamorphine 300 µg to spinal anaesthesia. Epidural morphine 2–3 mg or diamorphine 2–3 mg may be used as an alternative, for example, when an epidural catheter is used as part of a combined spinal‐epidural technique.
Prescribe paracetamol and a non‐steroidal anti‐inflammatory drug (NSAID) administered after delivery and continued regularly postoperatively.
Administer a single dose of intravenous (i.v.) dexamethasone after delivery in the absence of contra‐indications.
Consider a single injection of local anaesthetic infiltration, continuous wound local anaesthetic infusion and/or fascial plane blocks, if intrathecal morphine is not used.
Use a surgical technique that includes the Joel‐Cohen incision, non‐closure of the peritoneum and abdominal binders.
Consider the use of transcutaneous electrical nerve stimulation as an analgesic adjunct.
Why was this guideline developed?
Caesarean section is associated with moderate‐to‐severe postoperative pain which may influence recovery, psychological maternal well‐being, breastfeeding and mother‐child bonding. The aim of this guideline is to provide clinicians with updated evidence for optimal pain management following elective caesarean section under neuraxial anaesthesia.
What other guidelines are available on this topic?
The procedure‐specific postoperative pain management (PROSPECT) recommendations for pain management after caesarean section were published in 2014; however, an update assessing analgesic interventions was necessary given developments in clinical practice. The American College of Obstetricians and Gynecologists has provided recommendations for postpartum pain management which are available on their website.
How does this guideline differ from other guidelines?
The updated systematic review further confirms the previous recommendations. Also, an updated PROSPECT approach was used to develop the current recommendations such that the available evidence is critically assessed for current clinical relevance and the use of simple, non‐opioid analgesics such as paracetamol and NSAIDs as basic analgesics. This approach reports true clinical effectiveness by balancing the invasiveness of the analgesic interventions and the degree of pain after surgery, as well as balancing efficacy and adverse effects.
Introduction
Caesarean section is associated with moderate‐to‐severe postoperative pain in a significant proportion of women, which may delay recovery and return to activities of daily living; impair mother‐child bonding; impact maternal psychological well‐being; and may complicate breastfeeding [1]. Furthermore, inadequate postoperative pain relief may lead to hyperalgesia and persistent postoperative pain [2].
Pain after caesarean section is often under‐treated due to unfounded fears that analgesic drugs or interventions might induce maternal and neonatal side‐effects and because the severity of post‐caesarean section pain is often underestimated [3]. Based on a systematic review performed in 2014 [4], the PROSPECT Working Group [5, 6], which is a collaboration of surgeons and anaesthetists, previously provided recommendations for pain management in women undergoing caesarean section. Recently, several new techniques have been developed to manage pain after caesarean, such as the quadratus lumborum block; slow‐release local anaesthetics; and non‐pharmacological approaches. Additionally, in the last decade, attention has shifted to reduce opioid use and to implement protocols for enhanced recovery after caesarean section. Therefore, an updated systematic review on analgesic interventions for pain management after elective caesarean section performed using neuraxial anaesthesia was needed. In addition, it was deemed necessary to re‐assess the recommendations to align them with the updated PROSPECT approach that considers current clinical relevance and clinical effectiveness by balancing the invasiveness of the analgesic interventions and the degree of pain after surgery, as well as balancing efficacy and adverse effects [7, 8].
The aim of this systematic review was to provide updated recommendations based on recent literature assessing the impact of analgesic and surgical approaches on pain after elective caesarean section performed under neuraxial anaesthesia. Postoperative pain scores were the primary outcome measures. Other recovery outcomes assessed included cumulative opioid consumption and adverse effects. The limitations of the available evidence were also assessed. The ultimate aim was to develop recommendations for pain management after elective caesarean section performed under neuraxial anaesthesia.
Methods
The methods of this review adhered to the previously reported PROSPECT methodology [8]. Specific to this study, the Embase, MEDLINE, PubMed and Cochrane databases (Cochrane Central Register of Controlled Trials; Cochrane Database of Abstracts or Reviews of Effects; Cochrane Database of Systematic Reviews) were searched for randomised controlled trials, systematic reviews and meta‐analyses published between 1 May 2014 and 22 October 2020. The search terms used were: (cesarean section OR cesarean OR cesarean delivery) AND (pain OR postoperative pain OR analgesia OR anesthesia OR anaesthesia OR anesthetic) AND (anesthetics neuraxial OR intrathecal OR spinal OR epidural analgesia OR paravertebral blocks OR peripheral nerve OR peripheral block OR regional nerve OR transversus abdominis plane block OR infiltration OR instillation OR NSAID OR COX‐2 OR paracetamol OR acetaminophen OR gabapentin OR pregabalin OR clonidine OR opioid OR ketamine OR corticosteroid OR dexamethasone OR peritoneal closure OR skin incision OR skin closure). Only studies in which patients underwent elective caesarean section under neuraxial anaesthesia were included.
Quality assessment, data extraction and data analysis adhered to the PROSPECT methodology [8]. In this study, we defined a change of more than 10/100 mm on the visual analogue scale or numerical rating score as clinically‐relevant [8]. The effectiveness of each intervention for each outcome was evaluated qualitatively by assessing the number of studies showing a significant difference between treatment arms. We also evaluated for each study if patients received ‘basic’ analgesia (i.e. paracetamol and/or NSAIDs) and ‘baseline’ analgesia (i.e. routine administration of an analgesic additional to the study intervention). We decided not to perform a meta‐analysis a priori due to heterogeneity in study design and result reporting, restricting pooled analysis.
Recommendations were made according to PROSPECT methodology [8]. In brief, this involved a grading of A–D according to the overall level of evidence, as determined by the quality of studies included, consistency of evidence and study design. The proposed recommendations were sent to the PROSPECT Working Group for review and comments and a modified Delphi approach was utilised as previously described. Once a consensus was achieved the lead authors drafted the final document, which was ultimately approved by the Working Group. The Obstetric Anaesthetists’ Association Executive Committee were consulted on the final PROSPECT recommendations and offered their support.
Results
A total of 145 studies were included, of which 126 were randomised controlled trials and 19 were systematic reviews and meta‐analyses (Fig. 1) [9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139, 140, 141, 142, 143, 144, 145, 146, 147, 148, 149, 150, 151, 152, 153]. The methodological quality assessments of the 126 randomised controlled trials included in the final qualitative analysis are summarised in online Supporting Information Table S1. The characteristics of the included studies are shown in online Supporting Information Tables S2 and S3.
Figure 1.
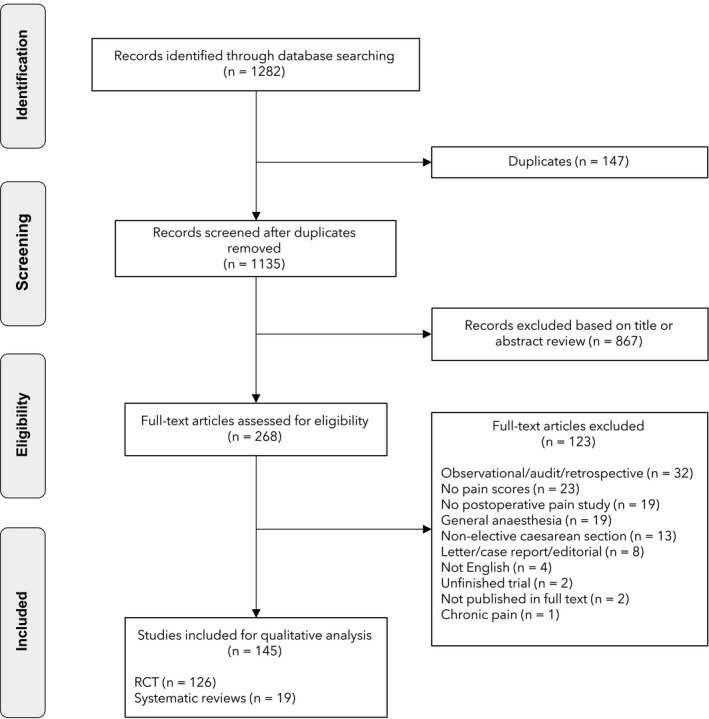
Flow diagram of studies included in this systematic review.
Systemic non‐opioid and opioid analgesics
When paracetamol was administered pre‐operatively rather than at the end of surgery, only minor differences were noted [9]. In one study, rectal paracetamol was shown to be superior to pre‐operative oral paracetamol combined with i.v. paracetamol at the end of surgery [10]. In one study, opioid consumption was reduced with i.v. paracetamol compared with placebo but there was no difference in pain scores [11]. In another study, no differences in opioid consumption and pain scores were noted with i.v. paracetamol [12].
A meta‐analysis concluded that systemic NSAIDs reduced pain scores, decreased opioid consumption, reduced opioid‐related side‐effects and increased patient satisfaction [13]. A Cochrane review evaluated oral analgesics, comprising primarily but not exclusively NSAIDs, but could not draw any conclusions due to the low quality of studies, small number of included patients and substantial heterogeneity in the studied drugs (paracetamol; celecoxib; ibuprofen; gabapentin; combination) [14]. Inthigood et al. evaluated a single dose of i.v. parecoxib 40 mg and noted better pain scores than with placebo [15]. Three studies compared an NSAID with an opioid and demonstrated equally effective or superior analgesia with NSAIDs [16, 17, 18]. The addition of rectal diclofenac to pentazocine was also associated with better analgesia then pentazocine alone [19].
Four randomised controlled trials [20, 21, 22, 23] and a meta‐analysis [24] evaluated pre‐operative gabapentinoids for analgesia after caesarean section. No significant benefits were reported with gabapentin when added to a multimodal analgesia regimen [20]. The multimodal regimen consisted of intrathecal morphine, rectal and oral paracetamol and i.v. and oral NSAID [20]. Administration of pregabalin combined with intramuscular diclofenac, but without intrathecal morphine, was associated with lower pain scores and reduced opioid requirements [21]. In another study, gabapentin provided superior analgesia compared with intrathecal fentanyl [22]. In the two latter studies, basic analgesia consisted of diclofenac [21, 22]. In a study conducted on patients who did not receive any basic analgesia, adding vitamin B complex to gabapentin reduced pain scores and opioid consumption compared with the use of gabapentin alone [23]. A systematic review reported a clinically significant reduction in 24‐h pain scores with pre‐operative gabapentin. Side‐effects such as sedation and dizziness were reported in several of the included studies [24].
Adding i.v. lidocaine to i.v. patient‐controlled analgesia (PCA) with morphine did not improve pain scores or opioid consumption [25]. One randomised controlled trial evaluated the effects of i.v. ketamine on postoperative analgesia [26]. A bolus of i.v. ketamine after delivery of the fetus reduced pain and rescue analgesics in the first 12 h after caesarean section [26]. In the latter study, no basic analgesia or additional baseline analgesia was given [26]. A meta‐analysis on the i.v. use of ketamine demonstrated marginal improvements in pain scores and a mild reduction in morphine consumption [27].
Compared with sufentanil PCA alone, the addition of dexmedetomidine to a sufentanil PCA in the postoperative period was associated with lower pain scores, reduced sufentanil consumption, reduced need for rescue analgesia and a higher patient satisfaction. However, the improved pain scores were not clinically relevant [28]. In the latter study, no basic or additional baseline analgesia was given [28].
Four randomised controlled trials evaluated the use of i.v. dexamethasone [29, 30, 31, 32]. Use of i.v. dexamethasone was associated with better pain scores; prolongation of analgesic effect [29]; a reduction in opioid consumption [30]; and a reduced need for postoperative anti‐emetics [31]. One study reported better analgesia when dexamethasone was administered as wound infiltration as opposed to i.v. administration [32]. Intravenous dexamethasone was not as effective as i.v. tramadol [32].
Several studies compared various systemic opioids (oxycodone; sufentanil; tramadol; dezocine; butorphanol; hydromorphone; tapentadol) [33, 34, 35, 36, 37, 38, 39, 40]. No individual drug was clearly superior in terms of analgesia or side‐effect profile compared with any other opioid.
Neuraxial adjuvant drugs
One meta‐analysis [41] and three randomised controlled trials [42, 43, 44] evaluated the administration of intrathecal morphine. The meta‐analysis compared low (50–100 µg) and high (> 100 µg) doses of intrathecal morphine and concluded that high doses increase the duration of analgesia but were more likely to be associated with side‐effects. Pain scores were similar in both groups [41]. A dose‐response study of intrathecal morphine showed that 50 µg doses were as effective as 100 µg and 150 µg, with a similar requirement for rescue opioids. The risk of pruritus was lowest after 50 µg morphine [42]. In patients with an anticipated high pain intensity (such as patients with chronic pelvic pain), pain scores with movement were lower in patients receiving 300 µg vs. those receiving 150 µg intrathecal morphine [43]. In a comparative study, intrathecal morphine provided better analgesia compared with epidural morphine and patient‐controlled epidural analgesia of ropivacaine with sufentanil [44]. In two studies, women were offered to choose the analgesic strategy and select either no intrathecal morphine or a low or high dose of intrathecal morphine [45, 46]. Having a choice did not impact on rescue opioid consumption, but women were very good in predicting their actual opioid needs. Choosing high‐dose intrathecal morphine was associated with increased rescue analgesia and more vomiting [45, 46]. Apart from one study [44], all studies used basic analgesia with NSAIDs [42, 43, 46] or a combination of NSAIDs and paracetamol [45]. Intrathecal morphine was similar to intrathecal hydromorphone in a recent trial by Sharpe et al. [47].
Ten trials evaluated the neuraxial administration of ɑ2‐agonists such as clonidine and dexmedetomidine [48, 49, 50, 51, 52, 53, 54, 55, 56, 57]. A meta‐analysis showed that neuraxial clonidine increased the duration and quality of analgesia and reduced morphine consumption [48]. However, more side‐effects such as hypotension and intra‐operative sedation were noted. No improvements in analgesia were reported with intrathecal or i.v. clonidine, whether administered alone [49] or in combination with intrathecal morphine [50]. One study demonstrated the superiority of intrathecal clonidine to intrathecal fentanyl [51]. Addition of epidural dexmedetomidine to combined spinal‐epidural anaesthesia resulted in improved intra‐operative and postoperative analgesia and less requirements for opioid rescue [52]. A comparison of intrathecal dexmedetomidine with intrathecal morphine did not demonstrate any significant differences in duration of analgesia, pain scores or need for rescue analgesia. However, both intrathecal morphine and intrathecal dexmedetomidine provided better analgesia when compared with isobaric bupivacaine (53). Administration of intrathecal dexmedetomidine resulted in improved postoperative analgesia when compared with isobaric bupivacaine or ropivacaine alone [54, 55]. Intrathecal dexmedetomidine combined with intrathecal magnesium sulphate or intrathecal morphine improved analgesia which was of longer duration than analgesia produced by magnesium sulphate alone [56, 57]. Adding intrathecal fentanyl to bupivacaine improved initial analgesia [58]. However, when morphine is also added to the intrathecal mixture, fentanyl might induce acute opioid tolerance and result in greater opioid consumption [59]. Intrathecal buprenorphine [60] and epidural hydromorphone [61] resulted in improved postoperative analgesia and reduced opioid consumption compared with intrathecal bupivacaine or ropivacaine alone.
A meta‐analysis evaluating the effect of neuraxial magnesium on postoperative analgesia demonstrated a longer duration of sensory block, lower pain scores and reduced rescue analgesia requirements then neuraxial mixtures of local anaesthetic without magnesium [62].
The use of intrathecal midazolam was evaluated in several studies [63, 64]. A comparative study demonstrated that intrathecal magnesium and intrathecal sufentanil were superior to intrathecal midazolam [63]. Intrathecal midazolam prolonged the duration of spinal anaesthesia when compared with placebo [64]. Intrathecal ketamine prolonged analgesia when compared with fentanyl [65, 66]. A meta‐analysis showed that intrathecal neostigmine improved analgesia after caesarean section, although it was associated with an increased risk of nausea and vomiting [67]. A study showed that a faster speed of intrathecal injection of fentanyl and local anaesthetic results in improved postoperative analgesia with a more sustained duration [68].
Local and regional analgesia techniques
Intraperitoneal local anaesthetic instillation resulted in lower early pain scores [69], and reduced pain scores at 24 h in a sub‐group in which the peritoneum was closed [69]. The use of topical analgesia (e.g. eutectic mixture of local anaesthetic cream) failed to reduce pain scores at 24 and 48 h [70].
Three studies demonstrated that local anaesthetic wound infiltration reduced pain scores and the need for rescue analgesia during the first 24 h after caesarean section [71, 72, 73], while one study showed only limited benefits [74]. Apart from one study [72], basic analgesia with ibuprofen and paracetamol was provided. Another two studies which used multimodal analgesia showed improved pain scores, less morphine consumption and higher breastfeeding comfort with continuous wound infusion compared with no infusion [75, 76]. Local anaesthetic wound infusion resulted in similar analgesic effects as intrathecal morphine [76]. A meta‐analysis confirmed that both single‐shot local anaesthetic wound infiltration and continuous wound infusion reduce postoperative opioid consumption and mildly improve pain scores [77]. Pain scores were similar whether the catheter was placed preperitoneal or subcutaneously [78]. Adding ketorolac improved analgesia of wound infiltration and reduced opioid consumption [79]. In a recent study, ketorolac added to wound infiltration did not improve analgesia but intrathecal morphine was administered in both groups [80]. Magnesium and dexmedetomidine as adjuvants to wound infiltration reduced pain scores [81, 82].
A rectus sheath block provides no additional analgesic benefit when added to multimodal analgesia which also includes intrathecal morphine [83]. Adding a field block after caesarean section to intrathecal morphine also did not improve analgesia after caesarean section [84].
There were five studies that compared transversus abdominis plane (TAP) blocks against placebo or no TAP block [85, 86, 87, 88, 89]. Apart from one study [85], all studies noted that TAP blocks improved pain relief, increased patient satisfaction and resulted in a reduction of rescue analgesia. A comparison between lateral and posterior approaches concluded that the posterior approach resulted in better pain scores which was only clinically relevant at 12 h postoperatively. This approach also resulted in reduced need for rescue analgesia [90]. Comparison between surgeon‐administered and anaesthetist‐administered TAP blocks did not show any differences in postoperative analgesia [91].
Several studies evaluated the role of local anaesthetic adjuvants for TAP blocks. Pain scores, opioid consumption and duration of analgesia were significantly improved when dexamethasone was added to local anaesthetic for TAP blocks [92]. Fentanyl added to TAP blocks failed to improve the quality of analgesia [93]. The addition of ɑ2‐agonists (clonidine or dexmedetomidine) prolonged the duration of analgesia, reduced the need for rescue drugs and improved patient satisfaction [94, 95, 96]. However, mild sedation was noted in some patients [94, 95, 96].
Several studies compared TAP blocks with alternative regional anaesthesia techniques [97, 98, 99, 100, 101, 102, 103]. In a comparison of TAP blocks with epidural analgesia which included high‐dose epidural morphine, improved analgesia with the epidural analgesia was noted [97]. Three studies compared intrathecal morphine with TAP blocks [98, 99, 100]. In two of these, there was better analgesia with intrathecal morphine and a reduced requirement for rescue analgesia. However, postoperative mobilisation and return of gastro‐intestinal function was better with TAP blocks [98, 99]. The third study could not discriminate between the two techniques in terms of pain relief and other clinical outcomes [100]. Three randomised controlled trials compared TAP blocks with continuous local anaesthetic wound infusion and noted no differences in postoperative analgesia [101, 102, 103].
Three meta‐analyses confirmed the efficacy of TAP blocks for analgesia after caesarean section but concluded that they do not confer any benefit over intrathecal morphine [104, 105, 106]. A combination of ilioinguinal and iliohypogastric nerves block with TAP blocks vs. no blocks resulted in less rescue opioid consumption and lower pain scores [107]. Adding dexmedetomidine to a ropivacaine bilateral ultrasound‐guided TAP block resulted in lower postoperative pain scores and less rescue opioid [108]. Quadratus lumborum blocks were evaluated in 11 trials [109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119]. Compared with a sham block, quadratus lumborum blocks produced better analgesia. In two trials quadratus lumborum blocks were found to be superior to a TAP blocks [113, 114, 118, 119]. In one study, quadratus lumborum blocks were less effective than a single epidural bolus of local anaesthetic [115]. Adding quadratus lumborum blocks to intrathecal morphine did not improve analgesia [116]. However, in a direct comparison, a quadratus lumborum block was similar to intrathecal morphine [117]. Two recent meta‐analyses evaluated TAP blocks, wound infusion and quadratus lumborum blocks with or without intrathecal morphine and concluded that all three regional anaesthetic techniques are superior to no regional technique in the absence of intrathecal morphine [120, 121]. When intrathecal morphine is administered, adding these techniques confers no further advantages.
Two studies recently evaluated the erector spinae plane block (ESP) compared with TAP block and intrathecal morphine and in both studies the ESP block improved analgesia [122, 123].
Patient‐controlled epidural analgesia
Patient‐controlled epidural analgesia added to intrathecal morphine resulted in a further lowering of postoperative pain scores and less need for rescue opioid [124]. Adding fentanyl to patient‐controlled epidural analgesia with levobupivacaine did not improve analgesia [125].
Postoperative interventions
Several investigators reported on the beneficial effects of transcutaneous electrical nerve stimulation on pain scores, rescue analgesia use and patient satisfaction [126, 127]. A study demonstrated that self‐administered oral opioid analgesia was as effective as parenteral nurse‐administered drugs [128]. A comparison of a fixed time‐interval with on‐demand oral analgesia concluded that the latter was associated with better pain scores [129]. One study evaluated the use of relaxation sounds intra‐ or postoperatively and showed improved pain scores [130]. One study evaluated the use of early skin‐to‐skin contact between mother and baby and noted no differences in postoperative pain scores [131].
Three studies evaluated the use of elastic abdominal binders after caesarean section [132, 133, 134]. In all three, a clinically‐relevant reduction in pain scores and rescue analgesia was noted [132, 133, 134]. Two studies evaluated the application of manual cervical dilation at the end of caesarean section and compared it with no cervical dilation and came to conflicting conclusions [135, 136]. One study noted improved pain scores until 7 days postoperatively [135] while the other did not report any pain reduction [36]. Pre‐operative vaginal cleansing resulted in minor but statistically significant reductions in postoperative pain scores [137].
Surgical interventions
A systematic review [138] confirmed the superiority of the Joel‐Cohen (also called modified Misgav‐Ladach) incision compared with Pfannenstiel incision in reducing postoperative pain [139]. No differences in pain scores were noted between using a scalpel vs. diathermy for the skin incision [139].
A blunt fascial opening resulted in less postoperative pain [140]. The older technique of extraperitoneal section was associated with better pain scores up to 48 h postoperatively [141]. In one study, the absence of making a bladder flap at opening the uterus resulted in clinically‐relevant improvements in postoperative pain scores [142]. A comparison between uterine exteriorisation and in situ closure of the uterus showed more postoperative pain with exteriorised uteri [143]. However, one meta‐analysis did not show any difference in postoperative pain between the two modalities of uterine closure [144].
A comparison between two techniques of pyramidalis muscle dissection found no differences in postoperative pain [145]. Reduced pain scores when the peritoneum was not closed were reported [146]. One study reported a significant reduction in postoperative pain scores when the rectus muscle was not re‐approximated [147]. A Cochrane review noted minimal evidence for reduced pain scores when the peritoneum was not closed after caesarean section [148]. When applying laser irradiation to the caesarean section wound at the end of surgery, less pain during the first 24 h postoperatively was noted [149, 150]. No differences in pain scores were noted between interrupted and continuous wound suturing [151]. Similarly, two meta‐analyses did not show any difference in pain scores whether skin closure was performed with sutures or staples [152, 153].
Discussion
The majority of the studies included in this systematic review were determined to be of high quality. The updated literature strengthens the previous PROSPECT recommendations for pain management in patients undergoing elective caesarean section and modifies it in certain aspects. The updated PROSPECT methodology further strengthens the recommendations, because it goes beyond assessment of the available evidence based solely on statistical analysis [8].
Of note, it is essential to highlight that this guideline focuses on elective caesarean section under neuraxial anaesthesia. Importantly, these recommendations should not be applied to other patient populations such as emergency or unplanned caesarean section or surgery performed under general anaesthesia.
The recommended strategies have sufficient procedure‐specific evidence and have a positive balance of clinical benefits and risk of side‐effects (Table 1). Basic analgesia after caesarean section should always consist of paracetamol and NSAIDs started intra‐operatively (after delivery) and continued postoperatively, unless there are contra‐indications. Of note, several studies demonstrated equally good pain control with NSAIDs compared with opioids. Regular administration of basic analgesics is important to limit the need for rescue opioid analgesia. Moreover, studies investigating an analgesic strategy to manage pain relief after caesarean section should not omit this basic strategy of analgesia so as to establish the additional value of an investigational approach. In addition to basic analgesics, i.v. dexamethasone demonstrated positive effects on pain scores and opioid consumption. In addition, i.v. dexamethasone provides anti‐emetic prophylaxis. Thus, i.v. dexamethasone is recommended. Caution is required in patients with glucose intolerance.
Table 1.
Overall recommendations for pain management in patients undergoing elective caesarean section.
| Pre‐operatively |
|
| Intra‐operative after delivery |
|
| Postoperative |
|
| Surgical technique |
|
Intrathecal morphine at doses of 100 µg or lower is recommended. Doses lower than 100 µg result in adequate analgesia with a reduced incidence of side‐effects. Recently, Sharawi et al. confirmed the safety of intrathecal morphine when used in patients undergoing caesarean section [154]. Importantly, basic analgesics (i.e. paracetamol and NSAIDs) and i.v. dexamethasone should be used with intrathecal morphine. Of note, the National Institute of Health and Care Excellence (NICE) guidelines in the UK recommend intrathecal diamorphine as an alternative to intrathecal morphine [155]. Intrathecal diamorphine 300 µg is recommended. When spinal anaesthesia is not possible or when an epidural catheter is in situ, epidural morphine or diamorphine both in doses of 2–3 mg can be used.
Various local anaesthetic techniques such as TAP blocks, quadratus lumborum blocks and local anaesthetic wound infiltration are effective in reducing pain scores and opioid requirements. Given that the potential side‐effects of these regional analgesic techniques are limited, they are recommended. However, the additional value of any of these techniques when combined with intrathecal morphine appears to be minimal. Therefore, these blocks may be administered if intrathecal morphine is not used.
Surgical techniques that have been shown to be beneficial and are therefore recommended include Joel‐Cohen incision and avoidance of peritoneum closure. Using abdominal binders postoperatively is recommended with sufficient procedure‐specific evidence being identified. Analgesic adjuncts such as listening to music via headphones and use of transcutaneous electrical nerve stimulation may be associated with improved pain relief and are recommended when available.
Although pre‐operative gabapentinoids were recommended previously, they are no longer recommended despite positive studies of their benefits due to concerns about side‐effects such as sedation and respiratory depression [156]. Furthermore, it is not clear if gabapentinoids add to our current recommendations of basic analgesia, i.v. dexamethasone and regional analgesia.
Several intra‐operative interventions are not recommended due to inconsistent or limited or lack of procedure‐specific evidence and/or concerns of side‐effects (Table 2). For example, intra‐operative dexmedetomidine infusion has been shown to provide improved postoperative pain relief; however, it is not recommended because its benefits on top of basic analgesia remain unknown, and due to concerns of side‐effects including hypotension and bradycardia which can be prolonged and might impede ambulation [157]. Similarly, although, a sub‐anaesthetic dose of i.v. ketamine has demonstrated positive effects on postoperative pain scores [158], it is not recommended because its benefits over basic analgesia are unknown, and concerns of side‐effects such as hallucinations that might impair the recollection of the birth experience and mother‐child bonding [158, 159].
Table 2.
Analgesic interventions that are not recommended for pain management in patients undergoing elective caesarean section.
| Intervention | Reason for not recommending | |
|---|---|---|
| Pre‐operative | Gabapentinoids | Limited procedure‐specific evidence and concerns of side‐effects |
| Intra‐operative | Intravenous ketamine | Limited procedure‐specific evidence and concerns of side‐effects |
| Intravenous dexmedetomidine | Limited procedure‐specific evidence and concerns of side‐effects | |
| Intravenous tramadol and butorphanol | Limited procedure‐specific evidence | |
| Neuraxial clonidine | Inconsistent procedure‐specific evidence and concerns of side‐effects | |
| Neuraxial dexmedetomidine | Inconsistent procedure‐specific evidence and concerns for side‐effects | |
| Intrathecal buprenorphine | Limited procedure‐specific evidence | |
| Epidural hydromorphone | Limited procedure‐specific evidence | |
| Intrathecal midazolam | Limited procedure‐specific evidence and concerns of side‐effects | |
| Intrathecal neostigmine | Concerns of side‐effects | |
| Intrathecal ketamine | Limited procedure‐specific evidence and concerns of side‐effects | |
| Intraperitoneal local anaesthetic | Lack of procedure‐specific evidence | |
| Topical skin analgesia | Lack of procedure‐specific evidence | |
| Clonidine added to TAP | Lack of procedure‐specific evidence | |
| Dexmedetomidine added to TAP | Limited procedure‐specific evidence | |
| Fentanyl added to TAP | Lack of procedure‐specific evidence | |
| Rectus sheath block | Lack of procedure‐specific evidence | |
| Field block | Lack of procedure‐specific evidence | |
| Music | Limited procedure‐specific evidence | |
| Postoperative | Skin‐to‐skin contact | Limited procedure‐specific evidence |
| Intravenous lidocaine | Lack of procedure‐specific evidence | |
| Patient controlled epidural analgesia | Limited procedure‐specific evidence and concerns of side‐effects | |
| Surgical technique | Method of incision: diathermy | Inconsistent procedure‐specific evidence |
| Absence of a bladder flap | Limited procedure‐specific evidence | |
| Blunt fascial opening | Limited procedure‐specific evidence | |
| Uterine exteriorisation | Inconsistent procedure‐specific evidence | |
| Skin incision lasering postoperatively | Limited procedure‐specific evidence | |
| Type of skin closure | Lack of procedure‐specific evidence | |
| Vaginal cleansing | Lack of procedure‐specific evidence | |
| Cervical dilation | Inconsistent procedure‐specific evidence | |
| Type of pyramidalis muscle dissection | Lack of procedure‐specific evidence | |
| Rectus muscle re‐approximation | Limited procedure‐specific evidence |
TAP, transversus abdominis plane block.
Intrathecal or epidural administration of buprenorphine, hydromorphone, midazolam, ɑ2‐adrenergic agonists, neostigmine and ketamine has been reported to prolong the analgesic duration of morphine. However, they cannot be recommended due to inconsistent procedure‐specific evidence and due to the potential side‐effects such as hypotension or sedation. Additionally, in most studies, hypotension occurs as frequently as sedation. Peritoneal instillation of local anaesthetics cannot be recommended due to a lack of procedure‐specific evidence. Similarly, topical local anaesthetic cream application is not recommended due to a lack of procedure‐specific evidence.
The limitations of this review are related to those of the included studies. There was considerable heterogeneity between studies with regard to dosing regimens and route of administration as well as the timing of pain assessments. The small size of most studies makes it impossible to draw conclusions about the safety profile of an individual intervention. In the majority of included studies, the analgesic intervention was not evaluated against an optimised multimodal analgesic regimen. Moreover, measuring just pain scores and/or opioid consumption is not sufficient and more comprehensive, patient‐centred tools to assess pain relief and functionality would better reflect day‐to‐day clinical practice but are unfortunately poorly reported in the literature. Also, because most studies include healthy, full‐term parturients, our recommendations may not be applicable to parturients with co‐existing medical conditions such as morbid obesity, chronic pain as well as preterm delivery. Furthermore, the PROSPECT methodology uses a minimal clinically important difference in pain scores of 1/10. However, this difference has never been validated in obstetric patients.
Future adequately powered studies should assess the effects of analgesic interventions not only on pain, opioid consumption, opioid‐related adverse events and complications associated with the intervention, but also outcome measures such as time to ambulation, hospital stay and the occurrence of chronic pain or chronic opioid consumption. Furthermore, it is necessary to examine the influence of analgesic interventions on patient‐reported outcomes such as mother‐child bonding, breast feeding ability, time to ambulation and return to activities of daily living. Validated scoring tools such as the quality of recovery‐11 are useful metrics that should be considered.
In summary, this review has identified an analgesic regimen that can be used for optimal pain management after elective caesarean section performed under neuraxial anaesthesia. A combination of basic analgesics such as paracetamol; NSAIDs or cyclo‐oxygenase‐2–selective inhibitors; and i.v. dexamethasone, along with a local/regional analgesic techniques (e.g. intrathecal morphine 50–100 µg or diamorphine 300 µg); local anaesthetic infiltration with or without a field blocks such as ilio‐inguinal and iliohypogastric nerves blocks or fascial plane blocks (e.g. TAP, quadratus lumborum or ESP blocks) are recommended. However, the benefits of local and regional analgesic techniques are not apparent with the use of intrathecal morphine or diamorphine. Analgesic adjuncts such as listening to music via headphones and transcutaneous electrical nerve stimulation may be used when available. Several aspects of the surgical technique clearly yield positive analgesic effects after caesarean section including the Joel‐Cohen incision, non‐closure of the peritoneum and the use of abdominal binders. The PROSPECT recommendation for postoperative analgesia after caesarean section has established a multimodal pre‐, intra‐ and postoperative analgesic strategy which combined with certain surgical approaches and adjuvant techniques may provide excellent analgesia.
Supporting information
Table S1. Quality assessment and level of evidence assigned to the randomised trials included in the review for analgesia after caesarean section.
Table S2. Summary of key results from studies evaluating systemic analgesics, analgesics adjuncts, regional anaesthesia and surgical procedures used to support the recommended interventions in patients after caesarean section.
Table S3. Summary of key results from studies evaluating systemic analgesics, analgesics adjuncts, regional anaesthesia and surgical procedures used to support the interventions that are not recommended in patients undergoing caesarean section.
Acknowledgements
This PROSPECT recommendation is supported by the Obstetric Anaesthetists’ Association. PROSPECT is supported by an unrestricted grant from the European Society of Regional Anaesthesia and Pain Therapy. In the past, PROSPECT has received unrestricted grants from Pfizer Inc. New York, NY, USA and Grunenthal, Aachen, Germany. GJ has received honoraria from Baxter and Pacira Pharmaceuticals. MVdV has received honoraria from Sintetica, Grunenthal, Vifor Pharma, MSD, Nordic Pharma, Janssen Pharmaceuticals, Heron Therapeutics and Aquettant. EP‐Z has received honoraria from Mundipharma, Grunenthal, MSD, Janssen‐Cilag GmbH, Fresenius Kabi and AcelRx. No other external funding or competing interests declared.
Appendix 1.
PROSPECT Working Group
G. P. Joshi, E. Pogatzki‐Zahn, M. Van de Velde, S. Schug, H. Kehlet, F. Bonnet, N. Rawal, A. Delbos, P. Lavand’homme, H. Beloeil, J. Raeder, A. Sauter, E. Albrecht, P. Lirk, D. Lobo, S. Freys.
This article is accompanied by an editorial by Landau and Richebé, Anaesthesia 2021; 76: 587–9.
Contributor Information
M. Van de Velde, Email: marc.vandevelde@uzleuven.be, @MarcVandeVelde6.
the PROSPECT Working Group* of the European Society of Regional Anaesthesia and Pain Therapy and supported by the Obstetric Anaesthetists’ Association:
G. P. Joshi, E. Pogatzki‐Zahn, M. Van de Velde, S Schug, H Kehlet, F Bonnet, N Rawal, A Delbos, P. Lavand’homme, H Beloeil, J Raeder, A Sauter, E Albrecht, P Lirk, D Lobo, and S Freys
References
- 1. Gamez BH, Habib AS. Predicting severity of acute pain after Cesarean delivery: a narrative review. Anesthesia and Analgesia 2018; 126: 1606–14. [DOI] [PubMed] [Google Scholar]
- 2. Kainu JP, Sarvela J, Tiippana E, Halmesmaki E, Korttila KT. Persistent pain after caesarean section and vaginal birth: a cohort study. International Journal of Obstetric Anesthesia 2010; 19: 4–9. [DOI] [PubMed] [Google Scholar]
- 3. PROSPECT . Recommendations for postoperative analgesia after caesarean section 2014. www.postoppain.org (accessed 04/11/2020).
- 4. Huang J, Cao C, Nelson G, Wilson RD. A review of enhanced recovery after surgery principles used for scheduled Caesarean delivery. Journal of Obstetrics and Gynecology 2019; 41: 1775–88. [DOI] [PubMed] [Google Scholar]
- 5. Joshi GP, Schug SA, Kehlet H. Procedure‐specific pain management and outcome strategies. Best Practice and Research Clinical Anaesthesiology. 2014; 28: 191–201. [DOI] [PubMed] [Google Scholar]
- 6. Lee B, Schug SA, Joshi GP, Kehlet H. Procedure‐specific pain management (PROSPECT) – an update. Best Practice and Research Clinical Anaesthesiology 2018; 32: 101–11. [DOI] [PubMed] [Google Scholar]
- 7. Joshi GP, Kehlet H. Guidelines for perioperative pain management: need for re‐evaluation. British Journal of Anaesthesia 2017; 119: 703–6. [DOI] [PubMed] [Google Scholar]
- 8. Joshi GP, Van de Velde M, Kehlet H. Development of evidence‐based recommendations for procedure‐specific pain management: procedure‐specific pain management (PROSPECT) methodology. Anaesthesia 2019; 74: 1298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Towers CV, Shelton S, van Nes J, et al. Preoperative caesarean delivery intravenous acetaminophen treatment for postoperative pain control: a randomized double‐blind placebo control trial. American Journal of Obstetrics and Gynecology 2018; 218: 353. e1–4. [DOI] [PubMed] [Google Scholar]
- 10. Mahajan L, Mittal V, Gupta R, Chhabra H, Vidhan J, Kaur A. Study to compare the effect of oral, rectal and intravenous infusion of paracetamol for postoperative analgesia in women undergoing Cesarean section under spinal anesthesia. Anesthesia Essays and Researches 2017; 11: 594–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Altenau B, Crisp CC, Devaiah CG, Lambers DS. Randomized controlled trial of intravenous acetaminophen for postcesarean delivery pain control. American Journal of Obstetrics and Gynecology 2017; 217: 362. e1–6. [DOI] [PubMed] [Google Scholar]
- 12. Bernstein J, Spitzer Y, Ohaegbulam K, Reddy S, Song J, Romanelli E, Nair S. The analgesic efficacy of IV acetaminophen for acute postoperative pain in C‐section patients: a randomized, double‐blind, placebo‐controlled study. Journal of Maternal‐Fetal and Neonatal Medicine 2020. Epub 10 March. 10.1080/14767058.2020.1735337. [DOI] [PubMed] [Google Scholar]
- 13. Zeng AM, Nami NF, Wu CL, Murphy JD. The analgesic efficacy of nonsteroidal anti‐inflammatory agents (NSAIDs) in patients undergoing cesarean deliveries, a meta‐analysis. Regional Anesthesia and Pain Medicine 2016; 41: 763–72. [DOI] [PubMed] [Google Scholar]
- 14. Mkontwana N, Novikova N. Oral analgesia for relieving post‐caesarean pain. Cochrane Database of Systematic Reviews 2015; 3: CD010450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Inthigood N, Lertbunnaphong JA. Efficacy of a single 40‐mg intravenous dose of parecoxib for postoperative pain control after elective cesarean delivery: a double‐blind randomized placebo controlled trial. Journal of Obstetrics and Gynecology Research 2017; 43: 92–9. [DOI] [PubMed] [Google Scholar]
- 16. Mahdavi A, Telkabadi Z, Aleyasin A, Hosseini MA, Safdarian L, Momenzadeh A. Comparison of morphine suppository and diclofenac suppository for pain management after elective caesarean section. Acta Medicine Iran 2016; 54: 709–12. [PubMed] [Google Scholar]
- 17. Thippeswamy T, Krishnaswamy B, Begalorkar GM, Mariyappa N. Comparison of efficiacy and safety of intramuscular piroxicam and tramadol for postoperative pain in patients undergoing Caesarean delivery. Journal of Clinical and Diagnostic Research 2016; 10: FC01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khezri MB, Mosallaei MA, Ebtehaj M, Mohammadi N. Comparison of preemptive effect of ketorolac versus meperidine on postoperative shivering and pain in patients undergoing caesarean section under spinal anesthesia: a prospective, randomized, double‐blind study. Caspian Journal Internal Medicine 2018; 9: 151–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Olajetu SO, Adenekan AT, Olufolabi AJ, et al. Pentazocine versus pentazocine with rectal diclofenac for postoperative pain relief after caesarean section – a double blind randomized placebo controlled trial in a low resource area. Middle East Journal of Anesthesia 2016; 23: 443–8. [PubMed] [Google Scholar]
- 20. Monks DT, Hoppe DW, Downey K, Shah V, Bernstein P, Carvalho JCA. A perioperative course of gabapentin does not produce a clinically meaningful improvement in analgesia after caesarean delivery. Anesthesiology 2015; 123: 320–6. [DOI] [PubMed] [Google Scholar]
- 21. El Kenany S, El Tahan MR. Effect of preoperative pregabalin on post‐caesarean delivery analgesia: a dose‐response study. International Journal of Obstetric Anesthesia 2016; 26: 24–31. [DOI] [PubMed] [Google Scholar]
- 22. Najafi Anaraki A, Mirzaei K. The effect of gabapentin versus intrathecal fentanyl on postoperative pain and morphine consumption in caesarean delivery: a prospective, randomized, double‐blind study. Archives Gynecology and Obstetrics 2014; 290: 47–52. [DOI] [PubMed] [Google Scholar]
- 23. Khezri MB, Nasseh N, Soltanian G. The comparative preemptive analgesic efficacy of addition of vitamin B complex to gabapentin versus gabapentin alone in women undergoing cesarean section under spinal anesthesia: a prospective randomized double‐blind study. Medicine 2017; 96: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Felder L, Saccone G, Scuotto S, et al. Perioperative gabapentin and post cesarean pain control: a systematic review and meta‐analysis of randomized controlled trials. European Journal of Obstetrics and Gynecology and Reproductive Biology 2019; 233: 98–106. [DOI] [PubMed] [Google Scholar]
- 25. Habibi A, Alipour A, Baradari AG, Gholinataj A, Habibi MR, Peivandi S. The effect of adding lidocaine to patient controlled analgesia with morphine on pain intensity after caesarean section with spinal anaesthesia: a double‐blind, randomized, clinical trial. Open Access Macedonian Journal of Medical Sciences 2019; 7: 1946–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rahmanian M, Leysi M, Hemmati AA, Mirmohammadkhani M. The effect of low‐dose intravenous ketamine on postoperative pain following Cesarean section with spinal anesthesia: a randomized clinical trial. Oman Medical Journal 2015; 30: 11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang J, Xu Z, Feng Z, Ma R, Zhang X. Impact of ketamine on pain management in Cesarean section: A systematic review and meta‐analysis. Pain Physician 2020; 23: 135–48. [PubMed] [Google Scholar]
- 28. Nie Y, Tu W, Shen X, et al. Dexmedetomidine added to sufentanil patient‐controlled intravenous analgesia relieves the postoperative pain after cesarean delivery: a prospective randomized controlled multicenter study. Nature Scientific Reports 2018; 8: 9952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shalu PS, Ghodki PS. To study the efficacy of intravenous dexamethasone in prolonging the duration of spinal anesthesia in elective cesarean section. Anesthesia Essays and Researches 2017; 11: 321–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ituk U, Thenuwara K. The effect of a single intraoperative dose of intravenous dexamethasone 8 mg on post‐cesarean delivery analgesia: a randomized controlled trial. International Journal of Obstetric Anesthesia 2018; 35: 57–63. [DOI] [PubMed] [Google Scholar]
- 31. Maged AM, Deeb WS, Elbaradie S, et al. Comparison of local and intravenous dexamethasone on postoperative pain and recovery after caesarean section. a randomized controlled trial. Taianese Journal of. Obstetrics and Gynecology 2018; 57: 346–50. [DOI] [PubMed] [Google Scholar]
- 32. Edomwonyi NP, Osazuwa MO, Iribhogbe OI, Esangbedo SE. Postoperative analgesia using bupivacaine wound infiltration with intravenous tramadol or dexamethasone following obstetric spinal anaesthesia. Nigerian Journal of Clinical Practice 2019; 20: 1584–9. [DOI] [PubMed] [Google Scholar]
- 33. Niklasson B, Arnelo C, Georgsson Ohman S, Segerdahl M, Blanck A. Oral oxycodone for pain after caesarean section: a randomized comparison with nurse administered IV morphine in a pragmatic study. Scandinavian Journal of Pain 2015; 7: 17–24. [DOI] [PubMed] [Google Scholar]
- 34. Chi X, Li M, Mei W, Liao M. Comparison of patient‐controlled intravenous analgesia with sufentanil versus tramadol in post‐cesarean section pain management and lactation after general anesthesia – a prospective, randomized, double‐blind, controlled study. Journal of Pain Research 2017; 10: 1521–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nie JJ, Sun S, Huang SQ. Effect of oxycodone patient‐controlled intravenous analgesia after cesarean section: a randomized controlled study. Journal of Pain Research 2017; 10: 2649–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhu J, Xu C, Wang X, Shi W. Comparison of the analgesic effects of dezocine, tramadol and butorphanol after cesarean section. Pakistanian Journal of Pharmacological Sciences 2018; 31: 2191–5. [PubMed] [Google Scholar]
- 37. Cai Q, Gong H, Fan M, Chen W, Cai L. The analgesic effect of tramadol combined with buorphanol on uterine cramping pain after repeat caesarean section: a randomized, controlled, double‐blind study. Journal of Anesthesia 2020; 34: 825–33. [DOI] [PubMed] [Google Scholar]
- 38. Duan G, Bao X, Yang G, et al. Patient‐controlled intravenous tramadol versus patient‐controlled intravenous hydromorphone for analgesia after secondary cesarean delivery: a randomized controlled trial to compare analgesic, anti‐anxiety and anti‐depression effects. Journal of Pain Research 2019; 12: 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ffrench‐O’Carroll R, Steinhaeuser H, Duff S, et al. A randomized controlled trial comparing tapentadol with oxycodone in non‐breastfeeding women post‐elective cesarean section. Current Medical Research and Opinion 2019; 35: 975–81. [DOI] [PubMed] [Google Scholar]
- 40. Makela K, Palomaki O, Pokkinen S, Yli‐Hankala A, Helminen M, Uotila J. Oral versus patient‐controlled intravenous administration of oxycodone for pain relief after cesarean section. Archives of Gynecology and Obstetrics 2019; 300: 903–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sultan P, Halpern SH, Pushpanathan E, Patel S, Carvalho B. The effect of intrathecal morphine dose on outcomes after elective Cesarean delivery: a meta‐analysis. Anesthesia and Analgesia 2016; 123: 154–64. [DOI] [PubMed] [Google Scholar]
- 42. Berger JS, Gonzalez A, Hopkins A, et al. Dose‐response of intrathecal morphine when administered with intravenous ketorolac for post‐cesarean analgesia: a two‐center, prospective, randomized, blinded trial. International Journal of Obstetric Anesthesia 2016; 28: 3–11. [DOI] [PubMed] [Google Scholar]
- 43. Booth JL, Harris LC, Eisenach JC, Pan PH. A randomized controlled trial comparing two multimodal analgesic techniques in patients predicted to have severe pain after Cesarean delivery. Anesthesia and Analgesia 2016; 122: 1114–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kaufner L, Heimann S, Zander D, et al. Neuraxial anesthesia for pain control after cesarean section: a prospective randomized trial comparing three different neuraxial techniques in clinical practice. Minerva Anestesiologica 2015; 82: 514–24. [PubMed] [Google Scholar]
- 45. Carvalho B, Sutton CD, Kowalczyk JJ, Flood PD. Impact of patient choice for different analgesic protocols on opioid consumption: a randomized prospective trial. Regional Anesthesia and Pain Medicine 2019; 44: 578–85. [DOI] [PubMed] [Google Scholar]
- 46. Carvalho B, Mirza F, Flood P. Patient choice compared with no choice of intrathecal morphine dose for caesarean analgesia: a randomized clinical trial. British Journal of Anaesthesia 2017; 118: 762–71. [DOI] [PubMed] [Google Scholar]
- 47. Sharpe EE, Molitor RJ, Arendt KW, et al. Intrathecal morphine versus intrathecal hydromorphone for analgesia after caesarean delivery. Anesthesiology 2020; 132: 1382–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Allen TK, Mishriky BM, Klinger RY, Habib AS. The impact of neuraxial clonidine on postoperative analgesia and perioperative adverse effects in women having elective Caesarean section – a systematic review and meta‐analysis. British Journal of Anaesthesia 2018; 120: 228–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Fernandes HS, Bliancheriene F, Vago TM, et al. Clonidine effect on pain after Cesarean delivery: a randomized controlled trial of different routes of administration. Anesthesia and Analgesia 2018; 127: 165–70. [DOI] [PubMed] [Google Scholar]
- 50. Carvalho FAE, Tenorio SB, Shiohara FT, Maria LR, Mota A. Randomized study of postcesarean analgesia with intrathecal morphine alone or combined with clonidine. Journal of Clinical Anesthesia 2016; 33: 395–402. [DOI] [PubMed] [Google Scholar]
- 51. Khezri MB, Rezaei M, Reihany MD, Javadi EHS. Comparison of postoperative analgesic effect of intrathecal clonidine and fentanyl added to bupivacaine in patients undergoing Cesarean section: a prospective randomized double‐blind study. Pain Research and Treatment 2014; 2014: 513628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Yousef AA, Salem HA, Moustafa MZ. Effect of mini‐dose epidural dexmedetomidine in elective cesarean section using combined spinal‐epidural anesthesia: a randomized double‐blind controlled study. Journal of Anesthesia 2015; 29: 708–14. [DOI] [PubMed] [Google Scholar]
- 53. Qi X, Chen D, Li G, et al. Comparison of intrathecal dexmedetomidine with morphine as adjuvants in Cesarean sections. Biology Pharmacology Bulletin 2016; 39: 1455–60. [DOI] [PubMed] [Google Scholar]
- 54. Bi YH, Cui XG, Zhang RQ, Song CY, Zhang YZ. Low dose of dexmedetomidine as an adjuvant to bupivacaine in cesarean surgery provides better intraoperative somato‐visceral sensory block characteristics and postoperative analgesia. Oncotarget 2017; 8: 63587–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bi YH, Wu JM, Zhang YZ, Zhang RQ. Effect of different doses of intrathecal dexmedetomidine as an adjuvant combined with hyperbaric ropivacaine in patients undergoing caesarean section. Frontiers in Pharmacology 2020; 11: 342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yang Y, Song C, Song C, Li C. Addition of dexmedetomidine to epidural morphine to improve anesthesie and analgesia for caesarean section. Experimental and Therapeutic Medicine 2020; 19: 1747–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mostafa MF, Herdan R, Fathy GM, et al. Intrathecal dexmedetomidine versus magnesium sulphate for postoperative analgesia and stress response after caesarean delivery: randomized controlled double‐blind study. European Journal of Pain 2020; 24: 182–91. [DOI] [PubMed] [Google Scholar]
- 58. Weigl W, Bierylo A, Wielgus M, et al. Analgesic efficacy of intrathecal fentanyl during the period of highest analgesic demand after cesarean section. Medicine 2016; 95: e3827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Weigl W, Bierylo A, Wielgus M, et al. Perioperative analgesia after intrathecal fentanyl and morphine or morphine alone for cesarean section. Medicine 2017; 96: e8892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ravindran R, Sajid B, Ramadas KT, Susheela I. Intrathecal hyperbaric bupivacaine with varying doses of buprenorphine for postoperative analgesia after Cesarean section: a comparative study. Anesthesia Essays and Researches 2017; 11: 952–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Yang M, Wang L, Chen H, Tang Y, Chen X. Postoperative analgesic effects of different doses of epidural hydromorphone coadministered with ropivacaine after Cesarean section: a randomized controlled trial. Pain Research and Management 2019; 2019: 99054538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wang SC, Pan PT, Chiu HY, Huang CJ. Neuraxial magnesium sulfate improves postoperative analgesia in Cesarean section delivery women: a meta‐analysis of randomized controlled trials. Asian Journal of Anesthesiology 2017; 55: 56–67. [DOI] [PubMed] [Google Scholar]
- 63. Abdollahpour A, Azadi R, Bandari R, Mirmohammadkhani M. Effects of adding midazolam and sufentanil to intrathecal bupivacaine on analgesia quality and postoperative complications in elective Cesarean section. Anesthesiology and Pain Medicine 2015; 5: e23565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Dodawad R, Sumalatha GB, Pandarpurkar S, Jajee P. Intrathecal midazolam as an adjuvant in pregnancy‐induced hypertensive patients undergoing an elective Caesarean section: a clinical comparative study. Anesthesiology and Pain Medicine 2016; 6: e38550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Khezri MB, Tahaei E, Atlasbaf AH. Comparison of postoperative analgesic effect of intrathecal ketamine and fentanyl added to bupivacaine in patients undergoing cesarean section: a prospective randomized double‐blind study. Middle East Journal of Anesthesia 2016; 23: 427–36. [PubMed] [Google Scholar]
- 66. Basuni AS. Addition of low‐dose ketamine to midazolam and low‐dose bupivacaine improves hemodynamics and postoperative analgesia during spinal anesthesia for cesarean section. Journal of Anaesthesiology and Clinical Pharmacology 2016; 32: 44–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cossu AP, De Giudici LM, Piras D, et al. A systematic review of the effects of adding neostigmine to local anesthetics for neuraxial administration in obstetric anesthesia and analgesia. International Journal of Obstetric Anesthesia 2015; 24: 237–46. [DOI] [PubMed] [Google Scholar]
- 68. Hussien RM, Rabie AH. Sequential intrathecal injection of fentanyl and hyperbaric bupivacaine at different rates: does it make a difference? A randomized controlled trial. Korean Journal of Anesthesiology 2019; 72: 150–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Patel R, Carvalho JCA, Downey K, Kanczuk M, Bernstein P, Siddiqui N. Intraperitoneal installation of lidocaine improves postoperative analgesia at cesarean delivery: a randomized, double‐blind, placebo‐controlled trial. Anesthesia and Analgesia 2017; 124: 554–9. [DOI] [PubMed] [Google Scholar]
- 70. Grosse‐Steffen T, Kramer M, Tuschy B, Weiss C, Sutterlin M, Berlit S. Topic anaesthesia with a eutectic mixture of lidocaine/prilocaine cream after elective caesarean section: a randomized, placebo‐controlled trial. Archives of Gynecology and Obstetrics 2017; 296: 771–6. [DOI] [PubMed] [Google Scholar]
- 71. Larsen KR, Kristensen BB, Rasmussen MA, et al. Effect of high volume systematic local infiltration analgesia in Caesarean section: a randomized, placebo‐controlled trial. Acta Anaesthesiologica Scandinavica 2015; 59: 632–9. [DOI] [PubMed] [Google Scholar]
- 72. Ghenaee MM, Rahmani S, Jafarabadi M. Local lidocaine 2% in postoperative pain management in Cesarean delivery. Journal of Family and Reproductive Health 2015; 9: 19–21. [PMC free article] [PubMed] [Google Scholar]
- 73. Nasir F, Sohail I, Sadiq H, Habib M. Local wound infiltration with ropivacaine for postoperative pain control in Caesarean section. Cureus 2019; 11: e5572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Reinikainen M, Syvaoja S, Hara K. Continuous wound infiltration with ropivacaine for analgesia after caesarean section: a randomized placebo‐controlled trial. Acta Anaesthesiologica Scandinavica 2014; 58: 973–9. [DOI] [PubMed] [Google Scholar]
- 75. Jolly C, Jathières F, Keita H, Jaouen E, Guyot B, Torre A. Cesarean analgesia using levobupivacaine continuous wound infiltration: a randomized trial. European Journal of Obstetrics and Gynecology and Reproductive Biology 2015; 194: 125–30. [DOI] [PubMed] [Google Scholar]
- 76. Lalmand M, Wilwerth M, Fils JF, Van der Linden P. Continuous ropivacaine subfascial wound infusion compared with intrathecal morphine for postcesarean analgesia: a prospective, randomized controlled double‐blind study. Anesthesia and Analgesia 2017; 125: 907–12. [DOI] [PubMed] [Google Scholar]
- 77. Adesope O, Ituk U, Habib AS. Local anaesthetic wound infiltration for postcaesarean section analgesia. European Journal of Anaesthesiology 2016; 33: 731–42. [DOI] [PubMed] [Google Scholar]
- 78. Thomas D, Panneerselvam S, Kundra P, Rudingwa P, Sivakumar RK, Dorairajan G. Continuous wound infiltration of bupivacaine at two different anatomical planes for caesarean analgesia – a randomized clinical trial. Indian Journal of Anaesthesia 2019; 63: 437–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Wagner‐Kovacec J, Povalej‐Brzan P, Mekis D. Efficacy of continuous in‐wound infusion of levobupivacaine and ketorolac for post‐caesarean section analgesia: a prospective, randomized, double‐blind, placebo‐controlled trial. BMC Anesthesiology 2018; 18: 165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Barney EZ, Pedro CD, Gamez BH, Fuller ME, Dominguez JE, Habib AS. Ropivacaine and ketorolac wound infusion for post‐cesarean delivery analgesia. Obstetrics and Gynecology 2020; 135: 427–35. [DOI] [PubMed] [Google Scholar]
- 81. Kundra S, Singh RM, Singh G, Singh T, Jarewal V, Katyal S. Efficacy of magnesium sulphate as an adjunct to ropivacaine in local infiltration for postoperative pain following lower segment caesarean section. Journal of Clinical and Diagnostic Research 2016; 10: UC18–UC22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Bhardwaj S, Devgan S, Sood D, Katyal S. Comparison of local wound infiltration with ropivacaine alone or ropivacaine plus dexmedetomidine for postoperative pain relief after lower segment cesarean section. Anesthesia Essays and Researches 2017; 11: 940–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Liu MW, Li TKT, Lui F, Ong CYT. A randomized, controlled trial of rectus sheath bupivacaine and intrathecal morphine, vs intrathecal bupivacaine and morphine after Caesarean section. Anaesthesia 2017; 72: 1225–9. [DOI] [PubMed] [Google Scholar]
- 84. Triyasunant N, Chinachoti T, Duangburong S. Direct field block with 40 mL of 0.125% bupivacaine in conjunction with intrathecal morphine for analgesia after Cesarean section: a randomized controlled trial. Journal of the Medical Association of Thailand 2015; 98: 1001–9. [PubMed] [Google Scholar]
- 85. McKeen DM, George RB, Boyd JC, Allen VM, Pink A. Transversus abdominis plane block does not improve early or late pain outcomes after Cesarean delivery: a randomized controlled trial. Canadian Journal of Anesthesia 2014; 61: 631–40. [DOI] [PubMed] [Google Scholar]
- 86. Fusco P, Cofini V, Petrucci E, et al. Transversus abdominis plane block in the management of acute postoperative pain syndrome after Caesarean section: a randomized controlled clinical trial. Pain Physician 2016; 19: 583–91. [PubMed] [Google Scholar]
- 87. Jadon A, Jain P, Chakraborty S, et al. Role of ultrasound guided transversus abdominis plane block as a component of multimodal analgesic regimen for lower segment caesarean section: a randomized double blind clinical study. BMC Anesthesiology 2018; 18: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Kupiec A, Zwierzchowski J, Kowal‐Janicka J, et al. The analgesic efficiency of transversus abdominis plane (TAP)block after caesarean section. Ginekologia Polska 2018; 89: 420–3. [DOI] [PubMed] [Google Scholar]
- 89. Kakade A, Wagh G. Evaluate the feasibility of surgical transversus abdominis plane block for postoperative analgesia after Cesarean section. Journal of Obstetrics and Gynecology of India 2019; 69: 330–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Faiz SHR, Alebouyeh MR, Derakhshan P, Imani F, Rahimzadeh P, Ashtiani MG. Comparison of ultrasound‐guided posterior transversus abdominis plane block and lateral transversus plane block for postoperative pain management in patients undergoing caesarean section: a randomized double‐blind clinical trial. Journal of Pain Research 2017; 11: 5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Narasimhulu DM, Scharfman L, Minkoff H, George B, Homel P, Tyagaraj K. A randomized trial comparing surgeon‐administered intraoperative transversus abdominis plane block with anesthesiologist‐administered transcutaneous block. International Journal of Obstetric Anesthesia 2018; 35: 26–32. [DOI] [PubMed] [Google Scholar]
- 92. Gupta A, Gupta A, Yadav N. Effect of dexamethasone as an adjuvant to ropivacaine on duration and quality of analgesia in ultrasound‐guided transversus abdominis plane block in patients undergoing lower segment cesarean section – a prospective, randomized, single‐blinded study. Indian Journal of Anaesthesia 2019; 63: 469–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. John R, Ranjan RV, Ramachandran TR, George SK. Analgesic efficacy of transverse abdominal plane block after elective cesarean delivery – bupivacaine with fentanyl versus bupivacaine alone: a randomized, double‐blind controlled clinical trial. Anesthesia Essays and Researches 2017; 11: 181–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Singh R, Kumar N, Jain A, Joy S. Addition of clonidine to bupivacaine in transversus abdominis plane block prolongs postoperative analgesia after cesarean section. Journal of Anaesthesiology Clinical Pharmacology 2016; 32: 501–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Acharya R, Baksi R, Mohapatra P. Comparative analysis of duration of postoperative analgesia between levobupivacaine and levobupivacaine with clonidine after ultrasound‐guided transversus abdominis plane block in patients undergoing lower segment cesarean section. Anesthesia Essays and Researches 2018; 12: 943–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Parameswari AR, Udayakumar P. Comparison of efficacy of bupivacaine with dexmedetomidine versus bupivacaine alone for transversus abdominis plane block for postoperative analgesia in patients undergoing elective caesarean section. Journal of Obstetrics and Gynecology of India 2018; 62: 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Canakci E, Gultekin A, Cebeci Z, Hanedan B, Kilinc A. The analgesic efficacy of transverse abdominis plane block versus epidural block after caesarean delivery: Which one is effective ? TAP block ? Epidural block ? Pain Research and Management 2018; 2018: 3562701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Jarraya A, Zghal J, Abidi S, Smaoui M, Kolsi K. Subarachnoid morphine versus TAP blocks for enhanced recovery after caesarean section delivery: a randomized controlled trial. Anaesthesia, Critical Care and Pain Medicine 2016; 35: 401–3. [DOI] [PubMed] [Google Scholar]
- 99. Dereu D, Savoldelli GL, Mercier Y, Combescure C, Mathivon S, Rehberg B. The impact of a transversus abdominis plane block including clonidine vs intrathecal morphine on nausea and vomiting after caesarean section. European Journal of Anaesthesiology 2019; 36: 575–82. [DOI] [PubMed] [Google Scholar]
- 100. Kwikiriza A, Kiwanuka JK, Firth PG, Hoeft MA, Modest VE, Ttendo SS. The analgesic effects of intrathecal morphine in comparison with ultrasound‐guided transversus abdominis plane block after caesarean section: a randomized controlled trial at a Ugandan regional referral hospital. Anaesthesia 2019; 74: 167–73. [DOI] [PubMed] [Google Scholar]
- 101. Telnes A, Skogvoll E, Lonnée H. Transversus abdominis plane block vs wound infiltration in Caesarean section: a randomized controlled trial. Acta Anaesthesiologica Scandinavica 2015; 59: 496–504. [DOI] [PubMed] [Google Scholar]
- 102. Klasen F, Bourgoin A, Antonini F, et al. Postoperative analgesia after caesarean section with transversus abdominis plane block or continuous infiltration wound catheter: A randomized clinical trial. TAP vs infiltration after caesarean section. Anaesthesiology, Critical Care and Pain Medicine 2016; 35: 411–6. [DOI] [PubMed] [Google Scholar]
- 103. Tawfik MM, Mohamed YM, Elbadrawi RE, Abdelkhalek M, Mogadeh MM, Ezz HM. Transversus abdomionis plane block versus wound infiltration for analgesia after cesarean delivery: a randomized controlled trial. Anesthesia and Analgesia 2017; 124: 1291–7. [DOI] [PubMed] [Google Scholar]
- 104. Fusco P, Scimia P, Paladini G, et al. Transversus abdominis plane block for analgesia after Cesarean delivery. A systematic review. Minerva Anestesiologica 2015; 81: 195–204. [PubMed] [Google Scholar]
- 105. Champaneria R, Shah L, Wilson MJ, Daniels JP. Clinical effectiveness of transversus abdominis plane (TAP) blocks for pain relief after caesarean section: a meta‐analysis. International Journal of Obstetric Anesthesia 2016; 28: 45–60. [DOI] [PubMed] [Google Scholar]
- 106. Ng SC, Habib AS, Sodha S, Carvalho B, Sultan P. High‐dose versus low‐dose local anaesthetic for transversus abdominis plane block post‐Caesarean delivery analgesia: a meta‐analysis. British Journal of Anaesthesia 2018; 120: 252–63. [DOI] [PubMed] [Google Scholar]
- 107. Staker JJ, Liu D, Church R, et al. a triple‐blind, placebo‐controlled randomized trial of the ilioinguinal‐transversus abdominis plane (I‐TAP) nerve block for elective caesarean section. Anaesthesia 2018; 73: 594–602. [DOI] [PubMed] [Google Scholar]
- 108. Qian H, Zhang Q, Zhu P, et al. Ultrasound‐guided transversus abdominis plane block using ropivacaine and dexmedetomidine in patients undergoing caesarean sections to relieve post‐operative analgesia: a randomized controlled clinical trial. Experimental and Therapeutic Medicine 2020; 20: 1163–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Blanco R, Ansari T, Girgis E. Quadratus lumborum block for postoperative pain after caesarean section. European Journal of Anaesthesiology 2015; 32: 812–8. [DOI] [PubMed] [Google Scholar]
- 110. Krohg A, Ullensvang K, Rosseland LA, Langesaeter E, Sauter AR. The analgesic effect of ultrasound‐guided quadratus lumborum block after Cesarean delivery: a randomized clinical trial. Anesthesia and Analgesia 2018; 126: 559–65. [DOI] [PubMed] [Google Scholar]
- 111. Hansen CK, Dam M, Steingrimsdottir GE, et al. Ultrasound‐guided transmuscular quadratus lumborum block for elective cesarean section significantly reduces postoperative opioid request: a double‐blind randomized trial. Regional Anesthesia and Pain Medicine 2019; 44: 896–900. [DOI] [PubMed] [Google Scholar]
- 112. Mieszkowski MM, Mayzner‐Zawadzka E, Tuyakov B, et al. Evaluation of the effectiveness of the quadratus lumborum block type I using ropivacaine in postoperative analgesia after a cesarean section – a controlled clinical study. Ginekologie Polska 2018; 89: 89–96. [DOI] [PubMed] [Google Scholar]
- 113. Blanco R, Ansari T, Riad W, Shetty N. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery. Regional Anesthesia and Pain Medicine 2016; 41: 757–62. [DOI] [PubMed] [Google Scholar]
- 114. Verma K, Malawat A, Jethava D, Jethava DD. Comparison of transversus abdominis plane block and quadratus lumborum block for post‐caesarean section analgesia: a randomized clinical trial. Indian Journal of Anaesthesia 2019; 63: 820–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Kang W, Lu D, Yang X, et al. Postoperative analgesic effects of various quadratus lumborum block approaches following cesarean section: a randomized controlled trial. Journal of Pain Research 2019; 12: 2305–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Tamura T, Yokota S, Ando M, Kubo Y, Nishiwaki K. A triple‐blinded randomized trial comparing spinal morphine with posterior quadratus lumborum block after cesarean section. International Journal of Obstetric Anesthesia 2019; 40: 32–8. [DOI] [PubMed] [Google Scholar]
- 117. Salama ER. Ultrasound‐guided bilateral quadratus lumborum block vs. intrathecal morphine for postoperative analgesia after caesarean section: a randomized controlled trial. Korean Journal of Anesthesiology 2020; 73: 121–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Yoshida K, Tanaka S, Watanabe K, Obara S, Murakawa M. The effectiveness of the intramuscular quadratus lumborum block in postoperative analgesia after caesarean section with vertical incision: a randomized, double‐blind placebo‐controlled study. Journal of Anesthesia 2020; 34: 849–56. [DOI] [PubMed] [Google Scholar]
- 119. Irwin R, Stanescu S, Buzaianu C, Rademan M, Roddy J, Gormley C, Tan T. Quadratus lumborum block for analgesia after caesarean section: a randomised controlled trial. Anaesthesia 2020; 75: 89–95. [DOI] [PubMed] [Google Scholar]
- 120. Sultan P, Patel SD, Jadin S, Carvalho B, Halpern SH. Transversus abdominis plane block compared with wound infiltration for postoperative analgesia following Cesarean delivery: a systematic review and network meta‐analysis. Canadian Journal of Anesthesia 2020; 67: 1710‐27. [DOI] [PubMed] [Google Scholar]
- 121. El‐Boghdadly K, Desai N, Halpern S, et al. Quadratus lumborum block versus transversus abdominis plane block for caesarean delivery: a systematic review and network meta‐analysis. Anaesthesia 2020. Epub 4 July. 10.1111/anae.15160. [DOI] [PubMed] [Google Scholar]
- 122. Boules ML, Goda AS, Abdelhady MA, Abu El‐Nour Abd El‐Azeem SA, Hamed MA. Comparison of analgesic effect between erector spinae plane block and transversus abdominis plane block after elective caesarean section: a prospective randomized single‐blind controlled study. Journal of Pain Research 2020; 13: 1073–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Hamed MA, Yassin HM, Botros JM, Abdelhady MA. Analgesic efficacy of erector spinae plane block compared with intrathecal morphine after elective caesarean section: a prospective randomized controlled study. Journal of Pain Research 2020; 13: 597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Sato I, Iwasaki H, Luthe SK, Lida T, Kanda H. Comparison of intrathecal morphine with continuous patient‐controlled epidural anesthesia versus intrathecal morphine alone for post‐cesarean section analgesia: a randomized controlled trial. BMC Anesthesiology 2020; 20: 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Chen SY, Liu FL, Cherng YG, et al. Patient‐controlled epidural levobupivacaine with or without fentanyl for post‐cesarean section pain relief. Biomedical Research International 2014; 965152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Khooshideh M, Rostami SSL, Sheikh M, Yekta BG, Shahriari A. Pulsed electromagnetic fields for postsurgical pain management in women undergoing cesarean section. A randomized, double‐blind, placebo‐controlled trial. Clinical Journal of Pain 2017; 33: 142–7. [DOI] [PubMed] [Google Scholar]
- 127. Chakravarthy M, Prashanth A, George A. Evaluation of percutaneous electrical nerve stimulation of the auricle for relief of postoperative pain following cesarean section. Medical Acupuncture 2019; 31: 281–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Bonnal A, Dehon A, Nagot N, Macioce V, Nogue E, Moreau E. Patient‐controlled oral analgesia versus nurse‐controlled parenteral analgesia after caesarean section: a randomized controlled trial. Anaesthesia 2016; 71: 535–43. [DOI] [PubMed] [Google Scholar]
- 129. Yefet E, Taha H, Salim R, et al. Fixed time interval compared with on‐demand oral analgesia protocols for post‐caesarean pain: a randomized controlled trial. British Journal of Obstetrics and Gynaecology 2017; 124: 1063–70. [DOI] [PubMed] [Google Scholar]
- 130. Farzaneh M, Abbasijahromi A, Saadatmand V, et al. Comparative effect of nature‐based sounds intervention and headphones intervention on pain severity after Cesarean section: a prospective double‐blind randomized trial. Anesthesiology and Pain Medicine 2019; 9: e67835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Kollmann M, Adrian L, Scheuchenegger A, et al. Early skin‐to‐skin contact after cesarean section: a randomized clinical pilot study. PLoS One 2017; 12: e0168783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Ghana S, Hakimi S, Mirghafourvand M, Abbasalizadeh F, Behnampour N. Randomized controlled trial of abdominal binders for postoperative pain, distress and blood loss after cesarean delivery. International Journal of Gynecology and Obstetrics 2017; 137: 271–6. [DOI] [PubMed] [Google Scholar]
- 133. Gustafson JL, Dong F, Duong J, Kuhlmann ZC. Elastic abdominal binders reduce cesarean pain postoperatively: a randomized controlled pilot trial. Kansas Journal of Medicine 2018; 11: 48–53. [PMC free article] [PubMed] [Google Scholar]
- 134. Karaca I, Ozturk M, Alay I, et al. Influence of abdominal binder usage after cesarean delivery on postoperative mobilization, pain and distress: a randomized controlled trial. Eurasian Journal of Medicine 2019; 51: 214–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Sakinci M, Kuru O, Olgan S, et al. Dilatation of the cervix at non‐labour caesarean section: does it improve the patients perception of pain postoperatively? Journal of Obstetrics and Gynecology 2015; 35: 681–4. [DOI] [PubMed] [Google Scholar]
- 136. Alalfy M, Yehia A, Samy A. Routine cervical dilatation at caesarean section and its influence on postoperative pain and complications in obese women: a double blind randomized controlled trial. Journal of Maternal‐Fetal and Neonatal Medicine 2019; 2019: 1651274. [DOI] [PubMed] [Google Scholar]
- 137. Goymen A, Simsek Y, Ozdurak HI, et al. Effect of vaginal cleansing on postoperative factors in elective caesarean sections: a prospective, randomized controlled trial. Journal of Maternal‐Fetal and Neonatal Medicine 2017; 30: 442–5. [DOI] [PubMed] [Google Scholar]
- 138. Gizzo S, Andrisani A, Noventa M, et al. Caesarean section: could different transverse abdominal incision techniques influence postpartum pain and subsequent quality of life? A systematic review. PLoS One 2015; 10: e0114190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Elbohoty AEH, Gomaa MF, Abdelaleim M, Abd‐El‐Gawad M, Elmarakby M. Diathermy versus scalpel in transverse abdominal incision in women undergoing repeated cesarean section: a randomized controlled trial. Journal of Obstetrics and Gynaecology Research 2015; 41: 1541–6. [DOI] [PubMed] [Google Scholar]
- 140. Yilmaz FY, Mathyk BA, Yildiz S, Yenigul NN, Saglam C. Postoperative pain and neuropathy after caesarean operation featuring blunt or sharp opening of the fascia: a randomized parallel group double‐blind study. Journal of Obstetrics and Gynaecology 2018; 38: 933–9. [DOI] [PubMed] [Google Scholar]
- 141. Yapca OE, Topdagi YE, Ragip AA. Fetus delivery time in extraperitoneal versus transperitoneal cesarean section: a randomized trial. Journal of Maternal‐Fetal and Neonatal Medicine 2020; 33: 657–63. [DOI] [PubMed] [Google Scholar]
- 142. Akhlagi F, Khazaie A, Jafaripour F. Comparing formation or non‐formation of bladder flap at cesarean section on perioperative and postoperative complications: double‐blind clinical trial. Journal of Family and Reproductive Health 2017; 11: 152–8. [PMC free article] [PubMed] [Google Scholar]
- 143. El‐Khayat W, Elsharkawi M, Hassan A. A randomized controlled trial of uterine exteriorization versus in situ repair of the uterine incision cesarean delivery. International Journal of Gynecology and Obstetrics 2014; 127: 163–6. [DOI] [PubMed] [Google Scholar]
- 144. Zaphiratos V, George RB, Boyd JC, Habib AS. Uterine exteriorization compared with in situ repair for Cesarean delivery: a systematic review and meta‐analysis. Canadian Journal of Anesthesia 2015; 62: 1209–20. [DOI] [PubMed] [Google Scholar]
- 145. Skret‐Magierlo J, Soja P, Drozdowska A, et al. Two techniques of pyramidalis muscle dissection in Pfannenstiel incision for cesarean section. Ginekologia Polska 2015; 86: 509–13. [DOI] [PubMed] [Google Scholar]
- 146. Eken MK, Ozkaya E, Tarhan T, et al. Effects of closure versus non‐closure of the visceral and parietalperitoneum at cesarean section: does it have any effect on postoperative vital signs? A prospective randomized study. Journal of Maternal‐Fetal and Neonatal Medicine 2017; 30: 922–6. [DOI] [PubMed] [Google Scholar]
- 147. Omran EF, Meshaal H, Hassan SM, Dieb AS, Nabil H, Saad H. The effect of rectus muscle re‐approximation at cesarean delivery onpain perceived after operation: a randomized control trial. Journal of Maternal‐Fetal and Neonatal Medicine 2018; 32: 3238–43. [DOI] [PubMed] [Google Scholar]
- 148. Bamigboye AA, Hofmeyr GJ. Closure versus non‐closure of the peritoneum at caesarean section: short‐ and long‐term outcomes. Cochrane Database of Systematic Reviews 2014; 8: CD000163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Poursalehan S, Nesioonpour S, Akhondzadeh R, Mokmeli S. The effect of low‐level laser on postoperative pain after elective cesarean section. Anesthesia Pain Medicine 2018; 8: e84195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Pires de Holanda AAM, Rocha de Sena KR, da Silva M, Filho E, Pegado R. Albuquerque Barbosa Cabral Micussi MT. Low‐level laser therapy improves pain in postcesarean section: a randomized clinical trial. Lasers in Medical Science 2020; 35: 1095–102. [DOI] [PubMed] [Google Scholar]
- 151. Maged AM, Mohesen MN, Elhalwagy A, et al. Subcuticular interrupted versus continuous skin suturing in elective cesarean section in obese women: a randomized controlled trial. Journal of Maternal‐Fetal and Neonatal Medicine 2019; 32: 4114–9. [DOI] [PubMed] [Google Scholar]
- 152. Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a metaanalysis. American Journal of Obstetrics and Gynecology 2015; 212(621): e1–10. [DOI] [PubMed] [Google Scholar]
- 153. Wang H, Hong S, Teng H, Qiao L, Yin H. Subcuticular sutures versus staples for skin closure after cesarean delivery: a meta‐analysis. Journal of Maternal‐Fetal and Neonatal Medicine 2016; 29: 3705–11. [DOI] [PubMed] [Google Scholar]
- 154. Sharawi N, Carvalho B, Habib AS, Blake L, Jm M, Sultan P. A systematic review evaluating neuraxial morphine and diamorphine associated respiratory depression after Cesarean delivery. Anesthesia and Analgesia 2018; 127: 1385–95. [DOI] [PubMed] [Google Scholar]
- 155. NICE . Caesarean section. [CG132]. last updated September 2019. www.nice.org.uk/guidance/cg132/ (accessed 30/06/2020).
- 156. Cavalcante AN, Sprung J, Schroeder DR, Weingarten TN. Multimodal analgesic therapy with gabapentin and its association with postoperative respiratory depression. Anesthesia and Analgesia 2017; 125: 141–6. [DOI] [PubMed] [Google Scholar]
- 157. Grape S, Kirkham KR, Frauenknecht J, Albrecht E. Intra‐operative analgesia with remifentanil vs. dexmedetomidine: a systematic review and meta‐analysis with trial sequential analysis. Anaesthesia 2019; 74: 793–800. [DOI] [PubMed] [Google Scholar]
- 158. Bauchat JR, Higgins N, Wojciechowski KG, McCarthy RJ, Toledo P, Wong CA. Low‐dose ketamine with multimodal postcesarean delivery analgesia: a randomized controlled trial. International Journal of Obstetric Anesthesia 2011; 20: 3–9. [DOI] [PubMed] [Google Scholar]
- 159. Carvalho B, Butwick AJ. Postcesarean delivery analgesia. Best Practice and Research Clinical Anaesthesiology 2017; 31: 69–79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Quality assessment and level of evidence assigned to the randomised trials included in the review for analgesia after caesarean section.
Table S2. Summary of key results from studies evaluating systemic analgesics, analgesics adjuncts, regional anaesthesia and surgical procedures used to support the recommended interventions in patients after caesarean section.
Table S3. Summary of key results from studies evaluating systemic analgesics, analgesics adjuncts, regional anaesthesia and surgical procedures used to support the interventions that are not recommended in patients undergoing caesarean section.


